Abstract
Objective
Food frequency questionnaires (FFQs) are often used to estimate food and nutrient intakes to rank individuals by their level of intake. We evaluated the relative validity of a semi-quantitative FFQ created for use in Tanzania by comparing it to two 24-hour diet recalls.
Design
We measured relative validity of the FFQ with deattenuated energy-adjusted rank correlations for nutrients, deattenuated rank correlations for food groups, and performed a cross-classification analysis of energy-adjusted nutrient quartiles using percent agreement, and Bland-Altman analysis.
Setting
Interviews were conducted in 2014 in participants’ homes in Ukonga, Dar es Salaam, Tanzania.
Subjects
We surveyed 317 adults aged 40 years and older from the general public.
Results
Deattenuated energy-adjusted rank correlation coefficients of nutrients ranged from −0.03 for riboflavin to 0.41 for percent energy from carbohydrates with a median correlation of 0.21. Coefficients for food groups ranged from 0.00 for root vegetables to 0.51 for alcohol, with a median of 0.35. Relative to the average of the two 24-hour diet recalls, the FFQ overestimated energy intake and intake of all nutrients and food groups, other than tea, with ratios among nutrients ranging from 1.34 for saturated fatty acids to 7.08 for Vitamin A; and among food groups from 0.92 for tea to 9.00 for fruit. The percentage of participants classified in the same nutrient intake quartile ranged from 23% for saturated fatty acids to 32% for both niacin and pantothenic acid, with a median of 28%.
Conclusions
The FFQ performed moderately well in urban Tanzanian adults.
Keywords: food frequency questionnaire, validation, nutritional epidemiology, Tanzania, sub-Saharan Africa
Introduction
Non-communicable diseases (NCDs) are a growing concern in sub-Saharan Africa (SSA). In this region, the number of cardiovascular deaths has nearly doubled from 1990 to 2015(1), the prevalence of diabetes has more than doubled from 1980 to 2014(2), and the prevalence of hypertension and obesity are both increasing(3,4). In rural SSA, the proportion of adult deaths due to NCDs has increased: from 16% in 2003 to 24% in 2007 in Tanzania(5) and from 35% in 2003 to 45% in 2010 in Kenya(6)
One of the potentially modifiable risk factors for NCDs is diet, which is well-documented to affect the risk for many cardiometabolic diseases and cancers(7-10). In sub-Saharan Africa (SSA), although data remain sparse, it is clear that access to food is increasing, but diet quality is worsening. Data from the Food and Agricultural Organization of the United Nations (FAO) show that per capita caloric intake has increased over the past 30 years(11), snack food and soft drink importation to the 15 countries that make up the Southern African Development Community (SADC) has quadrupled over the past two decades(12), and overall dietary quality has worsened(13). Reflecting the consequences of the worsening dietary situation in SSA, the Global Burden of Disease (GBD) study estimates that the proportion of deaths attributable to unhealthy diet in Tanzania has increased from 5.8% in 1990 to 9.3% in 2015(14,15).
As the burden of NCDs in SSA continues to grow, more research is needed to discover the causes of this rising burden and help governments develop prevention policies. Well-designed public health policies could influence diet through such means as education to inform and change food preferences, healthy food production, food subsidization, and taxation(16–19). However, obtaining reliable information on dietary intake can be challenging because validated tools for quantifying diet in SSA are limited. Food frequency questionnaires (FFQs) are the standard tool used to estimate dietary intake for diet-disease analyses in large cohorts(20). Such questionnaires, which were developed in the 1980s, have been widely used by researchers in the United States and Europe. However, as the validity of food frequency questionnaires is sensitive to cultural and regional factors(20–22), FFQs need to be validated before being extended for use outside of the United States and Europe, such as in SSA where diets, availability of foods and dishes, portion sizes, numeracy, literacy, and customs differ from those in the U.S. and Europe(23,24). Within SSA, full-length FFQs intended to measure the entire diet have been validated for use in Mali, South Africa, and Botswana(25–29). However, diets differ between sub-Saharan African countries, and an FFQ has not yet been validated for use in Tanzania. A previous validation of a Tanzanian FFQ against two 24-hour diet recalls only provided correlation coefficients and p-values for six broad food groups (fruits, cereals, beverages, vegetables, animal products, and fats) based on data from 50 women(30). Here, we report the validity of estimated intakes of energy, 25 nutrients, and 13 food groups as assessed by our FFQ compared to two repeated 24-hour diet recalls among adults in Dar es Salaam, Tanzania.
Methods
Sampling design and participants
The Dar es Salaam Health and Demographic Surveillance System (HDSS) was initiated in 2011 and collected demographic data on all individuals living in Ukonga, a peri-urban ward of Dar es Salaam(31). For the Dar es Salaam Urban Cohort Hypertension Study (DUCS-HTN), we attempted to contact everyone registered in the HDSS, aged 40 years and older, from two randomly selected neighborhoods of the seven neighborhoods in the HDSS (n=4,896). Additional information on the DUCS-HTN study has been reported previously(32). We randomly selected 1,024 of these potential participants to contact for the DUCS-HTN dietary sub-study. We excluded participants who were pregnant or physically or mentally incapable of participating in the DUCS-HTN study. For inclusion in the analytical sample, we required that participants complete an FFQ and two 24-hour diet recalls, have less than 10% of their FFQ items missing, and that their daily caloric intake from the FFQ be within a plausible range of 500 to 5000 kcal.
The Institutional Review Board of the Harvard T.H. Chan School of Public Health and the Muhimbili University of Health and Allied Sciences Ethical Committee approved the study protocol. Written informed consent was obtained from all participants, or, if the participant was unable to sign, a witness signed on behalf of the participant.
Dietary assessments
Trained interviewers conducted face-to-face interviews and physical examinations in participants’ homes from March to June 2014. The six interviewers who conducted dietary questionnaires had experience in public health data collection, but not in collecting FFQs or 24-hour diet recalls. The interviewers, therefore, received one full day of training and written instructions on how to conduct the FFQ and 24-hour diet recall. A nutritionist and epidemiologists conducted the dietary data collection training. Interviewers had two days of field practice before commencing data collection, during which supervisors observed interviews and provided feedback to the interviewers in order to standardize the interview technique between the six interviewers. Interviewers administered the FFQ and the first 24-hour diet recall at the first study visit. All interviews and exams proceeded in the same order: lifestyle questionnaire, blood pressure measurements, FFQ, anthropometric measurements, 24-hour diet recall, capillary blood measurements, and finally provision of instructions for the 24-hour urine collection. A second 24-hour diet recall was repeated at the start of the next study visit, a minimum of three days later. The median [interquartile range (IQR)] number of days between the two 24-hour diet recalls was 6 [4, 15]. Eighty-four percent of participants completed both 24-hour diet recalls during the workweek, 15% completed one on the weekend and one during the week, and 2% completed both during the weekend.
Interviewers verbally administered the 24-hour diet recall to participants. To help standardize participants’ understanding of serving size, the interviewers showed participants plastic sample dishes as well as drawn images of portion sizes (see images in Supplement) for the 24-hour diet recalls and the FFQ.
