Abstract
Primary care physicians increasingly have treated depressive disorders over the last decade. Unrecognized bipolar disorder, sometimes misdiagnosed as unipolar depression, may lead to treatment resistance or nonresponse. We describe differences between unipolar and bipolar disorders, focusing on recognition, diagnosis, and treatment of bipolar spectrum disorders such as bipolar I, bipolar II, antidepressant-induced mania, and cyclothymia. Broadening the understanding of these different disorders and their presentation in primary care settings can enable earlier and more targeted treatment. Though 3 mood stabilizers are U.S. Food and Drug Administration–approved for treatment of acute mania, no medications are currently approved for treating bipolar depression.
The 1990s saw an unprecedented emphasis and change in the clinical approach to depression in primary care settings. Motivated by the knowledge that depressive disorders are common and treatable; encouraged by educational efforts sponsored by government, industry, and advocacy groups; and armed with new antidepressants considered efficacious, tolerable, and safe, many primary care practitioners became comfortable with treating this clinical entity, which has significant personal, interpersonal, occupational, and social costs.1–3 Improvements in the clinical management of depressive disorders have produced significant gains in clinical outcomes and practice satisfaction.4,5 However, emerging data indicate a ceiling effect on response and remission rates for antidepressant monotherapies6 and, paradoxically, reports of treatment-emergent adverse responses, at times reported in dramatic fashion in the media.
A significant source of this treatment resistance and both patient and physician frustration may be unrecognized bipolar spectrum illness presenting as “unipolar” major depression.7,8 Patients with such “pseudo-unipolar”9 illnesses, when treated with antidepressant monotherapy, are unlikely to respond adequately and are at significant risk of treatment-emergent hypomania/mania, anxious and agitated states that represent a shift to a bipolar mixed state, and a rapid-cycling course10—all of which are forms of complicated and highly refractory mood disorders.11 Treatment with mood stabilizers either alone or in conjunction with an antidepressant may therefore be required for illness remission.12
An understanding of the bipolar spectrum and its presentation in primary care, proper assessment, and treatment approach can enable clinicians to benefit from advances in the treatment of bipolar illness. This understanding will also provide opportunities to successfully intervene in many clinical scenarios as an alternative to or during transition to specialty care. This article focuses on the diagnosis and treatment of bipolar spectrum disorders and highlights differences between bipolar and unipolar illness.
DEFINITION OF THE BIPOLAR SPECTRUM
The connection between melancholia and mania has been recognized since ancient times. In the early 1900s, the German psychiatrist Kraepelin13 offered descriptions and definitions of a spectrum of mood aberrations that endure to the present. Kraepelin, who coined the term manic-depressive, viewed the illness as a continuum of morbidity ranging from extremes of exalted mood and increased activity (mania) to periods of despondency and sluggishness of thought and action (depression). A recent revival of the spectrum concept based in biological, pedigree, and prospective studies that link the 2 extreme manifestations of the illness with mixed depressed/excited presentations and other less extreme excited states has emerged due to the work of Dunner,14 Akiskal,15 Angst,16 Goodwin and Jamison,17 and others. This concept has not been heavily emphasized in recent American psychiatric nosology contained in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),18 and its predecessors, though some subcategorization is included, as described below.
The bipolar spectrum includes, but is not limited to, bipolar I (mania), bipolar II (major depression and hypomania), depressions with possibly pharmacologically mobilized hypomania, cyclothymic disorder (“minor” depression and hypomania), depression arising from temperamental hypomanic traits, depression on a cyclothymic temperamental baseline, and periodic depression responsive to mood stabilizers.7,19 Only the first 3 diagnoses are specifically included in the current version of the DSM, while the others are subsumed as bipolar disorder not otherwise specified (NOS). For primary care physicians, the disorders classified under the NOS category are often most relevant. DSM-V may redefine bipolar disorder to include some additional bipolar spectrum illnesses.7
EPIDEMIOLOGY OF THE BIPOLAR SPECTRUM AND ITS POTENTIAL IMPACT ON PRIMARY CARE PSYCHIATRY
When bipolar disorder is narrowly defined as requiring manic states, most studies find a general population prevalence of around 1%.20,21 When the definition is expanded to include bipolar II disorder and related conditions, the prevalence increases to as much as 5%.22 Other estimates have reported even higher rates,23 but a figure considerably expanded beyond that of the older investigations (1%) to at least 5% is reasonable.
High prevalence of bipolarity in both outpatient psychiatric24,25 and primary care settings26,27 has been reported on the basis of histories sensitive for bipolar elements, careful examination of family history, and prospective follow-up. Only one third of mental health services are delivered in the specialty mental health sector,28 leaving the remaining two thirds to be delivered elsewhere by nonpsychiatrists, principally in the primary care sector; this suggests that generalists care for the majority of those with bipolar illness. The recognition of bipolar disorder has been problematic even in the specialty mental health sector, with delays in correct diagnosis of 8 to 12 years.29 Much of this delay appears to reflect misdiagnosis as unipolar depression,30,31 overlooking bipolar features and thereby potentially promoting inappropriate treatment choices.32
CLINICAL EVALUATION
Diagnosis
Since no clinically available biological markers with sufficient sensitivity and specificity exist, the diagnosis of bipolar illness depends on accurate history taking, exploration of family pedigree, and longitudinal examination during treatment. Diagnosis is an integrative process in which experienced clinicians using multiple sources of information over time are the gold standard.33 Though an average single primary care visit may be inadequate to complete such an assessment, serial observations combined with self-report instruments and psychoeducation make this assessment eminently possible for motivated clinicians and patients. Those in primary care may be well positioned to make these diagnoses because of continuity of care and opportunities to observe patients closely within the family systems they care for.
