Abstract
IMPORTANCE
Glaucoma is a common cause of visual impairment in the Veterans Affairs (VA) health care system, but to our knowledge, no data exist concerning tertiary glaucoma care (ie, laser and filtering surgery).
OBJECTIVE
To determine whether the rate of tertiary glaucoma care differs among veterans cared for through the 4 different eye care delivery models that are present in the VA: optometry-only clinics, ophthalmology-only clinics, clinics with optometry and ophthalmology functioning as a single integrated clinic with ophthalmology as the lead, and clinics with optometry and ophthalmology functioning as separate clinics.
DESIGN, SETTING, AND PARTICIPANTS
In this retrospective review of the Veterans Health Administration Support Service Center database, 490 926 veterans with a glaucoma-related diagnosis received care from 136 VA medical centers during fiscal year 2016. Demographic and baseline clinical factors, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, and Current Procedural Terminology codes, and the rates of glaucoma surgery procedures were extracted from the database. The organizational structure of each VA eye clinic was obtained. Univariate and multivariate regression analyses were performed for log percent for laser peripheral iridotomy (LPI), laser trabeculoplasty (LTP), and filtering surgery.
MAIN OUTCOMES AND MEASURES
Rates of LPI, LTP, and filtering surgery.
RESULTS
Of the 490 926 veterans with a glaucoma-related diagnosis, 465 842 (94.9%) were male, 309 677 (63.1%) were white, and 203 243 (41.4%) were aged 65 to 74 years. The rate of LPI was 0.30%, 0.28%, 0.67%, and 0.69% in optometry-only clinics, ophthalmology-only clinics, integrated clinics, and separated clinics, respectively (P < .001). The rate of LTP was 0.31%, 1.06%, 0.93%, and 0.92% in care delivery models that included optometry-only clinics, ophthalmology-only clinics, integrated clinics, and separated clinics, respectively (P < .001). The rate of filtering surgery was 0.32%, 0.51%, 0.69%, and 0.60% in optometry-only clinics, ophthalmology-only clinics, integrated clinics, and separated clinics, respectively (P < .001). Multivariate regression analyses showed that these differences remained significantly different even after adjusting for potential confounders.
CONCLUSIONS AND RELEVANCE
Disparities exist in the use of tertiary glaucoma services within the VA, and different care delivery models may play a role. Outcomes of glaucoma care for the different models of eye care delivery were not analyzed in this study.
The Veterans Health Administration is a major health care system in the United States and provides medical care to more than 6 million veterans each year.1 The Veterans Affairs (VA) health care system includes 170 medical facilities and more than 1200 community-based outpatient clinics,1 many of which are in rural communities. Eye care is the third busiest clinical service in the VA system. The VA renders care through a combination of VA-based services and non-VA community optometrists and ophthalmologists.
Currently, eye care is available in 136 of the 170 VA medical centers (80.0%) and is delivered through 4 main care models: clinics with optometrists only, with ophthalmologists only, with optometrists and ophthalmologists functioning as a single integrated clinic with ophthalmology as the lead, and with optometry and ophthalmology functioning as separate clinics. To our knowledge, no study has evaluated whether there is a significant difference in the care provided by these different delivery models.
Glaucoma is a leading cause of visual loss in the United States and a major eye pathology treated in the VA system. Timely diagnosis, early treatment, and good compliance have been shown to be critical in preserving vision and decreasing the likelihood of further visual loss from glaucoma.2,3 The pur pose of this study was to compare the glaucoma care provided by the 4 different care models that exist in the VA by evaluating the rate of use of tertiary glaucoma care.
Methods
Data Extraction
Information for fiscal year 2016 was extracted from the Veterans Health Administration Support Service Center (VSSC) database, which tracks patient care metrics, including the eye care provided to veterans seen within VA facilities and those who were referred out to the community. Most optometry-only clinics used primarily community ophthalmologists for tertiary care, which was captured by the non-VA care query. Demographic factors and patient location (rural vs urban) were obtained. The number of unique veterans with a glaucoma-related diagnosis was extracted from the VSSC database using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, code of H40. Glaucoma surgical procedures were extracted from the VSSC using Current Procedural Terminology codes and included laser iridotomy (LPI), laser trabeculoplasty (LTP), and incisional filtering surgery, which was defined as trabeculectomy, aqueous shunt devices, canaloplasty, and minimally invasive glaucoma surgery (MIGS). In addition, the eye clinic at each medical center was contacted regarding their organizational structure. The Emory University Institutional Review Board and the Atlanta VA Research and Development Committee reviewed and approved there search protocol. Informed consent was not required because the study used data from a deidentified database.
