Abstract
Background
The links between smoking, inflammation, and cardiovascular disease (CVD) are well-established. Several studies demonstrate that quitting smoking reverses the risk of coronary heart disease within five to ten years. However, the immediate effects of quitting smoking on inflammatory biomarkers associated with CVD risk are not well described.
Methods
In this pilot study, we examined a panel of circulating inflammatory biomarkers associated with CVD in ‘at risk’ women during the smoking cessation process. Forty-six women enrolled in a smoking cessation program consented to attend 4 study visits over 6–7 weeks. Health/medical information and blood was collected at each visit. Circulating levels of C-reactive protein (CRP), TNF, IL-6, soluble TNF receptors I and II, and soluble VCAM-1 were measured and changes between baseline levels (visit 1, while smoking) and visits 2–4 were determined.
Results
Significant reductions in circulating TNF, soluble TNF receptors I and II, and soluble VCAM-1 were observed among participants over the smoking cessation process. Both serum IL-6 and CRP levels declined during the smoking cessation process; however the changes were not statistically significant.
Conclusions
These findings suggest that there are rapid consequences of smoking cessation on inflammatory biomarkers in women at risk for CVD. Additional, larger studies including diverse smokers desiring to quit are required to confirm changes in ‘measurable milestones’ which could serve as motivating factors to assist smokers to quit.
Keywords: inflammatory biomarkers, smoking cessation, nicotine replacement therapy, nicotine, anti-inflammatory, cardiovascular disease
Introduction
Smoking promotes enhanced production of pro-inflammatory molecules by numerous cell types1–6 and contributes to systemic inflammation with elevated inflammatory biomarkers.7,8 Numerous studies have identified serum biomarkers (e.g. C-reactive protein (CRP), IL-6, TNF, soluble TNF receptors I and II (sTNFRI and sTNFRII)) that predict risk of chronic obstructive pulmonary disease (COPD)9–11 and cardiovascular disease (CVD).8,12–16 By contrast, smoking cessation is associated with improved COPD17 and CVD risk/mortality.18,19 However, it is not clear whether the benefits of quitting smoking are achieved immediately or require years.20,21 The purpose of this pilot study was to investigate the effect of quitting smoking on serum inflammatory biomarkers associated with CVD in women at risk for CVD during smoking cessation.
Methods and Materials
Subjects
Institutional Review Board approved this study and all subjects gave written informed consent prior to study procedures. Subjects were recruited from North Shore-LIJ Health System’s ‘Quit for Keeps’ smoking cessation program (a behavioral support program) between July 2005 and June 2007. Women smokers were enrolled if they were at risk for CVD, defined as having one or more of the following: abdominal obesity, elevated cholesterol, high blood pressure and/or history of heart disease, smoked ~1 pack of cigarettes/day for the past year (with exhaled carbon monoxide (CO) >15 ppm), were relatively healthy, and wanted to quit smoking. Subjects were excluded if taking anti-inflammatory agents (including oral corticosteroids), currently pregnant or trying to conceive, drinking beyond moderation, or using other tobacco products.
Study Design
Subjects consented to attend multiple visits that overlapped with the ‘Quit for Keeps Program’ (over 6–8 weeks, Table 1). At visit 1, subjects (n=46) were smoking and chose cessation aids (nicotine replacement therapy (NRT) and/or bupropion (Wellbutrin, GSK) – provided free) with trained nurses. Subjects completed questionnaires and the SF-36 form (physical and mental health assessment) at visits 1 and 3. Height, weight, body mass index (BMI), blood pressure, and smoking status (assessed using expired CO, serum cotinine levels, and self-report) were recorded at each visit. Visit 2 was within 24–72 hrs of their last cigarette (and 1 week after visit 1); visit 3 was 1–2 weeks after visit 2; and visit 4 was 3–5 weeks later. Peripheral blood was collected at each visit; serum was isolated, aliquoted and stored at −80°C until analyses of biomarkers and cotinine.
Table 1. Description of study visits for subjects attending smoking cessation program.
Study subjects (N) attended 4 study visits over a 6–7 week smoking cessation program. This table describes each study visit.
| Study Visit | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| N= | 46 | 42 | 39 | 36 |
| Smoking | + | 0 | 0 | 0 |
| Cessation Aids | 0 | + | + | + |
| Height | + | 0 | 0 | 0 |
| Weight | + | + | + | + |
| Blood Pressure | + | + | + | + |
| Exhaled CO | + | + | + | + |
| SF36 Form | + | 0 | + | 0 |
| Questionnaires | + | 0 | 0 | 0 |
| Review Smoking History | + | + | + | + |
| Review Medication History | + | + | + | + |
| Blood Collection | + | + | + | + |
denotes yes or assessed and 0 denotes no or not assessed.
Analysis of inflammatory biomarkers
Serum CRP levels were determined using ultrasensitive nephelemetry. Serum IL-6 and TNF levels were determined using high sensitivity ELISAs; serum sTNFRI, sTNFRII, and sVCAM-1 were determined by ELISAs (R&D Systems, Minneapolis, MN). All serum samples were analyzed in duplicate and samples for each subject (visits 1–4) were on the same plate with standards. The coefficients of variation for inter- and intra-assay variability for the inflammatory markers were between 1–5% and 2–8%, respectively.
