Abstract
Importance
While contact lenses have been used for decades to optically correct children after cataract surgery, there has never been a prospective study looking at contact lens adherence in aphakic children.
Objective
To evaluate contact lens adherence and its relationship to visual outcome in a cohort of children treated for unilateral cataract surgery.
Design, Setting and Participants
Secondary analysis of a multicenter randomized clinical trial (Infant Aphakia Treatment Study) of 57 infants (56% female; 86% White) born from August 1, 2004 through December 31, 2008 who were treated with 1 of 2 treatments for unilateral congenital cataract and followed and followed to an age of 5.0 years. Data analysis was performed from August 9, 2016 to August 6, 2017.
Intervention
Cataract extraction and randomization to implantation of an intraocular lens vs. being left aphakic for the first 5 years of life.
Main Outcomes and Measures
Contact lens adherence assessed by a 48 hour recall telephone interview which was developed for this project and was administered every 3 months starting 3 months after surgery to age 5 years. A traveling examiner assessed visual acuity at age 4.5 years. Adherence to prescribed contact lens use was estimated as the mean percent of waking hours as reported in two or more interviews for each year of life. For each participant who had at least two interviews during four or five years (n=47) we also calculated the mean percentage of waking hours in which the contact lens was worn over the entire study period.
Results
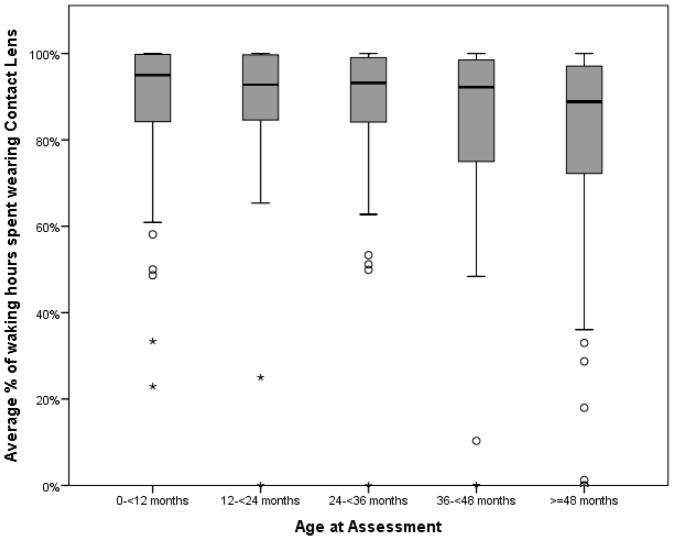
A total of 872 telephone interviews were completed. Most participants wore their contact lens nearly all waking hours with the median reported contact lens use of 95% (IQR 84%, 100%) in the first year of life, 93% (IQR 85%,99%) in the second, 93% (IQR 85%, 99%) in the third year, 93% (IQR 75%,99%) in the fourth year, and 89% (IQR 71%, 97%) in the fifth year of life. There was a tendency for poorer reported adherence at older ages (F=3.85 p=0.02 for repeated measures ANOVA with Greenhouse-Geisser adjustment). Using repeating measures ANOVA, there were no statistically significant differences in contact lens use by gender (f=0.08, p=−.77), insurance coverage (F=0.012, p=0.91) or age at cataract surgery(F=0.073, p=0.78). Using linear regression, children who wore the contact lens a greater proportion of waking hours over the entire study period tended to have had better visual acuity at age 4 ½, even after accounting for the adherence to patching (partial correlation = −0.026; p=0.08).
Conclusion and Relevance
These results confirm that it is possible to achieve a high level (median 88%, IQR=82%,94%) of aphakic contact lens adherence over a 5 year period in children.
Clinical Trial Registration
clinicaltrials.gov Identifier NCT00212134
Introduction
The Infant Aphakia Treatment study (IATS) was designed to compare the visual outcomes in children who were 1 to 6 months of age at the time of unilateral congenital cataract surgery and were randomized to either optical correction with contact lenses or an intraocular lens (IOL).1 Children who were randomized to aphakia were treated with a contact lens. At age 4.5 years, about 20% of treated eyes had visual acuity of 20/32 or better, 30% had 20/40 to 20/100 acuity and 50% had 20/200 or worse acuity.2 We have shown that the visual results are comparable for optical correction with either a contact lens or an IOL at both ages 1 and 4.5 years, but significantly more infants randomized to IOL implantation required additional intraocular surgeries.2–4 Therefore, we recommended that infants undergoing surgery for a unilateral cataract during the first 6 months of life be left aphakic and be optically corrected with a contact lens.3
Parental adherence to the treatment regimen of patching and visual correction with a contact lens or spectacles is believed to play an important role in the visual outcome of children with unilateral congenital cataracts.5 We have previously shown that adherence to patching is associated with visual acuity, and that overall about 10–14% of the variation in visual acuity at age 4.5 years in the IATS could be attributed to patching adherence.6 In previous publications, we described the clinical findings for children who were randomized to contact lens wear.7,8 We now report contact lens adherence for the infants randomized to contact lens wear in the IATS.
