Abstract
Background
Top managers’ transformational leadership is associated with significant influence on subordinates. Yet little is known about the extent to which top managers’ transformational leadership influences middle managers’ implementation leadership and, ultimately, frontline staff delivery of evidence-based health care practices.
Purpose
To test a multilevel leadership model examining the extent to which top managers’ transformational leadership, as mediated by implementation leadership of middle managers (i.e. those who supervise direct clinical services), affects staff attitudes towards evidence-based practices (EBPs) and their implementation.
Methodology/Approach
We used data collected in 2013 from 427 employees in 112 addiction health services programs in Los Angeles County, California. We relied on hierarchical linear models with robust standard errors to analyze multilevel data, individuals nested in programs. We conducted two path models to estimate multilevel relationships with two EBPs: contingency management and medication-assisted treatment.
Results
Findings partially supported our theory-driven multilevel leadership model. Specifically, results demonstrated that middle managers’ implementation leadership mediated the relationship between top managers’ transformational leadership and attitudes towards EBPs. At the same time, they showed the mediated relationship for delivery of contingency management treatment was only marginally significant (standardized indirect effect = .006, bootstrap p =.091). We did not find a mediation effect for medication-assisted treatment.
Discussion
Findings advance leadership theory in health care highlighting the importance of middle managers’ implementation leadership in transmitting the influence of top managers’ transformational leadership on staff attitudes towards EBPs. The full path model shows the extent to which transformational leadership may influence staff implementation of innovative practices as mediated through staff attitudes towards EBPs and middle managers’ implementation leadership.
Practice Implications
Our findings have implications for developing a multilevel leadership approach to implementation in health care. Leadership development should build on different competencies based on managers’ level, but align managers’ priorities on the same implementation goals.
Keywords: leadership styles, transformational leadership, leadership, implementation, evidence-based practices
Successful implementation and sustainment of evidence-based practices (EBPs) is complex, requiring strategies and interventions at multiple levels of organizations (Aarons, Hurlburt, Horwitz, 2011). Leadership at different levels of management is one mechanism for implementing organizational change. Both top and middle managers in health care organizations are responsible for implementation outcomes and therefore central to the study of organizational behavior. Yet, much work is needed to understand the influence of leadership at different levels of management on improving EBP implementation (Aarons, Ehrhart, Farahnak, & Sklar, 2014). This study tests the relationship between top and middle-level management leadership influence on the implementation of EBPs in addiction health services (AHS) organizations.
To elucidate the relationship between leadership styles and implementation of EBPs to treat addiction, we examined the influence of both top managers’ transformational leadership (ability to inspire employees to follow a particular course of action) and middle managers’ implementation leadership (supporting staff in implementing EBPs) on counselors’ attitudes towards and delivery of two EBPs: contingency management treatment (CMT) and medication-assisted treatment (MAT). CMT is a psychosocial intervention typically used in addiction treatment. It is based on principles of behavior modification (e.g., clients receive a gift card for a clean drug test), and has demonstrated positive outcomes in meta-analyses (Prendergast, Podus, Finney, Greenwell, & Roll, 2006). In contrast, MAT relies on the use of pharmacotherapies (e.g. buprenorphine, vivitrol, and naloxone) to reduce craving or block effects for alcohol and illegal drugs. It has been shown to substantially improve treatment adherence and reduce substance use (Lussier, Heil, Mongeon, Badger, & Higgins, 2006). Although cost-effective and responsive to client service needs, these EBPs are not routinely delivered in addiction treatment programs (Volkow, Frieden, Hyed, & Cha, 2014). Less than thirty percent of treatment programs in the United States have implemented MAT, and less than half deliver CMT (Knudsen, Abraham, & Oser, 2011). Even where such treatments are implemented, they may be poorly or inconsistently delivered (Manuel, Hagedorn, & Finney, 2011; McGovern & Carroll, 2003).
Program factors such as funding resources, regulation, and professionalization contribute to implementation of new practices in AHS (D’Aunno, 2006). Still, there is a need to explore the influence of leaders in shifting counselors’ attitudes and implementation behaviors. Because most treatment programs are small, both top and middle managers may directly influence on counselors.
We focus on two questions. First, to what extent is top managers’ transformational leadership associated with middle managers’ leadership for EBP implementation? Second, to what extent does middle managers’ leadership for EBP implementation mediate the relationship between top managers’ transformational leadership and employee attitudes toward EBPs and implementation of CMT and MAT? Our analysis contributes to the literature on EBP implementation, expanding understanding of the role of multilevel leadership in AHS organizations.
Theoretical Framework and Hypotheses
Foundational theories of implementation effectiveness highlight the role of top managers in establishing implementation policies and practices (Klein & Sorra, 1996). However, emerging research suggests that top managers’ transformational leadership behaviors are necessary to ensure the implementation of policies and practices (Guerrero & Kim, 2013). While a number of studies squarely focus on the role of middle managers (Aarons, Ehrhart, Farahnak, Hurlburt, 2015), the implementation literature would benefit from greater attention to the complexity of multilevel leadership and the role of middle managers play in the implementation process (Birken et al., 2012; Engle et al., 2016).