Analyses
The rate of glaucoma surgery, defined as the number of procedures performed at the VA and the number of procedures per-formed in the community by non-VA ophthalmologists divided by the number of unique veterans with glaucoma, was determined for each medical center. The difference in baseline demographic factors and the rate of glaucoma surgery between the 4 care delivery models was calculated with Kruskal-Wallis test. The difference between each pair of delivery models was evaluated with pairwise Wilcox test, with adjustment for multiple comparisons using the Benjamini-Hochberg technique.4
Each demographic factor, including each decade of life and care delivery model, was tested as a dependent variable in separate univariate linear regression models fitted with intercept with log percent for LTP, LPI, and filtering surgery as the outcome variable. Any factor that resulted in a P value less than .10 was forced into the multivariate regression model using log percent for each glaucoma surgery as the outcome. P values were 2-sided and adjusted for multiple comparisons, and a P value less than .05 was considered statistically significant. All analyses were performed with R version 3.2.2 (The R Foundation).
Results
Demographic and Baseline Clinical Factors
In fiscal year 2016, 6 144 324 veterans received care in the VA health care system nationally. A total of 1 791 676 veterans received eye care, and 490 926 of those had a glaucoma-related diagnosis. Thus, 8.0% of the veteran population that used VA health care and 27.4% of veterans seen in eye clinics had glaucoma. Of the veterans with glaucoma, 465 842 (94.9%) were male, 309 677 (63.1%) were white, and 203 243 (41.4%) were aged 65 to 74 years. African American individuals made up a disproportionate segment of veterans with glaucoma; while 972 979 (15.8%) of all veterans receiving VA care were African American, they accounted for 133 390 (27.2%) of patients with glaucoma. Hispanic and Latino patients made up a smaller segment of the glaucoma population; 32 152 of 490 926 veterans (6.5%) in the glaucoma population were Hispanic or Latino.
While 490 926 unique veterans had glaucoma, they were distributed in 14 subcategories. within subcategories was 867 885, as patients were included in multiple categories. For example, if the right eye of a patient had open-angle glaucoma and the left eye had traumatic glaucoma, then the patient was counted twice. Also, if one physician coded the patient as “open-angle with borderline findings low risk” but another physician coded the patient as “preglaucoma,” then the patient was counted twice. Of the 867 885 patients listed in glaucoma subcategories, 345 725 (39.8%) were suspected of having glaucoma in at least 1 eye, and 485 598 (56.0%) had a primary or secondary open-angle glaucoma in at least 1 eye. Of the 490 926 veterans with glaucoma, a mean of 151 382 (30.8%) lived in rural communities, and 407 959 (83.1%) met the financial criteria for cost-free VA health care (national mean, 79.4%).
Of the 136 VA medical centers, 29 centers (21.3%) were clinics with optometry only, 3 (2.2%) were clinics with ophthalmology only, 51 (37.5%) were integrated clinics with ophthalmology as the lead, and 53 (39.0%) were separated clinics (Table 1). Patients cared for in optometry-only clinics who needed surgical intervention could be referred to community-based ophthalmologists or referred to a VA facility with surgical glaucoma support via interfacility consultation.
Table 1.