Material and Methods
The overall design of the IATS has been reported previously.1 The IATS is a multicenter randomized clinical trial comparing IOL and contact lens treatment after unilateral congenital cataract surgery in children 6 months of age or younger who were born from August 1, 2004 through December 31, 2008. Data analysis was performed from August 9, 2016 to August 6, 2017. This study was approved by the institutional review boards of all the participating institutions and was in compliance with the Health Insurance Portability and Accountability Act. Written informed consent was obtained from a parent or legal guardian of all patients before randomization.
Contact Lens Correction
Within 1 week after cataract surgery, patients randomized to this group were fitted with either a silicone elastomer (SE) (Silsoft Super Plus; Bausch & Lomb, Rochester, NY) or gas permeable (GP) (X-cel Specialty Contacts, Duluth, GA) contact lens with a +2.00 diopter overcorrection to provide a near-point correction. The choice of the type of contact lens fitted was a shared decision between investigators and caregivers. Application and removal training was provided to each caregiver. The lens power was adjusted for infinity at approximately 2 years of age along with spectacle overcorrection with a straight top bifocal with a +3.00 diopter add bisecting the pupil. Contact lens professionals participating in the study were certified by written examination. Patients were evaluated by both the surgeon and the IATS certified contact lens professional at each study visit and parameter changes were made as needed to optimize the power and fit of the lens. Contact lenses were supplied at no cost to caregivers. Whenever a contact lens was prescribed, two contact lens were dispensed to that a spare contact lens would be available in the event that a contact lens was lost. A complete description of the fitting process, contact lens characteristics, and adverse events have been reported previously.8 IATS investigators were only allowed to implant a secondary IOL in an aphakic eye before age 5 years if a child was deemed to be a contact lens failure by the IATS Executive Committee. A patient was considered to be a contact lens failure if they wore a contact lens for fewer than 4 hours per day on average for a period of 8 consecutive weeks. Contact lens use prior to secondary IOL implantation was included in all analyses.
Evaluation of adherence
Adherence to contact lens use was assessed using adherence interviews of the caregivers.6,9 We modeled our assessment of adherence after dietary assessments that have been used in a variety of epidemiologic studies including in preschool-aged children.
For this study, adherence was evaluated using a quarterly telephone-administered 48-hour adherence interview. During the study period, interviews assessing patching and contact lens adherence were performed approximately every 3 months, starting 3 months after surgery. Each month, study staff compiled a list of all study patients due for a quarterly interview. A number was randomly generated from 1 to 31 (28 for February, 30 for April, June, September and November) indicating which day of the month the interviews would be conducted. If study staff was unable to complete an interview on the assigned day for that participant, they attempted to conduct the interview the next day for four consecutive days. In order to obtain as much information about both weekend and weekdays as possible, if the selected day was a weekend day, the interviews were attempted on four consecutive weekend days. If the selected day was a weekday, the interview was attempted on four consecutive weekdays. If the interview was not completed after four attempts the study staff made two additional attempts to conduct the interview over the next week, regardless of the day of the week.