Statistical Analyses
Statistics were analyzed using the SAS/PC statistical software package (version 9.1) (SAS Institute, Cary, NC).
Inflammatory markers
Repeated measures analysis of covariance (RMANCOVA), where time (visits 2, 3, and 4) was the within subjects effect (and there was no between subjects effect), was used to examine changes from baseline (at visit 1, while smoking) and visits 2–4 for all subjects who completed 4 visits. For each biomarker, the ratio of that marker to baseline was calculated, and then the log transformation was used to meet the assumptions of the RMANCOVA model. CO levels at each visit and BMI (at baseline) were included as covariates to control for potential effects on biomarkers. Exhaled CO was used as a surrogate marker for smoking status because it significantly associated with self-reported smoking (and NRT interfered with serum cotinine assays). To measure the degree of correlation between self-reported cigarettes/day and CO levels, the Spearman correlation coefficient was calculated for visits 2–4 (0.47 to 0.62). At visit 4 all subjects who reported not smoking exhaled ≤8ppm CO. Upon finding a significant effect of time on biomarker status, pair-wise comparisons of visits 2–4 were carried out (RMANCOVA). To determine whether the change from baseline was significant, the level of each marker at each visit was compared to baseline levels by testing whether the ratio of visit X:visit 1 differed from 1 using the t-test within the RMANCOVA model. For both comparisons, a Bonferroni adjustment was used, such that these comparisons were considered significant when p<0.0167. Additional models were examined (e.g. using serum cotinine levels as a surrogate for smoking instead of expired CO levels) and results did not differ qualitatively from the reported results.
Feelings of wellness (SF-36 form)
RMANCOVA, where visit was the ‘within subjects effect’ (and there was no ‘between subjects effect’) was used to examine the pattern of SF-36 scores during cessation. In addition, an RMANCOVA model was used to test for associations between each marker and SF-36 scores (total, physical and mental health scores). Baseline SF-36 scores (mental, physical, and total) for subjects who completed <4 visits were compared with those who completed 4 visits using the exact Mann-Whitney test.
Results
Characteristics of the study population
Of the 46 smoking female participants (average age=54.1±9.1), 36 (or 78.3%) completed 4 study visits and were included in the analyses. All subjects quit smoking at least 72 hrs prior to visit 2. Baseline characteristics are shown in Table 2. Baseline SF-36 scores for physical and mental health were 72.0 (±15.3, SD) and 72.5 (±13.9, SD), respectively and these values did not significantly change over the study. Many subjects had multiple risk factors for CVD (in addition to smoking) (Table 2). NRT (nicotine patch (14 or 21 mg), nicotine gum, nasal spray, inhalers, and lozenges (Cardinal Health, Dublin, OH)) and bupropion or NRT alone were used as smoking cessation aids (Fig. 1).
Table 2.
Baseline characteristics of the study population are shown as mean (SD) and median (IQR) (top half) and percent (lower half).
| N=36 | Mean (SD) | Median (IQR) |
|---|---|---|
| Age, yrs | 53.9 (9.1) | 54.4 (14.3) |
| BMI, lbs/in2 | 30.0 (5.8) | 29.4 (7.2) |
| Systolic blood pressure* | 130.2 (13.84) | 130.0 (19.0) |
| Diastolic blood pressure* | 77.5 (9.1) | 80.0 (12.0) |
| Cigarettes per day | 22.8 (5.7) | 20.0 (0.0) |
| Pack years | 39.0 (13.53) | 38.0 (14.0) |
| Total SF36 score | 74.4 (14.0) | 76.4 (20.4) |
| Physical health score | 72.0 (15.3) | 75.4 (25.8) |
| Mental health score | 72.5 (13.9) | 73.8 (22.6) |
| N=36 | Percent | |
|
| ||
| Ethnicity | ||
| Caucasian, % | 58 | |
| African American, % | 11 | |
| Hispanic, % | 3 | |
| Unknown, % | 28 | |
| CVD Risk factors | ||
| Elevated cholesterol, % | 61.1 | |
| Hypertension*, % | 36.1 | |
| Abdominal obesity, % | 19.4 | |
| Coronary artery disease, % | 13.9 | |
Subjects with high blood pressure were on anti-hypertensive medications.
Figure 1. Smoking cessation aids used by study subjects.
Most study subjects used nicotine replacement therapy (NRT, 97%), the majority of the individuals used NRT+bupropion (BUP), while 19% using NRT alone.
Approximately 85% of the subjects who completed 4 study visits quit smoking. Those who relapsed (15%) and continued in the study reported smoking fewer cigarettes; when these 6 subjects were excluded from the analyses, the results were similar to those observed for all subjects who attended 4 study visits. Several subjects (n=10) did not attend visit 4 due to relapse. Two differences were noted between subjects who did not complete 4 visits and those who did; women who completed ≤3 visits had (1) significantly lower quality of life (SF-36) scores (median (IQR) mental=61.8 (31.4) and total=62.6 (27.9)) than women who completed 4 visits (median (IQR) mental=73.8 (22.6) and total=76.4(20.4); p<0.01 and p<0.02, respectively); and (2) were less likely to use cessation aids.
