Abstract
Objective:
We sought to compare the experience of 2 different surgical units in the treatment of hepatocellular carcinoma (HCC) on cirrhosis with resection or percutaneous radiofrequency ablation (RFA), respectively.
Summary Background Data:
When allowed by the hepatic functional reserve, surgery is the therapy for HCC on cirrhosis; alternative treatments are proposed because of the high tumor recurrence rate after resection. RFA is being widely adopted to treat HCC.
Methods:
Over a 4-year period, 79 cirrhotics with HCC underwent resection in 1 surgical unit (group A) and another 79 had RFA at a different unit (group B). Patient selection, operative mortality, hospital stay, and 1- and 3-year overall and disease-free survival were analyzed.
Results:
Group A (surgery): mean follow-up was 28.9 ± 17.9 months; operative mortality was 3.8%, mean hospital stay 9 days; 1- and 3-year survival were, respectively, 83 and 65%. One- and 3-year disease-free survival were 79 and 50%. Group B (RFA): mean follow-up was 15.6 ± 11.7 months. Mean hospital stay was 1 day (range 1–8). One- and 3-year survival were 78 and 33%; 1- and 3-year disease-free survival were 60 and 20%. Overall and disease-free survival were significantly higher in group A (P = 0.002 and 0.001). The advantage of surgery was more evident for Child-Pugh class A patients and for single tumors of more than 3 cm in diameter. Results were similar in 2 groups for Child-Pugh class B patients
Conclusions:
RFA has still to be confirmed as an alternative to surgery for potentially-resectable HCCs.
We sought to compare percutaneous radiofrequency ablation to surgery in the treatment of hepatocellular carcinoma on cirrhosis, the series of 2 different units were retrospectively analyzed. During the same 4-year period, 79 patients were resected in one unit and 79 ablated in the other. Surgery offered better results.
Hepatocellular carcinoma (HCC) is the most frequent primary hepatic malignancy and is closely linked to chronic liver disease.1 The association between HCC and hepatitis B (HBV) or C (HCV) infection or alcoholism has been clearly demonstrated; surveillance programs of high-risk patients have been developed in many areas of the world where the prevalence of these diseases is high and have led to the early diagnosis of a great number of HCCs.2
The chronic liver disease that most often underlies the HCC can preclude surgical treatment of the malignancy which, on the other hand, is likely to recur even when radical resection is performed due to the persistence of the oncogenic agent.3,4 Transplantation has been shown to be an effective treatment of highly selected cases of HCC on cirrhosis, but it can only be offered to a limited number of patients because of the shortage of donors.5,6 The optimal treatment of HCC on cirrhosis is still under debate and is often guided by the availability of one technique and the relative expertise of the staff at the individual centers.
Percutaneous ethanol injection (PEI) was reported to be as effective as surgery for small single lesions7,8 in some reports, although the largest retrospective analysis available did not support this finding.9 Radiofrequency ablation (RFA) was recently reported to be more effective than PEI in achieving complete tumor necrosis in a single session of treatment and has become the ablative technique of choice in many institutions.10 However, no study has focused on the comparison between the results of surgery and RFA.
The purpose of the present study is to compare the results of different policies adopted by 2 different surgical units in the same period with HCCs undergoing resection in one unit and RFA in the other.
PATIENTS AND METHODS
Group A: Resection
From January 1, 1998, to December 31, 2002, 79 consecutive patients with HCC on cirrhosis (57 males, 22 females; average age: 65; range: 43–81) underwent hepatic resection at the Department of Surgery and Transplantation of the University of Bologna: The etiology of the underlying liver disease was as follows: chronic hepatitis 67 (hepatitis B: 16; hepatitis C: 47; hepatitis B+C: 4), alcoholic liver disease 7, and cryptogenic 5. Seventy of these patients had a Child A and 9 a Child B liver disease, according to the Child-Pugh scoring system.11 The characteristics of the tumors are reported in Table 1.
TABLE 1. Patients and Tumor Characteristics in the 2 Different Treatment Groups
Resection was considered the treatment of choice of HCC for patients with a Child A chronic liver disease; it was also considered in highly selected cases of Child B patients with small tumors in whom transplantation was not possible due to their advanced age (over 65).
To make data comparable to the radiofrequency group, tumor staging was defined based on the preoperative assessment with imaging techniques; however, pathology on surgical specimens confirmed the diagnosis in all cases.