Demographic Characteristics and Percentage of Patients With Glaucoma Receiving Laser Peripheral Iridotomy (LPI), Laser Trabeculoplasty (LTP), and Filtering Surgery by Care Delivery Model
| Characteristic | Optometry Only | Ophthalmology Only | Integrated | Separated | Total | Kruskal-Wallis P Value |
|---|---|---|---|---|---|---|
| No. of medical centers | 29 | 3 | 51 | 53 | 136 | NA |
| Male | 96.03 | 95.30 | 93.81 | 94.58 | 94.62 | <.001 |
| Age, y | ||||||
| ≤34 | 0.69 | 0.63 | 0.89 | 0.87 | 0.83 | .14 |
| 35–44 | 1.23 | 1.16 | 1.69 | 1.41 | 1.47 | <.001 |
| 45–54 | 5.82 | 6.47 | 6.99 | 6.24 | 6.43 | .10 |
| 55–64 | 17.14 | 19.64 | 20.32 | 18.47 | 18.89 | .01 |
| 65–74 | 41.89 | 41.74 | 40.79 | 41.69 | 41.40 | .71 |
| 75–84 | 20.20 | 19.15 | 18.06 | 19.45 | 19.09 | .08 |
| ≥85 | 13.04 | 11.21 | 11.25 | 11.87 | 11.88 | .31 |
| Race/ethnicity | ||||||
| American Indian | 0.53 | 1.08 | 0.66 | 0.94 | 0.75 | .58 |
| Asian | 0.21 | 0.21 | 0.74 | 1.12 | 0.76 | <.001 |
| African American | 8.53 | 20.22 | 18.49 | 12.23 | 13.97 | <.001 |
| Pacific Islander | 0.36 | 0.33 | 0.70 | 1.00 | 0.73 | <.001 |
| White | 80.27 | 70.85 | 67.62 | 72.19 | 72.17 | <.001 |
| Multiple | 0.57 | 0.59 | 0.88 | 0.82 | 0.79 | <.001 |
| Rural | 55.97 | 60.35 | 34.25 | 36.45 | 40.32 | <.001 |
| Model of eye care delivery | ||||||
| LPI | 0.30 | 0.28 | 0.67 | 0.69 | 0.59 | <.001 |
| LTP | 0.31 | 1.06 | 0.93 | 0.92 | 0.80 | <.001 |
| Filtering surgery | 0.32 | 0.51 | 0.69 | 0.60 | 0.57 | <.001 |
Abbreviation: NA, not applicable.
Values represent the mean percentage.
Significantly fewer African American individuals were seen by optometry-only clinics than the rest of the delivery models. Rural setting was significantly more common in optometryonly and ophthalmology-only clinics. There was a significant difference in the mean rate of all glaucoma surgeries (LPI, LTP, and filtering surgery) among the 4 care delivery models (Table 1). Univariate model results are presented in Table 2.
Table 2.
Univariate Association With Log Percent for Laser Peripheral Iridotomy, Laser Trabeculoplasty, and Filtering Surgerya
| Characteristic | Exp(β)(95%CI) | P Value | Exp(β)(95%CI) | P Value | Exp(β)(95%CI) | P Value |
|---|---|---|---|---|---|---|
| Male | 0.96(0.90–1.03) | .25 | 1.01 (0.93–1.10) | .75 | 0.97 (0.91–1.03) | .32 |
| Age, y | ||||||
| ≤34 | 1.33 (0.70–2.53) | .39 | 1.06 (0.49–2.31) | .87 | 0.88 (0.48–1.63) | .69 |
| 35–44 | 1.46(0.93–2.30) | .10 | 2.27 (1.34–3.84) | <.001 | 1.62 (1.06–2.48) | .03 |
| 45–54 | 1.06(0.92–1.21) | .45 | 1.28(1.09–1.51) | <.001 | 1.15(1.01–1.31) | .04 |
| 55–64 | 1.05(0.99–1.13) | .12 | 1.12 (1.04–1.21) | <.001 | 1.12(1.06–1.19) | <.001 |
| 65–74 | 1.03(0.95–1.11) | .46 | 0.99 (0.90–1.08) | .82 | 0.95 (0.88–1.02) | .15 |
| 75–84 | 0.94(0.87–1.02) | .13 | 0.89 (0.80–0.97) | .01 | 0.91 (0.85–0.99) | .02 |
| ≥85 | 0.94(0.88–1.01) | .08 | 0.90 (0.83–0.97) | <.001 | 0.94 (0.89–1.01) | .08 |
| Race/ethnicity | ||||||
| American Indian | 1.04(0.75–1.45) | .79 | 0.87 (0.59–1.29) | .50 | 0.93 (0.68–1.27) | .65 |
| Asian | 1.03 (0.88–1.19) | .74 | 1.06 (0.88–1.27) | .55 | 1.08 (0.93–1.25) | .29 |
| African American | 1.02 (0.99–1.04) | .19 | 1.05 (1.02–1.08) | <.001 | 1.05 (1.02–1.07) | <.001 |
| Pacific Islander | 1.02(0.85–1.23) | .81 | 1.04 (0.83–1.29) | .74 | 1.07 (0.90–1.28) | .42 |
| White | 0.98(0.96–1.00) | .08 | 0.95 (0.93–0.98) | <.001 | 0.95 (0.94–0.97) | <.001 |
| Multiple | 1.32 (0.74–2.33) | .35 | 1.14(0.57–2.27) | .71 | 1.22(0.71–2.10) | .47 |
| Rural | 0.98 (0.96–0.99) | <.001 | 0.97 (0.96–0.99) | <.001 | 0.98 (0.97–0.99) | <.001 |
| Model of eye care delivery | ||||||
| Optometry only (reference) | NA | NA | NA | NA | NA | NA |
| Ophthalmology only | 5.21(0.85–31.82) | .07 | 25.78 (2.90–229.50) | <.001 | 7.20 (1.20–43.24) | .03 |
| Integrated | 11.06(5.52–22.14) | <.001 | 17.52 (7.58–40.52) | <.001 | 8.05 (4.05–16.01) | <.001 |
| Separated | 8.71(4.37–17.36) | <.001 | 9.92 (4.32–22.82) | <.001 | 5.01 (2.53–9.92) | <.001 |
Variables with P values less than .10 were included in the subsequent multivariate model as covariates.
