Abstract
Importance:
Acute kidney injury (AKI) is a common and serious complication for pediatric cardiac surgery patients associated with increased morbidity, mortality, and length of stay. Current strategies focus on risk reduction and early identification, as there are no known preventive or therapeutic agents. Cardiac surgery and cardiopulmonary bypass lyse erythrocytes, releasing free hemoglobin and contributing to oxidative injury. Acetaminophen may prevent AKI by reducing the oxidation state of free hemoglobin.
Objective:
To test the hypothesis that early postoperative acetaminophen exposure is associated with reduced risk of AKI in pediatric cardiac surgery patients
Design, Setting, and Participants:
In this retrospective observational study, the setting was 2 tertiary referral children’s hospitals. The primary and validation cohorts included children older than 28 days admitted for cardiac surgery between July 1, 2008 and June 1, 2016. Exclusion criteria were postoperative extracorporeal membrane oxygenation and inadequate serum creatinine measurements to determine AKI status.
Exposure:
Acetaminophen exposure in the first 48 postoperative hours
Main Outcome Measure:
AKI, based on Kidney Disease Improving Global Outcomes creatinine criteria (increase by 1.5-fold or 0.3 mg/dL), in the first postoperative week
Results:
The primary cohort (N=666) had a median age of 6.5 months [interquartile range 3.9–44.7 months], and 341 (51%) had AKI. In unadjusted analyses, those with AKI had lower acetaminophen doses than those without AKI [47 (16–88) vs. 78 (43–104) mg/kg, P<0.001]. In logistic regression analysis adjusting for age, cardiopulmonary bypass time, red cell distribution width, nephrotoxin exposures, hypotension, and Risk Adjustment for Congenital Heart Surgery score, acetaminophen exposure was protective for postoperative AKI [odds ratio 0.86 per 10 mg/kg, 95% confidence interval (0.82–0.90)]. Findings were replicated in the validation cohort [N=333; age 14.1 (3.9–158.2) months; 162 (48.6%) with AKI; acetaminophen dose 60 (40–87) vs. 70 (45–94) mg/kg in AKI vs. no AKI, P=0.033; adjusted odds ratio 0.91 (95% confidence interval 0.84–0.99) for each additional 10 mg/kg].
Conclusions and Relevance:
The results indicate that early postoperative acetaminophen exposure may be associated with lower rate of AKI in pediatric patients who undergo cardiac surgery. Further analysis to validate these findings, potentially through a prospective, randomized trial, may establish acetaminophen as a preventive agent for AKI.
Introduction
Acute kidney injury (AKI) occurs in approximately 25% of children admitted to intensive care units (ICUs).1–9 Among pediatric ICU patients, AKI is associated with increased length of stay and consistently demonstrates odds ratios >3 for mortality.1,2,8–12 Rates of AKI among children who have cardiac surgery are even higher, with similar associations to increased morbidity, mortality, and length of stay.13–26 Currently, efforts to reduce the impact of AKI in pediatric patients are focused on early detection and risk reduction, as there are no proven therapeutics to prevent or treat AKI.
For children who undergo cardiac surgery, the necessary cardiopulmonary bypass (CPB) causes hemolysis; which together with the tissue damage from surgery and administration of packed red blood cells leads to relatively high circulating levels of free hemoglobin in these patients.27,28 Cell-free plasma hemoglobin has been associated with AKI after cardiac bypass in children.29 Based on data from animal models and adults, it is hypothesized that free hemoglobin contributes to AKI through oxidation of the central iron of the heme moiety to the highly reactive and nephrotoxic ferryl (Fe4+) form.30–32 This pathogenic mechanism for AKI illuminates a potential therapeutic agent. Acetaminophen, a well-established drug used for analgesia and fever reduction, is known to reduce oxidation of free hemoglobin by preventing the oxidation of iron from Fe3+ to Fe4+.32,33 The hemoreductant activity of acetaminophen derives from the structural similarity between the heme moiety of hemoglobin and the peroxidase moiety of cyclooxygenase. In recent years, acetaminophen has been increasingly used postoperatively in children in order to reduce opioid exposure.
The primary goal of this study was to test the hypothesis that acetaminophen use in the first 48 hours after cardiac surgery is associated with reduced risk of AKI in children. To test this hypothesis, we performed a retrospective observational study of children who had cardiac surgery in a primary cohort from the Monroe Carell Jr. Children’s Hospital at Vanderbilt, and we validated our findings in a second independent cohort from Duke Children’s Hospital.