Top Managers’ Transformational Leadership
Effective transformational leaders rely on communicating their values, goals and vision, and on building on the strengths of individuals in their organization so as to influence their followers’ decision making and behaviors (Bass, Avolio, Jung, & Berson, 2003). Top managers enacting transformational leadership can influence employee attitudes toward, adoption and implementation of, and use of innovations in addiction health services (D’Aunno, 2006; Guerrero, Padwa, Fenwick, Harris, & Aarons, 2016). Leadership influence on staff behaviors can occur through leader attitudes, priorities, role modeling, and allocation of resources and rewards (Hernandez, Eberly, Avolio, & Johnson, 2011; Schein & Schein, 2017). In particular, transformational leaders’ promotion of employees’ professional growth is an active component to gaining the trust of employees and their endorsing a leader’s vision (Hernandez et al., 2011) for example, on the implementation of EBPs. We suggest that in behavioral health services top managers’ transformational leadership creates buy-in for implementation through middle managers’ promotion of professional growth. In communicating their vision, top managers also influence middle managers’ implementation leadership. Thus, we posit in Hypothesis 1: Transformational leadership will be positively related to middle managers’ implementation leadership of EBPs.
Middle Managers’ Leadership for Implementation of EBPs
We draw from Birken and colleagues’ (2012) theory on middle-managers’ role in implementation of health care practices to advance understanding of the role of middle managers’ implementation leadership in addiction health services. Emerging evidence suggests that middle managers’ commitment to implementation comes from policies and practices enacted by top managers (Birken et al., 2015). Middle managers rely on several activities, such as communication, training, coaching, and encouragement (Engle et al., 2016), that fall in the domains of tasks, relations, and change behaviors to support the implementation of health care practices (Birken et al., 2012).
We consider these managerial behaviors embedded in an implementation leadership approach that is proactive, knowledgeable, supportive, and perseverant. Proactive leadership involves planning and problem-solving to accomplish implementation. Knowledgeable leadership is connected to the authority of knowledge about an innovation and its implementation needs. Supportive leadership is necessary to recognize, appreciate, and guide employee implementation efforts. Perseverant leadership challenges leaders to persist through challenges and address issues that may cause the implementation process to falter. Together, these four categories of leadership are connected to research outlining how managers execute tasks, lead relations, and change behavior to influence employee attitudes and implementation behavior.
Implementation requires expert-based influence directed toward specific tasks. Meaningful interactions are also necessary for first-level leaders (those who supervise employees providing direct services) to influence employees to deliver products and services and support organizational priorities (Priestland & Hanig, 2005). One of the main mechanisms middle managers use to support implementation is effectively communicating, integrating, interpreting, and synthesizing facts and issues relevant for strategic initiatives such as EBP implementation (Birken et al., 2015). Zohar and Luria (2004) highlight that managers rely on cognitive attention and communication to support implementation.
Middle managers may rely on three attributes of leadership behavior to communicate priorities: pattern orientation, variability, and simplicity. Pattern orientation refers to communicating a priority relative to other competing interests (e.g., implementation of an evidence-based practice over other issues). Pattern variability refers to the consistency of leader behavior in communicating a priority over time and among different employees (e.g. being consistent in communicating implementation priorities and consistent across different actors). Pattern simplicity is the number of contingencies that influence a priority.
Consistent with leadership for implementation of EBPs, managers who prioritize implementation and use innovations may communicate a priority by developing strategic goals and plans that support innovation implementation. These managers also allocate resources for the innovation, providing supervision and coaching on how to use it. They also persevere in the face of challenges to implementation, and reward employees based on innovation use (Engle et al., 2016). Communication that implementation is a priority at all times is a key leadership approach for influencing implementation-related attitudes and behaviors among employees (Schein & Schein, 2017). Communication with employees must come from middle managers, while top managers must influence employees to change attitudes and buy into overall implementation attitudes and efforts.
Top and Middle Management Leadership and Staff Attitudes towards and Delivery of EBPs
The relationship between transformational leadership and delivery of EBPs have been tested in behavioral health, substance abuse treatment (Aarons, Ehrhart, Torres, Finn, & Roesch, 2016; Guerrero, He, Kim & Aarons, 2014) and mental health treatment. Because EBPs in social services are considered to be “soft technologies,” they are especially vulnerable to the attitudes of users. Attitudes link leadership style and employee behavior (Avolio, Gardner, Walumbwa, Luthans, & May, 2004), with transformational leadership being associated with employee attitudes toward EBPs. This relationship has in turn been associated with interest in and more frequent use of EBPs (Henggeler et al., 2007). Yet there has been limited research in human services on the relationship between transformational and implementation leadership and employee attitudes and, in turn, implementation behaviors.
Influence across levels of the organization is generally driven by social exchange across individuals with different roles, status, competencies, and responsibilities (Gottfredson & Aguinis, 2017). We argue that implementation leadership, which is best evaluated at the level of managers who have direct supervision of and interaction with implementers (Guerrero, Aarons, et al., 2016; Priestland & Hanig, 2005) mediate the relationship between top managers’ transformational leadership and implementation outcomes. We propose that the cascading influence of multilevel leadership, from top managers to middle managers and from middle managers to employee attitudes and behaviors, can be explained by social learning theory.
