Abstract
Influenza B virus causes a significant amount of morbidity and mortality, yet the systems to produce high yield inactivated vaccines for these viruses have lagged behind the development of those for influenza A virus. We have established a plasmid-only reverse genetics system for the generation of recombinant influenza B virus that facilitates the generation of vaccine viruses without the need for time consuming coinfection and selection procedures currently required to produce reassortants. We cloned the eight viral cDNAs of influenza B/Yamanashi/166/98, which yields relatively high titers in embryonated chicken eggs, between RNA polymerase I and RNA polymerase II transcription units. Virus was detected as early as 3 days after transfection of cocultured COS7 and Madin–Darby canine kidney cells and achieved levels of 106-107 plaque-forming units per ml of cell supernatant 6 days after transfection. The full-length sequence of the recombinant virus after passage into embryonated chicken eggs was identical to that of the input plasmids. To improve the utility of the eight-plasmid system for generating 6 + 2 reassortants from recently circulating influenza B strains, we optimized the reverse transcriptase–PCR for cloning of the hemagglutinin (HA) and neuraminidase (NA) segments. The six internal genes of B/Yamanashi/166/98 were used as the backbone to generate 6 + 2 reassortants including the HA and NA gene segments from B/Victoria/504/2000, B/Hong Kong/330/2001, and B/Hawaii/10/2001. Our results demonstrate that the eight-plasmid system can be used for the generation of high yields of influenza B virus vaccines expressing current HA and NA glycoproteins from either of the two lineages of influenza B virus.
Influenza is a major cause of morbidity and mortality worldwide. In the USA alone, it is estimated that influenza is responsible for approximately 20,000 deaths each year (1). The morbidity associated with these epidemics is caused by both types of influenza virus, influenza A and influenza B. The immune response elicited by infection with a specific influenza strain is long lasting and protects the individual from experiencing illness on subsequent exposures to other strains that are antigenically similar. However, immunity conferred by infection with a specific influenza strain does not confer protection to other influenza types, subtypes, or antigenically divergent strains of the same subtype. Vaccines to prevent influenza generally contain the surface hemagglutinin (HA) and neuraminidase (NA) glycoproteins from the two currently circulating influenza A subtypes (i.e., H3N2 and H1N1) and one circulating influenza B strain. Because of the frequent emergence of new antigenic variants created by antigenic shift or antigenic drift, vaccines have to be updated frequently.
Currently, two major lineages of influenza B viruses are circulating in humans: the B/Yamagata/16/88-like and B/Victoria/2/87-like strains. Although the B/Yamagata/16/88-like strains have been the predominant strains circulating for the past 10 years, these two lineages circulate concurrently and both have been responsible for annual influenza epidemics (2–4). Antigenic drift is responsible for the divergence of influenza B surface antigens. Antigenic drift is caused by amino acid changes in HA and NA, which are caused by nucleotide misincorporation during viral replication. In addition, insertion and/or deletion of nucleotides in the HA and NA gene segments of influenza B viruses have been shown to be a source of antigenic diversity and evolution (5, 6). Although it is well established that influenza B viruses can evolve by reassortment (6, 7), little is known about the animal reservoir for this virus. Recently, influenza B viruses have been isolated from seals, demonstrating that influenza B viruses are not restricted to humans and raising concerns about the potential for influenza B viruses to emerge with new antigenic properties (8).
For optimal effectiveness, influenza vaccines must contain antigens that are similar to those of the currently circulating strains. The simplest approach to produce an inactivated vaccine is to identify a wild-type (wt) strain that has appropriate antigenic characteristics and grows well in eggs. However, this approach depends on the availability of a high yield wild-type isolate. A second method, classical reassortment, requires coinfection of two viruses, one expressing the desirable HA and/or NA and the other a vaccine strain that has the appropriate biological characteristics. The desired reassortant is identified among the progeny and purified. For inactivated influenza A vaccine production, the vaccine strain A/PR/8/34, which expresses the desirable characteristics of high yield in eggs, is coinfected with a virus expressing the current antigens, and a high growth reassortant is isolated (9). For live, attenuated influenza A vaccines, the wild-type HA and NA gene segments can be reassorted onto the live, attenuated ca A/Ann Arbor/6/60 background to produce attenuated vaccine strains (10). These reassorted vaccines have been shown to be safe and effective for the prevention of influenza (11). Currently, although live, attenuated influenza B vaccine strains can be produced by classical reassortment, there are no influenza B strains used for classical reassortment for production of inactivated vaccines. There are at least two limitations to producing these reassortants. First, influenza A/PR/8/34 cannot be used to reassort with influenza B HA and NA gene segments. Influenza A and B viruses have evolved separately, and reassortment between these two types has never been observed either in nature or in tissue culture (12, 13). An influenza B vaccine strain with high yield growth properties in eggs, analogous to A/PR/8/34, for production of inactivated vaccine has not been reported, and the procedures to produce 6 + 2 reassortants in the laboratory have been more difficult than for influenza A strains. Second, recent advances in reverse genetics of influenza A viruses may enable more efficient methods to generate recombinant vaccine strains expressing wt HA and NA from a vaccine strain with the appropriate biological characteristics (14–16). Generation of infectious virus directly from plasmid clones has enabled several different influenza A HA and NA subtypes to be expressed from the A/PR/8/34 backbone without the need for coinfection and extensive selection of the progeny (17, 18).
