Abstract
This paper proposes a framework based on the collective intelligence principle to understand how the healthcare ecosystem is facing the challenges posed by the COVID-19 by using the Internet of Things (IoT) combined with other digital technologies. The underlying assumption is to consider the Healthcare ecosystem as a collective intelligence system in which the multitude of actors can be coordinated to address the pandemic-specific management challenges. The Italian healthcare ecosystem is analyzed as scenario taking in consideration the ‘genes’ of the collective intelligence: What is being done?, Who is doing it?, Why are they doing it? and How is it being done?. Our analysis introduces policy implications based on a unique decision support system (DSS) to allocate a limited set of IoT devices to a larger group of patients, to balance the alternative needs to improve the conditions of the most severe patients but to maximize the efficiency of device use.
Keywords: Collective intelligence, COVID-19, Digital technologies, Healthcare ecosystem, Internet of Things (IoT), Pandemic
1. Introduction
The year 2020 was supposed to be the beginning of an exciting decade in medicine and science, with the development and maturation of several digital technologies to be applied to address major clinical problems and disease (Bardhan et al., 2020, Ting et al., 2020). But the urgent management of the health crisis caused by the new coronavirus (COVID-19), suddenly increased the adoption of digital technologies (Ienca and Vayena, 2020, Keesara et al., 2020, Majumdar et al., 2018, Xiang et al., 2020) such as big data, wireless communications and social networks, apps and global position systems (GPS), Internet of things (IoT), Artificial Intelligence (AI). This to collect and process large amounts of data in multiple contexts to support decision-making processes, businesses, and policies (European Commission, 2017, Nambisan, 2017, Nambisan et al., 2017, Trequattrini et al., 2016). Over the past 10 years digital technologies have started to be used for specific needs of the healthcare ecosystem such as telemedicine. During the global pandemic, such digital technologies have become vital for healthcare and to support the management of this disease (World Health Organization (WHO), 2020; Italian National Institute of Health, 2020; UNESCO, 2020). Prior the current diffusion of COVID-19, the most visible uses of emerging technologies, such as artificial intelligence (AI), social media and big data, have been in the entertainment or manufacturing industries; now, their potential application has reached far beyond across different sectors. Internet of things (IoTs) and next-generation telecommunication networks (e.g., 5G), big-data analytics, AI using deep learning and block-chain technology are enabling seamless interaction among several disposals connected to the patients. The digitally enhanced healthcare system will have the potential to allow individuals to be more directly informed about their care and to become responsible in managing their health (Bardhan et al., 2020, Young et al., 2013, Ting et al., 2020, Wang et al., 2020). In this scenario, governments and policymakers are taking several actions including contact tracing through smart technologies to prevent and manage the pandemic.
The contribution of digital technology to the COVID-19 pandemic management can take many forms and bring significant value (Ting et al., 2020). Thus, the investigation of big data and AI is connected to epidemic disasters (Shaluf, 2007), which have been plaguing our planet for decades (e.g. the Spanish flu, avian flu, Ebola, SARS, MERS and SARS-COV-2), as an interesting and important research-stream.
Along with the wide adoption of digital health technologies, another interesting phenomenon can be observed, related to the collective actions taken by the different stakeholders involved within the Healthcare Ecosystem (Iyawa et al., 2016, Secundo et al., 2019). Physicians, epidemiologists, supranational institutions, ministry, hospitals, device suppliers, and all the organizations that are contributing to reduce the spread of the pandemic are coordinating their efforts. Whereas the relevant actions are attempting to comply with the requirements related to quarantine, outbreak clusters and country lockdowns due to the absence of an effective specific vaccine. In this disruptive scenario, while the digital revolution (Shams and Solima, 2019, Verhoef et al., 2019) has “reshaped” the corporate sector (Elia, Margherita, & Passiante, 2020) and the academic context (Rippa & Secundo, 2019), the revolution towards their use to support, manage and overcome the COVID-19 outbreak (Ting et al., 2020) has yet to be explored (Wang et al., 2020). In this context, Adivar and Selen (2013) launched the call for further research on epidemics and their management: “Epidemics have occurred many times in the past and will continue to affect populations in the future…. It is important to emphasize the need for further research in both developing and developed countries because of the ease of dispersion, which constitutes a universal threat”. Accordingly, and coherently with the special issue goal, our aim is to explore the Healthcare ecosystem as a collective intelligence system comprised of multiple stakeholders (Shams, 2016), where the novel digital health technologies can support the management of this global pandemic. Specifically, taking the metaphor from biology (Malone et al., 2008, Malone et al., 2010), the framework is divided into four main blocks or genes that exploit epidemic disease management. The genes specifically aim to answer four questions: “What is being done?”, “Who is doing it?”, “Why it is done?”, and “How it is done?”. These questions provide the conceptual pillars to describe an comprehensive integrated approach on the application of digital technologies for health management and personalized care. Our findings are based on the influence of the Internet of Things (IoTs) combined with other digital technologies. In particular, we provide a framework for healthcare ecosystem focused on the analysis of the components or building blocks related to collective intelligence principle to understand how the healthcare ecosystem is facing the challenges posed by the COVID-19. Increasing healthcare management for the COVID-19 crisis is therefore a strategic priority for governments around the world to contribute to social welfare. This is achieved through optimizing IoT adoption because, due to budget, there is always a limit in terms of available IoT devices. A real healthcare ecosystem scenario, considered as a collective intelligence ecosystem, focuses on allocating a limited set of IoT devices to a heterogeneous set of patients. For this reason, we developed a decision support system (DSS), based on an optimization model, to help managers and service providers (physicians, hospital directors, and policy makers) support the management of patient-specific device allocation. The implications for practice and policy of our findings offer a system optimization model for allocating a limited set of IoT devices to a larger group of patients. We keep a balance between the need of improving the condition of the most severe patients and maximizing of the efficiency of the device use.
This paper is organized as follows. Section 2 analyses how digital technologies are being used in the healthcare ecosystem. Section 3 outlines the healthcare ecosystem as a collective intelligence system illustrating and discussing the application of all building blocks. Section 4 provides an application scenario of a multi-purpose optimization system of IoT device assignment, in order to allocate the devices to different patients in order to ensure optimal use of limited resources (e.g. the digital devices). Finally, Section 5 provides concluding remarks.
2. Digital technologies in the HealthCare ecosystem
Healthcare ecosystems involve a wide range of actors (patients, physicians, nurses, companies and government bodies, suppliers tech..). They incorporate knowledge flows originated from or co-produced with external actors such as academic researchers, research centers, industry, government, NGOs and public institutions with the aim of pursuing a collective goal (Secundo et al., 2019). The rapid adoption of digital technologies to address the global health crisis is generating new strategic and innovation frameworks in the health ecosystem (Hadzic and Sidhu, 2008, Ienca and Vayena, 2020, Keesara et al., 2020). Today, many other issues have emerged from the pandemic, but one enlightening aspect is the use of digital technology to manage the global health emergence (Ienca and Vayena, 2020, Keesara et al., 2020).