All resections were considered radical (tumor-free resection margins confirmed by pathology); in detail, 18 wedge, 35 segmentectomies, 9 bisegmentectomies 17 major resections (3 or more hepatic segments resected) were performed.
Group B: Percutaneous Radiofrequency Ablation
In the same period (January 1, 1998, to December 31, 2002) 79 consecutive patients with HCC on cirrhosis (67 males, 12 females; average age: 68; range: 41–88) underwent percutaneous radiofrequency ablation at the Department of Surgery of the University of Verona. The etiology of the underlying liver disease was as follows: chronic hepatitis 56 (hepatitis B: 10; hepatitis C: 43; hepatitis B+C: 3), alcoholic liver disease 21, and cryptogenic 2. Of these patients 43 had a Child A and 36 a Child B liver disease, according to the Child-Pugh scoring system.11
Diagnosis of HCC was based on the finding of a focal lesion greater than 2 cm in diameter with signs of arterial hypervascularization on 2 different imaging technique (computed tomography [CT], magnetic resonance imaging, and Doppler ultrasonography) or on the combination of imaging findings and elevation of alpha-fetoprotein level greater than 400 ng/mL; in 20 cases where the diagnosis was considered uncertain, fine-needle biopsy was performed to obtain histologic confirmation. The characteristics of the tumors are reported in Table 1.
Radiofrequency was considered the treatment of choice for patients with Child-Pugh B chronic liver disease or with multinodular tumors; RFA was also indicated for a small number of Child A patients with a single nodule potentially resectable. In detail, of 43 patients with Child A underlying liver disease, 23 had a single nodule of a mean diameter of 4 cm (range 1,5 to 7,5) involving 1 hepatic segment, 16 had 2 nodules that were located in the same segment in 1 case, in adjacent segments in 7 cases and in distant segments in 8, 3 had 3 nodules (2 in adjacent 1 in distant segments), and 1 had 4 nodules. Lesions adjacent to major intrahepatic vessels were not considered suitable for radiofrequency. All the patients in this group had no general contraindication to surgery.
Patients were treated with a radiofrequency generator (RITA Medical System model 500 and 1500; Mountain View, CA) with maximum power output of 50–150 Watts. Energy was delivered through a 15-gauge expandable electrode needle. The active part of the probe consisted of 4 to 9 curved hooks that could be deployed from the needle tip. Each prong was equipped with a thermocouple for real-time temperature monitoring during treatment. Tissue impedance was monitored by circuitry incorporated in the generator. Treatment was performed with the percutaneous approach under real-time ultrasonographic guidance.
All patients were treated in the operating room under general anesthesia. After placement of the probe in the tumor, hooks were deployed and the generator was set to reach an average temperature of the hooks of 100°C. Treatment consisted of one or more ablations lasting 12–20 minutes.
Blood count and liver function tests were performed 12 and 24 hours after RFA. All patients were discharged after 1 day, unless complications necessitated longer hospitalization. The efficacy of the treatment was assessed with 2 consecutive spiral CT scans performed after 1 month and after 3 months showing the absence of pathologic enhancement within or at the edge of the treated HCC. Incomplete necrosis or local recurrences detected during follow-up were retreated with RFA.
In group A patients were followed with liver ultrasonogram and serum alpha-fetoprotein measurement every 3 months in the first year after the treatment and subsequently every 6 months; each focal lesion detected at ultrasonogram was additionally assessed with spiral CT scan and considered as a recurrent tumor if the results of the 2 investigations coincided. In group B patients were followed with CT scan and serum alpha-fetoprotein measurement every 3 months in the first year after the treatment and subsequently every 6 months. No patient in either group had neoadjuvant or adjuvant treatment before or after the main procedure.
Statistical Analysis
Categorical variables were compared with the χ2 test and continuous variables were compared with the Student t test; P < 0.05 was considered statistically significant. Overall survival was computed from the day of surgery or radiofrequency ablation to the day of death or to the most recent follow-up visit. Disease-free survival was computed from the day of surgery or radiofrequency ablation to the first follow-up visit at which evidence of a tumor was clear or the most recent follow-up visit, death without recurrence ended the observation. Survival rates were calculated by the Kaplan-Meier method, and differences between the groups were assessed with the log-rank test, P < 0.05 was considered statistically significant.