Methods
Population and Electronic Health Record Data Extraction
This study was reviewed and approved by the institutional review boards of both Vanderbilt University Medical Center and Duke University. Inclusion criteria for the primary cohort were cardiac surgery at the children’s hospital between the dates of 3/1/2008 and 6/1/2016, and age over 28 days. Exclusion criteria were postoperative extracorporeal membrane oxygenation (as this may include renal replacement therapy and thus affect serum creatinine values) and absence of either the baseline or postoperative serum creatinine measurements to determine AKI status. If subjects had multiple cardiac surgeries, data from only the first surgery were included. After the primary cohort was analyzed, a second cohort was assembled to determine if the findings were unique to the institution, or if they could be replicated in an independent validation cohort. Inclusion criteria for the validation cohort were the same as for the primary cohort, with the exception that the study inclusion dates were 6/25/2013 to 3/29/2016. All study data, including demographic, laboratory, medication administration, and administrative data, were extracted from electronic health records data sources. Medications administered in the first 48 postoperative hours were categorized as high risk nephrotoxins (e.g. aminoglycosides, ketorolac, tacrolimus), moderate risk nephrotoxins, (e.g. loop diuretics, enalapril, trimethoprim/sulfamethoxazole, eTable1), or non-nephrotoxins. Postoperative hypotension was defined using the systolic blood pressure measurements documented in the first 48 postoperative hours, irrespective of any vasopressor support; hypotension was defined as one or more systolic blood pressure < [70mmHg + (2 x age in years)] if ≤10 years of age, and <90 mmHg if >10 years of age.34
Exposure and Outcome Definitions
Exposure was defined as dichotomous exposure to acetaminophen for the initial analysis, and then the cumulative weight-adjusted intravenous, enteral, and/or rectal acetaminophen dose (mg/kg), alone or in combination with other medications, received in the first 48 hours after surgery. Subjects were also categorized into those receiving no acetaminophen, or lowest (≤40 mg/kg), middle (40–80 mg/kg), or highest (>80 mg/kg) doses of acetaminophen. The AKI outcome was defined by change in creatinine. Baseline creatinine measurements were defined as the lowest obtained in the 28 days before surgery. Postoperative creatinine measurements were defined as those obtained in the 7 days after surgery. AKI was defined solely using the creatinine criteria, as reliable urine output data are not available for all pediatric inpatients,35 and accurate height measurements were not consistently available for pediatric inpatients for estimated glomerular filtration rate. Subjects were classified as having AKI using Kidney Disease Improving Global Outcomes (KDIGO) serum creatinine criteria if any postoperative creatinine measurement increased by ≥0.3 mg/dL from baseline (to convert to micromoles per liter, multiply by 88.4) or was ≥1.5-fold more than the baseline.7 Those not meeting these criteria were classified as no-AKI. AKI stage was determined for each AKI case, using serum creatinine based KDIGO definitions for Stage 1 (1.5-fold or 0.3 mg/dL increase), Stage 2 (2-fold increase), and Stage 3 (3-fold increase or creatinine ≥ 4 mg/dL) based on the highest creatinine measurement in the 7 days after surgery.
Statistical Analysis
Descriptive statistics were presented as median [interquartile range (IQR)] or frequency (%) as appropriate. Continuous variables were compared using the Wilcoxon rank-sum test and categorical variables using the Pearson chi-square test. The Kruskal-Wallis test was used to test weight-adjusted acetaminophen dose across AKI stage. We analyzed the association between AKI and dichotomous acetaminophen exposure using Pearson chi-square test. We also investigated the effect of acetaminophen dose (continuous variable, mg/kg) using logistic regression, after adjusting for pre-specified risk factors such as age, CPB time, red cell distribution width (RDW, given prior associations with AKI),36,37 nephrotoxin exposure, postoperative hypotension, and risk adjustment for congenital heart surgery (RACHS) score.38 The nonlinear effect of age was modeled using the restricted cubic spline with 3 knots chosen at the 10th, 50th, and 90th percentile. The same logistic regression model was used for both the primary and validation cohort. Subgroup analyses were also performed. First, logistic regression was performed as above for each cohort, excluding those individuals who had no acetaminophen exposure. In addition, a subgroup analysis was done by pooling individuals from both cohorts with RACHS score ≥3 as an alternative method to account for variability in clinical status after surgery and likely degree of cell-free hemoglobin. For this analysis, the same logistic regression was performed as above, with the inclusion of clinical site as an additional covariate. Sensitivity analyses of unmeasured confounding effects were also performed (see eAppendix). Multiple imputation was performed based on 10 completed datasets by applying predictive mean matching to handle missing data for the variables of RACHS score, RDW, and CPB time.39 All analyses were performed with the statistical programming language R, version 3.3.0 (R Development Core Team, Vienna, Austria). The statistical significance was determined at the level of 0.05, and all p-values were based on 2-sided tests.
Results
Study cohorts
The primary cohort included 666 subjects with baseline and postoperative serum creatinine measurements. Half were male, and half met criteria for AKI (Table 1). Of the 341 with AKI, 159 (47%) had Stage 1, 131 (38%) had Stage 2, and 51 (15%) had Stage 3 AKI. Those with AKI had more postoperative serum creatinine measurements than those without (8 [interquartile range (IQR) 4–7] vs. 5 [IQR 5–10]). Primary cardiac diagnoses are listed in eTable 2. The validation cohort comprised 333 individuals, with similar incidence of AKI (Table 1). Of the 162 with AKI, 51 (31%) had Stage 1, 91 (56%) had Stage 2, and 20 (12%) had Stage 3 AKI. Primary cardiac diagnoses for the validation cohort are listed in eTable 3.
Table 1.
Characteristics of the Primary and Validation Cohorts
| Primary Cohort (n=666) |
Validation Cohort (n=333) |
|
|---|---|---|
| Age (months) | 6.5 [3.9–44.7] | 14.1 [3.9–158.2] |
| Female Sex | 328 (49) | 172 (52) |
| Weight (kg) | 7.1 [5.0–14.6] | 9.2 [4.7–49.0] |
| Pre-Operative Baseline Serum Creatinine (mg/dL) |
0.35 [0.25–0.45] | 0.30 [0.20–0.60] |
| Post-Operative Peak Serum Creatinine (mg/dL) |
0.53 [0.45–0.66] | 0.50 [0.40–0.90] |
| RACHS Score* | ||
| 1 | 143 (22) | 88 (32) |
| 2 | 256 (40) | 112 (41) |
| ≥3 | 237 (37) | 73 (27) |
| CPB Time (min)** | 87 [59–122] | 95 [39–149] |
| AKI Outcome | ||
| No AKI | 325 (49) | 171 (51) |
| Stage 1 | 159 (24) | 51 (15) |
| Stage 2 | 131 (20) | 91 (27) |
| Stage 3 | 51 (8) | 20 (6) |
Median [Interquartile Range] for continuous variables; Frequency (%) for categorical variables
RACHS - Risk Adjustment for Congenital Heart Surgery, with scores available for n=636 in the primary cohort and n=273 in the validation cohort
CPB - Cardiopulmonary Bypass, with time available for n=665 in the primary cohort and all 333 of the validation cohort; AKI – Acute Kidney Injury. SI conversion factor: To convert creatinine to μmol/L, multiply by 88.4.
