Abstract
Objectives
To estimate a national disenrollment rate among children in Medicaid and the Children's Health Insurance Program (CHIP); to determine what share of disenrollment is due to acquiring other insurance or losing eligibility; and to examine what demographic and policy factors make disenrollment more likely.
Data Sources
Insurance status, income, and demographics from the Current Population Survey (CPS) March Supplement (1998–2001); eligibility data from the National Governors Association; and policy data from the former Health Care Financing Administration (HCFA), state welfare offices, and previous research.
Study Design
The study used a nationally representative sample of 5,551 children in Medicaid or CHIP. The key outcomes were the percentage of children still enrolled 1 year later, and the share of disenrollees who became uninsured despite remaining eligible. Multivariate logistic regression was used to explore demographics and policies predictive of disenrollment.
Data Collection and Analysis
CPS data were extracted using the Census Bureau's Federal Electronic Research and Review Extraction Tool 1.0. Data analysis was performed using Stata 7 (Stata Corporation 2001).
Principal Findings
Of the children enrolled in Medicaid or CHIP, 27.7 percent were no longer enrolled 12 months later. Of those, 45.4 percent dropped out despite apparently remaining eligible and having no other insurance—corresponding to 3.0 million children annually. Drop-out varied significantly across states. Children without siblings in public insurance were at a higher risk for drop-out. Children with more educated parents were more likely to leave Medicaid for private insurance or to lose Medicaid eligibility, while black children and infants were less likely to lose their eligibility. Decreased Medicaid provider reimbursement rates were strongly associated with drop-out, while Medicaid managed care increased the exodus to private insurance.
Conclusions
Drop-out from Medicaid and CHIP is a significant policy concern and helps explain the persistence of uninsurance among millions of eligible children. Clinical encounters with providers appear to play a key role in preventing drop-out.
Keywords: Medicaid, CHIP, uninsured, retention, disenrollment
This paper examines the enrollee retention of Medicaid and the Children's Health Insurance Program (CHIP) in an attempt to determine the extent to which drop-out is a problem for the programs, and what demographic and policy factors make disenrollment more likely.
Children without health insurance are more likely to go without needed care in times of illness and are less likely to receive preventive treatment (Newacheck et al. 1998). Some parents may fail to maintain their children's coverage because they expect to re-enroll in case of an emergency, but children with discontinuous coverage are 50 percent more likely to lack a regular source of care (Kogan et al. 1995), a factor associated with a tenfold increased risk of hospitalization for preventable health problems (Shi et al. 1999). Loss of insurance leads to lower rates of check-ups, vaccination, and follow-up care (Burstin et al. 1998), and total Medicaid costs per month go up as coverage becomes more sporadic (Ku and Ross 2002). Clearly, if many children are leaving Medicaid or CHIP and becoming uninsured, it would pose a significant public health and policy problem.
The current political climate adds to the significance of this issue. At both the state and federal level, expanded eligibility for Medicaid and CHIP has become a key tool in the incremental approach to covering the roughly 45 million Americans without health insurance. If Medicaid and CHIP struggle to keep current enrollees from dropping out despite continuing eligibility and lack of other insurance, then expansions without improved retention may not significantly decrease the ranks of the uninsured. Furthermore, since 2001, fiscal difficulties have forced states to look for ways to trim their Medicaid and CHIP budgets. While some states have simply cut beneficiaries off the rolls, many have used budget-saving changes that aim to maintain coverage for needy enrollees (KFF 2003a). In 2002–2003, 37 states froze or reduced reimbursement rates to providers (KFF 2003a). Other cost-saving measures include making the re-enrollment process more stringent (AHL 2002b), and switching to managed care, particularly for prescription drugs (AHL 2002a). Despite the appearance of trimming costs without increasing the number of uninsured, such changes may significantly exacerbate disenrollment.
