Abstract
Binge drinking is an increasingly common pattern of risky use associated with numerous health problems, including alcohol use disorders. Because low basal plasma levels of β-endorphin (β-E), and an increased β-E response to alcohol are evident in genetically at-risk human populations, this peptide is thought to contribute to the susceptibility for disordered drinking. Animal models suggest that the effect of β-E on consumption may be sex-dependent. Here, we studied binge-like EtOH consumption in transgenic mice possessing varying levels of β-E: wildtype controls with 100% of the peptide (β-E +/+), heterozygous mice constitutively modified to possess 50% of wildtype levels (β-E +/−), and mice entirely lacking the capacity to synthesize β-E (−/−). These three genotypes and both sexes were evaluated in a 4-day, 2-bottle choice, drinking in the dark (DID) paradigm with limited access to 20% EtOH. β-E deficiency determined sexually divergent patterns of drinking in that β-E −/− females drank more than their wildtype counterparts; an effect not observed in males. β-E −/− female mice also displayed elevated basal anxiety, plasma corticosterone, and corticotropin-releasing hormone (CRH) mRNA in the extended amygdala, and all of these were normalized by EtOH self-administration. These data suggest that a heightened risk for excessive EtOH consumption in female mice is related to the drug’s ability to ameliorate an overactive anxiety/stress-like state. Taken together, our study highlights a critical impact of sex on neuropeptide regulation of EtOH consumption.
Keywords: BNST, CeA, CRF, HPA-axis, POMC, stress
Introduction
The causes and consequences of drug use differ between men and women, though the mechanisms determining sex-dependent trajectories remain poorly understood. For example, a longstanding gap between the sexes in alcohol use disorders and their consequences has been shrinking as problematic incidence in females has risen over the past few years (Keyes et al. 2011). One possible contribution to this rise is an increase in female rates of binge drinking, a pattern that predicts negative health outcomes, including alcohol use disorders (Jennison 2004) According to the National Institute on Alcohol Abuse and Alcoholism, binge drinking is a pattern of excessive alcohol consumption that results in blood ethanol concentrations (BECs) of 80mg/dL or above; usually a result of a female having 4, or male having 5, drinks within about 2 hours (National Institute on Alcohol and Alcoholism Advisory Council 2004). Researchers hypothesize that females may be particularly susceptible to negative reinforcing effects of alcohol consumption because they are more prone to stress and anxiety (Lehavot et al. 2014).
The endogenous opioid peptide, β-endorphin (β-E), has long been implicated in EtOH consumption (Herz 1997). β-E, derived from the precursor proopiomelanocortin (POMC), is an agonist with high affinity for μ- and δ-opioid receptors (Raffin-Sanson et al. 2003) where it modulates EtOH (Gass & Olive 2007; Roth-Deri et al. 2008). In the clinic, basal levels of plasma β-E, as well as a rise in this peptide following alcohol administration, correlate with a heritable risk for high consumption (Dai et al. 2005; Kiefer et al. 2006). Our laboratory and others have demonstrated that β-E deficient mice exhibit altered patterns of EtOH consumption, which depend upon sex (Williams et al. 2007; Zhou et al. 2017) and a Pomc haplotype marker has been associated with human alcoholism in women, but not men (Racz et al. 2008). However, the mechanisms responsible for this interaction remain unknown.
β-E also regulates hypothalamic-pituitary-adrenal-axis (HPA-axis) activity via μ-opioid mediated inhibition (Buckingham 1986; Wynne & Sarkar 2013) influences basal anxiety-like behavior and EtOH-mediated anxiolysis (Grisel et al. 2008; Barfield et al. 2010; Barfield et al. 2013) and interacts with CRH in brain regions associated with stress and anxiety (Reyes et al. 2006; Lam & Gianoulakis 2011). Moreover, CRH signaling in the extended amygdala—comprised of the nucleus accumbens shell (NAc), bed nucleus of the stria terminalis (BNST), and central nucleus of the amygdala (CeA)—mediates binge-like EtOH consumption (Lowery-Gionta et al. 2012; Pleil et al. 2015; Rinker et al. 2017) and we recently observed increased Crh mRNA in the extended amygdala of β-E −/− female mice (McGonigle et al. 2016). Therefore, we hypothesized that binge-like drinking is regulated by sex and β-E through alterations in Crh expression and glucocorticoid secretion affecting stress circuitry and anxiety-like behavior.
Methods
Animals
Adult male and female C57BL/6J (β-E +/+), B6.129S2-Pomctm1Low/J (Stock number: 003191; β-E −/− mice), and heterozygous (β-E +/−) mice were either bred in-house and weaned at 21 days from stock obtained from Jackson Laboratories (Bar Harbor, ME) or purchased as adults from Jackson Laboratories in which case they were acclimated at least 10 days prior to the onset of any experimental procedures. The β-E deficient mice were developed in the laboratory of Malcolm Low and are now fully backcrossed onto a C57BL/6J background. Transgenic mice harbor a truncated Pomc transgene that prevents synthesis of β-E, although other POMC protein products remain unchanged, such that homozygotes cannot synthesize β-E and heterozygotes produce ~50% of wildtype levels (Rubinstein et al. 1996) β-E −/− males have been shown to exhibit an overweight phenotype that increases with age, although we observed no differences in weight across genotypes of either sex in the present study (supplemental results and Fig S1). Mice were group-housed by sex and genotype before the start of the experiment, and individually during the experiment, in Plexiglas® cages with corncob bedding and ad libitum access to chow and water. The animal colony and experimental room were maintained at ~21°C with a 12-h/12-h reverse light/dark cycle (lights off at 0930). All procedures were in accordance with the National Institute of Health guidelines and approved by the Bucknell University Institutional Animal Care and Use Committee.
Drinking in the Dark (DID) procedures
A 2-bottle, 4-day DID procedure was performed (Giardino & Ryabinin 2013) with water continuously available in one bottle for all mice. Mice were acclimated to individual housing for at least 7 days prior to the 4-day DID testing. On days 1–3 of DID testing, for 2hrs beginning 3hrs into the dark cycle, mice had access to two 25mL graduated cylinders containing either 20% EtOH in tap water (v/v) or tap water alone, while water control groups received tap water in both bottles. On day 4, access to EtOH or the additional water tube was extended to a 4hr binge test (BT) session. Sucrose control experiments were performed to assess whether differences in consumption between +/+ and −/− females were specific to EtOH. Animals underwent the same DID procedures, except that a 10% sucrose solution (w/v) was presented instead of a 20% EtOH solution. Fluid intake levels were measured by a trained observer blind to experimental condition by reading gradations on bottles with accuracy to the nearest 0.1mL.
Blood and tissue collection
Immediately following the 4hr BT on day 4, subjects were individually transported to an adjacent room, anesthetized using isoflurane, and rapidly decapitated. Trunk blood was collected and centrifuged to analyze plasma for blood EtOH concentrations (BEC; Analox Alcohol Analyzer, Analox Instruments, Stourbridge, UK) or stored at −20°C for subsequent processing of corticosterone (CORT) using an ELISA. Simultaneously, brains were removed, frozen on dry ice, and stored at −80° C for gene expression using qRT-PCR. Finally, left and right adrenal glands from each mouse were harvested and weighed. To control for potential effects of individual housing stress on CORT, a separate cohort of group-housed mice was sacrificed at the same time of day to assess homecage CORT.
