Abstract
Background.
Uncertainty regarding clopidogrel effectiveness attenuation due to a drug-drug interaction with proton pump inhibitors (PPI) has led to conflicting guidelines on concomitant therapy. In particular, the effect of this interaction in patients who undergo a percutaneous coronary intervention (PCI), a population known to have increased risk of adverse cardiovascular events, has not been systematically evaluated.
Objective.
To synthesize the evidence of the effect of clopidogrel-PPI drug interaction on adverse cardiovascular outcomes in a PCI patient population.
Methods.
We conducted a systematic literature review for studies reporting clinical outcomes in patients who underwent a PCI and were initiated on clopidogrel with or without a PPI. Studies were included in the analysis if they reported at least one of the clinical outcomes of interest (major adverse cardiovascular event (MACE), cardiovascular death, all-cause death, myocardial infarction, stroke, stent thrombosis, and bleed events). We excluded studies that were not exclusive to PCI patients or had no PCI subgroup analysis, and/or did not report at least a 6-month follow up. Statistical and clinical heterogeneity were evaluated and hazard ratios (HRs) and 95% confidence intervals (CIs) for adverse clinical events were pooled using the DerSimonian and Laird random-effects meta-analysis method.
Results.
We identified 12 studies comprising 50,277 PCI patients that met our inclusion and exclusion criteria. Our analysis included retrospective analyses of randomized control trials (2), health registries (3), claims databases (2), and institutional records (5); no prospective studies of PCI patients were identified. Patients were, on average, in their mid-60’s, male, and with an array of comorbidities including hyperlipidemia, diabetes, hypertension and smoking history. Concomitant therapy following PCI resulted in statistically significant increases in composite MACE (HR 1.28; 95% CI 1.24–1.32), myocardial infarction (HR 1.51; 95% CI 1.40–1.62) and stroke (HR 1.46; 95% CI 1.15–1.86). Only one study reported on GI bleed and pooled analysis couldn’t be conducted. Statistical testing suggested heterogeneity among studies, but subgroup analysis did not reveal a clear source.
Conclusions.
Concomitant clopidogrel-PPI therapy following PCI appears to be significantly associated with adverse cardiovascular events. Our findings suggest clinical guidelines should caution against the use of concomitant therapy in this patient population, and further research on the effect of individual PPIs is needed.
INTRODUCTION
Approximately 500,000 percutaneous coronary intervention (PCI) procedures to alleviate acute coronary syndrome (ACS) ischemia are performed in the United States each year.1 The standard of care following PCI is treatment with dual-antiplatelet therapy, consisting of a thienopyridine (typically clopidogrel) or ticagrelor with aspirin, to prevent re-infarction and other subsequent ischemic events.2 Proton pump inhibitors (PPI) are often added to this regimen to prevent gastrointestinal hemorrhage, a serious bleeding complication associated with long-term antiplatelet therapy.3
Pharmacokinetic studies have shown that PPIs as a class attenuate the antiplatelet effects of clopidogrel, however, the proposed cause of the interaction, inhibiting cytochrome P450 2C19 (CYP2C19)-facilitated metabolism of the prodrug to its active metabolite 2-oxo-clopidogrel, is stronger in some PPIs compared to others.4,5 Pharmacogenomic studies have shown that CYP2C19 variant[s] that lead to reduced enzymatic activity lead to attenuated clopidogrel effectiveness, however the results of studies populated by patients exhibiting a wide spectrum of ACS severity and invasive procedure use have largely been inconclusive.6 Notably, the most consistent and significant effects have been observed in patients undergoing percutaneous coronary intervention (PCI).7,8 These findings raise the question whether concomitantly-treated ACS patients, particularly those who undergo PCI, have a similarly elevated risk for poor cardiovascular outcomes.9
Clinical practice guidelines offer conflicting guidance on the significance of this interaction. In 2009 the FDA announced a non-boxed warning to “avoid concomitant use of clopidogrel with drugs that are strong or moderate CYP2C19 inhibitors (e.g. the PPIs omeprazole and esomeprazole).”10 More recently, in 2012, clinical guidelines from the American College of Cardiology Foundation and American Heart Association (ACCF/AHA) stated that they do “not prohibit the use of PPI agents in appropriate clinical settings,” and appeal for more randomized controlled trials until enough clinical evidence exists to inform a more scientifically derived recommendation.2,11–13
The preliminary results of the discontinued COGENT trial (3,761 ACS patients, 71% PCI) indicated no significant differences in clinical outcomes between clopidogrel monotherapy and concomitant omeprazole study arms.3 In the five ensuing years, a large number of retrospective cohort studies in various patient populations have been conducted to evaluate this drug-drug interaction and have produced largely conflicting results.14–19 Although a number of published meta-analyses have evaluated these studies, 20–22 they have not focused exclusively on a PCI population.
The objective of this study was to synthesize the evidence of the effect of clopidogrel-PPI drug interaction on adverse cardiovascular outcomes in a PCI patient population. We conducted a systematic literature review and meta-analysis of published clinical studies to evaluate whether drug-drug interactions between clopidogrel and a PPI lead to worse health outcomes in PCI patients than patients treated with clopidogrel only. The results of this study will be useful for informing clinical guidelines and practice for patients discharged with dual-antiplatelet therapy, consisting of clopidogrel and aspirin, after a PCI.
