Abstract
Introduction
Glucose excursion were assessed prior and post hypoglycaemia to increase understanding of hypoglycaemia incidence and recovery during hybrid closed-loop insulin delivery.
Methods
We retrospectively analysed data from 60 adults with type 1 diabetes who received in crossover randomised design day-and-night hybrid closed-loop insulin delivery and insulin pump therapy, the latter with or without real-time continuous glucose monitoring. Over 4-week study periods, we identified hypoglycaemic episodes defined as sensor glucose < 3.0mmol/l analysed sensor glucose relative to the onset of hypoglycaemia.
Results
We identified 377 hypoglycaemic episodes during hybrid closed-loop versus 662 during control intervention (P<0.001) with a predominant reduction of nocturnal hypoglycaemia. The slope of sensor glucose prior to hypoglycaemia was steeper during closed-loop than during control intervention (P<0.01), while insulin delivery was reduced (P<0.01). During both daytime and night-time, participants recovered from hypoglycaemia faster when treated by closed-loop. At 120 min post-hypoglycaemia, sensor glucose levels were higher during closed-loop compared to control period (P<0.05).
Conclusions
Closed-loop reduces the risk of hypoglycaemia particularly overnight with swift recovery from hypoglycaemia leading to higher 2-hour post-hypoglycaemia glucose levels.
Introduction
In type 1 diabetes, hypoglycaemia is a major barrier to achieving euglycaemia using modern tight glycaemic control strategies [1]. It may be accompanied by sweating, trembling and confusion and may require assistance from another person to treat [2].
Insulin pump therapy has been shown to reduce glycated haemoglobin levels without increasing the risk of hypoglycaemia [3]. Continuous glucose monitoring also leads to improved glucose control and reduces the risk of hypoglycaemia [4] and also severe hypoglycaemia in adults with type 1 diabetes [5]. Closed-loop glucose control combining insulin delivery with real-time glucose sensing to administer insulin in glucose responsive fashion further improves glucose control [6]. However, hypoglycaemia continues to be of concern during closed-loop insulin delivery. Detailed assessments of hypoglycaemia timing, incidence and other characteristics during home use of closed-loop insulin delivery are undocumented.
In the present analysis, we retrospectively assessed hypoglycaemic episodes from a large dataset comprising sensor glucose and insulin delivery from 60 adults with type 1 diabetes who participated in a randomised crossover study contrasting day-and-night hybrid closed-loop insulin delivery and sensor-augmented or conventional pump therapy. We report data over 4-week intervention periods and describe diurnal distribution of hypoglycaemia events whilst describing glucose excursion and insulin delivery before, during and after hypoglycaemic episodes.
Methods
Experimental data
We retrospectively analysed 4-week long periods of sensor glucose and insulin delivery data collected in 60 adults (27 from Cambridge, UK; 22 Graz, Austria; 11 Profil, Germany) with type 1 diabetes [31 male, age 40.0 (11.2) years, BMI 25.2 (3.8) kg/cm2, baseline HbA1c 7.7 (0.9) %, duration of diabetes 22.1 (10.4) years, total daily insulin 0.57 (0.14) U/kg] [7, 8].
Participants were randomly assigned to receive, in crossover randomised fashion, hybrid day-and-night closed-loop insulin delivery and sensor-augmented (32 participants) or conventional (28 participants) pump therapy. Participants’ pre-study rapid-acting insulin analogue (aspart or lispro) was used during the study. Real-time (closed-loop and sensor-augmented pump therapy) or masked (conventional pump therapy) glucose levels were measured by a continuous glucose monitoring device (FreeStyle Navigator II, Abbott Diabetes Care, Alameda, CA, USA) calibrated according to manufacturer’s instruction. The built-in bolus wizard of the study insulin pump (Dana Diabecare R, SOOIL, Seoul, Republic of Korea) was used by participants to calculate insulin boluses at mealtimes and when administering correction boluses. During closed-loop period, a model-predictive control algorithm directed basal insulin delivery [7, 8].