Serum biomarkers associated with CVD decline during smoking cessation
Based on the evidence that circulating TNF is associated with cardiovascular mortality/risk 22,7 we examined serum TNF levels during smoking cessation. The average baseline serum TNF concentration (1.213 pg/ml±0.703) in our subjects was higher than TNF levels at later visits (Table 3). Overall, there was a decline in serum TNF over the course of smoking cessation among women at risk for CVD with a significant difference between circulating TNF observed at visits 2 and 3 (P<0.0115) (Table 3).
Table 3. Inflammatory Markers Before and After Smoking Cessation.
Baseline inflammatory marker levels and the mean percent changes in inflammatory markers between each study visit 2–4 (V2–V4) vs. baseline (V1) are shown with the level of significance.
| Marker | Baseline value (mean±SD) | Visit | Mean % change from baseline (95% CI) | Significance |
|---|---|---|---|---|
| TNF | 1.213 (0.703) pg/ml | V1 | 0 | |
| V2 | −14.5 (−49.8, 45.5) | |||
| V3 | −27.7 (−57.6, 23.0) | vs. V2, P<0.0115 | ||
| V4 | −20.2 (−53.1, 35.9) | |||
| sTNFRI | 2667.9 (1066.4) pg/ml | V1 | 0 | vs. V4, P<0.0001 |
| V2 | −3.0 (−7.9, 2.2) | vs. V4, P<0.01 | ||
| V3 | −3.9 (−8.7, 1.2) | vs. V4, P<0.0068 | ||
| V4 | −11.6 (−16.1, −7.0) | |||
| sTNFRII | 2395.1 (993.1) pg/ml | V1 | 0 | vs. V4, P<0.0048 |
| V2 | −10.4 (−18.9, −1.0) | vs. V4, N.S. | ||
| V3 | −3.2 (−12.3, 6.9) | vs. V4, P<0.0021 | ||
| V4 | −13.7 (−21.8, −4.7) | |||
| sVCAM-1 | 310.1 (119.3) ng/ml | V1 | 0 | vs. V4, P<0.0001 |
| V2 | −0.6 (−8.8, 8.3) | vs. V4, P<0.0001 | ||
| V3 | −4.1 (−11.9, 4.4) | vs. V4, P<0.0001 | ||
| V4 | −19.5 (−26.0, −12.3) | |||
| IL-6* | 3.314 (2.873) pg/ml | V1 | 0 | N.S. |
| V2 | 15.0 (−10.8, 48.4) | |||
| V3 | 0.7 (−21.8, 29.7) | |||
| V4 | −9.6 (−29.8, 16.4) | |||
| CRP* | 0.462 (0.519) mg/dL | V1 | 0 | N.S. |
| V2 | −46.5 (−75.7, 18.0) | |||
| V3 | −54.4 (−79.1, −0.3) | |||
| V4 | −19.1 (−63.0, 76.8) |
Pairwise comparisons of visits 2 through 4 were not carried out due to non-significant (N.S.) findings.
Circulating sTNFRI and sTNFRII are significantly predictive indicators of coronary heart disease in women.12 Steady declines in serum sTNFRI and sTNFRII were observed after quitting (p<0.0121 and p<0.0023, respectively, Table 3). Serum sTNFRI was lower at visit 4 than visits 1, 2 and 3 and the average sTNFRII level at visit 4 was significantly lower than visits 1 and 3 (Table 3). The average baseline serum sTNFRI concentration in our subjects (2667.9 pg/ml ±1066.4, SD) was higher than levels described for healthy women (1267 pg/ml±354), whereas the average baseline sTNRII level among our subjects (2395.1 pg/ml ±993.1, SD) was comparable to healthy controls.12
Endothelial cell activation is proposed to play a role in the development of coronary artery disease and smoking-induced endothelial cell dysfunction.14,23 We found a significant decrease in serum sVCAM-1, a marker of endothelial cell activation, after quitting smoking (p<0.0001). Serum sVCAM-1 levels were significantly lower at visit 4 than visits 1, 2 and 3 (Table 3).
While both serum IL-6 and CRP are considered predictors of cardiovascular events in some studies,12 others report either weak or no association between IL-6 and CRP values and CVD15,16 or CVD severity.24 In this study, we found an insignificant reduction in serum IL-6 and CRP levels during smoking cessation.