Despite one recent report on the generation of virus like particles (VLP) for influenza B virus from plasmids (19), the development of a plasmid-only system for generation of recombinant, infectious influenza B virus poses major challenges. To date, no plasmid-based system for influenza B virus rescue has been reported. Obviously, the genomic sequence (14642 nucleotides), including the entire noncoding and coding regions of all eight gene segments, has to be cloned into plasmids and sequenced. Because the viral sequences in the plasmids possibly represent nonviable variants of the virus population or have mutations introduced by reverse transcriptase (RT)-PCR, multiple plasmids for each segment have to be characterized. A single mutation in one of the plasmids could result in failure to rescue virus. The established plasmid-only systems for influenza A virus are based on the in vivo transcription of viral RNA (vRNA) or cRNA from an RNA polymerase I (pol I) promoter on the plasmid (20, 21). These 5′ and 3′ termini of vRNAs or cRNAs are different between type A and type B virus and contain sequences that are unique for each of the eight segments. However, most sequences deposited in GenBank for influenza B virus do not include those end sequences. In addition, some of the published terminal regions differ between isolates either because the viruses have different sequences and/or because of sequencing errors.
The proteins of type A and type B viruses with analogous functions show homologies ranging from about 35% for nucleoprotein (NP) to 60% for the polymerase subunit PB1, the most conserved protein among influenza viruses (22, 23). In addition to sequence differences between influenza A and B virus, the genetic organization of these two viruses is different. RNA segment 6 of influenza A virus is monocistronic, coding for the NA protein, whereas segment 6 of influenza B virus encodes NA and NB proteins by using a bicistronic mRNA with two overlapping ORFs. The NB protein of influenza B virus is a membrane protein that is believed to serve a function similar to that of the M2 protein of influenza A viruses (24–26). Furthermore, although RNA segment 7 of both influenza A and B viruses encodes the matrix protein M1, the organizations of their respective M2 genes are quite different. The M2 protein of influenza A virus is translated from an mRNA generated by splicing (27, 28). RNA segment 7 of influenza B viruses is bicistronic, containing two ORFs characterized by overlapping of the termination codon of the M1 gene and the initiation codon of the BM2 gene (29). The BM2 protein is a phosphoprotein that is synthesized late in the phase of infection and incorporated into virions (30). Influenza A viruses have no counterpart for the BM2 protein. Recently, a second ORF in the PB1 gene of influenza A virus, termed PB1-F2, was reported; influenza B viruses do not have this ORF (31). The sequence and organizational differences between type A and type B viruses combined with uncertainties of vRNA stability and integrity do not allow one to predict the success of influenza B virus rescue. The utility of a reverse genetics system for generation of influenza B virus can be tested only by plasmid-driven expression of all influenza B virus genes and evaluation of growth conditions in suitable host cells for virus rescue.
Here, we report the establishment of an eight-plasmid system that enables the generation of infectious, recombinant influenza B vaccine strains, and provides a system that will enable the genetic characterization of influenza B viral genes. Our results demonstrate that the eight-plasmid system allows reproducible and rapid generation of B/Yamanashi/166/98 and 6 + 2 reassortants derived from influenza B strains circulating in humans. This system can be applied to the rapid generation of influenza B virus vaccines expressing current antigens.
Materials and Methods
Virus Strains.
The virus strain B/Yamanashi/166/98 was obtained from the repository of St. Jude Children's Research Hospital (Memphis, TN). B/Victoria/504/2000, B/Hong Kong/330/2001, and B/Hawaii/10/2001 viruses were provided by N. Cox and A. Klimov (Centers for Disease Control, Atlanta, GA).
RT-PCR.
The RNeasy Kit (Qiagen, Chatsworth, CA) was used to extract vRNA from 100 μl of allantoic fluid from infected embryonated chicken eggs. The RNA was eluted into 40 μl of H2O. For RT-PCR of the eight segments, the One Step RT-PCR kit (Qiagen) was used according to the protocol provided. One microliter of RNA was used for each reaction. The RT reaction was performed for 50 min at 50°C, followed by 15 min at 94°C. The PCR reaction was carried out by 25 cycles with the following conditions: 94°C for 30 s, 54°C for 30 s, and 72°C for 3 min. The primers used for construction of plasmids representing the eight segments of B/Yamanashi/166/98 are shown in Table 1. The PB1, PB2, and PA genes were amplified by using segment-specific primers with BsmBI sites that allow the generation of two fragments. The primers with nucleotides complementary to the internal regions of these genes have BsmBI sites facilitating the exact fusion of the two amplified fragments in a three-fragment ligation reaction with the BsmBI-digested vector pAD3000.
Table 1.