A hypoglycaemic episode was defined as sensor glucose <3 mmol/l for at least 10 min [9]. Hypoglycaemic episodes were at least 30min apart to be counted as separate events. We excluded episodes within 60 min of insulin bolus as these episodes may be predominantly attributable to bolus over-delivery and unrelated to closed-loop glucose control. The exclusion criterion was applied to both study periods.
Statistical analysis
We identified hypoglycaemic episodes for each participant separately. We evaluated for each participant the average sensor glucose and the average basal insulin infusion rates from −60 min to 120 min in 10 min steps relative to the onset of hypoglycaemic episodes. We then calculated the mean sensor glucose excursions and mean basal insulin infusion across all participants. The minimum glucose levels during hypoglycaemia, area-under-curve (AUC) hypoglycaemia and duration of hypoglycaemia were also calculated. Hypoglycaemic episodes identified during the night-time (midnight to 6h00) and the daytime (6h00 to midnight) periods were analysed separately.
A Student’s t-test contrasted endpoints collected during closed-loop and control periods. Statistical analyses were performed using SPSS, version 21 (IBM Software, Hampshire, U.K.). P values less than 0.05 were considered statistically significant. Data are presented as mean (SD) unless stated otherwise.
Results
Data were analysed from 1,680 days of closed-loop insulin delivery and 1,680 days of sensor-augmented or conventional insulin pump therapy. We identified 377 hypoglycaemic episodes during closed-loop period of which 87 were nocturnal (midnight to 6h00.), versus 662 episodes during control period of which 205 were nocturnal (closed-loop vs. control arm, 1.27 (1.17) vs. 2.48 (2.50) episodes per participant per week, P<0.001).
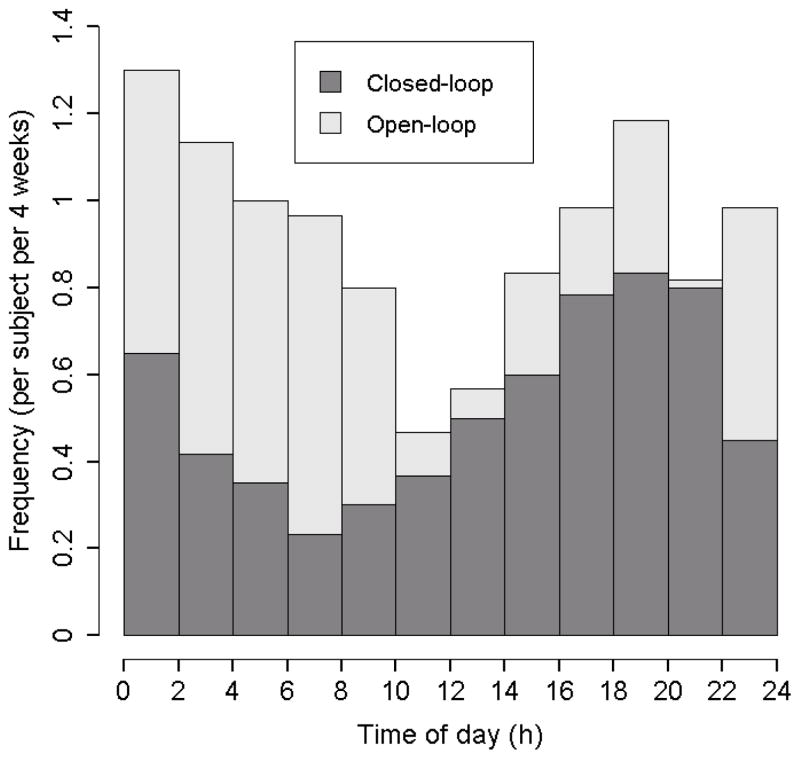
Figure 1 shows the diurnal distribution of hypoglycaemia incidence during two treatment periods. A reduced hypoglycaemia incidence was observed during closed-loop period compared to control period with a predominant reduction between 22h00 and 8h00 when the incidence of hypoglycaemia was halved. Figure S1 (Supplemental data) shows the risk of hypoglycaemia conditioned on ambient sensor glucose; with sensor glucose between 3 and 8 mmol/l, the risk of hypoglycaemia 60 min later is halved during closed-loop.