AKI and Acetaminophen
In the primary cohort, 72 (11%) of the cohort had no acetaminophen exposure in the first 48 hours after surgery. The incidence of AKI was higher among those with no acetaminophen exposure than among those who received acetaminophen (Figure 1A). Comparing those with and without AKI, those without AKI had significantly higher weight-adjusted acetaminophen dose in the first 48 hours after surgery compared to those with AKI (Table 2). Other variables significantly associated with AKI included younger age, longer CPB time, higher RDW, presence of hypotension, fewer high risk nephrotoxins, and higher RACHS score (Table 2). When stratified by AKI stage, those with no AKI had the highest median acetaminophen dose (78 [IQR 43–104] mg/kg), followed by those with stage 1 AKI (57 [IQR 17–100] mg/kg), stage 2 AKI (48 [IQR 28–78] mg/kg), and stage 3 AKI (31 [IQR 0–70] mg/kg, p<0.001 for difference in distribution across groups). Those with no acetaminophen exposure had the highest rates of AKI, with decreasing incidence in the lowest, middle, and highest acetaminophen dose groups (Figure 1B). In the logistic regression analysis adjusting for age, CPB time, RDW, hypotension, nephrotoxin exposure, and RACHS score, acetaminophen exposure was protective for postoperative AKI, with odds ratio 0.86 per 10 mg/kg (95% confidence interval (CI) 0.82–0.90, Figure 2). The relationship of continuous acetaminophen dose to adjusted odds for AKI is shown in Figure 3. The patients who did not receive acetaminophen were younger and had longer CPB times, higher RDW, and more hypotension than those who had acetaminophen exposure (eTable 4). When subset analysis of the primary cohort was performed excluding those with no acetaminophen exposure, acetaminophen remained protective against AKI (OR 0.85 per 10 mg/kg, 95% CI 0.80–0.90, p<0.001). Analysis of the sensitivity of our main findings to unmeasured confounding identified the joint minimum strength of association that an unmeasured confounder must have with acetaminophen exposure and AKI is >3.07 to make these findings statistically insignificant (eTable 5).
Figure 1. Incidence of AKI by Acetaminophen Exposure and Dose.
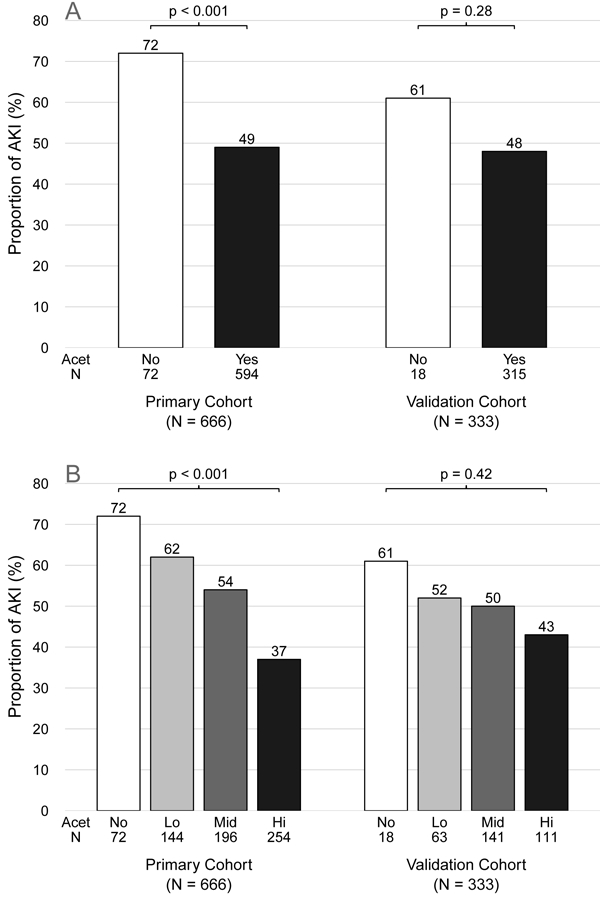
A) The incidence (%) of early postoperative AKI is shown for those administered no acetaminophen (white bars) or at least one dose of acetaminophen (black bars) in the first 48 hours after surgery. The primary cohort is shown on the left, and the validation cohort on the right. The number in each subset are indicated below each bar. P-values from Pearson chi-square test. B) The incidence (%) of early postoperative AKI is shown for those with no acetaminophen administered in the first 48 hours after surgery (white bars) and for lowest (Lo, ≤40 mg/kg, light gray), middle (Mid, 40–80 mg/kg, dark gray), and highest (Hi, >80 mg/kg, black) cumulative dose of acetaminophen in the first 48 hours after surgery. The number in each subset are indicated below each bar, and the percentage of those with AKI above each bar. P-values from Pearson chi-square test. AKI – Acute kidney injury. Acet – Acetaminophen.
Table 2.