Interviewers verbally administered the 179-food-item semi-quantitative FFQ with specified portion sizes and a recall period of 30 days. The FFQ was slightly modified, through the addition of food items, from the FFQ created by Lukmanji et al(33). Similar FFQs without published validation studies have previously been used in Tanzania(34). There were nine options for frequency of consumption, and servings per day were calculated from these frequencies as follows: never consumed over past thirty days (0 servings per day), 1-3 servings per month (0.067 servings per day), 1 serving per week (0.143 servings per day), 2-4 servings per week (0.429 servings per day), 5-6 servings per week (0.786 servings per day), 1 serving per day (1 serving per day), 2-3 servings per day (2.5 servings per day), 4-5 servings per day (4.5 servings per day), 6+ servings per day (6 servings per day). Participants selected one frequency of consumption for each of the 179 items in the FFQ. Portion sizes were provided for each food item (see FFQ in Supplement); however, participants were allowed to report that they consumed a portion of a serving size (e.g. ½ or ¼).
For both the 24-hour diet recall and FFQ data, nutrient information for individual foods was taken from the 2008 Tanzania Food Composition Tables(35). The food composition tables were primarily based on data from WorldFood Dietary Assessment System, with some information also taken from the Unites States Department of Agriculture (USDA) food composition database and the South Africa food composition tables. Chemical analysis of the nutrient composition of a small number of foods (mainly maize and some leafy greens) was conducted at Sokoine University of Agriculture. The Tanzanian Food Composition Tables includes nutrient composition of mixed dishes. The authors of the Tanzanian Food Composition Tables collected sample recipes from a variety of sources (e.g. street food vendors, student canteen, recipes books and websites). The nutrient composition of the recipes was then estimated from the nutrient composition of the individual ingredients. These tables provide information on the energy and nutrient content and grams per serving size of over 400 foods and dishes commonly consumed in Tanzania. Nutrient intakes for each individual included contributions from food but not supplements.
Statistical analysis
Descriptive statistics (means and standard deviations (SDs)) were calculated for energy, nutrient, and food group intakes as estimated by the FFQ and the average of the two 24-hour diet recalls. Foods were categorized into 13 groups (Supplement Table 1) for food group analyses. Nutrient intakes were adjusted for total energy intake using the residual method(36). We also adjusted for total energy intake when analyzing macronutrient intake by calculating macronutrient intake as a percent of total energy intake (i.e. the nutrient density method). Fats, carbohydrates, and protein were also separately adjusted for total energy intake using the nutrient density method.
Rank correlation coefficients and 95% confidence intervals were calculated to evaluate the strength of associations between nutrient and food group intakes derived from the FFQs versus the 24-hour diet recalls(37). To compare nutrient intake as measured by the two different dietary assessment methods, we calculated unadjusted, energy-adjusted, and deattenuated energy-adjusted correlation coefficients. To compare food group intake as measured by the two different dietary assessment methods, we calculated unadjusted and deattenuated correlation coefficients. Deattenuated correlations were used to adjust for random within-person variation across the 24-hour diet recalls(37). We also calculated intra-class correlations (ICCs) between nutrient and food group intake as measured by the FFQ and average of the two 24-hour diet recalls.
We also examined the ability of the two dietary questionnaires to categorize participants into the same energy-adjusted nutrient intake quartiles. The proportion of individuals that were classified correctly within the same quartile, within the same or adjacent quartile, and in opposite quartiles (lowest quartile according to one dietary questionnaire and highest quartile according to the other) was determined. Kappa statistics with linear weights were calculated to further quantify the agreement between energy-adjusted nutrient intake quartiles as measured by the FFQ and average of two 24-hour diet recalls(38,39).
We examined systematic differences in macronutrient intake as measured by the FFQ and 24-hour diet recalls by creating Bland-Altman plots of energy intake, percent energy from fat, percent energy from protein, and percent energy from carbohydrates(40). The plots were created by plotting the difference of nutrient intake from the two dietary intake measurement methods against the mean of the nutrient intake from the two dietary intake measurement methods. A relationship between the difference and the mean values indicates systematic bias (e.g. the FFQ tends to overestimate nutrient intake more for those with higher total energy intakes). Limits of agreement (mean(nutrientFFQ − nutrient24hDR) ± 1.96*SD(nutrientFFQ − nutrient24hDR)) were calculated and plotted.
Analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, North Carolina, USA). Figures were created using R 2.15.3(41).
Results
Among the 1,024 participants that we attempted to contact for the DUCS-HTN dietary sub-study, 265 were not home after 3 contact attempts, 239 had outmigrated, 42 had died, 15 were mentally or physically incapable of participating, 36 refused to participate, and 2 were pregnant (Figure 1), resulting in a sample of 415 participants. Of these individuals, 414 completed the FFQ and 357 also completed the two 24-hour diet recalls. None of the FFQs had missing data on more than 10% of FFQ food items. We excluded one participant who, according to the FFQ, consumed <500 calories per day, as well as 39 participants who consumed more than 5,000 calories per day, which led to an analytical sample of 317 participants. Among these, the median [IQR] age was 52 [45, 60] years, 61% of participants were female, 65% were overweight or obese, and 75% had less than secondary education (Table 1).
Figure 1.
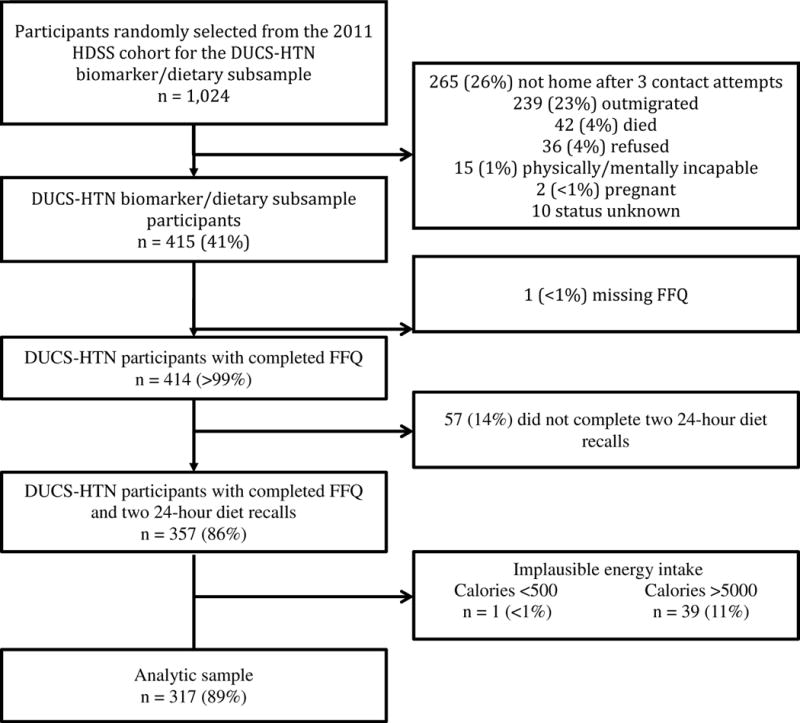
Flowchart of study participation and data completeness in the Dar es Salaam Urban Cohort Hypertension Study (DUCS-HTN), 2014
Table 1.