Figure 1.
Incidence of hypoglycaemia events (sensor glucose < 3.0 mmol/l for at least 10min) during hybrid closed-loop insulin delivery (dark grey bars) and control periods (light grey bars) (mean; N = 60).
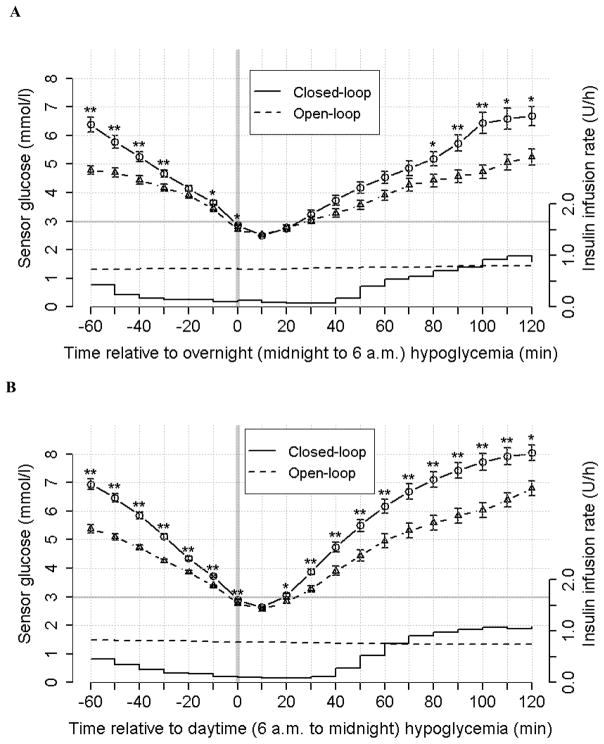
Figure 2 summarizes sensor glucose levels before, during, and after hypoglycaemic episodes during closed-loop and control periods. Sensor glucose prior to hypoglycaemia was declining steeper during closed-loop compared to control periods (P = 0.002). During daytime, the participants recovered from hypoglycaemia faster when treated by closed-loop (higher sensor glucose values from 20 min to 120 min post-hypoglycaemia, P<0.05). A similar trend was observed during night-time. Table S1 (Supplemental data) reports sensor glucose values from 30 min to 120 min relative to the onset of hypoglycaemia.
Figure 2.
Sensor glucose values from −60 min to 120 min relative to the onset of hypoglycaemia (sensor glucose < 3.0mmol/l; vertical bar) during hybrid closed-loop period (circles connected by solid line; mean ± SEM; N=60; * P < 0.05, ** P < 0.01 compared to control therapy) and during control period (triangles connected by dashed line). Piecewise-constant lines without error bars represent mean insulin infusion rates during closed-loop period and dashed lines without error bars are insulin infusions during control period. Panel A shows glycaemic and insulin infusion data during the night-time period (midnight to 6 a.m.) and panel B shows the daytime period (6 a.m. to midnight).
The mean basal insulin infusion rates were lower during closed-loop compared to control periods from −60 min to 80 min during daytime (P = 0.001) and from −60 min to 50 min during daytime (P = 0.003).
The minimum glucose levels during hypoglycaemia were not different between closed-loop and open-loop [2.4 (0.4) vs. 2.5 (0.4) mmol/l, P = 0.4 for the overnight period; 2.6 (0.2) vs. 2.5 (0.4) mmol/l, P = 0.1 for the daytime period]. The AUC hypoglycaemia was reduced during closed-loop compared to open-loop [40.3 (33.1) vs. 52.8 (43.9) mmol/l.min, P=0.04 for the overnight period; 22.4 (8.8) vs. 38.8 (52.9) mmol/l.min, P = 0.02 for the daytime period]. The duration of hypoglycaemia was reduced by 21 min during the closed-loop over the overnight period [51.9 (30.3) vs. 72.9 (37.8) min, P <0.001] with no difference during daytime [35.2 (11.9) vs. 45.5 (24.4) min, P = 0.06].