The adherence interview was a 30-minute, semi-structured telephone interview conducted in the primary caregiver’s preferred language (English, Spanish, Portuguese) by study staff at the Data Coordinating Center to minimize any concerns that the caregiver might have about confidentiality of the interview. For each family, the staff member who interviewed the caregiver was the same. The adherence interview was designed to gain information about the proportion of time that the child wore the contact lens during the previous 48-hours while awake. The structure of the interviews used questions about the child’s activities, sleep and wake times, meal times, bath times, etc. as anchors to improve recall. For example, research has shown that memory can be improved by asking the caregiver to recall what time the child woke, when he/she was dressed, and when he/she had breakfast, and then asking if the child was wearing his/her contact lens at these times. The reliability and validity of this questionnaire for assessing adherence to patching have previously been described (reference 6 – which now probably should be reference 9)
For the current analyses we estimated the mean percentage of waking hours that each child wore his/her contact lens adherence during five separate time frames: from surgery to 12 months of age, from 12 to 24 months of age, from 24 to 36 months of age, from 36 to 48 months of age and from 48 to 60 months of age since age may impact adherence to contact lens use. Additionally, we limited analyses within each time point to participants who had completed at least 2 adherence interviews during the time window to minimize the impact of day-to-day variation in reported contact lens use. We also calculated an overall percentage of waking hours spent wearing the contact lens over the 5 year period as a mean of the percentage reported in each of the five time periods. This analysis was limited to children for whom adherence to contact lens use was reported in at least 2 interviews during at least four of the five time periods.
Patching Regimen
Parents were instructed to have their child wear an adhesive occlusive patch over the unoperated eye for 1 hour/day for each month of age until age 8 months. Thereafter, patching was prescribed for one-half of waking hours.
Visual Acuity Assessment
Monocular optotype acuity was assessed at 4.5 years ± 1 month of age by a masked traveling examiner using the Amblyopia Treatment Study-HOTV test. Patients were tested wearing their best correction which had been updated at their last study visit three months earlier. Visual acuity was tested first in the aphakic/pseudophakic eye. The eye not being tested was occluded.
Statistical Analysis
Statistical analyses were completed using SPSS 23. The overall mean percentage of waking hours spent wearing a contact lens was estimated using a normal distribution. Differences in mean adherence by age were assessed using repeated measures Analyses of Variance. Differences in mean adherence by other characteristics such as gender, the availability of private health insurance and age at the time of surgery (≤48 days; > 48 days) were assessed using repeated measures Analysis of Variance. Multiple linear regression was used to assess the relationship between percentage of waking hours patched and visual acuity. Additionally, as the distribution of means across the population was highly skewed, with most children wearing a contact lens nearly 100% of waking hours, we repeated analyses using non-parametric statistics. Statistical significance was set at alpha = 0.05.
Results
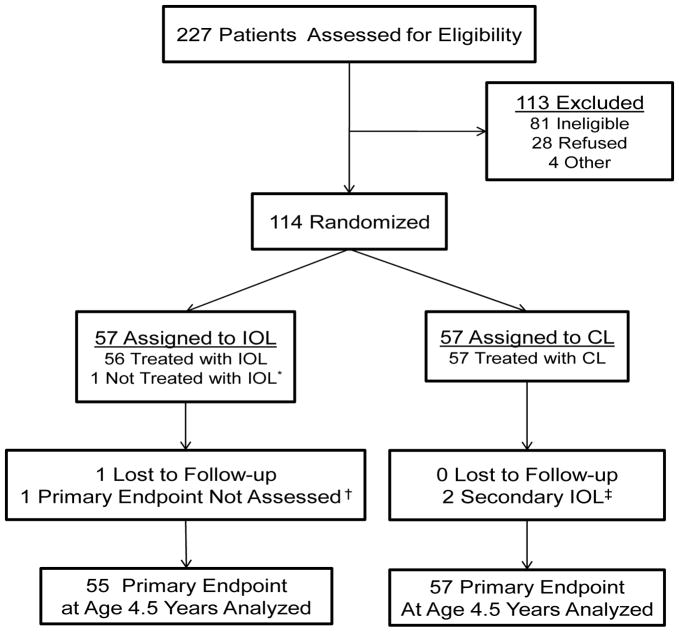
There were 114 patients enrolled in the study with 57 randomized to contact lens treatment (Figure 1). The median age for the contact lens group at the time of cataract surgery was 1.8 months (interquartile range (IRQ), 1.1–3.1 months); 32 (56%) were female and 49 (86%) were white. Two patients had non-amblyopic no light perception or light perception vision shortly after surgery and did not receive optical correction and therefore were not included in the analysis. Three had secondary IOLs implanted between ages 1 and 5 years after being deemed contact lens failures. In all three cases, caregivers were unable to manage the application and removal of contact lenses in their child’s eye. All three wore SE lenses only. Of the remaining 52 eyes who wore contact lenses, 24 (46%) were treated with SE lenses only, 11 (21%) were treated with GP lenses only, and 17 (33%) used both lens types and/or soft contact lenses at various points of time. Of the 41 patients wearing SE lenses between ages 1 and 5 years, 28 wore a lens on a continuous wear schedule (7–21 nights), 6 on a daily wear basis, 3 alternated between daily and continuous wear; the wear schedule was not documented for 4 patients. Children wearing a GP lens wore the lens on a daily wear basis.