Surgical Care
Laser Peripheral Iridotomy
Laser peripheral iridotomy was performed on 5467 of 490 926 veterans with glaucoma (1.1%). The mean (SD) LPI rate was 0.96% (1.11), and the median (range) rate was 0.69% (0%−8.51%). Laser peripheral iridotomy was performed by a non-VA community ophthalmologists in 1003 of 5467 veterans (18.3%).
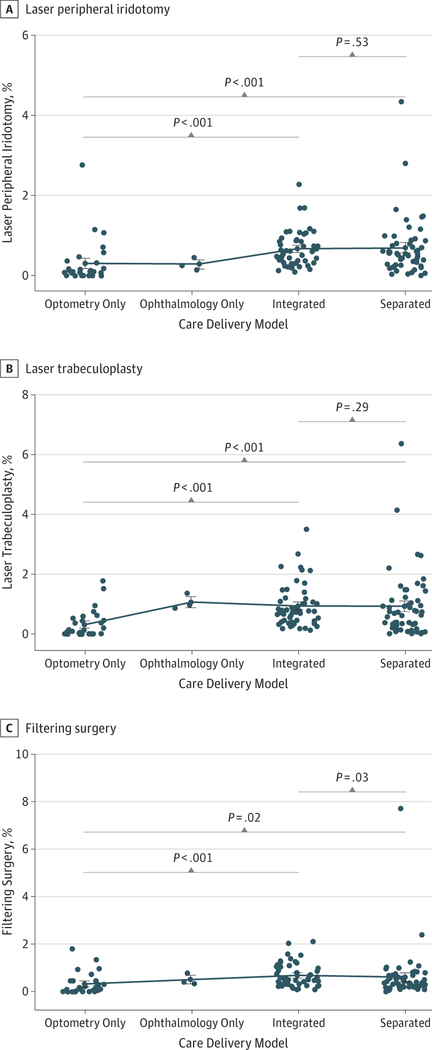
The percentage of patients with glaucoma who received LPI was significantly different among the 4 delivery models. Specifically, the LPI percentage was significantly different between optometry-only clinics and integrated clinics as well as between optometry-only clinics and separated clinics. There was no significant difference in the LPI percentage between clinics with integrated and separated care delivery models (Figure) (Table 3).
Figure. Percentage Rates of Glaucoma Surgery by Care Delivery Model.
Percentage rates of laser peripheral iridotomy (A), laser trabeculoplasty (B), and filtering surgery (C) at individual Veterans Affairs eye clinics by care delivery model. Each data point represents a single institution. The difference between each pair of delivery models was evaluated with pairwise Wilcoxon test adjusted for multiple comparisons. Error bars represent standard errors.
Table 3.
Pairwise Wilcoxon Test P Values Adjusted for Multiple Comparisons for Laser Peripheral Iridotomy, Laser Trabeculoplasty, and Filtering Surgical Rates by Delivery Care Model
| Delivery Care Model | Ophthalmology Only | Integrated | Separated | Ophthalmology Only | Integrated | Separated | Ophthalmology Only | Integrated | Separated |
|---|---|---|---|---|---|---|---|---|---|
| Optometry only | .32 | <.001 | <.001 | .04 | <.001 | <.001 | .23 | <.001 | .02 |
| Ophthalmology onh | NA | .15 | .25 | NA | .29 | .29 | NA | .68 | .67 |
| Integrated | NA | NA | .53 | NA | NA | .29 | NA | NA | .03 |
Abbreviation: NA, not applicable.