Social learning theory posits that individuals learn from observing and interacting with desirable role models (Bandura, 1986). Role-modeling, teaching, and coaching are aspects of leadership that facilitate communication about the importance of a strategic initiative (Schein & Schein, 2017). Because organizational leaders are typically viewed as role models, a top manager’s leadership behavior can influence the attitudes and behaviors of middle managers. Middle managers, in turn, may influence the attitudes and behaviors of lower-level employees, thereby generating congruent values across organizational levels. Empirical research has documented this trickle-down or cascading effect of leadership (Mayer, Kuenzi, Greenbaum, Bardes, & Salvador, 2009).
Managerial support and attitudes toward an innovation also affect staff at each phase of the implementation process (Damschroder et al., 2009). This suggests that values, attitudes, and behaviors specific to implementation also have a cascading effect. This reasoning leads to Hypothesis 2: Top managers’ transformational leadership will be indirectly related to employee attitudes toward EBPs through middle managers’ implementation leadership.
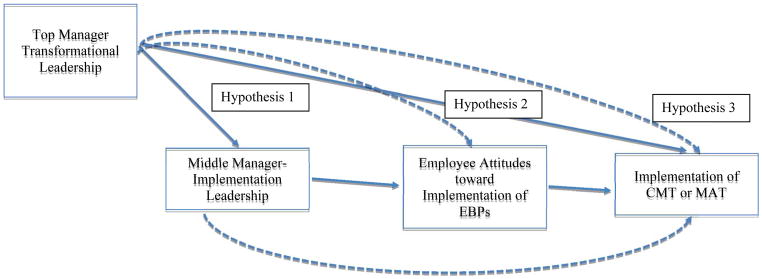
Researchers have sought to clarify the relationships among different conceptualizations of leadership and how they may operate simultaneously in an organization to influence front line workers’ performance (Avolio et al., 2004). Some research has explored how specific leadership approaches and organizational conditions mediate transformational leadership and organizational performance (Saboe, Taing, Way, & Johnson, 2015). For example, leader prioritization of safety moderated the effect of transformational leadership on employee safety practices (Zohar, 2002). Going beyond the dyadic leader–member exchange (Schein & Schein, 2017), we consider the relationship among three main actors (top manager, middle manager and counselor) in the implementation process. As previous studies show that transformational leadership is associated with employee attitudes toward EBPs and that higher support for EBPs is associated with their more frequent use (Henggeler et al., 2007), we posit Hypothesis 3: Top managers’ transformational leadership will be indirectly related to CMT and MAT implementation through middle managers’ implementation leadership.
Method
Sample and Data Collection
Data from the current study was collected as part of a larger longitudinal study. The sampling frame considered 408 AHS programs funded by a public health department in Los Angeles County between July 1, 2013, and December 31, 2013. Sampling relied on the random selection in 2010 of 147 outpatient programs from a total of 350 programs located in racial and ethnic minority communities. The current study relied on survey data from the second wave (2013) of the study, when all relevant variables were introduced and collected from an average of three direct-service providers per program (one supervisor and two counselors). The final analytic sample featured 112 programs and 427 participants, an average of 3.8 participants per program (108 top managers, 67 middle managers, 252 employees). Forty percent of participants were male and the full sample reported an average age of 47 years. Managers were primarily African American (45%) or Latino (32%), as were counselors (43% African American, 47% Latino). A full description of the sample and procedures is provided elsewhere (Guerrero, Fenwick, Kong, 2017).
Measures
Dependent variables
We analyzed three outcomes: attitudes towards EBPs, implementation of CMT, and implementation of MAT. We measured attitudes towards EBPs using the Evidence-Based Practice Attitude Scale (EBPAS; Aarons et al., 2010). The EBPAS is a 15-item measure with four subscales to assess attitudes related to openness to new practices (four items), requirements to adopt new practices (i.e., regulation; three items), appeal of EBPs (four items), and divergence (i.e., perceived difference between usual practice and EBPs; four items) (Aarons et al., 2010). All items were rated using a five-point Likert scale (1 = not at all to 5 = to a very great extent). The divergence subscale items were reverse-coded to be consistent with other subscales. Higher scores indicated more positive attitudes towards EBPs among counselors. Cronbach’s alpha for attitudes toward EBPs was .82.
The EBP implementation outcomes included delivery of CMT and MAT. Employees indicated the frequency with which they used each of these in their program. Measures were rated on a five-point Likert scale (1 = never to 5 = always) to represent degree of implementation, consistent with other studies (Guerrero et al., 2014). To represent implementation, we dichotomized these two measures by selecting 4 (often) and 5 (always) equal to 1 (i.e., good to excellent implementation), with responses equal to 1, 2, or 3 coded as 0 (i.e., no or poor implementation). Table 1 describes statistics for our measures and correlations among them.
Table 1.