Post-DID anxiety-like behavioral testing
To assess the behavioral effects of voluntary consumption and normalized CORT in β-E −/− females, we evaluated a separate cohort of β-E +/+ and β-E −/− females for anxiety-like behavior in the LDB following the EtOH DID procedure. Immediately following the BT on Day 4, subjects were transported to an adjacent room and placed in a LDB for 5 minutes (Grisel et al. 2008). Experimentally-blind observers scored time spent in the light and dark compartments and crossings between compartments were tallied as a measure of general locomotor activity. Immediately following LDB testing, animals were anesthetized, rapidly decapitated, and trunk blood was collected for analysis of BECs and CORT as described above.
Brain punch protocol and qRT-PCR
Frozen tissue was sliced on a Thermo Fisher HM 550 cryostat (Thermo Fisher Scientific, Waltham, MA) and bilateral 1.5mm cylindrical punches were taken of the NAc (AP: +1.94mm to +0.86mm; ML: ±0.75mm; DV: +1.0mm), BNST (AP: +0.62mm to −0.22mm; ML: ±1.0mm; DV +1.35mm), and CeA (AP: −0.82mm to −1.82mm, ML: ±2.35mm; DV: +1.25mm), relative to bregma, and immediately submerged in Qiazol lysis buffer (Qiagen GmbH, Hilden, Germany). Each sample tube containing one brain region from one mouse was homogenized immediately after sectioning. Total RNA was extracted using the Qiagen RNeasy Lipid Tissue Minikit (Qiagen GmbH, Hilden, Germany) according to manufacturer's instructions. Concentration and purity of eluted RNA was verified using the NanoDrop Lite UV spectrophotometer (Thermo Fisher Scientific, Waltham, MA) and five-hundred ng of total RNA was reverse-transcribed using the iScript™ cDNA Synthesis Kit (BioRad, Hercules, CA) also according to manufacturer's instructions. qRT-PCR was performed using FastStart Essential DNA Probes Master Mix (Roche Diagnostics, Indianapolis, IN) according to manufacturer's instructions. PrimeTime® XL qRT-PCR Assays designed by IDT (Integrated DNA Technologies, Coralville, IA) were performed using Crh (Assay ID: Mm.PT.58.32061593) and the reference gene, glyceraldehyde-3-phosphate dehydrogenase (GAPDH; Assay ID: Mm.PT.58.12733669) in duplicate on a LightCycler 96 (Roche Diagnostics, Indianapolis, IN). All assays had similar optimum PCR efficiencies. For all qRT-PCR experiments, GAPDH gene expression was used as the reference gene and relative changes in gene expression determined using the 2−ΔΔCT method (Schmittgen & Livak 2008).
Corticosterone ELISA
Corticosterone was measured by ELISA (Enzo Life Sciences, Farmingdale, NY), according to manufacturer’s instructions. Blood plasma was diluted 1:40 with assay buffer. Absorbance was read at 405nm using an iMark microplate reader (BioRad, Hercules, CA). Sample concentrations for corticosterone were calculated from a standard curve using GraphPad Prism version 7.0 software (GraphPad, La Jolla, CA). Assay sensitivity was 27pg/ml with a range of detection up to 20,000 pg/ml. All samples were assayed in duplicate.
Statistical analysis
Repeated measures (RM) ANOVAs with sex and genotype as factors were used to analyze EtOH consumption and preference, and sucrose consumption (only females) across days 1–3 of the DID paradigm. 2-way ANOVAs with genotype and sex as factors were used to analyze EtOH consumption and preference on the day-4 BT, average EtOH consumption and preference, average weight, and homecage CORT. 3-way ANOVAs with sex, genotype, and treatment as factors were used to analyze CORT, adrenal weights, and Crh expression in the NAc, BNST, and CeA. Simple linear regression was used to analyze relationships between BECs and anxiety-like behavior. Unpaired two-tailed t-tests were used to analyze genotype differences in anxiety-like behavior and locomotor activity in the LDB, and average and BT sucrose consumption. An F-test for equality of variances was used to compare variances in CORT levels in β-E −/− females based on intoxication threshold. Bonferroni post hoc tests were used to correct for multiple comparisons following significant main effects and interactions. Degrees of freedom may differ between groups/brain regions due to unquantifiable tissue or blood plasma samples. All data were analyzed using SPSS 24.0 software and GraphPad Prism 7.0. Data are presented as Mean±SEM. Effects were considered statistically significant at p ≤ 0.05.
Results
β-E deficiency promotes enhanced binge-like EtOH consumption in female, but not male mice
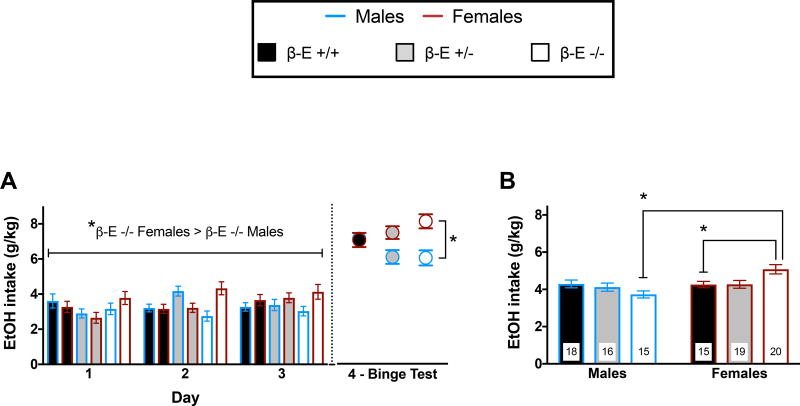
We evaluated male and female β-E +/+, β-E +/−, and β-E −/− mice in the DID model of binge drinking to test the hypothesis that β-E regulates binge-like EtOH consumption in a sexually dimorphic manner. Binge EtOH consumption across the 2hr periods (days 1–3), the 4hr BT (day 4), and average consumption are summarized in Figure 1 (n = 15–20/group). A RM ANOVA on days 1–3 revealed a significant sex by genotype interaction (F(2,97) = 5.648, p = 0.005). All other main effects and interactions were not significant – day (F(2,194) = 1.803, p = 0.167), day by genotype (F(4,194) = 2.197, p = 0.071), day by sex (F(2,194) = 1.724, p = 0.181), day by genotype by sex (F(4,194) = 1.476, p = 0.211), genotype (F(2,97) = 0.426, p = 0.654), and sex (F(1,97) = 2.532, p = 0.115). Post hoc analysis following the sex by genotype interaction indicated that β-E −/− females consumed more EtOH than β-E −/− males across days 1–3 (p <0.05). A 2-way ANOVA on day 4 BT revealed a main effect of sex (F(1,97) = 12.317, p = 0.001) and a sex by genotype interaction (F(2,97) = 3.853, p = 0.025), but no main effect of genotype (F(2,97) = 0.394, p = 0.675). Post hoc analyses following the sex by genotype interaction indicated that β-E −/− females consumed more EtOH than β-E −/− males during the BT (p < 0.05; Fig 1A). To determine the overall effect of β-E on binge-like EtOH consumption we analyzed average EtOH consumption across the 4-day DID paradigm. A 2-way ANOVA revealed a main effect of sex (F(1,97) = 7.631, p = 0.006) and a sex by genotype interaction (F(2, 97) = 5.962, p = 0.003), but no main effect of genotype (F(2, 97) = 0.476, p = 0.622). Post hoc analyses following the sex by genotype interaction indicated that β-E −/− females consumed more EtOH than β-E +/+ females (p < 0.05) and β-E −/− males (p < 0.05; Fig 1B). EtOH preference data from these experiments can be found in the supplemental results and Fig S2. We also conducted sucrose control experiments in a separate cohort of β-E +/+ and −/− females to assess whether differences in consumption were specific to EtOH. These data are presented in the supplemental results and Fig S4.
