Abstract
Importance
Men with metastatic prostate cancer (mPC) who have a poor response to initial androgen deprivation therapy (ADT) as reflected by a PSA > 4 ng/ml after 7 months of ADT, have a poor prognosis, based on historical controls.
Objective
To determine the efficacy of Abiraterone acetate with prednisone (AA + P) in these high-risk patients with a suboptimal response to hormonal induction.
Design
Phase II single-arm study of 41 patients enrolled between August 9, 2011, and closure on August 1, 2013.
Setting
National Clinical Trials Network – SWOG.
Participants
Eligible patients had mPC and a PSA of > 4ng/ml between 6–12 months after starting ADT. PSA could be rising or falling at the time of enrollment, but had to be > 4 ng/ml. No previous chemotherapy or secondary hormonal therapies were allowed, except in those patients receiving a standard, first-generation anti-androgen with a falling PSA at the time of enrollment, in whom this therapy was continued.
Intervention
1000 mg of AA once daily + 5 mg of prednisone twice daily.
Main Outcome Measures
The primary endpoint was a PSA of ≤ 0.2ng/ml within 12 months of starting AA + P. A partial response (PR) was a secondary end point, defined as a PSA level reduction to lower than 4.0 ng/mL but higher than 0.2 ng/mL. Data analysis was conducted from March 21 to November 29, 2016.
Results
One patient was deemed not analyzable due to not receiving any protocol treatment. Five (13%) patients achieved a PSA of ≤ 0.2ng/ml (95% CI 4%, 27%). Thirteen (33%) additional patients achieved a partial response, with a reduction in PSA to < 4 ng/ml, but with a level of > 0.2 ng/ml. Sixteen (40%) patients had no PSA response and six (15%) were not assessable and assumed to be non-responders. The median progression-free survival (PFS) was 17.5 months (95% CI; 8.6, 25.0) and the median Overall Survival (OS) was 25.8 months (95% CI; 15.7, 25.8). There was one incident each of Grade 4 alanine aminotransferase level elevation and rectal bleeding. Eleven patients reported Grade 3 adverse events.
Conclusions and Relevance
This study did not reach its prescribed level of 6 PSA responses of ≤0.2ng/ml, although 5 responses were observed. The OS and PFS observed in this trial are encouraging compared to historical controls. The therapy was generally well tolerated, without any clear signal of any unexpected toxicity.
Trial Registration
Introduction
The natural history of metastatic, hormone-naïve prostate cancer is variable. Those men with a suboptimal or incomplete response to initial hormone induction therapy fare poorly with a short overall survival. Although recent reports1,2 have described a role for upfront docetaxel chemotherapy combined with androgen deprivation therapy (ADT) for metastatic, hormone-sensitive prostate cancer, the use of next generation androgen therapy, such as abiraterone acetate + prednisone (AA + P), is not well studied in this setting. S1014 examines the role of AA + P in men with an inadequate response to hormone induction therapy in this setting.
SWOG trial 9346 tested the use of continuous versus intermittent hormonal therapy in men with treatment-naïve, metastatic prostate cancer (mPC).3 All men in S9346 were to receive 7 months of androgen deprivation therapy, at which time those with a PSA level of ≤ 4 ng/ml were randomized to continuous ADT versus intermittent therapy. In contrast, those with a PSA of > 4 ng/ml at month 7 (430/1395) were removed from the study due to an inadequate PSA response to the induction hormone therapy. At the end of the 7 month induction period, the median survival was 75 months for those with a PSA of ≤ 0.2 ng/ml; in contrast, for those with a PSA > 4 ng/ml, the median survival was 13 months, representing a very high-risk mPC population.
Since the inception of S9346, treatment with AA + P or enzalutamide has become a first-line treatment for metastatic castration-resistant prostate cancer (mCRPC). AA + P is approved for use in men with mCRPC based on the positive results of 2 large phase III randomized trials. In the COU-301 trial, AA + P treatment in men with mCRPC previously treated with docetaxel chemotherapy was associated with overall survival (OS) benefit (HR 0.65 p<0.001) compared to prednisone alone.4 In the subsequent COU-302 study, AA + P versus P + placebo was investigated in mCRPC patient not previously treated with docetaxel chemotherapy.5 There was also a substantial OS benefit in this pre-chemotherapy setting (HR of 0.75 p=0.01).
