Abstract
Antibodies have been used for more than 100 years in the therapy of infectious diseases but a new generation of highly potent and/or broadly cross-reactive human monoclonal antibodies (sometimes referred to as ‘super-antibodies’) offers new opportunities for intervention. The isolation of these antibodies, which are often rarely induced in human infections, has primarily been achieved by large-scale screening for suitable donors and new single B cell approaches to human monoclonal antibody generation. Engineering the antibodies to improve half-life and effector functions has further augmented their in vivo activity in some cases. Super-antibodies offer promise for the prophylaxis and therapy of infections with a range of viruses, including those that are highly antigenically variable and those that are newly emerging or have pandemic potential. The next few years will be decisive in the realization of the promise of super-antibodies.
TOC blurb
So-called ‘super-antibodies’ are highly potent, broadly reactive antiviral antibodies that offer promise for the treatment of various chronic and emerging viruses. This Review describes how recent technological advances led to their isolation from rare infected individuals and their development for the prevention and treatment of various viral infections.
The use of antibodies to ameliorate the adverse clinical effects of microbial infection can be traced back to the late nineteenth century and the work of von Behring and Kitasato on serum therapy of diphtheria and tetanus (reviewed in REFS 1,2). In these settings, the antibodies act to neutralize bacterial toxins. Therapies followed in which serum antibodies were targeted directly against bacterial and then viral pathogens. For viral pathogens, enriched polyclonal IgG molecules from immunized animals were shown to be effective in prophylaxis, and even post-exposure prophylaxis, for a number of viruses including hepatitis A virus, hepatitis B virus, hepatitis C virus, herpes simplex virus, measles virus, rabies virus, respiratory syncytial virus (RSV), smallpox virus and varicella zoster virus. Generally, the efficacy of antibody preparations declined with the duration of infection such that they were often regarded as poor therapeutic options. Of course, the major antiviral strategy of the twentieth century was vaccination.
Over the latter part of the twentieth and early part of the twenty-first century, there have been major developments in our understanding of and ability to manipulate antibodies. The advent of hybridoma technology in 1976 provided a reliable source of mouse monoclonal antibodies (mAbs), the first impact of which was not on antibody therapy but on the characterization of cells through the definition of cell surface markers. Broad implementation of mAbs in therapy had to wait until the development of humanized mouse antibodies and then the generation of fully human antibodies by various techniques described below. Such antibodies have been largely applied in the fields of oncology and autoimmunity. Only a single antiviral mAbs, the RSV-specific antibody palivizumab, is in widespread clinical use. The reasons for this have been discussed elsewhere1,3–6, although perhaps the most significant reasons are the relatively high cost of production of mAbs, the difficulties of administration and a belief that antibodies are largely only effective in a prophylactic setting, which can be achieved for many viruses by vaccination.
However, as we discuss here, an increasing number of antiviral antibodies with quite remarkable properties in terms of potency and/or cross-reactivity with other viruses or strains of the same virus are being isolated. These so-called ‘super-antibodies’ are changing our understanding of what we can hope to achieve with antibodies against microbial infection in the clinic. Increased potency can greatly reduce the unit costs of treatment, make feasible alternative routes of administration and extend the effective half-life of the antibody. Increased cross-reactivity can allow us to consider targeting multiple viruses with single antibodies. Antibody engineering can impact both potency and cross-reactivity and can greatly extend half-life of super-antibodies.
In this Review, we discuss how new approaches have fueled the identification of super-antibodies, where and how such antibodies may be best applied and future directions for the field.
Super-antibody discovery
Many acute viral infections induce robust neutralizing antibody responses in the large majority of individuals. In general, these viruses show little evidence for evasion of antibody responses and we have referred to them as ‘evasion lite’ 7. Typically, they either display limited antigenic variability in their surface protein (or proteins) or they show considerable variability but nevertheless express immunodominant conserved epitopes. Examples of viruses in this category include measles virus, poliovirus, chikungunya virus and RSV8–11. Presumably the life cycle of these viruses does not dictate immune evasion. For these types of viruses, the isolation of super-antibodies from immune donors has been achieved in a relatively straightforward manner8,9,12–14. However, some viruses have evolved mechanisms to evade effective neutralizing antibody responses (termed ‘evasion strong’) and induce such responses at much lower levels. Effective responses in the context of infection with highly antigenically variable viruses refers not only to their neutralization potency but also to their effectiveness against diverse circulating global isolates, often referred to as breadth. For these viruses —including HIV, influenza virus, Ebola virus and Lassa virus — only a proportion of infected individuals, sometimes quite small, will generate broad and potent neutralizing antibody responses15–21. Furthermore, within these individuals, potent broadly neutralizing antibody (bnAb) specificities generally only constitute a small fraction of the antigen-specific memory B cell pool.
For example, only a few percent of HIV-1-infected individuals develop broad and potent serum responses over time, and B cell cloning efforts have demonstrated that bnAbs generally comprise <1% of the HIV envelope (Env)-specific memory B cell repertoire22. Although there are probably multiple factors that contribute to the low abundance of bnAbs within these individuals, the intrinsic nature of the viral Env protein likely has a key role. The HIV Env protein has evolved a multitude of mechanisms to evade bnAb responses, including decoy forms of Env, enormous antigenic variability, an evolving glycan shield, immunodominant variable epitopes, and poorly accessible conserved epitopes23. Furthermore, most HIV-specific bnAbs incorporate unusual features for epitope recognition, such as uncommonly long (or short) complementarity determining region 3 (CDR3) loops, insertions and deletions, tyrosine sulfation and extensive somatic hypermutation, which likely also contribute to the rarity and delayed development of bnAbs during natural infection24–26.
In the case of influenza virus infection, the vast majority of neutralizing antibodies elicited by infection or vaccination bind to variable epitopes within the haemagglutinin (HA) globular head of the viral particles and display strain-specific neutralizing activity27. Influenza virus-specific bnAbs typically target the conserved HA stem, but this region has variable immunogenicity28–31. The relatively low frequency of bnAbs against the HA stem is perhaps due to the typically tight packing of HA trimers on the virus surface, which may limit antibody accessibility to this region. For Ebola and Lassa viruses, extensive glycosylation on the surface envelope proteins results in masking of conserved neutralizing epitopes15,32. In cases where super-antibodies are present at low frequency within immune repertoires, large-scale donor screening and high-throughput B cell isolation platforms have proven to be critical for the discovery of super-antibodies. Over the past several years, technological advances in these two areas have led to the identification large numbers of super-antibodies, mostly from infected individuals, against a plethora of viral pathogens.
Large-scale donor screening
In the case of HIV, which has served as a prototype virus for many studies in this field 33, systematic selection of donors with broadly neutralizing serum responses has proven to be critical for the identification of super-antibodies. Prior to 2009, the HIV field had been operating with a handful of bnAbs, all of which were limited either in breadth or in potency 34. A number of factors complicated the identification of bnAbs, including the inefficiency of traditional approaches to mAb discovery, the small fraction of B cells that secrete bnAbs, and the limited availability of samples from donors who had developed broad and potent neutralizing serum responses. Beginning in 2005, the problem of limited samples was addressed by establishing donor screening programmes to identify HIV-infected individuals with broadly neutralizing serum responses to serve as source material for the generation of bnAbs18,19,35,36. In one of the largest studies, ~1,800 HIV-1-infected individuals from Australia, Rwanda, Uganda, the United Kingdom and Zambia were screened for broadly neutralizing sera using a reduced pseudovirus panel representative of global circulating HIV-1 isolates19. A subset of individuals, termed “elite neutralizers”, were identified that exhibited exceptionally broad and potent neutralizing serum responses and were therefore prioritized for bnAb isolation.
Over the past eight years, mining of these and similar samples has led to the identification of dozens of remarkably broad and potent HIV super-antibodies37–41. Careful selection of donors with desirable serum profiles has also enabled the isolation of rare super-antibodies to influenza virus, RSV, human metapneumovirus (HMPV), rabies virus and Zika virus12,42–44. For example, the pan-influenza A virus-neutralizing mAb FI6 and the RSV and HMPV cross-neutralizing mAb MPE8 were isolated from donors who were selected on the basis of their strong heterotypic serum responses12,42. Similarly, two pan-lyssavirus neutralizing mAbs, called RVC20 and RVC58, were isolated from the memory B cells of four donors who exhibited potent serum neutralizing activity against multiple lyssavirus species43.
High-throughput human B cell isolation technologies
Human antiviral neutralizing mAbs have been isolated using various different technologies, including combinatorial display libraries, human immunoglobulin transgenic mice and single B cell isolation methods (Fig. 1). Although all of these technologies have proven valuable for mAb generation, the recent burst in super-antibody discovery has primarily been driven by advances in single B cell-based methods. There are several possible reasons for this, including inefficiencies in combinatorial library generation and interrogation (leading to the loss of rare clones), altered binding characteristics of antibody fragments produced in heterologous expression systems (for example, Escherichia coli or yeast), constraints on the generation of suitable recombinant antigens for immunization or library selections, the loss of native heavy and light chain pairing during immune library generation, and inherent differences between the adaptive immune systems of humanized mice and humans45.