Program characteristics and correlations, N=427 participants
| % or M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1. CMT | 49.5 | |||||||
| 2. MAT | 22.3 | .2801 | ||||||
| 3. Transformational leadership | 39.5 (4.9) | .0517 | −.0286 | |||||
| 4. Implementation leadership | 3.9 (0.8) | .0602 | −.1296 | .3153 | ||||
| 5. EBP attitudes | 37.4 (5.1) | .1705 | .0390 | −.0429 | .2051 | |||
| 6. Public funding | 67.9 (34.3) | −.0073 | −.1117 | −.0893 | .0159 | .1108 | ||
| 7. Graduate employees | 21.6 (18.3) | .1508 | .1778 | .0324 | .0431 | .1279 | .0458 | |
| 8. Accreditation | 32.7 | .0419 | .1285 | .0409 | −.1303 | −.0011 | −.1386 | −.0564 |
Note. Figures in bold are statistically significant at p < .05. CMT, contingency management treatment; EBP, evidence-based practice; MAT, medication-assisted treatment.
Independent variables
Our main independent variables were transformational leadership and implementation leadership for EBPs. Transformational leadership was reported by middle managers and counselors using a seven-item measure that rated top managers’ transformational leadership qualities on a five-point scale (1 = strongly disagree to 5 = strongly agree) (Edwards, Knight, Broome, & Flynn, 2010). Items included questions such as “leads by example,” “inspires others with his/her plans for this facility for the future,” and “takes time to listen carefully to and discuss people’s concerns.” Scores were totaled with higher scores representing employee perception of greater transformational leadership by top managers (Edwards et al., 2010). This measure has been validated in several studies of behavioral health settings (Guerrero, Aarons et al., 2016; Guerrero et al., 2015). Cronbach’s alpha for transformational leadership was .92.
We assessed middle managers’ leadership for EBP implementation using the Implementation Leadership Scale (ILS). Counselors responded to a brief 12-item measure with excellent reliability and validity that has been recently validated in AHS settings (Aarons et al., 2016). Counselors rated behavior of middle managers on four subscales—proactive, knowledgeable, supportive, and perseverant leadership—using a 5-point scale (0 = strongly disagree to 4 = strongly agree). These anchors were included to the original measure to be consistent with other measures in this study. Example items for each subscale were: Proactive - “developed a plan to facilitate EBP implementation;” Knowledgeable - “is able to answer employee questions about EBP;” Supportive - “supports employee efforts to use EBP;” and Perseverance - “reacts to critical issues regarding implementation of EBP.” We computed mean scores for each subscale and overall scores as suggested by the measure’s authors. Higher scores represented increased focus of middle managers on EBP implementation as perceived by program counselors. Cronbach’s alpha for this measure in the current study was .96.
Control variables (i.e., covariates)
Our control variables included regulation, public funding, and professionalization. We included two regulation measures that asked whether the program had a state license and accreditation by The Joint Commission. The public funding measure is the percentage of public revenue in each program’s budget for the past fiscal year. The professionalization measure is the percentage of employees in the organization with a graduate degree. Prior studies of implementation of new practices in AHS have used these variables to depict the context of implementation (D’Aunno, 2006).
Statistical Analysis
Guided by established procedures in organizational research (Glisson & James, 2002), we followed three steps to test our analytical models, which led to a path analysis using simultaneous equations. First, we used rWG to test the level of agreement within members of each of the 112 treatment programs on the leadership scales (James, Demaree, & Wolf, 1993). This within-program approach informs the extent to which individual responses can be aggregated to represent unit level program measures. Second, we relied on eta-squared via analysis of variance and an intraclass correlation coefficient via hierarchical linear modeling to test differences between programs for each construct. We considered both within-group consistency and between-group differences to determine our use of aggregated measures.
Finally, we ran the aggregated measures in two path-analysis models, one for each outcome (i.e., CMT and MAT). Hence, we used hierarchical linear modeling with robust standard errors to analyze multilevel data, individuals nested in programs (Bryk & Raudenbush, 1992). We conducted a Sobel test for indirect effects on each outcome to validate results. The two path models featured a random-intercepts model to estimate cross-level relationships between program-level variables and individual-level EBPs.
Results
Within- and Between-Group Consistency Analysis
Means, standard deviations, and correlations among study variables are reported in Table 1. Half of the respondents reported high implementation of CMT; less than 25 percent reported implementing MAT. There was a strong direct relationship between transformational leadership and implementation leadership (r = 0.315, p < .05). Implementation leadership was correlated with attitudes towards EBPs (r = 0.205, p < .05).
We computed indexes of within- and between-group consistency of responses for the EBP leadership implementation measure. The consistency of within-group responses and between-group differences justified composing the measure of middle managers’ implementation leadership. The within-group value averaged .66, the between-group value averaged .82. These values indicate high within-group consistency of responses. The Type 1 intraclass correlation coefficient value was .09 overall, showing that a significant proportion of the total variance in responses to each measure was explained by program membership. These results justify aggregation to the unit level. We used this program measure as a mediator in the proposed path analyses.
Path Analysis: Hypotheses Testing
We found support for Hypothesis 1. Transformational leadership was positively related to middle managers’ implementation leadership (standardized direct effect = .173, bootstrap p = .034). See Table 2 for path analysis results.
Table 2.