In multivariate regression analysis that controlled for 2 age categories (age of 35 to 44 years and 85 years and older) and white race, both rural setting and care delivery model were significantly associated with the likelihood of receiving LPI. Patients who received care in a rural area were significantly less likely to receive LPI than those in an urban setting. Compared with optometry-only clinics, patients seen by ophthalmology-only clinics had a 5.81-fold (95% CI, 0.96–35.14; P = .06) higher mean rate of LPI, but this did not reach significance. Compared with optometry-only clinics, patients seen by integrated clinics had a 9.30-fold (95% CI, 4.39–19.82; P < .001) higher mean rate of LPI, and those seen by separated clinics had a 6.96-fold (95% CI, 3.37–14.42; P < .001) higher mean rate of LPI (Table 4).
Table 4.
Multivariate Analysis for Percentage for Laser Peripheral Iridotomy, Laser Trabeculoplasty, and Filtering Surgery With Sensitivity Analysis
| Delivery Care Model | Exp(β)(95%CI) | P Value | Exp(β)(95%CI) | P Value | Exp(β)(95%CI) | P Value |
|---|---|---|---|---|---|---|
| Multivariate analysis | ||||||
| Optometry only (reference) | NA | NA | NA | NA | NA | NA |
| Ophthalmology only | 5.81 (0.96–35.14) | .06 | 19.11 (2.16–168.98) | .009 | 4.90 (0.87–27.36) | .07 |
| Integrated | 9.30 (4.39–19.82) | <.001 | 10.49 (4.19–26.25) | <.001 | 5.00 (2.42–10.35) | <.001 |
| Separated | 6.96 (3.37–14.42) | <.001 | 7.24(2.97–17.59) | <.001 | 3.39(1.68–6.88) | <.001 |
| Sensitivity analysis | ||||||
| Optometry only (reference) | NA | NA | NA | NA | NA | NA |
| Integrated | 9.27 (4.33–19.82) | <.001 | 10.44(4.14–26.31) | <.001 | 5.00 (2.41–10.40) | <.001 |
| Separated | 6.93 (3.33–14.42) | <.001 | 7.23(2.95–17.71) | <.001 | 3.41 (1.68–6.94) | <.001 |
Abbreviation: NA, not applicable.
Laser Trabeculoplasty
Laser trabeculoplasty was performed on 5877 of 490 926 veterans with glaucoma (1.2%). The mean (SD) LTP rate was 1.09% (1.32), and the median (range) rate was 0.76% (0%−9.67%). Laser trabeculoplasty was performed by a non-VA community ophthalmologist in 1071 of 5877 veterans (18.2%).
The percentage of patients with glaucoma who received LTP was significantly different among the 4 delivery models. Significant differences in the LTP percentage were seen between optometry-only clinics and integrated clinics as well as between optometry-only clinics and separated clinics. There was no significant difference in the LTP percentage between integrated and separated clinics (Figure) (Table 3).
Multivariate regression analysis showed that the only significant factor associated with LTP was the care delivery model. Compared with optometry-only clinics, patients seen by ophthalmology-only clinics had a 19.11-fold (95% CI, 2.16–168.98; P = .009) higher rate of LTP, those seen by integrated clinics had a 10.49-fold (95% CI, 4.19–26.25; P < .001) higher rate of LTP, and those seen by separated clinics had a 7.24-fold (95% CI, 2.97–17.59; P < .001) higher rate of LTP (Table 4).
Incisional Filtering Surgery
Incisional filtering surgery was performed on 3253 of 490 926 veterans with glaucoma (0.7%). The mean (SD) filtering surgery rate was 0.57% (0.77), and the median (range) rate was 0.39% (0%−7.71%). Minimally invasive glaucoma surgery made up 986 of 3253 procedures (30.3%); 612 patients underwent MIGS in a VA medical center and 374 underwent MIGS in the community. Non-VA community ophthalmologists performed 1029 of 3253 filtering procedures (31.6%).
The percentage of patients with glaucoma who received filtering surgery was significantly different among the 4 delivery models. The percentage was significantly different between optometry-only clinics and integrated clinics and between optometry-only clinics and separated clinics. The percentage of surgery between integrated and separated models also was significantly different, although very small (Figure) (Table 3).
The multivariate regression analysis controlled for age groups from age 35 years to 85 years and older, African American and white race, rural setting, and care delivery models. White race and care models were the only significant factors for receiving filtering surgery. White individuals were 4.8% less likely to receive filtering surgery (P = .02). Compared with optometry-only clinics, patients seen by ophthalmology-only clinics had a 4.90-fold (95% CI, 0.87–27.36; P = .07) higher rate of filtering surgery, those seen by integrated clinics had a 5.00-fold (95% CI, 2.42–10.35; P < .001) higher rate of filtering surgery, and those seen by separated clinics had a 3.39-fold (95% CI, 1.68–6.88; P < .001) higher rate of filtering surgery (Table 4).