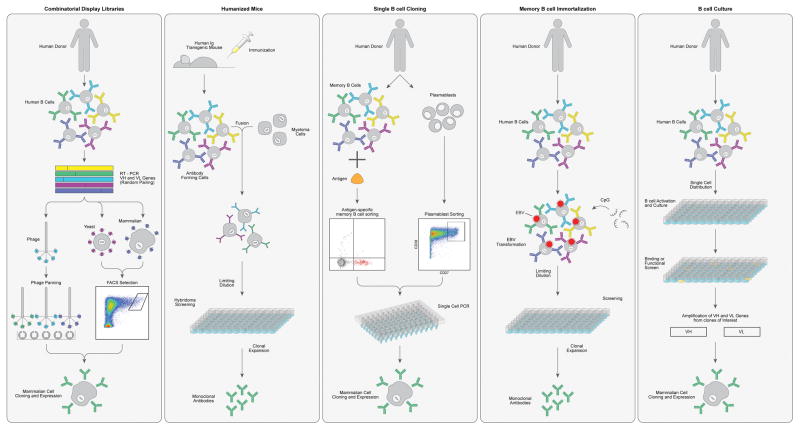
Figure 1. Technologies for monoclonal antibody generation.
a) Combinatorial display libraries. Human antibody heavy and light chain genes are amplified by PCR, and antibody fragments are displayed on the surface of a particle or cell in which the antibody genes are found (such as phage, yeast or mammalian cells142–145). Successive rounds of enrichment are performed to select for clones that bind to the target antigen. Genes encoding antibodies of interest are cloned into human IgG expression vectors to produce monoclonal antibodies (mAbs). b) Human immunoglobulin transgenic mice are generated by introducing human immuoglobulin loci into the mouse genome146,147. Upon immunization, the transgenic mice produce fully human antigen-specific antibodies. The B cells harvested from the immunized mice are fused with myeloma cells to generate antibody-secreting hybridomas, which are then screened for binding or functional activity. c) Single B cell cloning. Antigen-specific memory B cells or plasmablasts are single-cell sorted by flow cytometry and cognate heavy and light chain variable genes are amplified by RT-PCR57,58,148. The antibody variable genes are cloned into human IgG expression vectors to produce mAbs. d) Memory B cell immortalization. Memory B cells are immortalized by Epstein–Barr virus and B cell culture supernatants are screened for binding or functional activity149. Positive cultures are sub-cloned by limiting dilution. e) Memory B cell culture. Single B cells are activated and cultured, and B cell supernatants are screened for binding or functional activity37,150. Antibody variable genes are amplified from clones of interest by PCR and cloned into human IgG expression vectors to produce mAbs.
Over the past decade, several technological breakthroughs in the B cell cloning arena have fueled super-antibody identification. One of these advances came in 2009, when direct functional screening of thousands of B cell clones from an HIV elite neutralizer led to the isolation of two super-antibodies, PG9 and PG16, which were about an order of magnitude more potent than first-generation bnAbs37. Notably, PG9 and PG16 bind poorly to recombinant Env proteins and thus would not have been identified without direct functional screening of B cell supernatants. To date, many dozens of HIV-specific bnAbs targeting a diverse range of epitopes have been identified using functional screening approaches39,46–48. Highly potent super-antibodies to RSV, HMPV, Lassa virus and human cytomegalovirus (HCMV) have also been discovered using high-throughput functional screening technologies12,13,49,50 (Table 1).
Table 1.
Anti-viral SuperAbs
| Virus | Prototypic SuperAb | Similar antibodies* | Antigenic region | Antibody isolation technology |
|---|---|---|---|---|
| HIV | PG9, PGT145 | PG16, PGT141-144, CH01-04, PGDM1400–1412, CAP256- VRC26.01-12 | V2 apex | Human B cell isolation |
| VRC01 | VRC02, VRC03, 8ANC131, 8ANC37, 8ANC134, NIH45-46, 3BNC60, BNC62, 3BNC117, 12A12, 12A21,12A30, VRC-PG04, VRC-CH31, VRC27, VRC07-523, N6 | CD4 binding site | Human B cell isolation | |
| PGT121, PGT128, PGT135 | PGT122, PGT123, PGT125-PGT127, PGT130, PGT131, PGT136, PGT137, 10-1074 | V3 glycan | Human B cell isolation | |
| PGT151, 35O22, 8ANC195 | PGT152-158, ACS202, N123-VRC34.01 | gp120/gp41 interface | Human B cell isolation | |
| 10E8 | MPER | Human B cell isolation | ||
| Influenza | C05 | F045-092, 641 I-9 | HA head | Human B cell isolation, phage display |
| FI6 | MEDI8852, CR9114, 39.29, 81.39, CT149, 56.a.09, 31.b.09, 16.a.26, 31.a.83 | HA stem | Human B cell isolation | |
| RSV/HMPV | MPE8 | ADI-14448, 25P13 | Site III | Human B cell isolation |
| RSV | D25 | D25, AM22, 5C4, ADI-15618 | Site ø | Human B cell isolation |
| HCMV | 9I6, 8I21 | 1F11, 2F4, 6G4 | Pentameric complex | Human B cell isolation |
| Rabies | RVC58 | Site III | Human B cell isolation | |
| RVC20 | Site I | Human B cell isolation | ||
| Dengue/Zika | A11, C8 | A11, C8, C10, B2, B7, C4 | E-dimer interface | Human B cell isolation |
| Z004 | Z028, Z001, Z006, Z010, Z031, Z035, Z038, Z014, ZKA-190, ADI- 24192, ADI-24232, ADI-24227, ADI-24238 | DIII lateral ridge | Human B cell isolation | |
| Ebola | ADI-15878 | 6D6, ADI-15742, CA45, FVM09 | Fusion loop | Human or macaque B cell isolation |
| MERS | LCA60, REGN3051, REGN3048 | Receptor-binding domain | Human B cell isolation, humanized mice | |
| Lassa virus | 8.9F | Quaternary GPC-C epitope | Human B cell isolation | |
| 37.2D | 25.6A | Quaternary GPC-B epitope | Human B cell isolation | |
| 25.10C, 12.1F | Quaternary GPC-A epitope | Human B cell isolation |
This list of antbodies is not exhaustive and is caveated by the fact that different neutralization assays can give different results.
Similar to PG9 and PG16, these super-antibodies were isolated by screening B cell supernatants based on their capacity to neutralize infection in vitro and were subsequently found to react poorly with currently available recombinant envelope proteins. In the case of RSV, this approach led to the isolation of the highly potent mAb D25, which binds to an epitope that is exclusively expressed on the prefusion conformation of RSV fusion (F) glycoprotein49,51. An engineered variant of mAb D25 (MEDI8897), which exhibits 50–100 times greater neutralization potency than palivizumab, is now being tested in clinical trials for the prevention of RSV-associated disease in high-risk infants. A second RSV prefusion F-specific super-antibody, which cross-neutralizes several different paramyxoviruses including HMPV, was also isolated by screening B cell supernatants for neutralizing activity12 (Table 1).
In the case of HCMV, direct functional screening enabled the isolation of highly potent super-antibodies specific for conformational epitopes within the gH–gL–UL128–UL130–UL131A pentamer complex, which was not previously known to be a target for neutralizing antibodies13. Direct functional screening approaches have also led to the discovery of potent super-antibodies to Middle East respiratory syndrome coronavirus (MERS-CoV), Ebola virus, influenza virus, chikungunya virus, rabies virus and the poxvirus family9,42,43,52–56. Notably, in the case of MERS-CoV, only a single B cell culture out of 4,600 screened showed neutralizing activity53. Similarly, the pan-influenza A virus neutralizing mAb FI6 was isolated by testing 104,000 plasma cells from eight immune donors42. Finally, only two out of 500 mAbs that were selected based on their ability to neutralize rabies virus showed cross-neutralizing activity against multiple lyssavirus species43. These examples clearly illustrate that exhaustive interrogation of immune repertoires is often required for the identification of rare cross-neutralizing super-antibodies.
A second breakthrough in the HIV antibody field followed the development of technology for antigen-specific single B cell sorting57–59. This approach, coupled with the use of rationally designed Env probes, allowed for the discovery of two new potent HIV bnAbs that target the conserved CD4 binding site60,61 (Table 1). Following this discovery, several other potent bnAbs against the CD4 binding site were isolated using similar approaches38,62,63. Recently, advances in the generation of recombinant native-like HIV Env trimers have enabled the identification of exceptionally potent “PG9-class” bnAbs40.
Many HIV super-antibodies have now been generated using single B cell sorting technology38,40,60,62,63. The use of fluorescently labeled probes to sort antigen-specific memory B cells has also allowed for the discovery of highly potent super-antibodies to Ebola virus, RSV, human papilloma virus (HPV), Zika virus and influenza virus11,30,31,44,64,65. In the case of Ebola virus, a large-scale single B cell cloning effort led to the isolation of several hundred mAbs specific for Ebola virus surface glycoprotein (GP), two of which showed potent pan-Ebola virus neutralizing activity and protective efficacy64,66. A similar effort in the RSV field allowed for the isolation of several prefusion F protein-specific mAbs that show over 100 times more potent neutralizing activity than palivizumab11. In addition, multiple groups have used clever dual antigen labeling strategies to identify potent bnAbs to HIV, influenza virus, Ebola virus and HPV30,31,40,65,67,68. The structures of several super-antibodies bound to their viral targets are shown in Fig 2. Finally, a recent report showed that bnAbs to HIV can be readily elicited in cows using a single Env trimer immunogen and that this induction depends on the long heavy chain CDR3 loops of the bovine immunoglobulin repertoire 67. It is possible that this repertoire may provide advantages in generating super-antibodies against other pathogens.
