Abstract
Background
Complementary and alternative medicines (CAM) are commonly used in patients with cardiovascular disease. While there is lack of evidence regarding the benefit of CAM on cardiovascular morbidity and mortality, health status benefits could justify CAM use.
Hypothesis
Adoption of mind-body CAM after acute myocardial infarction (AMI) is associated with improved health status while other forms of CAM are not associated with health status improvement.
Methods
Patients with AMI from 24 US sites were assessed for CAM use (categorized as mind-body, biologic and manipulative therapies) prior to and 1 year after AMI. Among patients who reported not using CAM prior to their AMI, association of initiating CAM on patients’ health status at 1 year after AMI was assessed using Angina Frequency and Quality of Life domains from the Seattle Angina Questionnaire and the SF-12 Physical and Mental Component Scales. Multivariable regression helped examine association between use of different CAM therapies and health status.
Results
Among 1884 patients not using CAM at the time of their AMI, 33% reported initiating 1 or more forms of CAM therapy 1 year following AMI; 62% adopted mind-body therapies, 42% biological therapies, and 15% began using manipulative therapies. In both unadjusted and adjusted analyses, we found no association between different types of CAM use and health status improvement after AMI.
Conclusion
There was no association between CAM use and health status recovery after AMI. Until randomized trials suggest otherwise, these findings underscore the importance of focusing on therapies with proven effectiveness after AMI.
Keywords: health status, myocardial infarction, angina, complementary therapies
INTRODUCTION
The use of Complementary and alternative medicines (CAM) in the US is both prevalent and costly, accounting for $33.9 billion in out-of-pocket spending and 1.5% of total health care expenditures.2 One-third to one-half of patients with cardiovascular disease (CVD) use some form of CAM, 3,4 in an effort to improve cardiac symptoms or reduce cardiovascular risk.5 While some studies have shown limited benefit with certain CAM therapies,1, 6 such as relaxation and breathing techniques after an acute myocardial infarction (AMI),7 and meditation in patients with stable CVD8, others have shown no effect. 2, 9,10
Patients using mind-body CAM therapies (e.g., meditation, yoga) report that these therapies help them combat stress, promote emotional health, and improve overall well-being.4 Given the established effects of stress and depressive symptoms on angina and quality of life after an AMI,11 it is conceivable that use of mind-body therapies may improve health status. In addition, a number of supplements, such as Coenzyme Q10, Hawthorn Berry, and L-carnitine, have been reported to reduce angina;12–16 however, the true effects of these biological therapies, as well as manipulative CAM therapies (e.g, massage, chiropractic care), on health status outcomes after an AMI are unknown.
We therefore used a multicenter AMI registry to explore the association of CAM use after AMI with symptoms, physical function, and quality of life. If CAM use is associated with improvements in health status recovery after AMI, this could provide support and justification for its use, even in the absence of an effect on morbidity or mortality.
METHODS
Our analytic population was derived from the TRIUMPH study, a prospective, observational registry of AMI patients enrolled from 24 US hospitals between April 2005 and December 2008. Details of the TRIUMPH methodology have been previously published. 17 In brief, eligible patients were ≥18 years old and were admitted with a diagnosis of AMI. Baseline data were obtained through chart abstraction and a structured interview by trained research staff within 24 to 72 hours of admission. Institutional research boards at each participating center approved the study protocol, and each patient signed informed consent for baseline and follow-up interviews.
Follow-up was attempted on all surviving patients at 1, 6 and 12 months after AMI through a centralized telephone follow-up center. We excluded patients who reported taking CAM prior to their AMI to focus on the adoption of CAM therapy after AMI. We further excluded patients who died prior to 1 year and therefore had no ability to provide assessment of their health status or CAM use.