The press also discusses the role of IoT, big data and AI being used by governments to collect, manage, and prevent COVID- 19 (SARS-COV-2). COVID-19 and its myriad impacts are undeniably reshaping economies around the world for years and even decades to come (Brown, Collins, Lyke-Ho-Gland, Trees, & Tucker, 2020). Within a few days, starting in early March 2020, hospitals around the world have been forced to address the pandemic-specific health crises to an unpredictable dimension. In this emergency, new needs emerged, addressing with the existing challenges that were already putting the entire healthcare sector under enormous pressure and uncertainty. Until a decade ago, it was virtually impossible to track diseases. Today, using AI, machine learning, big data analytics and Global Information System (GIS), data mining and extracting insights, it is easier and more powerful to identify the location of viruses, in order to have a quicker response.
Such digital technologies are rapidly supporting the efficiency of the healthcare ecosystem. The time for new digital technologies theories invites scholars to deepen their analyses regarding to the use of digital technologies for solving the global crisis of healthcare management. Several scholars proposed different approaches and technological tools. For example, Cappelle et al. (2011) developed a GIS-based methodology in estimating of epidemiological contact rates. Hirsch, Winters, Clarke and McKay (2014) investigated the global positioning system (GPS) as opportunity to measure, describe, and compare mobility patterns in elderly health, assuming that this technology can become a powerful tool to accurately describe the interaction of people within a particular geographic space. Koylu, Delil, Guo, and Celik (2018) investigated the patient mobility system through a data-driven approach; Munyaneza et al. (2014) analyzed the same topic focusing on GIS. Young et al. (2013) investigated the role of AI through the machine learning approach connecting it to the epidemiology landscape.
Global healthcare issues, due to the pandemic emergence, include the increasing demand to provide adequate care to a growing number of COVID-19 patients, monitoring the growing number of infected people, the demand to manage unmet medical needs of non-COVID-19 patients, and the extension of service for non-emergency patients. Last but not least, the need to address budget constraints (Massaro et al., 2015, Yu et al., 2015) that has forced the governments around the world to optimize the adoption and use of ad hoc digital technologies such as smart devices only for critically ill patients. For instance, digital technologies can support the management and the coordination among healthcare institutions in several way (IBIMA et al., 2020). For example, social media can improve public health education and communication (Ting et al., 2020) such as WeChat, has been widely used as a way of communication, information sharing, administration and supervision in China. Big data enables the collection of data that can be used both for training new physicians and improving existing care techniques for COVID-19. In addition, big data also provides opportunities to perform viral activity pattern studies and guide health policy makers to support their preparedness for pandemic-specific health management.
By taking a comprehensive approach to digital technologies, healthcare institutions can deliver care and services to patient faster, ensure a safer society, and minimize costs. Urgent action is required to transform the delivery of healthcare service and to scale up our systems by unleashing the power of digital technologies (Keesara et al., 2020); as digitalization can lead to greater effectiveness by providing specialized care to relatively more people. Convergent thinking across different studies has led to the development of several definitions and many frameworks to develop insights related to specific digital healthcare ecosystems (Hadzic and Sidhu, 2008, Iyawa et al., 2016). A digital healthcare ecosystem is defined as a health ecosystem supported by digital technologies (Carroll, Cnossen, Schnell, & Simons, 2007), which allows for sufficient capacity to adequately treat patients infected with COVID-19, protect health care workers involved in fighting the pandemic, while caring for other patients with acute disease (Bashshur, Doarn, Frenk, Kvedar, & Woolliscroft, 2020). Among the digital technologies supporting healthcare ecosystem, Galetsi, Katsaliaki, and Kumar (2019) conducted a systematic review of using big data analytics in healthcare to show the clear value of big data analytics for improving public health and resource allocation. Georgalakis (2020) used from UCINet (a social network analysis software) to build a visualized network to understand the connection between policymakers and scientists. Other studies discussed the use of big data in the healthcare sector (e.g., Brunswicker et al., 2015, Hilbert, 2016, Zillner et al., 2014), emphasizing improvements in quality of care, by capturing and processing of streams of information about patient behaviors in real time.
Although we are aware of the many promising digital technologies available today to fuel epidemic management in the healthcare ecosystem, we decided to restrict our analysis to the following technologies: Internet of Things, big data analytics and artificial intelligence.
3. The healthcare ecosystem as a collective intelligence system
To provide an comprehensive interpretation of the outbreak management caused by COVID-19, we assume that the healthcare ecosystem is a collective intelligence system of multiple stakeholders that can be supported by digital technologies. To design a novel framework, the collective intelligence approach (Boder, 2006, Lévy, 1994, Malone et al., 2008) is adopted as our research approach, assuming that the healthcare ecosystem is a collective intelligence system. In the next subsections of this section, our conceptual framework is clarified by starting with collective intelligence as our research approach and then justifying our framework based on its application the Italian healthcare ecosystem.
3.1. The collective intelligence as a research approach
The basic idea of collective intelligence, which emerged in the late 1970s and then formalized in the 1990s, concerns a shared or group intelligence that arises from the collaboration and competition of many individual stakeholders (Boder, 2006, Lévy, 1994, Malone et al., 2008). The term ‘collective’ describes a group of individuals or stakeholders, who are not necessarily required to have the same attitudes or viewpoints, but work together to find solutions to a given problem. ‘Intelligence’ refers to the ability to learn, to understand and to adapt to an environment by using knowledge (Leimeister, 2010).
According to Lévy (1994), collective intelligence describes a phenomenon in which, under conditions of diversity (of the people involved /stakeholders), independence (individual's contributions are not influenced by those of other individuals) and aggregation (mechanisms for pooling and processing individual estimation into a collective estimation), large groups can perform better than any individual in the group. This phenomenon is also known as ‘wisdom of crowds’ (Surowiecki, 2004). In broader sense, collective intelligence studies how people or different stakeholders and technologies can be connected so that, collectively, the multiple stakeholders act smarter than any individual, group, or computer has ever done before (Malone et al., 2008, Malone et al., 2010). Thus, a collective intelligence system allows the knowledge, experience and resources of potentially thousands of individuals with the ultimate goal of solving a complex problem to collectively address complex issues or to achieve a common (though not necessarily consensual) goal (Mulgan, Mateos-Garcia, Marston, & Westlake, 2012).
The Massachusetts Institute of Technology (MIT) provided the following definition: “Collective intelligence is a group of individuals doing things collectively that seem intelligent” (Malone, 2006). The MIT researchers used an analogy from biology to identify the so-called building blocks, or ‘genes’, of the collective intelligence system. They define a gene as a particular answer to one of the key questions (what, who, why or how) associated with a single task in a collective intelligence system. Like the genes from which individual organisms develop, these organizational genes are the key elements from which collective intelligence systems evolved. The entire combination of genes associated with a specific example of collective intelligence can be viewed as the ‘genome’ of that system (Malone et al., 2010). To classify these building blocks, four questions have been defined: (1) what is being done? (2) Who is doing it? (3) Why are they doing it? (4) How is it being done? (Malone et al., 2010). The following is a brief description.
What? The organisation’s mission. It is obtained through two actions: create, the actors generate something new, and/or decide, the actors evaluate and select alternative actions. Identifying the basic goal determines which of these two genes are used to define new situations.
Who? The people involved in the actions developed to achieve the mission. People can be: hierarchy, someone in authority assigns a particular person or group of people to perform the task; or crowd, activities can be undertaken by anyone in a large group without being assigned by someone in a position of authority.
Why? The motivations behind the actions. These can be the motivations based on the intrinsic enjoyment of an activity; the recognition to be assigned to people, and finally, the financial gain as an important motivator for most actors in markets and traditional organizations.