Multilevel Mediation Logistic Models of Implementation Leadership of EBPs, Employee Attitudes towards EBPs, CMT, and MAT as Outcomes, N=427 participants
| Coeff. | SE | 95% CI | p | |
|---|---|---|---|---|
| Implementation leadership of EBPs | ||||
| Transformational leadership | 0.050 | 0.011 | 0.028, 0.072 | .000 |
| Public funding | 0.001 | 0.001 | −0.002, 0.003 | .611 |
| Graduate employees | 0.001 | 0.003 | −0.005, 0.007 | .716 |
| Accreditation | −0.243 | 0.105 | −0.448, −0.038 | .020 |
| Attitudes towards EBPs | ||||
| Implementation leadership of EBPs | 1.809 | 0.638 | 0.559, 3.059 | .005 |
| Transformational leadership | −0.173 | 0.081 | −0.332, −0.014 | .034 |
| Public funding | 0.013 | 0.014 | −0.013, 0.040 | .329 |
| Graduate employees | 0.049 | 0.021 | 0.008, 0.090 | .019 |
| Accreditation | 0.766 | 0.833 | −0.868, 2.399 | .358 |
| CMT | ||||
| Attitudes toward EBPs | 0.069 | 0.028 | 0.014, 0.123 | .013 |
| Transformational leadership | 0.079 | 0.031 | 0.019, 0.139 | .010 |
| Public funding | 0.002 | 0.005 | −0.007, 0.011 | .664 |
| Graduate employees | 0.015 | 0.007 | 0.002, 0.029 | .029 |
| Accreditation | 0.185 | 0.299 | −0.402, 0.771 | .537 |
| MAT | ||||
| Attitudes toward EBPs | −0.007 | 0.033 | −0.072, 0.059 | .837 |
| Transformational leadership | 0.014 | 0.048 | −0.080, 0.107 | .773 |
| Public funding | −0.005 | 0.005 | −0.015, 0.005 | .342 |
| Graduate employees | 0.033 | 0.012 | 0.009, 0.057 | .008 |
| Accreditation | 0.629 | 0.464 | −0.281, 1.539 | .175 |
Note. CI, confidence interval; Coeff, coefficient; CMT, contingent management treatment; EBP, evidence-based practice; MAT, medication-assisted treatment; SE, standard error.
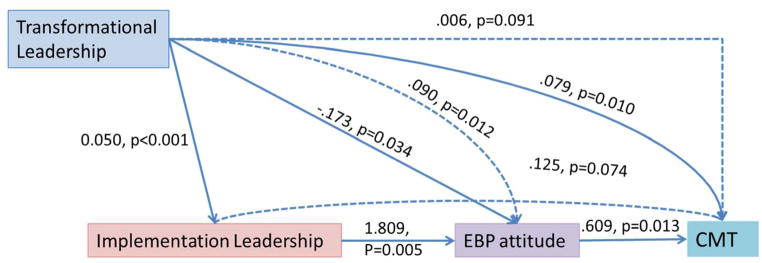
Hypothesis 2 was also supported. Transformational leadership was indirectly associated with employee attitudes toward EBPs via middle managers’ implementation leadership (standardized indirect effect = .090, bootstrap p = .012). See Figure 2 for path analysis results.
Figure 2.
Multilevel path analysis of transformational leadership, implementation leadership of EBPs, employee attitudes towards EBPs and program contingency management treatment, N=427 participants
Note. Control variables included public funding, percent of graduate employee, and program accreditation. Dotted lines represent indirect effects, whereas solid lines represent direct effects.
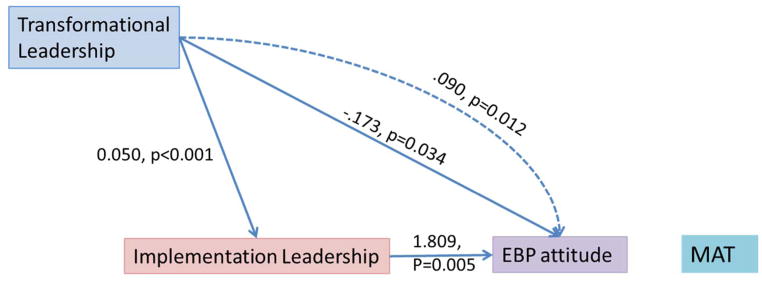
We did not find support for Hypothesis 3. Transformational leadership was indirectly associated with delivering CMT through middle managers’ implementation leadership, but only with marginal statistical significance (standardized indirect effect = .006, bootstrap p =.091). Findings did not support an indirect relationship between transformational leadership and implementation of MAT. See Figure 2 (CMT) and Figure 3 (MAT) for path analysis results.
Figure 3.
Multilevel path analysis of transformational leadership, implementation leadership of EBPs, employee attitudes towards EBPs and program medication assisted treatment, N=427 participants
Note. Control variables included public funding, percent of graduate staff, and program accreditation. Dotted lines represent indirect effects, whereas solid lines represent direct effects.
Most control variables were associated with mediators or outcomes. Most notable was the relationship between a program’s percentage of employees with graduate degrees and implementation of MAT. Overall, these two multilevel path analyses showed consistent and acceptable fit statistics (χ2 [131] = 180.49, CFI = .99, RMSEA = .03, SRMR = .03).
Discussion
The current study tested theory-driven hypotheses exploring multilevel leadership influences on EBP implementation. Results highlight the importance of middle managers’ implementation leadership in transmitting the influence of transformational leadership on employee attitudes toward innovative practices. Results also show a marginal relationship between transformational leadership and CMT implementation. The model captures the extent to which transformational leadership may shape attitudes and behaviors toward implementation of innovative practices as mediated through implementation leadership.