The standard use of AA + P or enzalutamide in clinical practice is limited to mCRPC and there is little information about its use to treat mPC in the hormone-sensitive or upfront setting. The use of upfront AA with ADT in hormone-sensitive prostate cancer was tested in a small randomized study in the neoadjuvant setting.6 Intraprostatic androgens were more effectively suppressed in the combined therapy group, compared to the ADT-alone group, consistent with a more effective targeting of the androgen axis with this approach.
In S1014, men with a PSA of > 4 ng/ml after 6–12 months of ADT for mPC were treated with the addition of AA + P. Men in this study had either a declining PSA (hormone-sensitive disease) or a rising PSA (castration-resistant disease), but all had a PSA > 4 ng/ml. The ability of AA + P to benefit these men with an inadequate PSA response to initial ADT was assessed.
Methods
Patients
The subjects were all 18 years or older with a histological or cytological diagnosis of adenocarcinoma of the prostate and a Zubrod performance status of 0–2.7 All men had metastatic disease defined as 1) visceral metastases, 2) bone metastases, or 3) distant lymph node disease (e.g. above the aortic bifurcation). Only patients with a suboptimal response to initial ADT were enrolled, defined as a PSA > 4 ng/ml between 6–12 months after initiation of continuous ADT for mPC. Patients on standard antiandrogen therapy with a rising PSA were required to undergo a formal washout period (e.g. 6 weeks for bicalutamide) before enrollment. For patients with a declining PSA who were taking an anti-androgen, it was continued. None of the patients had received prior cytotoxic chemotherapy, ketoconazole, sipuleucel-T or radiopharmaceuticals for mPC. Adequate liver, kidney and bone marrow function was required. A baseline testosterone level of < 50 ng/dl was confirmed to ensure adequate and ongoing ADT.
Study design and treatment
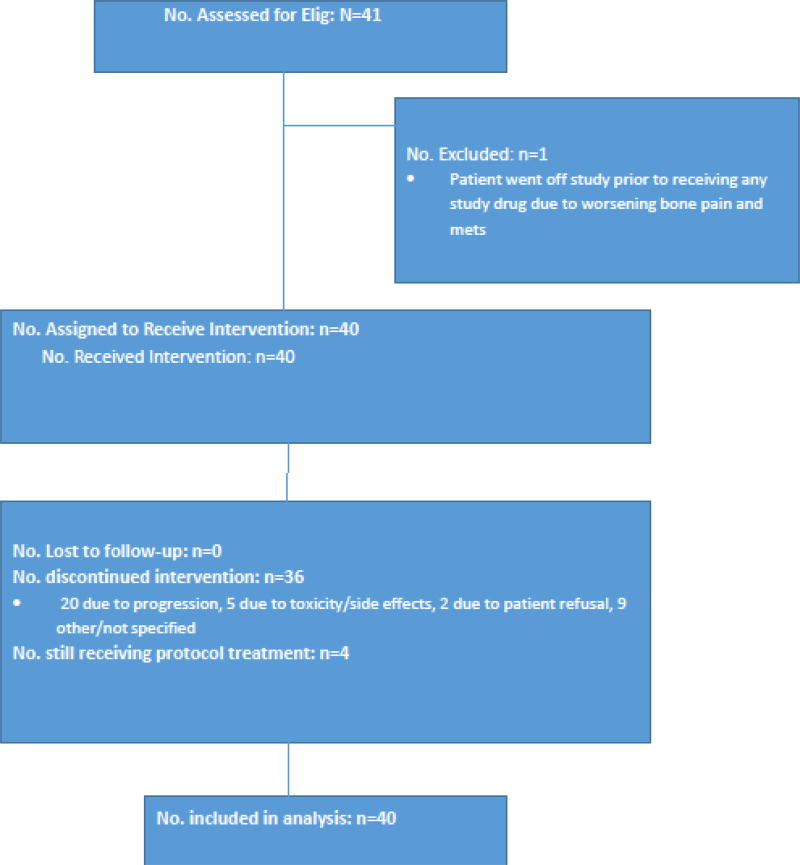
S1014 was a single arm, phase II study conducted by SWOG (Figure 1). All patients were given AA 1000 mg once daily by mouth with prednisone 5 mg twice daily by mouth. AA was provided by the study. Dose modification was allowed and stipulated in the protocol for adverse events with a reduction of AA to 750 or 500mg daily. Prednisone was not dose modified. Subjects were removed from the protocol for progression of disease (PSA rise alone was not sufficient), symptomatic deterioration, unacceptable toxicity, patient withdrawal of consent, or delay in AA dosing of > 4 weeks. Progression of disease was defined as unequivocal progression of disease, progressive disease as defined by RECIST 1.1,8 progressive disease by the prostate cancer working group bone scan progression criteria,9 or death due to disease. Radiographic assessments were performed every 12 weeks. Survival was calculated from date of registration to date of death due to any cause. Patients without the endpoint of interest (PFS or OS) were censored at date of last known contact.