How? Whether the different members of the crowd make their contributions and decisions independently of each other or whether there are strong dependencies between them. This insight gives rise to four types of ‘how’ genes associated with the actions ‘create’ and ‘decide’. The two ‘how’ genes associated with the create task are ‘collection’ and ‘collaboration’. Collection occurs when the items developed by members of the crowd are created independently to each other. Collaboration occurs when members of a crowd work together to create something with dependencies existing between their contributions. The two ‘how’ genes associated with the decide task are ‘group decision’ and ‘individual decisions’. Group decision occurs when inputs from members of the crowd are assembled to generate a decision that holds for the group as a whole. Individual decision occurs when the members of a crowd make decisions that, though informed by crowd input, do not need to be identical for all (Malone et al., 2010).
3.2. Research context
The health care system in Italy is a regionally based national health care service system called the Servizio Sanitario Nazionale (SSN). It provides free universal coverage at the point of service. While the SSN ensures that the overall goal and fundamental principles of the national health care system are met, regional governments in Italy are responsible for ensuring the delivery of a package of services to the population. Healthcare facilities vary in quality in different regions of Italy. During the initial phase of the COVID-19 pandemic in late February 2020, regional areas in Italy were most affected, including Lombardy and Veneto. When the Italian government issued the Decree of March 9, 2020 declaring the country lockdown, the healthcare ecosystem started unprecedented period of emergency with the need to address the complex challenges, based on collective collaborations.
3.3. Healthcare ecosystem: A collective intelligence in action
In the healthcare ecosystem, one crucial aspect has emerged during the first phase of the global pandemic management is the predominant nature of “self-organization” at local level, supported by some national and international orchestrating entity. Moreover, the existence of a complex set of goals and motivating factors that drive the involvement of ecosystem actors (physicians, volunteers, health device providers and inventors of, nurses, among others), along with the presence of a set of interconnections through the digital technologies (Gasser, Ienca, Scheibner, Sleigh, & Vayena, 2020), provides the health ecosystem with a characteristic typical of a collective intelligence system. The potential of adopting a collective intelligence framework may lie into two considerations. First, the management of the first phase of the COVID-19 challenges, is a complex and articulated process characterized by great uncertainty that can benefit from the collaboration of individuals and systems at a different level. Second, the use of digital technologies can streamline the dissemination of information to all stakeholders and amplify the impact of networking and sharing critical knowledge and expertise that would be useful in planning the next phase of the epidemic management.
Connections and coordination among stakeholders in the health ecosystem, such as hospitals and all the other institutions involved in health policy (i.e. the Italian National Institute of Health, regional health organizations, municipalities, WHO), enabled patients and their family to gain the support of well-managed digital technologies, such as IoT, social media, Cloud computing, big data analytics, and AI, as they are used in a synchronized way to communicate with families and for patient care based on an improved community health system. The collective intelligence framework for the digital healthcare ecosystem fighting the global epidemic is clarified through the key questions of what, who, how, and why questions that are discussed in the previous section (Malone et al., 2008, Malone et al., 2010). Fig. 1 illustrates the MIT Genoma model that was applied to the healthcare ecosystem during the COVID-19 pandemic.
Fig. 1.
The Healthcare Ecosystem as a collective intelligence ecosystem.
Below is a detailed description for each building block follows.
‘What is being done?: the goals of healthcare ecosystem in fighting against the COVID-19′. A digital healthcare ecosystem is a self-organizing community of interdependent actors, able to seize (technology-based) opportunities by leveraging the existence of a complex system of (digital) services and tools that enable actions and interactions across all different phases of the epidemic disease management. Objectives include two traditional public-health strategies for tackling COVID-19: (1) monitoring, surveillance, detection and prevention of COVID-19; and (2) mitigation of the impact to healthcare indirectly related to COVID-19.
‘Who is doing it? Defines the actors of the healthcare ecosystem’. Stakeholders around the world (from policymakers at global, national, and local levels, to other associated organizations and patients) need to make decisions that affect many lives and livelihoods across the world. Several disparate datasets, dashboards, information portals and repositories have been developed, aiming at providing frontline leaders and policy makers with critical information about the spread of the pandemic around the world. The ability to translate data into actionable insights from the several actors involved within the healthcare ecosystem became the priority during the pandemic management period. They can be classified as follows (Bessant, Künne, & Möslein, 2012):
-
•
regulators: Ministry of Health, National or Regional Committees who set regulatory guidelines;
-
•
providers: doctors, nurses and other health professionals who provide care in hospitals, doctor’s surgeries, nursing homes and others;
-
•
payers: statutory health insurance, private health insurance and government agencies;
-
•
suppliers: scientific institutions, universities, pharmaceutical and medical technology companies, who develop new products and devices for treatment; pharmacies and wholesalers, who mostly do resale; and
-
•
patients: beneficiaries of care.
The main obstacle in such healthcare ecosystems is an appropriate level of coordination between Institutions (Ministry of Health, AGID – National Agency for Digital Italy and State Regions Conference) and the Italian National Institute of Health to take useful actions to improve the supply-demand ratio through the use of IoT services and applications.
‘Why?’: the vision of healthcare ecosystem in fighting the COVID-19.
The Italian National Institute of Health in association of the other government institutions provided the guidelines to reduce the expansion of the epidemic disease and then to take care of the infected people while assuring the care assistance to the chronic patients. The health ecosystem is behaving as a system of collective intelligence through the lever of the crowd that is coordinating to create more favorable conditions for managing of public health in Italy and especially where the emergency has been managed, thanks to the availability of nurses, physicians and doctors also from other countries, such as Albania, Brazil, Poland influenced by the ultimate goal of motivation and love for their work.
‘How?’ Includes a set of processes and actions, which are enhanced bydigital technologies to achieve main goal.
Collective intelligence leverages collaboration to create more favorable conditions when both internal and external stakeholders are involved. It is important to distinguish between collective intelligence driven mainly by human physical connections over a limited geographical region and forms of collective intelligence that are global as enabled and augmented by digital information technology and digital services (Elia et al., 2020). To control this epidemic in various Italian regions, it is important to appropriately manage patients suspected of having the disease, immediately identify and isolate the source of infection, cut off the transmission route, and prevent viral transmission from these potential patients or virus carriers. Early data suggests that digital health solutions that relate to COVID-19 in Italy during the lockdown period includes:
-
•
e-Health consultations. e-Health (where a doctor speaks to the patient via a video conference and gives advice) has increased as people are locked down. For example, it is performing about 620 digital visits per day (up from previous 20).
-
•
Digital diagnostics. The next step from digital health is the inclusion of IoT devices to perform digital diagnostics. Hospitals are still experimenting with this. However, consumers are leading the way.
-
•
Remote monitoring. Remote monitoring, particularly of the elderly, is also on the rise. Livongo Health, which provides a line of remote IoT monitoring solutions for “chronic diseases” that increase the risk of dying due to COVID-19, unexpectedly raised its quarterly guidance on April 7, 2020.
-
•
Robot assistance. In particular, robots have been used to disinfect and clean hospitals and perform medical delivery.
The next section illustrates the detailed view of the digital technologies adopted in the Italian healthcare system.