Primer set used for RT-PCR amplification of the eight vRNAs of B/Yamanashi/166/98
| Gene | Forward primer | Reverse primer |
|---|---|---|
| PB1 | Bm-PB1b-1: | Bm-PB1b-1200R: |
| [1A] | TATTCGTCTCAGGGAGCAGAAGCGGAGCCTTTAAGATG | TATTCGTCTCGATGCCGTTCCTTCTTCATTGAAGAATGG |
| PB1 | Bm-PB1b-1220: | Bm-PB1b-2369R: |
| [1B] | TATTCGTCTCGGCATCTTTGTCGCCTGGGATGATGATG | ATATCGTCTCGTATTAGTAGAAACACGAGCCTT |
| PB2 | Bm-PB2b-1: | Bm-PB2b-1145R: |
| [2A] | TATTCGTCTCAGGGAGCAGAAGCGGAGCGTTTTCAAGATG | TATTCGTCTCTCTCATTTTGCTCTTTTTTAATATTCCCC |
| PB2 | Bm-PB2b-1142: | Bm-PB2b-2396R |
| [2B] | TATTCGTCTCATGAGAATGGAAAAACTACTAATAAATTCAGC | ATATCGTCTCGTATTAGTAGAAACACGAGCATT |
| PA | Bm-PAb-1: | Bm-PAb-1261R: |
| [3A] | TATTCGTCTCAGGGAGCAGAAGCGGTGCGTTTGA | TATTCGTCTCCCAGGGCCCTTTTACTTGTCAGAGTGC |
| PA | Bm-PAb-1283: | Bm-PAb-2308R: |
| [3B] | TATTCGTCTCTCCTGGATCTACCAGAAATAGGGCCAGAC | ATATCGTCTCGTATTAGTAGAAACACGTGCATT |
| HA | MDV-B 5′ BsmBI-HA: | MDV-B 3′ BsmBI-HA: |
| TATTCGTCTCAGGGAGCAGAAGCAGAGCATTTTCTAATATC | ATATCGTCTCGTATTAGTAGTAACAAGAGCATTTTTC | |
| NP | MDV-B 5′ BsmBI-NP: | MDV-B 3′ BsmBI-NP: |
| TATTCGTCTCAGGGAGCAGAAGCACAGCATTTTCTTGTG | ATATCGTCTCGTATTAGTAGAAACAACAGCATTTTTTAC | |
| NA | Bm-NAb-1: | Bm-NAb-1557R: |
| TATTCGTCTCAGGGAGCAGAAGCAGAGCA | ATATCGTCTCGTATTAGTAGTAACAAGAGCATTTT | |
| M | MDV-B 5′ BsmBI-M: | MDV-B 3′ BsmBI-M: |
| TATTCGTCTCAGGGAGCAGAAGCACGCACTTTCTTAAAATG | ATATCGTCTCGTATTAGTAGAAACAACGCACTTTTTCCAG | |
| NS | MDV-B 5′ BsmBI-NS: | MDV-B 3′ BsmBI-NS: |
| TATTCGTCTCAGGGAGCAGAAGCAGAGGATTTGTTTAGTC | ATATCGTCTCGTATTAGTAGTAACAAGAGGATTTTTAT |
The sequences complementary to the influenza sequences are shown in bold. The 5′-ends have recognition sequences for the restriction endonuclease BsmBI (Bm, CGTCTCN1/N5). The design of the primers for PB1, PB2, and PA allowed the amplification of two fragments (1A, 1B, 2A, 2B, 3A, 3B).
For RT-PCR amplification of the HA and the NA segments, we used the primer pair Bm-NAb-1/Bm-NAb-1557R (Table 1), which allowed the amplification of both segments under the same RT-PCR conditions as described above. The PCR products were sequenced with internal segment-specific primers to derive a consensus sequence. For amplification of the PA gene of wt and recombinant B/Yamanashi/166/98, the forward primer eh153s-1 (ATG AAA AGC GAA AAA GCT AAC GAAA ATT TCC) and reverse primer eh253r-2 (GTT ACT AAT ACA TTC TTG TAT TCC AGA ATA CA) were used. The sequence shown in Fig. 3 was obtained by sequencing the PCR product with the forward primer eh153s-1. The sequence of template DNA was determined by using Rhodamine or dRhodamine dye-terminator cycle sequencing ready reaction kits with AmpliTaq DNA polymerase FS (Perkin–Elmer). Samples were separated by electrophoresis and analyzed on PE/ABI model 373, model 373 Stretch, or model 377 DNA sequencers.
Fig 3.
Genetic characterization of recombinant influenza B viruses. RNA was isolated from allantoic fluid of chicken eggs either infected with wt B/Yamanashi/166/98 (1) or with supernatant of transfected COS7-MDCK cells with eight plasmids (2). RT-PCR was performed by using PA-specific primers. The PCR products were sequenced. The nucleotides in the electropherogram that differ between recombinant virus and wt virus are encircled.
Cloning of Plasmids.
The cloning vector pAD3000 was derived from pHW2000 (16) by replacing the bovine GH polyadenylation signal with the SV40 late mRNA polyadenylation signal. RT-PCR fragments were isolated, digested with BsmBI, and inserted into the BsmBI-digested plasmid pAD3000.
To ensure that the plasmids represent wt viral sequences, a consensus sequence for all eight segments of B/Yamanashi/166/98 was constructed from sequence data in GenBank for the coding regions PB1 (AF102007), PB2 (AF101990), PA (AF102024), HA (AF100355), NP (AF100373), M (AF100392), and nonstructural (NS) (AF100410) (7, 32), by direct sequencing of the RT-PCR product of segment 6, and by sequencing the noncoding regions (NCRs) of the viral RNAs. Two sets of eight plasmids derived from B/Yamanashi/166/98 were constructed independently; some of the plasmids had mutations resulting in amino acid changes. The changes were corrected to reflect the consensus sequence by site-directed mutagenesis using PfuTurbo DNA polymerase (Stratagene) or exchanged by cloning with other unaltered plasmid sequences. The resultant plasmids were sequenced and designated pAB251-PB1, pAB252-PB2, pAB253-PA, pAB254-HA, pAB255-NP, pAB256-NA, pAB257-M, and pAB258-NS. pAB253-PA differs in three nucleotides from the consensus at the following positions: 1280A → 1280G, 1283T → 1283C, and 1289C → 1289T. These substitutions served as a genetic tag for the recombinant virus and were introduced by using the primer Bm-PAb-1261R (Table 1). These nucleotide differences are silent, resulting in no change in the amino acid sequence of the PA protein.