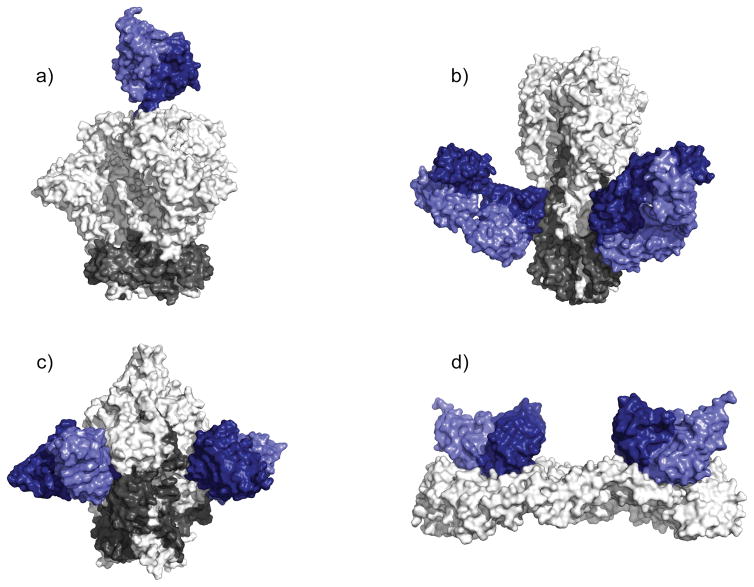
Figure 2. Structures of super-antibodies bound to their target antigens.
a) Cryoelectron microscopy structure of the broadly neutralizing anti-HIV-1 antibody PGT145 in complex with a recombinant HIV envelope trimer151. PGT145 binds to a glycan-dependent quaternary epitope at the trimer apex152. b) Crystal structure of the influenza virus group 1/group 2 neutralizing antibody CR9114 in complex with influenza virus haemagglutinin (HA)153. CR9114 recognizes a highly conserved epitope in the HA stem154,155. c) Crystal structure of the respiratory syncytial virus (RSV) and human metapneumovirus (HMPV) cross-neutralizing antibody MPE8 in complex with a stabilized RSV prefusion fusion glycoprotein trimer156. d) Crystal structure of the Zika virus and dengue virus cross-neutralizing antibody C8 in complex with a soluble Zika virus envelope ectodomain85. C8 targets a quaternary epitope that bridges two envelope protein subunits.
Vaccination or infection-induced antibody-secreting cell (ASC) responses have also proven to be a rich source of antigen-specific antibodies. Following early studies that showed a transient but large population of ASCs appears in peripheral blood 5–7 days after tetanus toxoid booster vaccination 69, it was shown that influenza virus vaccination produced a similar ASC response and that the large majority of mAbs cloned from these cells bound with high affinity to influenza virus, providing a proof-of-concept that the ASC response could be exploited to rapidly generate antigen-specific antibodies against any immunizing antigen 70. To date, plasmablast cloning has led to the isolation of mAbs against many different viruses, including dengue virus, Zika virus, HIV, influenza virus, vaccinia virus and rotavirus29,71–76.
One of the advantages of the plasmablast approach is that antigen baiting is not required for B cell sorting, thereby allowing for the isolation of antibodies that target epitopes that are poorly expressed on recombinant antigens. For example, in the case of dengue virus, potent bnAbs targeting E-dimer dependent epitopes were isolated using this approach72. However, it is important to emphasize that the ability to isolate super-antibodies using this method will depend on several factors. First, during a primary infection, the ASC population will be mainly composed of activated, low-affinity naive B cells (rather than affinity-matured memory B cells), making the possibility of identifying super-antibodies extremely unlikely. Second, in the context of a booster vaccination or secondary infection with an antigenically similar virus, most of the plasmablast response will be directed against immunodominant epitopes, which in many cases are not targeted by effective neutralizing antibodies. In such cases, exhaustive cloning, production and characterization of the plasmablast-derived mAbs would likely be required to identify rare super-antibodies. In contrast, secondary infection with an antigenically related but sufficiently divergent virus can drive the preferential expansion of B cells that target highly conserved epitopes, as exemplified by the unusually high frequency of bnAbs induced in donors who were infected with the novel H1N1 influenza virus in 200929,75. In principle, one could use this type of approach for the generation of super-antibodies in humanized mice or other animal models using suitably designed immunogens and immunization regimens.
Rapid response platforms for emerging viruses
Over the past two decades, humanity has faced a new emerging, or re-emerging, viral threat almost every year, including severe acute respiratory syndrome coronavirus (SARS), West Nile virus, pandemic influenza virus, Ebola virus, MERS-CoV and Zika virus. Due to their comparatively fast path to approval and generally favourable safety profiles, mAb therapies represent a promising alternative to vaccines and small molecule drugs for the treatment and prevention of emerging viral threats. Recently, several laboratories have demonstrated the feasibility of identifying, characterizing and scaling-up production of highly potent mAbs in remarkably short timeframes.
In response to the 2014–2015 MERS-CoV outbreak, two different groups illustrated the power of their mAb discovery platforms by isolating highly potent MERS-specific mAbs, producing the mAbs in gram quantities, and testing the lead mAbs in animal models at an unprecedented speed53,77. In one of these studies, a single highly potent MERS-CoV neutralizing mAb was identified from the memory B cells of a convalescent donor using a high-throughput functional screening approach53. This mAb, called LCA60, showed both pre- and post-exposure protection in a mouse model of MERS-CoV infection. Importantly, it only took the authors four months from the initial B cell screening to the development of a stable cell line that produces the neutralizing mAb at 5 g/L. In the second study, human immunoglobulin transgenic mice were immunized with the MERS-CoV Spike protein and then used to generate a panel of potent MER-CoV-specific neutralizing mAbs within several weeks77. The authors also quickly generated a humanized mouse model of MERS-CoV infection, which was used to demonstrate the therapeutic efficacy of their mAbs.
In a third study, vaccination of transchromosomal cows engineered to produce fully human IgG molecules with MERS-CoV was shown to yield high serum titres of MERS-CoV-specific neutralizing antibodies78. Importantly, administration of the purified polyclonal transchromosomal bovine human IgG to mice either 12 hours before or 24 and 48 hours after MERS-CoV infection resulted in a significant reduction in viral lung titres. Transchromosomal bovines have also been used to rapidly generate polyclonal neutralizing antibodies to Hanta virus, Venezuelan equine encephalitis virus and Ebola virus79–81, demonstrating the feasibility of using this platform to rapidly generate therapeutics to combat emerging viral threats. The antibodies arising from transchromosomal cows are polyclonal to date but there is potential for mAb isolation.
Between 2015 and 2016, several groups responded to the 2014–2015 Ebola virus outbreak by swiftly generating highly potent Ebola virus GP-specific neutralizing mAbs from the memory B cells of convalescent donors54–56,64,66. Many of these mAbs showed potent post-exposure therapeutic efficacy against either Ebola or Bundibugyo virus in animal models and a subset showed protective efficacy against multiple Ebola virus strains54,55,64,66. Similarly, several groups have recently reported on the isolation of potent Zika virus-specific neutralizing mAbs from human donors14,44,82,83. Notably, one of these neutralizing mAbs, called ZIKV-117, showed post-exposure protection against Zika virus in both pregnant and non-pregnant mice82.
In certain cases, the availability of super-antibodies that target highly conserved epitopes may shorten timelines further by bypassing the need for mAb discovery. For example, it was recently shown that a subset of dengue virus-specific mAbs potently cross-neutralize Zika virus84–86. These bnAbs — perhaps carrying Fc mutations that ablate Fc receptor binding to avoid potential for antibody-dependent enhancement14 — could immediately be used for prophylaxis for pregnant women living in Zika virus endemic regions. Notably, cocktails of super-antibodies targeting different epitopes, or bispecific or trispecific super-antibody constructs, will likely be required to prevent neutralization escape87–93.
Antibodies in prophylaxis and therapy
Antibodies can function against viruses by several mechanisms, primarily divided into activities against free virus particles and activities against infected cells. Neutralization, measured in vitro as the ability of antibody to prevent viral entry into target cells without a requirement for involvement of any other agents, is an activity against free virions that has been most correlated with protection in vivo. Activities against infected cells generally depend on Fc effector functions and involve host effector cells. They include antibody-dependent cellular cytotoxicity (ADCC), complement-dependent cytotoxicity (CDC) and antibody-dependent cellular phagocytosis (ADCP). It is presumed that these latter activities are likely to be important in therapy using antibodies. Since neutralization frequently correlates with the ability to bind to native structures on the virion surface, it can give some indication of the ability of antibodies to mediate effector activities such as ADCC and ADCP. The potency of super-antibodies is then often estimated from neutralization measurements, although ultimately it is of course in vivo activity that is crucial.
Prophylaxis
Vaccination is the most effective and low-cost method of preventing viral disease. However, the development of effective vaccines against many important viral pathogens — including HIV, RSV, hepatitis C virus, dengue virus and HCMV — has been met with limited success. Furthermore, vaccine development is a long complex process, often lasting 10–15 years, making immunization an impractical means of protecting individuals from new emerging viral threats, unless pan-virus family vaccines can be developed. For example, if antibodies can be identified that potently neutralize existing strains of Ebola virus, or even Ebola and Marburg filoviruses, then one could anticipate that a vaccine templated from the antibodies would be effective even against emerging strains of Ebola virus. However, at the current time, passive antibody prophylaxis represents a promising alternative to vaccination for a number of viral infections.
Currently, three purified polyclonal hyperimmune globulins derived from human donors immune to hepatitis B virus, HCMV or varicella zoster virus are on the market for the prevention of serious diseases associated with these viruses. A rabies virus-specific immune globulin, combined with vaccination, is also available for post-exposure prophylaxis. In 1998, palivizumab — a humanized mAb that targets the RSV F protein — became the first US Food and Drug Administration approved antiviral mAb. Palivizumab soon replaced RSV hyperimmune globulin (RespiGam) for the prevention of severe RSV-associated disease in high-risk infants. However, although palivizumab is more specific and 50–100 times more potent than RespiGam, the cost associated with the required dosing makes its use impractical for all infants94. A second-generation RSV-specific mAb, which shows up to 50 times greater neutralization potency than palivizumab and contains substitutions in the Fc domain that extend its serum half-life, is currently in phase 2 clinical trials for the prevention of severe RSV-associated disease in all infants95 (Table 2).
Table 2.