4. The digital technologies fighting for the epidemic disease management
Although some digital technologies, such as those used for telemedicine, have existed for decades, they have had little market penetration due to heavy regulation and poor supportive payment structures (Keesara et al., 2020). During the lockdown in Italy (March – May 2020), digital technologies started to strategically support all the processes related to the healthcare ecosystem. In this section, we explore the potential application of three interrelated digital technologies (the IoT, big-data analytics and AI) in connection to augmenting the following traditional public health strategies to address COVID-19: (1) monitoring, surveillance, detection and prevention of COVID-19; (2) mitigation of the impact to healthcare indirectly related to COVID-19 and (3) Assuring the care assistance to the chronic patients (see Table 1 ).
Table 1.
Digital technologies and their impact on Italian healthcare strategies.
| Strategic Objectives |
|||
|---|---|---|---|
| 1 - Monitoring, detection and prevention of COVID-19; | 2 - Mitigation of the impact to healthcare indirectly related to COVID-19. | 3 - Assuring the care assistance to the chronic patients. | |
| Big data | [+++] Light Contact Tracing (European Approach), infection rates, virus DNA analysis, identify potential patients, prevention methods, lockdown decision, lockdown exit strategies. | [+] Italian National Institute of Health Budget Simulation Strategies, Health Resource allocation, Emergency unit management, healthcare stakeholders connection | [+] Out-of-control patient detection, Social distancing campaign, identify high-risk patients |
| IoT, Wearable devices | [+++] Strong Contact Tracing (China Approach), lockdown monitoring, contactless payment, home monitoring for non-critical patient | [++] Human resource reduction, care path optimization, critical alert detection, smart working, predictive maintenance, smart inventory management, 3D printing of medical supplies | [+++] Remote patient monitoring, Healthcare reminder, Continuous Glucose Monitors, Smart inhalers, Smart sensors for health conditions, visit cost reduction |
| Artificial Intelligence | [++] Predictive analysis of progress, outbreak detection, vaccine development, disease management, new drug development, identify patients at high risk. | [++] Connecting healthcare systems and providers with each other and with public health. Tracking people with facial recognition. Fighting misinformation, identity patient | [+] Medical Chat Bot. Identify specific groups of high-risk patients due to lockdown (reduced mobility, social isolation). |
The likely impact of digital technologies on “monitoring, detection and prevention of COVID-19”, “mitigation of the impact to healthcare indirectly related to COVID-19” and “assuring the care assistance to the chronic patients”: +, low (no clear example yet in the official government website); ++, moderate (few clear example); +++, high (several examples).
4.1. Use of big data in the Italian healthcare ecosystem
Big data plays an critical role in monitoring, detecting and preventing COVID-19 infections. In fact, there are several examples in this area (Iqbal, Doctor, More, Mahmud, & Yousuf, 2020). The enormous amount of complex data related to number of patients, infection contacts, deaths etc. from different sources has led to the need to use big data technology to enable prompt identification of patient profiles, repetitive and similar patterns of the evolving disease behavior, use and response to treatments, and so on. The use of big data will be critical in the management the COVID-19 pandemic, along with the use of predictive algorithms that could help to understand the rate of transmission of the virus and the population at risk, the natural history of the disease, its mortality rate and the best treatment options and prevention and control measures (Ting et al., 2020). The European version of contact tracing relies on big data analytics because, due to privacy issues, no central government can track both people’s positions and social contacts: only Bluetooth-based device proximity interaction is allowed on citizens’ smartphones. Italy adopted the same approach. In addition, potential patients can be discovered with Big Data approaches. An important role of big data is based on the analysis of the infection rate, because an aggregation of data arising from different sources (public and private hospitals, public and private laboratories, Ministry of Health, regional centers, metropolitan cities) is a key issue. Finally, big data plays another crucial role in prevention methods, lockdown decision, and lockdown exit strategies in all Italian regions. The minor role of big data relates to other applications in “health impact mitigation indirectly related to COVID-19”, such as Italian National Institute of Health budget modelling approaches, health resource distribution, emergency unit organization, and health care participant association. Also, “ensuring health care for chronic patients” in discovering at-risk patient, promoting social distance, identifying critical patients.
4.2. IoT in the Italian healthcare ecosystem
IoTs is basically the networking of smart electronic devices or things to transmit data signals among them in the absence of human intervention (Aldossari & Sidorova, 2018). In COVID-19 times, IoTs technology has the potential to transform the traditional paper-based healthcare treatment through simplified access to real-time patient data and remote patient monitoring. Furthermore, availability of user-friendly devices, increasing need for stringent regulations, and decreasing price of sensor technology are some factors that are also expected to fuel the growth of the IoTs healthcare market size (Papa, Mital, Pisano, & Giudice, 2020). This digital healthcare technology allows better diagnostics and targeted therapeutic tools. It also provides remote monitoring of patient by physicians, but also functions as wellness tracker and provides reminders to patients. For example, in some regions of Italy, the successful implementation of IoTs in the remote monitoring of diabetic and asthmatic patients, coupled with high penetration of fitness and wellness devices, has created a high demand for healthcare IoTs market. To pursue the goal of “monitoring, detection and prevention of COVID-19”, IoT is doing an great job: Strong Contact Tracing App, devices for lockdown monitoring, growth of contactless payment, home monitoring for non-critical patient. In addition, to pursue the goal of “assuring the care assistance to the chronic patients”, we have several IoT applications, such as e-Health, reminders, continuous glucose monitors, smart inhalers, smart disease monitor devices, appointment management, and budget management. Also, in terms of staff management, care route optimization, severe alert detection, smart work, predictive maintenance, smart inventory management, 3D printing of medical supplies, IoT plays a significant role by “mitigating the impact of different pandemic-specific disruptions on healthcare, which is indirectly related to COVID-19”.
4.3. Artificial intelligence in the Italian healthcare ecosystem
Nguyen (2020) suggests a framework for COVID-19 detection using data obtained from smartphones sensors such as cameras, microphones, temperature, and inertial sensors. In Italy, as well as in many other countries around the world, the machine-learning method is used to learn and obtain knowledge about disease symptoms based on collected data. This approach offers an inexpensive and fast method for coronavirus detection compared to the traditional medical kits or professional scanners, because data inferred from the smartphone sensors can be used efficiently in different individual applications. For example, Rao and Vazquez (2020) recommended a method to collect people’s travel history and their common sign using a phone-based online interview. The collected data can be analyzed with machine learning algorithms to study and estimate the threat of infection; thus supporting early recognition of high-risk cases for isolation. It reduces the spread of the virus to vulnerable people. Allam and Jones (2020) suggest the use of AI and data sharing regulatory procedures for better global understanding and management of urban health during the COVID-19 pandemic. For example, additional benefits can be obtained when AI is integrated with IoTs devices installed in many smart cities for early outbreak detection. AI methods demonstrate great efficiency in supporting decision makers in the virus containment process when health data are collected and shared across and among smart cities.
5. Discussions: A multi-objective optimization model for assigning IoT devices to patients
This section illustrates and discusses an application scenario of the health ecosystem, as a collective intelligence system, involved into the adoption of new digital technologies to achieve the overall goal of reducing the spread of the pandemic. Specifically, moving from the strategic goal of the health system, identified in monitoring, detecting and preventing COVID-19, mitigating the impact to healthcare indirectly related to COVID-19, and assuring health care for chronic patients, we will present and discuss how decision makers could manage the patient/resource allocation through the adoption of an optimized model to assign a limited set of IoTs devices to patients with different characteristics and acuity levels. This scenario will indirectly impact the goal of ensuring care for chronic patients.