Enrollee retention has typically been a secondary or even tertiary concern in research on public insurance, after crowd-out and low take-up rates. However, several recent studies of CHIP have found a high turnover, ranging from 18 percent to 48 percent annually (Rosenbach et al. 2001; Shenkman et al. 2002). Medicaid studies provide estimates ranging from 20 percent to 33 percent, but these figures may no longer be applicable since they used data that preceded welfare reform (Ellwood and Lewis 1999; Ku and Ross 2002). One post-reform analysis estimates that 18 percent of low-income uninsured children had been enrolled in Medicaid or CHIP during the previous year but were not enrolled by the time of the survey (Kenney and Haley 2001). But, critically, previous research has failed to distinguish between three different causes of disenrollment, each with unique policy and public health implications: (1) acquisition of new insurance; (2) loss of eligibility; and (3) drop-out from the program despite continuing eligibility and no other form of insurance. Each outcome must be considered separately in order to make appropriate policy in this realm.
What leads to disenrollment? An eight-state study of CHIP reveals that, in some states, up to 24 percent of applications for continuing enrollment were denied due to incorrect paperwork, and up to 40 percent of individuals never reapplied at all (Hill and Lutzky 2003). Surveys of the parents of CHIP disenrollees indicate that roughly 25 percent consciously decided to disenroll, while the remainder indicated that they had forgotten to reenroll or did not understand the process (Perry et al. 2001). In terms of predictors of disenrollment, the literature is sparse. Two studies found that older children disenroll at higher rates (Miller and Phillips 2002; Shenkman et al. 2002), while inconsistent results have been found on race and disenrollment (Miller and Phillips 2002; Shenkman et al. 2002; Shulman 2003). At a policy level, passive re-enrollment—which presumes that enrollees remain eligible, unless they report otherwise—and the county-wide density of providers who accept CHIP patients were both strongly associated with lower disenrollment (Dick et al. 2002; Miller and Phillips 2002).
Overall, the existing literature offers several insights into the issue of public insurance disenrollment, but leaves much unanswered. Previous analyses have typically studied fewer than a dozen states at a time—often only one state per study—and thus were unable to capitalize on the state-level variation in Medicaid and CHIP policies. Most of these studies have focused on CHIP, despite the fact that it is by far the smaller program. Most importantly, previous research did not distinguish between the three different types of disenrollment discussed earlier. Thus, in addition to offering a national post-welfare reform estimate of Medicaid/CHIP childhood disenrollment, this paper explores two key policy questions that remain unanswered: first, how many of the children who leave Medicaid or CHIP become uninsured despite remaining eligible for public coverage? Second, what policies and demographic indicators affect disenrollment and could shape future attempts to improve Medicaid and CHIP retention?
CONCEPTUAL FRAMEWORK FOR DISENROLLMENT
Let us explore in more depth the three broad explanations for why a person may stop participating in Medicaid or CHIP: (1) loss of eligibility, (2) acquisition of other health insurance, and (3) the residual, which this paper refers to as “drop-out.” Note that the discussion and analysis that follow focus on Medicaid—this is because for the years in this study, CHIP enrollment was less than one-tenth of the Medicaid enrollment of children (Rosenbach et al. 2001).
Loss of Eligibility: Medicaid eligibility is determined at the state level, within broad federal guidelines. More specifically, as of 2003, the following children were required to be eligible under federal law: children under age six in households below 133 percent of the Federal Poverty Line (FPL); children 18 or younger in households below 100 percent FPL; families meeting the requirements of Section 1931 of the Social Security Act, corresponding to eligibility for the former Aid to Families with Dependent Children (AFDC); and Supplemental Security Income (SSI) recipients, who qualify based on disability status (CMS 2002). However, Medicaid eligibility varies across states, which have wide discretion in extending coverage above these thresholds. When an individual loses eligibility for Medicaid, it could be due to an increase in household income; a change in family status, such as the aging of a child or marriage disrupting welfare-linked eligibility; loss of disability status; or legislative cutbacks in eligibility. Regardless of the cause, these cases represent the expected result of the legislation that defines each state's eligibility, and therefore should not be considered failures in the Medicaid program per se. Whether the current eligibility guidelines in various states are societally optimal is a critical policy question, but I leave that debate for another day.
Acquisition of Other Health Insurance: A child may leave Medicaid after acquiring insurance from another source, such as through a parent's new employer. This should not be seen as a policy failure because these children do not become uninsured—and it is the lack of any insurance that is associated with the adverse health outcomes discussed earlier.