Figure 1. β-E masks sex differences in binge-like EtOH drinking.
(A) Daily consumption of 20% EtOH vs water across the 2hr sessions (days 1–3) and 4hr binge test (day 4) of the DID procedure. A RM ANOVA across days 1–3 revealed a significant sex by genotype interaction and post hoc analysis indicated that β-E −/− females consumed more EtOH than β-E −/− males. A 2-way ANOVA on the day-4 BT revealed a main effect of sex (females > males) and a sex by genotype interaction There was a main effect of sex and a sex by genotype interaction for the 4hr BT. Post hoc analysis indicated that β-E −/− females consumed more EtOH than β-E −/− males. These data are summarized in (B) as average consumption across the 4-day paradigm. There was a main effect of sex (females > males) and a sex by genotype interaction with Post hoc analysis indicated that β-E −/− females consumed more EtOH overall than β-E +/− and β-E +/+ females and β-E −/− males. Data are presented as Means±SEM; *p < 0.05 (Bonferroni corrected); n’s for each group are displayed within their respective bar.
Binge-like EtOH consumption normalizes elevated CORT levels in female, but not male, β-E −/− mice
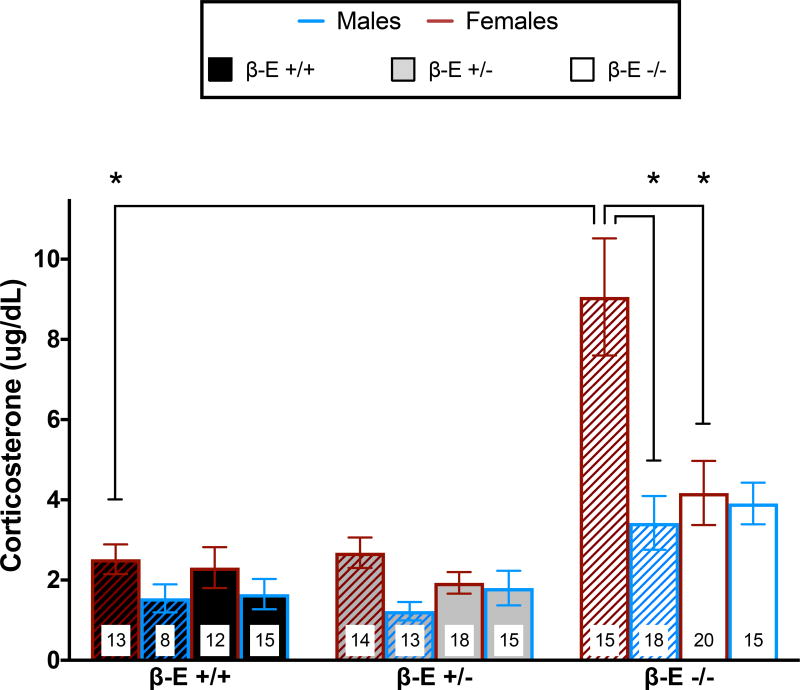
To determine the role of HPA-axis activity in the sexually divergent pattern of EtOH consumption, we assessed plasma CORT levels immediately following water or EtOH consumption on the day 4 BT. A 3-way ANOVA revealed main effects of genotype (F(2,159) = 30.688, p < 0.001) and sex (F(1,159) = 14.730, p < 0.001), but not treatment (F(1,159) = 3.854, p = 0.051). There were also significant interactions of genotype by sex (F(2,159) = 3.470, p = 0.033), genotype by treatment (F(2, 159) = 3.440, p = 0.034), sex by treatment (F(1, 159) = 8.721, p = 0.004), and genotype by sex by treatment (F(2, 159) = 3.934, p = 0.022). Post hoc analysis following the 3-way interaction indicated that water control β-E −/− females have higher CORT levels than β-E +/+ water control females (p <0.05) and water control β-E −/− males (p <0.05). However, CORT levels are reduced by EtOH drinking in β-E −/− females to levels similar to wildtype females (p > 0.05; Fig 2). To control for potential effects of individual housing, we also measured CORT levels in a separate cohort of naive, water-drinking group-housed male and female β-E +/+ and −/− mice (see supplemental results and Fig S3).
Figure 2. Binge-like EtOH consumption normalizes CORT in female, but not male β-E −/− mice.
Plasma CORT levels obtained immediately following the day-4 BT from β-E +/+, +/−, and −/− female and male mice consuming either EtOH & water (solid bars) or water controls (hatched bars). A 3-way ANOVA revealed a significant genotype by sex by treatment interaction. Post hoc analysis indicated that β-E −/− females exhibit greater CORT than β-E +/+ females and β-E −/− males under basal conditions, but voluntary binge-like EtOH consumption significantly reduces β-E −/− female CORT levels to near wildtype levels. Data are presented as Means±SEM; *p < 0.05 (Bonferroni corrected); n’s for each group are displayed within their respective bar.
Anxiolytic effects of EtOH in female mice depend upon β-E
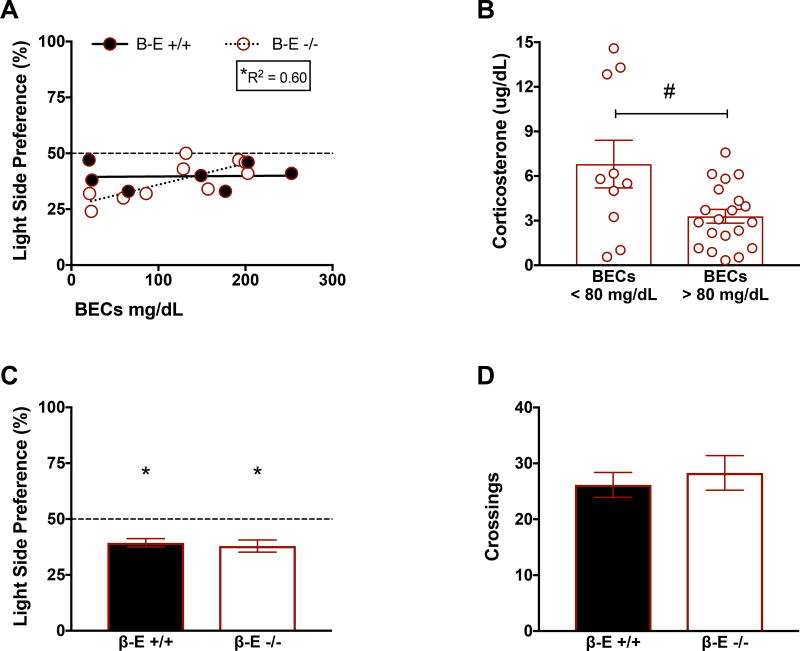
Previous research had demonstrated an inverse relationship between β-E levels and anxiety-like behaviors in these lines (Grisel et al. 2008; Barfield et al. 2010; Barfield et al. 2013) but in order to assess the behavioral relevance of the physiological changes in endocrine measures, we tested a separate group containing only female +/+ and −/− mice for anxiety-like behavior in the light-dark box (LDB) after the 4-day DID procedure. Linear regression revealed a significant relationship between BECs and preference for the light side of a LDB in β-E −/− females (F(1,8) = 12.02, p = 0.0085, R2 = 0.60), but not β-E +/+ females (F(1,5) = 0.008, p = 0.93), supporting the contention that β-E −/− females exhibit heightened sensitivity to the anxiolytic effects of EtOH (Fig 3A). One-sample t-tests revealed that mean light side preference was significantly less than 50% for both genotypes [β-E +/+ (t(7) = 5.71, p = 0.0007); β-E −/− (t(9) = 4.432, p = 0.0016)] and an unpaired t-test revealed no differences between genotypes (t(16) = 0.423, p = 0.6779), suggesting that both groups exhibited similar anxiety-like behavior in the LDB on average (Fig 3C). An unpaired t-test also indicated that there were no genotype differences in locomotor activity, as assessed by crossings between light/dark compartments (t(15) = 0.5176, p = 0.612; Fig 3D).