Figure 1.
Consort diagram for the Infant Aphakia Treatment Study.
A total of 872 telephone interviews were completed for children randomized to the contact lens group. Prior to age 4, more than half of all children randomized to receive a contact lens wore the lens at least 90% of waking hours. In year 5, the median the median reported use was 89% of waking hours (Table 1). There was a tendency for contact lens adherence to decrease slightly with age (p<0.01) be higher in the first years after surgery (Figure 2). However, there were a number of individuals who reported wearing their contact lens for less than 90% of waking hours in one age bin, but in a later age bin reported better adherence.
Table 1.
Reported percentage of waking hours spent wearing contact lenses from ages 1 to 5 years in the Infant Aphakia Treatment Study
| Age, mo | No. (%) | Mean (SD) | Median (IQR) | Wearing Contact Len ≥80% of Waking Hours | Wearing Contact Len ≥90% of Waking Hours |
|---|---|---|---|---|---|
| <12 | 50 (90.9%) | 87.6 (17.9) | 95.0 (83.7,99.8) | 40 (80.0%) | 33 (66.0%) |
| 12–24 | 52 (94.5%) | 87.5 (18.4) | 92.8 (84.6,99.8) | 41 (78.9%) | 33 (63.4%) |
| 24–36 | 48 (87.2%) | 86.5 (18.7) | 93.2 (80.9,99.5) | 37 (77.0%) | 32 (66.7%) |
| 36–48 | 48 (87.2%) | 80.6 (27.5) | 92.2 (75.0,98.6) | 33 (68.8%) | 29 (60.4%) |
| ≥48 | 44 (80.0%) | 76.0 (29.7) | 88.8 (70.7,97.1) | 28 (63.6%) | 21(47.7%) |
| Overall | 47 (85.4%) | 85.6 (13.1) | 88.3 (81.9,94.1) | 38 (80.9%) | 21 (44.7%) |
CL=contact lens
Number of participants who had completed at least two adherence interviews in the year
Number of participants who had completed at least two adherence interviews in at least four of the five years.
Figure 2. Reported percent of waking hours spent wearing contact lenses by age in the Infant Aphakia Treatment Study.
The horizontal line in the middle of the box indicates median; top and bottom borders of the boxes 75th and 25th percentiles; whiskers 2 SD from median; data points shown as circles, outliers and asterisks, extreme outliers.
Additional analyses were performed in order to evaluate potential predictors of contact lens adherence, including gender, private insurance, and age at time of surgery. Using repeating measures ANOVA, there were no statistically significant differences in contact lens use by gender (f=0.08, p=−.77), insurance coverage (F=0.012, p=0.91) or age at cataract surgery (F=0.073, p=0.78) (eFigures 1–3).
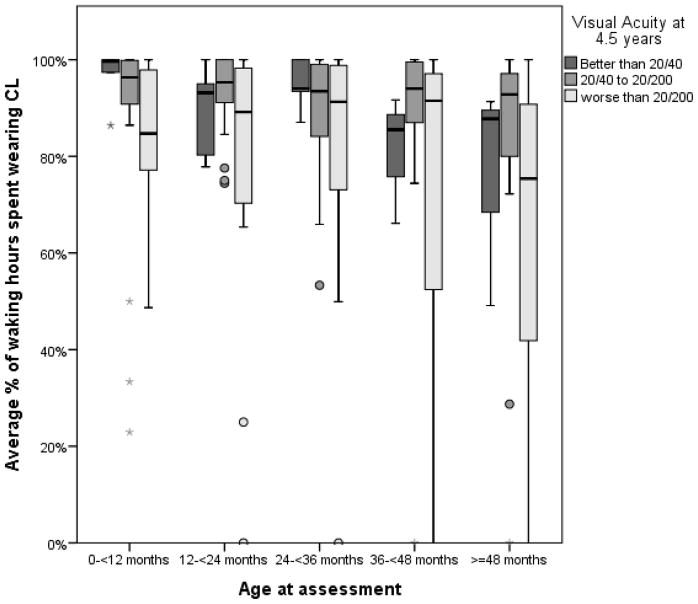
We evaluated the contact lens adherence in groups defined by the visual acuity outcome at 4.5 years (20/32 or better, 20/40–20/200, worse than 20/200) (Figure 3). In linear regression, a greater average number of hours of contact lens use over the five year period tended to be associated with better visual acuity at age 4 ½ years (partial correlation = −0.26; p=0.08), even after accounting for the number of hours spent wearing an occlusive patch; and together, average waking hours wearing the patch and average percentage of waking time spent wearing a contact lens 12% of the variation in visual acuity.