Transfection and Generation of Virus.
The protocol used for the rescue of influenza B virus was based on the protocol for generation of influenza A virus (16). Briefly, COS7 cells were transiently cocultured with Madin–Darby canine kidney (MDCK) cells in six-well plates. Two microliters of TransIT-LT-1 (Mirrus, Madison, WI) per 1 μg of DNA was mixed, incubated at room temperature for 45 min, and added to the cells. After 6–15 h, the DNA-transfection mixture was replaced by Opti-MEM I (Life Technologies, Rockville, MD). The cells were incubated at 33°C. To ensure that the generated recombinant viruses were able to replicate (cleavage of the HA to produce infectious virus) 2, 4, and 6 days after transfection, 1 ml of Opti-MEM I containing 1 μg/ml l-1-tosylamido-2-phenylethyl chloromethyl ketone (TPCK)-trypsin was added to the cells.
For plaque assay, supernatants were titrated on MDCK cells, which were incubated with an 0.8% agarose overlay for 3 days at 33°C. For infection of eggs, the supernatants of transfected cells were harvested 6 or 7 days after transfection, and 100 μl of the virus dilutions in Opti-MEM I were injected into 11-day-old embryonated chicken eggs at 33°C. The titer was determined 3 days after inoculation by TCID50 (tissue culture 50% infective dose) assay in MDCK cells.
Results
Generation of B/Yamanashi/166/98 from Eight Plasmids.
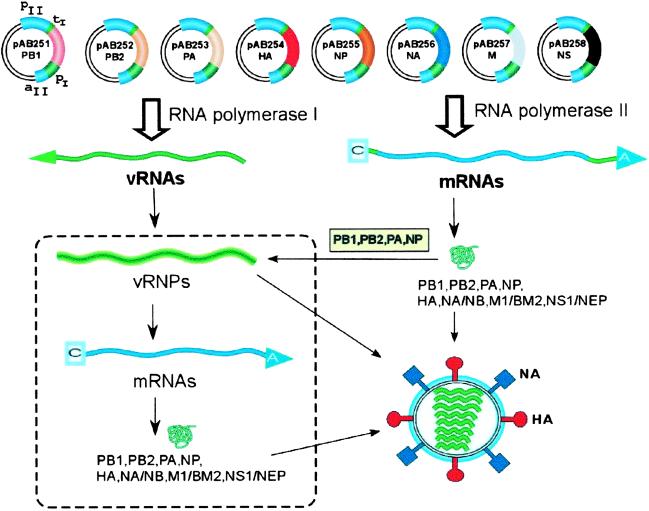
To construct eight plasmids representing the virus strain B/Yamanashi/166/98, viral RNA was reverse transcribed and amplified by PCR. The resultant cDNA fragments were inserted into pAD3000, which contains a pol I transcription unit designed to synthesize vRNA from one strand, flanked by an RNA polymerase II (pol II) transcription unit to synthesize mRNA from the opposite strand. All viral RNAs and mRNAs/proteins should be produced intracellularly after transfection of a primate cell (Fig. 1). The viral cDNAs cloned into the resultant plasmids were sequenced in their entirety and represent the consensus sequence of the eight segments of B/Yamanashi/166/98. These plasmids were designated pAB251-PB1, pAB252-PB2, pAB253-PA, pAB254-HA, pAB255-NP, pAB256-NA, pAB257-M, and pAB258-NS.
Fig 1.
Eight-plasmid bidirectional transcription system for the generation of influenza B virus. The eight plasmids contain cDNAs representing the eight gene segments of influenza B virus. In each of the plasmids, the cDNAs are flanked by pol I (pI) promoter/terminator (tI) sequences. The RNA pol I transcription unit is flanked by pol II promoter (pII)/polyadenylation (aII) sequences. After transfection of these constructs into COS7 cells, cellular pol I synthesize virus-like noncapped negative sense vRNAs and pol II capped mRNAs encoding the viral proteins. After translation of PB1, PB2, PA, and NP proteins, the eight negative sense vRNAs are transcribed and replicated. Ultimately, the viral ribonucleoproteins (vRNPs) and structural proteins derived from cellular transcription or viral amplification (dashed rectangle) are assembled into new virus particles.
To test whether infectious B/Yamanashi/166/98 virus could be generated from the constructed eight plasmids, cocultured COS7-MDCK cells were transfected with 1 μg of each plasmid. Characteristic virus induced cytopathic effect (CPE) was evident in the MDCK cells 5 to 7 days posttransfection and required the transfection of all eight plasmids to produce CPE (Table 2). In addition, the supernatants from these transfected cells were plated out at a variety of dilutions on fresh monolayers of MDCK cells, and infectious virus was detected only when all eight plasmids were present. These results indicated that infectious virus was generated from cloned cDNAs.
Table 2.