Patient classification systems (PCSs) are commonly used in healthcare systems to define health status (Malloch & Meisel, 2013) and to assess how many resources are needed to care for patients. These systems then provide recommendations on the allocation of resource–patient for a given patient census based on these acuity scores (Sir et al., 2015, Sun et al., 2014). PCS are useful for increasing patient outcomes and monitoring budget. Usually, a PCS classifies patients into one of several types based on the sum of the weights associated with each patient indicator. The weights associated with patient indicators and the ranges by which the patients are classified are determined through extensive surveys and data analysis. Acuity indicates the level of severity of a diseases and is one of the parameters considered in patient classification systems that are designed to serve as guidelines for resource (human and nonhuman) allocation, to justify decisions, and to aid in long-term staffing and budget projection. In other words, acuity can be defined as a measure of the intensity of care required by a patient. Finally, a summary value for “acuity” is issued for each patient; for simplicity, a range of values from 0% to 100% is assumed.
Before assigning a group of IoT devices to a patient set, staff should assess the perception of patients with chronic conditions about the device use. Indeed, only a portion of patients believes that the development of digital tools in healthcare is an important opportunity and a minority see it as a danger. In particular, patients fear that the misuse of technology will lead to unwanted replacement of humans and threaten the humanistic aspect of health and care. For this reason, patients are asked quantitative, open-ended questions about the potential benefits and dangers of using these new technologies, and staff assesses their readiness to use IoT devices.
We refer to “efficiency” as the quality of patient’s use of an IoT device, without misuse of time and money, producing the desired result. Factors such as user compliance for new technologies, ownership of a smartphone or PC, and the attitude towards change influence patient efficiency in exploiting IoT devices. Furthermore, for simplicity we adopt a range of efficiency values from 0% to 100%.
Practitioners and researchers criticize fixed resource-patient assignment ratios, because they fail to account for patients' acuity levels and result in an unbalanced distribution of resources (Lin, Liu, & Lin, 2019). Incorporating information from such analyses into decision support tools and optimization models would lead to better resource allocation.
For example, a patient with a high acuity score may have more needs using IoT devices. Moreover, older people may not be as comfortable handling these new tools, while younger population may prefer them. Existing approaches to support device assignment decisions for patients represent only the acuity score. On the one hand, IoT devices enable significant increases in patient health status. On the other, some patients may not be comfortable using them; as a result, the efficiency of IoT devices may be low. In general, IoT devices should ensure that patients having high values for both acuity and efficiency, which is not always the case.
For example, referring to Fig. 2 , seven patients are represented in terms of acuity and efficiency scores. Assuming that only one IoT device is available, patient 1 is best suited for the assignment. Indeed, patient 1 needs the device because of the 75% acuity level and is able to use it efficiently (75%).
Fig. 2.
Patient 2-factor comparison considering both efficiency and acuity scores.
Assuming that two IoT devices are accessible, the second one can be assigned to patient 2 or 3 since the Pareto comparison between 2 and 3 returns that no patient is better than the other in terms of both acuity and efficiency. Indeed, patient 3 needs the device because of his/her acuity, whereas patient 2 can use IoT efficiently.
5.1. Mathematical problem formulation
Considering n devices to be assigned to m patients, suppose that for each patient j = 1,…,m the corresponding acuity scores aj and efficiency scores ej are available. Supposing m > n, we define an assignment as a set A of n patients (selected from m total patients) for the n available devices. For each assignment A, two performance parameters are defined as follows:
The parameters and represent the average of the acuity and efficiency values for the selected patients. Considering the patient set described in previous example (see par. 5.1) and assuming three available devices, we have m = 7 and n = 3. The assignment A1 = {1,2,3} leads to:
By choosing another assignment A2 = {1,3,6} the corresponding performance parameters are:
The A2 assignment is better than A1 in terms of the “acuity” parameter but worse considering the “efficiency” parameter. Therefore, considering a 2-factor comparison A1 and A2 are both optimal. Considering all possible assignments of 3 devices to 7 patients, we have feasible assignments. For such assignments, we report the corresponding performance parameters in Table 2 . A graphical representation is shown in Fig. 3 .
Table 2.
Performance parameters for assignments of 3 devices to 7 patients.
| Assignment | Acuity [%] | Efficiency [%] |
|---|---|---|
| {1,2,3} | 67 | 67 |
| {1,2,4} | 58 | 67 |
| {1,2,5} | 50 | 75 |
| {1,2,6} | 67 | 58 |
| {1,2,7} | 50 | 58 |
| {1,3,4} | 67 | 58 |
| {1,3,5} | 58 | 67 |
| {1,3,6} | 75 | 50 |
| {1,3,7} | 58 | 50 |
| {1,4,5} | 50 | 67 |
| {1,4,6} | 67 | 50 |
| {1,4,7} | 50 | 50 |
| {1,5,6} | 58 | 58 |
| {1,5,7} | 42 | 58 |
| {1,6,7} | 58 | 42 |
| {2,3,4} | 58 | 58 |
| {2,3,5} | 50 | 67 |
| {2,3,6} | 67 | 50 |
| {2,3,7} | 50 | 50 |
| {2,4,5} | 42 | 67 |
| {2,4,6} | 58 | 50 |
| {2,4,7} | 42 | 50 |
| {2,5,6} | 50 | 58 |
| {2,5,7} | 33 | 58 |
| {2,6,7} | 50 | 42 |
| {3,4,5} | 50 | 58 |
| {3,4,6} | 67 | 42 |
| {3,4,7} | 50 | 42 |
| {3,5,6} | 58 | 50 |
| {3,5,7} | 42 | 50 |
| {4,5,6} | 50 | 50 |
| {4,5,7} | 33 | 50 |
| {4,6,7} | 50 | 33 |
| {5,6,7} | 42 | 42 |
Fig. 3.
Performance parameters, and Pareto frontier, for assignments of 3 devices for 7 patients.
When multiple (possibly conflicting) objectives need to be optimized, there is no longer a single optimal solution (Lazzerini and Pistolesi, 2018, Lioliou et al., 2019, Llopis-Albert et al., 2015, Nucci, 2018). Multi-objective optimization can produce a whole set of potential solutions which are optimal in some sense and give managers the ability to evaluate tradeoffs among different solutions.
The Pareto frontier is obtained considering the trade-off of the two objectives (acuity maximization and efficiency maximization). As shown in Fig. 3, the Pareto front (in black color) represents the optimal solution set over the feasible solutions reported in blue color. The three assignments {1,2,5} {1,3,6} and {1,2,3} represent 3 optimal solutions for the proposed problem. For example, solution {2,4,5} is not optimal because optimal solution {1,2,5} is better in terms of acuity and efficiency; also, optimal solution {1,2,3} has the same acuity value as solution {2,4,5} but the efficiency for optimal solution {1,2,3} is better than efficiency for solution {2,4,5}.
5.2. Applicative scenario
An applicative scenario was developed considering a set of 50 IoT devices to be assigned to a set of 100 patients. For the considered set of patients, the efficiency and acuity scores are reported in Fig. 4 .
Fig. 4.
Efficiency and acuity scores for 100 patients Case study.
