Abstract
Objectives
To quantify the improvement in US life expectancy required to reach parity with high-resource nations by 2030, to document historical precedent of this rate, and to discuss the plausibility of achieving this rate in the United States.
Methods
We performed a demographic analysis of secondary data in 5-year periods from 1985 to 2015.
Results
To achieve the United Nations projected mortality estimates for Western Europe in 2030, the US life expectancy must grow at 0.32% a year between 2016 and 2030. This rate has precedent, even in low-mortality populations. Over 204 country-periods examined, nearly half exhibited life-expectancy growth greater than 0.32%. Of the 51 US states observed, 8.2% of state-periods demonstrated life-expectancy growth that exceeded the 0.32% target.
Conclusions
Achieving necessary growth in life expectancy over the next 15 years despite historical precedent will be challenging. Much all-cause mortality is structured decades earlier and, at present, older-age mortality reductions in the United States are decelerating. Addressing mortality decline at all ages will require enhanced political will and a strong commitment to equity improvement in the US population.
In its 2012 report “For the Public’s Health: Investing in a Healthier Future,”1 the Institute of Medicine (IOM; later split into the National Academy of Medicine and the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine), in a section called “Setting a National Target for Improvement,” made its first recommendation that the Secretary of the US Department of Health and Human Services “should adopt an interim explicit life expectancy target … to be achieved by 2030.”1(p4) They indicate that reaching this target should “engage all health system stakeholders in actions intended to achieve parity with high resource peer nation averages”1(p4) by that date.
Although the recommendation refers to life expectancy at birth, the committee noted (drawing from the National Research Council2) some of the increases that will be needed with regard to life expectancy at age 50 years. To equal the average peer nation for women by 2030 would require an increase in life expectancy at 50 years of 1.5 years; 4.1 years is needed to reach the highest-performing nation. For men, there would need to be a 0.8-year increase in 50-year-old life expectancy to match the average peer nation and a 2.3-year increase to equal the nation with the highest life-expectancy values. These gains would only be sufficient to achieve parity if there were no additional improvements in life expectancy of other countries. It is the purpose of this perspective to more fully analyze the plausibility of achieving this outcome in the light of historical life-expectancy improvement performance for low-mortality countries and for individual states within the United States.
HISTORICAL DIVERGENCE IN LIFE EXPECTANCY
Between 1960 and 1985, life expectancy in the United States increased alongside that of other resource-rich countries, including Sweden, France, and Japan,3 growing at an average of 0.26% a year. Beginning around 1985, increases in US life expectancy began to fall behind those of “peer” high-income nations, slowing to 0.20% a year during 1985 to 2010, to 0.06% between 2012 and 2013, and falling to negative growth by 2014 to 2015. By 2005, US life expectancy had fallen nearly 2 years below the average life expectancy in Western European populations. This disparity has persisted into the present and is not predicted to narrow.4,5 Though the gap amounts to a small absolute number of years in the life-expectancy metric, when distributed across the US population, it represents an extraordinarily large number of life years lost. Given the global pace of change in life expectancy, it is akin to falling roughly 2 decades behind peer countries.6
Figure 1 demonstrates these trends for women and men. The gap for women is noticeably larger. Patterns of life expectancy at older ages (e.g., 50 and 60 years) display marginally smaller gaps—and, in fact, the United States has a life expectancy at age 80 years that is comparable with that of other high-income nations—but the US standing on life expectancy relative to other high-income nations demonstrates a similar steep downward trend at all ages.3,7
FIGURE 1.