Risk Factors for Acute Kidney Injury (AKI) in the Primary and Validation Cohorts
| Primary Cohort (n=666) |
Validation Cohort (n=333) |
|||||
|---|---|---|---|---|---|---|
|
No AKI (n=325) |
AKI (n=341) |
Unadjusted P-value |
No AKI (n=171) |
AKI (n=162) |
Unadjusted P-value |
|
| Acetaminophen Dose (mg/kg) |
78 [43–104] |
47 [16–88] |
<0.001 | 70 [45–94] |
60 [40–87] |
0.031 |
| Age (months) | 15.2 [4.5–70.9] |
5.5 [3.3–16.6] |
<0.001 | 39.8 [5.3– 203.9] |
6.7 [2.9–46.9] |
<0.001 |
| Female Sex | 171 (53) | 157 (46) | 0.09 | 95 (56) | 77 (48) | 0.14 |
| Weight (kg) | 9.2 [5.6–20.2] |
6.1 [4.7–9.3] |
<0.001 | 13.7 [5.3–62.0] |
6.5 [4.4–16.9] |
<0.001 |
| Baseline Serum Creatinine (mg/dL) |
0.43 [0.36– 0.52] |
0.26 [0.21– 0.34] |
<0.001 | 0.40 [0.30– 0.80] |
0.30 [0.20– 0.50] |
<0.001 |
| Peak Serum Creatinine (mg/dL) |
0.52 [0.44– 0.62] |
0.54 [0.45– 0.71] |
0.005 | 0.50 [0.40– 0.80] |
0.60 [0.50– 1.00] |
0.004 |
| CPB Time (min)* | 80 [51–111] |
99 [68–132] |
<0.001 | 85 [32–123] |
110 [41–170] |
0.011 |
| RDW (%)** | 13.2 [12.7– 14.4] |
14 [13.2– 15.3] |
<0.001 | 13.9 [13.2– 15.3] |
15.4 [14.2– 16.8] |
<0.001 |
| Hypotension | 238 (73) | 280 (82) | 0.006 | 74 (43) | 85 (52) | 0.093 |
| High Risk Nephrotoxins |
0.018 | 0.002 | ||||
| 0 | 158 (49) | 192 (56) | 52 (30) | 72 (44) | ||
| 1 | 148 (46) | 117 (34) | 77 (45) | 73 (45) | ||
| 2 | 18 (6) | 29 (9) | 35 (20) | 12 (7) | ||
| ≥3 | 1 (0) | 3 (1) | 7 (4) | 5 (3) | ||
| Moderate Risk Nephrotoxins |
0.2 | 0.36 | ||||
| 0 | 17 (5) | 13 (4) | 6 (4) | 2 (1) | ||
| 1 | 151 (46) | 147 (43) | 21 (12) | 14 (9) | ||
| 2 | 128 (39) | 134 (39) | 54 (32) | 54 (33) | ||
| ≥3 | 29 (9) | 47 (14) | 90 (53) | 92 (57) | ||
| RACHS Score# | <0.001 | 0.018 | ||||
| 1 | 93 (29) | 50 (16) | 57 (40) | 31 (24) | ||
| 2 | 123 (38) | 133 (42) | 52 (36) | 60 (46) | ||
| ≥3 | 104 (32) | 133 (42) | 34 (24) | 39 (30) | ||
Median [Interquartile Range], p-value from the univariate Wilcoxon rank-sum test for continuous variables; Number (%), p-value from the univariate Pearson chi-square test for categorical variables
CPB - Cardiopulmonary Bypass, with time available for n=665 in the primary cohort and all 333 of the validation cohort
RDW – Red Cell Distribution Width, with values available for n=613 in the primary cohort and n=329 in the validation cohort
RACHS - Risk Adjustment for Congenital Heart Surgery, with scores available for n=636 in the primary cohort and n=273 in the validation cohort; SI conversion factor: To convert creatinine to μmol/L, multiply by 88.4.
Figure 2. Multivariable Analyses of the Primary and Validation Cohorts.
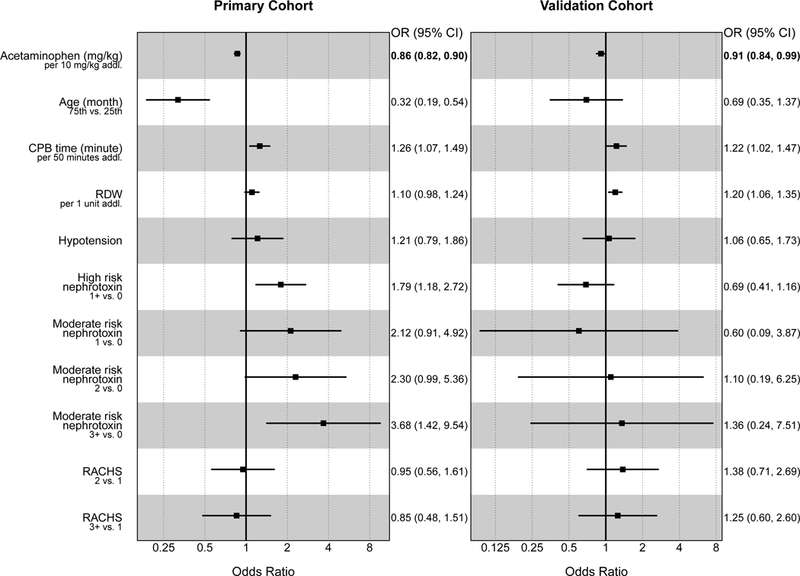
Shown are the ORs and the 95% CI for each of the clinical variables in the multiple logistic model for association to AKI in the primary cohort (left, N=666) and validation cohort (right, N=333). ORs are for weight-adjusted acetaminophen dose (per additional 10 mg/kg); Age (75th vs. 25th percentile for each cohort); CPB time (per additional 50 minutes); RDW (per additional 1%); Hypotension (present vs. absent); High risk nephrotoxins (one or more vs. none); Moderate risk nephrotoxins (one, two, and three or more vs. none); and RACHS score (two and three or more vs. one). Point estimates and 95% CI are listed to the right of each plot. AKI – Acute kidney injury. OR – Odds ratio. CI – Confidence interval. CPB – Cardiopulmonary bypass. RDW – Red cell distribution width. RACHS – Risk Adjustment for Congenital Heart Surgery.
Figure 3. Adjusted Odds Ratios for AKI by Acetaminophen Dose.