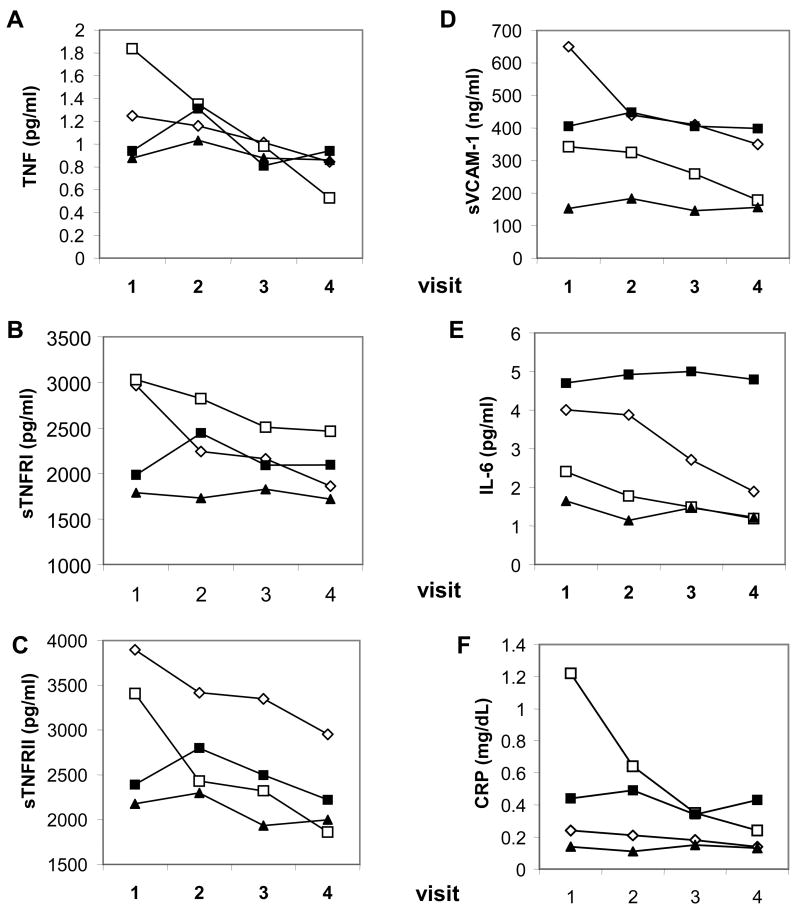
We observed variable responses among subjects. Some subjects showed steady declines in serum biomarkers over the course of smoking cessation (Fig. 2), while others exhibited either no pattern or no change in circulating biomarkers (Fig. 2).
Figure 2. Individual subject patterns of inflammatory mediators during the quit process.
Individual subject patterns of serum inflammatory mediators (associated with increased risk of CVD) during the smoking cessation process (visits 1–4) are shown for: (A) TNF; (B) sTNFRI; (C) sTNFRII; (D) sVCAM-1; (E) IL-6; and (F) CRP. Open symbols denote mediator values for individual subjects (taking NRT+bupropion) whose inflammatory mediators declined over the smoking cessation program; closed symbols denote values for individual subjects where no changes in inflammatory mediator levels were observed.
Discussion
Smoking has deadly consequences The long-term health benefits of smoking cessation for every age group are indisputable. The ultimate goal of smoking cessation programs is to assist smokers in quitting and remaining smoke-free. A very recent study reported that informing smokers of the ‘age and health’ of their lungs (based on spirometric assessment) significantly improved quit rates.25 We propose a similar program focused on improving cardiovascular health for smokers. In order to develop a smoking cessation program centered on a ‘healthy heart’, it is necessary to identify measurable early biomarkers (in men and women) associated with cardiovascular risk that are sensitive to change with smoking cessation. Once established, these biomarkers can be assessed before and during smoking cessation. Quantifiable information reflecting cardiovascular health may act as positive reinforcement for those trying to quit and remain smoke-free. Similarly, biomarkers (indicative of lung dysfunction) could be determined for smokers with compromised lung function to establish smoking cessation programs focused on ‘healthy lungs’.
Several studies report elevated inflammatory biomarkers among smokers vs. non-smokers.13,26,27 Others describe a decline in inflammatory biomarkers at some point after quitting smoking.21,28 Twenty years is required to reverse CRP, fibrinogen, and fibrin levels of smokers to levels found in non-smokers.21 Similarly, 10 years is required to observe a 50% reduction in inflammatory/haemostatic markers after quitting smoking.29 These improvements in biomarker scores translate to a decline in cardiovascular risks ranging between 5–10 years for reducing the risk of myocardial infarctions to that of non-smokers.30,31 Likewise, a recent report showed that women gained 61% of the full benefit of quitting smoking with regard to coronary disease mortality within 5 years of quitting.19
This is the first study to examine serum biomarkers associated with inflammation in women smokers at risk for CVD during smoking cessation. Based on our experience with smokers who complained of physical feelings that mimicked flu-like symptoms immediately after quitting, we hypothesized that smoking cessation might produce an initial spike in inflammatory markers (immediately after quitting) reminiscent of ‘serum-sickness’ with elevated circulating cytokines found after experimental administration of endotoxin. This undesirable physical feeling would be an obstacle to quitting. In several subjects, we observed a slight (insignificant) increase in biomarkers at visit 2 (compared to baseline). These data suggest that either: (a) there is no sharp inflammatory ‘peak’ after quitting; (b) the immediate rise was not found because blood was not sampled within a narrow time-frame of quitting; (c) NRT (used by 97%) blunted inflammatory responses; and/or (d) variable responses to smoking cessation occur and a much larger population is required to examine these variable responses.