Discussion
The present analysis reports incidence and diurnal distribution of hypoglycaemia in adults with type 1 diabetes during home use of hybrid closed-loop insulin delivery and sensor-augmented or conventional insulin pump therapy. We evaluated sensor glucose excursions and basal insulin infusion rates prior and post-hypoglycaemia. We found different patterns of hypoglycaemia incidence and hypoglycaemia recovery between the two interventions.
Many prospective and retrospective studies of hypoglycaemia incidence are based on self-reported data with considerable variation in reported outcomes such as 43 episodes per patient-year in [10], 73 in [11] and 94 in [12]. In the present analysis, we report incidence of clinically significant hypoglycaemia at 144 episodes per patient-year during insulin pump therapy using sensor glucose data. Continuous glucose monitoring provides comprehensive glucose levels over 24 hours a day, and enables transparent definition and recording of hypoglycaemic episodes when device usage is high such in the present analysis with median sensor wear time at 94% and 95% of the total time for closed-loop and control periods, respectively.
Our analyses document the risk of hypoglycaemia to be reduced during closed-loop compared to control periods (377 vs. 662 hypoglycaemic episodes) in adults with type 1 diabetes and with baseline HbA1c levels ranging from 5.8 to 9.7%. Figure 1 shows that predominant reduction of hypoglycaemia was overnight. Figure 2 shows that during closed-loop period, sensor glucose was reducing more rapidly prior to hypoglycaemia compared to control intervention. Our interpretation is that closed-loop was capable of preventing hypoglycaemia when sensor glucose was not decreasing rapidly. Thus, only rapid decline of sensor glucose lead to hypoglycaemia during closed-loop. This is supported by reducing the risk of hypoglycaemia within 60 min stratified according to ambient sensor glucose (Figure S1, Supplemental data).
Two peaks of hypoglycaemia incidence were observed during two treatment periods, one around 16h00 to 20h00 and the other around 0h00 to 2h00 (Figure 1). The former may be related to increased physical activity and the latter resulting from post-meal insulin corrections due to delayed meal effects following high-fat evening meals [13].
Previous studies have shown that closed-loop improves glycaemic control in type 1 diabetes through the system’s ability to adjust insulin delivery in response to varying insulin requirements [14]. Figure 2 demonstrates this paradigm; comparing the mean insulin delivery at around 0.8 U/h observed even during imminent onset of hypoglycaemia, closed-loop reduced insulin delivery −60 min to 80 min relative to onset of overnight hypoglycaemia and from −60 min to 50 min relative to daytime hypoglycaemia. The reduced amount of insulin resulted in faster recovery and higher 2-hour post-hypoglycaemia glucose levels during closed-loop (Table S1 and Figure 2).
Glucose troughs during hypoglycaemia were not different during closed-loop and open-loop. However, during closed-loop, both AUC hypoglycaemia and the duration of hypoglycaemic events were reduced on account of a swifter recovery from hypoglycaemia.
An observational study reported that in real-life settings a majority of patients overtreated their hypoglycaemic episodes [15]. Given that post-hypoglycaemia glucose levels were higher during closed-loop compared to control periods, a reasonable recommendation for clinical practitioners would be to reinforce and possibly revise the patients’ education about hypoglycaemia correction especially for those during closed-loop treatment. Further studies are warranted to explore optimal strategies for hypoglycaemia treatment during closed-loop glucose control.
The strength of our analysis is the multicentre multinational crossover randomised study design where each subject serves as his/her own control, and the considerable volume of sensor glucose data used to identify the hypoglycaemic episodes. The data were collected during unsupervised home studies and thus glucose excursions reflect hypoglycaemia incidence and patients’ self-treatment of hypoglycaemia under free-living settings. Limitations are the lack of reliable data about the amount of rescue carbohydrates.
Conclusions
Hybrid closed-loop reduces the risk of hypoglycaemia particularly overnight with a swift recovery from hypoglycaemia during daytime and leads to a slightly elevated 2-hour post-hypoglycaemia glucose levels compared to insulin pump therapy.