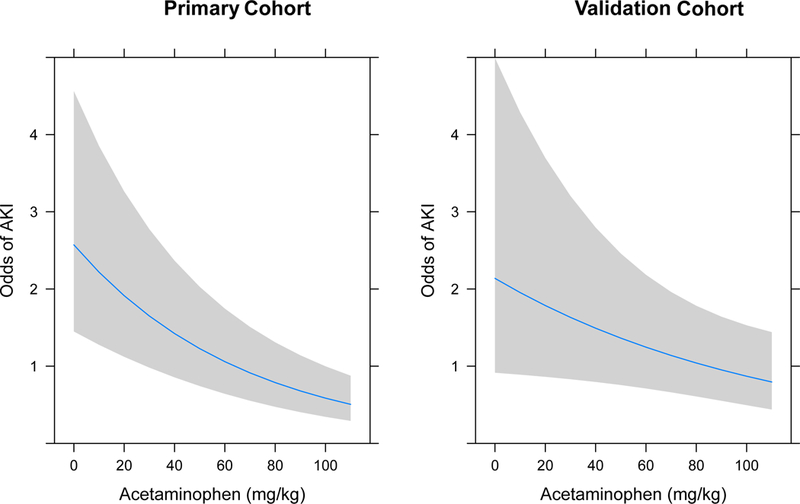
The odds of AKI are shown on the Y-axes, with weight-adjusted acetaminophen dose (mg/kg) on the X-axes, based on multivariable analyses adjusting for age, cardiopulmonary bypass time, red cell distribution width, hypotension, nephrotoxin exposure, and Risk Adjustment for Congenital Heart Surgery (RACHS) score, which were set to their median values. Shaded areas indicate 95% confidence intervals. Left panel – Primary cohort (N=666). Right Panel – Validation cohort (N=333). AKI – Acute kidney injury.
For the validation cohort, 18 (6%) had no acetaminophen exposure, and there was no significant difference in AKI incidence between those with no acetaminophen and those who received acetaminophen (Figure 1A). Comparing those with and without AKI, the median early postoperative acetaminophen dose was again higher among those without AKI than those with AKI (Table 2). Younger age, longer CPB time, higher RDW, fewer high risk nephrotoxins, and higher RACHS score were also associated with postoperative AKI. When stratified by AKI stage, those with no AKI again had the highest median weight-adjusted acetaminophen dose (70 [IQR 45–94] mg/kg). Those with stage 1 AKI has the lowest median dose (50 [IQR 26–76] mg/kg), and acetaminophen doses were similar in those with stage 2 and stage 3 AKI as those with no AKI (67 [IQR 43–88] mg/kg, and 66 [IQR 45–87] mg/kg, respectively, p=0.018). Those with no acetaminophen exposure again had the highest rates of AKI, with decreasing incidence in the lowest, middle, and highest acetaminophen dose groups, without statistical significance (Figure 1B). In multivariable analysis, adjusting for the same variables as above, postoperative acetaminophen had a protective effect for AKI, with adjusted odds ratio 0.91 (95% CI 0.84–0.99) for each additional 10 mg/kg (Figure 2). The relationship of continuous acetaminophen dose to adjusted odds for AKI in the validation cohort is shown in Figure 3. When those with no acetaminophen exposure were excluded, acetaminophen exposure remained protective (OR 0.90 per 10 mg/kg, 95% CI 0.82–0.99, p=0.03).
Pooled subgroup analysis
The pooled subgroup analysis included a total of 310 individuals with RACHS score ≥3 from both clinical sites (237 and 73 individuals from the primary cohort and the validation cohort, respectively). After adjusting for clinical site as well as the same covariates as above, acetaminophen dose (mg/kg) in this subgroup again showed a protective effect for AKI (OR 0.86, 95% CI 0.81–0.93, for each additional 10 mg/kg, eFigure 1).
Discussion
We present the finding of a protective association of acetaminophen for AKI in children who undergo cardiac surgery. The weight-adjusted total dose of acetaminophen given in the first 48 hours after surgery was inversely correlated with incidence of AKI in the primary cohort using the dichotomous indicator of acetaminophen exposure, acetaminophen dose as a continuous variable, and after adjusting for potential confounders including age, CPB time, RDW, RACHS score, postoperative hypotension, and nephrotoxin exposures. Given this novel finding, we sought to confirm these observations in an independent data set, where after adjusting for confounding variables which were not balanced across acetaminophen exposure groups, the protective effect of acetaminophen was again observed. Subgroup analyses of only those patients who received acetaminophen and those with RACHS score ≥3, representing more clinically homogenous patients, yielded consistent results.
The hypothesis that acetaminophen may be protective against AKI in the setting of cardiac surgery stemmed from several observations. In a case-control study of adults undergoing cardiac surgery, the 10 individuals with postoperative AKI had higher intraoperative peak free hemoglobin concentrations than risk-matched controls (289.0 vs. 104.4 mg/dL, p=0.01).30 This association was replicated in a cohort study of 60 children undergoing surgery requiring CPB, where those with AKI had greater increase in plasma hemoglobin concentration (53.9 vs. 38.3 mg/dL, p=0.03), and increase in plasma hemoglobin was an independent risk factor for AKI (OR 1.02 (95% CI 1.00–1.03) per mg/dL increase).29 The mechanism whereby free hemoglobin leads to nephrotoxicity is postulated to be through lipid peroxidation, catalyzed by oxidized cell-free hemoglobin, a process that can be inhibited by acetaminophen.32,40
Cell-free hemoglobin was also associated with death in a retrospective observational study of critically ill adults with sepsis, and acetaminophen exposure had a protective association with in-hospital mortality.31 Interestingly, in the subset of patients with no detectable plasma hemoglobin, there was no protective effect of acetaminophen. This potential protective effect of acetaminophen was evaluated prospectively in the Acetaminophen for the Reduction of Oxidative Injury in Severe Sepsis (ACROSS) Trial. This single-center, randomized, placebo-controlled trial of acetaminophen 1g enterally every 6 hours for 3 days found no difference in the primary endpoint, F2-Isoprostanes at day 3 (a measure of oxidative injury) or hospital mortality, but did observe that acetaminophen treatment impacted secondary outcomes. Namely, acetaminophen lowered F2-Isoprostanes at day 2 (24 vs. 36 pg/mL, p=0.047) and serum creatinine at day 3 (1.0 vs. 1.3 mg/dl, p=0.039).33 In another randomized trial including 700 adult ICU patients with fever, there was no difference in the primary outcome (ICU-free days), nor was there a difference in the peak creatinine in the first week after randomization.41 This negative result may indicate that acetaminophen has protective effects only in specific patient populations.