Anti-viral mAbs in clinical development
| Antibody | Virus | Antibody isolation technology | Target | Stage of development | Manufacturer | Indication |
|---|---|---|---|---|---|---|
| Porgaviximab | Ebola | Immunization/Chimerization | Viral envelope glycoprotein | Phase I/II | Mapp Biopharmaceutical; LeafBio | Post-exposure treatment of Ebola virus infection |
| MBL HCV1 | HCV | Humanized mice | HCV E2 glycoprotein | Phase II | MassBiologics | Prevention of HCV recurrence in patients receiving a liver transplant |
| PRO 140 | HIV | Immunization/Humanization | CCR5 | Phase III | Progenics Pharmaceuticals | Treatment of HIV-1 infection |
| Ibalizumab | HIV | Immunization/Humanization | CD4 | Phase III | TaiMed Biologics | Treatment of HIV-1 infection |
| UB 421 | HIV | Immunization/Humanization | CD4 | Phase II | United Biomedical | Treatment of HIV-1 infection |
| VRC01-LS | HIV | Human B cell isolation | HIV gp120 | Phase I | National Institute of Allergy and Infectious Diseases | Prevention of HIV-1 infection |
| VRC01 | HIV | Human B cell isolation | HIV gp120 | Phase I | National Institute of Allergy and Infectious Diseases | Treatment of HIV-1 infection |
| 3BNC117-LS | HIV | Human B cell isolation | HIV gp120 | Phase I | Rockefeller University | Treatment of HIV-1 infection |
| 10-1074 and 3BNC117 | HIV | Human B cell isolation | HIV gp120 | Phase I | Rockefeller University | Treatment of HIV-1 infection |
| PGT121 | HIV | Human B cell isolation | HIV gp120 | Phase I | International AIDS Vaccine Initiative | Treatment and prevention of HIV-1 infection |
| PGDM1400 and PGT121 | HIV | Human B cell isolation | HIV gp120 | Phase I | International AIDS Vaccine Initiative | Treatment and prevention of HIV-1 infection |
| MB 66 | HIV/HSV | Human B cell isolation | HIV gp120, HSV glycoprotein D | Phase I | Mapp Biopharmaceutical | Prevention of HIV-1 and HSV sexual transmission |
| VIS 410 | Influenza | Unknown | Influenza hemagglutinin | Phase II | Visterra | Treatment and prevention of influenza A virus infection |
| MHAA 4549A | Influenza | Human B cell isolation | Influenza virus haemagglutinin | Phase II | Genentech | Treatment of influenza A virus infection |
| CT P27 | Influenza | Human B cell isolation | Influenza virus haemagglutinin | Phase II | Celltrion | Treatment and prevention of influenza A virus infection |
| Diridavumab | Influenza | Phage display | Influenza virus haemagglutinin | Phase II | National Institute of Allergy and Infectious Diseases | Treatment and prevention of influenza A virus infection |
| CR8020 | Influenza | Human B cell isolation | Influenza virus haemagglutinin | Phase II | Crucell | Treatment and prevention of influenza A virus infection |
| RG 6024 | Influenza | Human B cell isolation | Influenza virus haemagglutinin | Phase I | Genentech | Treatment of influenza B virus infection |
| MEDI 8852 | Influenza | Human B cell isolation | Influenza virus haemagglutinin | Phase II | MedImmune | Treatment of influenza A virus infection |
| TCN 032 | Influenza | Human B cell isolation | Influenza M2e protein | Phase II | Theraclone Sciences; Zenyaku Kogyo | Treatment of influenza A virus infection |
| m 102.4 | Nipah and Hendra virus | Phage display | Viral envelope glycoprotein G | Phase I | Profectus Biosciences, Inc. | Prevention and treatment of Nipah and Hendra virus infections |
| Rabimabs | Rabies | Immunization | Viral envelope G protein | Phase I/II | World Health Organization; Zydus Cadila | Treatment and prevention of rabies |
| RAB-1 | Rabies | Humanized mice | Viral envelope G protein | Approved | Serum Institute of India; MassBiologics | Post-exposure prophylaxis of rabies |
| Foravirumab | Rabies | Phage display, Human B cell isolation | Viral envelope G protein | PhaseII/III | Crucell; Sanofi Pasteur | Post-exposure prophylaxis of rabies |
| Palivizumab | RSV | Immunization/Humanization | Viral fusion protein | Approved | MedImmune | Prophylaxsis in high-risk infants |
| MEDI 8897 | RSV | Human B cell isolation | Viral fusion protein | Phase II | MedImmune | Prophylaxsis in high-risk infants |
Although palivizumab is the only commercially available mAb for the prevention of a viral disease, there are multiple antiviral mAbs in preclinical and clinical development that have shown pre-exposure efficacy in animal models. For example, the potent MERS-CoV-specific mAbs described above were shown to prophylactically protect humanized mice against MERS-associated disease. Similarly, mAbs to chikungunya virus, influenza virus, HIV and Ebola virus have shown potent prophylactic efficacy in animal models9,85,96–102. Recently, a broadly neutralizing anti-Zika virus mAb (ZIKV-117) was shown to protect against maternal-fetal transmission in a mouse model of Zika virus infection82. If this observation translates to humans, prophylaxis with ZIKV-117 or similar neutralizing mAbs may be a promising means of protecting at-risk pregnant women against Zika virus infection and fetal transmission.
In the case of HIV, multiple studies have shown that passively administered neutralizing mAbs provide protection against intravenous, vaginal, rectal and oral challenge in non-human primate and mouse models99–101,103–106. A large ongoing study (the antibody mediated prevention (AMP) study) will assess the ability of the VRC01 mAb specific for the CD4 binding site to decrease the risk of HIV acquisition in humans (See Further reading). Although animal studies have provided proof-of-principle that a vaccine capable of inducing sufficient titres of bnAbs could prevent the establishment of HIV infection in humans, and the AMP study will investigate this directly, the design of immunogens that efficiently elicit these rare antibodies remains a formidable challenge. To bypass the challenges associated with active vaccination against HIV, a number of groups have proposed alternative strategies based on vector-mediated antibody gene transfer to express bnAbs in vivo107. Unlike traditional passive immunization, which would require long-term repeated treatment with bnAbs, vectored immunoprophylaxis only involves a single injection and enables continuous and sustained delivery of antibodies. In 2009, pioneering work demonstrated that vector-mediated delivery of antibody-like molecules can provide vaccine-like protection against SIV challenge in non-human primate models108.
Subsequent studies have shown that vectored immunoprophylaxis is also compatible with full-length IgG molecules and CD4-like molecules109–111. If the preclinical results in mice and macaques translate to humans, vectored antibody gene delivery strategies could provide an alternative form of prophylaxis against HIV and other challenging vaccine targets such as hepatitis C virus, pandemic influenza virus and malaria. Recently, non-viral vector nucleic acid delivery technologies have also been developed to obviate the potential safety issues associated with viral vector-mediated delivery, such as long-term persistence and potential viral DNA integration into the host genome112–117. In a recent study, it was shown that the administration of lipid encapsulated, nucleoside-modified mRNAs encoding the heavy and light chain genes of the broadly neutralizing HIV-1-specific antibody VRC01 to humanized mice resulted in high serum antibody concentrations and protection against intravenous HIV-1 challenge114.
Similar proof-of-concept studies have also been performed using synthetic DNA plasmid-mediated antibody gene transfer112,113. In one such study, synthetic DNA plasmids encoding cross-neutralizing anti-dengue virus antibodies were delivered to mice by electroporation and resulted in biologically relevant levels of serum antibody112. Importantly, a single intramuscular injection of plasmid DNA conferred protection against severe dengue disease in a mouse model. Although several technical challenges remain to be addressed, such as enhancing in vivo antibody expression levels and reducing the potential for immunogenicity, these studies demonstrate the feasibility of using plasmid DNA and modified mRNA-based antibody delivery technologies for passive immunotherapy.
Therapy
Conventional wisdom says that antibodies are effective if present before or shortly after viral exposure but their efficacy declines markedly once infection is established. For example, the anti-RSV antibody palivizumab is effective in the clinic prophylactically but not therapeutically 118. However, there are indications that the dogma may be challenged by super-antibodies. An example is the ability of a new generation of bnAbs against HIV to strongly impact ongoing infection in animal models 87,119,120, in which an earlier generation of less potent mAbs had very limited effects 121. This likely reflects the increased neutralization potency of the super-antibodies but also the increased breadth of neutralization that may restrict escape pathways 119. A number of super-antibodies are now being evaluated in humans for their activities against established HIV infection122–126 (Table 2). Initial results are interesting, providing for example an indication of enhanced immune responses following bnAb administration 127. The emerging results will be followed closely, including in the context of combining bnAbs with drugs and other antiviral agents to attempt HIV cure.
For other viruses, clear evidence of a strong therapeutic effect for super-antibodies has not been gathered yet. A number of cases such as antibody treatment of rabies virus and Junin virus infections 43,128 are probably better interpreted as post-exposure prophylaxis rather than therapy of established infection. Two promising examples of possible therapy are the successful treatment of Ebola virus- or Lassa virus-infected monkeys with mAbs once symptoms have appeared 89,129. Unfortunately, no definitive evidence of the efficacy of mAbs in Ebola or Lassa-symptomatic humans yet exists.
Camelid-derived single-domain antibodies (sdAbs), which are comprised of a single heavy-chain variable domain, represent a promising new class of antibody-based therapeutics for RSV and other viruses that cause lower respiratory tract infections 130–133. Due to their small size and high solubility and stability, sdAbs can be rapidly delivered to the site of infection via inhalation. Notably, a neutralizing anti-RSV sdAb (ALX-0171) that targets an epitope overlapping that bound by palivizumab recently showed a trend towards a therapeutic effect in a phase I/IIa clinical trial based on reduced viral loads and clinical symptoms in hospitalized RSV-infected infants. Prefusion F protein-specific sdAbs that show up to 180,000 times greater neutralization potency than ALX-0171 have recently been identified and may offer even greater therapeutic benefit 133.