METHODS
Literature Review and Eligibility Criteria
The meta-analysis followed recommendations described in the Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) statement.23 We conducted a systematic literature search for all relevant clinical studies and meta-analyses using PubMed, Cochrane Database, and EMBASE databases up to March 2015 using the key words ‘proton pump inhibitor’ and ‘clopidogrel’. We then searched the bibliographies of all database-extracted papers for additional relevant studies that the database search may have missed. Our study included any randomized controlled trial or observational study that reported at least one of the following outcomes: major adverse cardiovascular event (MACE; a composite outcome typically comprised of myocardial infarction, stroke, and/or cardiovascular death), cardiovascular (CV) death, all-cause (AC) death, myocardial infarction (MI), stroke, stent thrombosis (ST), thrombolysis in myocardial infarction (TIMI) bleed, and gastrointestinal (GI) bleed. Studies were excluded if they were composed of non-PCI patients, if there was no PCI subgroup analysis, or if there was not at least a 6-month follow-up period to avoid studies focusing on short term or in-hospital outcomes. Clopidogrel dose and concurrent aspirin therapy were evaluated but not used as exclusion criteria. We also collected data on study design, study size, follow-up length and PPI used, however, did not exclude studies based on which individual PPI was used. Studies were assessed by two reviewers based on the inclusion and exclusion criteria.
Analysis
We conducted a DerSimonian and Laird method random-effects meta-analysis, which considers both within-study and between-study variation, using STATA statistical software.24 We assumed similarity between hazard ratios and odds ratios in all outcomes of uncommon events (α<5%), and we evaluated the odds ratios in event rates over 5% in sensitivity analyses.25 To mitigate the risk of bias and confounding in cohort studies, we used adjusted hazard ratios or propensity score matching hazard ratios from these studies if available.26–28 Heterogeneity was evaluated using the X2 statistic and the degree assessed using the I2 measure to display overall variability of inter-study versus intra-study heterogeneity. We also conducted sensitivity analysis by individual exclusion of each study for each outcome to assess their effect on the pooled outcome hazard ratio. We measured significance using a P value of less than 0.05; adjustment to the P value criteria for multiple comparisons was not conducted because of the complementary nature of the hypothesis.8 Results are presented as hazard ratios and their 95% confidence intervals.
RESULTS
Studies Identified
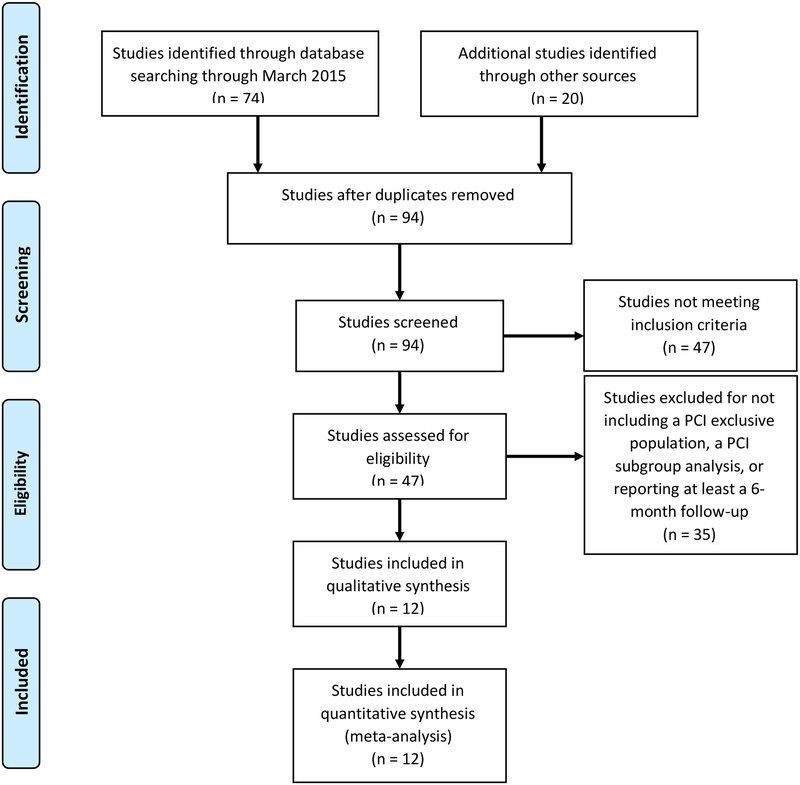
We identified 94 potentially relevant studies and screened each for inclusion, collecting data on study design, study size, follow-up length, PPI used, and both efficacy and safety. Of those, 82 were not used because they were not an exclusively PCI population, only provided pharmacodynamic or pharmacokinetic data, did not report on any of the relevant outcomes, or were not conducted for the minimum amount of time (Figure 1).