Figure 1. Study Flow.
Study accrual with patients receiving intervention, lost to follow-up, and included for statistical analysis.
The study was approved by the institutional review board of each participating institution. The subjects were recruited with IRB approval from these sites: University of Utah, Salt Lake City; University of Colorado, Aurora; Baylor College of Medicine; Wayne State University, Detroit, Michigan; Yale University; City of Hope National Medical Center, Duarte, California; Kaiser Permanente NCORP, Oakland California; Nevada Cancer Research Foundation NCORP; University of Southern California, Los Angeles; Wichita NCORP, Wichita, Kansas; Hawaii Minority Underserved NCORP, Honolulu, Hawaii; Henry Ford Hospital, Detroit, Michigan; University of Kansas, Lawrence, Kansas; Louisiana State University, in Shreveport/Gulf South Minority Underserved NCORP, New Orleans, Louisiana; Memorial Hospital Center, University of Colorado Health, Colorado Springs/Colorado, U of; Montana Cancer Consortium NCORP, Billings, Montana; Southeast Clinical Oncology Research Consortium Southeast CCC NCORP; University of Texas, San Antonio; SW Cancer & Res Ctr/San Antonio, U of TX; Tulane Medical/Cancer Center Minority-Based Community Clinical Oncology Program, Tulane University, New Orleans, Louisiana; University of Arkansas, Little Rock. Patients provided written informed consent and there was no financial compensation.
The primary endpoint in S1014 was the number of subjects achieving an undetectable PSA, defined as a PSA of ≤ 0.2 ng/ml. Patients not responding in the first year were deemed non-responders. A partial response (PR) was a secondary endpoint defined as a PSA reduction to < 4 ng/ml, but with a level of > 0.2 ng/ml. Responses were required within 12 months of registration and a 12 month landmark analysis was also performed for PSA responses. Other evaluation of PSA metrics were proscribed for descriptive analysis.
Statistical Analyses
The main objective of this study was to test whether this regimen has promise in terms of rates of achieving an undetectable PSA (≤ 0.2 ng/ml), confirmed at least 4 weeks later. If the proportion of men with undetectable PSA is 20% or greater, the regimen would be of further interest, whereas further testing would not be pursued if the proportion of men with undetectable PSA was 5% or less. Six or more subjects with undetectable PSA out of the total 38 eligible patients would indicate that further study of this regimen is warranted. The design has a significance level (chance of falsely determining further study is warranted of a treatment with < 5% response rate) of 5.0% and a power (probability of correctly identifying the agent as warranting further study for a likely response rate of > 20%) of 90%.
A sample size of 38 eligible patients was deemed to be sufficient to estimate the PSA undetectable and PSA normalization rate, the progression-free survival (PFS) and the overall survival (OS) at a specified time point, and the probability of a particular adverse event to within +/− 16% (95% confidence interval). Any toxicity occurring with at least a 5% probability is likely to be seen at least once (83%).
The 20% alternative hypothesis is based on the observation that approximately 20% of castrate-resistant prostate cancer (CRPC) patients treated with AA + P were observed to have a > 90% PSA reduction, indicating that dramatic PSA responses may be expected in 20% of traditional CRPC patients treated. The trial was designed with 90% power to correctly identify the agent as warranting further study for a likely response rate of greater than 20% with a 1-sided significance level of 0.05. Data analysis for this trial was conducted from March 21 to November 29, 2016, using SAS, version 9.4 (SAS Institute Inc).
Results
Forty-one subjects were enrolled between August 9, 2011, and closure on August 1, 2013. One subject was not evaluable and not included in the analysis. Patient Characteristics are shown in Table 1. The median PSA at study entry was 23.6 ng/ml. Thirty of the 40 (74%) evaluable patients had high-grade disease with a Gleason Score10 of 8–10 and 6 (15%) of the subjects had visceral metastatic disease. Thirty-four patients (85%) had a rising PSA and 6 (15%) had a stable/falling PSA. Patients with an increase in PSA of more than 0.1 ng/ml from nadir were assessed as having a rising PSA at study entry.