Basic characteristics of Dar es Salaam Urban Cohort Hypertension Study (DUCS-HTN) participants, 2014 (n=317)
| Characteristic | Median [IQR] or % |
|---|---|
| Age, years | 52 [45, 60] |
| 40-44 | 21% |
| 45-49 | 21% |
| 50-54 | 20% |
| 55-59 | 12% |
| 60-64 | 11% |
| 65-69 | 7% |
| ≥ 70 | 9% |
| Male | 39% |
| Religion | |
| Muslim | 51% |
| Christian | 49% |
| Education | |
| None | 12% |
| At least some primary | 64% |
| At least some secondary | 25% |
| BMI, kg/m2 | 27.2 [23.0, 31.8] |
| Underweight (<18.5) | 6% |
| Normal weight (18.5-<25) | 29% |
| Overweight (25-<30) | 31% |
| Obese (≥30) | 34% |
The intra-class correlations of the FFQ and average of the two 24-hour diet recalls for nutrients ranged from 0.09 for Vitamin A to 0.38 for total energy and for food groups it ranged from 0.12 for vegetables (excluding roots) to 0.58 for tea. The mean daily energy, nutrient, and food intakes estimated by the FFQ were higher than those estimated by the average of the two 24-hour diet recalls (Table 2). This was true for all nutrients and all foods, other than tea. Total energy intake as estimated by the FFQ was 1.68 times that estimated by the average of the two 24-hour diet recalls: mean (standard deviation) total energy intake was 2599 (1030) kcal according to the FFQ and 1546 (431) kcal according to the average of the two 24-hour diet recalls. The ratio of nutrient intake comparing FFQ estimates to 24-hour diet recall estimates ranged from 1.34 for saturated fatty acids to 7.08 for Vitamin A. Among food groups, the ratio of consumption comparing FFQ estimates to 24-hour diet recall estimates ranged from 0.92 for tea to 9.00 for fruits.
Table 2.
Daily food and nutrient intake estimated by food frequency questionnaire (FFQ) and two 24-hour diet recalls in the Dar es Salaam Urban Cohort Hypertension Study (DUCS-HTN), 2014 (n=317)
| Item (units/day) | FFQ | 24-hour diet recall average |
|---|---|---|
|
| ||
| Energy and nutrients | Mean (SD) | Mean (SD) |
| Energy (kcal) | 2599 (1030) | 1546 (431) |
|
| ||
| Macronutrients | ||
|
| ||
| Carbohydrate (g) | 361 (145) | 237 (65) |
| Carbohydrate (% energy) | 67% (8%) | 73% (7%) |
| Protein (g) | 94 (50) | 38 (15) |
| Protein (% energy) | 17% (5%) | 11% (4%) |
| Fat (g) | 91 (42) | 52 (22) |
| Fat (% energy) | 17% (4%) | 16% (5%) |
| Saturated fatty acids (g) | 50 (25) | 36 (17) |
| Monounsaturated fatty acids (g) | 23 (11) | 8 (4) |
| Polyunsaturated fatty acids (g) | 12 (9) | 4 (3) |
| Cholesterol (mg) | 185 (124) | 51 (46) |
|
| ||
| Vitamins | ||
|
| ||
| Vitamin A (μg RAE) | 1762 (1461) | 249 (394) |
| Niacin (mg) | 18 (9) | 8 (3) |
| Pantothenic Acid (mg) | 6 (3) | 3 (1) |
| Thiamin (mg) | 2 (2) | 0.8 (0.3) |
| Riboflavin (mg) | 3 (2) | 0.9 (1.1) |
| Vitamin B6 (mg) | 2 (1) | 0.9 (0.4) |
| Vitamin B12 (μg) | 6 (7) | 2.0 (2.7) |
| Folate (μg) | 471 (229) | 136 (65) |
| Vitamin C (mg) | 163 (104) | 39 (37) |
| Vitamin D (μg) | 6 (6) | 1.5 (2.9) |
| Vitamin E (μg) | 10 (6) | 2.4 (1.7) |
|
| ||
| Minerals | ||
|
| ||
| Calcium (mg) | 604 (508) | 283 (282) |
| Phosphorous (mg) | 1271 (678) | 677 (262) |
| Iron (mg) | 19 (16) | 7 (5) |
| Magnesium (mg) | 546 (361) | 230 (104) |
| Sodium (mg) | 957 (540) | 377 (224) |
| Potassium (mg) | 3800 (1806) | 1271 (513) |
| Zinc (mg) | 9 (5) | 5 (2) |
|
| ||
| Foods groups (servings) | ||
|
| ||
| Cereals | 5.0 (1.9) | 2.7 (0.9) |
| Legumes & nuts | 0.8 (0.8) | 0.5 (0.6) |
| Root vegetables | 0.6 (0.8) | 0.4 (0.5) |
| Vegetables (excluding roots) | 3.8 (2.7) | 0.7 (0.7) |
| Fruit | 1.8 (1.3) | 0.2 (0.4) |
| Unprocessed red meat | 0.6 (0.5) | 0.4 (0.5) |
| Fish | 0.9 (0.7) | 0.5 (0.5) |
| Chicken | 0.2 (0.3) | 0.1 (0.3) |
| Eggs | 0.2 (0.2) | 0.0 (0.1) |
| Dairy | 0.6 (0.7) | 0.1 (0.3) |
| Sugar-sweetened beverages | 0.2 (0.4) | 0.1 (0.2) |
| Alcohol | 0.2 (0.7) | 0.1 (0.2) |
| Tea | 1.2 (0.7) | 1.3 (0.7) |
Energy-adjustment tended to reduce correlations and deattenuation tended to increase correlations (Table 3). The median deattenuated energy-adjusted correlation for nutrients was 0.21 and ranged from −0.03 for riboflavin to 0.41 for percent energy from carbohydrates. Macronutrients when measured as percent of total energy intake (i.e. the nutrient density method) had higher correlations than did macronutrients adjusted for energy using the residual method: 0.41 versus 0.25 for carbohydrates, 0.40 versus 0.22 for protein, and 0.36 versus 0.15 for fat. The median deattenuated correlation for food groups was 0.35 and ranged from 0.00 for root vegetables to 0.51 for alcohol.
Table 3.