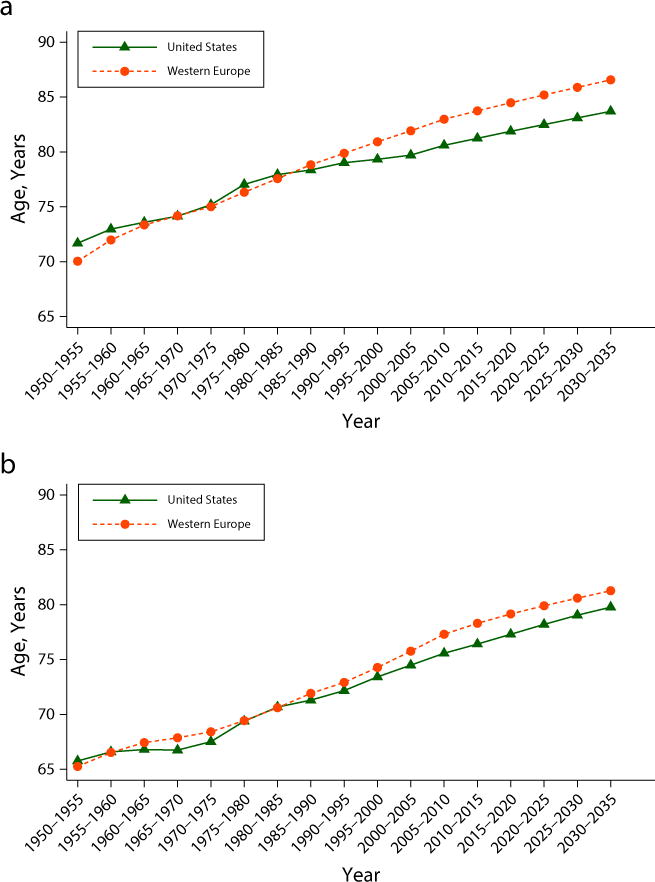
Life Expectancy at Birth by Period, Observed and Projected Among (a) Women and (b) Men: United States and Western Europe, 1950–2035
Source. United Nations Population Division.4
Note. Estimates following 2010 are United Nations projections.
The sources of the 1980s’ divergence— and the persistent life-expectancy disadvantage—have received considerable attention from scholars across disciplines.7–12 The disadvantage does not have a single or even a small set of underlying causes. The US mortality disadvantage spans sources of death arising from complications at birth, accidents, injuries, homicide, HIV/AIDS, heart disease, diabetes, and sources of death exacerbated by obesity. These proximate causes cannot be attributed to a few specific behaviors or a few dimensions of context. Instead, a number of features of US society are implicated, including caloric consumption patterns, gun violence, unprotected sexual intercourse, environments that hinder physical activity, barriers to health care access, child poverty, and high (and rising) income inequality.3,13 The US disadvantage is accrued across most age groups, all socioeconomic groups, most ethno-racial groups, and many causes of death. For example, mortality and morbidity among the wealthiest, highest-educated, and highest-income persons in the United States exceeds that of their matched-socioeconomic-status counterparts in Western European populations.11,14
A 2013 National Academies report, US Health in International Perspective: Shorter Lives, Poorer Health, analyzed country-specific mortality variation in detail, using data from the United States and 16 other high-income nations. As expected, the United States ranked last in life expectancy, both for men and women. Analysis revealed that two fifths of the life-expectancy disadvantage for women, relative to that of other high-income nations, is accrued before the age of 50 years and three fifths is accrued between age 50 and 75 years.9,13 For men, two thirds of the disparity is attributable to mortality before the age of 50 years and one third attributable to mortality between age 50 and 75 years. The report concluded that mortality rates after age 75 years were not disparately high in the United States, yet more recent efforts contradict these findings, suggesting that even the oldest persons in the United States exhibit a survival disadvantage.15
We considered 3 questions: (1) What improvement in US life expectancy would be required to reach parity with high-resource nations by 2030? (2) Is growth in life expectancy of this speed possible? (3) Given that mortality lags health inputs by years and even decades, is life-expectancy growth of this speed plausible for the current US population in the coming years? To answer these questions, we examined life-expectancy growth in other periods and in other populations. Before proceeding, an important note about life-expectancy construction is warranted: life expectancy is a summary indicator—and specifically, a weighted average—of mortality across age groups. Growth in life expectancy in 2 populations may occur at different ages and for different reasons. By construction, declines in mortality rates of infants and children will generate much larger increases in life expectancy relative to mortality rate reductions of the same magnitude among the elderly.