At baseline and at each follow-up, patients were asked “do you use any of the following things to help your health”: natural products or herbal supplements (nonvitamin, nonmineral), deep breathing exercises, meditation, massage, yoga or pilates, or chiropractic care. Due to the breadth of therapies used by the patients and difficulty to determine the association of individual CAM therapies with outcomes, these therapies were categorized as biological (supplements), mind-body (deep breathing, meditation, yoga/pilates), and manipulative (massage, chiropractic care). As fish oil is prescribed by many cardiologists to patients with coronary artery disease, this was not considered an alternative medicine.18,19
Health status was assessed at baseline and each follow-up time point using the Seattle Angina Questionnaire (SAQ) and the Medical Outcomes Study Short-Form 12 (SF-12) questionnaire. The SAQ is a disease-specific health status measure that assesses angina frequency, disease specific quality of life, angina stability, physical limitations, and treatment satisfaction in patients with coronary artery disease.20 For this study, we focused on angina frequency (SAQ-AF; quantifies the frequency and burden of angina) and quality of life (SAQ-QoL; evaluates how the patient perceives that angina is impacting his or her quality of life) domains. Domain scores range from 0 to 100, with higher scores reflecting fewer symptoms and better quality of life. A clinically important difference for the SAQ domains is ~5 points. The SF-12 is a generic health status measure that is derived from the SF-36 and provides mental and physical summary scores that are scaled to overall US norms of 50 and a standard deviation of 10, with higher scores indicating better quality of life.21 The minimum clinically important difference for the SF-12 physical and mental summary scores is considered ~2 points.22
Baseline demographic and clinical characteristics of patients who did and didn’t use CAM (all categories combined) at 1 year after the AMI hospitalization were compared using t-tests for continuous variables and chi-square tests for categorical variables. Demographic and clinical characteristics of patients reporting different categories of CAM couldn’t be quantitatively compared because these groups were not mutually exclusive. We used hierarchical, multivariable linear regression to evaluate effect of CAM use over the year following AMI on 1-year health status outcomes. As patients could be simultaneously using more than 1 type of CAM, this model was specifically designed to separately examine the association of each type of CAM with health status, while controlling for use of other types of CAM as well as other patient characteristics. In addition to the 3 categories of CAM, the model included factors that could confound the association between CAM use and health status. The following covariates were selected a priori based on clinical judgment and prior evidence of their association with health status outcomes: age, sex, race, high school education, marital status, medical insurance, current smoking, diabetes mellitus, dyslipidemia, chronic kidney disease, history of bypass graft surgery, history of percutaneous coronary intervention, coronary angiogram during the index AMI hospitalization, coronary revascularization during the index AMI hospitalization, and participation in cardiac rehabilitation after AMI. Site was entered in the model as a random effect to account for clustering of patients by site, and covariates were site-centered.
Our primary analysis examined the association of CAM use, as reported at the 1-year interview, with 1-year health status. However, it is not known whether CAM use reported at 1 year after AMI represented consistent use over the prior year or if there is a necessary duration for CAM to be used for there to be an effect on health status. As such, we performed a sensitivity analysis in which we included only patients who reported use (or non-use) of CAM at both 6 months and 1 year (in order to compare prolonged use of CAM with those not using CAM).
Baseline data were generally complete, with 10% of patients missing 1 baseline covariate, 5% missing more than 1 covariate, and an average of 0.23 items missing per patient. Missing data were estimated using sequential regression imputation conditioning on all covariates and outcomes (IVEware; Institute for Social Research, Ann Arbor, MI). In order to examine the effect of selection bias due to loss to follow-up, we constructed a multivariable logistic regression model to determine the probability of having missing data. We then weighted each of the patients in the analytic cohort by the inverse probability of the likelihood of having missing data.23 Results of this analysis were consistent with the primary analysis, and thus only the unweighted analyses are presented. All statistical analyses were performed with SAS version 9.2 (SAS Institute Inc., Cary, North Carolina), and a 2-sided α level of 0.05 was used to determine statistical significance.