There have been two pilot studies of the impact of acetaminophen on lipid peroxidation in patients undergoing CPB. In a prospective double-blind clinical trial, 60 adult patients were treated with four doses of intravenous acetaminophen over 24 hours (1g for those >50kg and 15mg/kg for those <50kg) or placebo starting prior to initiation of CPB.42 The primary outcome was oxidative stress, measured by plasma and urine F2-Isoprostanes and isofurans. The acetaminophen treatment group had smaller increases in plasma isofuran concentrations compared to the placebo group (p=0.05), though there were no significant differences between groups in plasma F2-Isoprostanes, urinary markers of lipid peroxidation, or AKI. The second pilot study randomized 30 children to be treated with four doses of intravenous acetaminophen (15 mg/kg for age ≥2 years and 12.5mg/kg for age <2 years) or placebo, starting before the start of CPB.43 As in the adult trial, acetaminophen attenuated increases in plasma isofurans (p=0.02), but there were no differences between the intervention and control groups in F2-Isoprostanes, AKI prevalence, AKI severity, or the AKI biomarker NGAL. There were several limitations to these pilot studies, including limited power due to the small number of participants and the administration of one or more doses of acetaminophen before and during CPB, when circulating concentration of the drug may not have reached therapeutic levels due to hemodilution. These studies were not definitive in determining the potential role of acetaminophen to protect against AKI in patients with elevated cell-free hemoglobin.
Our results indicate a modest effect size for acetaminophen with respect to AKI. Namely, we see an approximately 10% reduction in AKI risk for each additional 10 mg/kg administered in the first 48 hours after surgery (one typical dose of acetaminophen). In the subgroup analysis of those with RACHS score ≥3, we observed a 14% reduction per 10 mg/kg of additional acetaminophen. The ideal dose for renal protection while avoiding dose-related hepatotoxicity or other adverse events has not been established. There may be several sources of inter-individual variability contributing to differences in the exposure and response to acetaminophen in both adults and children.44,45 Further delineation of individualized therapeutic concentrations through a precision medicine approach may be required to maximize benefit and minimize risk of acetaminophen use.
Our study has several limitations. This is a retrospective, observational study. Thus, causality between acetaminophen exposure and reduced incidence of AKI cannot be established. The apparent protective effect of acetaminophen may be due to residual confounding. Patients with acetaminophen exposure had fewer risk factors for AKI. Furthermore, these patients may have the most frequent serum creatinine testing, increasing AKI detection. We have attempted to control for this potential confounding through multivariable analysis, adjusting for factors such as age, bypass time, and RACHS score. Despite inclusion of these variables, acetaminophen remained protective. Our analyses of the sensitivity of our data to unmeasured confounding indicate that our data are robust. Of note, those with AKI had fewer exposures to highly nephrotoxic drugs, an observation we have seen in multiple cohorts3,37 and that may be due to avoidance of these drugs among high-risk patients. Another limitation of our study comes from the definition of AKI. We used the consensus KDIGO definition based on serum creatinine, but did not define AKI based on urine output (which may be inaccurately represented in these retrospective data sets) or biomarkers such as NGAL or cystatin C.46 Our initial finding from one tertiary referral center was validated in independent data from a second tertiary referral center. However, these results may not be generalizable to institutions with different patient mix, operative procedures, and postoperative care.
In summary, in two independent cohorts of children undergoing cardiac surgery, we observed a dose-dependent inverse relationship between postoperative receipt of acetaminophen and development of AKI. Taken together with other retrospective and prospective studies showing protective effects of acetaminophen for AKI in several conditions associated with release of cell-free hemoglobin, these findings provide compelling rationale to justify prospective evaluation of acetaminophen for prevention of AKI in children undergoing CPB.
Supplementary Material
Key Points
Question:
Does early postoperative acetaminophen reduce the incidence of acute kidney injury in children who undergo cardiac surgery?
Findings:
In this retrospective observational study, acetaminophen exposure in the first postoperative 48 hours was associated with lower rate of acute kidney injury in pediatric patients who underwent cardiac surgery in primary and validation cohorts from 2 tertiary referral children’s hospitals.
Meaning:
Postoperative use of acetaminophen may protect pediatric cardiac surgery patients from acute kidney injury.
Acknowledgments:
The authors thank the PACS study nurses, Kim Crum, Carla Hissam, and Darlene Fountain, and all study participants and families.
Funding: The project described was supported by CTSA award UL1 TR000445 from the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS), R01 HD084461 from the NIH Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and the Doris Duke Clinical Scientist Development Award to SLV. SLV has been supported by NIH/NCATS KL2 TR000446. LBW is supported by NIH HL103836 and NIH HL135849.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Competing interests: SLV has received an honorarium as an invited speaker to Merck. The authors have no awarded or filed patents pertaining to the results presented in the paper.