The usual clinical process contains steps that are common to all patient interactions. The state of dysfunction and impairment must be recognized, pertinent medical conditions and psychosocial comorbidities assessed, and a differential diagnosis formulated. Diagnostic confirmation of bipolar disorders includes careful assessment of the morbid phenomenology (presenting signs and symptoms), temperamental predisposition, longitudinal course of the illness, previous responses to treatment, and a multigenerational review of family history. These steps do not all need to be made in an initial visit, and full confirmation often requires information from collateral sources. Steps that ensure proper diagnosis often lay strong foundations for solid therapeutic alliances between patients and clinicians, which allow candid discussions about treatment modalities and lead to appropriate selection and better compliance.
The morbid phenomenology of bipolar disorders has traditionally hinged on identifying periods of abnormal expansive or irritable mood that cause significant dysfunction and that are not the result of another general medical illness or substance. These periods of expansive mood, mania and hypomania, are described in DSM-IV (Table 1).18 Those meeting the criteria for a manic episode are diagnosed with bipolar I disorder. Those experiencing periods of expansive/irritable mood of lesser duration and severity plus an episode of major depression are diagnosed with bipolar II disorder, the most prevalent form of bipolar illness.34 It should be noted, however, that bipolar I patients often experience hypomania, and the diagnosis can be modified to communicate a most recent episode of hypomania. Hypomania, by definition, is nonpsychotic. Of significance is the fact that patients, when interviewed in a depressed episode, may not remember past hypomania.35 External sources of information are important, and the DSM-IV requires observation of the hypomania by others to confirm the diagnosis. Though the DSM-IV requires a hypomania duration of 4 days, a duration of 2 to 3 days does not seem to reduce diagnostic specificity.36 The mean modal duration of hypomania was found to be 1 to 3 days in one study.37 A large prospective study found temperamental factors to be more predictive than DSM-IV hypomanic episodes in the diagnosis of bipolar illness.38 Hypomania may be an abrupt “switch” from a depressed to an energetic state, typically occurring in the morning on arising (1–2 hours before one's usual awakening) or in the late evening, which may be preceded and followed by a period of hypersomnic, retarded depression and, though usually elated or euphoric in quality, can be mixed with severe irritability, especially as the hypomania continues.15
Table 1.
DSM-IV Criteria for Manic and Hypomanic Episodea

Clinicians need to be aware of the phenomenon of antidepressant-induced hypomania/mania. This type of response typically occurs within the first 2 weeks of antidepressant therapy and is characterized by sudden switches from depression into symptoms of expansive mood or restless agitation and insomnia with racing thoughts. These abrupt “recoveries” are often welcomed by patients and their clinicians, but are short lived, and their disappearance may prompt an increase in antidepressant doses to regain the improvement. In many of these cases, further increases in antidepressant doses fail to replicate the initial switch and may incite the periods of intense dysphoria, insomnia, irascibility, and restlessness seen in bipolar mixed states. Tricyclic antidepressants are more prone to cause switching than selective serotonin reuptake inhibitors. There is evidence that bupropion and monoamine oxidase inhibitors (MAOIs) are less likely to cause hypomanic/manic switches and rapid cycling.39
The emergence of resistance to antidepressant therapy is also common in bipolar disorder. The first episode of antidepressant therapy may be quite successful, only to be followed in subsequent episodes by nonresponse, partial response, or the treatment-emergent problems discussed earlier. While unipolar treatment-resistant depression may be effectively treated with antidepressant combination or augmentation strategies, failure to respond to 3 or more adequate antidepressant trials suggests an increased likelihood of bipolar illness.40
Differential Diagnosis
Depressive episodes associated with bipolar II disorder can sometimes be difficult to distinguish from unipolar depression. For example, primary care physicians may first suspect bipolar disorder only after symptoms of mania are precipitated by an antidepressant or if depressive symptoms do not respond to an antidepressant. In one major investigation, mood lability, depressions mixed with increased mental or physical energy, intense daydreaming, and social anxiety were significantly associated with bipolar II disorder over unipolar depression.38 Mood lability alone was 86% specific. This study also suggested that Axis II personality features mixing cluster B (erratic) and cluster C (avoidant) were more common in bipolar II patients.
Table 2 summarizes the performance of various factors in determining whether patients who first present with depression are ultimately diagnosed as having unipolar or bipolar disorder. Bipolar depressions often take on the features of “atypical depression,” with greater tendency for emotional reaction to external events than is typical for depression, as well as hypersomnia, hyperphagia, and rejection sensitivity. The predictive value of atypical depression as an early indicator of bipolarity has been the subject of much debate, but recent longitudinal studies using sensitive interviews have found a high rate of bipolar disorder in those affected.41 Atypical depressions, with symptoms such as increased appetite and increased sleep, are more common in younger females with an early onset of depressive episodes and predict a nonresponse to tricyclic antidepressants and a greater responsiveness to MAOI antidepressants. At the very least, the presence of atypical depression should serve as an impetus to screen carefully for evidence of bipolarity.
Table 2.