Correlations and intraclass correlations of daily intake of nutrients and food groups as assessed with two 24-hour diet recall and one food-frequency questionnaire in the Dar es Salaam Urban Cohort Hypertension Study (DUCS-HTN), 2014 (n=317)
| Rosner rank correlation(37) |
ICCb | |||
|---|---|---|---|---|
| Item | Unadjusted (95% CI) |
Energy-adjusteda (95% CI) |
Deattenuateda (95% CI) |
|
| Energy and nutrients | ||||
|
| ||||
| Energy (kcal) | 0.12 (0.02, 0.22) | – | 0.16 (0.02, 0.30) | 0.38 |
|
| ||||
| Nutrients (median) | 0.15 | 0.12 | 0.21 | 0.21 |
| Macronutrients (median) | 0.22 | 0.16 | 0.26 | 0.20 |
|
| ||||
| Carbohydrate (g) | 0.07 (−0.04, 0.17) | 0.16 (0.06, 0.26) | 0.25 (0.09, 0.40) | 0.26 |
| Carbohydrate (% energy) | 0.23 (0.12, 0.32) | – | 0.41 (0.24, 0.55) | 0.18 |
| Protein (g) | 0.20 (0.10, 0.30) | 0.11 (0.01, 0.22) | 0.22 (0.03, 0.39) | 0.18 |
| Protein (% energy) | 0.22 (0.12, 0.32 | – | 0.40 (0.24, 0.54) | 0.18 |
| Fat (g) | 0.21 (0.10, 0.31) | 0.09 (−0.02, 0.19) | 0.15 (−0.03, 0.33) | 0.20 |
| Fat (% energy) | 0.22 (0.12, 0.32) | – | 0.36 (0.19, 0.51) | 0.16 |
| Saturated fatty acids (g) | 0.18 (0.08, 0.28) | 0.04 (−0.07, 0.14) | 0.06 (−0.12, 0.24) | 0.20 |
| Monounsaturated fatty acids (g) | 0.24 (0.13, 0.33) | 0.26 (0.16, 0.36) | 0.40 (0.25, 0.53) | 0.26 |
| Polyunsaturated fatty acids (g) | 0.15 (0.04, 0.25) | 0.17 (0.06, 0.27) | 0.26 (0.10, 0.41) | 0.26 |
| Cholesterol (mg) | 0.26 (0.16, 0.36) | 0.17 (0.06, 0.27) | 0.26 (0.10, 0.41) | 0.26 |
|
| ||||
| Vitamins (median) | 0.11 | 0.12 | 0.19 | 0.25 |
|
| ||||
| Vitamin A (μg RAE) | 0.09 (−0.01, 0.20) | 0.05 (−0.06, 0.15) | 0.11 (−0.14, 0.35) | 0.09 |
| Niacin (mg) | 0.14 (0.04, 0.24) | 0.14 (0.03, 0.24) | 0.25 (0.06, 0.42) | 0.18 |
| Pantothenic Acid (mg) | 0.13 (0.03, 0.23) | 0.19 (0.09, 0.29) | 0.26 (0.12, 0.39) | 0.36 |
| Thiamin (mg) | −0.04 (−0.15, 0.06) | 0.15 (0.05, 0.25) | 0.24 (0.08, 0.39) | 0.26 |
| Riboflavin (mg) | 0.16 (0.05, 0.26) | −0.02 (−0.12, 0.09) | −0.03 (−0.19, 0.14) | 0.25 |
| Vitamin B6 (mg) | 0.10 (−0.00, 0.21) | 0.13 (0.02, 0.23) | 0.19 (0.03, 0.33) | 0.29 |
| Vitamin B12 (μg) | 0.15 (0.04, 0.25) | 0.08 (−0.02, 0.19) | 0.14 (−0.04, 0.31) | 0.21 |
| Folate (μg) | 0.00 (−0.10, 0.11) | 0.08 (−0.03, 0.18) | 0.12 (−0.04, 0.28) | 0.25 |
| Vitamin C (mg) | 0.11 (0.01, 0.22) | 0.12 (0.01, 0.22) | 0.19 (0.02, 0.34) | 0.25 |
| Vitamin D (μg) | 0.12 (0.01, 0.22) | 0.02 (−0.09, 0.12) | 0.03 (−0.16, 0.22) | 0.18 |
| Vitamin E (μg) | 0.02 (−0.08, 0.13) | 0.12 (0.01, 0.22) | 0.21 (0.03, 0.37) | 0.20 |
|
| ||||
| Minerals (median) | 0.09 | 0.15 | 0.26 | 0.23 |
|
| ||||
| Calcium (mg) | 0.10 (−0.01, 0.20) | 0.15 (0.05, 0.26) | 0.26 (0.09, 0.42) | 0.22 |
| Iron (mg) | 0.04 (−0.06, 0.15) | 0.18 (0.07, 0.28) | 0.27 (0.12, 0.42) | 0.26 |
| Magnesium (mg) | 0.05 (−0.06, 0.15) | 0.16 (0.06, 0.27) | 0.26 (0.10, 0.40) | 0.26 |
| Sodium (mg) | 0.20 (0.10, 0.30) | 0.16 (0.06, 0.26) | 0.25 (0.09, 0.40) | 0.27 |
| Phosphorous (mg) | 0.09 (−0.01, 0.20) | 0.14 (0.04, 0.24) | 0.26 (0.08, 0.43) | 0.17 |
| Potassium (mg) | 0.09 (−0.02, 0.19) | 0.15 (0.05, 0.25) | 0.25 (0.08, 0.41) | 0.23 |
| Zinc (mg) | 0.11 (0.01, 0.21) | 0.12 (0.02, 0.22) | 0.22 (0.04, 0.40) | 0.17 |
|
| ||||
| Food groups (median) | 0.21 | – | 0.35 | 0.25 |
|
| ||||
| Cereals | 0.21 (0.11, 0.31) | – | 0.29 (0.15, 0.42) | 0.34 |
| Legumes & nuts | 0.01 (−0.09, 0.12) | – | 0.02 (−0.17, 0.21) | 0.18 |
| Root vegetables | 0.00 (−0.11, 0.11) | – | 0.00 (−0.16, 0.16) | 0.25 |
| Vegetables (excluding roots) | 0.01 (−0.09, 0.12) | – | 0.02 (−0.20, 0.25) | 0.12 |
| Fruit | 0.11 (0.01, 0.21) | – | 0.16 (0.01, 0.32) | 0.28 |
| Unprocessed red meat | 0.23 (0.13, 0.33) | – | 0.47 (0.33, 0.59) | 0.15 |
| Fish | 0.08 (−0.02, 0.19) | – | 0.18 (−0.03, 0.38) | 0.13 |
| Chicken | 0.22 (0.12, 0.32) | – | 0.38 (0.22, 0.52) | 0.20 |
| Eggs | 0.20 (0.10, 0.30) | – | 0.40 (0.23, 0.54) | 0.15 |
| Dairy | 0.25 (0.14, 0.34) | – | 0.35 (0.21, 0.48) | 0.32 |
| Sugar-sweetened beverages | 0.25 (0.15, 0.35) | – | 0.37 (0.22, 0.50) | 0.29 |
| Alcohol | 0.42 (0.33, 0.51) | – | 0.51 (0.40, 0.60) | 0.55 |
| Tea | 0.35 (0.26, 0.44) | – | 0.41 (0.30, 0.51) | 0.58 |
Nutrient intakes, but not food group intakes, were adjusted for total energy intake by the residual method
ICCs for residual method energy-adjusted nutrients except for energy and “percent calorie” variables.