RESULTS
Among 4340 patients enrolled in the TRIUMPH registry, we excluded 1224 patients who reported using CAM prior to their AMI and 228 patients who died over the 1 year after AMI and were therefore ineligible for follow-up. Among 2888 patients who reported not using CAM at baseline and were eligible for follow-up, 1004 patients (34.8%) were excluded due to missing data at 1 year. The final analytic cohort consisted of 1884 patients, of whom 618 patients (32.8%) reported using 1 or more forms of CAM therapy at 1 year after their AMI: 384 patients (62%) used mind-body therapies, 260 (42%) used biological therapies, and 91 (15%) used manipulative type of CAM (Figure 1). Compared with those in the analytic cohort, patients who were eligible but had missing data were likely to be younger, non-white race, lower socioeconomic status, and current smokers. Patients with missing data also had worse disease-specific and generic health status at baseline compared with patients in the analytic cohort (Supplemental Table 1).
Figure 1.
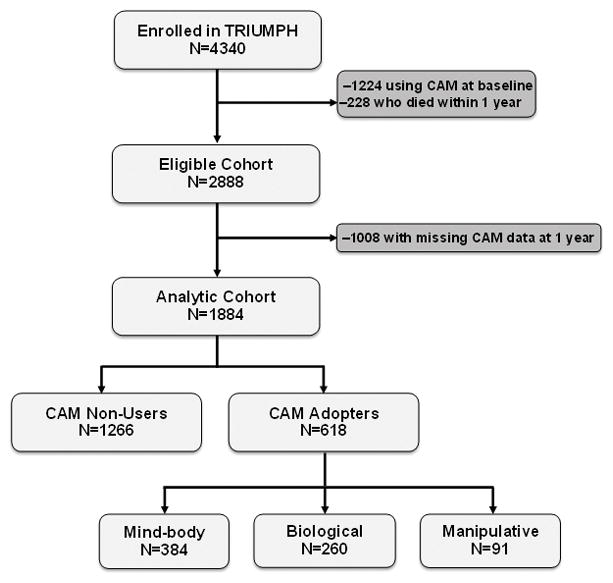
Flow chart of the analytic cohort
Table 1 shows a comparison of baseline characteristics of patients who adopted any CAM therapy with those who did not. The demographic and clinical characteristics of patients using different types of CAM are also shown in Table 1 (patients could report using more than 1 type of CAM and thus contribute data to more than 1 column).
Table 1.
Baseline characteristics of patients according to use of complementary and alternative medicine at 1 year after AMI
| Non-user n=1266 |
CAM adopters n=618 |
Mind-body n=384 |
Biological n=260 |
Manipulative n=91 |
|
|---|---|---|---|---|---|
| Demographics | |||||
| Age (yrs) | 60.0 ± 12.0 | 59.2 ± 12.4 | 60.0 ± 12.1 | 58.6 ± 12.7 | 56.9 ± 11.2 |
| Male sex | 70.6% | 62.5%1 | 54.7% | 71.5% | 72.5% |
| White race | 71.0% | 65.9%1 | 60.6% | 74.1% | 64.4% |
| Hispanic/Latino | 6.5% | 5.1% | 5.6% | 5.9% | 7.0% |
| Socioeconomomic status | |||||
| High school education | 77.6% | 83.2%1 | 83.7% | 84.8% | 88.9% |
| Married | 55.7% | 52.3% | 47.2% | 60.9% | 51.7% |
| Unemployed | 51.6% | 54.4% | 60.9% | 42.9% | 45.6% |
| No medical insurance | 18.8% | 16.3% | 18.5% | 12.2% | 16.7% |
| Self-reported avoidance of medications due to cost | 2.9% | 2.1% | 2.6% | 1.6% | 2.2% |
| Clinical characteristics | |||||
| Prior AMI | 18.6% | 19.1% | 21.4% | 16.9% | 18.7% |
| Prior bypass graft surgery | 11.6% | 11.3% | 12.5% | 11.2% | 12.1% |
| Prior coronary stenting | 18.6% | 18.1% | 16.1% | 20.8% | 19.8% |
| Chronic heart failure | 7.3% | 7.3% | 9.1% | 5.8% | 4.4% |
| Body mass index (kg/m2) | 29.4 ± 6.3 | 30.2 ± 6.81 | 30.1 ± 7.0 | 30.4 ± 6.7 | 31.1 ± 7.0 |
| Hematocrit (%) | 41.4 ± 5.5 | 40.8 ± 5.91 | 40.3 ± 6.1 | 41.2 ± 5.7 | 41.7 ± 4.6 |
| Creatinine (mg/dL) | 1.2 ± 0.9 | 1.2 ± 0.9 | 1.2 ± 1.0 | 1.2 ± 0.7 | 1.2 ± 0.7 |
| Patient Health Questionnaire-9 depression score2 | 4.8 ± 5.1 | 4.9 ± 5.4 | 5.3 ± 5.6 | 4.4 ± 4.9 | 4.2 ± 4.9 |
| Smoking status | |||||