METHODS
Following previous benchmarking of US life expectancy,11,13,14 we calculated the rate of life-expectancy growth necessary to match United Nations projections of life expectancy among Western European nations in 2030. To consider the plausibility of this growth for the United States, we tested whether such life-expectancy growth has historical precedent across a wider range of high-income populations. We selected the 34 Organisation for Economic Cooperation and Development countries as providing relevant comparative value. For these populations, we measured life-expectancy growth during each 5-year period between 1985 and 2015. We also assessed other metrics to consider whether these populations provided appropriate comparisons.
Specifically, because mortality decline tends to decelerate as survival gains become concentrated in adulthood, we measured the crude death rate (or deaths per thousand persons per year) and the infant mortality rate (or deaths among children younger than 1 year in a year divided by births in that year). We measured the purchasing power–adjusted gross domestic product per capita to capture economic variation across place, which is a known predictor of life expectancy change over time. Because mortality rates of place-specific populations can be influenced heavily by migration, we also assessed estimates of net migration.
Finally, to assess whether growth in period life expectancy has precedent within the United States, we conducted a similar analysis for US state populations, by using state-specific data provided by the Institute for Health Metrics and Evaluation.16
RESULTS
Achieving the IOM goal of reaching parity with the average life expectancy in high-income nations by 2030 would require significant gains in US life expectancy over the next 15 years. Because life expectancy elsewhere will also continue to increase, US life expectancy would need to accelerate considerably. Between 2014 and 2015, US life expectancy decreased by 0.13%. To achieve the United Nations projected mortality estimates for Western Europe in 2030,4 the US life expectancy would need to average growth of 0.32% a year, or 1.6% every 5 years, between 2016 and 2030 (0.32 = ln[Western Europe LE 2030–2035/US LE 2010–2015]/20; Figure 2).
FIGURE 2.
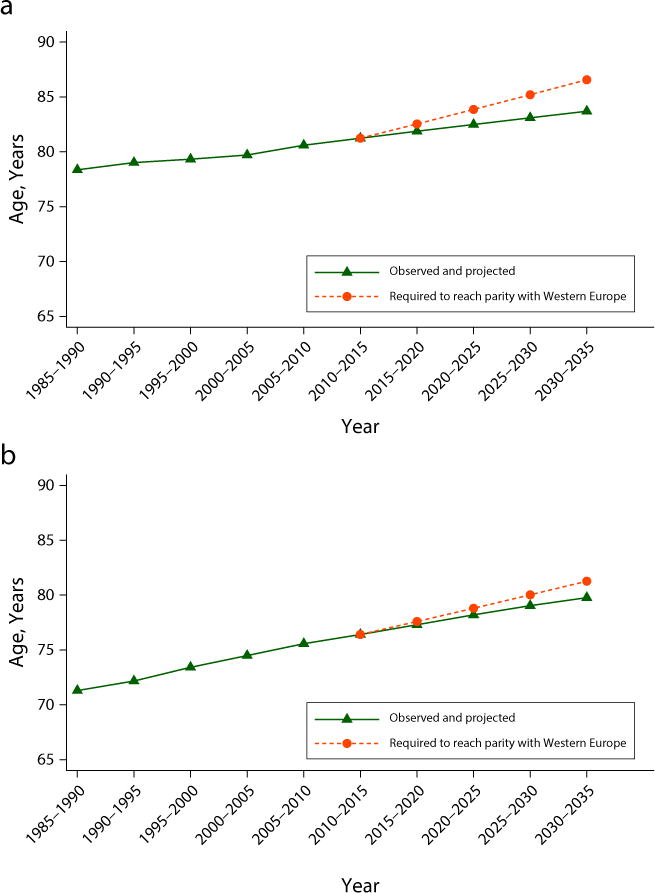
Life Expectancy at Birth by Period, Observed, Projected, and Necessary for Parity Among (a) Women and (b) Men: United States, 1985–2035
Source. United Nations Population Division.4
Note. Estimates following 2010 are United Nations projections.The dashed line represents author calculations of US life expectancy needed to reach United Nations projection of life expectancy in Western European nations in 2030-2035.