Figure 1:
Flow Diagram of Article Selection
The final analysis included 12 retrospective analyses of randomized control trials (2), health registries (3), claims databases (2), and institutional records (5), and comprised a total of 50,277 patients; no prospective studies of PCI patients were identified (Table 1). Eleven of the twelve included studies (42,295 patients, 19,695 on concomitant therapy) reported a MACE or other composite cardiovascular outcome, while one study only report MI as an outcome. 27–36 studies Included were conducted in a variety of countries over three continents (Asia, Europe, and North America), indicating broad international use of concomitant therapy in PCI patients. Overall, patient populations had similar proportions of comorbidities including hypertension, hyperlipidemia, diabetes mellitus, and smoking status (Table 2). Aspirin dose and PPI drug choice varied among studies with aspirin doses ranging from 75 mg per day to 325 mg per day, and individual PPIs including omeprazole, esomeprazole, pantoprazole, rabeprazole, or lansoprazole. Compared to cardiovascular outcomes, fewer studies reported on TIMI (3 studies) and GI (1 study) bleed outcomes.26,28,31,34 Of those reporting a TIMI bleed outcome, 2 reported a major bleed outcome and the other, Harjai et al. on a major or minor bleed outcome.28,31,34
Table 1:
Study Characteristics
| Study | Study design of included studies | Original study selection criteria | Aspirin dose | PPIs included (in order of most use) | Follow-up time | Individual outcomes reported | MACE or composite outcome definition |
|---|---|---|---|---|---|---|---|
| O’Donoghue et al. 200931 | Secondary retrospective analysis of the TRITON-TIMI 38 RCT | Patients who underwent PCI and were randomized into TRITON-TIMI 38 trial. | 75–162mg | Pantoprazole, Omerprazole, Esomeprazole, Landoprazole, Rabeprazole | 15 months | All-cause death, Cardiovascular death, MI, Stent thrombosis, TIMI major bleed | Cardiovascular death, MI, and stroke |
| Zairis et al. 20 1 030 | Retrospective cohort | Patients who underwent a coronary stenting due to stable angina or ACS | 100–325mg | Omeprazole | 1 year | Cardiovascular death, MI, Stent thrombosis | Cardiovascular death and hospitalization for nonfatal MI |
| Kreutz et al. 201032 | Retrospective cohort | Patients at least 18 years of age and had a hospitalization claim for a PCI with stent placement. | NS | Esomeprazole, Omeprazole, Pantoprazole, lansoprazole, Rabeprazole | 1 year | Cardiovascular death, MI, Stroke | Hospitalization for cerebrovascular event, ACS, Cardiovascular death, coronary revascularization |
| Tentzeris et al. 201033 | Prospective registry | Patients who underwent PCI and stent implantation | 100mg | Pantoprazole, Esomeprazole, Omeprazole, Lansoprazole, Rabeprazole | 1 year | All-cause death, Cardiovascular death, Stent thrombosis | All-cause death, re-ACS, or stent thrombosis |
| Evanchan et al. 201042 | Retrospective cohort | Patients who underwent PCI with stent placement. | NS | Not stated | 1 year | MI | No composite outcome |
| Rossini et al. 201134 | Retrospective cohort | Patients who underwent PCI and DES implantation | NS | Lansoprazole, Pantoprazole, Omeprazole | 1 year | All-cause death, Stent thrombosis, TIMI major bleed | All-cause death, MI, destabilizing symptoms leading to hospitalization, and nonfatal stroke |
| Harjai et al. 201128 | Retrospective cohort | Patients who underwent successful PCI of a native coronary artery or bypass graft for stable or unstable coronary artery disease | NS | Omeprazole, Esomeprazole (others not stated) | 6 months | All-cause death, MI, Stent thrombosis, TIMI major or minor bleed | All-cause death, MI, target vessel revascularization, and stent thrombosis |
| Burkard et al. 201235 | Secondary retrospective analysis of the BASKET RCT | Patients were an allcomer population undergoing PCI irrespective of the clinical indication | 100mg | Esomeprazole, Pantoprazole, Omeprazole, Lansoprazole | 3 years | MI | Cardiovascular death, nonfatal MI, target vessel revascularization |