References
- 1.Sutherland SM, Ji J, Sheikhi FH, et al. AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin J Am Soc Nephrol CJASN 2013;8(10):1661–1669. doi:10.2215/CJN.00270113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 2007;71(10):1028–1035. doi:10.1038/sj.ki.5002231. [DOI] [PubMed] [Google Scholar]
- 3.McGregor TL, Jones DP, Wang L, et al. Acute Kidney Injury Incidence in Noncritically Ill Hospitalized Children, Adolescents, and Young Adults: A Retrospective Observational Study. Am J Kidney Dis 2016;67(3):384–390. doi:10.1053/j.ajkd.2015.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey D, Phan V, Litalien C, et al. Risk factors of acute renal failure in critically ill children: A prospective descriptive epidemiological study. Pediatr Crit Care Med 2007;8(1):29–35. doi:10.1097/01.pcc.0000256612.40265.67. [DOI] [PubMed] [Google Scholar]
- 5.Moghal NE, Brocklebank JT, Meadow SR. A review of acute renal failure in children: incidence, etiology and outcome. Clin Nephrol 1998;49(2):91–95. [PubMed] [Google Scholar]
- 6.Selewski DT, Cornell TT, Heung M, et al. Validation of the KDIGO acute kidney injury criteria in a pediatric critical care population. Intensive Care Med 2014;40(10):1481–1488. doi:10.1007/s00134–014-3391–8. [DOI] [PubMed] [Google Scholar]
- 7.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int 2012;2(Suppl):1–138. [Google Scholar]
- 8.Alkandari O, Eddington KA, Hyder A, et al. Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care 2011;15(3):R146. doi:10.1186/cc10269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soler YA, Nieves-Plaza M, Prieto M, García-De Jesús R, Suárez-Rivera M. Pediatric Risk, Injury, Failure, Loss, End-Stage renal disease score identifies acute kidney injury and predicts mortality in critically ill children: a prospective study. Pediatr Crit Care Med 2013;14(4):e189-195. doi:10.1097/PCC.0b013e3182745675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Piccinni P, Cruz DN, Gramaticopolo S, et al. Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol 2011;77(11):1072–1083. [PubMed] [Google Scholar]
- 11.Schneider J, Khemani R, Grushkin C, Bart R. Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med 2010;38(3):933–939. doi:10.1097/CCM.0b013e3181cd12e1. [DOI] [PubMed] [Google Scholar]
- 12.Hsu C- N, Chen H- L, Tain Y- L. Epidemiology and outcomes of community-acquired and hospital-acquired acute kidney injury in children and adolescents. Pediatr Res November 2017. doi:10.1038/pr.2017.262. [DOI] [PubMed] [Google Scholar]
- 13.Watkins SC, Williamson K, Davidson M, Donahue BS. Long-term mortality associated with acute kidney injury in children following congenital cardiac surgery. Paediatr Anaesth May 2014. doi:10.1111/pan.12419. [DOI] [PubMed] [Google Scholar]
- 14.Soni M, Piggott KD, DeCampli W, et al. Are We Overdiagnosing Acute Kidney Injury in Pediatric Patients Following Cardiac Surgery? World J Pediatr Congenit Heart Surg 2015;6(4):496–501. doi:10.1177/2150135115593129. [DOI] [PubMed] [Google Scholar]
- 15.Miklaszewska M, Korohoda P, Sobczak A, et al. Acute Kidney Injury in a Single Pediatric Intensive Care Unit in Poland: A Retrospective Study. Kidney Blood Press Res 2014;39(1):28–39. doi:10.1159/000355774. [DOI] [PubMed] [Google Scholar]
- 16.Madsen NL, Goldstein SL, Frøslev T, Christiansen CF, Olsen M. Cardiac surgery in patients with congenital heart disease is associated with acute kidney injury and the risk of chronic kidney disease. Kidney Int April 2017. doi:10.1016/j.kint.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 17.Li S, Krawczeski CD, Zappitelli M, et al. Incidence, risk factors, and outcomes of acute kidney injury after pediatric cardiac surgery: a prospective multicenter study. Crit Care Med 2011;39(6):1493–1499. doi:10.1097/CCM.0b013e31821201d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alcaraz AJ, Gil-Ruiz MA, Castillo A, et al. Postoperative neutrophil gelatinase-associated lipocalin predicts acute kidney injury after pediatric cardiac surgery*. Pediatr Crit Care Med 2014;15(2):121–130. doi:10.1097/PCC.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 19.Hazle MA, Gajarski RJ, Aiyagari R, et al. Urinary biomarkers and renal near-infrared spectroscopy predict intensive care unit outcomes after cardiac surgery in infants younger than 6 months of age. J Thorac Cardiovasc Surg 2013;146(4):861–867.e1. doi:10.1016/j.jtcvs.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lex DJ, Tóth R, Cserép Z, et al. A Comparison of the Systems for the Identification of Postoperative Acute Kidney Injury in Pediatric Cardiac Patients. Ann Thorac Surg 2014;97(1):202–210. doi:10.1016/j.athoracsur.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 21.Meersch M, Schmidt C, Van Aken H, et al. Validation of cell-cycle arrest biomarkers for acute kidney injury after pediatric cardiac surgery. PloS One 2014;9(10):e110865. doi:10.1371/journal.pone.0110865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gil-Ruiz Gil-Esparza MA, Alcaraz Romero AJ, Romero Otero A, et al. Prognostic relevance of early AKI according to pRIFLE criteria in children undergoing cardiac surgery. Pediatr Nephrol Berl Ger 2014;29(7):1265–1272. doi:10.1007/s00467–014-2757-z. [DOI] [PubMed] [Google Scholar]
- 23.Ruf B, Bonelli V, Balling G, et al. Intraoperative renal near-infrared spectroscopy indicates developing acute kidney injury in infants undergoing cardiac surgery with cardiopulmonary bypass: a case-control study. Crit Care Lond Engl 2015;19:27. doi:10.1186/s13054–015-0760–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sugimoto K, Toda Y, Iwasaki T, et al. Urinary Albumin Levels Predict Development of Acute Kidney Injury After Pediatric Cardiac Surgery: A Prospective Observational Study. J Cardiothorac Vasc Anesth 2016;30(1):64–68. doi:10.1053/j.jvca.2015.05.194. [DOI] [PubMed] [Google Scholar]