Our findings revealed important relationships among leadership style, middle manager’s implementation leadership, employee attitudes, and CMT implementation. Specifically, we found that transformational leadership had an indirect relationship with CMT implementation. The key mechanism by which top managers’ leadership play a role in CMT implementation was middle managers’ implementation leadership. The empirical examination of these relationships supported the role of focused leadership highlighted in emerging literature.
We did not find a significant mediational process for MAT implementation. This suggests that implementation of different practices may rely on different specific paths or may have different top or middle-management predictors. For example, relative to CMT, MAT is more costly and cumbersome, has different regulatory guidelines to dispense medication, different staffing structure (e.g., the need to hire medical doctors to supervise this practice), and ideological barriers to using a prescribed drug to treat addiction (Knudsen, Abraham, & Oser, 2011). Our findings suggest that differences in the nature of innovations being implemented may inform the ways in which leadership and organizational context are structured and ultimately tailored to support adoption and implementation.
Implications for Theory and Research
Few studies have investigated implementation from the perspective of multilevel-leadership influence. This study offers theoretical contributions to the literature regarding the importance of middle management EBP implementation leadership in enhancing the influence of top managers’ transformational leadership. Our primary contribution lies in providing empirical support for key aspects (implementation tasks, communicating implementation as a priority, and supporting change behavior) of the theory of the role of middle managers in health care implementation (Birken et al., 2012). The components of middle managers’ implementation leadership rely on implementation tasks, communicating implementation as a priority, and supporting change behavior to influence employee attitudes regarding EBPs. Our findings also build on and advance knowledge about how transformational leadership positively influences employee attitudes towards EBPs and EBP program delivery (Aarons et al., 2016; Guerrero et al., 2014).
Our results are consistent with other findings suggesting a trickle-down or cascading effect of leadership that operates through social learning (Mayer et al., 2009). Given the current strong emphasis on EBPs in health care, we expected that top managers valued EBPs and incorporated them into their organization’s vision and identity. We also expected that top managers with high transformational leadership consistently sought new opportunities to improve service quality by delivering EBPs. These managers successfully influence and motivate middle managers to similarly value EBP implementation (Birken et al., 2015). In turn, middle managers will be motivated to communicate the importance of EBP implementation to staff (Birken et al., 2012; Engle et al., 2016), who then model their middle manager’s implementation-related attitudes.
Our results also show how top management leadership influences employee attitudes and behavior through middle managers’ EBP implementation leadership. The literature suggests several explanations for this process. Top managers with high transformational leadership may set the tone regarding implementation as an organizational priority, then middle managers filter, interpret, and direct this information to employees (Engle et al., 2016) in such a way that top managers’ leadership indirectly affects employee attitudes and behavior (Birken et al., 2012; Mayer et al., 2009; Priestland & Hanig, 2005). Alternately, top managers with transformational styles might create a context that promotes employee growth, trust, and buy-in, and middle managers leverage this growth and buy-in toward implementation.
Implications for Practice
Our findings have several practical implications for strategic management and organizational development. Because middle managers’ EBP implementation leadership is associated with greater likelihood of implementation, leadership development initiatives can focus on structuring incentives and promoting communication and behaviors that are consistent with implementation goals. Staff attitudes and experience with EBPs which may enhance their future development should be emphasized during recruitment and promotion. Leaders should also establish professional development plans that include promoting and systematically measuring implementation attitudes and behaviors and use of measurement and feedback to improve the implementation processes. These strategies are consistent with creating an organizational context conducive to specific organizational norms and goals (Schein & Schein, 2017).
Leaders of treatment teams should establish a growth-promoting and implementation-focused model that guides, motivates, and supports employees to implement EBPs. Top managers should adopt a transformational leadership style and work with middle managers to demonstrate coherent alignment of implementation priorities. This should generate a cohesive leadership model that enables employees to enhance their implementation capacity. For example, the Leadership and Organizational Change for Implementation organizational intervention addresses top management buy-in and support coupled with first-level leader development. It uses Schein & Schein, 2017) notion of “embedding mechanisms” to positively influence employee attitudes and behaviors to support use of EBPs. This approach promotes a focused or strategic climate for implementation that signals to employees what is expected, supported, and rewarded regarding EBPs (Erhart, Torres, Wright, Martinez, & Aarons, 2016). Further exploration of the leadership-climate linkages for implementation and delivery of innovative practices in behavioral health services is emerging highlighting critical mechanisms of influence (Guerrero, Fenwick & Kong, 2017). Overall, these findings can inform current national and local efforts to train leaders on different competencies based on managers’ level, but align managers’ priorities on the same implementation goals to effectively improve standards of care.
Limitations and Conclusion
Our work has three main limitations. First, although we examined direct and indirect relationships, our results did not examine causal or temporal relationships, nor could we test a cascading effect with multiple respondents because our data were cross-sectional and featured one middle manager under a leader in top management. Second, our sample had an average number of three employees per workgroup to measure within-program agreement. Nevertheless, the health care programs included in the sample were typically small and independent units with shared work settings in which employees’ views of leadership likely coincide. Third, we measured implementation at the program level (delivery of CMT and MAT) rather than the direct behaviors of employees delivering these practices. Despite these limitations, our findings are based on strong estimates from a large number of program managers and employees serving a region with more than seven million residents.