Practical considerations arising with super-antibodies
Intuitively, the enhanced potency of super-antibodies is immediately recognized as beneficial in antibody prophylaxis and therapy. However, there are also a number of additional effects from this enhanced potency that may not be instantly appreciated and that can be further strengthened by antibody engineering. For example, enhanced potency means that less antibody needs to be used and this can allow easier to develop low-concentration subcutaneous administration, rather than more difficult to develop high-concentration subcutaneous formulations or less convenient (low concentration) intravenous administration. Enhanced potency also means that the life-time of effective antibody following administration is extended, thereby requiring fewer administrations to maintain a useful protective or therapeutic effect. Antibody engineering can also extend half-life significantly 95,134–139 so that for the most potent super-antibodies, one could envisage requiring administrations perhaps only every 3–6 months for efficacy. Antibody engineering can also deliver greater efficacy through enhanced Fc effector function 140,141.
Conclusions
The deployment of antibodies as antiviral agents has progressed through a number of stages over the years, corresponding to increasing levels of potency of the reagent administered. It began with immune serum over a century ago, then to polyclonal antibodies, then mAbs and now into highly potent human mAbs dubbed super-antibodies. Thanks to research that has been primarily carried out in the cancer field, technologies have been developed to endow these super-antibodies with enhanced in vivo function.
Will super-antibodies change the landscape of antiviral prophylaxis and therapy? The answer to this question will depend on a number of factors, including, first, the rapidity of development of antiviral vaccines; vaccines will likely remain the cheapest and most effective antiviral measure but some viruses such as HIV present a huge vaccine challenge. Second, the effective cost of antibody treatment, which incorporates not only manufacturing cost but also the durability of administered antibody and the route of administration. Third, the success of antibodies in the treatment of established viral infections. Particularly in the therapeutic setting, the answers can only be obtained with clinical trials using the best super-antibodies available.
Acknowledgments
We thank J. Mascola, D. Sok and M. Vasquez for comments on the manuscript. We also thank L. Hangartner and C. Corbaci for assistance with figure preparation. D.R.B. acknowledges the financial support from the National Institutes of Allergy and Infectious Disease, the International AIDS Vaccine Initiative, the Bill and Melinda Gates Foundation and the Ragon Institute.
GLOSSARY
- Humanized mouse antibody
A genetically engineered mouse antibody in which the protein sequence has been modified to increase its similarity to human antibodies, thereby decreasing its potential immunogenicity.
- Transchromosomal cows
Cows that have been genetically modified to incorporate human chromosomes so that upon immunization they generate human antibodies.
- Antibody-dependent cellular cytotoxicity
A mechanism by which Fc receptor-bearing effector cells such as natural killer (NK) cells recognize and kill antibody-coated target cells, such as virus-infected cells. The Fc portions of the coating antibodies interact with an Fc receptor (e.g. FcγRIII; also known as CD16 that is expressed by NK cells) thereby initiating a signalling cascade that results in the release of 22 cytotoxic granules (containing perforin and granzyme B) from the effector cell, which lead to cell death of the antibody-coated cell.
- Complement-dependent cytotoxicity
A mechanism of antibody-mediated immunity whereby the association of antibody on a target cell surface leads to binding of the complement component C1q and triggering of the classical complement cascade. The cascade leads to elimination of taeget cells by a number of mechanisms including the formation of the membrane attack complex, the cytolytic end product of the complement cascade.
- Hyperimmune globulins
An antibody preparation generated from the plasma of donors with high titers of antibody against a specific pathogen or antigen. Hyperimmune globulins are available against rabies, hepatitis B and varicella-zoster viruses amongst other viruses.
Footnotes
FURTHER READING
The AMP study: https://ampstudy.org/about
Competing interests
The authors have no competing interests.
Author contributions
Both authors contributed to research and discussion of content of the article, and to writing, reviewing and editing of the manuscript before submission.
- Antibodies have been used for over a century prophylactically and, less often, therapeutically against viruses.
- “Super-antibodies” — a new generation of highly potent and/or broadly cross-reactive human monoclonal antibodies — offer new opportunities for prophylaxis and therapy of viral infections.
- Super-antibodies are typically generated in natural infection infrequently and/or in a limited number of individuals.
- Isolation of these antibodies has primarily been achieved by large-scale screening for suitable donors and new single B cell approaches to human monoclonal antibody generation.
- Super-antibodies may offer the possibility of treating multiple viruses of a given family with single reagents. They are also valuable templates for rational vaccine design.
- The great potency of super-antibodies has many advantages for practical development as therapeutic reagents. These advantages can be enhanced by a variety of antibody engineering technologies.
Subject categories
Biological sciences/Immunology/Infectious diseases/Viral infection [URI/631/250/255/2514]
Biological sciences/Biotechnology/Biologics/Antibody therapy [URI/631/61/51/1568]
References
- 1.Hey A. History and Practice: Antibodies in Infectious Diseases. Microbiol Spectr. 2015;3 doi: 10.1128/microbiolspec.AID-0026-2014. AID-0026-2014. [DOI] [PubMed] [Google Scholar]
- 2.Graham BS, Ambrosino DM. History of passive antibody administration for prevention and treatment of infectious diseases. Curr Opin HIV AIDS. 2015;10:129–134. doi: 10.1097/COH.0000000000000154. An excellent account of the history of passive antibody administration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sparrow E, Friede M, Sheikh M, Torvaldsen S. Therapeutic antibodies for infectious diseases. Bull World Health Organ. 2017;95:235–237. doi: 10.2471/BLT.16.178061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berry JD, Gaudet RG. Antibodies in infectious diseases: polyclonals, monoclonals and niche biotechnology. N Biotechnol. 2011;28:489–501. doi: 10.1016/j.nbt.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saylor C, Dadachova E, Casadevall A. Monoclonal antibody-based therapies for microbial diseases. Vaccine. 2009;27(Suppl 6):G38–46. doi: 10.1016/j.vaccine.2009.09.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson PC, Andrews SF. Tools to therapeutically harness the human antibody response. Nat Rev Immunol. 2012;12:709–719. doi: 10.1038/nri3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burton DR. What Are the Most Powerful Immunogen Design Vaccine Strategies? Reverse Vaccinology 2.0 Shows Great Promise. Cold Spring Harb Perspect Biol. 2017 doi: 10.1101/cshperspect.a030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Z, et al. Cross-neutralizing human anti-poliovirus antibodies bind the recognition site for cellular receptor. Proc Natl Acad Sci U S A. 2013;110:20242–20247. doi: 10.1073/pnas.1320041110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith SA, et al. Isolation and Characterization of Broad and Ultrapotent Human Monoclonal Antibodies with Therapeutic Activity against Chikungunya Virus. Cell Host Microbe. 2015;18:86–95. doi: 10.1016/j.chom.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tahara M, et al. Functional and structural characterization of neutralizing epitopes of measles virus hemagglutinin protein. J Virol. 2013;87:666–675. doi: 10.1128/JVI.02033-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gilman MS, et al. Rapid profiling of RSV antibody repertoires from the memory B cells of naturally infected adult donors. Sci Immunol. 2016;1 doi: 10.1126/sciimmunol.aaj1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corti D, et al. Cross-neutralization of four paramyxoviruses by a human monoclonal antibody. Nature. 2013;501:439–443. doi: 10.1038/nature12442. One of the first descriptions of a monoclonal antibody with pan-virus type neutralizing ability. [DOI] [PubMed] [Google Scholar]
- 13.Macagno A, et al. Isolation of human monoclonal antibodies that potently neutralize human cytomegalovirus infection by targeting different epitopes on the gH/gL/UL128-131A complex. J Virol. 2010;84:1005–1013. doi: 10.1128/JVI.01809-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stettler K, et al. Specificity, cross-reactivity, and function of antibodies elicited by Zika virus infection. Science. 2016;353:823–826. doi: 10.1126/science.aaf8505. [DOI] [PubMed] [Google Scholar]
- 15.Sommerstein R, et al. Arenavirus Glycan Shield Promotes Neutralizing Antibody Evasion and Protracted Infection. PLoS Pathog. 2015;11:e1005276. doi: 10.1371/journal.ppat.1005276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sather DN, et al. Factors associated with the development of cross-reactive neutralizing antibodies during human immunodeficiency virus type 1 infection. J Virol. 2009;83:757–769. doi: 10.1128/JVI.02036-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gray ES, et al. The neutralization breadth of HIV-1 develops incrementally over four years and is associated with CD4+ T cell decline and high viral load during acute infection. J Virol. 2011;85:4828–4840. doi: 10.1128/JVI.00198-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doria-Rose NA, et al. Breadth of human immunodeficiency virus-specific neutralizing activity in sera: clustering analysis and association with clinical variables. J Virol. 2010;84:1631–1636. doi: 10.1128/JVI.01482-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simek MD, et al. Human immunodeficiency virus type 1 elite neutralizers: individuals with broad and potent neutralizing activity identified by using a high-throughput neutralization assay together with an analytical selection algorithm. J Virol. 2009;83:7337–7348. doi: 10.1128/JVI.00110-09. Describes the assembly and use of a large cohort of HIV-infected individuals with broad neutralizing sera as the starting point for super-antibody generation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jahrling PB, Frame JD, Rhoderick JB, Monson MH. Endemic Lassa fever in Liberia. IV. Selection of optimally effective plasma for treatment by passive immunization. Trans R Soc Trop Med Hyg. 1985;79:380–384. doi: 10.1016/0035-9203(85)90388-8. [DOI] [PubMed] [Google Scholar]