- 25.Park S- K, Hur M, Kim E, et al. Risk Factors for Acute Kidney Injury after Congenital Cardiac Surgery in Infants and Children: A Retrospective Observational Study. PloS One 2016;11(11):e0166328. doi:10.1371/journal.pone.0166328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hirano D, Ito A, Yamada A, et al. Independent Risk Factors and 2-Year Outcomes of Acute Kidney Injury after Surgery for Congenital Heart Disease. Am J Nephrol 2017;46(3):204–209. doi:10.1159/000480358. [DOI] [PubMed] [Google Scholar]
- 27.Haase M, Bellomo R, Haase-Fielitz A. Novel biomarkers, oxidative stress, and the role of labile iron toxicity in cardiopulmonary bypass-associated acute kidney injury. J Am Coll Cardiol 2010;55(19):2024–2033. doi:10.1016/j.jacc.2009.12.046. [DOI] [PubMed] [Google Scholar]
- 28.Vercaemst L Hemolysis in cardiac surgery patients undergoing cardiopulmonary bypass: a review in search of a treatment algorithm. J Extra Corpor Technol 2008;40(4):257–267. [PMC free article] [PubMed] [Google Scholar]
- 29.Kim-Campbell N, Gretchen C, Callaway C, et al. Cell-Free Plasma Hemoglobin and Male Gender Are Risk Factors for Acute Kidney Injury in Low Risk Children Undergoing Cardiopulmonary Bypass. Crit Care Med 2017;45(11):e1123-e1130. doi:10.1097/CCM.0000000000002703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Billings FT, Ball SK, Roberts LJ, Pretorius M. Postoperative acute kidney injury is associated with hemoglobinemia and an enhanced oxidative stress response. Free Radic Biol Med 2011;50(11):1480–1487. doi:10.1016/j.freeradbiomed.2011.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Janz DR, Bastarache JA, Peterson JF, et al. Association between cell-free hemoglobin, acetaminophen, and mortality in patients with sepsis: an observational study. Crit Care Med 2013;41(3):784–790. doi:10.1097/CCM.0b013e3182741a54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boutaud O, Moore KP, Reeder BJ, et al. Acetaminophen inhibits hemoprotein-catalyzed lipid peroxidation and attenuates rhabdomyolysis-induced renal failure. Proc Natl Acad Sci U S A 2010;107(6):2699–2704. doi:10.1073/pnas.0910174107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Janz DR, Bastarache JA, Rice TW, et al. Randomized, placebo-controlled trial of acetaminophen for the reduction of oxidative injury in severe sepsis: the Acetaminophen for the Reduction of Oxidative Injury in Severe Sepsis trial. Crit Care Med 2015;43(3):534–541. doi:10.1097/CCM.0000000000000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Heart Association. PALS Provider Manual 1st ed. Amer Heart Assn Inc; 2017. [Google Scholar]
- 35.James MT, Hobson CE, Darmon M, et al. Applications for detection of acute kidney injury using electronic medical records and clinical information systems: workgroup statements from the 15(th) ADQI Consensus Conference. Can J Kidney Health Dis 2016;3:9. doi:10.1186/s40697–016-0100–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee SW, Yu M- Y, Lee H, et al. Risk Factors for Acute Kidney Injury and In-Hospital Mortality in Patients Receiving Extracorporeal Membrane Oxygenation. PloS One 2015;10(10):e0140674. doi:10.1371/journal.pone.0140674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang L, McGregor TL, Jones DP, et al. Electronic health record-based predictive models for acute kidney injury screening in pediatric inpatients. Pediatr Res 2017;82(3):465–473. doi:10.1038/pr.2017.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 2002;123(1):110–118. [DOI] [PubMed] [Google Scholar]
- 39.Rubin DB. Multiple imputations in sample surveys: a phenomenological Bayesian approach to nonresponse (with discussion). Proc Am Stat Assoc Sect Surv Res Methods 1978:20–34. [Google Scholar]
- 40.Ouellet M, Percival MD. Mechanism of acetaminophen inhibition of cyclooxygenase isoforms. Arch Biochem Biophys. 2001;387(2):273–280. doi:10.1006/abbi.2000.2232. [DOI] [PubMed] [Google Scholar]
- 41.Young P, Saxena M, Bellomo R, et al. Acetaminophen for Fever in Critically Ill Patients with Suspected Infection. N Engl J Med 2015;373(23):2215–2224. doi:10.1056/NEJMoa1508375. [DOI] [PubMed] [Google Scholar]
- 42.Billings FT, Petracek MR, Roberts LJ, Pretorius M. Perioperative intravenous acetaminophen attenuates lipid peroxidation in adults undergoing cardiopulmonary bypass: a randomized clinical trial. PloS One 2015;10(2):e0117625. doi:10.1371/journal.pone.0117625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simpson SA, Zaccagni H, Bichell DP, et al. Acetaminophen attenuates lipid peroxidation in children undergoing cardiopulmonary bypass. Pediatr Crit Care Med 2014;15(6):503–510. doi:10.1097/PCC.0000000000000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Court MH, Zhu Z, Masse G, et al. Race, Gender, and Genetic Polymorphism Contribute to Variability in Acetaminophen Pharmacokinetics, Metabolism, and Protein-Adduct Concentrations in Healthy African-American and European-American Volunteers. J Pharmacol Exp Ther 2017;362(3):431–440. doi:10.1124/jpet.117.242107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allegaert K, Vanhaesebrouck S, Verbesselt R, van den Anker JN. In vivo glucuronidation activity of drugs in neonates: extensive interindividual variability despite their young age. Ther Drug Monit 2009;31(4):411–415. doi:10.1097/FTD.0b013e3181a8cc0a. [DOI] [PubMed] [Google Scholar]
- 46.Toda Y, Sugimoto K. AKI after pediatric cardiac surgery for congenital heart diseases-recent developments in diagnostic criteria and early diagnosis by biomarkers. J Intensive Care 2017;5:49. doi:10.1186/s40560–017-0242-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