“Drop-Out”: The remaining disenrollment from Medicaid and CHIP comprises individuals who are still eligible for the programs, and who do not have any other form of insurance. Simply put, they drop out of public insurance and return to the realm of the needy and uninsured. Unlike the previous two categories, this outcome should be considered a policy failure: based on the legislative intent of eligibility standards these children should still be enrolled, but they are not, making them susceptible to the adverse health consequences of being uninsured.
Why would someone drop out of a free insurance program to become uninsured? Medicaid reenrollment, while financially free of cost, is not free from other kinds of costs. Enrollees must recertify their eligibility at least once a year to remain in the program, and for many reasons, enrollees' parents may not find the process worth their time or effort. Individuals will therefore remain in the program if their parents perceive that the marginal benefit of Medicaid coverage outweighs the direct and indirect costs of recertifying. The marginal nature of the benefit is key. Parents reasonably compare Medicaid coverage with the next best option, which may be private insurance, a hospital free-care plan, or uninsurance with its combination of out-of-pocket payments and charity care. Or, they may (in many cases correctly) believe that their children will be able to re-enroll in Medicaid in the future should an emergency strike.
As for the costs, typically there is no direct charge for recertification, although some households are required to pay a monthly premium for CHIP. But the indirect costs can be numerous, including but not limited to transportation, time lost from work, child care, paperwork costs, and postage. Furthermore, the entire process may be stressful and demanding of one's effort and attention, which can be considered psychological costs.
Thus, any factors that lead to a high total cost (direct, indirect, and psychological) of recertification or a low marginal benefit of Medicaid may contribute to drop-out. This basic tradeoff generates the following list of possible factors affecting drop-out:
Administrative Hassle—Both the frequency and complexity of re-enrolling in Medicaid are likely to be critical determinants of drop-out (Hill and Lutzky 2003). Requiring re-enrollment more than once a year or requiring a face-to-face interview (rather than phone or mail applications) would increase the total cost to families of re-enrollment. As of July 2000, roughly one-third of states employed at least one of these restrictive re-enrollment requirements (Ross and Cox 2000).
Access to Health Care Providers under Medicaid—Many providers refuse to treat Medicaid patients, since reimbursement is much lower than under Medicare or private insurance. If Medicaid does not provide enrollees with adequate access to a broad choice of physicians, the benefit of remaining in the program may not be large enough for some to justify re-enrolling, a hypothesis supported by a previous retention study (Miller and Phillips 2002).
Availability of Charity Care—States and regions vary significantly as to how easily uninsured patients can receive charity care. If enrollees know they can obtain at least some health care without insurance, the marginal benefit of Medicaid coverage is reduced.
Outreach—Outreach may make it easier to recertify (or simply to remember to recertify). Such efforts may be conducted by the state, managed care plans, or health care providers.
Medicaid Managed Care—Many states and some counties require Medicaid enrollees to join managed care organizations (MCOs), with roughly 60 percent enrolled nationally (KFF 2003b). This may change the perceived benefit of Medicaid coverage. In addition, MCO penetration could affect the ease of reenrollment, if plans send reminders or otherwise facilitate recertification to a different degree than traditional Medicaid. Given the heterogeneity of MCO's across the nation, some plans may produce lower drop-out and others higher drop-out.
Generosity of Benefits—Within federal guidelines, states can choose which services to cover. The marginal benefit of Medicaid coverage is directly related to these benefits.
Stigma—Receipt of welfare benefits is often associated with stigma that may reduce the attractiveness of Medicaid. This stigma may be social, bureaucratic, or self-generated.
Demographic Characteristics—Age, race, ethnicity, gender, education, number of siblings, and urban versus rural residency may all impact the benefit and/or cost of Medicaid re-enrollment.
DATA AND METHODS
The data on individual insurance status, household income, family size, demographics, and state and county of residence all come from the Current Population Survey (CPS) March Supplement from the years 1998–2001.1 These years were chosen for analysis since they were the first full years following welfare reform and the creation of CHIP in 1997. The study sample is comprised of all children 18 years or younger enrolled in Medicaid with no other reported form of insurance during the preceding 12 months. Note that this sample includes a small percentage of children who were actually enrolled in CHIP, not Medicaid. However, until 2001, there was no separate question regarding CHIP on the CPS, and CHIP was simply lumped in with Medicaid on insurance status items. As mentioned earlier, CHIP enrollment in this period was less than one-tenth of the Medicaid enrollment of children; thus, this analysis uses Medicaid data for state-level polices, with the exception of eligibility as discussed below.