Over the 204 country-periods examined (34 countries assessed over six 5-year periods), 92 country-periods—nearly half of those examined—exhibited life-expectancy growth of the speed necessary for the United States to achieve parity with Western Europe by 2030.
Results for all 34 countries are available in Tables A–C (available as a supplement to the online version of this article at http://www.ajph.org). Table 1 displays 9 examples representing populations with a range of mortality and income levels among the 34 OECD countries. It shows the most recent period during which the population life-expectancy value grew at a rate exceeding 0.32% a year and gives the mean rate of growth during the period specified under an assumption of exponential growth (linear growth generates nearly identical values for periods this short). Table 1 also lists the period-specific rates spanning 1985 to 2015 to demonstrate variation across the years considered.
TABLE 1.
Life Expectancy Growth by Country and Period: Selected Organization for Economic Cooperation and Development Countries, 1985–2015
| Country | Perioda | Rate of Change,b % | Estimated Annual Rate for Each 5-Year Periodc
|
|||||
|---|---|---|---|---|---|---|---|---|
| 1985–1990, % | 1990–1995, % | 1995–2000, % | 2000–2005, % | 2005–2010, % | 2010–2015, % | |||
| Australia | 1990–2010 | 0.35 | 0.25 | 0.38 | 0.32 | 0.38 | 0.32 | 0.17 |
| Denmark | 2000–2010 | 0.33 | 0.08 | 0.13 | 0.21 | 0.32 | 0.33 | 0.19 |
| France | 2005–2010 | 0.35 | 0.35 | 0.33 | 0.28 | 0.29 | 0.35 | 0.20 |
| Germany | 1995–2005 | 0.35 | 0.36 | 0.23 | 0.35 | 0.35 | 0.30 | 0.22 |
| Italy | 1995–2010 | 0.34 | 0.41 | 0.28 | 0.33 | 0.38 | 0.31 | 0.20 |
| Korea | 1985–2015 | 0.63 | 0.88 | 0.69 | 0.56 | 0.64 | 0.66 | 0.35 |
| Mexico | 1985–2010 | 0.47 | 0.61 | 0.56 | 0.52 | 0.33 | 0.34 | 0.29 |
| Turkey | 1985–2015 | 0.74 | 0.92 | 0.76 | 0.90 | 0.82 | 0.55 | 0.46 |
| United Kingdom | 2000–2010 | 0.33 | 0.25 | 0.30 | 0.24 | 0.33 | 0.33 | 0.20 |
Source. Authors’ calculations from United Nations Population Division.4
Note. Values in 2010–2015 represent United Nations projections.
The most recent period during which life expectancy (LE) growth exceeded an average of 0.32% a year over a 5-year period.
The average annual rate of change during the specified period under the assumption of exponential growth. For example, for Australia the annual rate of change for the selected period 1990–2010 = ln(LE_2005–2010/LE_1985–1990)/20.
The annual rates of change in LE combined for each 5-year segment in the period 1985–2015. For example the value of 0.25% for Australia between 1985–1990 = ln(LE 1985–1990/LE 1980–1985)/5.
Are mortality-related conditions in these populations comparable on even basic terms with those of the contemporary United States? We compared values on several indicators (Table D, available as a supplement to the online version of this article at http://www.ajph.org). As expected, Turkey and Mexico achieved high life-expectancy growth during periods of significant economic growth and improvement in infant and child survival. By contrast, every other country had a starting infant mortality rate that was close in magnitude or smaller than that of the present-day US population. These populations experienced infant mortality rate decline over the period of high life-expectancy growth, but reductions of modest absolute magnitude (e.g., 3/1000 contributes roughly a third of a year increase in life expectancy at birth). It is clear, then, that precedent for life-expectancy growth of 0.32% a year is well established in other populations with similar (or lower) starting mortality levels, similar levels of economic resources, and similar positive values of net migration.