This study contributes to the theoretical and empirical research on leadership and organizational studies on implementation by exploring the role of leadership at multiple organizational levels in the implementation of health care practices shown to be effective and beneficial to patients. Federal and private institutions have supported EBP implementation because of the need for patients to receive cost-effective and cutting-edge treatment (Institute of Medicine, 2001). We demonstrated that both top- and mid-level managers should aim to enact leadership behaviors supporting the implementation of innovative practices. We also highlighted the importance of testing implementation leadership as a mediator of influence on employees and service provision. Treatment staff at AHS organizations would benefit from targeted leadership strategies from their managers (Guerrero et al., 2016), as well as experience in quality improvement (Lukas et al., 2010) and other resources to effectively implement EBPs. Together, top and middle managers in AHS organizations can work to create an organizational leadership context that supports EBP implementation and with these efforts improve quality of care in AHS.
Figure 1.
Hypothesized Model
Note. Dotted lines represent indirect effects, whereas solid lines represent direct effects.
Acknowledgments
Funding for Erick G. Guerrero’s role in this study was provided by National Institute on Drug Abuse research (R01DA038608 and R33DA035634) and implementation fellowship training (R25MH080916) grants. Gregory A. Aarons’ participation was supported by National Institute of Drug Abuse (R01DA038466) and National Institute of Mental Health (R01MH072961 and R01MH092950) grants. Funders had no further role in study design; collection, analysis, and interpretation of data; writing of this report; or decision to submit for publication. We appreciate all participants who provided organizational data. We also thank Eric Lindberg, who assisted with the preparation and proofreading of the manuscript.
Footnotes
The authors declare no conflict of interests, financial or otherwise, and consent to publish this manuscript.
Contributor Information
Erick G. Guerrero, University of Southern California
Jemima Frimpong, John Hopkins University.
Yinfei Kong, California State University.
Karissa Fenwick, University of Southern California.
Gregory A. Aarons, University of California, San Diego
References
- Aarons GA, Ehrhart MG, Farahnak LR, Hurlburt MS. Leadership and organizational change for implementation (LOCI): a randomized mixed method pilot study of a leadership and organization development intervention for evidence-based practice implementation. Implementation Science. 2015;10(1):11. doi: 10.1186/s13012-014-0192-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Ehrhart MG, Farahnak LR, Sklar M. Aligning leadership across systems and organizations to develop strategic climate for evidence-based practice implementation. Annual Review of Public Health. 2014;35:255–274. doi: 10.1146/annurev-publhealth-032013-182447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Ehrhart MG, Torres EM, Finn NK, Roesch SC. Validation of the Implementation Leadership Scale (ILS) in substance use disorder treatment organizations. Journal of Substance Abuse Treatment. 2016;68:31–35. doi: 10.1016/j.jsat.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Glisson C, Hoagwood K, Kelleher K, Landsverk J, Cafri G. Psychometric properties and U.S. national norms of the Evidence-Based Practice Attitude Scale (EBPAS) Psychological Assessment. 2010;22:356–365. doi: 10.1037/a0019188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avolio BJ, Gardner WL, Walumbwa FO, Luthans F, May DR. Unlocking the mask: A look at the process by which authentic leaders impact follower attitudes and behaviors. Leadership Quarterly. 2004;15:801–823. doi: 10.1016/j.leaqua.2004.09.003. [DOI] [Google Scholar]
- Bandura A. Social foundations of thought & action. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bass BM, Avolio BJ, Jung DI, Berson Y. Predicting unit performance by assessing transformational and transactional leadership. Journal of Applied Psychology. 2003;88:207–218. doi: 10.1037/0021-9010.88.2.207. [DOI] [PubMed] [Google Scholar]
- Birken SA, Lee SY, Weiner BJ. Uncovering middle managers’ role in healthcare innovation implementation. Implementation Science. 2012;2(7):28. doi: 10.1186/1748-5908-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birken SA, Lee SYD, Weiner BJ, Chin MH, Chiu M, Schaefer CT. From strategy to action: how top managers’ support increases middle managers’ commitment to innovation implementation in healthcare organizations. Health care management review. 2015;40(2):159. doi: 10.1097/HMR.0000000000000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Aunno T. The role of organization and management in substance abuse treatment: Review and roadmap. Journal of Substance Abuse Treatment. 2006;31:221–233. doi: 10.1016/j.jsat.2006.06.016. [DOI] [PubMed] [Google Scholar]
- Edwards JR, Knight DK, Broome KM, Flynn PM. The development and validation of a transformational leadership survey for substance use treatment programs. Substance Use & Misuse. 2010;45:1279–1302. doi: 10.3109/10826081003682834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engle RL, Lopez ER, Gormley KE, Chan JA, Charns MP, Lukas CV. What roles do middle managers play in implementation of innovative practices? Health Care Manage Review. 2016;42(1):14–27. doi: 10.1097/HMR.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glisson C, James LR. The cross-level effects of culture and climate in human service teams. Journal of Organizational Behavior. 2002;23:767–94. [Google Scholar]
