Abstract
AIMS—The effect of local anaesthetics on optic nerve function can be investigated by quantifying the relative afferent pupillary defect (RAPD). METHODS—The study compared the depth of induced RAPD following posterior sub-Tenon's, retrobulbar, and peribulbar local anaesthetics using crossed polarising filters before cataract surgery (time 1 = 5 minutes), immediately after surgery (time 2 = 42 minutes (av)), and once again on the ward (time 3 = 107 minutes (av)). RESULTS—All patients developed a RAPD. There was no significant difference in the depth of RAPD between the groups at any one time period. The peribulbar group had a significantly steeper decay in RAPD from time 1 to time 2 (p = 0.014). This effect was reduced when the shorter operation time for this group was entered as a cofactor (p = 0.063). By time 3 the RAPDs for all groups had decayed similarly so that no differences could be detected. CONCLUSION—All three anaesthetic methods caused a similar level of disruption to optic nerve conduction immediately following administration and at the time of day case discharge.
Full Text
The Full Text of this article is available as a PDF (80.3 KB).
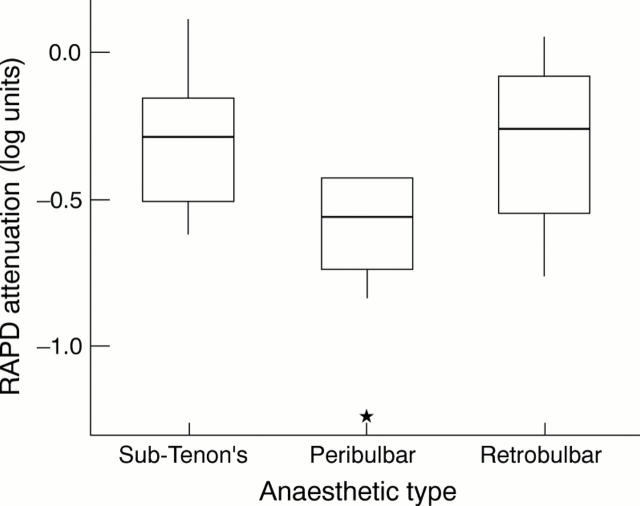
Figure 1 .
Attenuation of RAPD (measured with crossed polarising filters) with time following administration of sub-Tenon's, peribulbar, and retrobulbar anaesthetics.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bell R. A., Waggoner P. M., Boyd W. M., Akers R. E., Yee C. E. Clinical grading of relative afferent pupillary defects. Arch Ophthalmol. 1993 Jul;111(7):938–942. doi: 10.1001/archopht.1993.01090070056019. [DOI] [PubMed] [Google Scholar]
- Buys Y. M., Trope G. E. Prospective study of sub-Tenon's versus retrobulbar anesthesia for inpatient and day-surgery trabeculectomy. Ophthalmology. 1993 Oct;100(10):1585–1589. doi: 10.1016/s0161-6420(93)31440-5. [DOI] [PubMed] [Google Scholar]
- Guise P. A. Single quadrant sub-Tenon's block. Evaluation of a new local anaesthetic technique for eye surgery. Anaesth Intensive Care. 1996 Apr;24(2):241–244. doi: 10.1177/0310057X9602400217. [DOI] [PubMed] [Google Scholar]
- Levin M. L., O'Connor P. S. Visual acuity after retrobulbar anesthesia. Ann Ophthalmol. 1989 Sep;21(9):337–339. [PubMed] [Google Scholar]
- Ramsay A., Williamson T. H., Parks S., Keating D. Crossed polarising filters to measure relative afferent pupillary defects: reproducibility, correlation with neutral density filters and use in central retinal vein occlusion. Eye (Lond) 1995;9(Pt 5):624–628. doi: 10.1038/eye.1995.151. [DOI] [PubMed] [Google Scholar]
- Ropo A., Nikki P., Ruusuvaara P., Kivisaari L. Comparison of retrobulbar and periocular injections of lignocaine by computerised tomography. Br J Ophthalmol. 1991 Jul;75(7):417–420. doi: 10.1136/bjo.75.7.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ropo A., Ruusuvaara P., Setälä K. Visual evoked potentials after retrobulbar or periocular anaesthesia. Br J Ophthalmol. 1992 Sep;76(9):541–544. doi: 10.1136/bjo.76.9.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M. L., Oliva A. The use of crossed polarized filters in the measurement of the relative afferent pupillary defect. Am J Ophthalmol. 1990 Jul 15;110(1):62–65. doi: 10.1016/s0002-9394(14)76939-9. [DOI] [PubMed] [Google Scholar]
- Talks S. J., Chong N. H., Gibson J. M., Francis I. R. Visual acuity and pupillary reactions after peribulbar anaesthesia. Br J Ophthalmol. 1994 Jan;78(1):41–43. doi: 10.1136/bjo.78.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson H. S., Corbett J. J., Cox T. A. How to measure the relative afferent pupillary defect. Surv Ophthalmol. 1981 Jul-Aug;26(1):39–42. doi: 10.1016/0039-6257(81)90124-7. [DOI] [PubMed] [Google Scholar]