| Aihara et al. 201226 | Retrospective cohort | Patients who underwent PCI including coronary stenting. | 200mg | Lansoprazole, Omeprazole, Rabeprazole | 1 year | All-cause death, MI, Stroke | All-cause death or MI |
| Gupta et al. 201036 | Retrospective cohort | Patients who underwent PCI | 75 mg | Rabeprozole, Omeprazole, Lansoprazole | 4 years | All-cause death | Cardiovascular and all-cause death, non-fatal MI, and target vessel failure |
| Banerjee et al. 201127 | Retrospective cohort | Patients who underwent PCI with coronary stent implantation | NS | Omeprazole, Lansoprazole, Esomeprazole, Pantoprazole, Rabeprazole | 1 year | All-cause death | All-cause death, nonfatal MI, and repeat revascularization |
| Zou et al. 201429 | Retrospective cohort | Patients who underwent PCI with DES placement | 100mg | Omeprazole, Esomeprazole, Pantoprazole | 1 year | Cardiovascular death, MI, Stent thrombosis | All-cause Death, MI, target vessel revascularization, target lesion revascularization CABG, stent thrombosis |
PPI-Proton Pump Inhibitor, MACE-Major Adverse Cardiovascular Event, PCI-Percutaneous Coronary Intervention, NS-Not Stated, DES-Drug-Eluting Stent, MIMyocardial Infarction, ACS-Acute Coronary Syndrome, CABG-Coronary Artery Bypass Graft
Table 2:
Patient Characteristics
| Study | N | Age (range) | Male | Hypertension | Hyperlipidemia | DM | Smoker |
|---|---|---|---|---|---|---|---|
| Aihara26 | |||||||
| +PPI | 500 | 68 (+/−11) | 363 (72.6%) | 356 (71.2%) | 415 (83.0%) | 204 (40.8%) | 223 (44.6%) |
| -PPI | 500 | 69 (+/−11) | 379 (75.8%) | 345 (69.0%) | 419 (83.8%) | 197 (39.4%) | 216 (43.2%) |
| Burkard35 | |||||||
| +PPI | 109 | 66.5 (+/−10.5) | 75 (68.8%) | 79 (72.5%) | 80 (73.4%) | 32 (29.4%) | 27 (24.8%) |
| -PPI | 692 | 63.3 (+/−11.3) | 553 (79.9%) | 450 (65.0%) | 525 (75.9%) | 119 (17.2%) | 206 (29.8%) |
| Harjai28 | |||||||
| +PPI | 751 | 66 (+/−11) | 463 (61.7%) | 548 (73.0%) | 591 (78.7%) | 225 (30.0%) | 160 (21.3%) |
| -PPI | 1902 | 64 (+/−12) | 1368 (71.9%) | 1237 (65.0%) | 1335 (70.2%) | 505 (26.6%) | 494 (26.0%) |
| Rossini34 | |||||||
| +PPI | 1158 | 64 (+/−11) | 875 (75.6%) | 736 (63.6%) | 762 (65.8%) | 314 (27.1%) | 571 (49.3%) |
| -PPI | 170 | 63 (+/−11) | 138 (81.2%) | 111 (65.3%) | 123 (72.4%) | 48 (28.2%) | 84 (49.4%) |
| Evanchan42 | |||||||
| +PPI | 1369 | 63.5 (NR) | NR | 837 (61.1%) | 850 (62.1%) | 630 (46.0%) | NR |
| -PPI | 4425 | 62.9 (NR) | NR | 2835 (64.1%) | 2734 (61.8%) | 1601 (36.2%) | NR |
| Kreutz32 | |||||||
| +PPI | 6828 | 67.5 (+/−10.4) | 4232 (62.0%) | 3454 (50.6%) | 4630 (67.8%) | 1767 (25.9%) | NR |
| -PPI | 9862 | 65.2 (+/−10.6) | 7290 (73.9%) | 4581 (46.5%) | 6254 (63.4%) | 2238 (22.7%) | NR |
| Zairis30 | |||||||
| +PPI | 340 | 62.1 (+/−10.5) | 280 (82.4%) | 173 (50.9%) | 226 (66.5%) | 102 (30.05) | 169 (49.7%) |
| -PPI | 248 | 61.7 (+/−10.8) | 203 (81.9%) | 115 (46.4%) | 162 (65.3%) | 65 (26.2%) | 126 (50.8%) |
| Tentzeris33 | |||||||
| +PPI | 691 | 64.1 (+/−12.4) | 452 (65.4%) | 509 (73.7%) | 528 (76.4%) | 129 (18.7%) | 193 (27.9%) |
| -PPI | 519 | 64.4 (+/−11.9) | 377 (72.6%) | 406 (78.2%) | 400 (77.1%) | 135 (26.0%) | 120 (23.1%) |
| O’Donoghue31 | |||||||
| +PPI | 2257 | 62 (+/−8) | 1587 (70.3%) | 1488 (65.9%) | 1274 (56.4%) | 547 (24.2%) | 828 (36.7%) |
| -PPI | 4538 | 60 (+/−8) | 3390 (74.7%) | 2883 (63.5%) | 2516 (55.4%) | 1023 (22.5%) | 1755 (38.7%) |
| Gupta36 | |||||||
| +PPI | 72 | 61.7 (+/−1.2) | NR | 55 (76.4%) | 48 (66.7%) | 26 (36.1%) | 18 (25.0%) |
| -PPI | 243 | 62 (+/−0.7) | NR | 166 (68.3%) | 146 (60.1%) | 73 (30.0%) | 81 (33.3%) |
| Banerjee27 | |||||||
| +PPI | 867 | 64.5 (+/−10.3) | 851 (98.2%) | 801 (92.4%) | 777 (89.6%) | 446 (51.4%) | 347 (40.0%) |
| -PPI | 3678 | 63.8 (+/−9.9) | 3615 (98.3%) | 3269 (88.9%) | 3141 (85.4%) | 1630 (44.3%) | 1428 (38.8%) |
| Zou29 | |||||||
| +PPI | 6188 | 66.2 (+/−10.2) | 4548 (73.5%) | 4412 (71.3%) | 3725 (60.2%) | 1597 (25.8%) | 1993 (32.2%) |