Plasmid set used for the generation of B/Yamanashi/166/98 and 6 + 2 reassortants
| Segment | Plasmid set | ||||
|---|---|---|---|---|---|
| 1 | — | pAB251-PB1 | pAB251-PB1 | pAB251-PB1 | pAB251-PB1 |
| 2 | pAB252-PB2 | pAB252-PB2 | pAB252-PB2 | pAB252-PB2 | pAB252-PB2 |
| 3 | pAB253-PA | pAB253-PA | pAB253-PA | pAB253-PA | pAB253-PA |
| 4 | pAB254-HA | pAB254-HA | pAB281-HA | pAB285-HA | pAB287-HA |
| 5 | pAB255-NP | pAB255-NP | pAB255-NP | pAB255-NP | pAB255-NP |
| 6 | pAB256-NA | pAB256-NA | pAB291-NA | pAB295-NA | pAB297-NA |
| 7 | pAB257-M | pAB257-M | pAB257-M | pAB257-M | pAB257-M |
| 8 | pAB258-NA | pAB258-NA | pAB258-NA | pAB258-NA | pAB258-NA |
| Recombinant virus | 8 | 6 + 2 | 6 + 2 | 6 + 2 | |
| B/Yamanashi/166/98 | B/Victoria/504/2000 | B/Hawaii/10/2001 | B/Hong Kong/330/2001 | ||
| pfu/ml | 0 | 4 × 106 | 9 × 106 | 6 × 106 | 7 × 106 |
Supernatants of cocultured COS7-MDCK cells were titrated 6 or 7 days after transfection, and the viral titer was determined by plaque assays on MDCK cells. Plasmids containing the HA or NA cDNA of currently circulating strains are shown in bold.
To determine the efficiency of the DNA transfection system for virus generation, supernatants of transfected COS7-MDCK cells or COS7 cells alone were titrated at day 2, 3, 4, 5, and 6 after transfection on fresh MDCK cells. No virus could be detected 2 days after transfection. Three days after transfection, 2 × 103 plaque-forming units (pfu)/ml of virus were detected in the supernatant of transfected COS7-MDCK cells, and 1 × 101 pfu/ml were detected on COS7 cells alone (Fig. 2). This yield increased in COS7-MDCK cells to 5 × 107 pfu/ml and in COS7 cells alone to 2 × 103 pfu/ml 6 days posttransfection. No virus was detected in supernatants derived from cells transfected with only seven plasmids.
Fig 2.
Kinetics of virus generation after transfection. COS7 or cocultured COS7-MDCK cells were transfected with eight plasmids representing the eight segments of B/Yamanashi/166/98. The virus yield of the supernatant was determined at different times after transfection by plaque assay on MDCK cells.
To formally prove that the virus in the supernatants of infected cells was derived from the input plasmids, the presence of the three silent nucleotide differences in PA were identified. RT-PCR was performed with allantoic fluid from embryonated chicken eggs infected with either wt B/Yamanashi/166/98 (wtB-Yam) or supernatant from cells transfected with eight plasmids (recB-Yam). The region of the PA gene encompassing nucleotides 1280–1290 was amplified by RT-PCR and sequenced (Fig. 3). Sequencing of the PCR products revealed that recB-Yam contained the three expected nucleotide changes relative to wtB-Yam. Thus, the recombinant virus was derived from the input plasmids.
In addition, all eight gene segments of recB-Yam were amplified by RT-PCR to evaluate the fidelity of the in vivo transcription of the type B segments. The sequences of the PCR products were determined by sequencing using segment-specific primers. There were no nucleotide differences between the sequences of the plasmid-derived, recombinant virus and those of the plasmids used for transfection. These data show that, after transfection of eight plasmids, all viral cDNAs are transcribed with high fidelity intracellularly, resulting in reproducible and efficient de novo generation of the influenza virus B/Yamanashi/166/98.
RT-PCR and Cloning of Genes Representing the HA and NA of Influenza B Virus.
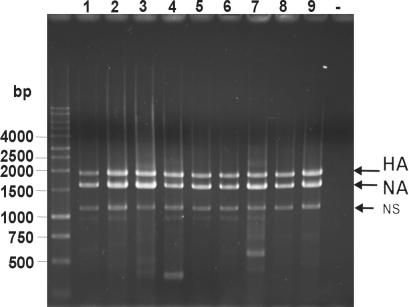
In general, for use of the plasmid-based system for rescue of vaccine virus strains, it would be advantageous to have a simple and reliable method for sequence determination and cloning of the genes representing the HA and NA glycoproteins. The primers were optimized for simultaneous RT-PCR amplification of the HA and NA segments. Comparison of the terminal regions of the vRNA representing the NCR of segment 4 (HA) and segment 6 (NB/NA) revealed that the 20 terminal nucleotides at the 5′ end and 15 nucleotides at the 3′ end were identical between the HA and NA genes of influenza B viruses. A primer pair for RT-PCR [(underlined sequences are influenza B virus specific) Bm-NAb-1, TAT TCG TCT CAG GGA GCA GAA GCA GAG CA; Bm-NAb-1557R, ATA TCG TCT CGT ATT AGT AGT AAC AAG AGC ATT TT] was synthesized and used to simultaneously amplify the HA and NA genes from various influenza B strains (Fig. 4). The HA and NA PCR fragments of B/Victoria/504/2000, B/Hawaii/10/2001, and B/Hong Kong/330/2001 were isolated, digested with BsmBI, and inserted into pAD3000 (Table 2). These results demonstrated the applicability of these primers for the efficient generation of plasmids containing the influenza B HA and NA genes from several different wt viruses. The RT-PCR products can be used for sequencing and/or cloning into the expression plasmids. Previously, a similar approach was used for the amplification of all eight segments of influenza A virus (33).
Fig 4.