Bipolar and Unipolar Depression: Distinguishing Factorsa

Temperament is another aspect of early detection of bipolar disorders. Temperament may be defined as early-onset (childhood or adolescence), nonimpairing (subsyndromal), habitual traits observable by others that precede and endure episodes of disturbed mood. Temperaments differ from personality disorders and other long-term conditions in that they do not necessarily constitute any pathology or impairment. For example, cyclothymic personality disorder and dysthymic disorder, according to DSM-IV, are considered mental illnesses, whereas cyclothymic and dysthymic temperaments are not. The importance of temperament was put forth by Kraepelin,13 later championed by Kretschmer,42 and more recently operationalized by Akiskal and Mallya, who outlined criteria for hyperthymic, dysthymic, cyclothymic, and irritable temperaments.15,43
Hyperthymic temperaments are more “manic,” and persons with these temperaments may be overinvolved, overconfident, euthymic, excessively talkative, extraverted, highly energetic, and habitual short sleepers. Dysthymic persons, on the other hand, tend to worry and are more introverted, self-critical, pessimistic, preoccupied with inadequacy and failure, and habitually hypersomnolent. Cyclothymic temperaments chronically alternate between hyperthymic and dysthymic features. For example, a person with cyclothymic temperament will experience hypersomnia alternating with decreased need for sleep, or quiet phases alternating with disproportionate talkative periods. Irritable temperaments include excessive complaining, impulsive behavior, dysphoric restlessness, and habitual moodiness. Awareness of affective temperaments helps clinicians recognize early presentations of bipolar illness. Temperamental presentations in the children of bipolar patients are common and may offer opportunities to intervene before disruptive episodes occur. Hyperthymic and cyclothymic temperaments are particularly associated with bipolar disorders.11,44 The irritable temperament is a subsyndromal mixing of dysthymic and hyperthymic temperaments and often an extension of cyclothymic precursors. It may be viewed as a temperamental mixed state.
Family History
Close examination of a patient's family history is invaluable in the early and accurate detection of bipolarity. Most affected children of bipolar I probands have illnesses that pursue a predominately depressive course.45 In the absence of a history of a clear manic episode in the patient presenting, eliciting during an interview a positive response for a parent or sibling with the disorder should arouse strong suspicions of bipolarity. Bipolar pedigrees also differ from those of unipolar illness in that they are more loaded for mood disorders and related conditions (substance abuse/dependency, sociopathy, etc.).15
Longitudinal Course
The longitudinal courses of bipolar and unipolar illness also differ significantly. Bipolar illness typically begins during childhood or adolescence (usually earlier than 26 years of age). Depressive episodes usually precede hypomanic or manic episodes. Indeed, minor mood aberrations in either the depressive (more common) or manic (less common) direction are easily overlooked in younger patients and attributed to age-appropriate excitability and reactions to external contexts. Careful examination of pedigree and longitudinal course are important in the evaluation of “minor” mood fluctuations that may be heralds of syndromal illness and resulting dysfunction.
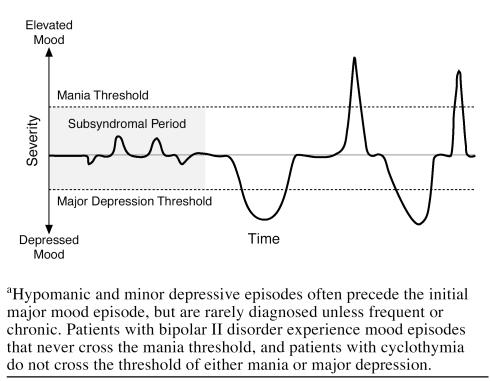
Figure 1 represents the longitudinal course of bipolar disorder. Hypomania and minor depressive episodes often precede a full-blown major mood episode, but are rarely diagnosed as such until a more intense episode is recognized. Diagnosis is more likely when these minor episodes occur frequently or become chronic. Major depressive episodes usually occur before mania in bipolar disorders. Careful history taking is necessary to uncover possible hypomanic episodes that may have preceded these episodes, greatly assisting the physician in recognizing that a patient probably has bipolar and not unipolar disorder. Uncovering such episodes, as well as gathering additional clues from family history, enduring temperaments, personality traits, and functional disturbances, is crucial to initiating proper therapies.
Figure 1.
Longitudinal Course of Bipolar I Illnessa
Mood stabilizer therapy (in combination with an antidepressant when appropriate) would attenuate mood elevations and depressions, if initiated at appropriate times. By contrast, antidepressant prescription in the absence of a mood stabilizer risks precipitating hypomanic or manic episodes and may accelerate cycling frequency.30
SCREENING FOR BIPOLAR DISORDER
For the screening of bipolar disorder, a self-administered questionnaire recently proposed by Hirschfeld and colleagues has been validated to some extent in outpatient specialty mood disorder centers, but the populations used to evaluate the instrument had predominately bipolar I illness.46 In these more classically ill patients in tertiary care settings, the Mood Disorder Questionnaire (MDQ) achieved sensitivity and specificity of 73% and 90%, respectively. However, most bipolarity is in the “soft” bipolar spectrum (bipolar II and related disorders). At present, limited data on sensitivity, specificity, or predictive value exist for the MDQ in this part of the bipolar spectrum. Validation of the MDQ in primary care settings is needed to achieve greater applicability to bipolar spectrum disorders. More sensitive instruments that assess enduring traits of patients with bipolar disorder would also be useful.19
TREATMENT OF BIPOLAR SPECTRUM ILLNESS
The treatment of bipolar spectrum illness begins with recognizing that mood stabilization is essential to illness remission. A number of mood stabilizers are available and are listed in Table 3.