We further hypothesized that an early spike would be followed by steady declines in circulating inflammatory mediators after quitting. This proposed decrease is based on previous reports showing that: smoking enhances systemic inflammation7,8, quitting is associated with declines in inflammatory biomarkers21,28, and that nicotine (used to relieve cravings) exerts anti-inflammatory effects in patients with ulcerative colitis32–34 and in experimental models of systemic inflammation (e.g. endotoxemia35, sepsis36, and ischemia37,38).
Based on data obtained from 36 subjects at risk for CVD who completed 4 visits, we found significant changes in serum TNF, sTNFRI, sTNFRII, and sVCAM-1 from baseline (Table 3). Although no significant changes in serum CRP and IL-6 levels were observed (Table 3), serum CRP levels declined slightly during smoking cessation. Our observations are consistent with a report showing that a significant reduction in serum CRP levels among heavy smokers following smoking cessation requires 5–9 years; 20 years are needed to reverse serum CRP to levels found among ‘never-smokers’.21 Together, these findings suggest that CRP, a stable downstream inflammatory marker, may not be useful as an ‘early milestone’ for smokers. CRP synthesis is determined by IL-6 and to a lesser extent by TNF39 which are elevated among smokers40,41 and have potential prognostic values in predicting cardiovascular health.42 We observed a significant decrease in serum TNF after quitting but no significant decline in IL-6 (Table 3).
The physiological response of circulating TNF is mediated through TNFRI and TNFRII which are shed from circulating leukocytes during inflammation. Soluble TNFRs, significant markers of coronary heart disease for women12, act as slow release reservoirs of bioactive TNF and extend its half-life.43 Thus, circulating sTNFR levels reflect a systemic pan-inflammatory state better than individual short-lived cytokines and should be better predictors of inflammation than TNF.43 Interestingly, a recent study implicates sTNFRI and sTNRII in the pathogenesis of COPD.44 Together with our observations, these findings suggest that quitting smoking could improve inflammatory responses systemically and within the lung.
Our quit rate was 65% and 83.3% among all subjects and subjects who completed visit 4, respectively. The major differences between subjects who completed 4 visits vs. ≤3 visits were their SF-36 scores and use of cessation aids. Our results suggest that higher mental and physical SF-36 scores are associated with a greater likelihood of attending classes, increased use of smoking cessation aids, and quitting smoking. Thus, smokers with low SF-36 scores may need additional support to quit or might want to postpone quitting until their SF-36 scores are elevated.
This study has several limitations. While it was designed and funded to be a pilot study enrolling women only, the most critical limitation was the small sample size. This, in part, was related to FDA approval of varenicline (Chantix, Pfizer) in May 2006. While we had a smaller than anticipated enrollment, most of our subjects (97%) used NRT and 78% of the subjects completed 4 visits. SF-36 scores did not change significantly with biomarkers during the smoking cessation program. While the SF-36 form is recommended for the assessment of general health45, a major disadvantage is that it may not be sensitive to short-term changes in feelings of wellness experienced by our subjects who were relatively ‘healthy’. In addition, the smokers might have reduced smoking prior to visit 1 and this might have reduced baseline values. Assessment of smoking status based on exhaled CO and self-report is another limitation. Serum cotinine was measured throughout the study, but values were confounded by NRT (and for ethical reasons subjects were encouraged to continue their NRT). It is important to note that variable responses in inflammatory markers were observed. Variability might be associated with: ethnicity, health status, quit aids (although 97% of our subjects used NRT), genetics, and age. Areas of future investigation include determining the sources of variability in inflammatory responses during smoking cessation and whether this variability influences successful long-term smoking cessation.
CVD is the most common cause of preventable death among adult Americans. Smoking as few as 1–4 cigarettes to one pack per day significantly increases the risk of fatal coronary heart disease by more than 2-fold and 5-fold, respectively.46 Each year more women die from CVD than men.47 Although numerous CVD risk factors have been identified, poor implementation of programs to reduce these risk factors in women is widely documented.48,49 Because of these factors and the reported gender differences in smoking cessation rates, with women having less success than men50,51, we included women at risk for CVD in our study.51 Thus, until a similar study can be repeated with a much larger, diverse population, our results can be only generalized to women at risk for CVD.
The development of successful smoking cessation programs for men and women is critical to reduce deaths associated with smoking. We propose the identification of a panel of inflammatory biomarkers that could be used as measurable milestones for quitters in a smoking cessation program focused on improving cardiovascular health for smokers at risk. This quantifiable information reflecting cardiovascular health may serve as positive reinforcement for those trying to quit smoking and remain smoke-free. Likewise, a panel of markers could be established for smokers with abnormal lung function.
Acknowledgments
Funding Sources
The work presented in this manuscript was the result of a Clinically Applied Research Grant awarded to CNM by the American Heart Association for improving cardiovascular risk in women through a smoking cessation program. In addition, CNM was funded by NIHRO1GM070727.
We acknowledge Dr. Martin Lesser for his assistance with statistical analyses.