We also observed that several state populations within the United States have achieved this kind of growth in life expectancy. Results from all states are available in the supplements to the online version of this article at http://www.ajph.org. Table 2 summarizes findings from states that experienced average annual growth exceeding 0.32% for both men and women for at least 5 years between 1985 and 2010. Of the 51 states observed over 25 years (1985–2010), 105 observations (8.2%) demonstrated life-expectancy growth that exceeded the 0.32% target for both men and women; 156 (12.2%) exhibited life-expectancy growth that exceeded the target for women only; 433 (34%) exhibited life-expectancy growth that exceeded the target for men only. Unsurprisingly, the states with high life-expectancy growth are also states with higher levels of immigration, relative to the national average.17
TABLE 2.
Life Expectancy Growth by State and Period: Selected US States, 2005–2010
| Gender and State | Perioda | Rate of Change,b % | Estimated Annual Ratec
|
|||||
|---|---|---|---|---|---|---|---|---|
| 2005, % | 2006, % | 2007, % | 2008, % | 2009, % | 2010, % | |||
| Women | ||||||||
| California | 2005–2010 | 0.33 | 0.22 | 0.31 | 0.29 | 0.28 | 0.21 | 0.53 |
| Delaware | 2002–2007 | 0.32 | −0.05 | 0.39 | 0.51 | −0.04 | 0.06 | 0.37 |
| District of Columbia | 2005–2010 | 0.54 | −0.16 | 0.08 | 0.36 | 0.66 | 0.69 | 0.91 |
| Louisiana | 2005–2010 | 0.32 | −0.08 | 0.53 | 0.36 | 0.17 | 0.05 | 0.51 |
| Maryland | 2003–2008 | 0.32 | 0.25 | 0.24 | 0.35 | 0.30 | 0.19 | 0.40 |
| Nevada | 2003–2008 | 0.33 | 0.09 | 0.27 | 0.54 | 0.29 | 0.00 | 0.44 |
| New Jersey | 2002–2007 | 0.34 | 0.31 | 0.40 | 0.32 | 0.22 | 0.16 | 0.45 |
| New York | 2002–2007 | 0.32 | 0.32 | 0.31 | 0.27 | 0.21 | 0.17 | 0.43 |
|
| ||||||||
| Men | ||||||||
| California | 2005–2010 | 0.45 | 0.14 | 0.34 | 0.42 | 0.41 | 0.44 | 0.63 |
| Delaware | 2003–2008 | 0.32 | 0.19 | 0.30 | 0.40 | 0.36 | 0.21 | 0.21 |
| District of Columbia | 2005–2010 | 1.03 | 0.57 | 0.46 | 1.00 | 0.94 | 0.79 | 1.95 |
| Louisiana | 2005–2010 | 0.43 | 0.10 | 0.53 | 0.31 | 0.54 | 0.08 | 0.69 |
| Maryland | 2003–2008 | 0.39 | 0.35 | 0.36 | 0.43 | 0.36 | 0.40 | 0.67 |
| Nevada | 2005–2010 | 0.44 | 0.08 | 0.18 | 0.54 | 0.60 | 0.35 | 0.52 |
| New Jersey | 2003–2008 | 0.43 | 0.28 | 0.39 | 0.51 | 0.36 | 0.26 | 0.34 |
| New York | 2002–2007 | 0.45 | 0.28 | 0.41 | 0.44 | 0.21 | 0.18 | 0.46 |
The most recent 5-year period during which LE growth exceeds an average of 0.32% a year.
The average annual rate of change in LE during the specified period under the assumption of exponential growth.
The annual rates of change in life expectancy (LE) for the years 2005–2010.