Figure 3. β-E −/− females exhibit increased sensitivity to EtOH’s anxiolytic effects.
(A) Linear regressions depicting the relationship between BECs and preference for the light side of the LDB in β-E +/+ and −/− females immediately following the BT. There was a significant positive relationship between degree of intoxication (BECs) and reduced anxiety-like behavior in β-E −/−, but not β-E +/+, females suggesting that β-E −/− females exhibited greater EtOH-mediated anxiolysis. The dashed line represents the value at which equal time is spent in both compartments of the LDB; *denotes a significant regression and corresponding goodness of fit value. (B) Because the only significant regressions between BECs and CORT were observed in β-E −/− females (see Results) we further explored the effect of EtOH consumption on CORT. All β-E −/− females were split into two groups based on intoxication threshold (BECs < 80mg/dL and BECs > 80mg/dL) and CORT levels were compared. β-E −/− females that achieved intoxication tended to exhibit reduced CORT, relative to β-E −/− females that did not, although this did not reach statistical significance (p = 0.060). However, an F-test comparing variances indicated that β-E −/− females with BECs > 80mg/dL exhibited significantly reduced variability in CORT levels, relative to β-E −/− females with BECs < 80mg/dL (#p = 0.05). (C) Mean summary of data in (A) indicating that overall, both β-E +/+ and −/− exhibited anxiety-like behavior in the LDB, however there was no significant difference between genotypes. *denotes mean light side preference significantly lower than the null hypothesis of 50%. (D) There was also no significant genotype difference in locomotor activity, assessed by crossings, during LDB testing. Data are presented as Means±SEM.
To further explore the relationship between binge-like drinking and CORT, we ran a linear regression that revealed a significant relationship between BECs and CORT solely in β-E −/− females (F(1,29) = 5.721, p = 0.023, R2 = 0.16; not shown). All other regressions were nonsignificant [β-E −/− males (F(1,13) = 1.187, p = 0.295), β-E +/+ males (F(1,12) = 3.04, p = 0.10) and females (F(1,17) = 0.568, p = 0.461), and β-E +/− males (F(1,13) = 0.043, p = 0.837) and females (F(1,16) = 1.595, p = 0.224)). We next split β-E −/− females based on level of intoxication, those with BECs < 80mg/dL or > 80mg/dL, and analyzed CORT as a function of pharmacological intoxication. An unpaired t-test with Welch’s correction revealed a strong trend for reduced CORT only in β-E −/− females that achieved intoxication (t(10.54) = 2.105, p = 0.060), although this did not reach statistical significance. However, an F-test to compare variances indicated that variance in β-E −/− females achieving intoxicating BECs (Mean±SEM = 3.294±0.463, n =20) was significantly reduced relative to β-E −/− females that did not achieve intoxication (Mean±SEM = 6.802 ±1.601, n =10; F(9,19) = 5.968, p = 0.001), suggesting that intoxicating doses of EtOH serve to reduce the variability of glucocorticoid secretion in β-E −/− females (Fig 3B).
β-E −/− mice have elevated BNST Crh expression, which is normalized by binge-like EtOH consumption
To determine a potential mechanism underlying the enhanced EtOH consumption and elevated CORT levels in β-E −/− females we used qRT-PCR to analyze Crh mRNA in the NAc, BNST, and CeA in a subset of male and female β-E +/+, β-E +/−, and β-E −/− mice from the water and EtOH DID experiments. Our hypothesis was focused on the BNST and CeA, and the NAc was included as a neuroanatomical control region. However, we did observe changes in this forebrain region that were dependent upon sex (see supplemental results and Fig S5).
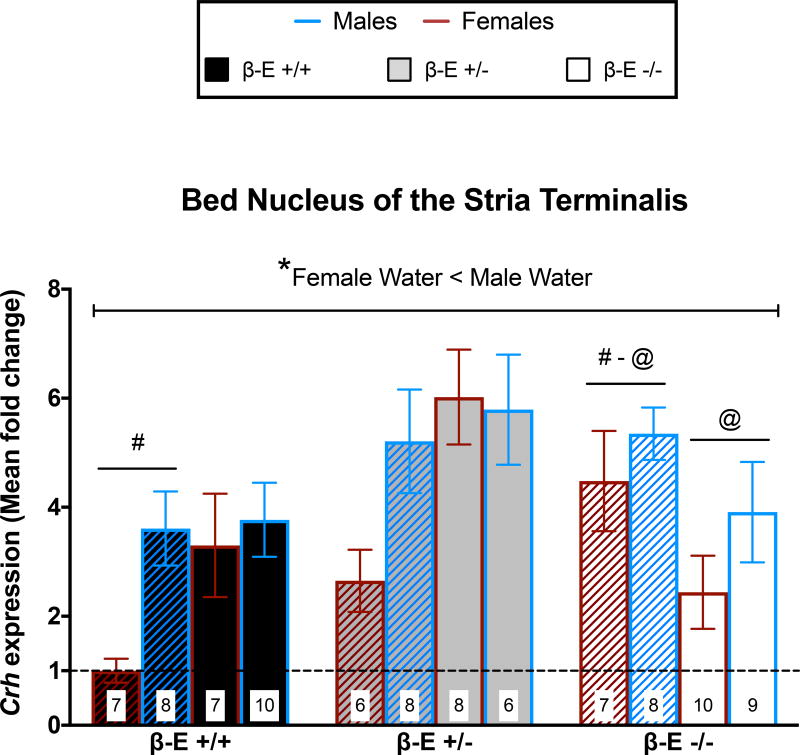
A 3-way ANOVA on BNST Crh revealed significant main effects of genotype (F(2,82) = 7.020, p = 0.002) and sex (F(1,82) = 10.857, p = 0.001), but not treatment (F(1,82) = 0.531, p = 0.468). There was also significant genotype by treatment (F(2, 82) = 9.242, p < 0.001) and sex by treatment (F(1, 82) = 3.979, p = 0.049) interactions, but not genotype by sex (F(2, 82) = 1.226, p = 0.299) or genotype by sex by treatment (F(2, 82) = 1.741, p = 0.182). Post hoc analysis following the genotype by treatment interaction indicated that β-E −/− water controls have higher Crh expression than β-E +/+ water controls (p < 0.05). However, in EtOH drinking β-E −/− mice Crh expression is reduced, relative to β-E −/− water controls (p < 0.05), to levels similar to β-E +/+ EtOH drinking mice (p > 0.05), suggesting that β-E −/− mice exhibit elevated BNST Crh under basal conditions, but binge-like EtOH drinking normalizes Crh. Post hoc analyses following the sex by treatment interaction indicated that male water controls have higher BNST Crh than female water controls (p < 0.05), suggesting that under basal conditions females have less Crh mRNA in the BNST than males (Fig 4).