| Current | 39.3% | 38.3% | 40.0% | 34.1% | 31.1% |
| Former | 34.6% | 32.6% | 32.6% | 35.3% | 30.0% |
| Never | 26.0% | 29.0% | 27.4% | 30.6% | 38.9% |
| In-hospital and treatment factors | |||||
| Moderate/severe LV dysfunction | 16.3% | 16% | 16.9% | 14.7% | 13.3% |
| ST-elevation AMI | 43.3% | 41.7% | 38.8% | 48.1% | 36.3% |
| Coronary angiogram | 93.8% | 92.2% | 91.1% | 93.1% | 86.8% |
| Revascularization | 76.0% | 75.6% | 72.4% | 78.1% | 76.9% |
| Participation in cardiac rehabilitation | 35.5% | 40.6% | 36.8% | 47.1% | 45.9% |
Data are reported as mean ± standard deviation or %. For CAM categories, patients reported using more than 1 type of CAM contributing data to more than 1 column. As such, columns are not mutually exclusive, and no statistical comparisons are presented for CAM categories. LV, left ventricular; AMI, acute myocardial infarction
p<0.05 comparing CAM non-users and CAM adopters
Scores range from 0–27, with higher scores indicating more depressive symptoms and a score of ≥10 corresponding to a level of at least moderate depression.31
There were no clinically meaningful differences in health status among groups either at baseline or follow-up in the unadjusted analyses (Table 2). After adjusting for demographic and clinical characteristics and accounting for overlap in CAM use among different types of CAM, there remained no significant association between any of the types of CAM use and any of the measures of health status at 1 year after AMI (Table 3). Results from our multivariable linear regression analysis are shown in detail in Supplemental Table 2.
Table 2.
Health status at baseline and 1 year after AMI according to use of complementary and alternative medicine at 1 year after AMI
| Non-user n=1266 |
CAM adopters n=618 |
Mind-body n=384 |
Biological n=260 |
Manipulative n=91 |
|
|---|---|---|---|---|---|
| Baseline Health Status | |||||
| SAQ Angina Frequency | 87.2 ± 19.7 | 86.6 ± 19.1 | 85.8 ± 19.7 | 87.7 ± 18.7 | 84.9 ± 21.3 |
| SAQ Quality of Life | 64.7 ± 23.2 | 63.4 ± 23.1 | 63.0 ± 23.3 | 64.2 ± 22.7 | 61.4 ± 23.0 |
| SF-12 Physical Component Summary | 43.3 ± 12.0 | 43.1 ± 12.1 | 42.1 ± 12.6 | 44.1 ± 11.5 | 43.8 ± 12.2 |
| SF-12 Mental Component Summary | 50.3 ± 11.2 | 50.1 ± 11.3 | 49.4 ± 12.0 | 51.0 ± 10.7 | 51.4 ± 10.5 |
| 1-year Health Status | |||||
| SAQ Angina Frequency | 93.2 ± 15.9 | 92.4 ± 16.7 | 91.1 ± 17.9 | 93.9 ± 15.4 | 94.4 ± 15.6 |
| SAQ Quality of Life | 81.9 ± 20.9 | 80.5 ± 21.7 | 79.0 ± 23.0 | 82.8 ± 20.0 | 82.7 ± 17.1 |
| SF-12 Physical Component Summary | 43.6 ± 11.8 | 42.5 ± 12.0 | 41.2 ± 12.5 | 44.2 ± 11.4 | 43.5 ± 10.0 |
| SF-12 Mental Component Summary | 51.7 ± 10.6 | 51.9 ± 10.3 | 51.2 ± 10.7 | 52.8 ± 9.7 | 51.3 ± 10.0 |
Patients reporting using more than 1 type of CAM contribute data to more than 1 column. As such, columns are not mutually exclusive, and no statistical comparisons are presented. AMI, acute myocardial infarction; SAQ, Seattle Angina Questionnaire; SF-12, Short form-12
Table 3.