- 21.Andrews SF, et al. Immune history profoundly affects broadly protective B cell responses to influenza. Sci Transl Med. 2015;7:316ra192. doi: 10.1126/scitranslmed.aad0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kwong PD, Mascola JR. Human antibodies that neutralize HIV-1: identification, structures, and B cell ontogenies. Immunity. 2012;37:412–425. doi: 10.1016/j.immuni.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burton DR, Mascola JR. Antibody responses to envelope glycoproteins in HIV-1 infection. Nat Immunol. 2015;16:571–576. doi: 10.1038/ni.3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwong PD, Mascola JR, Nabel GJ. Broadly neutralizing antibodies and the search for an HIV-1 vaccine: the end of the beginning. Nat Rev Immunol. 2013;13:693–701. doi: 10.1038/nri3516. [DOI] [PubMed] [Google Scholar]
- 25.Burton DR, Hangartner L. Broadly Neutralizing Antibodies to HIV and Their Role in Vaccine Design. Annu Rev Immunol. 2016;34:635–659. doi: 10.1146/annurev-immunol-041015-055515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.West AP, Jr, et al. Structural insights on the role of antibodies in HIV-1 vaccine and therapy. Cell. 2014;156:633–648. doi: 10.1016/j.cell.2014.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corti D, Lanzavecchia A. Broadly neutralizing antiviral antibodies. Annu Rev Immunol. 2013;31:705–742. doi: 10.1146/annurev-immunol-032712-095916. A comprehensive review of broadly neutralizing antibodies against multiple viruses. A comprehensive review of broadly neutralizing antibodies against multiple viruses. [DOI] [PubMed] [Google Scholar]
- 28.Li Y, et al. Immune history shapes specificity of pandemic H1N1 influenza antibody responses. J Exp Med. 2013;210:1493–1500. doi: 10.1084/jem.20130212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li GM, et al. Pandemic H1N1 influenza vaccine induces a recall response in humans that favors broadly cross-reactive memory B cells. Proc Natl Acad Sci U S A. 2012;109:9047–9052. doi: 10.1073/pnas.1118979109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Joyce MG, et al. Vaccine-Induced Antibodies that Neutralize Group 1 and Group 2 Influenza A Viruses. Cell. 2016;166:609–623. doi: 10.1016/j.cell.2016.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andrews SF, et al. Preferential induction of cross-group influenza A hemagglutinin stem-specific memory B cells after H7N9 immunization in humans. Sci Immunol. 2017;2 doi: 10.1126/sciimmunol.aan2676. [DOI] [PubMed] [Google Scholar]
- 32.Lee JE, et al. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature. 2008;454:177–182. doi: 10.1038/nature07082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burton DR, Poignard P, Stanfield RL, Wilson IA. Broadly neutralizing antibodies present new prospects to counter highly antigenically diverse viruses. Science. 2012;337:183–186. doi: 10.1126/science.1225416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burton DR. A vaccine for HIV type 1: the antibody perspective. Proc Natl Acad Sci U S A. 1997;94:10018–10023. doi: 10.1073/pnas.94.19.10018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li Y, et al. Broad HIV-1 neutralization mediated by CD4-binding site antibodies. Nat Med. 2007;13:1032–1034. doi: 10.1038/nm1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Medina-Ramirez M, et al. Broadly cross-neutralizing antibodies in HIV-1 patients with undetectable viremia. J Virol. 2011;85:5804–5813. doi: 10.1128/JVI.02482-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walker LM, et al. Broad and potent neutralizing antibodies from an African donor reveal a new HIV-1 vaccine target. Science. 2009;326:285–289. doi: 10.1126/science.1178746. The isolation of the first of a new generation of HIV broadly neutralizing antibodies and one of the first super-antibodies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Falkowska E, et al. PGV04, an HIV-1 gp120 CD4 binding site antibody, is broad and potent in neutralization but does not induce conformational changes characteristic of CD4. J Virol. 2012;86:4394–4403. doi: 10.1128/JVI.06973-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walker LM, et al. Broad neutralization coverage of HIV by multiple highly potent antibodies. Nature. 2011;477:466–470. doi: 10.1038/nature10373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sok D, et al. Recombinant HIV envelope trimer selects for quaternary-dependent antibodies targeting the trimer apex. Proc Natl Acad Sci U S A. 2014;111:17624–17629. doi: 10.1073/pnas.1415789111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Falkowska E, et al. Broadly neutralizing HIV antibodies define a glycan-dependent epitope on the prefusion conformation of gp41 on cleaved envelope trimers. Immunity. 2014;40:657–668. doi: 10.1016/j.immuni.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Corti D, et al. A neutralizing antibody selected from plasma cells that binds to group 1 and group 2 influenza A hemagglutinins. Science. 2011;333:850–856. doi: 10.1126/science.1205669. Describes a very broad influenza super-antibody of the type that indicates a universal flu vaccine may be possible. [DOI] [PubMed] [Google Scholar]
- 43.De Benedictis P, et al. Development of broad-spectrum human monoclonal antibodies for rabies post-exposure prophylaxis. EMBO Mol Med. 2016;8:407–421. doi: 10.15252/emmm.201505986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robbiani DF, et al. Recurrent Potent Human Neutralizing Antibodies to Zika Virus in Brazil and Mexico. Cell. 2017;169:597–609 e511. doi: 10.1016/j.cell.2017.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mestas J, Hughes CC. Of mice and not men: differences between mouse and human immunology. J Immunol. 2004;172:2731–2738. doi: 10.4049/jimmunol.172.5.2731. [DOI] [PubMed] [Google Scholar]
- 46.Bonsignori M, et al. Analysis of a clonal lineage of HIV-1 envelope V2/V3 conformational epitope-specific broadly neutralizing antibodies and their inferred unmutated common ancestors. J Virol. 2011;85:9998–10009. doi: 10.1128/JVI.05045-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang J, et al. Identification of a CD4-Binding-Site Antibody to HIV that Evolved Near-Pan Neutralization Breadth. Immunity. 2016;45:1108–1121. doi: 10.1016/j.immuni.2016.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Doria-Rose NA, et al. Developmental pathway for potent V1V2-directed HIV-neutralizing antibodies. Nature. 2014;509:55–62. doi: 10.1038/nature13036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kwakkenbos MJ, et al. Generation of stable monoclonal antibody-producing B cell receptor-positive human memory B cells by genetic programming. Nat Med. 2010;16:123–128. doi: 10.1038/nm.2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Robinson JE, et al. Most neutralizing human monoclonal antibodies target novel epitopes requiring both Lassa virus glycoprotein subunits. Nat Commun. 2016;7:11544. doi: 10.1038/ncomms11544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McLellan JS, et al. Structure of RSV fusion glycoprotein trimer bound to a prefusion-specific neutralizing antibody. Science. 2013;340:1113–1117. doi: 10.1126/science.1234914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gilchuk I, et al. Cross-Neutralizing and Protective Human Antibody Specificities to Poxvirus Infections. Cell. 2016;167:684–694 e689. doi: 10.1016/j.cell.2016.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Corti D, et al. Prophylactic and postexposure efficacy of a potent human monoclonal antibody against MERS coronavirus. Proc Natl Acad Sci U S A. 2015;112:10473–10478. doi: 10.1073/pnas.1510199112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Flyak AI, et al. Cross-Reactive and Potent Neutralizing Antibody Responses in Human Survivors of Natural Ebolavirus Infection. Cell. 2016;164:392–405. doi: 10.1016/j.cell.2015.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Corti D, et al. Protective monotherapy against lethal Ebola virus infection by a potently neutralizing antibody. Science. 2016;351:1339–1342. doi: 10.1126/science.aad5224. [DOI] [PubMed] [Google Scholar]
- 56.Misasi J, et al. Structural and molecular basis for Ebola virus neutralization by protective human antibodies. Science. 2016;351:1343–1346. doi: 10.1126/science.aad6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Babcook JS, Leslie KB, Olsen OA, Salmon RA, Schrader JW. A novel strategy for generating monoclonal antibodies from single, isolated lymphocytes producing antibodies of defined specificities. Proc Natl Acad Sci U S A. 1996;93:7843–7848. doi: 10.1073/pnas.93.15.7843. The first description of single B cell technology for the isolation of multiple monoclonal antibodies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tiller T, et al. Efficient generation of monoclonal antibodies from single human B cells by single cell RT-PCR and expression vector cloning. J Immunol Methods. 2008;329:112–124. doi: 10.1016/j.jim.2007.09.017. Application of single B cell technology to the isolation of human monoclonal antibodies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wardemann H, et al. Predominant autoantibody production by early human B cell precursors. Science. 2003;301:1374–1377. doi: 10.1126/science.1086907. [DOI] [PubMed] [Google Scholar]
- 60.Wu X, et al. Rational design of envelope identifies broadly neutralizing human monoclonal antibodies to HIV-1. Science. 2010;329:856–861. doi: 10.1126/science.1187659. Isolation of the prototype broadly neutralizing super-antibody to the CD4 binding site, VRC01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhou T, et al. Structural basis for broad and potent neutralization of HIV-1 by antibody VRC01. Science. 2010;329:811–817. doi: 10.1126/science.1192819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Scheid JF, et al. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science. 2011;333:1633–1637. doi: 10.1126/science.1207227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wu X, et al. Focused evolution of HIV-1 neutralizing antibodies revealed by structures and deep sequencing. Science. 2011;333:1593–1602. doi: 10.1126/science.1207532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bornholdt ZA, et al. Isolation of potent neutralizing antibodies from a survivor of the 2014 Ebola virus outbreak. Science. 2016;351:1078–1083. doi: 10.1126/science.aad5788. Isolation of large numbers of monoclonal antibodies from an Ebola survivor immediately following the outbreak and rapid identification of super-antibodies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Scherer EM, et al. Characteristics of memory B cells elicited by a highly efficacious HPV vaccine in subjects with no pre-existing immunity. PLoS Pathog. 2014;10:e1004461. doi: 10.1371/journal.ppat.1004461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wec AZ, et al. Antibodies from a Human Survivor Define Sites of Vulnerability for Broad Protection against Ebolaviruses. Cell. 2017;169:878–890 e815. doi: 10.1016/j.cell.2017.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sok D, et al. Rapid elicitation of broadly neutralizing antibodies to HIV by immunization in cows. Nature. 2017;548:108–111. doi: 10.1038/nature23301. Reliable generation of broadly neutralizing HIV antibodies by simple immunization in cows suggesting this animal might have special value in super-antibody generation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhao X, et al. Immunization-Elicited Broadly Protective Antibody Reveals Ebolavirus Fusion Loop as a Site of Vulnerability. Cell. 2017;169:891–904 e815. doi: 10.1016/j.cell.2017.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stevens RH, Macy E, Morrow C, Saxon A. Characterization of a circulating subpopulation of spontaneous antitetanus toxoid antibody producing B cells following in vivo booster immunization. J Immunol. 1979;122:2498–2504. [PubMed] [Google Scholar]