| -PPI | 1465 | 65.7 (+/−10.6) | 1083 (73.9%) | 1031 (70.4%) | 913 (62.3%) | 346 (23.6%) | 454 (31.0%) |
| Total/AVG | |||||||
| +PPI | 21130 | 64.1 | 13726 (69.7%)* | 13448 (63.6%) | 13906 (65.8%) | 6019 (28.5%) | 4529 (35.0%)* |
| -PPI | 28242 | 63.7 | 18396 (78.0%)* | 17429 (61.7%) | 18668 (66.1%) | 7980 (28.3%) | 4964 (35.6%)* |
DM-Diabetes Mellitus, NR-Not Reported, +PPI-With Proton Pump Inhibitor, -PPI- Without Proton Pump Inhibitor
-Percentages exclude populations without reported outcome
Heterogeneity assessment
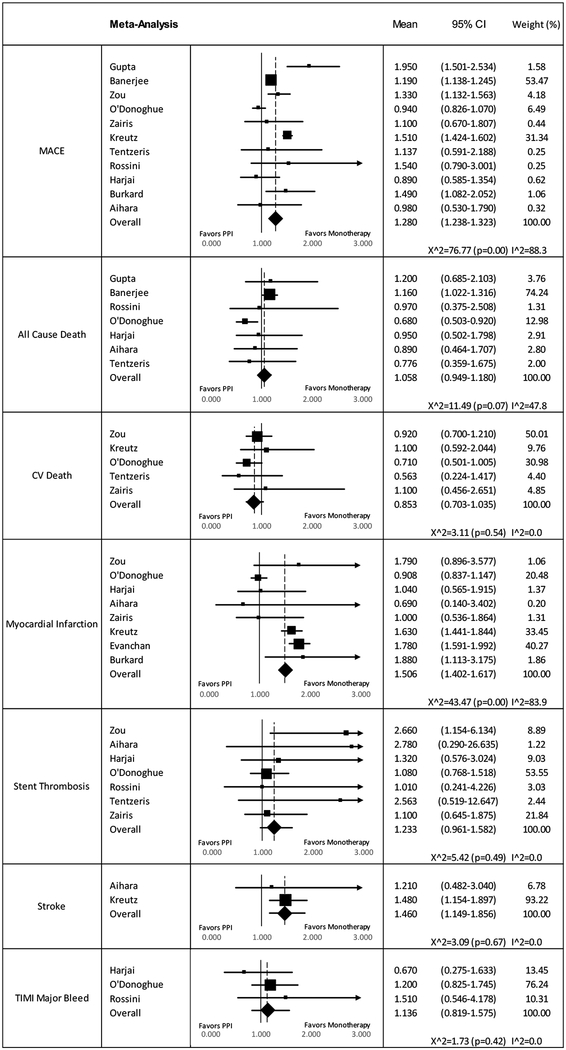
For the MACE composite outcome, Heterogeneity X2 was 77.57 p<0.005 and I2 was 87.1% displaying a high variability between studies. Comparing heterogeneity using the X2 and I2 statistics within each of the five listed outcomes under MACE generated the following results: a X2 of 11.49 (p=0.07) and an I2 of 47.8% for AC death, X2 of 3.11 (p=0.54) and I2 0% for CV death, X2 of 43.47 (p<0.05) and I2 of 83.9% for MI, X2 of 5.42 (p=0.49) and I2 0% for ST, and lastly X2 of 3.09 (p=0.67) and I2 0% for stroke. The statistically significant heterogeneity observed for MI could not be eliminated through exclusion of any single study. We did not identify evidence of heterogeneity for the safety outcome of TIMI bleed; X2 of 0.17 (p=0.678) and I2 of 0%.
Efficacy Outcomes
Concomitant therapy showed a statistically significant increase in composite MACE outcomes compared to clopidogrel monotherapy (HR 1.28; 95% CI 1.24–1.32) (Figure 2). Of the individual components of MACE there were statistically significant increases in risk with concomitant therapy for MI (HR 1.51; 95% CI 1.40–1.62) and stroke (HR 1.46; 95% CI 1.15–1.86). The other three outcomes of all-cause death (HR, 1.06; 95% CI 0.95–1.18), cardiovascular death (HR, 0.85; 95%CI, 0.70–1.04), and stent thrombosis 1.23 (95% CI 0.96–1.58) were not statistically significant.
Figure 2.
Results of Pooled Analyses for MACE and Individual Clinical Outcomes.
Safety Outcomes
The major bleed outcome had a pooled HR of 1.14 (95% CI 0.82–1.58), however, the pooled analysis could have been impacted by the grouping of both major and minor bleed in the Harjai study. When this study was removed from the analysis the pooled HR for the remaining studies was 1.23 (95% CI 0.87–1.75). Only one study reported a GI bleed outcome, and therefore no pooled analysis was conducted.
Sensitivity Analysis
The high level of heterogeneity in MACE could be due to the different criteria for the composite outcome, with many studies having little overlap in the criteria to constitute a MACE compared to others (Table 1). Attempts were made to separate out studies by similar definitions of the MACE outcome, yet the little overlap in composite outcome definition made any logical grouping with a majority of the eleven studies difficult.
In sensitivity analysis by single study exclusion for each outcome, the greatest differences were for AC death. Exclusion of Banerjee et al. changed the results in favor of concomitant therapy, to HR 0.81 (95% CI 0.66–1.01) while remaining not statistically significant, while the exclusion of O’Donoghue et al. made the results statistically significant with a HR of 1.06 (95% CI 1.01–1.27). For every other outcome the exclusion of any study did not significantly alter the results or the heterogeneity, except in MI where exclusion of O’Donoghue et al. changed the estimate to a HR of 1.68 (95% CI 1.55–1.82) and substantially altered the X2 to 7.68 (p=0.262) and I2 to 21.9%.
DISCUSSION
We conducted a meta-analysis of 12 studies that included a total of >50,000 PCI patients on concomitant therapy with clopidogrel and a PPI. We found concomitant therapy is associated with a significantly increased risk of adverse cardiovascular events. Individual cardiovascular outcomes of MI and stroke significantly increased with concomitant therapy; however, concomitant therapy had no trending effect on mortality measured by all-cause or cardiovascular death.