Association of type of complementary and alternative medicine adoption and health status outcomes, as derived from multivariable linear regression models
| Health Status Outcome | CAM adopters | Mind-body | Biological | Manipulative |
|---|---|---|---|---|
| β-estimate1 (95% CI) | β-estimate1 (95% CI) | β-estimate1 (95% CI) | β-estimate1 (95% CI) | |
| SAQ Angina Frequency | −1.00 (−2.76 to 0.77) | 0.33 (−1.72 to 2.38) | 2.32 (−0.98 to 5.62) | |
| SAQ Quality of Life | −1.54 (−3.80 to 0.72) | 0.66 (−1.97 to 3.29) | 3.08 (−1.15 to 7.31) | |
| SF-12 Physical Component Summary | −0.95 (−2.13 to 0.24) | 0.15 (−1.22 to 1.53) | 0.38 (−1.88 to 2.64) | |
| SF-12 Mental Component Summary | −0.01 (−1.15 to 1.14) | 0.85(−0.48 to 2.17) | −0.59 (−2.78 to 1.60) |
CAM, complementary and alternative medicine; SAQ, Seattle Angina Questionnaire; SF-12, Short Form-12
β-estimates represent the difference in health status score expected with use (vs. non-use) of each CAM therapy, adjusting for sociodemographic factors, clinical factors, baseline health status, and site of care. Confidence intervals that contain 0 are not statistically significant. Non-users of CAM form the reference group.
In the sensitivity analysis where we required consistent use of the reported CAM (or non-use) at 6 months and 1 year after AMI, our analytic cohort included 784 non-users of CAM and 236 consistent adopters of CAM: 162 who used mind-body therapies, 95 who used biological therapies, and 34 who used manipulative type of CAM. In the adjusted analyses, consistent use of manipulative therapies was associated with a 6.7 point higher score on the SAQ angina frequency domain at 1 year (i.e., patients reported less angina; CI 1.28–12.12; Supplemental Table 3). Otherwise, results were generally similar to the main analysis.
DISCUSSION
In our large multicenter registry of AMI patients, we found that a little over a third of patients began using some form of CAM (mind-body, biological or manipulative) over the year following AMI. In both unadjusted analyses and analyses adjusting for demographic and clinical factors, we found no association between different types of CAM use and improvement in health status after AMI.