Abbreviation list
- BMI
body mass index
- CVD
cardiovascular disease
- CO
carbon monoxide
- COPD
chronic obstructive pulmonary disease
- CRP
C-reactive protein
- ELISAs
enzyme-linked immunosorbent assays
- IQR
interquartile range
- NRT
nicotine replacement therapy
- RMANCOVA
repeated measures analysis of covariance
- sTNFRI
soluble TNF receptor I
- sTNFRII
soluble TNF receptor II
- sVCAM-1
soluble VCAM-1
Footnotes
Work was performed at: The Feinstein Institute for Medical Research and The Center for Tobacco Control
Summary of conflicts: All authors (VR, XX, DB, DJ, CF, PF, NK, AT, and CNM) have no conflicts to disclose.
References
- 1.Mochida-Nishimura K, Surewicz K, Cross JV, et al. Differential activation of MAP kinase signaling pathways and nuclear factor-kappaB in bronchoalveolar cells of smokers and nonsmokers. Mol Med. 2001;7(3):177–185. [PMC free article] [PubMed] [Google Scholar]
- 2.Mio T, Romberger DJ, Thompson AB, et al. Cigarette smoke induces interleukin-8 release from human bronchial epithelial cells. Am J Respir Crit Care Med. 1997;155(5):1770–1776. doi: 10.1164/ajrccm.155.5.9154890. [DOI] [PubMed] [Google Scholar]
- 3.Matsumoto K, Aizawa H, Inoue H, et al. Eosinophilic airway inflammation induced by repeated exposure to cigarette smoke. Eur Respir J. 1998;12(2):387–394. doi: 10.1183/09031936.98.12020387. [DOI] [PubMed] [Google Scholar]
- 4.Chalmers GW, MacLeod KJ, Thomson L, et al. Smoking and airway inflammation in patients with mild asthma. Chest. 2001;120(6):1917–1922. doi: 10.1378/chest.120.6.1917. [DOI] [PubMed] [Google Scholar]
- 5.Walters MJ, Paul-Clark MJ, McMaster SK, et al. Cigarette smoke activates human monocytes by an oxidant-AP-1 signaling pathway: implications for steroid resistance. Mol Pharmacol. 2005;68(5):1343–1353. doi: 10.1124/mol.105.012591. [DOI] [PubMed] [Google Scholar]
- 6.Barbieri SS, Weksler BB. Tobacco smoke cooperates with interleukin-1beta to alter beta-catenin trafficking in vascular endothelium resulting in increased permeability and induction of cyclooxygenase-2 expression in vitro and in vivo. FASEB J. 2007;21(8):1831–1843. doi: 10.1096/fj.06-7557com. [DOI] [PubMed] [Google Scholar]
- 7.Frohlich M, Sund M, Lowel H, et al. Independent association of various smoking characteristics with markers of systemic inflammation in men. Results from a representative sample of the general population (MONICA Augsburg Survey 1994/95) Eur Heart J. 2003;24(14):1365–1372. doi: 10.1016/s0195-668x(03)00260-4. [DOI] [PubMed] [Google Scholar]
- 8.Koenig W, Sund M, Frohlich M, et al. C-Reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99(2):237–242. doi: 10.1161/01.cir.99.2.237. [DOI] [PubMed] [Google Scholar]
- 9.Karadag F, Kirdar S, Karul AB, et al. The value of C-reactive protein as a marker of systemic inflammation in stable chronic obstructive pulmonary disease. Eur J Intern Med. 2008;19(2):104–108. doi: 10.1016/j.ejim.2007.04.026. [DOI] [PubMed] [Google Scholar]
- 10.Wouters EF, Groenewegen KH, Dentener MA, et al. Systemic inflammation in chronic obstructive pulmonary disease: the role of exacerbations. Proc Am Thorac Soc. 2007;4(8):626–634. doi: 10.1513/pats.200706-071TH. [DOI] [PubMed] [Google Scholar]
- 11.Groenewegen KH, Postma DS, Hop WC, et al. Increased systemic inflammation is a risk factor for COPD exacerbations. Chest. 2008;133(2):350–357. doi: 10.1378/chest.07-1342. [DOI] [PubMed] [Google Scholar]
- 12.Pai JK, Pischon T, Ma J, et al. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004;351(25):2599–2610. doi: 10.1056/NEJMoa040967. [DOI] [PubMed] [Google Scholar]
- 13.Wannamethee SG, Tchernova J, Whincup P, et al. Plasma leptin: associations with metabolic, inflammatory and haemostatic risk factors for cardiovascular disease. Atherosclerosis. 2007;191(2):418–426. doi: 10.1016/j.atherosclerosis.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Demerath E, Towne B, Blangero J, et al. The relationship of soluble ICAM-1, VCAM-1, P-selectin and E-selectin to cardiovascular disease risk factors in healthy men and women. Ann Hum Biol. 2001;28(6):664–678. doi: 10.1080/03014460110048530. [DOI] [PubMed] [Google Scholar]
- 15.Cesari M, Penninx BW, Newman AB, et al. Inflammatory markers and cardiovascular disease (The Health, Aging and Body Composition [Health ABC] Study) Am J Cardiol. 2003;92(5):522–528. doi: 10.1016/s0002-9149(03)00718-5. [DOI] [PubMed] [Google Scholar]