Figure 4. β-E −/− mice have elevated BNST Crh under basal conditions, but binge-like ethanol consumption normalizes Crh expression.
Crh mRNA expression from mice consuming either EtOH & water (solid bars) or water controls (hatched bars) is represented as Mean fold change(±SEM) normalized to β-E +/+ female water mice as indicated by the dashed line. A 3-way ANOVA revealed a genotype by treatment interaction and a sex by treatment interaction. Post hoc analysis following the genotype by treatment interaction indicated that β-E −/− water controls exhibit increased Crh expression, relative to β-E +/+ water controls. However, binge-like EtOH consumption reduced Crh in β-E −/−, relative to water controls, such that there was no longer a genotype difference in BNST Crh expression. Note that these effects are primarily driven by differences in females, however the lack of a significant 3-way interaction precluded our ability to statistically assess such comparisons. Although, post hoc analysis following the sex by treatment interaction indicated that, overall, female water controls have lower BNST Crh mRNA than male water controls (*), which provides novel evidence for basal sex differences in BNST Crh expression. Like symbols indicate significant differences between groups (p < 0.05; Bonferroni corrected); n’s for each group are displayed within their respective bar.
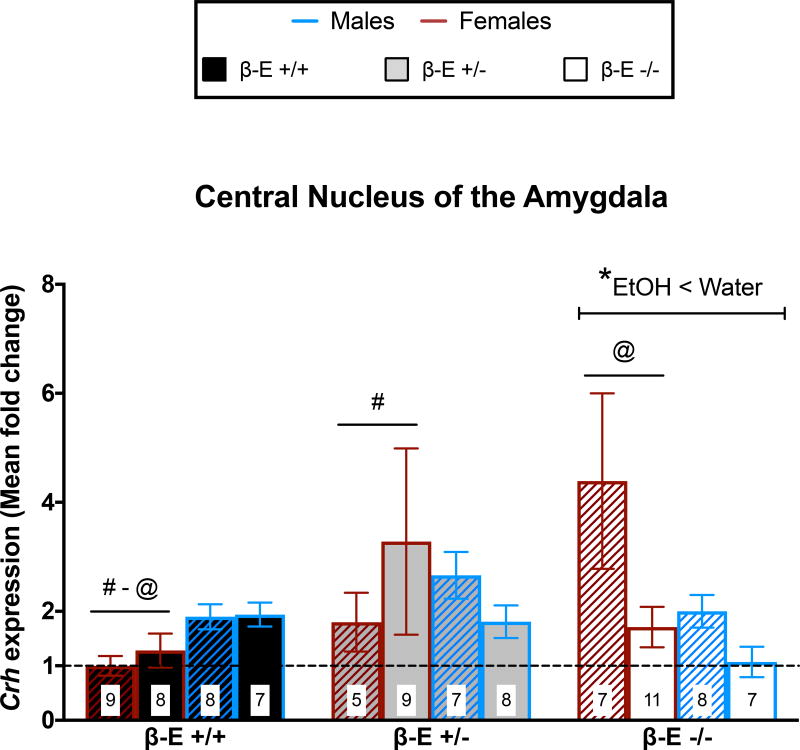
β-E levels negatively correlate with CeA Crh expression in female, but not male, mice
A 3-way ANOVA on CeA Crh revealed significant genotype by sex (F(2, 82) = 4.478, p = 0.014) and genotype by treatment (F(2, 82) = 4.577, p = 0.013) interactions. All other main effects and interactions were not significant – genotype (F(2, 82) = 3..040, p = 0.053), sex (F(1, 82) = 0.287, p = 0.594), treatment (F(1, 82) = 2.508, p = 0.117), sex by treatment (F(1, 82) = 0.917, p = 0.341), and genotype by sex by treatment (F(2, 82) = 1.673, p = 0.194). Post hoc analyses following the genotype by sex interaction indicated that β-E −/− and β-E +/− females had greater CeA Crh expression than β-E +/+ females (p < 0.05), suggesting that β-E negatively correlates with CeA Crh in female, but not male, mice. Post hoc analyses following the genotype by treatment interaction indicated that EtOH drinking β-E −/− mice had lower Crh than β-E −/− water controls (p < 0.05), suggesting that in β-E −/− mice binge-like EtOH consumption reduces Crh expression in the CeA (Fig 5).
Figure 5. Sex differences in CeA Crh mRNA: β-E is inversely associated with CeA Crh in females, but not males.
Crh mRNA expression from mice consuming either EtOH & water (solid bars) or water controls (hatched bars) is represented as Mean fold change(±SEM) normalized to β-E +/+ female water mice as indicated by the dashed line. A 3-way ANOVA revealed a genotype by sex interaction and a genotype by treatment interaction. Post hoc analysis following the genotype by sex interaction indicated that β-E −/− and β-E +/− females exhibit higher CeA Crh than β-E +/+ females, however these effects were not observed in males. Post hoc analysis following the genotype by treatment interaction indicated that binge-like EtOH consumption reduced Crh only in β-E −/− mice (*), which was likely driven by the magnitude of reduction in β-E −/− females. Like symbols indicate significant differences between groups (p < 0.05; Bonferroni corrected); n’s for each group are displayed within their respective bar.
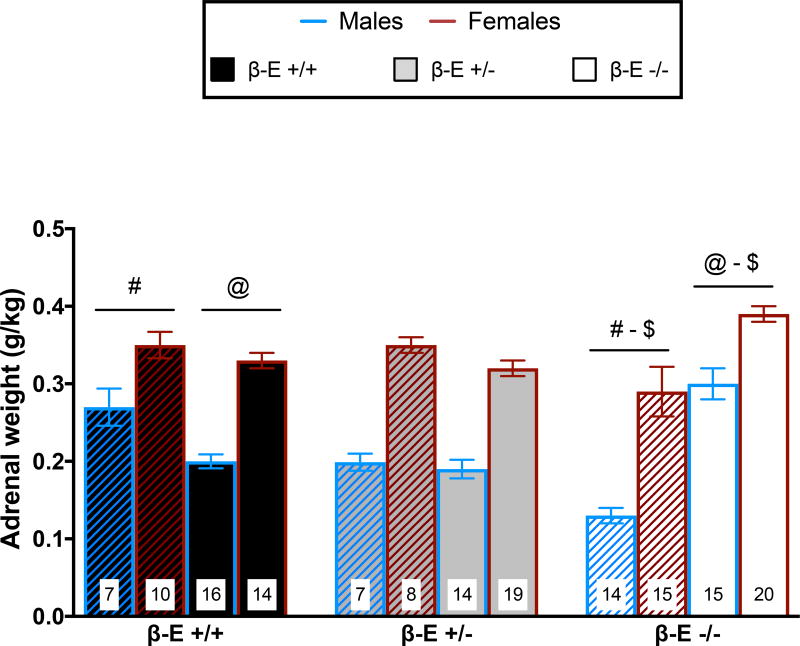
Adrenal glands of β-E deficient mice are more sensitive to EtOH-induced alterations
We previously observed increased adrenal gland weight in β-E deficient mice following EtOH exposure (Grisel et al. 2008; McGonigle et al. 2016) but did not explore basal or sex differences. Therefore, immediately following the BT on day 4, the left and right adrenal glands were harvested and total adrenal weight (normalized by body weight, g/kg) was calculated and is summarized in Figure 6. A 3-way ANOVA revealed a main effect of sex (F(1, 144) = 103.975, p < 0.001), indicating female adrenals weighed more than male adrenals, and a significant genotype by treatment interaction (F(2, 144) = 21.445, p < 0.001). No other main effects or interactions were significant: genotype (F(2, 144) = 1.251, p = 0.289), treatment (F(1, 144) = 2.662 p = 0.105), genotype by sex (F(2, 144) = 1.112, p = 0.332), sex by treatment (F(1, 144) = 0.015, p = 0.902), and genotype by sex by treatment (F(2, 144) = 1.712, p = 0.184). Post hoc analysis following the genotype by treatment interaction indicated that water control β-E −/− mice have smaller adrenals than β-E +/+ water controls (p < 0.05). However, binge-like EtOH drinking increases adrenal size in β-E −/− mice (p < 0.05), such that EtOH drinking β-E −/− mice exhibit larger adrenals than EtOH drinking β-E +/+ mice (p < 0.05).