Sensitivity Analysis
As a sensitivity analysis, ophthalmology-only clinics were excluded from the multivariate models. The delivery of care model remained a significant variable in all 3 models (Table 4).
Discussion
Of 6 144 324 veterans who received medical care during fiscal year 2016, 490 926 veterans had a glaucoma-related diagnosis, and a total of 14 597 glaucoma surgery procedures (defined as LPI, LTP, and filtering surgery) were performed. Rural setting was significantly more common in optometry-only and ophthalmology-only clinics. Significantly more African American patients were seen by ophthalmology-only clinics or ophthalmology-led integrated clinics. The rate of glaucoma surgery was significantly lower in patients seen in optometry-only clinics compared with ophthalmology-only clinics, integrated clinics, and separated clinics, even after controlling for patients’ age, sex, race, and location.
The association of the availability of ophthalmology services with the care of patients with serious eye conditions has previously been reported. Gibson5 found that greater county-level availability of ophthalmologists but not optometrists was associated with a significantly lower likelihood of vision loss in patients with age-related macular degeneration. It is possible that a comparable situation exists with regard to complex glaucoma care. In Oklahoma, where both ophthalmologists and optometrists perform LTP, patients who received LTP by optometrists were 2.89-fold (95% CI, 2.00–4.17; P < .001) more likely to require additional LTPs in the same eye compared with those receiving LTP by ophthalmologists.6 Further evaluations on the visual outcomes of our study population will be important to understand the clinical implications of the difference in glaucoma surgery rate we found.
Several hypotheses exist to explain the difference in glaucoma surgery rate between optometry-only clinics and other models that include an ophthalmology service. It is possible that patients cared for in optometry-only clinics had less severe glaucoma than patients seen in other facilities (ie, lower need), did not receive appropriate referral for ophthalmology evaluation and surgical intervention (ie, low use), were referred to the community for surgical intervention but never completed the appointment (ie, low access), were referred to the community for surgical intervention and had that intervention paid for through private insurance that was not reported to the VA (ie, low reporting), or were referred to another VA for care and absorbed into that facility’s database. The latter possibility seems less likely, as many of the optometry-only clinics were in remote and rural communities. Most of the veterans with glaucoma met the financial criteria to receive cost-free VA health care, but they may not have had the resources to travel to a distant facility for care. In some VA facilities with optometry-only clinics, patients with complex ophthalmic disorders are referred to other VA facilities with subspecialty care. The VA tracks the number of interfacility consultations sent to ophthalmology from each facility but does not track the subtype of the consultations by diagnosis. Thus, it is impossible to tell which consultations were for cataract, glaucoma, or macula care. Additionally, in fiscal year 2016, more than two-thirds of optometry-only clinics had minimal to no interfacility consultations to ophthalmology services within the VA system, and most used primarily community ophthalmologists for tertiary care.1
It is possible that veterans cared for in clinics with staff ophthalmologists had unusually high rates of glaucoma surgery, potentially from having more advanced glaucoma or better access to tertiary glaucoma care. However, the glaucoma surgery rate in the delivery models that included ophthalmology (0.05%) is comparable with other studies and representative of current practice patterns in the community. Mansouri et al7 estimated the global glaucoma surgery rate in the general population as 0.014% based on surveys of ophthalmic societies and nongovernmental organizations worldwide. Quigley et al8 reported the glaucoma surgery rate as 0.1% (ie, 1670 filtering surgeries in 1.68 million people) based on a 5% sampling of 2009 Medicare beneficiaries. In 2012, approximately 51 million people were enrolled in Medicare.9 Using these data, Arora et al10 estimated that 38 906 Medicare Part B beneficiaries underwent glaucoma surgical procedures in 2012, resulting in a glaucoma surgery rate of 0.08%. Based on these comparable glaucoma surgery rates, the difference that we found is less likely from overuse by ophthalmology-related clinics.