RESULTS
Group A: Resection
Operative mortality (within 30 days of surgery) for those patients who underwent resection was 3.8%; mean hospital stay was 9 days (range 2–72). One- and 3-year survival were respectively 83% and 65%, with 1- and 3-year disease-free survival of 79% and 50%.
Group B: Percutaneous Radiofrequency Ablation
There was no in-hospital mortality after percutaneous radiofrequency ablation; mean hospital stay was 1 day (range 1–8). One- and 3-year survival were, respectively, 78% and 33%, with 1- and 3-year disease-free survival of 60% and 20%.
The mean number of RFA treatments for each patient was 1.4 (range 1–4). Forty of 46 (87%) patients with a single nodule were considered successfully treated (100% necrosis confirmed by imaging); complete necrosis was achieved in 100% of nodules equal to or less than 3 cm in diameter, in 84% of nodules between 3 and 5 cm and in 71% of nodules equal to or over 5 cm. Tumor recurred in 38 patients (48.1%): recurrence developed at the site of the treated tumor in 12 and at a different intrahepatic site in 26 of these patients.
Comparison Between the Two Groups
Mean follow-up was 28.9 ± 17.9 months for resected patients and 15.6 ± 11.7 months for patients treated with RFA. The overall and disease-free survival were significantly higher for those patients treated with resection (P = 0.002 and 0.001) (Fig. 1); further analysis showed that Child A patients survived longer when treated with surgery (P = 0.02; Tables 2 and 3) (Fig. 2). Surgery was more effective in terms of survival for those patients with a main lesion of more than 3 cm in diameter (P = 0.007 for overall and = 0.003 for disease-free survival): when this last category of patients is considered in detail the survival was higher in group A for those patients with a single tumor and a Child A underlying liver disease. Survival of patients with a main lesion of 3 or less centimeters in diameter was higher in the resection group in comparison to the RFA one (overall 3-year survival 79% versus 50%; 3-year disease-free survival 67% versus 34%), although statistical significance was not reached probably because of the small size of the sample. Single tumors equal to or less than 3 cm in diameter had a similar overall survival in the 2 groups; however, disease-free survival of this category of patients was remarkably higher in the resection group. Survival of patients with a Child B chronic liver disease was similar in the 2 treatment groups (Table 2 and 3).
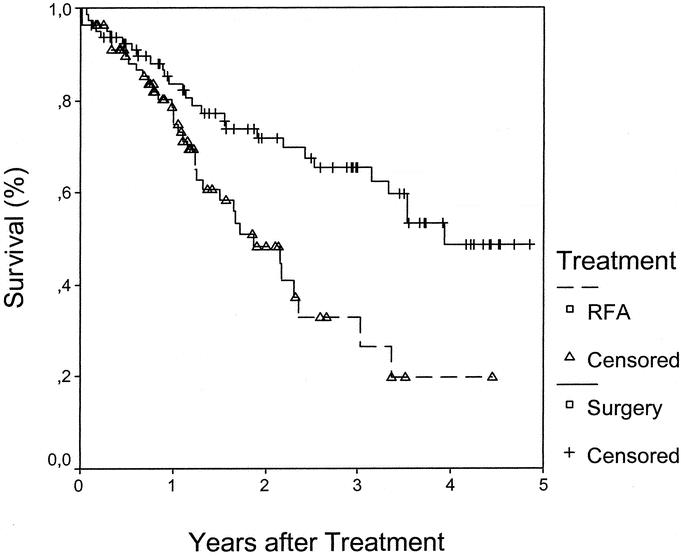
FIGURE 1. overall survival of all patients in the 2 treatment groups: survival was significantly higher in the resection group (P = 0.002). RFA: radiofrequency ablation.