- 70.Wrammert J, et al. Rapid cloning of high-affinity human monoclonal antibodies against influenza virus. Nature. 2008;453:667–671. doi: 10.1038/nature06890. Description of a plasmablast approach to super-antibody generation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Priyamvada L, et al. B Cell Responses during Secondary Dengue Virus Infection Are Dominated by Highly Cross-Reactive, Memory-Derived Plasmablasts. J Virol. 2016;90:5574–5585. doi: 10.1128/JVI.03203-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dejnirattisai W, et al. A new class of highly potent, broadly neutralizing antibodies isolated from viremic patients infected with dengue virus. Nat Immunol. 2015;16:170–177. doi: 10.1038/ni.3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nair N, et al. VP4- and VP7-specific antibodies mediate heterotypic immunity to rotavirus in humans. Sci Transl Med. 2017;9:eaam5434. doi: 10.1126/scitranslmed.aam5434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Silveira EL, et al. Vaccine-induced plasmablast responses in rhesus macaques: phenotypic characterization and a source for generating antigen-specific monoclonal antibodies. J Immunol Methods. 2015;416:69–83. doi: 10.1016/j.jim.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wrammert J, et al. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J Exp Med. 2011;208:181–193. doi: 10.1084/jem.20101352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rogers TF, et al. Zika virus activates de novo and cross-reactive memory B cell responses in dengue-experienced donors. Sci Immunol. 2017 doi: 10.1126/sciimmunol.aan6809. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pascal KE, et al. Pre- and postexposure efficacy of fully human antibodies against Spike protein in a novel humanized mouse model of MERS-CoV infection. Proc Natl Acad Sci U S A. 2015;112:8738–8743. doi: 10.1073/pnas.1510830112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Luke T, et al. Human polyclonal immunoglobulin G from transchromosomic bovines inhibits MERS-CoV in vivo. Sci Transl Med. 2016;8:326ra321. doi: 10.1126/scitranslmed.aaf1061. [DOI] [PubMed] [Google Scholar]
- 79.Hooper JW, et al. DNA vaccine-derived human IgG produced in transchromosomal bovines protect in lethal models of hantavirus pulmonary syndrome. Sci Transl Med. 2014;6:264ra162. doi: 10.1126/scitranslmed.3010082. [DOI] [PubMed] [Google Scholar]
- 80.Gardner CL, et al. Antibody Preparations from Human Transchromosomic Cows Exhibit Prophylactic and Therapeutic Efficacy against Venezuelan Equine Encephalitis Virus. J Virol. 2017:91. doi: 10.1128/JVI.00226-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dye JM, et al. Production of Potent Fully Human Polyclonal Antibodies against Ebola Zaire Virus in Transchromosomal Cattle. Sci Rep. 2016;6:24897. doi: 10.1038/srep24897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sapparapu G, et al. Neutralizing human antibodies prevent Zika virus replication and fetal disease in mice. Nature. 2016;540:443–447. doi: 10.1038/nature20564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang Q, et al. Molecular determinants of human neutralizing antibodies isolated from a patient infected with Zika virus. Sci Transl Med. 2016;8:369ra179. doi: 10.1126/scitranslmed.aai8336. [DOI] [PubMed] [Google Scholar]
- 84.Priyamvada L, et al. Human antibody responses after dengue virus infection are highly cross-reactive to Zika virus. Proc Natl Acad Sci U S A. 2016;113:7852–7857. doi: 10.1073/pnas.1607931113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barba-Spaeth G, et al. Structural basis of potent Zika-dengue virus antibody cross-neutralization. Nature. 2016;536:48–53. doi: 10.1038/nature18938. [DOI] [PubMed] [Google Scholar]
- 86.Beltramello M, et al. The human immune response to Dengue virus is dominated by highly cross-reactive antibodies endowed with neutralizing and enhancing activity. Cell Host Microbe. 2010;8:271–283. doi: 10.1016/j.chom.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shingai M, et al. Antibody-mediated immunotherapy of macaques chronically infected with SHIV suppresses viraemia. Nature. 2013;503:277–280. doi: 10.1038/nature12746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Prabakaran M, et al. Combination therapy using chimeric monoclonal antibodies protects mice from lethal H5N1 infection and prevents formation of escape mutants. PLoS One. 2009;4:e5672. doi: 10.1371/journal.pone.0005672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mire CE, et al. Human-monoclonal-antibody therapy protects nonhuman primates against advanced Lassa fever. Nat Med. 2017;23:1146–1149. doi: 10.1038/nm.4396. First demonstration in non-human primates that monoclonal antibodies can protect against advanced Lassa fever. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Magnani DM, et al. Neutralizing human monoclonal antibodies prevent Zika virus infection in macaques. Sci Transl Med. 2017:9. doi: 10.1126/scitranslmed.aan8184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Xu L, et al. Trispecific broadly neutralizing HIV antibodies mediate potent SHIV protection in macaques. Science. 2017;358:85–90. doi: 10.1126/science.aan8630. Novel design of antibodies to cope with HIV diversity by incorporating three specificities into a single antibody-like molecule. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Julg B, et al. Protection against a mixed SHIV challenge by a broadly neutralizing antibody cocktail. Sci Transl Med. 2017:9. doi: 10.1126/scitranslmed.aao4235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang J, et al. A Human Bi-specific Antibody against Zika Virus with High Therapeutic Potential. Cell. 2017;171:229–241 e215. doi: 10.1016/j.cell.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Palivizumab, a humanized respiratory syncytial virus monoclonal antibody reduces hospitalization from respiratory syncytial virus infection in high-risk infants. The IMpact-RSV Study Group. Pediatrics. 1998;102:531–537. [PubMed] [Google Scholar]
- 95.Zhu Q, et al. A highly potent extended half-life antibody as a potential RSV vaccine surrogate for all infants. Sci Transl Med. 2017:9. doi: 10.1126/scitranslmed.aaj1928. Description of an RSV super-antibody that shows about ten times greater in vivo efficacy than palivizumab in cotton rats. [DOI] [PubMed] [Google Scholar]
- 96.Sui J, et al. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nat Struct Mol Biol. 2009;16:265–273. doi: 10.1038/nsmb.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Qiu X, et al. Ebola GP-specific monoclonal antibodies protect mice and guinea pigs from lethal Ebola virus infection. PLoS Negl Trop Dis. 2012;6:e1575. doi: 10.1371/journal.pntd.0001575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wilson JA, et al. Epitopes involved in antibody-mediated protection from Ebola virus. Science. 2000;287:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- 99.Mascola JR, et al. Protection of Macaques against pathogenic simian/human immunodeficiency virus 89.6PD by passive transfer of neutralizing antibodies. J Virol. 1999;73:4009–4018. doi: 10.1128/jvi.73.5.4009-4018.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mascola JR, et al. Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nat Med. 2000;6:207–210. doi: 10.1038/72318. [DOI] [PubMed] [Google Scholar]
- 101.Parren PW, et al. Antibody protects macaques against vaginal challenge with a pathogenic R5 simian/human immunodeficiency virus at serum levels giving complete neutralization in vitro. J Virol. 2001;75:8340–8347. doi: 10.1128/JVI.75.17.8340-8347.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Paules CI, et al. The Hemagglutinin A Stem Antibody MEDI8852 Prevents and Controls Disease and Limits Transmission of Pandemic Influenza Viruses. J Infect Dis. 2017;216:356–365. doi: 10.1093/infdis/jix292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hessell AJ, et al. Effective, low-titer antibody protection against low-dose repeated mucosal SHIV challenge in macaques. Nat Med. 2009;15:951–954. doi: 10.1038/nm.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hessell AJ, et al. Broadly neutralizing human anti-HIV antibody 2G12 is effective in protection against mucosal SHIV challenge even at low serum neutralizing titers. PLoS Pathog. 2009;5:e1000433. doi: 10.1371/journal.ppat.1000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shingai M, et al. Passive transfer of modest titers of potent and broadly neutralizing anti-HIV monoclonal antibodies block SHIV infection in macaques. J Exp Med. 2014;211:2061–2074. doi: 10.1084/jem.20132494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Julg B, et al. Broadly neutralizing antibodies targeting the HIV-1 envelope V2 apex confer protection against a clade C SHIV challenge. Sci Transl Med. 2017:9. doi: 10.1126/scitranslmed.aal1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Deal CE, Balazs AB. Vectored antibody gene delivery for the prevention or treatment of HIV infection. Curr Opin HIV AIDS. 2015;10:190–197. doi: 10.1097/COH.0000000000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Johnson PR, et al. Vector-mediated gene transfer engenders long-lived neutralizing activity and protection against SIV infection in monkeys. Nat Med. 2009;15:901–906. doi: 10.1038/nm.1967. Initial report of vectored prophylaxis applied in macaques. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gardner MR, et al. AAV-expressed eCD4-Ig provides durable protection from multiple SHIV challenges. Nature. 2015;519:87–91. doi: 10.1038/nature14264. Extreme breadth for an engineered antibody molecule incorportaing novel features. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Balazs AB, et al. Antibody-based protection against HIV infection by vectored immunoprophylaxis. Nature. 2011;481:81–84. doi: 10.1038/nature10660. Development of vectored immunoprophylaxis for HIV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Saunders KO, et al. Sustained Delivery of a Broadly Neutralizing Antibody in Nonhuman Primates Confers Long-Term Protection against Simian/Human Immunodeficiency Virus Infection. J Virol. 2015;89:5895–5903. doi: 10.1128/JVI.00210-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Flingai S, et al. Protection against dengue disease by synthetic nucleic acid antibody prophylaxis/immunotherapy. Sci Rep. 2015;5:12616. doi: 10.1038/srep12616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Muthumani K, et al. Optimized and enhanced DNA plasmid vector based in vivo construction of a neutralizing anti-HIV-1 envelope glycoprotein Fab. Human vaccines & immunotherapeutics. 2013;9:2253–2262. doi: 10.4161/hv.26498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pardi N, et al. Administration of nucleoside-modified mRNA encoding broadly neutralizing antibody protects humanized mice from HIV-1 challenge. Nat Commun. 2017;8:14630. doi: 10.1038/ncomms14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nault JC, et al. Recurrent AAV2-related insertional mutagenesis in human hepatocellular carcinomas. Nat Genet. 2015;47:1187–1193. doi: 10.1038/ng.3389. [DOI] [PubMed] [Google Scholar]