- 16.Tuomisto K, Jousilahti P, Sundvall J, et al. C-reactive protein, interleukin-6 and tumor necrosis factor alpha as predictors of incident coronary and cardiovascular events and total mortality. A population-based, prospective study. Thromb Haemost. 2006;95(3):511–518. doi: 10.1160/TH05-08-0571. [DOI] [PubMed] [Google Scholar]
- 17.Celli BR. Update on the management of COPD. Chest. 2008;133(6):1451–1462. doi: 10.1378/chest.07-2061. [DOI] [PubMed] [Google Scholar]
- 18.Mohiuddin SM, Mooss AN, Hunter CB, et al. Intensive smoking cessation intervention reduces mortality in high-risk smokers with cardiovascular disease. Chest. 2007;131(2):446–452. doi: 10.1378/chest.06-1587. [DOI] [PubMed] [Google Scholar]
- 19.Kenfield SA, Stampfer MJ, Rosner BA, et al. Smoking and smoking cessation in relation to mortality in women. JAMA. 2008;299(17):2037–2047. doi: 10.1001/jama.299.17.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ockene IS, Miller NH. Cigarette smoking, cardiovascular disease, and stroke: a statement for healthcare professionals from the American Heart Association. American Heart Association Task Force on Risk Reduction. Circulation. 1997;96(9):3243–3247. doi: 10.1161/01.cir.96.9.3243. [DOI] [PubMed] [Google Scholar]
- 21.Wannamethee SG, Lowe GD, Shaper AG, et al. Associations between cigarette smoking, pipe/cigar smoking, and smoking cessation, and haemostatic and inflammatory markers for cardiovascular disease. Eur Heart J. 2005;26(17):1765–1773. doi: 10.1093/eurheartj/ehi183. [DOI] [PubMed] [Google Scholar]
- 22.Van Den Biggelaar AH, De Craen AJ, Gussekloo J, et al. Inflammation underlying cardiovascular mortality is a late consequence of evolutionary programming. FASEB J. 2004;18(9):1022–1024. doi: 10.1096/fj.03-1162fje. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez MA, Selwyn AP. Endothelial function, inflammation, and prognosis in cardiovascular disease. Am J Med. 2003;115(Suppl 8A):99S–106S. doi: 10.1016/j.amjmed.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 24.Rifai N, Joubran R, Yu H, et al. Inflammatory markers in men with angiographically documented coronary heart disease. Clin Chem. 1999;45(11):1967–1973. [PubMed] [Google Scholar]
- 25.Parkes G, Greenhalgh T, Griffin M, et al. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ. 2008;336(7644):598–600. doi: 10.1136/bmj.39503.582396.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Madsen C, Nafstad P, Eikvar L, et al. Association between tobacco smoke exposure and levels of C-reactive protein in the Oslo II Study. Eur J Epidemiol. 2007;22(5):311–317. doi: 10.1007/s10654-007-9121-6. [DOI] [PubMed] [Google Scholar]
- 27.Lofdahl JM, Wahlstrom J, Skold CM. Different inflammatory cell pattern and macrophage phenotype in chronic obstructive pulmonary disease patients, smokers and non-smokers. Clin Exp Immunol. 2006;145(3):428–437. doi: 10.1111/j.1365-2249.2006.03154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hammett CJ, Prapavessis H, Baldi JC, et al. Variation in blood levels of inflammatory markers related and unrelated to smoking cessation in women. Prev Cardiol. 2007;10(2):68–75. doi: 10.1111/j.1520-037x.2007.05957.x. [DOI] [PubMed] [Google Scholar]
- 29.Negri E, La VC, D’Avanzo B, et al. Acute myocardial infarction: association with time since stopping smoking in Italy. GISSI-EFRIM Investigators. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto. Epidemiologia dei Fattori di Rischio dell’Infarto Miocardico. J Epidemiol Community Health. 1994;48(2):129–133. doi: 10.1136/jech.48.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dobson AJ, Alexander HM, Heller RF, et al. How soon after quitting smoking does risk of heart attack decline? J Clin Epidemiol. 1991;44(11):1247–1253. doi: 10.1016/0895-4356(91)90157-5. [DOI] [PubMed] [Google Scholar]
- 31.Heath and Human Services . The Health Benefits of Smoking Cessation. A Report of the Surgeon General. HHS, PHS, CDC, NCCDPHP, Office on Smoking and Health; 1990. [Google Scholar]
- 32.Pullan RD, Rhodes J, Ganesh S, et al. Transdermal nicotine for active ulcerative colitis. N Engl J Med. 1994;330(12):811–815. doi: 10.1056/NEJM199403243301202. [DOI] [PubMed] [Google Scholar]
- 33.Green JT, Thomas GA, Rhodes J, et al. Nicotine enemas for active ulcerative colitis--a pilot study. Aliment Pharmacol Ther. 1997;11(5):859–863. doi: 10.1046/j.1365-2036.1997.00220.x. [DOI] [PubMed] [Google Scholar]