Table 1.
Patient Characteristics for Eligible Patients
| Abiraterone Acetate (n=40) |
||
|---|---|---|
| AGE | ||
| Median, (range) | 66 (39, 85) | |
| TESTOSTERONE (ng/dl) | ||
| Median, (range) | 12.8 (3.0, 50.0) | |
| PSA AT ENTRY (ng/ml) | ||
| Median (Q1, Q3) ng/ml | 23.6 (11.7, 64.4) | |
| HISPANIC | ||
| Yes | 4 | 10% |
| No, unknown | 36 | 90% |
| RACE | ||
| White | 27 | 67% |
| Black | 10 | 25% |
| Asian | 2 | 5% |
| Native American | 1 | 2% |
| SWOG PS | ||
| 0–1 | 39 | 97% |
| 2 | 1 | 3% |
| GLEASON SCORE | ||
| 2–6 | 3 | 8% |
| 7 | 7 | 18% |
| 8–10 | 30 | 74% |
| METS TO BONE | 37 | 93% |
| LYMPH NODE METS | 8 | 20% |
| VISCERAL METS | 6 | 15% |
| PROSTATE RT | 5 | 13% |
| PROSTATECTOMY | 5 | 13% |
| ANTI-ANDROGEN USE | 35 | 88% |
| TIME FROM ANTI-ANDROGEN TO REG IN DAYS, MEDIAN (RANGE) | 74 (10, 371) | N=34 patients |
| PSA Status at Reg | N=40 patients | |
| Rising PSA | 34 | 85% |
| Stable/Falling PSA | 6 | 15% |
Abbreviations: Mets, Metastatic disease; PS, Performance status; PSA, Prostate specific antigen; REG, registration; RT, radiation therapy
Efficacy
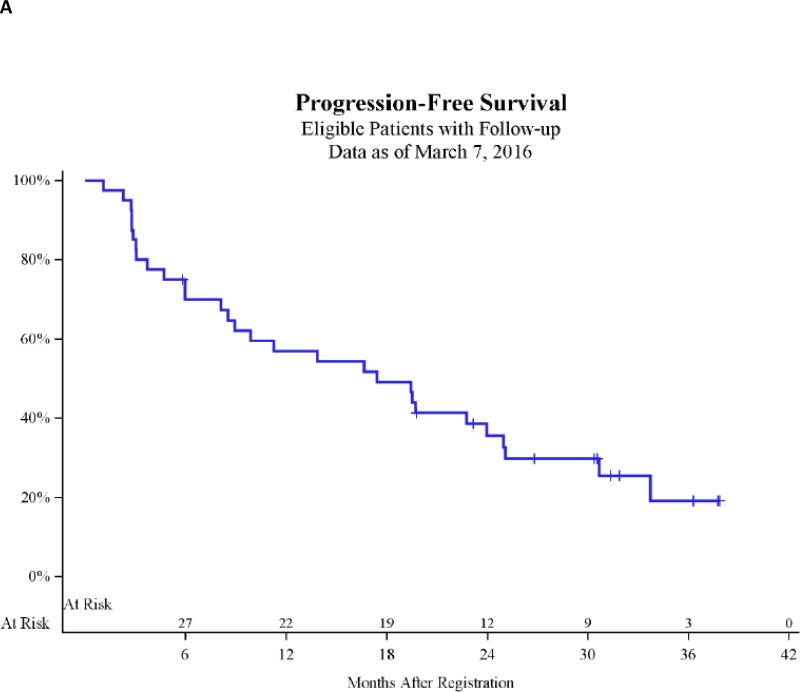
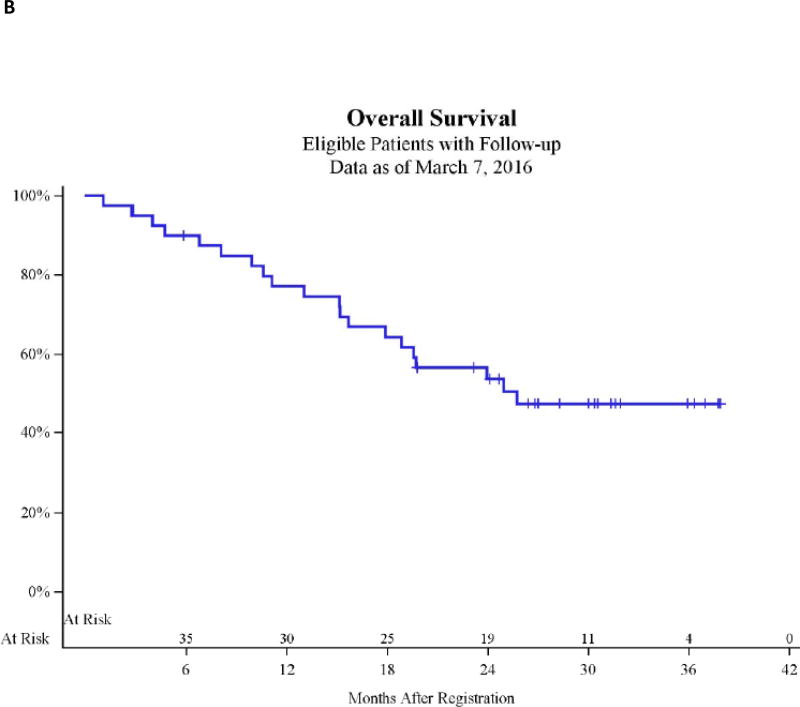
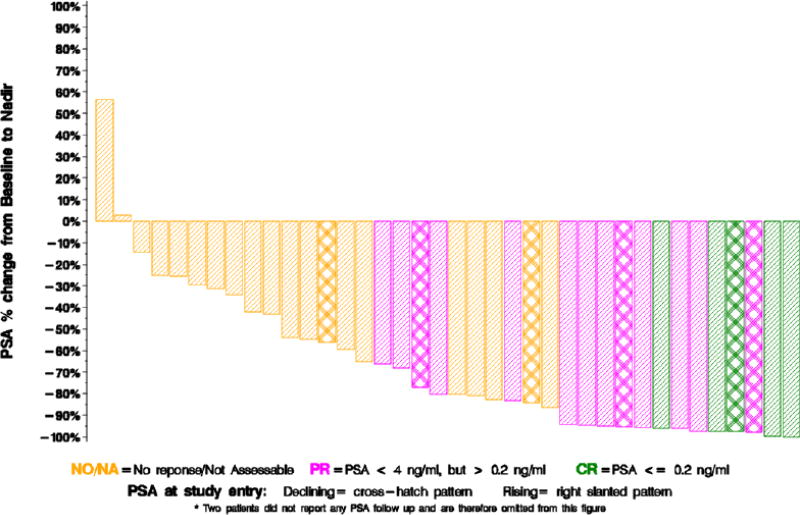
Although the study over-accrued by two patients, the same threshold of PSA response activity specified in the Statistical Analysis section for n=38 also held for n=40. A nadir PSA of ≤ 0.2 ng/ml was obtained in 5 (13%) patients (95% CI 4%, 27%). Thirteen additional patients achieved