Table 3.
Available Mood Stabilizersa

Lithium has been used in the mood stabilization of bipolar illness since the early 1970s. It is effective in predominantly euphoric manic states, especially in patients with non–rapid cycling illness (≤ 4 mood switches per year). To date, lithium is the best-established agent for relapse prevention in bipolar disorder, and is the only one with a U.S. Food and Drug Administration–approved indication for maintenance therapy. Lithium has been shown to be an effective augmentation of antidepressants for both unipolar and bipolar patients,47 and some have reported favorable results as a monotherapy for bipolar depression, but a recent review concluded that its efficacy is not clear.48 Lithium use may have significant disadvantages, however. These include lack of efficacy as a primary agent in mixed presentations, a narrow therapeutic window, teratogenicity, and a side effect profile that may limit patient adherence. Nephrogenic diabetes insipidus (due to competitive inhibition of antidiuretic hormone in the renal collecting tubules), nausea, diarrhea, tremor, and negative cognitive effects are common with lithium levels in the therapeutic range. Subjective impression of “memory impairment” is the most common explanation by patients for noncompliance with lithium.49 Lithium-associated hypothyroidism may affect ≥ 20% of patients on lithium maintenance therapy. Regular thyroid monitoring is advisable. Though lithium is not nephrotoxic at therapeutic doses, lithium toxicity has been associated with permanent renal insufficiency. Periodic monitoring of renal function is advisable. Dose adjustments may be necessary, as renal function declines with age. In spite of these limitations, lithium continues to have a role in the management of bipolar illness, particularly in doses in the lower therapeutic range or just below the traditional therapeutic range in combination with other mood stabilizers. It may be especially useful in the treatment of bipolar depression.
Several antiepileptic drugs are potentially useful in bipolar illness.50 Reports of efficacy date to the early 1960s for valproic acid and the 1970s for carbamazepine. Gastrointestinal side effects limited the use of valproic acid, but the introduction of divalproex in the late 1980s enabled extensive clinical testing and use. Divalproex has demonstrated effectiveness in acute mania, as well as for the manic aspects of mixed presentations. We are not aware of any controlled evidence of antidepressant efficacy. Open-label maintenance data are promising, but neither divalproex nor lithium was effective in the only placebo-controlled trial of divalproex maintenance to date.51 Plasma level monitoring is recommended, with the aim of maintaining levels from 50 to 125 ng/mL. The most common adverse effects are nausea, diarrhea, cognitive blunting, somnolence, hair loss, and tremor. Weight gain occurs over a number of months. These effects may be limited in patients taking maintenance divalproex by using the extended-release formulation of the drug. Elevations in hepatic transaminases and thrombocytopenia can occur. Pancreatitis is associated with divalproex but is uncommon. Hepatic failure is uncommon and more likely in infants taking divalproex in combination with other, usually multiple, antiepileptic drugs. Significant abdominal pain or persistent gastrointestinal complaints should prompt investigation. Potential teratogenicity is also of concern, especially given that many patients affected by bipolar disorder are of childbearing age. The disease may result in decreased ability to comply with medication instructions, thus increasing the risk of side effects. Divalproex may be a reasonable choice in bipolar patients with comorbid migraine, panic attacks, or substance abuse since it is indicated for migraine prophylaxis, open and controlled investigations suggest efficacy in treatment-resistant panic attacks,52–54 and bipolar substance abusers tend to have more rapid cycling and mixed patterns of illness.55 Carbamazepine has shown efficacy in controlled studies of mania and may be effective for rapid-cycling states. However, it may be associated with blood dyscrasias (such as agranulocytosis) and hepatitis, and blood monitoring is required. Moreover, it is an inducer of the cytochrome oxidase system; over time, it speeds its own metabolism as well as that of other medications that share its metabolic pathway. Gabapentin demonstrated efficacy in open reports,56,57 but not in placebo-controlled trials58 of manic states. Its usefulness is being explored for panic attacks or social anxiety that may be comorbid with bipolar disorder.
Lamotrigine has also shown efficacy in the treatment of bipolar disorder, notably in bipolar depression59 and rapid-cycling states,60 although limited trials have not shown efficacy for mania. Its efficacy extends into the soft (nonmanic) bipolar spectrum,61 although at present most investigations have focused on bipolar I disorder. Lamotrigine, like carbamazepine, may induce a hypersensitivity rash that in rare cases can progress to Stevens-Johnson syndrome. Slow upward titration of dose is thought to limit this side effect. Concomitant use with divalproex (increasing lamotrigine levels) is associated with an increased risk of rash and necessitates even slower titrations. Other possible side effects include insomnia, jitteriness, headache, and anorexia.