- Gottfredson RK, Aguinis H. Leadership behaviors and follower performance: Deductive and inductive examination of theoretical rationales and underlying mechanisms. Journal of Organizational Behavior. 2017;38:558–591. doi: 10.1002/job.2152. [DOI] [Google Scholar]
- Guerrero EG, Aarons GA, Grella CE, Garner BR, Cook B, Vega WA. Program capacity to eliminate outcome disparities in addiction health services. Administration and Policy in Mental Health and Mental Health Services Research. 2016;43:23–35. doi: 10.1007/s10488-014-0617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Fenwick K, Kong Y. Advancing theory development: Exploring the leadership-climate relationship as a mechanism of the implementation of cultural competence. Implementation Science. 2017;12:133. doi: 10.1186/s13012-017-0666-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero GE, Kim A. Organizational structure, leadership and readiness for change and the implementation of organizational cultural competence in addiction health services. Evaluation and Program Planning. 2013;40:74–81. doi: 10.1016/j.evalprogplan.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Guerrero EG, He A, Kim A, Aarons G. Organizational implementation of evidence-based substance abuse treatment in racial and ethnic minority communities. Administration and Policy in Mental Health and Mental Health Services Research. 2014;41(6):737–749. doi: 10.1007/s10488-013-0515-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Padwa H, Fenwick K, Harris LM, Aarons GA. Identifying and ranking implicit leadership strategies to promote evidence-based practice implementation in addiction health services. Implementation Science. 2016;11:69. doi: 10.1186/s13012-016-0438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Chapman JE, Rowland MD, Halliday-Boykins CA, Randall J, Shackelford J, Schoenwald SK. If you build it, they will come: Statewide practitioner interest in contingency management for youths. Journal of Substance Abuse Treatment. 2007;32:121–131. doi: 10.1016/j.jsat.2006.07.006. [DOI] [PubMed] [Google Scholar]
- Hernandez M, Eberly MB, Avolio BJ, Johnson MD. The loci and mechanisms of leadership: Exploring a more comprehensive view of leadership theory. Leadership Quarterly. 2011;22:1165–1185. doi: 10.1016/j.leaqua.2011.09.009. [DOI] [Google Scholar]
- Institute of Medicine. Crossing the quality chasm: A new health system for the twenty-first century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- James LR, Demaree RG, Wolf G. rwg: An assessment of within-group interrater agreement. Journal of Applied Psychology. 1993;78:306–309. doi: 10.1037/0021-9010.78.2.306. [DOI] [Google Scholar]
- Klein KJ, Sorra JS. The challenge of innovation implementation. Academy of management review. 1996;21(4):1055–1080. [Google Scholar]
- Knudsen HK, Abraham AJ, Oser CB. Barriers to the implementation of medication-assisted treatment for substance use disorders: The importance of funding policies and medical infrastructure. Evaluation and Program Planning. 2011;34:375–381. doi: 10.1016/j.evalprogplan.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukas CV, Engle RL, Holmes SK, Parker VA, Petzel RA, Seibert MN, … Sullivan JL. Strengthening organizations to implement evidence-based clinical practices. Health Care Management Review. 2010;35(3):235–245. doi: 10.1097/HMR.0b013e3181dde6a5. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Manuel JK, Hagedorn HJ, Finney JW. Implementing evidence-based psychosocial treatment in specialty substance use disorder care. Psychology of Addictive Behaviors. 2011;25(2):225. doi: 10.1037/a0022398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer DM, Kuenzi M, Greenbaum R, Bardes M, Salvador RB. How low does ethical leadership flow? Test of a trickle-down model. Organizational Behavior and Human Decision Processes. 2009;108:1–13. doi: 10.1016/j.obhdp.2008.04.002. [DOI] [Google Scholar]
- McGovern MP, Carroll KM. Evidence-based practices for substance use disorders. The Psychiatric Clinics of North America. 2003;26(4):991. doi: 10.1016/s0193-953x(03)00073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: A meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Priestland A, Hanig R. Developing first-level leaders. Harvard Business Review. 2005;83:112–120. [PubMed] [Google Scholar]
- Saboe KN, Taing MU, Way JD, Johnson RE. Examining the unique mediators that underlie the effects of different dimensions of transformational leadership. Journal of Leadership & Organizational Studies. 2015;22:175–186. doi: 10.1177/1548051814561028. [DOI] [Google Scholar]
- Schein EH, Schein P. Organizational culture and leadership. 5. San Francisco, CA: Jossey-Bass; 2017. [Google Scholar]
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies — tackling the opioid-overdose epidemic. New England Journal of Medicine. 2014;370:2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Zohar D. The effects of leadership dimensions, safety climate, and assigned priorities on minor injuries in work groups. Journal of Organizational Behavior. 2002;23:75–92. doi: 10.1002/job.130. [DOI] [Google Scholar]
- Zohar D, Luria G. Climate as a social-cognitive construction of supervisory safety practices: Scripts as proxy of behavior patterns. Journal of Applied Psychology. 2004;89:322–333. doi: 10.1037/0021-9010.89.2.322. [DOI] [PubMed] [Google Scholar]