Figure 6. β-E −/− mice exhibit heightened sensitivity to EtOH-induced changes in adrenal gland size.
Total adrenal gland weight (Mean±SEM, normalized by body weight) from mice consuming either EtOH & water (solid bars) or water controls (hatched bars). A 3-way ANOVA revealed a main effect of sex, indicated that overall females have larger adrenals than males, and a genotype by treatment interaction. Post hoc analysis following the genotype by treatment interaction indicated that β-E −/− water controls have smaller adrenals than β-E +/+ water controls. However, binge-like EtOH consumption increased adrenal size only in β-E −/− mice, relative to β-E −/− water controls, which resulted in β-E −/− EtOH mice possessing larger adrenals than β-E +/+ EtOH mice. Like symbols indicate significant differences between groups (p < 0.05; Bonferroni corrected); n’s for each group are displayed within their respective bar.
Discussion
We investigated behavioral, neuroendocrine, and genetic substrates of EtOH consumption in a binge-drinking model that reliably produces pharmacological intoxication (Giardino & Ryabinin 2013). Using transgenic mice (Rubinstein et al. 1996) we show that β-E deficiency results in sexually divergent patterns of EtOH consumption with corresponding alterations in HPA-axis activity and Crh expression in the extended amygdala.
β-E deficiency enhances voluntary binge-like EtOH consumption in female, but not male, mice. β-E −/− females also exhibit elevated CORT, which is normalized by voluntary EtOH drinking, coincident with a decrease in anxiety-like behavior. Under basal (i.e., water-drinking) conditions, β-E −/− mice exhibit increased BNST Crh expression, and EtOH consumption obviates this difference. Similarly, β-E levels negatively correlate with CeA Crh expression in females, but not males, and the elevated basal expression is normalized following EtOH consumption. β-E −/− mice also exhibit heightened sensitivity to EtOH-induced changes in adrenal gland size. These data suggest that genetic and neuroendocrine markers of exaggerated stress sensitivity correlate with binge-like EtOH drinking, perhaps contributing to sex-dependent trajectories in alcohol use disorders. We also provide novel evidence for sex differences in Crh expression. That is, females have lower basal BNST Crh than males, but this difference is abolished following binge-like EtOH consumption.
Previous research demonstrated that β-E influences EtOH consumption (Grisel et al. 1999; Racz et al. 2008) and that the peptide’s impact may be sex dependent (Williams et al. 2007; Zhou et al. 2017). β-E is synthesized in both hypothalamic and pituitary neurons, but since we used a global knockout the current study does not delineate the source of influence (Logan et al. 2015). However, Zhou et al. (2017) did not see an effect of a pituitary-specific POMC knockout on drinking in the DID model. Variations in β-E also influence anxiety-like behavior sex-dependently, as β-E −/− females display heightened stress responses relative to other groups (Grisel et al. 2008; Barfield et al. 2010; Barfield et al. 2013). In the present study we demonstrate that β-E −/− females also exhibit ~2–3-fold increases in plasma CORT and Crh mRNA in the BNST and CeA compared to wildtype females. Because the BNST and CeA regulate stress, anxiety, and alcohol-related behaviors, primarily through CRH signaling (Gilpin et al. 2015; Vranjkovic et al. 2017), these differences are likely to contribute to high-drinking, high-stress phenotype of β-E −/− females. The BNST regulates HPA-axis activation via excitatory and inhibitory projections to the paraventricular nucleus of the hypothalamus (PVN) and the CeA can modulate these inputs via GABAergic projections to the BNST (Choi et al. 2007). Both CRH and EtOH can increase CeA GABAergic transmission onto inhibitory PVN-projecting BNST neurons, resulting in disinhibition of PVN CRH neurons and activation of the HPA-axis (Gilpin 2012). Thus, increased Crh in the CeA and/or BNST of β-E −/− females may explain elevations in basal CORT. While acute EtOH has also been shown to increase adrenal size, the increase in β-E −/− mice, following only 4 days of EtOH drinking, suggests they exhibit enhanced adrenal sensitivity to EtOH, which might be associated with their dysregulated HPA-axis activity (Rivier & Vale 1985; Rasmussen et al. 2000).
Elevated CRH in the BNST and CeA are hallmarks of a negative affective state that drives excessive EtOH consumption, presumably to alleviate the associated symptoms (Koob 2013). Toward that end, Olive and colleagues demonstrated that extracellular levels of CRH increase during EtOH withdrawal, and that subsequent consumption following reintroduction of EtOH reduced CRH to basal levels (Olive et al. 2002) a pattern observed with CORT levels and Crh mRNA in our β-E −/− female mice following binge EtOH consumption. Moreover, chemogenetic inhibition of BNST CRH neurons reduces binge-like EtOH consumption, suggesting a causal role for BNST CRH signaling in regulating excessive drinking (Pleil et al. 2015; Rinker et al. 2017). Similarly, extracellular CRH in the CeA also increases during EtOH withdrawal, and immunoreactivity in the CeA is upregulated following binge-like EtOH consumption, but blockade of CRH1 receptors in the CeA prevents the excessive EtOH consumption associated with these effects (Funk et al. 2006; Lowery-Gionta et al. 2012). Taken together, these findings suggest a potential mechanism that puts β-E −/− females at increased risk for binge-like EtOH consumption.
The tension reduction hypothesis proposes that the motivation to consume alcohol manifests from a desire to reduce stress and anxiety (Cappell & Herman 1972) a clinical phenomenon that is more pronounced in female subjects (Sinha et al. 1998). In addition, rodents displaying heightened anxiety-like behavior are more susceptible to the anxiolytic effects of EtOH (Stewart et al. 1993; Grisel et al. 2008) and anxiety-like behavior has been shown to predict high levels of EtOH consumption and preference (Spanagel et al. 1995). The present results suggest that low β-E confers elevated anxiety-like behavior and enhanced EtOH-mediated anxiolysis in females, which corresponds with clinical data correlating low plasma β-E with anxiety and negative affect-related psychopathologies (Dai et al. 2005; Merenlender-Wagner et al. 2009).
Similarly, stress also modulates EtOH intake, often leading to increases in consumption and instigating alcohol seeking behavior (Spanagel et al. 2014). Stress-induced EtOH consumption is regulated by glucocorticoids (Ostroumov et al. 2016) suggesting that the elevated glucocorticoid tone in β-E −/− females may contribute to their increased EtOH consumption.