a PSA normalization with a PSA < 4 ng/ml, confirmed at least 4 weeks later, but had a nadir PSA of >0.2 ng/ml. Of these, 8 had ongoing PSA normalization at a 12-month time point of assessment, whereas all of those with a PSA decrease of ≤ 0.2 ng/ml were maintained a 12 months. Sixteen patients had no PSA response and six were not assessable and assumed to be non-responders (Table 2). The median progression-free survival (PFS) was 17.5 months (95% CI; 8.6, 25.0) (Figure 2A) and based on radiographic, not biochemical progression. The median OS was 25.8 months (95% CI; 15.7, 25.8) (Figure 2B). Of the 40 evaluable patients, 34 had a rising PSA at study entry and 6 had a stable or falling PSA (Table 2). The Median PSA at registration for those with a complete response was 11.5 ng/ml (Q1, Q3; 7.1, 13.4) compared to 16.3 ng/ml (Q1, Q3; 10.4, 20.8) in the PSA normalization group and 41 (Q1, Q3; 19.9, 265.8) in the no response group. A waterfall plot of the best maximum relative PSA reduction for each subject is shown as figure 3. The results of a Wilcoxon rank-sum test yielded no evidence of an association between baseline testosterone levels (nanograms per deciliter) and response to abiraterone (testosterone levels for combined CR/PR patients: median, 10.8; range, 3–40 ng/dL;P = 0.54)Patient characteristics included PSA and testosterone levels at registration and the duration of androgen deprivation therapy prior to registration is shown by PSA response group in Table 3.