DISCUSSION
In 1985, life expectancy in the United States matched that of Western Europe; the gaps between the United States and other nations are relatively new in historical terms. The rate of change in mortality needed to achieve parity by 2030 (0.32 years of life expectancy per year) does have historical precedent in some populations. Do these precedents have any meaning for the present-day US population? Is there room for optimism about resuming life-expectancy parity with peer nations by 2030? Several general features of the US population make significant life-expectancy gains in the future plausible: the United States has a larger share of immigrants (who are typically healthier than native-born residents) relative to some other high-income nations. Smoking rates have declined across younger cohorts, and this is projected to increase life expectancy as these cohorts age.18 Perhaps most importantly, several state populations within the United States have achieved this kind of growth in life expectancy.
At the same time, achieving this necessary acceleration in life expectancy over the next 15 years may prove difficult. Because health traits accumulate over the life course— with particular sensitivity to developmental periods early in life—a nontrivial proportion of all-cause mortality in any given year is structured many decades earlier.19,20 Some component of mortality over the next 15 years has, in a sense, already been determined. At present, life-expectancy gains in high-income nations are largely driven by survival improvements in adulthood.8,21 This is projected to continue over the next 15 years.5 Because of these patterns, assessment of precedent that might be plausibly relevant for the United States must focus on other populations at similar points in the mortality transition—that is, other low-mortality nations.20 Achieving high annual life-expectancy growth is arguably more costly in populations with low levels (from a global standpoint) of infant and child mortality. Moreover, at present, older-age mortality reductions appear to be decelerating,15 and female mortality is increasing in a number of US counties.22 US mortality decelerations warrant additional note. Our analysis of historical patterns indicate that 78% of the above-mentioned 92 country-periods in which life-expectancy growth exceeded 0.32% per year followed periods of acceleration in mortality decline, underscoring the present disadvantaged position of the United States.
Finally, of the major causes of US life-expectancy disadvantage—caloric consumption patterns, gun violence, drug overdoses, unprotected sexual intercourse, environments that hinder physical activity, barriers to health care access, child poverty, and high (and rising) income inequality— few indicate significant signs of improvement since the early 2000s (see Flegal et al.23 and Ogden et al.24 on stably high obesity levels but Welsh et al.25 and Kit et al.26 on reductions in the consumption of added sugars; Marczak et al.27 on marginal declines in firearm death but Rudd et al.28 on the tripling in drug overdose death; Liu et al.29 on stability in adolescent sexual behavior, Fanfair et al.30 on some reductions in sexually transimitted infection seroprevalance; Institute for Research on Poverty31 on increases in child poverty; and Saez and Zucman32 on increases in wealth inequality).
In the absence of a shift in these trends, gains in infant and child survival cannot offset decelerations in adult mortality sufficient to reach life-expectancy parity with other high-income nations; halving the United States’ current infant mortality rate would extend overall US life expectancy by only one third of a year. Instead, efforts to reverse the deceleration of adult survival gains and to continue reductions in infant and child mortality will require enhanced political will and a strong national public and private commitment to equity improvement in the coming decades.
We are presently in a time of significant transition at the federal level. The rhetoric and policy directions are concerning, and retreating from a national standard for health care access would be a major setback. However, it is also important to keep in mind that health care is not the most important determinant of health, and that we have not yet achieved health care affordability or value (outcomes per unit of expenditure) compared with other developed nations. Much work remains to be done if we are to improve population health, not all of it focused on health care.33 Population health problems are often decades in the making, and solutions will likely take similarly long periods to implement. Therefore, it is crucial to continue our work in the coming years and to find openings where we can. The next 4 years may also be an opportunity for state-level innovation, enhancing partnerships with the business community, and making sure that job creation and economic development are done equitably and in health-promoting ways.
However challenging, we think that it is useful to set targets as the National Academy of Medicine/IOM suggested, and in particular to think of measuring progress in short-term increments. Longer-term goals, such as a 15-year increase, can be less motivating and less accountable in the short run. As an example, other scholarship reports the comparative annual change in White and Black mortality rates over the 1999 to 2013 period in per-year rate-reduction terms.34 Benchmarking annual life-expectancy improvements we highlight here and making them known publicly can contribute to motivation and action.