Optometry-only clinics were more commonly found in rural communities compared with urban settings. Thus, fewer tertiary glaucoma care options may have been available, indicating that veterans in rural communities may be medically underserved. However, veterans in optometry-only clinics also had lower rates of being diagnosed as having narrow-angle glaucoma or acute angle-closure glaucoma. This would suggest that these conditions are either not present in rural communities or, more likely, underdiagnosed. Underreferring or referring patients too late for tertiary glaucoma care has been reported for both the VA11 and non-VA eye care professionals.12 Marks et al13 reported that there may be a significant difference in the management of glaucoma between optometrists and ophthalmologists. The agreement for glaucoma management decisions, including timing of follow-up and referral to a glaucoma specialist (ophthalmologist), between optometrists and glaucoma specialists was 72% (weighted κ, 0.65) and for glaucoma stability was 67% to 70% (weighted κ, 0.42–0.50). The authors advocated for confirming the ability of optometrists to diagnose and follow up patients with glaucoma appropriately. In another study comparing the glaucoma-trained optometrists and glaucoma specialist consultants in the United Kingdom,14 the diagnostic accuracy of optometrists in detecting glaucoma was shown to be higher for specificity (0.93; 95% CI, 0.85–0.97) but lower for sensitivity (0.76; 95% CI, 0.57–0.89).
A 2016 report15 showed that most individuals in the United States live within a 30-minute driving distance of an ophthalmologist. Veterans are able to receive care through non-VA community ophthalmologists when there is no appropriate specialty care at their nearest VA medical center. Thus, early detection of glaucoma in veterans, even when no ophthalmology care is available in-house, will be important so patients can receive appropriate evaluation, follow-up, and potential surgical intervention by a community ophthalmologist. In addition, the integration of a teleophthalmology system that would extend care to a large number of rural veterans is currently being evaluated within the VA.16 With teleophthalmology, patients with high-risk features could be reviewed by ophthalmologists at a distant, centralized location to determine whether a face-to-face ophthalmology evaluation with possible surgical intervention is warranted. Teleophthalmology has been used in other health care systems that render care to rural patients.17,18
Limitations
Several limitations exist. First, our data were extracted from International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, and Current Procedural Terminology codes, and patient-level data (eg, type of glaucoma, glaucoma severity, progression rate, and compliance) were not available. Outcomes of care for the different models of eye care delivery could not be analyzed in this study. Second, data on non-VA care were extracted from the VA administrative database; inadequate or inaccurate coding cannot be ruled out. In addition, it is possible that some veteran patients with glaucoma received surgical care in the community that was paid for by Medicare or a commercial insurance carrier. If surgery was not paid through non-VA care funds, the VA would have no record of the surgery. Finally, this study examined the care that was provided in 1 fiscal year. Therefore, if more patients with mild glaucoma were followed up by optometry-only clinics, these patients would not have the need for tertiary glaucoma care. However, the decision to recommend and perform LPI depends primarily on the detection of an anatomical finding and not necessarily on disease progression. In our study, the reduced rate of LPI (in addition to LTP) in optometry-only clinics make this possibility less likely.
Conclusions
In the VA, a disparity exists in the use of glaucoma surgery. The rate of glaucoma laser and filtering surgery is significantly lower in patients seen by optometry-only clinics compared with patients cared for by clinics that have integrated optometry and ophthalmology. Further studies will be needed to determine which factors accounted for the disparity in glaucoma surgery rates across the VA and whether or not these disparities were associated with different clinical outcomes.
Key Points
Question
What is the rate of glaucoma surgery within the Veterans Affairs health care system?
Findings
In this database review of fiscal year 2016 data, 490 926 veterans receiving care at 136 Veterans Affairs medical centers were given a glaucoma-related diagnosis. Data showed a 3.39-fold to 19.11-fold higher rate of glaucoma laser and filtering surgery use in care delivery models that included ophthalmologists compared with centers that included optometrists only.
Meaning
This study suggests that a disparity exists in glaucoma surgery rates across the Veterans Affairs health care system and that different care delivery models play a role, although outcomes of glaucoma care for the different models of eye care delivery were not analyzed.
Acknowledgments
Funding/Support: This study was supported by an unrestricted research grant from Research to Prevent Blindness (Drs A. Lee and C. Lee), grant K23EY024921 from the National Eye Institute (Dr C. Lee), Nvidia Corporation (Dr A. Lee), and Lowy Medical Research Institute (Drs A. Lee and C. Lee).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Dr Aaron Lee has received grants from Microsoft Corporation and Novartis. No other disclosures were reported.
Publisher's Disclaimer: Disclaimer: The views expressed here are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the US government.
Meeting Presentation: This paper was presented as a poster at the 2017 meeting of the American Academy of Ophthalmology; November 11–14, 2017; New Orleans, Louisiana.
REFERENCES
- 1.US Department of Veterans Affairs. Veterans Health Administration: about VHA. https://www.va.gov/health/aboutvha.asp. Accessed February 12, 2018.