Table 2.
PSA Best Responses within First 12 Months Post-Registration
| Best PSA Response |
PSA Status at Registration (N=40) | ||
|---|---|---|---|
| Rising | Stable/Falling | Total | |
| NO/NA | 20 (59%) | 2 (33%) | 22 (55%) |
| PR | 10 (29%) | 3 (50%) | 13 (32%) |
| CR | 4 (12%) | 1 (17%) | 5 (12%) |
| Total | 34 | 6 | 40 |
| Responses at 12 month time point | |||
| NO/NA | 25 (74%) | 2 (33%) | 27 (67%) |
| PR | 5 (15%) | 3 (50%) | 8 (20%) |
| CR | 4 (12%) | 1 (17%) | 5 (12%) |
| Total | 34 | 6 | 40 |
Abbreviations: CR, Complete response with a PSA of ≤ 0.2 ng/ml; NO/NA, no response or not applicable; PR, partial response (PSA level > 0.2 but < 4 ng/ml.); PSA, Prostate Specific Antigen
Figure 2.
Figure 3.
Change in Prostate-Specific Antigen (PSA) Levels From Baseline in 38 Patients
Table 3.
Patient characteristics by best PSA response
| CR | PR | NO/NA | |
|---|---|---|---|
| Age (median, range) years | 64 (51, 72) | 63 (55, 79) | 71 (39, 85) |
| Entry PSA (median, Q1 Q3) ng/dL | 11.5 (5.1, 13.4) | 12.2 (7.4, 20.8) | 50.6 (22.9, 266.9) |
| Testosterone (median, range) ng/dL | 10 (3, 36) | 17 (3, 40) | 13.8 (3, 50) |
| Days from ADT to Registration (median, range) | 137 (13, 308) | 116 (44, 316) | 54 (10, 371) |
Abbreviations: ADT, Androgen Deprivation Therapy; CR, Complete response with a PSA of ≤ 0.2 ng/ml; NO/NA, no response or not applicable; PR, partial response (PSA level > 0.2 but < 4 ng/ml.); PSA, Prostate Specific Antigen
Treatment administration and safety
The median duration of therapy was 8.2 months. A summary of the adverse events is included in Table Supplemental 1, excluding adverse events deemed unlikely or not related to the study drug and also excluding adverse events with no Grade 3–5 entries. No Grade 5 toxicities were noted. One instance each of Grade 4 alanine aminotransferase level increase and rectal hemorrhage were observed. The most common Grade 3 toxicities (2 incidences each) were hypertension, increased AST, hyperglycemia, hypokalemia, nausea and vomiting.
Discussion
Patients with mPC and a PSA of > 4 ng/ml after 7 months of ADT have a very poor prognosis based on historical controls. In S1014, AA therapy was administered to these patients with the aim of reducing the PSA to ≤ 0.2 ng/ml, converting a hormone-induction failure to a traditional complete PSA response. Although encouraged by 5 such responses to the addition of AA, this did not reach the protocol pre-specified level of 6 responses.
The treatment paradigm for hormone-sensitive mPC has changed since the initiation of S1014, based on data from the CHAARTED study.1 In CHAARTED, 790 men with hormone-sensitive mPC were randomized to ADT with or without 6 cycles of docetaxel chemotherapy, with a primary objective of improvement in the OS. As reported in 2015, there was a 13.6 month improvement in the OS with the addition of docetaxel, from 44.0 to 57.6 months (HR 0.61; 95% CI 0.47 to 0.80; p<0.001). In this study, the rate of attaining a PSA of < 0.2 ng/ml at 12 months was 16.7% with ADT versus 27.7% with the combination. Therefore, the improvement in OS correlated with the increased attainment of a PSA < 0.2 ng/ml in CHAARTED, further validating the relevance of this endpoints. The British STAMPEDE trial of hormone sensitive mPC was also recently published.2 In metastatic (M1) patients, the addition of 6 cycles of docetaxel to ADT was associated with an improvement in the median OS from 43 to 65 months (HR 0.73; 95% CI 0.59 to 0.89; p=0.002).