The potential health impacts of this interaction are considerable given that approximately 500,000 PCI procedures are performed annually in the United States alone.1,37,38 Our findings imply that clinical guidelines and practice should carefully consider this interaction, and that additional studies evaluating the impact of individual PPIs in this patient population are warranted.
The results of our study were directionally similar to those of other concomitant therapy meta-analyses on a broader population of patients. Huang et al. included a patient population of approximately 160,000 and found a statistically significant increase in MACE (HR: 1.40; 95% CI 1.19–1.64), however their findings for all-cause death, 1.30 (95% CI 0.91–1.86) and cardiovascular death, 1.21 (95% CI 0.60–2.43) were non-significant.21 In another recent meta-analysis by Focks et al., the odds ratio for MACE was found to be 1.63 (95% CI 1.45–1.83); however, the odds ratio was nominally non-significant in prospective studies, 1.13 (95% CI 0.98–1.30). Both of these large studies included non-PCI patients.20 In contrast, our study focused specifically on PCI patients, in whom the effect of this DDI could potentially have a larger absolute effect because of the higher baseline risk of MACE outcomes in PCI patients.
Current FDA recommendations warn against the use of concomitant therapy of clopidogrel with omeprazole or esomeprazole, but not other PPIs.10 Conversely, our study evaluated PPIs as a class and no separate analysis could be done for only combination therapy with omeprazole or esomeprazole because of a lack of subgroup reporting. However, a previous meta-analysis by Kwok et al. looked at this interaction by individual PPI type, and found that all PPIs displayed increases in MACE when taken with clopidogrel.22 This evaluation was not exclusively PCI patients; yet, the study showed that individual PPIs, such as the more potent CYP2C19 inhibitor omeprazole, might not be exclusive offenders of this DDI. Furthermore, a recent study by Shah et al. identified an independent association between PPIs and adverse cardiovascular events using a large data-mining approach, but this was also not specific to PCI patients.39
Evaluation of rare individual events such as all-cause or cardiovascular death would require extremely large studies to achieve sufficient statistical power to detect differences; hence the MACE composite outcome is typically used in clinical trials. When we explored individual outcomes we found a significant increase in MIs and strokes HR 1.51 (95% CI 1.40–1.62), HR 1.46 (95% CI 1.15–1.86) respectively, with concomitant therapy. Counter intuitively, outcomes of all-cause and cardiovascular death did not show a similar increased risk with combined therapy. The most likely explanation for this finding is that the studies were underpowered to assess mortality.
Limitations
A significant limitation of our study was that the composite MACE outcomes were not defined uniformly among the pooled studies. While most studies included some combination of MI, stroke, and/or cardiovascular death, the exclusion of any of these or the inclusion of additional outcomes such as stent thrombosis may have impacted our results. While an attempt was made to stratify based on MACE definition, the lack of overlap between studies made it difficult to pool studies in large enough groups to perform separate analyses. Other limitations included (1) not studying PPIs by individual drug, (2) the lack of standardization for aspirin dosage among studies, (3) non-uniform time to endpoint in each study, (4) a lack of studies reporting on gastrointestinal events and (5) possible confounding by indication, i.e., patients taking PPIs are more likely to be older and sicker and thus more likely to experience a MACE outcome, is a concern in all of the observational studies included in our analysis. The overall consistent increase in MIs and strokes exhibited in patients on concomitant therapy after a PCI suggest our findings are robust to some confounding factors.
A further limitation is the possibility of inconsistent quality between studies. Drepper et al. raised this issue in a systematic review of PCI and non-PCI patients; findings from three previous meta-analyses suggested high (well performed randomized-clinical trials) and moderate quality (post hoc analysis of RCTs and propensity matched studies) studies found a decreased MACE interaction, or lack of a statistically significant interaction, when compared to low quality studies (observational studies without propensity matching or adjustment).40 Thus unmeasured confounders might be a cause of the results in lower quality studies.41 In our study, where no high quality randomized control trials met inclusion criteria, separate analysis by study quality was not performed, however, all of the studies included in our analysis had either internal adjustments or used propensity matching. Yet, in the O’Donoghue study, a post hoc analysis of an RCT and likely the study of highest quality in our analysis, the MACE interaction HR showed no risk difference for concomitant therapy.31
Conclusion
In conclusion, our meta-analysis of studies evaluating PCI-specific patients receiving concomitant PPI-clopidogrel versus clopidogrel monotherapy patients suggests that concomitant therapy may be associated with an increased risk of major adverse cardiovascular events. These findings suggest caution should be used with the use of concomitant therapy following PCI, and limitation of PPIs for the most at-risk patients where gastrointestinal protection could outweigh the additional cardiovascular risks.
What is already known about the subject?
PPIs, including omeprazole and esomeprazole, inhibit CYP 2C19 metabolism to varying degrees and have been shown to have a pharmacokinetic effect on clopidogrel when administered concomitantly.
Meta-analyses have shown an increased risk of major adverse cardiovascular events with concomitant therapy, but none have focused on exclusively on high-risk PCI patients.
What this study adds?
This meta-analysis of PCI patients shows an increased risk of MACE with concomitant therapy.
The results of this study support limiting concomitant therapy following PCI to individuals at increased risk of gastrointestinal bleed where gastrointestinal protection could outweigh the risk of increased cardiovascular events.