Similar to prior studies, almost a third of the patients from our analytic cohort were using some form of CAM.3, 4 The data on the use of CAM for improvement in symptoms and quality of life after an AMI are scarce, but these studies have generally been positive. 1,24, 25, 26–28 Among patients hospitalized for an acute coronary syndrome who were surveyed at 6 months after hospitalization, patients who had used CAM were more likely to report “feeling some degree of improvement in their quality of life and heart disease” as compared with those who did not use CAM.24 In a study of 65 patients with CVD, progressive relaxation and Qigong (a group of Chinese energy exercises) was shown to decrease blood pressure and heart rate and to decrease symptoms of anxiety and depression.25 Tai chi, another Chinese practice that involves breathing and movement exercises, was also shown to improve quality of life and exercise capacity in a study of 30 patients with chronic heart failure.7 Prior studies on the effect of biological agents in patients with CVD are primarily limited to assessment of physiologic parameters or clinical symptoms. In a study of 50 patients with an ST-elevation AMI, red ginseng was shown to improve coronary blood flow over the 8 months after the AMI, 26 which could, theoretically, have a beneficial effect on angina and quality of life, although this was not explicitly studied. In another study of 79 patients with non-ST-elevation acute coronary syndromes, Bulbus allii macrostemi, a perennial herb, was shown to improve angina.27 Finally, in a study of 120 patients after AMI, 6 months of treatment with the Shengmai Capsule, a Chinese herbal preparation, was shown to improve angina and Activity of Daily Living scores in living capacity.27 There are no studies that we are aware of that have investigated the effects of manipulative therapies on angina and quality of life in patients with CVD. In conflict with these studies, we found that none of the different types of CAM were significantly associated with improvement in patients’ angina symptoms, their general physical or mental health, or their disease-specific quality of life. With more prolonged use, in the sensitivity analysis, manipulative therapies were associated with a small improvement in angina. However, this was a small group of patients, and there was no effect seen in the larger sample. There are likely multiple reasons for the discrepancy in our results and prior studies. Our sample size was much larger than prior studies and we used well-established, validated, disease-specific and generic health status measures; as such, our results could be viewed as more robust compared with prior studies. However, as we grouped different types of CAM together (e.g., all biological therapies were included in 1 group), there may have been effects of very specific types of CAM (e.g., L-carnitine, ginsing, etc.) that were used infrequently and therefore their effects were diluted by ineffective therapies. However, our results do not support CAM use after AMI for the purposes of improving cardiac symptoms and quality of life.
The economic implications of our findings could be substantial. In addition to prior studies demonstrating no benefit in mortality, we found no significant association of CAM use with improvement in quality of life after an AMI. In the US, patients spend more than $30 billion dollars per year on CAM. 29 Furthermore, use of CAM can lead to non-compliance with traditional medications,30 which could adversely impact our efforts at secondary prevention. As some CAM therapies (e.g., deep breathing, yoga) involve no harm, some potential non-cardiac benefits (e.g., stress reduction), and have minimal costs, it should be noted that we are not recommending against all forms of CAM after AMI. We believe that our study adds support to the notion that CAM should not be recommended explicitly for improvement in quality of life after an AMI. A change in practice to treatments with an established evidence base could markedly reduce out of pocket costs for a substantial proportion of cardiac patients.
Our study should be considered in light of the following potential limitations. First, as we used the 1-year follow-up to determine adoption of CAM, patients may have started taking CAM at different times after their AMI, leading to variable periods of exposure. We conducted a sensitivity analysis requiring use (or non-use) at both 6 months and 1 year to attempt to mitigate this effect, and the results were generally consistent. In addition, we did not have an assessment of the intensity of the exposure to CAM (e.g., infrequent medication use vs. daily use), which also could have affected our results. Second, although we included a variety of CAM therapies, it is possible that there are other CAM therapies that we did not capture that could have a potential benefit (e.g., energy therapies, acupuncture and chelation therapy). Third, our categorization of CAM therapies into 3 broad groups was admittedly coarse. However, given the low frequency of use of specific treatments, this study design allowed for power to be able to detect differences but also provided some categorization of CAM into broad types (i.e., it would not be expected that mind-body therapies would provide similar effects as supplements). Also there may be a particular type of CAM therapy that is rarely used but effective, and, due to its limited use in the study cohort, we were unable to identify this effect. Furthermore, we were limited to 1 year of follow-up, which could have missed an effect of a CAM therapy that did not manifest until a patient used this for a more prolonged period of time. Finally, 35% patients who were eligible for the study had missing follow-up data and were thus excluded from the analyses. While these patients did differ in their demographic and clinical characteristics from included patients, the weighted analysis based on the probability of participating in follow-up showed similar results to our primary analyses, indicating little bias from missing follow-up data.