With the success of upfront chemotherapy, the earlier application of more potent hormonal approaches, such as AA, in the disease process needs additional investigation. S1014 gives a signal of activity in a subset of the very high-risk patients studied here. Although a negative study, a larger study or perhaps a less rigorous endpoint, such as a reduction of PSA by 50%, may have yielded a different outcome. The OS of the patients in S1014 was 25.8 months, which compares favorably to historical controls including the 13-month OS in the S9346 patients with failure to achieve a PSA of < 4 ng/ml on which S1014’s entry criteria were modeled. As shown in Figure 2A, there is a small group of highly responsive patients with a prolonged PFS and ongoing response to AA + P therapy with a median follow up of nearly 3 years, despite the very high-risk nature of this group. It is also notable that there appears to be a “tail” on the OS curve, suggesting a subset of patients with prolonged survival despite their high-risk nature. With this small sample, it is difficult to identify any specific clinical characteristics to differentiate these patients and identify any predictive clinical characteristics in those who respond. It is also clear there are additional FDA-approved agents for mCRPC are available to the patients on S1014 that we not available at the time of S9346. It remains unknown if high-risk mPC patients, including those with rapid progression while on ADT, should initially be treated with agents such as AA or enzalutamide versus cytotoxic chemotherapy with the development of mCRPC. The data from this study demonstrate that, despite their high-risk nature, subjects in S1014 demonstrated clinically-relevant responses to AA, supporting a trial of a next generation hormonal therapy such as AA in this setting before chemotherapy in select patients.
The biologic mechanism of early resistance to ADT seen in the patients enrolled S1014 is not clear. Since the initiation of S1014, AR-V7 has been identified as a biomarker of response to AA and enzalutamide in prostate cancer patients.11 This Androgen Receptor (AR) splice variant lacks the ligand binding domain, which is the target of these therapies, and is constitutively active. In a study of 62 mCRPC patients starting AA or enzalutamide, the AR-V7-positive patients had a PSA response rate of 0% versus response rates of 53% and 68% with enzalutamide and AA treatment, respectively. AR-V7 does not appear to be a general marker of drug resistance and is not associated with complete resistance to docetaxel chemotherapy.11 The incidence of AR-V7 in those patients with resistance to primary hormone induction therapy including those treated in S1014 is not known. With ongoing technical advances in molecular testing, additional study of the biologic mechanisms contributing to the high-risk nature of these patients is needed.
Going forward, the optimal upfront approach to treating hormone-sensitive mPC will be an area of ongoing investigation. With the CHAARTED and Stampede data, the addition of docetaxel to ADT should be considered in hormone-sensitive, chemotherapy-eligible men with mPC. Due to age, comorbidities and patient preference, many hormone-sensitive mPC patients will not receive docetaxel. The upfront use of drugs such as AA or enzalutamide therapy in mPC, either in conjunction with chemotherapy or alone, needs further investigation. S1216 (NCT01809691) is an ongoing trial of hormone-sensitive mPC patients to ADT + TAK-700 (orteronel) versus ADT + Bicalutamide.12 Orteronel is an experimental agent which acts as an androgen synthesis inhibitor of steroid 17alpha-monooxygenase (17,20 lyase) with possible antiandrogen activity as well. With the future clinical integration of AR-V7 testing, the ability to select AR-V7-negative patients who are most likely to benefit from testosterone blocking agents in the upfront setting may also be possible. The data from the current study suggests activity with early AA therapy in this high-risk group of mPC patients. This clinical trial also provides modern data on this high-risk group of primary ADT-refractory patients which may be used to inform additional study in this important patient subgroup.
There are several limitations to this report. This was a single-arm intervention study, using a comparable subset of patients from the SWOG 9346 trial as a historical control. A larger, randomized study would provide a contemporary comparator to the intervention arm described here to better determine the benefit of abiraterone in this setting. The most appropriate PSA response surrogate in this hormone-induction failure group is also not known; the PSA CR level here (PSA<0.2 ng/mL), based on information from S9346, was ambitious, but a 50% PSA reduction, PSA normalization to 4 ng/mL, or other PSA reduction could also have been utilized. Biologic correlative studies were not performed in this study. The identification of biomarkers that predict which of these high-risk patients may respond to abiraterone acetate would also improve the clinical application of such an approach.
In summary, S1014 tested AA + P in mPC patients with a PSA > 4 ng/ml after 6–12 months of ADT. There were 5 patients with a PSA reduction to ≤ 0.2 ng/nl, which is less than the 6 responses prescribed in the study for a positive result. However, the OS of patients in this study was 25.8 months and appears favorable compared with data in historical controls. Ongoing and future studies should evaluate the use of next generation hormonal agents in the upfront setting and its integration with chemotherapy for these patients.