Cross-classification analyses of estimated nutrient intake found low to moderate agreement (Table 4). The median proportion classified within the same quartile was 29%, which is higher than the 25% that is expected due to chance alone. The proportion correctly classified within the same quartile ranged from 23% for saturated fatty acid to 32% for niacin and pantothenic acid. The proportion classified within the same or adjacent quartiles ranged from 60% for riboflavin to 72% for monounsaturated fatty acids. The proportion classified into opposite quartiles (Q1 according to one questionnaire and Q4 according the other) ranged from 7% for percent energy from protein to 13% for total energy, cholesterol, vitamin A, and riboflavin. The median proportion classified into opposite quartiles was 10%, which is the same as what would be expected by chance. Weighted kappas ranged from −0.03 for riboflavin to 0.14 for niacin and pantothenic acid.
Table 4.
Cross-classification of energy-adjusted daily intake of food group and food quartiles as assessed with average of two 24-hour diet recall and one food-frequency questionnaire in the Dar es Salaam Urban Cohort Hypertension Study (DUCS-HTN), 2014 (n=32017)
| Correctly classified | Same or adjacent quartile | Opposite quartiles (Q1 and Q4) | Weighted kappa | |
|---|---|---|---|---|
| Expected if randomly distributed | 25% | 63% | 13% | 0.00 |
|
| ||||
| Energy and nutrients | ||||
|
| ||||
| Energy (kcal) | 28% | 68% | 13% | 0.08 |
|
| ||||
| Macronutrients | ||||
|
| ||||
| Carbohydrate (g) | 28% | 65% | 11% | 0.05 |
| Carbohydrate (% energy) | 29% | 66% | 9% | 0.09 |
| Protein (g) | 28% | 66% | 8% | 0.09 |
| Protein (% energy) | 31% | 64% | 7% | 0.11 |
| Fat (g) | 26% | 64% | 11% | 0.03 |
| Fat (% energy) | 29% | 66% | 11% | 0.08 |
| Saturated fatty acids (g) | 23% | 60% | 11% | −0.02 |
| Monounsaturated fatty acids (g) | 25% | 72% | 9% | 0.10 |
| Polyunsaturated fatty acids (g) | 29% | 69% | 10% | 0.10 |
| Cholesterol (mg) | 26% | 66% | 13% | 0.04 |
|
| ||||
| Vitamins | ||||
|
| ||||
| Vitamin A (μg RAE) | 27% | 64% | 13% | 0.02 |
| Niacin (mg) | 32% | 69% | 9% | 0.14 |
| Pantothenic Acid (mg) | 32% | 69% | 8% | 0.14 |
| Thiamin (mg) | 29% | 66% | 9% | 0.09 |
| Riboflavin (mg) | 26% | 60% | 13% | −0.03 |
| Vitamin B6 (mg) | 29% | 69% | 9% | 0.11 |
| Vitamin B12 (μg) | 29% | 68% | 10% | 0.10 |
| Folate (μg) | 30% | 66% | 11% | 0.08 |
| Vitamin C (mg) | 25% | 64% | 9% | 0.04 |
| Vitamin D (μg) | 24% | 62% | 11% | 0.01 |
| Vitamin E (μg) | 30% | 64% | 12% | 0.06 |
|
| ||||
| Minerals | ||||
|
| ||||
| Calcium (mg) | 31% | 68% | 9% | 0.12 |
| Iron (mg) | 31% | 68% | 10% | 0.11 |
| Magnesium (mg) | 31% | 68% | 12% | 0.09 |
| Sodium (mg) | 31% | 70% | 10% | 0.13 |
| Phosphorous (mg) | 29% | 69% | 11% | 0.10 |
| Potassium (mg) | 26% | 65% | 10% | 0.05 |
| Zinc (mg) | 26% | 65% | 10% | 0.05 |
| Median | 28% | 66% | 10% | 0.07 |
Bland-Altman plots of energy and percent energy from the three major macronutrients show moderate agreement (Figure 2). The plots also show potential systemic bias in energy intake because the difference between energy intake by FFQ and 24-hour diet recalls is larger among participants with higher mean reported energy intake. However, systematic bias was not seen in percent energy from fat, protein, or carbohydrates. Ranges for limits of agreement were relatively wide, which indicates that there was wide variability in how the FFQ measured macronutrient intake relative to the average of the two 24-hour diet recalls.
Figure 2.
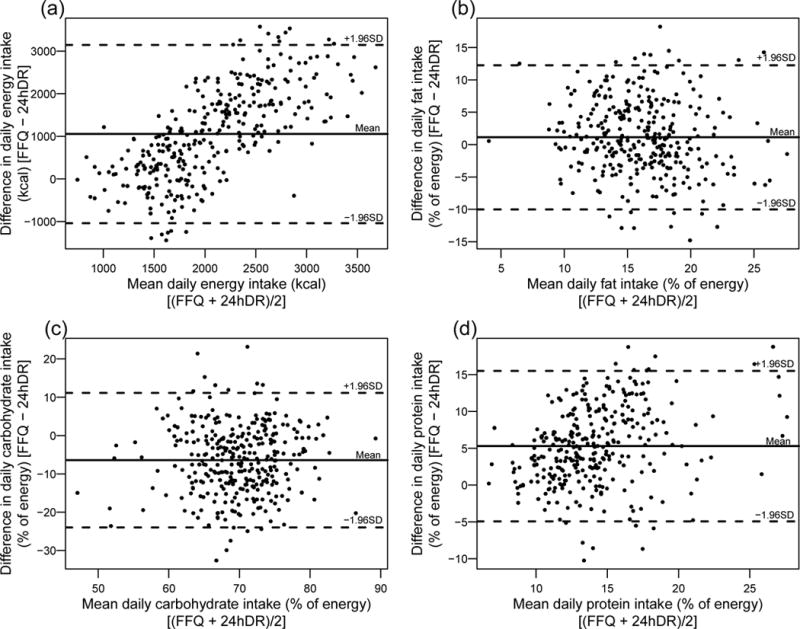
Bland-Altman plots to assess agreement between the FFQ and averaged 24-hour diet recalls for (a) energy, (b) fat (% of energy), (c) carbohydrates (% of energy), and (d) protein (% of energy) in the Dar es Salaam Urban Cohort Hypertension Study (DUCS-HTN), 2014 (n=317)
Discussion
Our results indicate a moderate validity of the Tanzanian FFQ when compared to two 24-hour diet recalls in an urban adult population in Dar es Salaam. As has been observed in previous validation studies, we found that the FFQ generally overestimated intake relative to the 24-hour diet recalls(25,29,42–45) and deattenuation tended to increase estimated correlation coefficients(46). Coefficients comparing estimated nutrient intakes from the FFQ and two 24-hour diet recalls were low to moderate. We found that the FFQ performed best for macronutrients when quantified as a percent of energy intake, but less well for nutrients adjusted for energy intake using the residual method. The FFQ appeared to be a better measure of macronutrients and minerals than vitamins. This may be because vitamin intake tends to vary greatly from day to day (as many vitamins are only found in a small selection of foods), whereas macronutrient intake remains relatively constant.