In conclusion, in a large, multicenter registry, we found that adoption of CAM use was exceedingly common after AMI. Despite the frequent CAM use, we found no significant association between various types of CAM use and health status recovery after AMI. Unless future clinical trials provide evidence to the contrary, our findings do not support CAM use after AMI for the purposes of improving cardiac symptoms and quality of life and underscore the importance of focusing on therapies with proven effectiveness.
Supplementary Material
Footnotes
Disclosures: Dr Spertus reports research grants: NHLBI, AHA, ACCF, Gilead, Lilly, EvaHeart, Amorcyte; Consultant honoraria: United Healthcare, Genentech, Amgen; Copyright: Seattle Angina Questionnaire. The other authors report no potential conflicts.
References
- 1.Arthur HM, Patterson C, Stone JA. The role of complementary and alternative therapies in cardiac rehabilitation: a systematic evaluation. Eur J Cardiovasc Prev Rehabil. 2006;13(1):3–9. doi: 10.1097/00149831-200602000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Rabito MJ, Kaye AD. Complementary and alternative medicine and cardiovascular disease: an evidence-based review. Evid Based Complement Alternat Med. 2013;2013:672097. doi: 10.1155/2013/672097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buettner C, Phillips RS, Davis RB, et al. Use of dietary supplements among United States adults with coronary artery disease and atherosclerotic risks. The American journal of cardiology. 2007;99(5):661–666. doi: 10.1016/j.amjcard.2006.09.116. [DOI] [PubMed] [Google Scholar]
- 4.Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. Am J Cardiol. 2006;98(5):673–680. doi: 10.1016/j.amjcard.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 5.Bekke-Hansen S, Pedersen CG, Thygesen K, et al. Faith and use of complementary and alternative medicine among heart attack patients in a secular society. Complement Ther Med. 2012;20(5):306–315. doi: 10.1016/j.ctim.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Yeh GY, Wood MJ, Lorell BH, et al. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117(8):541–548. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 7.van Dixhoorn JJ, Duivenvoorden HJ. Effect of relaxation therapy on cardiac events after myocardial infarction: a 5-year follow-up study. J Cardiopulm Rehabil. 1999;19(3):178–185. doi: 10.1097/00008483-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Schneider RH, Grim CE, Rainforth MV, et al. Stress reduction in the secondary prevention of cardiovascular disease: randomized, controlled trial of transcendental meditation and health education in Blacks. Circ Cardiovasc Qual Outcomes. 2012 Nov;5(6):750–758. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stabler SN, Tejani AM, Huynh F, Fowkes C. Garlic for the prevention of cardiovascular morbidity and mortality in hypertensive patients. Cochrane Database Syst Rev. 2012;8:CD007653. doi: 10.1002/14651858.CD007653.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuller LH, Ives DG, Fitzpatrick AL, et al. Does Ginkgo biloba reduce the risk of cardiovascular events? Circ Cardiovasc Qual Outcomes. 2010 Jan;3(1):41–47. doi: 10.1161/CIRCOUTCOMES.109.871640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arnold SV, Smolderen KG, Buchanan DM, et al. Perceived stress in myocardial infarction: long-term mortality and health status outcomes. J Am Coll Cardiol. 2012;60(18):1756–1763. doi: 10.1016/j.jacc.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamikawa T, Kobayashi A, Yamashita T, et al. Effects of coenzyme Q10 on exercise tolerance in chronic stable angina pectoris. Am J Cardiol. 1985;56(4):247–251. doi: 10.1016/0002-9149(85)90843-4. [DOI] [PubMed] [Google Scholar]
- 13.Tran MT, Mitchell TM, Kennedy DT, et al. Role of coenzyme Q10 in chronic heart failure, angina, and hypertension. Pharmacotherapy. 2001;21(7):797–806. doi: 10.1592/phco.21.9.797.34564. [DOI] [PubMed] [Google Scholar]
- 14.Chang WT, Dao J, Shao ZH. Hawthorn: potential roles in cardiovascular disease. Am J Chin Med. 2005;33(1):1–10. doi: 10.1142/S0192415X05002606. [DOI] [PubMed] [Google Scholar]
- 15.Ferrari R, Merli E, Cicchitelli G. Therapeutic effects of L-carnitine and propionyl-L-carnitine on cardiovascular diseases: a review. Ann N Y Acad Sci. 2004;1033:79–91. doi: 10.1196/annals.1320.007. [DOI] [PubMed] [Google Scholar]
- 16.Weil A. Angina. 2015 http://www.drweil.com/drw/u/ART00299/angina.html.