This is a typical case where Italian medical staff selects patients based on their acuity level only. In other words, the 50 patients with the highest acuity scores are selected. Graphically, in Fig. 4, the 50 highest points are selected. All this neglects efficiency parameter.
Considering the approach presented in the previous example, a valid assignment A is made of 50 patients over 100 and assignment performance parameters α(A) and ε(A) can be calculated.
Since the number of feasible assignments is equal to , it is not possible to enumerate them as in previous example to determine the optimal solutions.
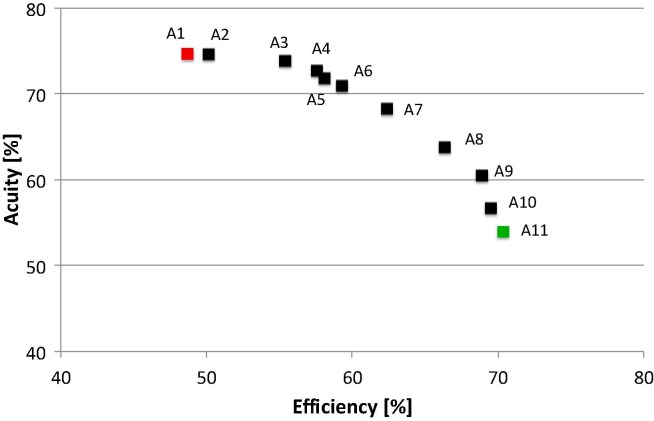
A Multiple-purpose Linear Program (MOLP) model allows us identifying 11 optimal assignments A1, A2 … A11. Fig. 5 shows the Pareto Optimal Frontier. The red marker stands for the assignment A1 considering acuity scores only, whereas green marker A11 represents that focuses only on efficiency. As it is possible to note, there are nine other optimal solutions (see A2, … A10 in black) having a good compromise between the two opposing criteria.
Fig. 5.
Case study Pareto frontier.
For example, assignment A3 significantly improves efficiency score over A1, with limited loss of acuity. Similarly, A9 significantly increases acuity score compared to A11, with a small reduction in efficiency. Decision makers are supported in the assignment problem by first considering the Pareto frontier and then the change in performance by moving from a solution to another. For decision maker, the most interesting solutions are A3, A4, A6, A7, A8 and A9. Finally, decision maker can select any of them considering other criteria.
Multi-purpose linear programming is a sub-area of mathematical optimization. A MOLP is a linear program with more than one objective function. We developed a MOLP model to detect the optimal solution set of the above problem. MOLP represents the technological platform of the collective intelligence systems and provides a concrete way to implement the principles behind the collective intelligence for healthcare management.
The key advantage of the developed system is the ability to compare all the patients simultaneously. It provides the healthcare managers with all the information to make a correct and timely decision based on two completely heterogeneous parameters (acuity and efficiency). Since the information processed by the model is anonymous, there are no privacy issues for individuals. Only the collaboration of physicians is needed to obtain the anonymous data (related to the two parameters considered by the model) for patients extracted from their medical records.
6. Conclusions and future research
The COVID-19 pandemic has catalyzed numerous changes worldwide in healthcare ecosystem. Many health systems around the world are relying on digital healthcare technologies. Consequently, digital transformation in the healthcare sector is gaining disruptive momentum due to the unexpected epidemic crisis of the COVID-19 outbreak. Managing the epidemic is a strategic priority for governments around the world to ensure social welfare.
Implications for theory. Our findings provide a framework for the health ecosystem acting as a collective intelligence system in which distributed actors/stakeholders supported by digital technologies, such as the Internet of Things (IoTs), big data analytics, and artificial intelligence, are coordinated towards achieving the goal of the public health service. The research used the collective intelligence genome as an approach to analyze how the Italian health system is working to address the COVID-19 health emergency from March 2020. Collective intelligence refers to the collective insights of multiple actors (patients, physicians, clinicians, institutions, and digital technology providers) working on a task to generate more accurate solutions and decisions than individuals can make on their own. The conceptual framework for the Italian public health sector harnesses the power of digital technology-based solutions used by the collective efforts of multiple actors. The main components of the healthcare ecosystem as collective intelligence system are: the ultimate goal of the public healthcare system (what needs to be done); the collective actors to achieve the goal (who will undertake the activities to pursue the goal); the processes and digital technologies adopted within the health system (how); and finally, the motivations behind achieving the goal (why). This concept has the potential to improve the current epidemic management.
Widespread adoption of the Internet of Things (IoTs), artificial intelligence, and big data analytics has been used by the health ecosystem to enable monitoring, surveillance, detection, and prevention of COVID-19 and to support mitigation of healthcare impact indirectly related to COVID-19. A new perspective for managing digital transformation in health ecosystems is provided and discussed through the principles of collective intelligence. Indeed, the disruptive role played by Internet of Things (IoTs) combined with big data analytics, and AI is clarified to achieve the capability, in order to protect the crowd mutually, based on a digitally enhanced healthcare ecosystem that can explore the right solution and make urgent decision.
Implications for practices. Implications for healthcare decision makers are provided through an optimized model with a multi-purpose application to allocate limited IoT devices to patients. The use of an optimized model for allocating devices to patients represents a major innovation for the Italian National Institute of Health. Usually, only physicians based on patient acuity scores perform the assignment. This unfortunately means that, in some cases, patients are unable to benefit from device use. With the proposed assignment approach, a team of physicians and medical directors collaboratively achieve the right allocation by considering the efficiency parameter. As a result, the Italian National Institute of Health return of investment can be significantly improved.
Limitations of the study and future research. The research is exploratory, and the framework offers opportunities for refinement. In the long term, the COVID-19 crisis reminds us that we should nurture the socially beneficial applications of digital technologies and focus on improving access and use in countries where they are lacking. Digital-first healthcare strategies adopted by several countries to control the spread of the virus have irrevocably rerouted the way healthcare systems function. Remote monitoring and e-Health platforms, AI-powered apps, and IoT devices have become the new norm. Furthermore, advances in sensors and wearable devices will bring diagnostics closer to patients and the proliferation of body sensors will enable understanding of the virus spread. Future research is needed to collect empirical data and to test the framework in other countries.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors are very grateful to the corresponding guest editor Prof. Rosa Lombardi - University of Roma la Sapienza (Italy) - for the insights provided to the manuscript’s research idea and to the anonymous reviewers for their helpful comments during the review process.
Biographies
Giustina Secundo is Senior Researcher in Management Engineering at University of Salento (Italy). She is Project Manager for the Contamination Lab at University of Salento (Lecce, Italy) aimed to create entrepreneurial capabilities in University’s students. She teaches Digital Transformation and Project Management at University of Salento. She is the Director of the Master in Digital transformation of the Public Administration at LUM Giuseppe Degennaro University (Bari). Her research regards the Digital transformation of the Academic entrepreneurship, Technology Entrepreneurship and Open Innovation and Knowledge Transfer. She received several award for her research activities, such as, the Emerald Literati Award, the best papers award and the highly commended award from Emerald. She authored more than 180 international papers her research appeared in Technovation, Technological Forecasting & Social Change, Journal of Business Research, International Journal of Entrepreneurial Behavior & Research, Journal of Knowledge Management, Journal of Intellectaul Capital. Across the 2014–2015 she has been visiting research at the Innovation Insights Lab at University of the Arts London (UK).