TABLE 2. Overall Survival by Patient and Tumor Characteristics in the 2 Different Treatment Group
TABLE 3. Disease-Free Survival by Tumor Characteristics in the 2 Different Treatment Groups
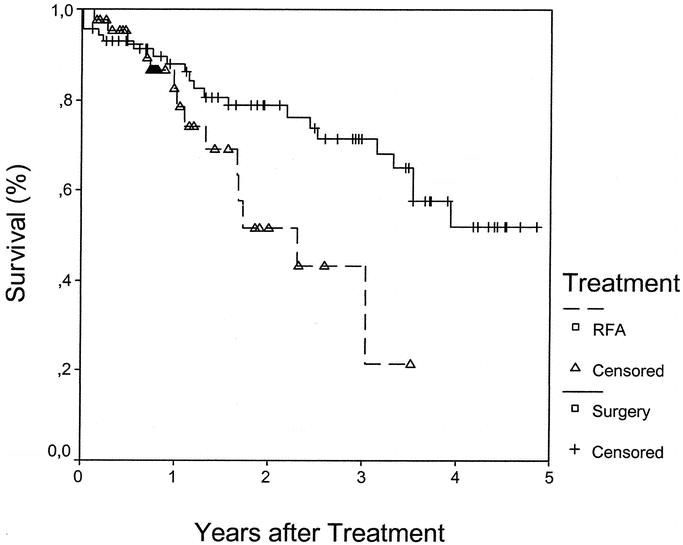
FIGURE 2. overall survival of all Child A patients in the 2 treatment groups: survival was significantly higher in the resection group (P = 0.02). RFA: radiofrequency ablation.
DISCUSSION
The treatment of hepatocellular carcinoma in patients with chronic liver disease is a major challenge. With the intention of avoiding the risk of hepatic failure that can follow hepatic resection in such patients, percutaneous ablative treatments have been proposed, of which radiofrequency ablation is progressively gaining consensus due to the efficacy, tolerability and low-risk of the procedure.10
Although there is a certain agreement about avoiding surgery in patients with more advanced chronic liver disease, which treatment has to be offered to patients with a relatively preserved liver function is still a matter for debate.12 Surgery has been shown to achieve good long-term results in terms of overall and disease-free survival; however even in the most experienced hands, an operative mortality ranging from 1.6 to 10% can be expected.13 Radiofrequency is much less invasive, involves a short hospital stay, and an extremely low mortality associated with the procedure; however, long-term results are difficult to ascertain as the majority of the reports focus on the evaluation of the percentage of success in terms of tumor necrosis and few data are available on the overall and disease-free survival of the patients.14–18
In the present study, 2 different surgical units employed surgery and RFA respectively to treat HCC over a 4-year period; as a result of different selection criteria it was possible to retrospectively identify subgroups of patients with similar characteristics and compare their outcome.
Although there were differences in the 2 patient populations, namely a higher number of Child B patients and more advanced tumors in the RFA group that may have influenced the results, overall survival was higher in the resection group.
With regard to the tumor dimension, in the presents study, overall and disease-free survival of patients with tumor greater than 3 cm was significantly higher in the resection group (P = 0.007 and 0.003, respectively). Three-year overall and disease-free survival were clearly in favor of surgery (79% versus 50% and 67% versus 34%, respectively) also for patients with a main lesion of 3 or less centimeters in diameter; however this difference was not significant at the statistical analysis, probably due to the small number of patients in this subgroup.
When considering Child A patients, an evident benefit of surgical treatment in the 3-year results was observed in each of the subgroups analyzed in this study, while the results of surgery and RFA were similar for patients with Child B disease. The higher efficacy of surgery was particularly remarkable for Child A patients with tumors greater than 3 cm: overall 3-year survival was 66% after surgery versus 37% in the RFA group (P = 0.004) and 3-year disease-free survival 44 versus 19% (P = 0.001).
These findings do not support the conclusions drawn in previous reports on percutaneous RFA and confirm that surgery should be the treatment of choice for HCC on compensated cirrhosis. To our knowledge similar evidence had never been so clearly demonstrated in the past: Livraghi and colleagues showed a high percentage of complete necrosis after RFA of tumor nodules, even when tumor diameter was greater than 3 cm; however, it was hard to translate this observation into a clinically useful prognostic judgment as once again no mention of the follow-up of the patients was made.13,14
Surgical resection is the established therapy for hepatocellular carcinoma whenever functional hepatic reserve allows it;19–21 however in the cirrhotic patient, especially when the chronic liver disease is caused by viral hepatitis, the high recurrence rate of the tumor caused by the persistence of the causative agent can justify the search of alternative options. Nevertheless, any nonsurgical treatment proposed for patients eligible for resection has to be evaluated very carefully, preferably in the context of a multidisciplinary approach where the surgeon is involved in the clinical decision and as part of prospective controlled trials. Clear evidence is still needed to propose RFA as an alternative to surgery for resectable HCCs on cirrhosis.