Supplementary Material
Acknowledgments
Author Disclosures: Thomas Flaig discloses Honoraia from GTX and BN Immunotherapeutics, Consulting fees from GTX, Research support from Novartis, Bavarian Nordic, Cougar Biotechnology, Dendreon, GTx, Janssen Oncology, Medivation, Sanofi, Pfizer, Bristol-Myers Squibb, Roche/Genentech, Exelixis, Aragon Pharmaceuticals, Sotio, Tokai Pharmaceuticals, astrazeneca/MedImmune, Lilly, and Astellas. Ulka Vaishampayan has consulted and received honoria from Janssen. Neeraj Agarwal has served in a consulting or advisory role for Pfizer, Exelixis, Cerulean Pharma, Medivation, Eisai, and Argos Therapeutics. Maha Hussain discloses a consulting or advisory role with Genentech/Roche, Abbvie and Bayer. Dr. Hussain has research funding from Genentech, Medivaion, Pfizer and Bayer as well as patent/intellectual property disclosures for prostate cancer treatment and detection.
This work was supported by National Institutes of Health/National Cancer Institute/National Clinical Trials Network [grant numbers CA180888, CA180819, CA180818, CA180834, CA180835, CA180826, CA180830, CA12644]; National Institutes of Health/National Cancer Institute Community Oncology Research Program [grant numbers CA189821, CA189829, CA189808, CA189854, CA189872, CA189858, CA189804]; National Institutes of Health/National Cancer Institute legacy grants [grant numbers CA 46368, CA58416, CA52623, CA22433, CA37981]; and in part by Janssen Biotech, Inc.
The National Cancer Institute and Janssen Biotech, Inc., played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, or approval of the manuscript; and decision to submit the manuscript for publication, however, both entities were given the opportunity to review the manuscript and to provide comment.
Thomas Flaig and Melissa Plets had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Presented as poster presentation at ASCO GU Cancers Symposium (February 26–28, 2015, Orlando, FL); http://meetinglibrary.asco.org/content/141041-159
References
- 1.Sweeney CJ, Chen YH, Carducci M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373(8):737–746. doi: 10.1056/NEJMoa1503747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James ND, Sydes MR, Clarke NW, et al. STAMPEDE investigators. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163–1177. doi: 10.1016/S0140-6736(15)01037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hussain M, Tangen CM, Higano C, et al. Southwest Oncology Group Trial 9346 (INT-0162). Absolute prostate-specific antigen value after androgen deprivation is a strong independent predictor of survival in new metastatic prostate cancer: data from Southwest Oncology Group Trial 9346 (INT-0162) J Clin Oncol. 2006;24(24):3984–3990. doi: 10.1200/JCO.2006.06.4246. [DOI] [PubMed] [Google Scholar]
- 4.de Bono JS, Logothetis CJ, Molina A, et al. COU-AA-301 Investigators. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364(21):1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryan CJ, Smith MR, de Bono JS, et al. COU-AA-302 Investigators. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368(2):138–148. doi: 10.1056/NEJMoa1209096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taplin ME, Montgomery B, Logothetis CJ, et al. Intense androgen-deprivation therapy with abiraterone acetate plus leuprolide acetate in patients with localized high-risk prostate cancer: results of a randomized phase II neoadjuvant study. J Clin Oncol. 2014;32(33):3705–3715. doi: 10.1200/JCO.2013.53.4578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655. [PubMed] [Google Scholar]
- 8.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 9.Scher HI, Halabi S, Tannock I, et al. Prostate Cancer Clinical Trials Working Group. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26(7):1148–1159. doi: 10.1200/JCO.2007.12.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein JI, Allsbrook WC, Jr, Amin MB, Egevad LL ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol. 2005;29(9):1228–1242. doi: 10.1097/01.pas.0000173646.99337.b1. [DOI] [PubMed] [Google Scholar]
- 11.Antonarakis ES, Lu C, Wang H, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med. 2014;371(11):1028–1038. doi: 10.1056/NEJMoa1315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.clinicalTrials.gov. S1216, Phase III ADT+TAK-700 vs. [Updated February 23, 2017. Accessed February 23, 2017];ADT+Bicalutamide for Metastatic Prostate Cancer. NCT01809691. https://clinicaltrials.gov/ct2 /show/ NCT01809691.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.