RT-PCR for amplification of the HA and NA segments. RT-PCR was performed with the primer pair Bm-NAb-1/Bm-NAb-1557R. The PCR products were subjected to gel electrophoresis on a 1% agarose gel. RNA isolated from the following virus isolates were used: 1, B/Lee/40; 2, B/Ann Arbor/1/94; 3, B/Yamanashi/166/98; 4, B/Johannesburg/5/99; 5, B/Victoria/504/2000; 6, B/Sichuan/317/2001; 7, B/Shizuoka/15/2001; 8, B/Hawaii/10/2001; 9, B/Hong Kong/330/2001; –, no RNA.
Generation of 6 + 2 Reassortants with B/Yamanashi/166/98 as Backbone.
Influenza B viruses segregate between two distinct lineages, B/Victoria/2/87-like viruses and B/Yamagata/16/88-like viruses (2–6). To demonstrate the utility of B/Yamanashi/166/98 (a B/Yamagata/16/88-like virus) to efficiently express antigens from both these lineages, reassortants containing PB1, PB2, PA, NP, M, NS from B/Yamanashi/166/98, and the HA and NA from strains representing both the Victoria and Yamagata lineages (6 + 2 reassortants) were generated.
Transiently cocultured COS7-MDCK cells were cotransfected with six plasmids representing B/Yamanashi/166/98 and two plasmids containing the cDNA of the HA and NA segments of two strains from the B/Victoria/2/87 lineage, B/Hong Kong/330/2001 and B/Hawaii/10/2001, and one strain from the B/Yamagata/16/88 lineage, B/Victoria/504/2000. Six to seven days after transfection, the supernatants were titrated on fresh MDCK cells. All three 6 + 2 reassortant viruses had titers between 4–9 × 106 pfu/ml (Table 2). These data demonstrated that the six internal genes of B/Yamanashi/166/98 could efficiently form infectious virus with HA and NA gene segments from both influenza B lineages.
Relatively high titers are obtained by replication of wt B/Yamanashi/166/98 in eggs. Experiments were performed to determine whether this property was an inherent phenotype of the six “internal” genes of this virus. To evaluate this property, the yield of WT B/Victoria/504/2000, which replicated only moderately in eggs, was compared with the yield of the 6 + 2 reassortant expressing the B/Victoria/504/2000 HA and NA. These viruses in addition to wt and recombinant B/Yamanashi/166/98 were each inoculated into three or four embryonated chicken eggs, at either 100 or 1,000 pfu. Three days after infection, the allantoic fluids were harvested from the eggs and the TCID50 titers were determined on MDCK cells. The 6 + 2 reassortants produced similar quantities of virus in the allantoic fluid to the wt and recombinant B/Yamanashi/166/98 strain (Fig. 5). The difference in titer between B/Victoria/504/2000 and the 6 + 2 recombinant was ≈1.6 log10 TCID50 (0.7–2.5 log10 TCID50/ml, 95% confidence interval). The difference between B/Victoria/504/2000 and the 6 + 2 recombinant was confirmed on three separate experiments (P < 0.001). These results demonstrated that the egg growth properties of B/Yamanashi/166/98 could be conferred to HA and NA antigens that are normally expressed from strains that replicated poorly in eggs.
Fig 5.
Growth of 6 + 2 reassortants in eggs. Embryonated chicken eggs were inoculated with wt or recombinant virus. The virus titer was determined by titration on MDCK cells .
Discussion
The fact that we are now able to rescue influenza A and influenza B virus reproducibly from a small number of plasmids containing the bidirectional RNA pol I-pol II transcription system proves the utility of this approach for generation of infectious virus entirely from cloned cDNA. Recently, the rescue of Thogoto virus, a tick-transmitted type D orthomyxovirus with a genome consisting of six negative-stranded RNA segments, was reported (34). This system required two plasmid sets: one set for the expression of the six vRNAs, which utilizes the human pol I promoter, and the other set for the expression of mRNAs for the viral structural proteins under the control of a T7 promoter. Expression of this latter set of RNAs required coinfection with a vaccinia virus expressing T7 RNA polymerase. Transfection of these 12 plasmids into 293T cells resulted in the efficient recovery of recombinant Thogoto virus. Possibly, the dual pol I-pol II promoter system could simplify and improve the Thogoto virus rescue by reducing the number of plasmids to six and eliminate the need for coinfection with vaccinia virus. The high efficiency of the dual promoter system for both type A and type B virus suggests that infectious influenza C virus, which consists of seven segments, can be rescued by cotransfecting seven pol I-pol II plasmids.
In principle, plasmid-only systems allow the manipulation of the noncoding and coding regions of the viral RNA. The non coding regions contain cis-acting signals for the regulation of transcription and replication of viral RNA (35, 36). Type-specific differences of the NCRs between members of the Orthomyxovirus family were analyzed in the last decade mostly by using in vitro transcription assays or in vivo reconstitution of vRNA–like templates encoding reporter genes such as chloramphenicol acetyltransferase (37–40). Those studies can now be extended to characterize sequence elements that are type specific and those that modulate gene expression and can be exchanged between types in the context of infectious viruses. Compared with influenza A virus, the NCRs of influenza B viruses are relatively large, extending up to 100 nt. By using the ribonucleoprotein transfection method (41) combined with an efficient antibody-driven selection method, the HA-NCR of influenza B virus was shown to be flexible in sequence and in length (42). Because the eight-plasmid system for influenza B virus does not require any selection procedure, similar mutagenesis studies can now be applied to all eight gene segments.