Footnotes
Reprints: Dr Marco Vivarelli, Dipartimento di Discipline Chirurgiche, Rianimatorie e dei Trapianti, Chirurgia II, Policlinico S. Orsola, Via Massarenti, 9, 40138 Bologna, Italy. E-mail: vivarelli@orsola-malpighi.med.unibo.it.
REFERENCES
- 1.Martin P. Hepatocellular carcinoma: risk factors and natural history. Liver Transpl Surg. 1998;4(Suppl 1):87–91. [PubMed] [Google Scholar]
- 2.Bolondi L, Sofia S, Siringo S, et al. Surveillance programme of cirrhotic patients for early diagnosis and treatment of hepatocellular carcinoma: a cost effectiveness analysis. Gut. 2001;48:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamamoto J, Kosuge T, Takyama T, et al. Recurrence of hepatocellular carcinoma after surgery. Br J Surg. 1996;83:1219–1222. [PubMed] [Google Scholar]
- 4.Poon R T-P, Fan S-T, Lo C-M, et al. Intrahepatic recurrence after curative resection of hepatocellular carcinoma. Long-term results of treatment and prognostic factors. Ann Surg. 1999;229:216–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wall JW, Marotta PJ. Surgery and transplantation for hepatocellular carcinoma. Liver Transpl. 2000;6:S16–S22. [DOI] [PubMed] [Google Scholar]
- 6.Vivarelli M, Bellusci R, Cucchetti A, et al. Low recurrence rate of hepatocellular carcinoma after liver transplantation: better patient selection or lower immunosuppression? Transplantation. 2002;74:1746–1751. [DOI] [PubMed] [Google Scholar]
- 7.Fried MW. Treatment of hepatocellular carcinoma: medical options. Liver Transpl Surg. 1998;4:S92–S97. [PubMed] [Google Scholar]
- 8.Yamamoto J, Okada S, Shimada K, et al. Treatment strategy for small hepatocellular carcinoma: comparison of long-term results after percutaneous ethanol injection therapy and surgical resection. Hepatology. 2001;34:707–713. [DOI] [PubMed] [Google Scholar]
- 9.Arii S, Yamaoka Y, Futagawa S, et al. Results of surgical and nonsurgical treatment for small-sized hepatocellular carcinomas: a retrospective and nationwide survey in Japan. Hepatology. 2000;32:1224–1229. [DOI] [PubMed] [Google Scholar]
- 10.Befler AS, Di Bisceglie AM. Hepatocellular carcinoma: diagnosis and treatment. Gastroenterology. 2002;122:1609–1619. [DOI] [PubMed] [Google Scholar]
- 11.Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. [DOI] [PubMed] [Google Scholar]
- 12.Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. J Hepatol. 2001;35:421–430. [DOI] [PubMed] [Google Scholar]
- 13.Choti MA. Surgical management of hepatocellular carcinoma: resection and ablation. J Vasc Interv Radiol. 2002;13:S197–S203. [DOI] [PubMed] [Google Scholar]
- 14.Livraghi T, Goldberg SN, Lazzaroni S, et al. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999;210:655–661. [DOI] [PubMed] [Google Scholar]
- 15.Livraghi T, Goldberg SN, Lazzaroni S, et al. Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology. 2000;214:761–768. [DOI] [PubMed] [Google Scholar]
- 16.Bonny C, Abergel A, Gayard P, et al. Radiofrequency ablation of hepatocellular carcinoma in patients with cirrhosis. Gastroenterol Clin Biol. 2002;2002:735–741. [PubMed] [Google Scholar]
- 17.Jiang H-C, Liu L-X, Piao D-X, et al. Clinical short-term results of radiofrequency ablation in liver cancers. World J Gastroenterol. 2002;8:624–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Curley SA, Izzo F, Ellis LM, et al. Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg. 2000;232:381–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johson PJ. Hepatocellular carcinoma: is currently therapy really altering outcome? Gut. 2002;51:459–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bruix J, Llovet JM. Prognostic prediction and treatment strategies in hepatocellular carcinoma. Hepatology. 2002;35:519–524. [DOI] [PubMed] [Google Scholar]
- 21.Grazi GL, Ercolani G, Pierangeli F, et al. Improved results of liver resection for hepatocellular carcinoma on cirrhosis give the procedure added value. Ann Surg. 2001;234:71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]