Conventional antipsychotics were used as adjunctive medications for bipolar disorder in the past, but lost favor because of higher risks of extrapyramidal symptoms (EPS) and tardive dyskinesia (TD), as well as a propensity for cognitive impairment. Moreover, they appear more antimanic than mood stabilizing; that is, they may promote dysphoria or depressive episodes. By contrast, atypical antipsychotics retain activity against psychosis while improving cognitive impairments and other symptoms in patients with schizophrenia and therefore have more recently been identified as mood-stabilizing medications. Olanzapine is the only atypical antipsychotic with an indication for acute mania, demonstrating efficacy in placebo-controlled clinical trials.62,63 It has activity comparable to or exceeding that of divalproex in mania (both pure and mixed types). Olanzapine, but not divalproex sodium or lithium, reduces symptoms of depression in manic states.64,65
Olanzapine requires no plasma level monitoring, has a limited number of drug-drug interactions, and is typically well tolerated. It has a low incidence of EPS in its usual therapeutic range and has a low incidence of associated TD. Appetite increases associated with olanzapine are not dose related, occur early in treatment, and plateau after several months of therapy.66,67 Subsequent weight gain occurs more often in patients with a low body mass index at the beginning of therapy. As with other atypical antipsychotics, appetite increases may be positively associated with therapeutic response and often respond to behavioral and drug interventions.67
Recent data suggest that olanzapine alone or in combination with fluoxetine has efficacy in treating bipolar depression.68,69 Tohen and colleagues found that olanzapine monotherapy (5–20 mg/day) significantly improved bipolar depressive symptoms (p < .001 vs. placebo; baseline to endpoint).68 Moreover, the combination of olanzapine (6 or 12 mg/day) and fluoxetine (25 or 50 mg/day) significantly improved depressive symptoms versus both placebo (p < .001) and olanzapine monotherapy (p = .002). Patients may benefit from combination therapy with olanzapine plus fluoxetine chosen for a suspected bipolar depression while it is being differentially diagnosed. If the result of the diagnostic inquiry confirms the diagnosis of unipolar depression with a significant level of treatment resistance, the combination of olanzapine and fluoxetine is still a rational and effective option. In a pilot study by Shelton and colleagues40 and in subsequent studies combining antidepressants and atypicals, the combination of olanzapine and fluoxetine consistently has shown significantly increased response in treatment-resistant depression with side effects no greater than those of either of the 2 components when evaluated separately.
Olanzapine maintenance data are limited to date; one controlled 18-month study found that patients whose acute mania responded to a combination of olanzapine and lithium or divalproex were about half as likely to relapse when maintained on the combination versus those randomly assigned to monotherapy with lithium or divalproex.70
TREATMENT STRATEGIES
When bipolar disorder is recognized at presentation, mood stabilizers are the preferred medications for initiating treatment.71 Combinations of mood stabilizers may be necessary to adequately treat or prevent periods of expansive and depressed mood. Antidepressants may be added to mood stabilizers for treating bipolar depression. Whether the antidepressant should be discontinued as the episode of depression ends (to avoid antidepressant-associated mood deterioration) or continued as prophylaxis against further episodes of depression is a subject of discussion and research.
Because depression is the most prevalent manifestation of bipolar II disorder and the initial episode of bipolar I disorder, clinicians managing bipolar disorder patients are most often faced with treating depression. These patients often are already taking an antidepressant that is yielding only partial or inconsistent response, and then receive a revised diagnosis of bipolar spectrum disorder during these ineffective antidepressant therapies. In this clinical scenario, the decision is often whether to discontinue the antidepressant prior to instituting a mood stabilizer or add the mood stabilizer to the antidepressant. Unfortunately, no evidence-based research is available to guide clinicians, though many prefer to add a mood stabilizer to the existing antidepressant to avoid acute worsening of the depressed episode before the mood stabilizer becomes effective. This strategy should be altered somewhat if the antidepressant is clearly causing significant mixed symptoms (anxiety, racing thoughts, irascibility, agitation), in which case a dose reduction or elimination of the antidepressant should be seriously considered. The choice of the mood stabilizer used to augment or replace such an antidepressant is inadequately researched. Olanzapine may be a reasonable choice, however, because of its efficacy across a variety of bipolar presentations—manic and mixed presentations as well as bipolar depression—relative ease of use, efficacy in combination with antidepressants such as fluoxetine for difficult-to-treat depressive episodes, and emerging evidence of efficacy for relapse prevention.72
CONCLUSION
Bipolar spectrum disorder is more common in primary care than previously believed. When bipolar disorder remains unrecognized, patients are at risk of inappropriate antidepressant treatment that is unlikely to result in robust, sustained response. Paradoxically, such antidepressant use is associated with acute and chronic deterioration apart from the negative effects of living with a debilitating condition. Primary care clinicians, responsible for delivering the majority of mental health services in the United States, are becoming more aware of this phenomenon and are more prepared to recognize these patients early and consult, refer, or initiate disease-specific interventions on the basis of the clinical context. Such interventions are well within the capabilities of clinicians who are expanding their knowledge base of mood disorder nosology and psychopharmacology to accommodate this important clinical reality.
Drug names: bupropion (Wellbutrin and others), carbamazepine (Tegretol and others), divalproex sodium (Depakote), fluoxetine (Prozac and others), gabapentin (Neurontin), lamotrigine (Lamictal), lithium (Eskalith, Lithobid, and others), olanzapine (Zyprexa), valproic acid (Depakene and others).
Pretest and Objectives
Posttest
Registration and Evaluation
Footnotes
In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the faculty for this CME activity were asked to complete a full disclosure statement. The information received is as follows: Dr. Manning is a consultant for, has received grant/research support from, and is a member of the speakers/advisory board for Lilly. Drs. Ahmed and Hay and Ms. McGuire are employees of Lilly.