- 116.Gao G, et al. Erythropoietin gene therapy leads to autoimmune anemia in macaques. Blood. 2004;103:3300–3302. doi: 10.1182/blood-2003-11-3852. [DOI] [PubMed] [Google Scholar]
- 117.Tjelle TE, et al. Monoclonal antibodies produced by muscle after plasmid injection and electroporation. Mol Ther. 2004;9:328–336. doi: 10.1016/j.ymthe.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 118.Hu J, Robinson JL. Treatment of respiratory syncytial virus with palivizumab: a systematic review. World J Pediatr. 2010;6:296–300. doi: 10.1007/s12519-010-0230-z. [DOI] [PubMed] [Google Scholar]
- 119.Barouch DH, et al. Therapeutic efficacy of potent neutralizing HIV-1-specific monoclonal antibodies in SHIV-infected rhesus monkeys. Nature. 2013;503:224–228. doi: 10.1038/nature12744. Surpisingly effective monotherapy of SHIV infection in macaques. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Horwitz JA, et al. HIV-1 suppression and durable control by combining single broadly neutralizing antibodies and antiretroviral drugs in humanized mice. Proc Natl Acad Sci U S A. 2013;110:16538–16543. doi: 10.1073/pnas.1315295110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Poignard P, et al. Neutralizing antibodies have limited effects on the control of established HIV-1 infection in vivo. Immunity. 1999;10:431–438. doi: 10.1016/s1074-7613(00)80043-6. [DOI] [PubMed] [Google Scholar]
- 122.Caskey M, et al. Viraemia suppressed in HIV-1-infected humans by broadly neutralizing antibody 3BNC117. Nature. 2015;522:487–491. doi: 10.1038/nature14411. First use of a super-antibody in HIV infection in humans. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Scheid JF, et al. HIV-1 antibody 3BNC117 suppresses viral rebound in humans during treatment interruption. Nature. 2016;535:556–560. doi: 10.1038/nature18929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Caskey M, et al. Antibody 10-1074 suppresses viremia in HIV-1-infected individuals. Nat Med. 2017;23:185–191. doi: 10.1038/nm.4268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lynch RM, et al. Virologic effects of broadly neutralizing antibody VRC01 administration during chronic HIV-1 infection. Sci Transl Med. 2015;7:319ra206. doi: 10.1126/scitranslmed.aad5752. [DOI] [PubMed] [Google Scholar]
- 126.Bar KJ, et al. Effect of HIV Antibody VRC01 on Viral Rebound after Treatment Interruption. The New England journal of medicine. 2016;375:2037–2050. doi: 10.1056/NEJMoa1608243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Schoofs T, et al. HIV-1 therapy with monoclonal antibody 3BNC117 elicits host immune responses against HIV-1. Science. 2016;352:997–1001. doi: 10.1126/science.aaf0972. Super-antibody HIV therapy appears to enhance host immune responses generally. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zeitlin L, et al. Monoclonal antibody therapy for Junin virus infection. Proc Natl Acad Sci U S A. 2016;113:4458–4463. doi: 10.1073/pnas.1600996113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Qiu X, et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature. 2014;514:47–53. doi: 10.1038/nature13777. First demonstration of successful antibody therapy against established Ebola virus disease in non-human primates. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Van Heeke G, et al. Nanobodies(R) as inhaled biotherapeutics for lung diseases. Pharmacol Ther. 2017;169:47–56. doi: 10.1016/j.pharmthera.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 131.Schepens B, et al. Nanobodies(R) specific for respiratory syncytial virus fusion protein protect against infection by inhibition of fusion. J Infect Dis. 2011;204:1692–1701. doi: 10.1093/infdis/jir622. [DOI] [PubMed] [Google Scholar]
- 132.Detalle L, et al. Generation and Characterization of ALX-0171, a Potent Novel Therapeutic Nanobody for the Treatment of Respiratory Syncytial Virus Infection. Antimicrobial agents and chemotherapy. 2015;60:6–13. doi: 10.1128/AAC.01802-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rossey I, et al. Potent single-domain antibodies that arrest respiratory syncytial virus fusion protein in its prefusion state. Nat Commun. 2017;8:14158. doi: 10.1038/ncomms14158. Use of single-domain antibody against RSV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hinton PR, et al. Engineered human IgG antibodies with longer serum half-lives in primates. J Biol Chem. 2004;279:6213–6216. doi: 10.1074/jbc.C300470200. [DOI] [PubMed] [Google Scholar]
- 135.Dall’Acqua WF, Kiener PA, Wu H. Properties of human IgG1s engineered for enhanced binding to the neonatal Fc receptor (FcRn) J Biol Chem. 2006;281:23514–23524. doi: 10.1074/jbc.M604292200. [DOI] [PubMed] [Google Scholar]
- 136.Zalevsky J, et al. Enhanced antibody half-life improves in vivo activity. Nat Biotechnol. 2010;28:157–159. doi: 10.1038/nbt.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Yu XQ, et al. Safety, Tolerability, and Pharmacokinetics of MEDI4893, an Investigational, Extended-Half-Life, Anti-Staphylococcus aureus Alpha-Toxin Human Monoclonal Antibody, in Healthy Adults. Antimicrobial agents and chemotherapy. 2017:61. doi: 10.1128/AAC.01020-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ko SY, et al. Enhanced neonatal Fc receptor function improves protection against primate SHIV infection. Nature. 2014;514:642–645. doi: 10.1038/nature13612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gautam R, et al. A single injection of anti-HIV-1 antibodies protects against repeated SHIV challenges. Nature. 2016;533:105–109. doi: 10.1038/nature17677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lazar GA, et al. Engineered antibody Fc variants with enhanced effector function. Proc Natl Acad Sci U S A. 2006;103:4005–4010. doi: 10.1073/pnas.0508123103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Presta LG. Molecular engineering and design of therapeutic antibodies. Curr Opin Immunol. 2008;20:460–470. doi: 10.1016/j.coi.2008.06.012. Review of strategies for enhancing antibody effector function. [DOI] [PubMed] [Google Scholar]
- 142.Bowers PM, et al. Coupling mammalian cell surface display with somatic hypermutation for the discovery and maturation of human antibodies. Proc Natl Acad Sci U S A. 2011;108:20455–20460. doi: 10.1073/pnas.1114010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Boder ET, Wittrup KD. Yeast surface display for screening combinatorial polypeptide libraries. Nat Biotechnol. 1997;15:553–557. doi: 10.1038/nbt0697-553. [DOI] [PubMed] [Google Scholar]
- 144.McCafferty J, Griffiths AD, Winter G, Chiswell DJ. Phage antibodies: filamentous phage displaying antibody variable domains. Nature. 1990;348:552–554. doi: 10.1038/348552a0. [DOI] [PubMed] [Google Scholar]
- 145.Huse WD, et al. Generation of a large combinatorial library of the immunoglobulin repertoire in phage lambda. Science. 1989;246:1275–1281. doi: 10.1126/science.2531466. [DOI] [PubMed] [Google Scholar]
- 146.Lee EC, et al. Complete humanization of the mouse immunoglobulin loci enables efficient therapeutic antibody discovery. Nat Biotechnol. 2014;32:356–363. doi: 10.1038/nbt.2825. [DOI] [PubMed] [Google Scholar]
- 147.Murphy AJ, et al. Mice with megabase humanization of their immunoglobulin genes generate antibodies as efficiently as normal mice. Proc Natl Acad Sci U S A. 2014;111:5153–5158. doi: 10.1073/pnas.1324022111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Scheid JF, et al. A method for identification of HIV gp140 binding memory B cells in human blood. J Immunol Methods. 2009;343:65–67. doi: 10.1016/j.jim.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lanzavecchia A, Corti D, Sallusto F. Human monoclonal antibodies by immortalization of memory B cells. Curr Opin Biotechnol. 2007;18:523–528. doi: 10.1016/j.copbio.2007.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Huang J, et al. Isolation of human monoclonal antibodies from peripheral blood B cells. Nat Protoc. 2013;8:1907–1915. doi: 10.1038/nprot.2013.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lee JH, et al. A Broadly Neutralizing Antibody Targets the Dynamic HIV Envelope Trimer Apex via a Long, Rigidified, and Anionic beta-Hairpin Structure. Immunity. 2017;46:690–702. doi: 10.1016/j.immuni.2017.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.McCoy LE, Burton DR. Identification and specificity of broadly neutralizing antibodies against HIV. Immunol Rev. 2017;275:11–20. doi: 10.1111/imr.12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Dreyfus C, et al. Highly conserved protective epitopes on influenza B viruses. Science. 2012;337:1343–1348. doi: 10.1126/science.1222908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Corti D, et al. Tackling influenza with broadly neutralizing antibodies. Current opinion in virology. 2017;24:60–69. doi: 10.1016/j.coviro.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wu NC, Wilson IA. A Perspective on the Structural and Functional Constraints for Immune Evasion: Insights from Influenza Virus. Journal of molecular biology. 2017;429:2694–2709. doi: 10.1016/j.jmb.2017.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wen X, et al. Structural basis for antibody cross-neutralization of respiratory syncytial virus and human metapneumovirus. Nature microbiology. 2017;2:16272. doi: 10.1038/nmicrobiol.2016.272. [DOI] [PMC free article] [PubMed] [Google Scholar]