Acknowledgments
DISCLOSURES
Serbin, Guzauskas and Veenstra were supported by the NIH Common Fund and NIA (1U01AG047109–01, Veenstra, PI) via the Personalized Medicine Economics Research (PriMER) project.
References:
- 1.Marso SP, Teirstein PS, Kereiakes DJ, Moses J, Lasala J, Grantham JA. Percutaneous coronary intervention use in the united states: Defining measures of appropriateness. JACC Cardiovasc Interv. 2012;5(2):229–235. [DOI] [PubMed] [Google Scholar]
- 2.Eikelboom JW, Hirsh J, Spencer FA, Baglin TP, Weitz JI. Antiplatelet drugs: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e89S–119S. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278069/ Accessed 11/11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatt DL, Cryer BL, Contant CF, et al. Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med. 2010;363(20):1909–1917. Available at: http://www.nejm.org/doi/full/10.1056/NEJMoa1007964 Accessed 11/11, 2015. [DOI] [PubMed] [Google Scholar]
- 4.Arbel Y, Birati EY, Finkelstein A, et al. Platelet inhibitory effect of clopidogrel in patients treated with omeprazole, pantoprazole, and famotidine: A prospective, randomized, crossover study. Clin Cardiol. 2013;36(6):342–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gilard M, Arnaud B, Cornily JC, et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: The randomized, double-blind OCLA (omeprazole CLopidogrel aspirin) study. J Am Coll Cardiol. 2008;51(3):256–260. [DOI] [PubMed] [Google Scholar]
- 6.Holmes MV, Perel P, Shah T, Hingorani AD, Casas JP. CYP2C19 genotype, clopidogrel metabolism, platelet function, and cardiovascular events: A systematic review and meta-analysis. JAMA. 2011;306(24):2704–2714. [DOI] [PubMed] [Google Scholar]
- 7.Gaglia MA Jr, Torguson R, Hanna N, et al. Relation of proton pump inhibitor use after percutaneous coronary intervention with drug-eluting stents to outcomes. Am J Cardiol. 2010;105(6):833–838. [DOI] [PubMed] [Google Scholar]
- 8.Mega JL, Simon T, Collet JP, et al. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: A meta-analysis. JAMA. 2010;304(16):1821–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kazui M, Nishiya Y, Ishizuka T, et al. Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab Dispos. 2010;38(1):92–99. [DOI] [PubMed] [Google Scholar]
- 10.Interaction between esomeprazole/omeprazole and clopidogrel label change. http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm327922.htm. Updated 2012. Accessed 06/21, 2015. [Google Scholar]
- 11.Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: A report of the american college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol. 2014;64(24):e139–228. [DOI] [PubMed] [Google Scholar]
- 12.Abraham NS, Hlatky MA, Antman EM, et al. ACCF/ACG/AHA 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines: A focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. Am J Gastroenterol. 2010;105(12):2533–2549. [DOI] [PubMed] [Google Scholar]
- 13.American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, O’Gara PT, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the american college of cardiology foundation/american heart association task force on practice guidelines. J Am Coll Cardiol. 2013;61(4):e78–140. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt M, Johansen MB, Robertson DJ, et al. Concomitant use of clopidogrel and proton pump inhibitors is not associated with major adverse cardiovascular events following coronary stent implantation. Aliment Pharmacol Ther. 2012;35(1):165–174. [DOI] [PubMed] [Google Scholar]
- 15.Ray WA, Murray KT, Griffin MR, et al. Outcomes with concurrent use of clopidogrel and proton-pump inhibitors: A cohort study. Ann Intern Med. 2010;152(6):337–345. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3176584/ Accessed 11/11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stockl KM, Le L, Zakharyan A, et al. Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor. Arch Intern Med. 2010;170(8):704–710. [DOI] [PubMed] [Google Scholar]
- 17.Goodman SG, Clare R, Pieper KS, et al. Association of proton pump inhibitor use on cardiovascular outcomes with clopidogrel and ticagrelor: Insights from the platelet inhibition and patient outcomes trial. Circulation. 2012;125(8):978–986. Available at: http://circ.ahajournals.org/content/125/8/978.long Accessed 11/11, 2015. [DOI] [PubMed] [Google Scholar]
- 18.Garcia Rodriguez LA, Johansson S, Cea Soriano L. Use of clopidogrel and proton pump inhibitors after a serious acute coronary event: Risk of coronary events and peptic ulcer bleeding. Thromb Haemost. 2013;110(5):1014–1024. doi: 10.1160/TH13-03-0225 [doi]. [DOI] [PubMed] [Google Scholar]
- 19.Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009;301(9):937–944. [DOI] [PubMed] [Google Scholar]
- 20.Focks JJ, Brouwer MA, van Oijen MG, Lanas A, Bhatt DL, Verheugt FW. Concomitant use of clopidogrel and proton pump inhibitors: Impact on platelet function and clinical outcome- a systematic review. Heart. 2013;99(8):520–527. [DOI] [PubMed] [Google Scholar]
- 21.Huang B, Huang Y, Li Y, et al. Adverse cardiovascular effects of concomitant use of proton pump inhibitors and clopidogrel in patients with coronary artery disease: A systematic review and meta-analysis. Arch Med Res. 2012;43(3):212–224. [DOI] [PubMed] [Google Scholar]