- 34.Sandborn WJ, Tremaine WJ, Leighton JA, et al. Nicotine tartrate liquid enemas for mildly to moderately active left-sided ulcerative colitis unresponsive to first-line therapy: a pilot study. Aliment Pharmacol Ther. 1997;11(4):663–671. doi: 10.1046/j.1365-2036.1997.00208.x. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Liao H, Ochani M, et al. Cholinergic agonists inhibit HMGB1 release and improve survival in experimental sepsis. Nat Med. 2004;10(11):1216–1221. doi: 10.1038/nm1124. [DOI] [PubMed] [Google Scholar]
- 36.Huston JM, Ochani M, Rosas-Ballina M, et al. Splenectomy inactivates the cholinergic antiinflammatory pathway during lethal endotoxemia and polymicrobial sepsis. J Exp Med. 2006;203(7):1623–1628. doi: 10.1084/jem.20052362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bernik TR, Friedman SG, Ochani M, et al. Cholinergic antiinflammatory pathway inhibition of tumor necrosis factor during ischemia reperfusion. J Vasc Surg. 2002;36(6):1231–1236. doi: 10.1067/mva.2002.129643. [DOI] [PubMed] [Google Scholar]
- 38.Yeboah MM, Xue X, Duan B, et al. Cholinergic agonists attenuate renal ischemia-reperfusion injury in rats. Kidney Int. 2008;74(1):62–69. doi: 10.1038/ki.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yudkin JS, Kumari M, Humphries SE, et al. Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis. 2000;148(2):209–214. doi: 10.1016/s0021-9150(99)00463-3. [DOI] [PubMed] [Google Scholar]
- 40.Heinrich PC, Castell JV, Andus T. Interleukin-6 and the acute phase response. Biochem J. 1990;265(3):621–636. doi: 10.1042/bj2650621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zeidel A, Beilin B, Yardeni I, et al. Immune response in asymptomatic smokers. Acta Anaesthesiol Scand. 2002;46(8):959–964. doi: 10.1034/j.1399-6576.2002.460806.x. [DOI] [PubMed] [Google Scholar]
- 42.Valgimigli M, Ceconi C, Malagutti P, et al. Tumor necrosis factor-alpha receptor 1 is a major predictor of mortality and new-onset heart failure in patients with acute myocardial infarction: the Cytokine-Activation and Long-Term Prognosis in Myocardial Infarction (C-ALPHA) study. Circulation. 2005;111(7):863–870. doi: 10.1161/01.CIR.0000155614.35441.69. [DOI] [PubMed] [Google Scholar]
- 43.Aderka D. The potential biological and clinical significance of the soluble tumor necrosis factor receptors. Cytokine Growth Factor Rev. 1996;7(3):231–240. doi: 10.1016/s1359-6101(96)00026-3. [DOI] [PubMed] [Google Scholar]
- 44.D’hulst AI, Bracke KR, Maes T, et al. Role of tumour necrosis factor-alpha receptor p75 in cigarette smoke-induced pulmonary inflammation and emphysema. Eur Respir J. 2006;28(1):102–112. doi: 10.1183/09031936.06.00059305. [DOI] [PubMed] [Google Scholar]
- 45.Haywood KL, Garratt AM, Fitzpatrick R. Quality of life in older people: a structured review of generic self-assessed health instruments. Qual Life Res. 2005;14(7):1651–1668. doi: 10.1007/s11136-005-1743-0. [DOI] [PubMed] [Google Scholar]
- 46.Willett WC, Green A, Stampfer MJ, et al. Relative and absolute excess risks of coronary heart disease among women who smoke cigarettes. N Engl J Med. 1987;317(21):1303–1309. doi: 10.1056/NEJM198711193172102. [DOI] [PubMed] [Google Scholar]
- 47.Heron MP, Smith BL. Deaths: leading causes for 2003. Natl Vital Stat Rep. 2007;55(10):1–92. [PubMed] [Google Scholar]
- 48.Goff DC, Jr, Bertoni AG, Kramer H, et al. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006;113(5):647–656. doi: 10.1161/CIRCULATIONAHA.105.552737. [DOI] [PubMed] [Google Scholar]
- 49.Barnhart J, Lewis V, Houghton JL, et al. Physician knowledge levels and barriers to coronary risk prevention in women: survey results from the Women and Heart Disease Physician Education Initiative. Womens Health Issues. 2007;17(2):93–100. doi: 10.1016/j.whi.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 50.Bohadana A, Nilsson F, Rasmussen T, et al. Gender differences in quit rates following smoking cessation with combination nicotine therapy: influence of baseline smoking behavior. Nicotine Tob Res. 2003;5(1):111–116. doi: 10.1080/1462220021000060482. [DOI] [PubMed] [Google Scholar]
- 51.Perkins KA. Smoking cessation in women. Special considerations CNS Drugs. 2001;15(5):391–411. doi: 10.2165/00023210-200115050-00005. [DOI] [PubMed] [Google Scholar]