Dr. Riad Shams is a lecturer at the Newcastle Business School, Northumbria University, UK. He has published eleven books, contributed articles to top-tier international journals, and guest-edited for various reputable journals, including the Journal of International Management, Journal of Business Research, International Marketing Review, and Technological Forecasting and Social Change. He is the Associate Editor of the Journal of Social Entrepreneurship, and founder and co-editor of the Annals of Business Research, and the Palgrave Studies in Cross-Disciplinary Business Research. His research interests are in the areas of strategic agility and international business, social entrepreneurship, stakeholder relationship management, cross-cultural management, and brand and reputation management in international market. He obtained a second place in the Cambridge-Kent-Czinkota Competition for Excellence in International Business Research – 2019 and is entered into the Kent Business School’s Book of Honour. He received the Emerald Literati Award (Outstanding Paper) in 2019, the Emerald Literati Award (Outstanding Reviewer) in 2018, and the EuroMed Research Award in 2014.
Francesco Nucci is Assistant professor and Researcher at Department of engineering for Innovation at the University of Salento-Lecce. His research activities deal with the configuration and management of flexible production systems considering the uncertainty presence. He works in the scheduling of flexible production systems, under different management conditions. He is currently involved in a series of national research programs, partially, financed by companies and is a member AITeM (Association Italian Mechanical Technology). He is reviewer of J. of Manufacturing System, Int. J. of Flex. Serv. Manuf., Int. J. of Knowledge-Based Development, and Networks.
References
- Adivar B., Selen E. Review of research studies on population specific epidemic disasters. Disaster Prevention and Management. 2013;22(3):243–264. [Google Scholar]
- Aldossari M.Q., Sidorova A. Consumer acceptance of Internet of Things (IoT): Smart home context. Journal of Computer Information Systems. 2018 doi: 10.1080/08874417.2018.1543000. [DOI] [Google Scholar]
- Allam, Z., & Jones, D. S. (2020). On the coronavirus (COVID-19) outbreak and the smart city network: universal data sharing standards coupled with artificial intelligence (AI) to benefit urban health monitoring and management. In Healthcare (Vol. 8, no. 1, p. 46). MDPI. [DOI] [PMC free article] [PubMed]
- Bardhan I., Chen H., Karahanna E. Connecting systems, data and people: a multidisciplinary research roadmap for chronic disease management. MIS. 2020;44(1):185–200. doi: 10.25300/MISQ/2020/14644. Q2020. [DOI] [Google Scholar]
- Bessant J., Künne C., Möslein K. AIM Research; United Kingdom: 2012. Opening up healthcare innovation: Innovation solutions for a 21st century healthcare system. [Google Scholar]
- Boder A. Collective intelligence: A keystone in knowledge management. Journal of Knowledge Management. 2006;10(1):81–93. [Google Scholar]
- Brown, M., Collins, R., Lyke-Ho-Gland, H., Trees, L., & Tucker, E. (2020). COVID-19 Organizational Survival Guide, available at: https://www.apqc.org/resource-library/resource-listing/covid-19-organizational-survival-guide.
- Brunswicker S., Bertino E., Matei S. Big data for open digital innovation–a research roadmap. Big Data Research. 2015;2(2):53–58. [Google Scholar]
- Bashshur R., Doarn C.H.R., Frenk J.M., Kvedar J.C., Woolliscroft J.O. Telemedicine and e-Health; 2020. Telemedicine and the COVID-19 Pandemic, Lessons for the Future. [DOI] [PubMed] [Google Scholar]
- Cappelle J., Gaidet N., Iverson S.A., Takekawa J.Y., Newman S.H., Fofana B., Gilbert M. Characterizing the interface between wild ducks and poultry to evaluate the potential of transmission of avian pathogens. International Journal of Health Geographics. 2011;10(1):60. doi: 10.1186/1476-072X-10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll R., Cnossen R., Schnell M., Simons D. Continua: An interoperable personal healthcare ecosystem. IEEE Pervasive Computing. 2007;6(4):90–94. [Google Scholar]
- Elia G., Margherita A., Passiante G. Digital entrepreneurship ecosystem: How digital technologies and collective intelligence are reshaping the entrepreneurial process. Technological Forecasting and Social Change. 2020;150 [Google Scholar]
- European Commission (2017). Digital Transformation Scoreboard 2017. Available at. https://ec.europa.eu/growth/tools-databases/dem/monitor/scoreboard.
- Galetsi P., Katsaliaki K., Kumar S. Values, challenges and future directions of big data analytics in healthcare: A systematic review. Social Science & Medicine. 2019 doi: 10.1016/j.socscimed.2019.112533. [DOI] [PubMed] [Google Scholar]
- Gasser, U., Ienca, M., Scheibner, J., Sleigh, J., & Vayena, E. (2020). Digital tools against COVID-19: Framing the ethical challenges and how to address them. arXiv preprint arXiv:2004.10236. [DOI] [PMC free article] [PubMed]
- Georgalakis J. A disconnected policy network: The UK’s response to the Sierra Leone Ebola epidemic. Social Science & Medicine. 2020 doi: 10.1016/j.socscimed.2020.112851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadzic, M., & Sidhu, A. (2008) Digital health ecosystems, in: 2nd IEEE International Conference on Digital Ecosystems and Technologies, pp. cv–cvii.
- Hilbert M. Big data for development: A review of promises and challenges. Development Policy Review. 2016;34(1):135–174. [Google Scholar]
- Hirsch J.A., Winters M., Clarke P., McKay H. Generating GPS activity spaces that shed light upon the mobility habits of older adults: a descriptive analysis. International journal of health geographics. 2014;13(1):1–14. doi: 10.1186/1476-072X-13-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ienca M., Vayena E. On the responsible use of digital data to tackle the COVID-19 pandemic. Nature Medicine. 2020;26(4):463–464. doi: 10.1038/s41591-020-0832-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal R., Doctor F., More B., Mahmud S., Yousuf U. Big data analytics: Computational intelligence techniques and application areas. Technological Forecasting and Social Change. 2020;153 doi: 10.1016/j.techfore.2018.03.024. [DOI] [Google Scholar]
- Iyawa G.E., Herselman M., Botha A. Digital health innovation ecosystems: From systematic literature review to conceptual framework. Procedia Computer Science. 2016;100:244–252. doi: 10.1016/j.procs.2016.09.149. [DOI] [Google Scholar]
- Koylu C., Delil S., Guo D., Celik R.N. Analysis of big patient mobility data for identifying medical regions, spatio-temporal characteristics and care demands of patients on the move. International Journal of Health Geographics. 2018;17(1):32. doi: 10.1186/s12942-018-0152-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keesara S., Jonas A., Schulman K. COVID-19 and healthcare’s digital revolution. New England Journal of Medicine. 2020 doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- Lazzerini B., Pistolesi F. Multiobjective personnel assignment exploiting workers' sensitivity to risk. IEEE Transactions on Systems, Man, and Cybernetics: Systems. 2018;48(8):1267–1282. doi: 10.1109/TSMC.2017.2665349. [DOI] [Google Scholar]
- Leimeister J.M. Collective Intelligence. Business & Information Systems Engineering. 2010;2(4):245–248. [Google Scholar]
- Lévy, P. (1994), L’Intelligence Collective. Pour une Anthropologie du Cyberspace, La Découverte, Paris.