The validity of the FFQ to measure food group intake was also moderate. However, we found that the FFQ has poor validity for measuring legume and nut intake, and vegetable (both root vegetables and other vegetables) intake. The poor validity of the FFQ for these food groups may be due to the difficulty of quantifying the intake of foods that tend to be a component of a dish, such as vegetables added to stews. This can be particularly challenging in Tanzania, where vegetables are often consumed in mixed dishes along with many other vegetables, and possibly meat or fish, rather than independently. Tanzanian meals are often composed of a starch (i.e. rice or stiff porridge (called ugali in Swahili)) and a stew, making it difficult for individuals to assess the quantity of each component of the food. An additional challenge in Tanzania and elsewhere in SSA is that food is often consumed communally, from a shared household dish rather than from individual plates, which complicates estimating portion size, as well as portion content. To account for this, we included “handful” (ujazo wa kiganja cha mkono in Swahili) as a serving size option in the FFQ.
Previous FFQ validation studies have similarly found that correlations tend to be lower for vegetables than other food groups(22,25,45,47–49). A cross-check question on the daily number of servings of vegetable could be added to future versions of the FFQ to help correct for over-reporting of vegetable intake(22).
Our results are similar to those from previous FFQ validations that have been conducted in SSA. We identified four full-length FFQs that have been validated for use in sub-Saharan African populations: a 164-item quantitative FFQ with a recall period of 7-days was validated against 2-day weighed food records using data from 70 participants in Mali, a 122-item FFQ was validated against four 24-hour diet recalls using data from 79 participants in Botswana, a 145-item FFQ was validated against a 7-day weighed food record using data from 74 participants in South Africa, and a quantitative FFQ was validated against two 24-hour diet recalls using data from 50 women in Tanzania (information was not provided on number of food-items)(25,27,29,30). We found a median correlation of 0.35 for food groups, which is comparable to median correlations of 0.28, 0.38, and 0.37 that were found in Mali, Botswana, and SA, respectively. Our food group correlations ranged from 0.00 to 0.51, compared to correlations ranging from −0.04 to 0.56, 0.18 to 0.58, and 0.14 to 0.56 in Mali, Botswana, and SA, respectively.
For most nutrients and food groups that we examined, we found relatively similar population-level intakes to what has been found by other researchers in Tanzania. Lukmanji et al. found a similar distribution of macronutrient intake in a study of pregnant women with HIV in Dar es Salaam(33). A global study estimated that sugar-sweetened beverage intake in Tanzanians aged 40 years and older ranged from 0.16 to 0.32 servings per day, depending on age and sex(50). This is similar in range to our findings of 0.2 servings per day, according to the FFQ, and 0.1 servings per day, according to the 24-hour diet recalls. However, we also observed some intake values that differed considerably from previous studies. For example, a global study estimated that, on average, Tanzanians consume 2.75 (95% CI: 2.45 – 3.08) grams of sodium per day,(51) which is more than double the intakes of 0.96 grams per day estimated from our FFQ and 0.38 grams per day estimated from our 24-hour diet recalls.
Our study had several limitations. We used two 24-hour diet recalls as our reference method instead of several weighed food records. Our 24-hour diet recalls may have underestimated dietary intake due to multiple factors including under-reporting due to recall bias (e.g forgot to report snacks or small food items) and under-representativeness of weekend diet (which is often larger than weekday diet). Other studies have found that participants incorrectly report portion sizes on 24-hour diet recalls(52) and a meta-analysis of FFQ validation studies found that correlations of nutrient intake were lower for FFQs validated against 24-hour diet recalls rather than food records(53). However, weighed food records may affect participants’ behavior and it is not possible to conduct food records in populations that have low literacy levels such as ours, unless an interviewer observes and records every meal, as was done for the FFQ validation in Mali(25). A meta-analysis of FFQ validation studies also found that nutrient correlations were lower when the reference method of dietary questionnaire was conducted fewer than 8 times(53). We conducted two 24-hour diet recalls per participant due to financial and logistic constraints. Further factors that may have lowered the agreement and correlation between our FFQ and the reference method were the limited training received by the study interviewers in how to conduct dietary questionnaires (i.e. one full-day session and two days of field tests) and questionnaire fatigue, for both participants and interviewers, due to the lengthy questionnaires conducted prior to the dietary questionnaires. The non-dietary DUCS-HTN questionnaire and measurements took approximately one hour to complete and each dietary questionnaire took 30-45 minutes to complete.
Our FFQ queried participants about many individual foods. A future study could include questions on frequency of consumption of food groups in addition to questions on individual food items. This may help quantify whether asking about individual foods overestimates the food group consumption. It is possible that an FFQ that focused on the most common mixed dishes and amount and types of sauces added to dishes, rather than asking mainly about individual food items might improve dietary assessment in this population.
In summary, our results indicate moderate agreement between the FFQ and two 24-hour diet recalls for use in urban Tanzania. Our results could be used to inform the creation and implementation of improved dietary questionnaires for use in SSA. Future FFQ validation studies may wish to examine the effect of intensity of interviewer training on FFQ validation quality. In addition, future studies might conduct FFQ validations using more than two 24-hour diet recalls spaced out over a longer period of time as the reference method.
Supplementary Material
Acknowledgments
We would like to thank Dr. Ramadhani Abdallah Noor for his feedback on the FFQ and Stella Lawrence for her help in training interviewers on conducting dietary questionnaires. We would also like to acknowledge participants who generously gave their time and invited interviewers to their homes. This project would not have been possible without the hard work of many interviewers, data entry clerks, administrative staff, and drivers. Their enthusiasm and hospitality made this project possible and a pleasure to work on.
Financial Support: This work was supported by a pilot grant through the Center for the Global Demography of Aging. RMZ was supported by an NIH T32 training-grant (CA 09001).
Abbreviations
- FFQ
food frequency questionnaire
- NCDs
Non-communicable diseases
- SSA
sub-Saharan Africa
- FAO
Food and Agricultural Organization of the United Nations
- SADC
Southern African Development Community
- GBD
global burden of disease
- HDSS
Dar es Salaam Health and Demographic Surveillance System
- DUCS-HTN
Dar es Salaam Urban Cohort Hypertension Study
- IQR
interquartile range
- SD
standard deviation
- CI
confidence interval
Footnotes
Conflict of Interest
None.
Authorship
RMZ, GD, and JK designed the study; KI, RMZ, GD, PK and JK led the fieldwork and data collection; RMZ, conducted the analysis with input from all co-authors; RMZ wrote the first draft of the manuscript and all co-authors provided comments and input; GD had primary responsibility for final content. All authors read and approved the final manuscript.