Life expectancy is certainly not the only or the best population health metric to use to measure progress over time. Indeed, the same National Academy of Medicine committee called for the development of health-related quality of life measures with similar future targets. Measures that can change more rapidly in the shorter term such as infant mortality or the Centers for Disease Control and Prevention unhealthy days metric may be more useful in stimulating investment and policy changes in the short run. Similar targets for achieving subpopulation life-expectancy equity and other outcomes are needed as well, given the large variations seen within and across states and communities.
Finally, we need to examine more closely the nations and states who have met or exceeded the target to identify possible sources of success and consider whether these are replicable in a given jurisdiction and context. Such comparative cost-effectiveness evidence35 can serve as the basis for the steady population health improvement urgently needed for fairness and prosperity.
Supplementary Material
Acknowledgments
Partial funding was provided by a small grant from the Robert Wood Johnson Foundation Health and Society Scholars program and from the Center for Demography and Ecology at University of Wisconsin–Madison (NICHD P2C HD047873).
The authors thank Alberto Palloni for conversations about this research.
Footnotes
Reprints can be ordered at http://www.ajph.org by clicking the “Reprints” link
CONTRIBUTORS
D. Kindig participated in the concept, design, writing, and revision of the article. J. Nobles and M. Zidan participated in the concept, design, analysis, writing, and revision of the article.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not required, as only secondary data were used in this study.
Contributor Information
David Kindig, Department of Population Health Sciences, University of Wisconsin–Madison.
Jenna Nobles, Department of Sociology, University of Wisconsin–Madison.
Moheb Zidan, Department of Economics, University of Wisconsin–Madison.
References
- 1.Institute of Medicine. For the Public’s Health Investing in a Healthier Future. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 2.National Research Council. International Differences in Mortality at Older Ages: Dimensions and Sources. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 3.Avendano M, Kawachi I. Why do Americans have shorter life expectancy and worse health than people in other high-income countries? Annu Rev Public Health. 2014;35:307–325. doi: 10.1146/annurev-publhealth-032013-182411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations. World Population Prospects 2012 Edition. Available at: https://esa.un.org/unpd/wpp. Accessed October 21, 2017.
- 5.Kontis V, Bennett JE, Mathers CD, et al. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389(10076):1323–1335. doi: 10.1016/S0140-6736(16)32381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verguet S, Jamison DT. Improving life expectancy: how many years behind has the USA fallen? A cross-national comparison among high-income countries from 1958 to 2007. BMJ Open. 2013;3(7) doi: 10.1136/bmjopen-2013-002814. pii: e002814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crimmins EM, Preston SH, Cohen B. Explaining Divergent Levels of Longevity in High-Income Countries. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 8.Dow WH, Rehkopf D. Socioeconomic gradients in health in international and historical context. Ann N Y Acad Sci. 2010;1186:24–36. doi: 10.1111/j.1749-6632.2009.05384.x. [DOI] [PubMed] [Google Scholar]
- 9.Ho JY. Mortality under age 50 accounts for much of the fact that US life expectancy lags that of other high-income countries. Health Aff (Millwood) 2013;32(3):459–467. doi: 10.1377/hlthaff.2012.0574. [DOI] [PubMed] [Google Scholar]
- 10.Martinson ML. Income inequality in health at all ages: a comparison of the United States and England. Am J Public Health. 2012;102(11):2049–2056. doi: 10.2105/AJPH.2012.300929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martinson ML, Teitler JO, Reichman NE. Health across the lifespan in the United States and England. Am J Epidemiol. 2011;173(8):858–865. doi: 10.1093/aje/kwq325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Hedel K, Avendano M, Berkman LF, et al. The contribution of national disparities to international differences in mortality between the United States and 7 European countries. Am J Public Health. 2015;105(4):e112–e119. doi: 10.2105/AJPH.2014.302344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woolf SH, Aron L, editors. US Health in International Perspectives: Shorter Lives, Poorer Health Committee on Population. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 14.Avendano M, Glymour MM, Banks J, Mackenbach P. Health disadvantage in US adults aged 50 to 74 years: a comparison of the health of rich and poor Americans with that of Europeans. Am J Public Health. 2009;99(3):540–548. doi: 10.2105/AJPH.2008.139469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palloni A, Yonker J. Is the US old-age mortality advantage vanishing? Popul Dev Rev. 2016;42(3):465–489. doi: 10.1111/j.1728-4457.2016.00157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Institute for Health Metrics and Evaluation. US data for download. 2015 Available at: http://www.healthdata.org/us-health/data-download. Accessed August 8, 2016.