Figure 3. Reported percent of waking hours spent wearing contact lenses from ages 1 to 5 years for different visual outcomes in the Infant Aphakia Treatment Study.
The horizontal line in the middle of the box indicates median; top and bottom borders of the boxes 75th and 25th percentiles; whiskers 2 SD from median; data points shown as circles, outliers and asterisks, extreme outliers.
We also evaluated the relationship between reported patching and contact lens adherence. Children with more reported hours of patching also had a greater percentage of waking hours wearing a contact lens with Pearson’s correlation coefficients ranging from 0.13 between 24 and 36 months of age (p=0.36) to 0.0.43 (p<0.01) between 48 and 60 months of age. The correlation was highest in the first year and after 36 months of age. Although it is not surprising that patients with poor adherence to one form of therapy would be less adherent to another, this means that it may be difficult to separate the relationship between visual acuity and contact lens adherence from visual acuity and occlusion therapy adherence.
Discussion
We found that most families reported that their child wore a contact lens more than 80% of their waking hours from the time of cataract extraction through age 5 years. Only three children randomized to contact lenses stopped wearing them for adherence reasons.
We are unaware of any previous studies that have evaluated aphakic contact lens adherence in children after congenital cataract surgery. Most other studies evaluating contact lens use after congenital cataract surgery have been retrospective. For example, Autrata and coworkers10 reported the visual outcomes for 23 children who underwent unilateral congenital cataract surgery and were optically corrected with aphakic contact lenses, but they did not report contact lens adherence. While the IoLunder2 cohort study was a prospective study, patients were not randomized to different optical treatments and no contact lens adherence data have been published to date from the study.11
We were unable to show a clear relationship between contact lens adherence and visual outcomes. There are a number of possible reasons for this. First, contact lens adherence was quite high in our series and there may be only a small additional benefit to wearing a contact lens for all waking hours even in an aphakic eye. Second, there are likely many other factors that influenced visual outcomes in addition to contact lens adherence including patching adherence, age at surgery, socioeconomic factors and adverse events.,12,13 Lastly, our sample size may have been too small to identify a significant relationship between contact lens adherence and visual outcomes.
In our study, 3 of 57 (6%) of patients randomized to contact lens wear underwent secondary IOL placement before age 5 years. In all 3 cases it was due to caregivers having difficulty applying and removing contact lenses rather than adverse events arising from wearing contact lenses. Most previous studies have reported a higher contact lens failure rate. Mittelviefhies et al14 reported 20 of 90 (22%) children discontinued contact lens wear after congenital cataract surgery; 12 who were aphakic in one eye and 8 in both eyes. The most common reasons cited for discontinuing contact lens use included: poor vision, parental noncompliance, and patient intolerance. Ozbek and coworkers reported 5 of 51 (10%) children discontinued SE contact lens wear after congenital cataract surgery. The reasons cited for doing so included the frequent loss of lenses or financial problems (n=3) and recurrent irritation and corneal infiltrates (n=2). Loudot et al15 reported that 3 of 17 (17%) children discontinued GP contact lenses use because their caregiver had problems manipulating the lenses. Amaya and coworkers reported that 12 of 83 (15%) children discontinued hydrogel contact lens use because caregivers had difficulty handling the lenses, frequent lens loss, hypoxic corneal ulcerations (n=2) and caregiver preference for glasses. The hypoxic corneal ulcerations were likely related to the low oxygen transmissibility of hydrogel contact lenses in high plus powers. Finally, Aasuri et al16 reported that one-third of aphakic children switched to glasses or had an IOL implanted within 6 months of being fitted with SE contact lenses. The low contact lens failure rate in the IATS is likely due to many factors such as the lenses being provided at no cost to caregivers, quarterly telephone interviews assessing contact lens adherence and participating surgeons only implanting secondary IOLs if patients met strict contact lens failure criteria.