Supplementary Material
Acknowledgments
We are grateful to study volunteers for their participation. We acknowledge support by the staff at the Addenbrooke’s Wellcome Trust Clinical Research Facility. Jasdip Mangat and John Lum (Jaeb Center) supported development and validation of the closed-loop system. Josephine Hayes (University of Cambridge) provided administrative support. Karen Whitehead (University of Cambridge) provided laboratory support. We acknowledge support by the staff at Profil Institut; Krisztina Schmitz-Grozs provided support as a research physician, Martina Haase supported the study as an insulin pump expert, and Maren Luebkert, Kirstin Kuschma and Elke Przetak provided administrative, coordinating and documentation support.
Funding: Seventh Framework Programme of the European Union (ICT FP7- 247138) and Swiss National Science Foundation (P1BEP3_165297). Additional support for the Artificial Pancreas work by JDRF, National Institute for Health Research Cambridge Biomedical Research Centre, Wellcome Strategic Award (100574/Z/12/Z), EC Horizon 2020 (H2020-SC1-731560), NIDDK (DP3DK112176 and 1UC4DK108520-01), Efficacy and Mechanism Evaluation Programme of National Institute for Health Research (14/23/09).
Footnotes
Conflict of interest
RH reports having received speaker honoraria from Eli Lilly, Novo Nordisk and Astra Zeneca, serving on advisory panel for Eli Lilly and Novo Nordisk, receiving license fees from BBraun and Medtronic; and having served as a consultant to BBraun. MEW has received license fees from Becton Dickinson and has served as a consultant to Beckton Dickinson. MLE reports having received speaker honoraria from Abbott Diabetes Care, Novo Nordisk and Animas, serving on advisory panels for Novo Nordisk, Abbott Diabetes Care, Medtronic, Roche and Cellnovo and holding stock options in Cellnovo. SH serves as a consultant for Novo-Nordisk and for the ONSET group, and reports having received speaker/training honoraria from Medtronic. RH and MEW report patents and patent applications. JKM reports having received speaker honoraria from Abbott Diabetes Care, AstraZeneca, Eli Lilly & Co, NintaMed, NovoNordisk, Roche Diabetes Care, Sanofi, Servier, Takeda, and serving on advisory panel for Becton Dickinson, MSD, Sanofi and Boehringer Ingelheim. TRP is an advisory board member of Novo Nordisk A/S, a consultant for Roche, Novo Nordisk A/S, Eli Lilly & Co, Infineon, Carnegie Bank and on speaker’s bureau of Novo Nordisk A/S and Astra Zeneca. LL reports having received speaker honoraria from Minimed Medtronic, Animas, Sanofi and Novo Nordisk, serving on advisory panel for Animas Minimed Medtronic and Novo Nordisk. LB, HT, SD, CB, MH, HK, and SA declare no competing financial interests exist.
Author contributions
YR and RH had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. RH coordinated the study. RH, MLE, LL, CB, SA, HT, LB, MEW, TP and JKM co-designed the study. HT, LB, SH, SD, JKM, MH, HK, and JP were responsible for screening and enrolment of participants, and arranged informed consent from the participants. HT, LB, SH, SD, JKM, MH, and HK provided patient care and/or took samples. YR and RH carried out data analysis. YR and RH wrote the manuscript. All authors critically reviewed the report.