References
- 1.Mensah GA, Roth GA, Sampson UKA, Moran AE, Feigin VL, Forouzanfar MH, Naghavi M, Murray CJL, GBD 2013 Mortality and Causes of Death Collaborators Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015;26:S6–10. doi: 10.5830/CVJA-2015-036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet Lond Engl. 2016;387:1513–30. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NCD Risk Factor Collaboration (NCD-RisC) Di Cesare M, Bentham J, Stevens GA, Zhou B, Danaei G, Lu Y, Bixby H, Cowan MJ, Riley LM, et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 192 million participants. Lancet Lond Engl. 2016;387:1377–96. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, Farzadfar F, Stevens GA, Lim SS, Riley LM, et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5 4 million participants. Lancet. 2011;377:568–77. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 5.Narh-Bana SA, Chirwa TF, Mwanyangala MA, Nathan R. Adult deaths and the future: a cause-specific analysis of adult deaths from a longitudinal study in rural Tanzania 2003-2007. Trop Med Int Health. 2012;17:1396–404. doi: 10.1111/j.1365-3156.2012.03080.x. [DOI] [PubMed] [Google Scholar]
- 6.Phillips-Howard PA, Laserson KF, Amek N, Beynon CM, Angell SY, Khagayi S, Byass P, Hamel MJ, van Eijk AM, Zielinski-Gutierrez E, et al. Deaths ascribed to non-communicable diseases among rural Kenyan adults are proportionately increasing: evidence from a health and demographic surveillance system, 2003-2010. PloS One. 2014;9:e114010. doi: 10.1371/journal.pone.0114010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reedy J, Krebs-Smith SM, Miller PE, Liese AD, Kahle LL, Park Y, Subar AF. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144:881–9. doi: 10.3945/jn.113.189407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liese AD, Krebs-Smith SM, Subar AF, George SM, Harmon BE, Neuhouser ML, Boushey CJ, Schap TE, Reedy J. The Dietary Patterns Methods Project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145:393–402. doi: 10.3945/jn.114.205336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115:780–800.e5. doi: 10.1016/j.jand.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, Willett WC, Rimm EB, Hu FB. Changes in Diet Quality Scores and Risk of Cardiovascular Disease Among US Men and Women. Circulation. 2015;132:2212–9. doi: 10.1161/CIRCULATIONAHA.115.017158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steyn NP, McHiza ZJ. Obesity and the nutrition transition in Sub-Saharan Africa. Ann N Y Acad Sci. 2014;1311:88–101. doi: 10.1111/nyas.12433. [DOI] [PubMed] [Google Scholar]
- 12.Thow AM, Sanders D, Drury E, Puoane T, Chowdhury SN, Tsolokile L, Negin J. Regional trade and the nutrition transition: opportunities to strengthen NCD prevention policy in the Southern African Development Community. Glob Health Action [Internet] 2015 doi: 10.3402/gha.v8.28338. [cited 2016 Oct13];8. Available from: http://www.globalhealthaction.net/index.php/gha/artide/view/28338. [DOI] [PMC free article] [PubMed]
- 13.Imamura F, Micha R, Khatibzadeh S, Fahimi S, Shi P, Powles J, Mozaffarian D, Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE) Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob Health. 2015;3:e132–142. doi: 10.1016/S2214-109X(14)70381-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Institute for Health Metrics and Evaluation (IHME) GBD Compare | IHME Viz Hub [Internet] 2015 [cited 2017 Feb 17]. Available from: http://vizhub.healthdata.org/gbd-compare.
- 15.Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2015;386:2287–323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rees K, Dyakova M, Wilson N, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev. 2013:CD002128. doi: 10.1002/14651858.CD002128.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hooper L, Summerbell CD, Thompson R, Sills D, Roberts FG, Moore HJ, Smith GD. Reduced or modified dietary fat for preventing cardiovascular disease. São Paulo Med J Rev Paul Med. 2016;134:182–3. doi: 10.1590/1516-3180.20161342T1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hooper L, Martin N, Abdelhamid A, Davey Smith G. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2015:CD011737. doi: 10.1002/14651858.CD011737. [DOI] [PubMed] [Google Scholar]
- 19.Afshin A, Penalvo J, Del Gobbo L, Kashaf M, Micha R, Morrish K, Pearson-Stuttard J, Rehm C, Shangguan S, Smith JD, et al. CVD Prevention Through Policy: a Review of Mass Media, Food/Menu Labeling, Taxation/Subsidies, Built Environment, School Procurement, Worksite Wellness, and Marketing Standards to Improve Diet. Curr Cardiol Rep. 2015;17:98. doi: 10.1007/s11886-015-0658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Willett W. Nutritional Epidemiology. 3rd. New York: Oxford University Press; 2013. [Google Scholar]
- 21.Saloheimo T, Gonzâlez SA, Erkkola M, Milauskas DM, Meisel JD, Champagne CM, Tudor-Locke C, Sarmiento O, Katzmarzyk PT, Fogelholm M. The reliability and validity of a short food frequency questionnaire among 9-11-year olds: a multinational study on three middle-income and high-income countries. Int J Obes Suppl. 2015;5:S22–28. doi: 10.1038/ijosup.2015.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cade J, Thompson R, Burley V, et al. Development, validation and utilisation of food-frequency questionnaires – a review. Public Health Nutr. 2002;5:567–587. doi: 10.1079/PHN2001318. [DOI] [PubMed] [Google Scholar]
- 23.Gibson R, Knight A, Asante M, Thomas J, Goff LM. Comparing dietary macronutrient composition and food sources between native and diasporic Ghanaian adults. Food Nutr Res. 2015;59:27790. doi: 10.3402/fnr.v59.27790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mattei J, Malik V, Wedick NM, Hu FB, Spiegelman D, Willett WC, Campos H, Global Nutrition Epidemiologic Transition Initiative Reducing the global burden of type 2 diabetes by improving the quality of staple foods: The Global Nutrition and Epidemiologic Transition Initiative. Glob Health. 2015;11:23. doi: 10.1186/s12992-015-0109-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parr CL, Barikmo I, Torheim LE, Ouattara F, Kaloga A, Oshaug A. Validation of the second version of a quantitative food-frequency questionnaire for use in Western Mali. Public Health Nutr. 2002;5:769–81. doi: 10.1079/PHN2002357. [DOI] [PubMed] [Google Scholar]
- 26.Torheim LE, Barikmo I, Hatl0y A, Diakité M, Solvoll K, Diarra MM, Oshaug A. Validation of a quantitative food-frequency questionnaire for use in Western Mali. Public Health Nutr. 2001;4:1267–77. doi: 10.1079/phn2001181. [DOI] [PubMed] [Google Scholar]