- 22.Kwok CS, Jeevanantham V, Dawn B, Loke YK. No consistent evidence of differential cardiovascular risk amongst proton-pump inhibitors when used with clopidogrel: Meta-analysis. Int J Cardiol. 2013;167(3):965–974. [DOI] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Open Med. 2009;3(3):e123–30. [PMC free article] [PubMed] [Google Scholar]
- 24.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: An update. Contemp Clin Trials. 2007;28(2):105–114. [DOI] [PubMed] [Google Scholar]
- 25.Symons MJ, Moore DT. Hazard rate ratio and prospective epidemiological studies. J Clin Epidemiol. 2002;55(9):893–899. [DOI] [PubMed] [Google Scholar]
- 26.Aihara H, Sato A, Takeyasu N, et al. Effect of individual proton pump inhibitors on cardiovascular events in patients treated with clopidogrel following coronary stenting: Results from the ibaraki cardiac assessment study registry. Catheter Cardiovasc Interv. 2012;80(4):556–563. [DOI] [PubMed] [Google Scholar]
- 27.Banerjee S, Weideman RA, Weideman MW, et al. Effect of concomitant use of clopidogrel and proton pump inhibitors after percutaneous coronary intervention. Am J Cardiol. 2011;107(6):871–878. [DOI] [PubMed] [Google Scholar]
- 28.Harjai KJ, Shenoy C, Orshaw P, Usmani S, Boura J, Mehta RH. Clinical outcomes in patients with the concomitant use of clopidogrel and proton pump inhibitors after percutaneous coronary intervention: An analysis from the guthrie health off-label stent (GHOST) investigators. Circ Cardiovasc Interv. 2011;4(2):162–170. Available at: http://circinterventions.ahajournals.org/content/4/2/162.long Accessed 11/11, 2015. [DOI] [PubMed] [Google Scholar]
- 29.Zou JJ, Chen SL, Tan J, et al. Increased risk for developing major adverse cardiovascular events in stented chinese patients treated with dual antiplatelet therapy after concomitant use of the proton pump inhibitor. PLoS One. 2014;9(1):e84985 Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3885647/ Accessed 11/11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zairis MN, Tsiaousis GZ, Patsourakos NG, et al. The impact of treatment with omeprazole on the effectiveness of clopidogrel drug therapy during the first year after successful coronary stenting. Can J Cardiol. 2010;26(2):e54–7. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2851393/ Accessed 11/11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Donoghue ML, Braunwald E, Antman EM, et al. Pharmacodynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: An analysis of two randomised trials. Lancet. 2009;374(9694):989–997. [DOI] [PubMed] [Google Scholar]
- 32.Kreutz RP, Stanek EJ, Aubert R, et al. Impact of proton pump inhibitors on the effectiveness of clopidogrel after coronary stent placement: The clopidogrel medco outcomes study. Pharmacotherapy. 2010;30(8):787–796. [DOI] [PubMed] [Google Scholar]
- 33.Tentzeris I, Jarai R, Farhan S, et al. Impact of concomitant treatment with proton pump inhibitors and clopidogrel on clinical outcome in patients after coronary stent implantation. Thromb Haemost. 2010;104(6):1211–1218. [DOI] [PubMed] [Google Scholar]
- 34.Rossini R, Capodanno D, Musumeci G, et al. Safety of clopidogrel and proton pump inhibitors in patients undergoing drug-eluting stent implantation. Coron Artery Dis. 2011;22(3):199–205. [DOI] [PubMed] [Google Scholar]
- 35.Burkard T, Kaiser CA, Brunner-La Rocca H, et al. Combined clopidogrel and proton pump inhibitor therapy is associated with higher cardiovascular event rates after percutaneous coronary intervention: A report from the BASKET trial. J Intern Med. 2012;271(3):257–263. [DOI] [PubMed] [Google Scholar]
- 36.Gupta E, Bansal D, Sotos J, Olden K. Risk of adverse clinical outcomes with concomitant use of clopidogrel and proton pump inhibitors following percutaneous coronary intervention. Dig Dis Sci. 2010;55(7):1964–1968. [DOI] [PubMed] [Google Scholar]
- 37.Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: What the clinician needs to know. Therap Adv Gastroenterol. 2012;5(4):219–232. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3388523/ Accessed 11/11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Donald Cutlip M Antiplatelet therapy after coronary artery stenting. http://www.uptodate.com/contents/antiplatelet-therapy-after-coronary-artery-stenting. Updated 2015. Accessed 7/20, 2015. [Google Scholar]
- 39.Shah NH, LePendu P, Bauer-Mehren A, et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS One. 2015;10(6):e0124653 Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462578/ Accessed 11/11, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drepper MD, Spahr L, Frossard JL. Clopidogrel and proton pump inhibitors--where do we stand in 2012? World J Gastroenterol. 2012;18(18):2161–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kwok CS, Loke YK. Meta-analysis: The effects of proton pump inhibitors on cardiovascular events and mortality in patients receiving clopidogrel. Aliment Pharmacol Ther. 2010;31(8):810–823. [DOI] [PubMed] [Google Scholar]
- 42.Evanchan J, Donnally MR, Binkley P, Mazzaferri E. Recurrence of acute myocardial infarction in patients discharged on clopidogrel and a proton pump inhibitor after stent placement for acute myocardial infarction. Clin Cardiol. 2010;33(3):168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]