Conclusions
Females experience increased susceptibility for many stress-related psychiatric disorders, which often co-occur with alcohol use disorders and exacerbate excessive alcohol use (McLean et al. 2011). Despite formidable evidence that females are more sensitive to stress, alcohol, and their interaction (Logrip et al. 2017) the neural mechanisms underlying sex-specific regulation of alcohol use have been poorly understood. The present findings help fill this gap by demonstrating sexually dimorphic neuropeptide regulation of EtOH sensitivity.
Our data suggest that sex and β-E interact to determine sexually dimorphic effects on excessive alcohol consumption, and tie this tendency to heightened HPA-axis activity, enhanced EtOH-mediated anxiolysis, and elevated Crh in the BNST and CeA. Given the importance of neuropeptide signaling in EtOH-related behaviors (Koob 2013) it seems plausible that other neuropeptides also demonstrate distinct sex-specific effects. Taken together, our observations shed light on the previously unknown impact of sex and β-E on EtOH consumption and suggest understanding the trajectory toward disordered drinking may depend on better knowledge of sex-dependent substrates.
Supplementary Material
Acknowledgments
This work was supported by the National Institute on Alcohol Abuse and Alcoholism (R15 AA022506). The authors would like to thank David Freestone for discussions regarding statistics; Colleen McGonigle for her technical assistance and help with data collection; Grace Leung, Bernadette Chaney, Kiarah Leonard, and Ellie Mack for their assistance with sample collection and data entry.
Footnotes
The authors have no conflicts of interest to disclose.
Authors contribution:
TBN performed data acquisition, DEW assisted with qRT-PCR data collection. TBN, EMR, and JEG designed the study and performed data analysis. TBN and JEG wrote the manuscript. All authors critically reviewed content and approved final version for publication.
References
- Barfield ET, Barry SM, Hodgin HB, Thompson BM, Allen SS, Grisel JE. Beta-endorphin mediates behavioral despair and the effect of ethanol on the tail suspension test in mice. Alcoholism, clinical and experimental research. 2010;34:1066–72. doi: 10.1111/j.1530-0277.2010.01182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barfield ET, Moser VA, Hand A, Grisel JE. β-endorphin modulates the effect of stress on novelty-suppressed feeding. Frontiers in behavioral neuroscience. 2013;7:19. doi: 10.3389/fnbeh.2013.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckingham JC. Stimulation and inhibition of corticotrophin releasing factor secretion by beta endorphin. Neuroendocrinology. 1986;42:148–52. doi: 10.1159/000124266. [DOI] [PubMed] [Google Scholar]
- Cappell H, Herman CP. Alcohol and tension reduction. A review. Q J Stud Alcohol. 1972;33:33–64. [PubMed] [Google Scholar]
- Choi D, Furay A, Evanson N, Ostrander M, Ulrich-Lai Y, Herman J. Bed Nucleus of the Stria Terminalis Subregions Differentially Regulate Hypothalamic–Pituitary–Adrenal Axis Activity: Implications for the Integration of Limbic Inputs. J Neurosci. 2007;27:2025–2034. doi: 10.1523/JNEUROSCI.4301-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai X, Thavundayil J, Gianoulakis C. Differences in the peripheral levels of beta-endorphin in response to alcohol and stress as a function of alcohol dependence and family history of alcoholism. Alcohol Clin Exp Res. 2005;29:1965–75. doi: 10.1097/01.alc.0000187599.17786.4a. [DOI] [PubMed] [Google Scholar]
- Funk CK, O'Dell LE, Crawford EF, Koob GF. Corticotropin-releasing factor within the central nucleus of the amygdala mediates enhanced ethanol self-administration in withdrawn, ethanol-dependent rats. J Neurosci. 2006;26:11324–11332. doi: 10.1523/JNEUROSCI.3096-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gass JT, Olive MF. Effects of immunoneutralization of beta-endorphin in the nucleus accumbens on intravenous ethanol self-administration in rats. Alcoholism, clinical and experimental research. 2007;31:87A. doi: 10.1111/j.1530-0277.2007.00480.x. [DOI] [PubMed] [Google Scholar]
- Giardino WJ, Ryabinin AE. CRF1 receptor signaling regulates food and fluid intake in the drinking-in-the-dark model of binge alcohol consumption. Alcoholism, clinical and experimental research. 2013;37:1161–70. doi: 10.1111/acer.12076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin NW. Corticotropin-releasing factor (CRF) and neuropeptide Y (NPY): effects on inhibitory transmission in central amygdala, and anxiety- & alcohol-related behaviors. Alcohol. 2012;46:329–37. doi: 10.1016/j.alcohol.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin NW, Herman MA, Roberto M. The central amygdala as an integrative hub for anxiety and alcohol use disorders. Biol Psychiatry. 2015;77:859–69. doi: 10.1016/j.biopsych.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grisel JE, Bartels JL, Allen SA, Turgeon VL. Influence of beta-Endorphin on anxious behavior in mice: interaction with EtOH. Psychopharmacology. 2008;200:105–15. doi: 10.1007/s00213-008-1161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grisel JE, Mogil JS, Grahame NJ, Rubinstein M, Belknap JK, Crabbe JC, Low MJ. Ethanol oral self-administration is increased in mutant mice with decreased beta-endorphin expression. Brain Res. 1999;835:62–7. doi: 10.1016/s0006-8993(99)01384-0. [DOI] [PubMed] [Google Scholar]
- Herz A. Endogenous opioid systems and alcohol addiction. Psychopharmacology. 1997;129:99–111. doi: 10.1007/s002130050169. [DOI] [PubMed] [Google Scholar]
- Jennison KM. The short-term effects and unintended long-term consequences of binge drinking in college: a 10-year follow-up study. Am J Drug Alcohol Abuse. 2004;30:659–84. doi: 10.1081/ada-200032331. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: a review and synthesis. Alcoholism, clinical and experimental research. 2011;35:2101–2112. doi: 10.1111/j.1530-0277.2011.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiefer F, Jahn H, Otte C, Nakovics H, Wiedemann K. Effects of treatment with acamprosate on beta-endorphin plasma concentration in humans with high alcohol preference. Neurosci Lett. 2006;404:103–6. doi: 10.1016/j.neulet.2006.05.015. [DOI] [PubMed] [Google Scholar]
- Koob GF. Addiction is a Reward Deficit and Stress Surfeit Disorder. Front Psychiatry. 2013;4:72. doi: 10.3389/fpsyt.2013.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam MP, Gianoulakis C. Effects of acute ethanol on corticotropin-releasing hormone and β-endorphin systems at the level of the rat central amygdala. Psychopharmacology. 2011;218:229–39. doi: 10.1007/s00213-011-2337-x. [DOI] [PubMed] [Google Scholar]