- 27.MacIntyre UE, Venter CS, Vorster HH. A culture-sensitive quantitative food frequency questionnaire used in an African population: 2. Relative validation by 7-day weighted records and biomarkers. Public Health Nutr. 2001;4:63–71. doi: 10.1079/phn200041. [DOI] [PubMed] [Google Scholar]
- 28.MacIntyre UE, Venter CS, Vorster HH, Steyn HS. A combination of statistical methods for the analysis of the relative validation data of the quantitative food frequency questionnaire used in the THUSA study. Transition, Health and Urbanisation in South Africa. Public Health Nutr. 2001;4:45–51. doi: 10.1079/phn200039. [DOI] [PubMed] [Google Scholar]
- 29.Jackson MD, Motswagole BS, Kwape LD, et al. Validation and reproducibility of an FFQ for use among adults in Botswana. Public Health Nutr. 2013;16:1995–2004. doi: 10.1017/S1368980012004636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jordan I, Hebestreit A, Swai B, Krawinkel MB. Dietary patterns and breast cancer risk among women in northern Tanzania: a case-control study. Eur J Nutr. 2013;52:905–15. doi: 10.1007/s00394-012-0398-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leyna GH, Berkman LF, Njelekela MA, Kazonda P, Irema K, Fawzi W, Killewo J. Profile: The Dar Es Salaam Health and Demographic Surveillance System (Dar es Salaam HDSS) Int J Epidemiol. 2017 doi: 10.1093/ije/dyw324. [DOI] [PubMed] [Google Scholar]
- 32.Zack RM, Irema K, Kazonda P, Leyna GH, Liu E, Spiegelman D, Fawzi W, Njelekela M, Killewo J, Danaei G. Determinants of high blood pressure and barriers to diagnosis and treatment in Dar es Salaam, Tanzania. J Hypertens. 2016 doi: 10.1097/HJH.0000000000001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lukmanji Z, Hertzmark E, Spiegelman D, Spiegleman D, Fawzi WW. Dietary patterns, nutrient intake, and sociodemographic characteristics in HIV-infected Tanzanian pregnant women. Ecol Food Nutr. 2013;52:34–62. doi: 10.1080/03670244.2012.705768. [DOI] [PubMed] [Google Scholar]
- 34.Abioye AI, Isanaka S, Liu E, Mwiru RS, Noor RA, Spiegelman D, Mugusi F, Fawzi W. Gender differences in diet and nutrition among adults initiating antiretroviral therapy in Dar es Salaam, Tanzania. AIDS Care. 2015;27:706–15. doi: 10.1080/09540121.2014.996517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lukmanji Z, Hertzmark E, Mlingi N, Assey V, Ndossi G, Fawzi W. Tanzania Food Composition Tables [Internet] 2008 Available from: http://www.hsph.harvard.edu/nutritionsource/food-tables/
- 36.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124:17–27. doi: 10.1093/oxfordjournals.aje.a114366. [DOI] [PubMed] [Google Scholar]
- 37.Rosner B, Glynn RJ. Interval estimation for rank correlation coefficients based on the probit transformation with extension to measurement error correction of correlated ranked data. Stat Med. 2007;26:633–46. doi: 10.1002/sim.2547. [DOI] [PubMed] [Google Scholar]
- 38.Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968;70:213–20. doi: 10.1037/h0026256. [DOI] [PubMed] [Google Scholar]
- 39.Cicchetti DV, Allison T. A New Procedure for Assessing Reliability of Scoring EEG Sleep Recordings. Am J EEG Technol. 1971;11:101–10. [Google Scholar]
- 40.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet Lond Engl. 1986;1:307–10. [PubMed] [Google Scholar]
- 41.R Core Team. R: A language and environment for statistical computing [Internet] Vienna, Austria: R Foundation for Statistical Computing; Available from: http://www.R-project.org/ [Google Scholar]
- 42.Bohlscheid-Thomas S, Hoting I, Boeing H, Wahrendorf J. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the German part of the EPIC project. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol. 1997;26(Suppl 1):S59–70. doi: 10.1093/ije/26.suppl_1.s59. [DOI] [PubMed] [Google Scholar]
- 43.Bohlscheid-Thomas S, Hoting I, Boeing H, Wahrendorf J. Reproducibility and relative validity of energy and macronutrient intake of a food frequency questionnaire developed for the German part of the EPIC project. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol. 1997;26:S71. doi: 10.1093/ije/26.suppl_1.s71. [DOI] [PubMed] [Google Scholar]
- 44.Dehghan M, Martinez S, Zhang X, Seron P, Lanas F, Islam S, Merchant AT. Relative validity of an FFQ to estimate daily food and nutrient intakes for Chilean adults. Public Health Nutr. 2013;16:1782–8. doi: 10.1017/S1368980012004107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodríguez MM, Méndez H, Torứn B, Schroeder D, Stein AD. Validation of a semi-quantitative food-frequency questionnaire for use among adults in Guatemala. Public Health Nutr. 2002;5:691–9. doi: 10.1079/PHN2002333. [DOI] [PubMed] [Google Scholar]
- 46.Longnecker MP, Lissner L, Holden JM, Flack VF, Taylor PR, Stampfer MJ, Willett WC. The reproducibility and validity of a self-administered semiquantitative food frequency questionnaire in subjects from South Dakota and Wyoming. Epidemiol Camb Mass. 1993;4:356–65. doi: 10.1097/00001648-199307000-00012. [DOI] [PubMed] [Google Scholar]
- 47.Cade JE, Burley VJ, Warm DL, Thompson RL, Margetts BM. Food-frequency questionnaires: a review of their design, validation and utilisation. Nutr Res Rev. 2004;17:5–22. doi: 10.1079/NRR200370. [DOI] [PubMed] [Google Scholar]
- 48.Barbieri P, Crivellenti LC, Nishimura RY, Sartorelli DS. Validation of a food frequency questionnaire to assess food group intake by pregnant women. J Hum Nutr Diet Off J Br Diet Assoc. 2015;28(Suppl 1):38–44. doi: 10.1111/jhn.12224. [DOI] [PubMed] [Google Scholar]
- 49.Haftenberger M, Heuer T, Heidemann C, Kube F, Krems C, Mensink GB. Relative validation of a food frequency questionnaire for national health and nutrition monitoring. Nutr J. 2010;9:36. doi: 10.1186/1475-2891-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Singh GM, Micha R, Khatibzadeh S, Shi P, Lim S, Andrews KG, Engell RE, Ezzati M, Mozaffarian D, Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE) Global, Regional, and National Consumption of Sugar-Sweetened Beverages, Fruit Juices, and Milk: A Systematic Assessment of Beverage Intake in 187 Countries. PloS One. 2015;10:e0124845. doi: 10.1371/journal.pone.0124845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733. doi: 10.1136/bmjopen-2013-003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Korkalo L, Erkkola M, Fidalgo L, Nevalainen J, Mutanen M. Food photographs in portion size estimation among adolescent Mozambican girls. Public Health Nutr. 2013;16:1558–64. doi: 10.1017/S1368980012003655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Molag ML, de Vries JHM, Ocké MC, Dagnelie PC, van den Brandt PA, Jansen MCJF, van Staveren WA, van’t Veer P. Design characteristics of food frequency questionnaires in relation to their validity. Am J Epidemiol. 2007;166:1468–78. doi: 10.1093/aje/kwm236. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