The cost of contact lenses is likely a significant factor affecting contact lens adherence for many children after congenital cataract surgery. Russell and coworkers7 reported that on average children in the IATS cohort required 11 SE replacement lenses or 17 GP replacement lenses from infancy to age 5 years. Kruger and coworkers17 have estimated that the cost of supplies (e.g. contact lenses, spectacles and patches) is twice as high for children randomized to aphakia and contact lens wear compared to primary IOL implantation. Since the cost of these supplies is not covered by most public or private health insurance plans in the United States, this is a significant obstacle for many children wearing contact lenses on a long-term basis. This is one of the reasons cited for considering primary IOL implantation during infancy despite the higher rate of adverse events and additional intraocular surgeries associated with IOL implantation in this age group.3 The high success rate of contact lens wear following congenital cataract surgery in countries with socialized health care systems suggests that cost is an important factor when treating children with aphakic contact lenses.15,18 The IATS provides further evidence that when the economic burden of contact lens use is removed from caregivers that excellent contact lens adherence can be achieved. It is the opinion of the authors that both public and private health insurance should cover the cost of aphakic contact lenses for children given their important role in the visual rehabilitation of these eyes after cataract surgery.
There are a number of potential limitations to the current analyses, and particularly the estimates of contact lens adherence. First, there may be substantial day-to-day variation in contact lens use. We attempted to minimize this concern by not having the caregiver informed, ahead of time, about the timing of the call, by averaging at least 3 adherence assessments and by having adherence interviews conducted on both weekdays and weekends. Second, caregivers may over-report their adherence to prescribed contact lens use. Further, the specific instrument that we used to assess adherence has not been externally validated. However, errors in the percentage of waking hours spent wearing contact lenses is unlikely to have a substantial impact on our findings, particularly since more than 50% of the children wore contact lenses on an extended wear basis. Additionally, by having the interviews completed by the same person each time, and by ensuring that the interview was not associated with clinical care, we attempted to minimize the risk of caregivers exaggerating contact lens use stemming from a social desirability bias. Although it would be preferable to have objective measures of contact lens adherence, at this point, no such devices are available. Furthermore, we have previously shown that reported adherence to prescribed occlusion therapy in this population is similar to that reported for similar populations using occlusion dose monitors.6 Finally, patching adherence may be a confounding variable for contact lens adherence since we have shown that they correlate closely with one another. A key concern, however, is that the provision of contact lenses to participants’ families may reduce financial barriers to contact lens use. Therefore, contact lens use in other contexts may not be as high as we report here.
Conclusions
In this study, we found that most caregivers were able to manage contact lens application and removal and to achieve high levels of adherence to full-time contact lens wear for their child. We also found that there was no significant effect of gender, private insurance as an indicator of socioeconomic status, or age at time of surgery on contact lens adherence.
Supplementary Material
Key Points.
Question
How successful is contact lens wear in children following unilateral cataract surgery during infancy if contact lenses are provided at no charge to caregivers?
Findings
We found that most families reported that their child wore a contact lens more than 80% of waking hours from the time of cataract extraction through age 5 years.
Meaning
These results suggest that excellent contact lens adherence can be consistently achieved by most caregivers of children with unilateral aphakia if the cost of contact lenses is eliminated as a barrier.