- 2.Kwon YH, Kim C-S, Zimmerman MB, Alward WL, Hayreh SS. Rate of visual field loss and long-term visual outcome in primary open-angle glaucoma. Am J Ophthalmol. 2001;132(1):47–56. doi: 10.1016/S0002-9394(01)00912-6 [DOI] [PubMed] [Google Scholar]
- 3.Susanna R Jr, De Moraes CG, Cioffi GA, Ritch R. Why do people (still) go blind from glaucoma? Transl Vis Sci Technol. 2015;4(2):1. doi: 10.1167/tvst.4.2.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
- 5.Gibson DM. The local availability of eye care providers and the vision health of adults in the United States. Ophthalmic Epidemiol. 2016;23(4): 223–231. doi: 10.1080/09286586.2016.1193208 [DOI] [PubMed] [Google Scholar]
- 6.Stein JD, Zhao PY, Andrews C, Skuta GL. Comparison of outcomes of laser trabeculoplasty performed by optometrists vs ophthalmologists in Oklahoma. JAMA Ophthalmol. 2016;134(10): 1095–1101. doi: 10.1001/jamaophthalmol.2016.2495 [DOI] [PubMed] [Google Scholar]
- 7.Mansouri K, Medeiros FA, Weinreb RN. Global rates of glaucoma surgery. Graefes Arch Clin Exp Ophthalmol. 2013;251(11):2609–2615. doi: 10.1007/s00417-013-2464-7 [DOI] [PubMed] [Google Scholar]
- 8.Quigley HA, Cassard SD, Gower EW, Ramulu PY, Jampel HD, Friedman DS. The cost of glaucoma care provided to Medicare beneficiaries from 2002 to 2009. Ophthalmology. 2013;120(11):2249–2257. doi: 10.1016/j.ophtha.2013.04.027 [DOI] [PubMed] [Google Scholar]
- 9.US Office of Retirement and Disability Policy. Annual Statistical Supplement, 2012: Medicare program description and legislative history. https://www.ssa.gov/policy/docs/statcomps/supplement/2012/medicare.html. Accessed February 12, 2018.
- 10.Arora KS, Robin AL, Corcoran KJ, Corcoran SL, Ramulu PY. Use of various glaucoma surgeries and procedures in Medicare beneficiaries from 1994 to 2012. Ophthalmology. 2015;122(8):1615–1624. doi: 10.1016/j.ophtha.2015.04.015 [DOI] [PubMed] [Google Scholar]
- 11.Maa J, Hedstrom K. College advocates for ensuring quality eye care for America’s veterans. Bull Am Coll Surg. 2010;95(9):8–10. [PubMed] [Google Scholar]
- 12.Stürmer JPE, Faschinger C. Do we perform glaucoma surgery too late? [in German] [published online August 24, 2017]. Klin Monbl Augenheilkd. [Google Scholar]
- 13.Marks JR, Harding AK, Harper RA, et al. Agreement between specially trained and accredited optometrists and glaucoma specialist consultant ophthalmologists in their management of glaucoma patients. Eye (Lond). 2012;26(6):853–861. doi: 10.1038/eye.2012.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azuara-Blanco A, Burr J, Thomas R, Maclennan G, McPherson S. The accuracy of accredited glaucoma optometrists in the diagnosis and treatment recommendation for glaucoma. Br J Ophthalmol. 2007;91(12):1639–1643. doi: 10.1136/bjo.2007.119628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee CS, Morris A, Van Gelder RN, Lee AY. Evaluating access to eye care in the contiguous United States by calculated driving time in the United States Medicare population. Ophthalmology. 2016;123(12):2456–2461. doi: 10.1016/j.ophtha.2016.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maa AY, Wojciechowski B, Hunt KJ, et al. Early Experience with Technology-Based Eye Care Services (TECS): a novel ophthalmologic telemedicine initiative. Ophthalmology. 2017;124(4):539–546. doi: 10.1016/j.ophtha.2016.11.037 [DOI] [PubMed] [Google Scholar]
- 17.Bartnik SE, Copeland SP, Aicken AJ, Turner AW. Optometry-facilitated teleophthalmology: an audit of the first year in Western Australia [published online February 14, 2018]. Clin Exp Optom. [DOI] [PubMed] [Google Scholar]
- 18.Kotecha A, Brookes J, Foster PJ. A technician-delivered ‘virtual clinic’ for triaging low-risk glaucoma referrals. Eye (Lond). 2017;31(6): 899–905. doi: 10.1038/eye.2017.9 [DOI] [PMC free article] [PubMed] [Google Scholar]