- 17.Arnold SV, Chan PS, Jones PG, Decker C, Buchanan DM, et al. Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH): design and rationale of a prospective multicenter registry. Circ Cardiovasc Qual Outcomes. 2011;4(4):467–476. doi: 10.1161/CIRCOUTCOMES.110.960468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weitz D, Weintraub H, Fisher E, Schwartzbard AZ. Fish oil for the treatment of cardiovascular disease. Cardiol Rev. 2010;18(5):258–263. doi: 10.1097/CRD.0b013e3181ea0de0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris WS, Dayspring TD, Moran TJ. Omega-3 fatty acids and cardiovascular disease: new developments and applications. Postgrad Med. 2013;125(6):100–113. doi: 10.3810/pgm.2013.11.2717. [DOI] [PubMed] [Google Scholar]
- 20.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 21.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Ware JEKM, Bjorner JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s Manual for the SF-36v2 Health Survey. 2. Lincoln, RI: QualityMetric Inc; 2007. pp. 125–133. Determining important differences scores. [Google Scholar]
- 23.Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–625. doi: 10.1097/01.ede.0000135174.63482.43. [DOI] [PubMed] [Google Scholar]
- 24.Grant SJ, Bin YS, Kiat H, Chang DH. The use of complementary and alternative medicine by people with cardiovascular disease: a systematic review. BMC Public Health. 2012;12:299. doi: 10.1186/1471-2458-12-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hui PN, Wan M, Chan WK, Yung PM. An evaluation of two behavioral rehabilitation programs, qigong versus progressive relaxation, in improving the quality of life in cardiac patients. J Altern Complement Med. 2006;12:373–378. doi: 10.1089/acm.2006.12.373. [DOI] [PubMed] [Google Scholar]
- 26.Ahn CM, Hong SJ, Choi SC, Park JH, Kim JS, Lim DS. Red ginseng extract improves coronary flow reserve and increases absolute numbers of various circulating angiogenic cells in patients with first ST-segment elevation acute myocardial infarction. Phytother Res. 2011;25:239–249. doi: 10.1002/ptr.3250. [DOI] [PubMed] [Google Scholar]
- 27.Liu Y, Zhang L, Liu YF, Yan FF, Zhao YX. Effects of Bulbus allii macrostemi on clinical outcomes and oxidized low-density lipoprotein and plasminogen in unstable angina/non-ST-segment elevation myocardial infarction patients. Phytother Res. 2008;22:1539–1543. doi: 10.1002/ptr.2534. [DOI] [PubMed] [Google Scholar]
- 28.Zhang YC, Chen RM, Lu BJ, Zhao MH, Rong YZ. Influence of shengmai capsule on recovery of living capacity in patients after myocardial infarction. Chin J Integr Med. 2009;15:333–336. doi: 10.1007/s11655-009-0333-3. [DOI] [PubMed] [Google Scholar]
- 29.MacLennan AH, Wilson DH, Taylor AW. The escalating cost and prevalence of alternative medicine. Prev Med. 2002;35:166–173. doi: 10.1006/pmed.2002.1057. [DOI] [PubMed] [Google Scholar]
- 30.Ernst E. Noncompliance with conventional medicine and use of complementary/alternative medicine. Journal of postgraduate medicine. 2007;53:85. doi: 10.4103/0022-3859.32204. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