- Lehavot K, Stappenbeck CA, Luterek JA, Kaysen D, Simpson TL. Gender differences in relationships among PTSD severity, drinking motives, and alcohol use in a comorbid alcohol dependence and PTSD sample. Psychol Addict Behav. 2014;28:42–52. doi: 10.1037/a0032266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan RW, Wynne O, Maglakelidze G, Zhang C, O'Connell S, Boyadjieva NI, Sarkar DK. β-Endorphin neuronal transplantation into the hypothalamus alters anxiety-like behaviors in prenatal alcohol-exposed rats and alcohol-non-preferring and alcohol-preferring rats. Alcohol Clin Exp Res. 2015;39:146–157. doi: 10.1111/acer.12611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logrip ML, Oleata C, Roberto M. Sex differences in responses of the basolateral-central amygdala circuit to alcohol, corticosterone and their interaction. Neuropharmacology. 2017;114:123–134. doi: 10.1016/j.neuropharm.2016.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowery-Gionta EG, Navarro M, Li C, Pleil KE, Rinker JA, Cox BR, Sprow GM, Kash TL, Thiele TE. Corticotropin Releasing Factor Signaling in the Central Amygdala is Recruited during Binge-Like Ethanol Consumption in C57BL/6J Mice. J Neurosci. 2012;32:3405–3413. doi: 10.1523/JNEUROSCI.6256-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGonigle CE, Nentwig TB, Wilson DE, Rhinehart EM, Grisel JE. β-endorphin regulates alcohol consumption induced by exercise restriction in female mice. Alcohol (Fayetteville, NY) 2016;53:51–60. doi: 10.1016/j.alcohol.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45:1027–35. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merenlender-Wagner A, Dikshtein Y, Yadid G. The beta-endorphin role in stress-related psychiatric disorders. Curr Drug Targets. 2009;10:1096–108. doi: 10.2174/138945009789735147. [DOI] [PubMed] [Google Scholar]
- National Institue on Alcohol Abuse and Alcoholism. NIAAA council approves definition of binge drinking. NIAAA Newsletter. 2004;3:3. [Google Scholar]
- Olive MF, Koenig HN, Nannini MA, Hodge CW. Elevated extracellular CRF levels in the bed nucleus of the stria terminalis during ethanol withdrawal and reduction by subsequent ethanol intake. Pharmacol Biochem Behav. 2002;72:213–20. doi: 10.1016/s0091-3057(01)00748-1. [DOI] [PubMed] [Google Scholar]
- Ostroumov A, Thomas AM, Kimmey BA, Karsch JS, Doyon WM, Dani JA. Stress Increases Ethanol Self-Administration via a Shift toward Excitatory GABA Signaling in the Ventral Tegmental Area. Neuron. 2016;92:493–504. doi: 10.1016/j.neuron.2016.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleil KE, Rinker JA, Lowery-Gionta EG, Mazzone CM, McCall NM, Kendra AM, Olson DP, Lowell BB, Grant KA, Thiele TE, Kash TL. NPY signaling inhibits extended amygdala CRF neurons to suppress binge alcohol drinking. Nat Neurosci. 2015;18:545–52. doi: 10.1038/nn.3972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racz I, Schürmann B, Karpushova A, Reuter M, Cichon S, Montag C, Fürst R, Schütz C, Franke PE, Strohmaier J, Wienker TF, Terenius L, Osby U, Gunnar A, Maier W, Bilkei-Gorzó A, Nöthen M, Zimmer A. The opioid peptides enkephalin and beta-endorphin in alcohol dependence. Biological psychiatry. 2008;64:989–97. doi: 10.1016/j.biopsych.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raffin-Sanson ML, de Keyzer Y, Bertagna X. Proopiomelanocortin, a polypeptide precursor with multiple functions: from physiology to pathological conditions. Eur J Endocrinol. 2003;149:79–90. doi: 10.1530/eje.0.1490079. [DOI] [PubMed] [Google Scholar]
- Rasmussen DD, Boldt BM, Bryant CA, Mitton DR, Larsen SA, Wilkinson CW. Chronic daily ethanol and withdrawal: 1. Long-term changes in the hypothalamo-pituitary-adrenal axis. Alcohol Clin Exp Res. 2000;24:1836–49. [PubMed] [Google Scholar]
- Reyes BA, Glaser JD, Magtoto R, Van Bockstaele EJ. Pro-opiomelanocortin colocalizes with corticotropin-releasing factor in axon terminals of the noradrenergic nucleus locus coeruleus. Eur J Neurosci. 2006;23:2067–77. doi: 10.1111/j.1460-9568.2006.04744.x. [DOI] [PubMed] [Google Scholar]
- Rinker JA, Marshall SA, Mazzone CM, Lowery-Gionta EG, Gulati V, Pleil KE, Kash TL, Navarro M, Thiele TE. Extended Amygdala to Ventral Tegmental Area Corticotropin-Releasing Factor Circuit Controls Binge Ethanol Intake. Biol Psychiatry. 2017;81:930–940. doi: 10.1016/j.biopsych.2016.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivier C, Vale W. Effect of the long-term administration of corticotropin-releasing factor on the pituitary-adrenal and pituitary-gonadal axis in the male rat. J Clin Invest. 1985;75:689–694. doi: 10.1172/JCI111748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth-Deri I, Green-Sadan T, Yadid G. β-Endorphin and drug-induced reward and reinforcement. Prog Neurobiol. 2008;86:1–21. doi: 10.1016/j.pneurobio.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Rubinstein M, Mogil JS, Japón M, Chan EC, Allen RG, Low MJ. Absence of opioid stress-induced analgesia in mice lacking beta-endorphin by site-directed mutagenesis. Proc Natl Acad Sci USA. 1996;93:3995–4000. doi: 10.1073/pnas.93.9.3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative CT method. Nature Protocols. 2008;3:1101–1108. doi: 10.1038/nprot.2008.73. [DOI] [PubMed] [Google Scholar]
- Sinha R, Robinson J, O’Malley S. Stress response dampening: effects of gender and family history of alcoholism and anxiety disorders. Psychopharmacology (Berl) 1998;137:311–20. doi: 10.1007/s002130050624. [DOI] [PubMed] [Google Scholar]
- Spanagel R, Montkowski A, Allingham K, Stohr T, Shoabib M, Holsboer F, Landgraf R. Anxiety: a potential predictor of vulnerability to the initiation of ethanol self-administration in rats. Psychopharmacology (Berl) 1995;122:369–373. doi: 10.1007/BF02246268. [DOI] [PubMed] [Google Scholar]
- Spanagel R, Noori HR, Heilig M. Stress and alcohol interactions: animal studies and clinical significance. Trends Neurosci. 2014;37:219–27. doi: 10.1016/j.tins.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Stewart RB, Gatto GJ, Lumeng L, Li TK, Murphy JM. Comparison of alcohol-preferring (P) and nonpreferring (NP) rats on tests of anxiety and for the anxiolytic effects of ethanol. Alcohol. 1993 doi: 10.1016/0741-8329(93)90046-q. [DOI] [PubMed] [Google Scholar]
- Vranjkovic O, Pina M, Kash TL, Winder DG. The bed nucleus of the stria terminalis in drug-associated behavior and affect: A circuit-based perspective. Neuropharmacology. 2017;122:100–106. doi: 10.1016/j.neuropharm.2017.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams SB, Holloway A, Karwan K, Allen S, Grisel JE. Oral Self-Adminstration of Ethanol in Transgenic Mice lacking B-endorphin. Impulse Online Journal 2007 [Google Scholar]
- Wynne O, Sarkar DK. Stress and neuroendocrine-immune interaction: a therapeutic role for β-endorphin. In: Kuscnecov A, Anisman H, editors. Handbook of Psychoneuroimmunology. 2013. pp. 198–211. [Google Scholar]
- Zhou Y, Rubinstein M, Low M, Kreek M. Hypothalamic-specific proopiomelanocortin deficiency reduces alcohol drinking in male and female mice. Genes, Brain and Behavior. 2017;16:499–461. doi: 10.1111/gbb.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.