REFERENCES
- Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA. 1989;262:914–919. [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Linzer M, et al. Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 Study. JAMA. 1995;274:1511–1517. [PubMed] [Google Scholar]
- Hays RD, Wells KB, Sherbourne CD, et al. Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry. 1995;52:11–19. doi: 10.1001/archpsyc.1995.03950130011002. [DOI] [PubMed] [Google Scholar]
- Simon GE, Katon WJ, VonKorff M, et al. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. Am J Psychiatry. 2001;158:1638–1644. doi: 10.1176/appi.ajp.158.10.1638. [DOI] [PubMed] [Google Scholar]
- Lin EH, VonKorff M, Russo J, et al. Can depression treatment in primary care reduce disability? a stepped care approach. Arch Fam Med. 2000;9:1052–1058. doi: 10.1001/archfami.9.10.1052. [DOI] [PubMed] [Google Scholar]
- Nierenberg AA, DeCecco LM. Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry. 2001;62(suppl 16):5–9. [PubMed] [Google Scholar]
- Akiskal HS, Bourgeois ML, Angst J, et al. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. J Affect Disord. 2000;59(suppl 1):S5–S30. doi: 10.1016/s0165-0327(00)00203-2. [DOI] [PubMed] [Google Scholar]
- Berman RM, Narasimhan M, Charney DS. Treatment-refractory depression: definitions and characteristics. Depress Anxiety. 1997;5:154–164. doi: 10.1002/(sici)1520-6394(1997)5:4<154::aid-da2>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Mendels J. Lithium in the treatment of depression. Am J Psychiatry. 1976;133:373–378. doi: 10.1176/ajp.133.4.373. [DOI] [PubMed] [Google Scholar]
- Dunner DL, Patrick V, Fieve RR. Rapid cycling manic depressive patients. Compr Psychiatry. 1977;18:561–566. doi: 10.1016/s0010-440x(97)90006-7. [DOI] [PubMed] [Google Scholar]
- Henry C, Sorbara F, Lacoste J, et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001;62:249–255. doi: 10.4088/jcp.v62n0406. [DOI] [PubMed] [Google Scholar]
- Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549–550. doi: 10.1192/bjp.164.4.549. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Manic-Depressive Illness. Edinburgh, Scotland: ES Livingstone. 1921 [Google Scholar]
- Dunner DL, Gershon ES, Goodwin FK. Heritable factors in the severity of affective illness. Biol Psychiatry. 1976;11:31–42. [PubMed] [Google Scholar]
- Akiskal HS, Mallya G. Criteria for the “soft” bipolar spectrum: treatment implications. Psychopharmacol Bull. 1987;23:68–73. [PubMed] [Google Scholar]
- Angst J, Merikangas K. The depressive spectrum: diagnostic classification and course. J Affect Disord. 1997;45:31–39. doi: 10.1016/s0165-0327(97)00057-8. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Jamison K. Manic-Depressive Illness. New York, NY: Oxford University Press. 1990 [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association. 1994 [Google Scholar]
- Cassano GB, Dell'Osso L, Frank E, et al. The bipolar spectrum: a clinical reality in search of diagnostic criteria and an assessment methodology. J Affect Disord. 1999;54:319–328. doi: 10.1016/s0165-0327(98)00158-x. [DOI] [PubMed] [Google Scholar]
- Regier DA, Boyd JH, Burke JD Jr, et al. One-month prevalence of mental disorders in the United States: based on five Epidemiologic Catchment Area sites. Arch Gen Psychiatry. 1988;45:977–986. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry. 1995;34:454–463. [PubMed] [Google Scholar]
- Angst J. The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. 1998;50:143–151. doi: 10.1016/s0165-0327(98)00142-6. [DOI] [PubMed] [Google Scholar]
- Allilaire JF, Hantouche EG, Sechter D, et al. Frequency and clinical aspects of bipolar II disorder in a French multicenter study: EPIDEP. Encéphale. 2001;27:149–158. [PubMed] [Google Scholar]
- Benazzi F. Prevalence of bipolar II disorder in outpatient depression: a 203-case study in private practice. J Affect Disord. 1997;43:163–166. doi: 10.1016/s0165-0327(96)01421-8. [DOI] [PubMed] [Google Scholar]
- Manning JS, Haykal RF, Connor PD, et al. On the nature of depressive and anxious states in a family practice setting: the high prevalence of bipolar II and related disorders in a cohort followed longitudinally. Compr Psychiatry. 1997;38:102–108. doi: 10.1016/s0010-440x(97)90089-4. [DOI] [PubMed] [Google Scholar]
- Manning JS, Zylstra RG, Connor PD. Teaching family physicians about mood disorders: a procedure suite for behavioral medicine. Primary Care Companion J Clin Psychiatry. 1999;1:18–23. doi: 10.4088/pcc.v01n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Rae DS, et al. The de facto US mental and addictive disorders service system: epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Hennen J, et al. Latency and episodes before treatment: response to lithium maintenance in bipolar I and II disorders. Bipolar Disord. 1999;1:91–97. doi: 10.1034/j.1399-5618.1999.010206.x. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Ko JY, Goodwin FK. “Cade's disease” and beyond: misdiagnosis, antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47:125–134. doi: 10.1177/070674370204700202. [DOI] [PubMed] [Google Scholar]
- Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52:51–55. doi: 10.1176/appi.ps.52.1.51. [DOI] [PubMed] [Google Scholar]
- Lish JD, Dime-Meenan S, Whybrow PC, et al. The National Depressive and Manic Depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–294. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL. Psychiatric diagnosis: are clinicians still necessary? Compr Psychiatry. 1983;24:399–411. doi: 10.1016/0010-440x(83)90032-9. [DOI] [PubMed] [Google Scholar]
- Simpson SG, Folstein SE, Meyers DA, et al. Bipolar II: the most common bipolar phenotype? Am J Psychiatry. 1993;150:901–903. doi: 10.1176/ajp.150.6.901. [DOI] [PubMed] [Google Scholar]
- Dunner DL, Tay LK. Diagnostic reliability of the history of hypomania in bipolar II patients and patients with major depression. Compr Psychiatry. 1993;34:303–307. doi: 10.1016/0010-440x(93)90015-v. [DOI] [PubMed] [Google Scholar]
- Benazzi F. Is 4 days the minimum duration of hypomania in bipolar II disorder? Eur Arch Psychiatry Clin Neurosci. 2001;251:32–34. doi: 10.1007/s004060170065. [DOI] [PubMed] [Google Scholar]
- Wicki W, Angst J. The Zurich Study, X: hypomania in a 28- to 30-year-old cohort. Eur Arch Psychiatry Clin Neurosci. 1991 339–348. [DOI] [PubMed] [Google Scholar]
- Akiskal H, Maser D, Zeller PJ, et al. Switching from “unipolar” to bipolar II: an 11-year prospective study of clinical and temperamental predictors in 559 patients. Arch Gen Psychiatry. 1995;52:114–123. doi: 10.1001/archpsyc.1995.03950140032004. [DOI] [PubMed] [Google Scholar]
- Frances AJ, Kahn DA, Carpenter D, et al. The expert consensus guidelines for treating depression in bipolar disorder. J Clin Psychiatry. 1998;59(suppl 4):73–79. [PubMed] [Google Scholar]
- Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry. 2001;158:131–134. doi: 10.1176/appi.ajp.158.1.131. [DOI] [PubMed] [Google Scholar]
- Benazzi F. Prevalence of bipolar II disorder in atypical depression. Eur Arch Psychiatry Clin Neurosci. 1999;249:62–65. doi: 10.1007/s004060050067. [DOI] [PubMed] [Google Scholar]
- Kretschmer E. Physique and Character. New York, NY: Macmillan Publishing Co. 1936 [Google Scholar]
- Akiskal HS, Perugi G, Hantouche EG, and et al. The affective temperament scales of Memphis, Pisa, Paris, and San Diego: progress towards a self-rated auto-questionnaire version (TEMP-A). J Affect Disord. 2002 In press. [Google Scholar]
- Akiskal HS. The temperamental borders of affective disorders. Acta Psychiatr Scand Suppl. 1994;379:32–37. doi: 10.1111/j.1600-0447.1994.tb05815.x. [DOI] [PubMed] [Google Scholar]
- Lapalme M, Hodgins S, LaRoche C. Children of parents with bipolar disorder: a meta-analysis of risk for mental disorders. Can J Psychiatry. 1997;42:623–631. doi: 10.1177/070674379704200609. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Williams JB, Spitzer RL, et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873–1875. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- Peet M, Pratt JP. Lithium: current status in psychiatric disorders. Drugs. 1993;46:7–17. doi: 10.2165/00003495-199346010-00002. [DOI] [PubMed] [Google Scholar]
- Vieta E, Martinez-Aran A, Goikolea JM, et al. A randomized trial comparing paroxetine and venlafaxine in the treatment of bipolar depressed patients taking mood stabilizers. J Clin Psychiatry. 2002;63:508–512. doi: 10.4088/jcp.v63n0607. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR. Maintenance medical treatment. In: Goodwin FK, Jamison KR. Manic-Depressive Illness. New York, NY: Oxford University Press. 1990 665–724. [Google Scholar]
- De Leon OA. Antiepileptic drugs for the acute and maintenance treatment of bipolar disorder. Harv Rev Psychiatry. 2001;9:209–222. doi: 10.1093/hrp/9.5.209. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Calabrese JR, McElroy SL, and et al. for the Divalproex Maintenance Study Group. A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Arch Gen Psychiatry. 2000 57:481–489. [DOI] [PubMed] [Google Scholar]
- Baetz M, Bowen RC. Efficacy of divalproex sodium in patients with panic disorder and mood instability who have not responded to conventional therapy. Can J Psychiatry. 1998;43:73–77. doi: 10.1177/070674379804300109. [DOI] [PubMed] [Google Scholar]
- Keck PE Jr, Taylor VE, Tugrul KC, et al. Valproate treatment of panic disorder and lactate-induced panic attacks. Biol Psychiatry. 1993;33:542–546. doi: 10.1016/0006-3223(93)90010-b. [DOI] [PubMed] [Google Scholar]
- Keck PE Jr, McElroy SL, Tugrul KC, et al. Antiepileptic drugs for the treatment of panic disorder. Neuropsychobiology. 1993;27:150–153. doi: 10.1159/000118971. [DOI] [PubMed] [Google Scholar]
- Sonne SC, Brady KT. Substance abuse and bipolar comorbidity. Psychiatr Clin North Am. 1999;22:609–627. doi: 10.1016/s0193-953x(05)70098-8. [DOI] [PubMed] [Google Scholar]