- 17.Preston SH, Elo IT. Anatomy of a municipal triumph: New York City’s upsurge in life expectancy. Popul Dev Rev. 2014;40(1):1–29. doi: 10.1111/j.1728-4457.2014.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Preston SH, Stokes A, Mehta N, Cao B. Projecting the effect of changes in smoking and obesity on future life expectancy in the United States. Demography. 2014;51(1):27–49. doi: 10.1007/s13524-013-0246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dowd JB, Hamoudi A. Is life expectancy really falling for groups of low socio-economic status? Lagged selection bias and artefactual trends in mortality. Int J Epidemiol. 2014;43(4):983–988. doi: 10.1093/ije/dyu120. [DOI] [PubMed] [Google Scholar]
- 20.Guillot M, Canudas-Romo V. Revisiting life expectancy rankings in countries that have experienced fast mortality decline. In: Schoen R, editor. Dynamic Demographic Analysis. Heidelberg, Germany: Springer, Cham; 2016. pp. 51–67. [Google Scholar]
- 21.Wilmoth JR. The future of human longevity: a demographer’s perspective. Science. 1998;280(5362):395–397. doi: 10.1126/science.280.5362.395. [DOI] [PubMed] [Google Scholar]
- 22.Kindig DA, Cheng E. Even as mortality fell in most US counties, female mortality nevertheless rose in 42.8 percent of counties from 1992 to 2006. Health Aff (Millwood) 2013;32(3):451–458. doi: 10.1377/hlthaff.2011.0892. [DOI] [PubMed] [Google Scholar]
- 23.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr. 2011;94(3):726–734. doi: 10.3945/ajcn.111.018366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013;98(1):180–188. doi: 10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marczak L, O’Rourke K, Shepard D. Firearm deaths in the United States and globally, 1990–2015. JAMA. 2016;316(22):2347. doi: 10.1001/jama.2016.16676. [DOI] [PubMed] [Google Scholar]
- 28.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 29.Liu J, Calzavara L, Mendelsohn JB, et al. Impact evaluation of a community-based intervention to reduce risky sexual behaviour among female sex workers in Shanghai China. BMC Public Health. 2015;15:147. doi: 10.1186/s12889-015-1439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fanfair RN, Zaidi A, Taylor LD, Xu F, Gottlieb S, Markowitz L. Trends in seroprevalence of herpes simplex virus type 2 among non-Hispanic Blacks and non-Hispanic Whites aged 14 to 49 years—United States, 1988–2010. Sex Transm Dis. 2013;40(11):860–864. doi: 10.1097/OLQ.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 31.Institute for Research on Poverty. How many children are poor? 2016 Available at: http://www.irp.wisc.edu/faqs/faq3.htm#children. Accessed March 8, 2017.
- 32.Saez E, Zucman G. Wealth inequality in the United States since 2013: evidence from capitalized income tax data. Q J Econ. 2016;131(2):519–578. [Google Scholar]
- 33.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood) 2002;21(2):78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- 34.Kindig D, Lardinois N, Chattergee D. Can states simultaneously improve health outcomes and reduce health outcome disparities? Prev Chronic Dis. 2016 doi: 10.5888/pcd13.160126. epub ahead of print August 25, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kindig D, Mullahy J. Comparative effectiveness—of what? Evaluating strategies to improve population health. JAMA. 2010;304(8):901–902. doi: 10.1001/jama.2010.1215. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