References
- 1.Cryer PE. Hypoglycaemia: the limiting factor in the glycaemic management of Type I and Type II diabetes. Diabetologia. 2002 Jul;45:937–48. doi: 10.1007/s00125-002-0822-9. [DOI] [PubMed] [Google Scholar]
- 2.Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013 May;36:1384–95. doi: 10.2337/dc12-2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Misso ML, Egberts KJ, Page M, O’Connor D, Shaw J. Continuous subcutaneous insulin infusion (CSII) versus multiple insulin injections for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2010 Jan 20;:CD005103. doi: 10.1002/14651858.CD005103.pub2. [DOI] [PubMed] [Google Scholar]
- 4.G. Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study. Bode B, Beck RW, Xing D, Gilliam L, Hirsch I, et al. Sustained benefit of continuous glucose monitoring on A1C, glucose profiles, and hypoglycemia in adults with type 1 diabetes. Diabetes Care. 2009 Nov;32:2047–9. doi: 10.2337/dc09-0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heinemann L, Freckmann G, Ehrmann D, Faber-Heinemann G, Guerra S, Waldenmaier D, et al. Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycaemia awareness or severe hypoglycaemia treated with multiple daily insulin injections (HypoDE): a multicentre, randomised controlled trial. Lancet. 2018 Feb 15; doi: 10.1016/S0140-6736(18)30297-6. [DOI] [PubMed] [Google Scholar]
- 6.Weisman A, Bai JW, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. 2017 Jul;5:501–512. doi: 10.1016/S2213-8587(17)30167-5. [DOI] [PubMed] [Google Scholar]
- 7.Thabit H, Tauschmann M, Allen JM, Leelarathna L, Hartnell S, Wilinska ME, et al. Home use of an artificial beta cell in type 1 diabetes. N Engl J Med. 2015 Nov 17;373:2129–40. doi: 10.1056/NEJMoa1509351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bally L, Thabit H, Kojzar H, Mader JK, Qerimi-Hyseni J, Hartnell S, et al. Day-and-night glycaemic control with closed-loop insulin delivery versus conventional insulin pump therapy in free-living adults with well controlled type 1 diabetes: an open-label, randomised, crossover study. Lancet Diabetes Endocrinol. 2017 Apr;5:261–270. doi: 10.1016/S2213-8587(17)30001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.G. International Hypoglycaemia Study. Glucose concentrations of less than 3.0 mmol/L (54 mg/dL) should be reported in clinical trials: a joint position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2017 Jan;40:155–157. doi: 10.2337/dc16-2215. [DOI] [PubMed] [Google Scholar]
- 10.Donnelly LA, Morris AD, Frier BM, Ellis JD, Donnan PT, Durrant R, et al. Frequency and predictors of hypoglycaemia in Type 1 and insulin-treated Type 2 diabetes: a population-based study. Diabet Med. 2005 Jun;22:749–55. doi: 10.1111/j.1464-5491.2005.01501.x. [DOI] [PubMed] [Google Scholar]
- 11.Khunti K, Alsifri S, Aronson R, Cigrovski Berkovic M, Enters-Weijnen C, Forsen T, et al. Rates and predictors of hypoglycaemia in 27 585 people from 24 countries with insulin-treated type 1 and type 2 diabetes: the global HAT study. Diabetes Obes Metab. 2016 Sep;18:907–15. doi: 10.1111/dom.12689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ostenson CG, Geelhoed-Duijvestijn P, Lahtela J, Weitgasser R, Markert Jensen M, Pedersen-Bjergaard U. Self-reported non-severe hypoglycaemic events in Europe. Diabet Med. 2014 Jan;31:92–101. doi: 10.1111/dme.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elleri D, Allen JM, Harris J, Kumareswaran K, Nodale M, Leelarathna L, et al. Absorption patterns of meals containing complex carbohydrates in type 1 diabetes. Diabetologia. 2013 May;56:1108–17. doi: 10.1007/s00125-013-2852-x. [DOI] [PubMed] [Google Scholar]
- 14.Ruan Y, Thabit H, Leelarathna L, Hartnell S, Willinska ME, Dellweg S, et al. Variability of Insulin Requirements Over 12 Weeks of Closed-Loop Insulin Delivery in Adults With Type 1 Diabetes. Diabetes Care. 2016 May;39:830–2. doi: 10.2337/dc15-2623. [DOI] [PubMed] [Google Scholar]
- 15.Savard V, Gingras V, Leroux C, Bertrand A, Desjardins K, Mircescu H, et al. Treatment of Hypoglycemia in Adult Patients with Type 1 Diabetes: An Observational Study. Can J Diabetes. 2016 Aug;40:318–23. doi: 10.1016/j.jcjd.2016.05.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.