The classical method for generating influenza B inactivated vaccine virus is to grow the wt strain in embryonated chicken eggs. However, not all influenza B strains grow to high titers in eggs; therefore, occasionally a wt virus that is antigenically similar to, but not identical to, the circulating wt strain and that grows to acceptable titers in eggs is selected for vaccine production. The process of evaluating suitable vaccine candidates that meet these criteria is time consuming and laborious and may result in a candidate that lacks the optimal antigenicity. Here, we have demonstrated that the eight-plasmid system allows the generation of 6 + 2 reassortants expressing antigens from both influenza B lineages with the B/Yamanashi/166/98 backbone. These reassortants grew well in eggs and in most cases to higher titers than the wt parent expressing the HA and NA antigens.
The plasmid rescue system for influenza B virus described here should advance the reliability and quality of vaccines expressing appropriate HA and NA antigens. The consensus sequence of the recombinant transfectant virus was identical to the viral inserts in the plasmid clones. This high level of sequence integrity has been demonstrated with several other rescued type A viruses (43, 44). In addition, plasmid collections representing all antigenic variants of the B/Yamagata/16/88 and B/Victoria/2/87 lineages can now be created by using primers suitable for simultaneous RT-PCR of the HA and NA genes. Two to three weeks are required for sequencing and cloning of the HA and NA genes; subsequently, the reassortant viruses can be generated within 1 week. In addition to the faster generation of reassortants, using a standard master strain such as B/Yamanashi/166/98 may result in a more homogenous virus population with regard to the size and shape of virus particles. The growth of the reassortant viruses to high HA titers in eggs indicates that the growth is not restricted by incompatibilities between the six internal genes of B/Yamanashi/166/98 and the glycoproteins from the selected vaccine strains. Genetic engineering of the B/Yamanashi/166/98 plasmids or use of a different high growing master strain such as B/Lee/40, which has recently been rescued in our laboratory, may even increase the virus yield.
The plasmid rescue system for influenza B will enable molecular genetic studies of influenza B viruses. Influenza A and B viruses have distinctive molecular biological properties and produce different gene products. The advent of a molecular genetics system that allows recombinant viruses to be made without requiring a selective pressure should allow dissection of specific gene functions of influenza B virus. This system can be used to evaluate attenuating lesions in attenuated influenza B strains, such as B/Ann Arbor/1/66, and discover the requirement for specific gene products during the viral replication cycle.
Acknowledgments
We thank the members of the tissue culture facility at MedImmune Vaccines for supplying cells. We thank Jackie Zhao, Dan Ye, Anantha Rojanala, and Marla Chu for excellent technical assistance. We thank Mark Prichard for constructing pAD3000. These studies were supported in part by Public Health Research Grants AI95357 and AI29680 from the National Institute of Allergy and Infectious Diseases and by the American Lebanese Syrian Associated Charities.
Abbreviations
HA, hemagglutinin
MDCK, Madin–Darby canine kidney
NCR, noncoding region
NA, neuraminidase
NP, nucleoprotein
NS, nonstructural
pol I, RNA polymerase I
pol II, RNA polymerase II
pfu, plaque-forming unit
RT, reverse transcriptase
vRNA, viral RNA
wt, wild type
TCID50, tissue culture 50% infective dose
References
- 1.Klimov A., Simonsen, L., Fukuda, K. & Cox, N. (1999) Vaccine 17, Suppl. 1, S42-S46. [DOI] [PubMed] [Google Scholar]
- 2.Rota P. A., Wallis, T. R., Harmon, M. W., Rota, J. S., Kendal, A. P. & Nerome, K. (1990) Virology 175, 59-68. [DOI] [PubMed] [Google Scholar]
- 3.Rota P. A., Hemphill, M. L., Whistler, T., Regnery, H. L. & Kendal, A. P. (1992) J. Gen. Virol. 73, 2737-2742. [DOI] [PubMed] [Google Scholar]
- 4.Kanegae Y., Sugita, S., Endo, A., Ishida, M., Senya, S., Osako, K., Nerome, K. & Oya, A. (1990) J. Virol. 64, 2860-2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nerome R., Hiromoto, Y., Sugita, S., Tanabe, N., Ishida, M., Matsumoto, M., Lindstrom, S. E., Takahashi, T. & Nerome, K. (1998) Arch. Virol. 143, 1569-1583. [DOI] [PubMed] [Google Scholar]
- 6.McCullers J. A., Wang, G. C., He, S. & Webster, R. G. (1999) J. Virol. 73, 7343-7348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindstrom S. E., Hiromoto, Y., Nishimura, H., Saito, T., Nerome, R. & Nerome, K. (1999) J. Virol. 73, 4413-4426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osterhaus A. D., Rimmelzwaan, G. F., Martina, B. E., Bestebroer, T. M. & Fouchier, R. A. (2000) Science 288, 1051-1053. [DOI] [PubMed] [Google Scholar]