- Lin T., Liu P., Lin C. Home healthcare matching service system using the internet of things. Mobile Networks and Applications. 2019;24:736–747. doi: 10.1007/s11036-018-1087-y. [DOI] [Google Scholar]
- Lioliou E., Willcocks L., Liu X. Researching IT multi-sourcing and opportunistic behavior in conditions of uncertainty: A case approach. Journal of Business Research. 2019;103:387–396. doi: 10.1016/j.jbusres.2019.04.002. [DOI] [Google Scholar]
- Llopis-Albert C., Rubio F., Valero F. Improving productivity using a multi-objective optimization of robotic trajectory planning. Journal of Business Research. 2015;68(7):1429–1431. doi: 10.1016/j.jbusres.2015.01.027. [DOI] [Google Scholar]
- Majumdar D., Kumar B.P., Chakrabarti S. Disruptive technology and disruptive innovation: Ignore at your peril! Technology Analysis & Strategic Management. 2018;30(11):1247–1255. [Google Scholar]
- Malloch K., Meisel M. Patient classification systems: State of the science 2013. Nurse Leader. 2013;11(6):35–40. doi: 10.1016/j.mnl.2013.09.008. [DOI] [Google Scholar]
- Malone T.W., Laubacher R.J., Dellarocas C. The collective intelligence genome. MIT Sloan Management Review. 2010;51(3):21–31. [Google Scholar]
- Malone, T. W., Atlee, T., & Lévy, P. (2008). Collective intelligence. Social Text, available at www.academia.edu/download/35995585/2010_Collective_Intelligence_Book.pdf.
- Malone, T. W. (2006), “What is collective intelligence and what will we do about it?”, Edited transcript of remarks presented at the official launch of the MIT Center for Collective Intelligence, October 13, Cambridge, MA, available at http://cci.mit.edu/about/MaloneLaunchRemarks.html.
- Massaro M., Dumay J., Garlatti A. Public sector knowledge management: A structured literature review. Journal of Knowledge Management. 2015;19(3):530–558. [Google Scholar]
- Mulgan, G., Mateos-Garcia, J., Marston, L., & Westlake, S. (2012). Draft Discussion Paper on Collective Intelligence, NESTA REPORT, Plough Place London EC4A 1DE.
- Munyaneza F., Hirschhorn L.R., Amoroso C.L., Nyirazinyoye L., Birru E., Mugunga J.C.…Ntaganira J. Leveraging community health worker system to map a mountainous rural district in low resource setting: A low-cost approach to expand use of geographic information systems for public health. International Journal of Health Geographics. 2014;13(1):49. doi: 10.1186/1476-072X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nambisan S. Digital entrepreneurship: Toward a digital technology perspective of entrepreneurship. Entrepreneurship Theory and Practice. 2017;41(6):1029–1055. [Google Scholar]
- Nambisan S., Lyytinen K., Majchrzak A., Song M. Digital innovation management: Reinventing innovation management research in a digital world. MIS Quarterly. 2017;41(1):223–238. [Google Scholar]
- Nguyen, T. T. (2020). Artificial intelligence in the battle against coronavirus (COVID-19): A survey and future research directions. Preprint, DOI: 10.13140/RG.2.2.36491.23846.
- Nucci F. Fuzzy uncertainty management in multi-shift single-vehicle routing problem. Advances in Science, Technology and Engineering Systems. 2018;3(6):33–45. doi: 10.25046/aj030603. [DOI] [Google Scholar]
- Papa A., Mital M., Pisano P.D., Giudice M. E-health and wellbeing monitoring using smart healthcare devices: An empirical investigation. Technological Forecasting and Social Change. 2020;153 doi: 10.1016/j.techfore.2018.02.018. [DOI] [Google Scholar]
- Rao A.S.S., Vazquez J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone-based survey in the populations when cities/towns are under quarantine. Infection Control and Hospital Epidemiology. 2020:1–18. doi: 10.1017/ice.2020.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rippa P., Secundo G. Digital academic entrepreneurship: The potential of digital technologies on academic entrepreneurship. Technological Forecasting and Social Change. 2019;146:900–911. [Google Scholar]
- Secundo G., Toma A., Schiuma G., Passiante G. Knowledge transfer in open innovation: A classification framework for healthcare ecosystems. Business Process Management Journal. 2019;25(1):144–163. [Google Scholar]
- Shaluf I.M. An overview on disasters. Disaster Prevention and Management. 2007;16(5):687–703. [Google Scholar]
- Shams S.M.R. Capacity building for sustained competitive advantage: A conceptual framework. Marketing Intelligence & Planning. 2016;34(5):671–691. [Google Scholar]
- Shams S.M.R., Solima L. Big data management: Implications of dynamic capabilities and data incubator. Management Decision. 2019;57(8):2113–2123. [Google Scholar]
- Sir M., Dundar B., Barker Steege L., Pasupathy K. Nurse–patient assignment models considering patient acuity metrics and nurses’ perceived workload. Journal of Biomedical Informatics. 2015;55:237–248. doi: 10.1016/j.jbi.2015.04.005. [DOI] [PubMed] [Google Scholar]
- Sun L., DePuy G., Evans G. Multi-objective optimization models for patient allocation during a pandemic influenza outbreak. Computers & Operations Research. 2014;51:350–359. doi: 10.1016/j.cor.2013.12.001. [DOI] [Google Scholar]
- Surowiecki, J. (2004), The Wisdom of Crowds: Why the Many are Smarter than the Few and How Collective Wisdom Shapes Business, Economies, Societies, and Nations, 1st Doubleday Books, New York.
- Ting D.S.W., Carin L., Dzau V., Wong T.Y. Digital technology and COVID-19. Nature Medicine. 2020;26:459–461. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trequattrini R., Shams R., Lardo A., Lombardi R. Risk of an epidemic impact when adopting the Internet of Things: The role of sector-based resistance. Business Process Management Journal. 2016;22(2):403–419. [Google Scholar]
- Verhoef P.C., Broekhuizen T., Bart Y., Bhattacharya A., Dong J.Q., Fabian N., Haenlein M. Digital transformation: A multidisciplinary reflection and research agenda. Journal of Business Research. 2019 doi: 10.1016/j.jbusres.2019.09.022. [DOI] [Google Scholar]
- Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: Big Data Analytics, new technology, and proactive testing. JAMA. 2020 doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- WHO (2020). Events as they happen. Rolling updates on coronavirus disease (COVID-19). WHO, available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed 30 April 2020.
- Xiang Y.T., Li W., Zhang Q., Jin Y., Rao W.W., Zeng L.N.…Hall B.J. Timely research papers about COVID-19 in China. The Lancet. 2020;395(10225):684–685. doi: 10.1016/S0140-6736(20)30375-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S.G., Tullis J.A., Cothren J. A remote sensing and GIS-assisted landscape epidemiology approach to West Nile virus. Applied Geography. 2013;45:241–249. [Google Scholar]
- Yu T.H.K., Wang D.H.M., Wu K.-L. Reexamining the red herring effect on healthcare expenditures. Journal of Business Research. 2015;68(4):783–787. [Google Scholar]
- Zillner, S., Oberkampf, H., Bretschneider, C., Zaveri, A., Faix, W., & Neururer, S. (2014, August). Towards a technology roadmap for big data applications in the healthcare domain. In Proceedings of the 2014 IEEE 15th international conference on information reuse and integration (IEEE IRI 2014) (pp. 291–296). IEEE.