- Young LT, Robb JC, Hasey GM, et al. Gabapentin as an adjunctive treatment in bipolar disorder. J Affect Disord. 1999;55:73–77. doi: 10.1016/s0165-0327(98)00192-x. [DOI] [PubMed] [Google Scholar]
- Cabras PL, Hardoy MJ, Hardoy MC, et al. Clinical experience with gabapentin in patients with bipolar or schizoaffective disorder: results of an open-label study. J Clin Psychiatry. 1999;60:245–248. doi: 10.4088/jcp.v60n0408. [DOI] [PubMed] [Google Scholar]
- Pande AC, Crockatt JG, Janney CA, and et al. for the Gabapentin Bipolar Disorder Study Group. Gabapentin in bipolar disorder: a placebo-controlled trial of adjunctive therapy. Bipolar Disord. 2000 2:249–255. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Bowden CL, Sachs GS, and et al. for the Lamictal 602 Study Group. A double-blind placebo controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. J Clin Psychiatry. 1999 60:79–88. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Suppes T, Bowden CL, and et al. for the Lamictal 614 Study Group. A double-blind, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry. 2000 61:841–850. [DOI] [PubMed] [Google Scholar]
- Manning JS, Haykal RF, Connor PD, and et al. Depressed women with cyclothymic temperament: sustained remission with lamotrigine. J Affect Disord. 2002 In press. [DOI] [PubMed] [Google Scholar]
- Tohen M, Sanger TM, McElroy SL, et al. Olanzapine versus placebo in the treatment of acute mania. Olanzapine HGEH Study Group. Am J Psychiatry. 1999;156:702–709. doi: 10.1176/ajp.156.5.702. [DOI] [PubMed] [Google Scholar]
- Tohen M, Jacobs TG, Grundy SL, and et al. for the Olanzapine HGGW Study Group. Efficacy of olanzapine in acute bipolar mania: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2000 57:841–849. [DOI] [PubMed] [Google Scholar]
- Tohen M, Baker RW, Altshuler L, and et al. Olanzapine versus divalproex for the treatment of acute mania. Presented at the 14th annual congress of the European College of Neuropsychopharmacology; Sept 9, 2001; Munich, Germany. [Google Scholar]
- Zajecka JM, Weisler R, Swann AC, and et al. Divalproex sodium vs olanzapine for the treatment of mania in bipolar disorder. Presented at the 39th annual meeting of the American College of Neuropsychopharmacology; Dec 10, 2000; San Juan, Puerto Rico. [Google Scholar]
- Kinon BJ, Basson BR, Gilmore JA, et al. Long-term olanzapine treatment: weight change and weight-related health factors in schizophrenia. J Clin Psychiatry. 2001;62:92–100. [PubMed] [Google Scholar]
- Basson B, Kinon BJ, Taylor C, et al. Factors influencing acute weight change in patients with schizophrenia treated with olanzapine, haloperidol or risperidone. J Clin Psychiatry. 2001;62:231–238. doi: 10.4088/jcp.v62n0404. [DOI] [PubMed] [Google Scholar]
- Tohen M, Risser R, Baker RW, and et al. Olanzapine in the treatment of bipolar depression. In: New Research Abstracts of the 155th Annual Meeting of the American Psychiatric Association; May 22, 2002; Philadelphia, Pa. Abstract NR489:132. [Google Scholar]
- Tohen M, Vieta E, Ketter T, and et al. Olanzapine and olanzapine-fluoxetine combination (OFC) in the treatment of bipolar depression. Presented at the 155th annual meeting of the American Psychiatric Association; May 18, 2002; Philadelphia, Pa. [Google Scholar]
- Tohen M, Chengappa KNR, Suppes T, and et al. Olanzapine combined with mood stabilizers in prevention of recurrence in bipolar disorder: an 18-month study. Presented at the 23rd annual meeting of the Congress of the Collegium Internationale Neuro-Psychopharmacologicum; June 25, 2002; Montreal, Canada. [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients With Bipolar Disorder [Revision] Am J Psychiatry. 2002;159(suppl 4):1–50. [PubMed] [Google Scholar]
- Tohen M, Chengappa KN, Suppes T, et al. Efficacy of olanzapine in combination with valproate or lithium in the treatment of mania in patients partially nonresponsive to valproate or lithium monotherapy. Arch Gen Psychiatry. 2002;59:62–69. doi: 10.1001/archpsyc.59.1.62. [DOI] [PubMed] [Google Scholar]
- Bunney WE Jr, Goodwin FK, Murphy DL, et al. The “switch process” in manic-depressive illness, 2: relationship to catecholamines, REM sleep, and drugs. Arch Gen Psychiatry. 1972;27:304–309. doi: 10.1001/archpsyc.1972.01750270014002. [DOI] [PubMed] [Google Scholar]
- Menchon JM, Gasto C, Vallejo J, et al. Rate and significance of hypomanic switches in unipolar melancholic depression. Eur Psychiatry. 1993;8:125–129. [Google Scholar]
- Altshuler LL, Post RM, Leverich GS, et al. Antidepressant-induced mania and cycle acceleration: a controversy revisited. Am J Psychiatry. 1995;152:1130–1138. doi: 10.1176/ajp.152.8.1130. [DOI] [PubMed] [Google Scholar]
- Post RM, Denicoff KD, Leverich GS, et al. Drug-induced switching in bipolar disorder. CNS Drugs. 1997;8:352–365. [Google Scholar]
- Benazzi F. Antidepressant-associated hypomania in outpatient depression: a 203-case study in private practice. J Affect Disord. 1997;46:73–77. doi: 10.1016/s0165-0327(97)00082-7. [DOI] [PubMed] [Google Scholar]