- 9.Baez M., Palese, P. & Kilbourne, E. D. (1980) J. Infect. Dis. 141, 362-365. [DOI] [PubMed] [Google Scholar]
- 10.Maassab H. F. & DeBorde, D. C. (1985) Vaccine 3, 355-369. [DOI] [PubMed] [Google Scholar]
- 11.Belshe R. B. & Gruber, W. C. (2001) Philos. Trans. R. Soc. London B Biol. Sci. 356, 1947-1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaverin N. V., Varich, N. L., Sklyanskaya, E. I., Amvrosieva, T. V., Petrik, J. & Vovk, T. C. (1983) J. Gen. Virol. 64, 2139-2146. [DOI] [PubMed] [Google Scholar]
- 13.Mikheeva A. & Ghendon, Y. Z. (1982) Arch. Virol. 73, 287-294. [DOI] [PubMed] [Google Scholar]
- 14.Neumann G., Watanabe, T., Ito, H., Watanabe, S., Goto, H., Gao, P., Hughes, M., Perez, D. R., Donis, R., Hoffmann, E., Hobom, G. & Kawaoka, Y. (1999) Proc. Natl. Acad. Sci. USA 96, 9345-9350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fodor E., Devenish, L., Engelhardt, O. G., Palese, P., Brownlee, G. G. & García-Sastre, A. (1999) J. Virol. 73, 9679-9682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoffmann E., Neumann, G., Kawaoka, Y., Hobom, G. & Webster, R. G. (2000) Proc. Natl. Acad. Sci. USA 97, 6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schickli J. H., Flandorfer, A., Nakaya, T., Martinez-Sobrido, L., García-Sastre, A. & Palese, P. (2001) Philos. Trans. R. Soc. London B Biol. Sci. 356, 1965-1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffmann, E., Krauss, S., Perez, D., Webby, R. & Webster, R. G. (2002) Vaccine, in press. [DOI] [PubMed]
- 19.Paragas J., Talon, J., O'Neill, R. E., Anderson, D. K., García-Sastre, A. & Palese, P. (2001) J. Virol. 75, 7375-7383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zobel A., Neumann, G. & Hobom, G. (1993) Nucleic Acids Res. 21, 3607-3614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neumann G. & Kawaoka, Y. (2001) Virology 287, 243-250. [DOI] [PubMed] [Google Scholar]
- 22.Londo D. R., Davis, A. R. & Nayak, D. P. (1983) J. Virol. 47, 642-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamashita M., Krystal, M., Fitch, W. M. & Palese, P. (1988) Virology 163, 112-122. [DOI] [PubMed] [Google Scholar]
- 24.Betakova T., Nermut, M. V. & Hay, A. J. (1996) J. Gen. Virol. 77, 2689-2694. [DOI] [PubMed] [Google Scholar]
- 25.Brassard D. L., Leser, G. P. & Lamb, R. A. (1996) Virology 220, 350-360. [DOI] [PubMed] [Google Scholar]
- 26.Sunstrom N. A., Premkumar, L. S., Premkumar, A., Ewart, G., Cox, G. B. & Gage, P. W. (1996) J. Membr. Biol. 150, 127-132. [DOI] [PubMed] [Google Scholar]
- 27.Inglis S. C. & Brown, C. M. (1981) Nucleic Acids Res. 9, 2727-2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lamb R. A., Zebedee, S. L. & Richardson, C. D. (1985) Cell 40, 627-633. [DOI] [PubMed] [Google Scholar]
- 29.Horvath C. M., Williams, M. A. & Lamb, R. A. (1990) EMBO J. 9, 2639-2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Odagiri T., Hong, J. & Ohara, Y. (1999) J. Gen. Virol. 80, 2573-2581. [DOI] [PubMed] [Google Scholar]
- 31.Chen W., Calvo, P. A., Malide, D., Gibbs, J., Schubert, U., Bacik, I., Basta, S., O'Neill, R., Schickli, J., Palese, P., Henklein, P., Bennink, J. R. & Yewdell, J. W. (2001) Nat. Med. 7, 1306-1312. [DOI] [PubMed] [Google Scholar]
- 32.Hiromoto Y., Saito, T., Lindstrom, S. E., Li, Y., Nerome, R., Sugita, S., Shinjoh, M. & Nerome, K. (2000) J. Gen. Virol. 81, 929-937. [DOI] [PubMed] [Google Scholar]
- 33.Hoffmann E., Stech, J., Guan, Y., Webster, R. G. & Perez, D. R. (2001) Arch. Virol. 146, 2275-2289. [DOI] [PubMed] [Google Scholar]
- 34.Wagner E., Engelhardt, O. G., Gruber, S., Haller, O. & Kochs, G. (2001) J. Virol. 75, 9282-9286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Desselberger U., Racaniello, V. R., Zazra, J. J. & Palese, P. (1980) Gene 8, 315-328. [DOI] [PubMed] [Google Scholar]
- 36.Stoeckle M. Y., Shaw, M. W. & Choppin, P. W. (1987) Proc. Natl. Acad. Sci. USA 84, 2703-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neumann G. & Hobom, G. (1995) J. Gen. Virol. 76, 1709-1717. [DOI] [PubMed] [Google Scholar]
- 38.Flick R., Neumann, G., Hoffmann, E., Neumeier, E. & Hobom, G. (1996) RNA 2, 1046-1057. [PMC free article] [PubMed] [Google Scholar]
- 39.Crescenzo-Chaigne B., Naffakh, N. & van der Werf, S. (1999) Virology 265, 342-353. [DOI] [PubMed] [Google Scholar]
- 40.Tchatalbachev S., Flick, R. & Hobom, G. (2001) RNA 7, 979-989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luytjes W., Krystal, M., Enami, M., Pavin, J. D. & Palese, P. (1989) Cell 59, 1107-1113. [DOI] [PubMed] [Google Scholar]
- 42.Barclay W. S. & Palese, P. (1995) J. Virol. 69, 1275-1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Takeda M., Pekosz, A., Shuck, K., Pinto, L. H. & Lamb, R. A. (2002) J. Virol. 76, 1391-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Perez D. R. & Donis, R. O. (2001) J. Virol. 75, 8127-8136. [DOI] [PMC free article] [PubMed] [Google Scholar]