Acknowledgments
Funding/Support: Supported by National Institutes of Health Grants U10 EY13272, U10 EY013287, UG1 EY013272, 1UG1 EY025553, P30 EY026877 and Research to Prevent Blindness, Inc, New York, New York
Footnotes
Author Contributions: Dr Lambert had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: All authors
Acquisition, analysis or interpretation of data: All authors
Drafting of the manuscript: All authors
Conflicts of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Role of the Funder/Sponsor: The sponsors did not participate in the design of the study; analysis and interpretation of the data; preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Lambert SR, Buckley EG, Drews-Botsch C, et al. The infant aphakia treatment study: design and clinical measures at enrollment. Arch Ophthalmol. 2010;128(1):21–27. doi: 10.1001/archophthalmol.2009.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Infant Aphakia Treatment Study G. Lambert SR, Lynn MJ, et al. Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol. 2014;132(6):676–682. doi: 10.1001/jamaophthalmol.2014.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lambert SR, Buckley EG, Drews-Botsch C, et al. A randomized clinical trial comparing contact lens with intraocular lens correction of monocular aphakia during infancy: grating acuity and adverse events at age 1 year. Arch Ophthalmol. 2010;128(7):810–818. doi: 10.1001/archophthalmol.2010.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plager DA, Lynn MJ, Buckley EG, Wilson ME, Lambert SR. Infant Aphakia Treatment Study G. Complications in the First 5 Years Following Cataract Surgery in Infants With and Without Intraocular Lens Implantation in the Infant Aphakia Treatment Study. Am J Ophthalmol. 2014 doi: 10.1016/j.ajo.2014.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birch EE, Stager DR. Prevalence of good visual acuity following surgery for congenital unilateral cataract. Arch Ophthalmol. 1988;106(1):40–43. doi: 10.1001/archopht.1988.01060130046025. [DOI] [PubMed] [Google Scholar]
- 6.Drews-Botsch C, Cotsonis G, Celano M, Lambert SR. Assessment of Adherence to Visual Correction and Occlusion Therapy in the Infant Aphakia Treatment Study. Contemp Clin Trials Commun. 2016;3:158–166. doi: 10.1016/j.conctc.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Russell B, DuBois L, Lynn M, Ward MA, Lambert SR Infant Aphakia Treatment Study G. The Infant Aphakia Treatment Study Contact Lens Experience to Age 5 Years. Eye Contact Lens. 2017;43(6):352–357. doi: 10.1097/ICL.0000000000000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Russell B, Ward MA, Lynn M, Dubois L, Lambert SR. The infant aphakia treatment study contact lens experience: one-year outcomes. Eye Contact Lens. 2012;38(4):234–239. doi: 10.1097/ICL.0b013e3182562dc0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drews-Botsch C, Celano M, Cotsonis G, Hartmann EE, Lambert SR Infant Aphakia Treatment Study G. Association Between Occlusion Therapy and Optotype Visual Acuity in Children Using Data From the Infant Aphakia Treatment Study: A Secondary Analysis of a Randomized Clinical Trial. JAMA Ophthalmol. 2016;134(8):863–869. doi: 10.1001/jamaophthalmol.2016.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Autrata R, Rehurek J, Vodickova K. Visual results after primary intraocular lens implantation or contact lens correction for aphakia in the first year of age. Ophthalmologica. 2005;219(2):72–79. doi: 10.1159/000083264. [DOI] [PubMed] [Google Scholar]
- 11.Solebo AL, Russell-Eggitt I, Cumberland PM, Rahi JS British Isles Congenital Cataract Interest G. Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: the IoLunder2 cohort study. Br J Ophthalmol. 2015;99(11):1471–1476. doi: 10.1136/bjophthalmol-2014-306394. [DOI] [PubMed] [Google Scholar]
- 12.Hartmann EE, Lynn MJ, Lambert SR Infant Aphakia Treatment Study G. Baseline characteristics of the infant aphakia treatment study population: predicting recognition acuity at 4.5 years of age. Invest Ophthalmol Vis Sci. 2015;56(1):388–395. doi: 10.1167/iovs.14-15464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freedman SF, Lynn MJ, Beck AD, et al. Glaucoma-Related Adverse Events in the First 5 Years After Unilateral Cataract Removal in the Infant Aphakia Treatment Study. JAMA Ophthalmol. 2015;133(8):907–914. doi: 10.1001/jamaophthalmol.2015.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mittelviefhaus H, Mittelviefhaus K, Gerling J. Etiology of contact lens failure in pediatric aphakia. Indications for intraocular lenses? Ophthalmologe. 1998;95(4):207–212. doi: 10.1007/s003470050263. [DOI] [PubMed] [Google Scholar]
- 15.Loudot C, Jourdan F, Benso C, Denis D. Aphakia correction with rigid contact lenses in congenital cataract. J Fr Ophtalmol. 2012;35(8):599–605. doi: 10.1016/j.jfo.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Aasuri MK, Venkata N, Preetam P, Rao NT. Management of pediatric aphakia with silsoft contact lenses. CLAO J. 1999;25(4):209–212. [PubMed] [Google Scholar]
- 17.Kruger SJ, DuBois L, Becker ER, et al. Cost of intraocular lens versus contact lens treatment after unilateral congenital cataract surgery in the infant aphakia treatment study at age 5 years. Ophthalmology. 2015;122(2):288–292. doi: 10.1016/j.ophtha.2014.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amaya LG, Speedwell L, Taylor D. Contact lenses for infant aphakia. Br J Ophthalmol. 1990;74(3):150–154. doi: 10.1136/bjo.74.3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.