The CPS is a nationally representative sample conducted by the U.S. Census Bureau, using a cycle of 4 months on, 8 months off, and 4 months on for its sample. Thus, in any single March Supplement, half the households are supposed to be surveyed the following March. Of course, there is some attrition, as households that move or otherwise fail to respond do not appear in the following year's data. In this study sample, these factors led to an attrition rate of 16 percent. In terms of possible bias, if anything, this attrition will likely lead to an underestimate of drop-out: families that move or otherwise lose contact with the survey are likely to have less stable circumstances than those who remain in the survey for both years, and would therefore be more likely to experience discontinuities in health care coverage (due to moving to a new state, losing contact with welfare agencies, etc.). Therefore, if this study detects a significant drop-out rate despite this attrition bias towards underestimation, it will provide strong evidence of a significant policy problem. Using household and personal identification numbers to link files across consecutive years, a sample was constructed of 2-year linked files for 5,551 children.2
State- and year-specific eligibility cut-offs are from the National Governors Association (1998,1999,2000,2001). Using CPS data on family income and the appropriate cutoff for the FPL for each family, the percentage of the FPL was calculated. For this study, children were considered eligible if they met eligibility standards for either CHIP or Medicaid, given their age and %FPL. Loss of Eligibility was defined as someone who was eligible in Year 1 but not in Year 2. A small share of the sample qualified in Year 1 despite a %FPL above the eligibility threshold. These are likely due to categorical forms of eligibility such as disability, as well as certain states' use of income deductions for costs such as child-care when calculating a family's eligibility. To avoid labeling categorical eligibles as having lost eligibility (since they appear ineligible in both years), only those going from “eligible” to “ineligible” were classified as losing eligibility.
State-level data come from several sources. A variable called Frequent Recertification was defined as 1 for children living in states in a year when recertification was required more than once annually, and 0 for children who were required to recertify once a year. Face-to-Face was defined as 1 for children living in states in a year when face-to-face interviews were required for reenrollment, and 0 otherwise. Both of these variables were obtained directly from the welfare offices in all 50 states and the District of Columbia, supplemented with data for the year 2000 from previous studies (Ross and Cox 2000; Broaddus et al. 2002).3 These two policies were chosen to measure the administrative hassle of reenrollment because they have been the subject of considerable attention in the move to streamline the process (Ross and Cox 2000), evident in the fact that 13 states changed at least one of these policies during the study period.
Statewide annual managed care enrollment in Medicaid was obtained from the former Health Care Financing Administration (HCFA 1998–2000). When available, annual county MCO penetration was obtained from the states' departments overseeing Medicaid managed care.4 Statewide Medicaid reimbursement rates were obtained from the American Academy of Pediatrics (1998/1999,2001). The representative rate used was “Preventive Medical Care Checkup, Established Patient aged 12–17.” Rates were adjusted for inflation—converted to real 1998 U.S. dollars—and statewide cost of living (American Federation of Teachers 1998; BLS 2003).
DESCRIPTIVE STATISTICS: HOW MUCH DISENROLLMENT AND WHY?
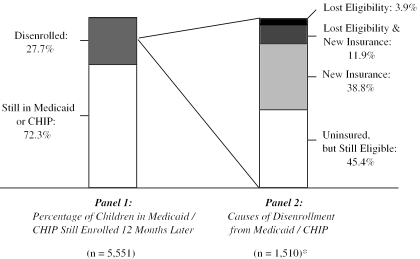
Figure 1 presents the descriptive statistics on disenrollment. Of the 5,551 children in the sample, who all reported being in Medicaid or CHIP in Year 1 of the survey, 27.7 percent were no longer in either program 12 months later. This figure is comparable to previous estimates in the literature. Why did these children disenroll? Figure 1 shows that, of those who left public coverage, 38.8 percent acquired other health insurance (almost all of which was private coverage), 3.9 percent became ineligible for CHIP and Medicaid, and 11.9 percent both acquired new insurance and became ineligible. The remaining 45.4 percent lost Medicaid and CHIP coverage despite remaining eligible and having no other insurance. Defining only this last group as “drop-out”—the result most troubling from a policy perspective—we are left with an annual 12.6 percent drop-out rate among children in public insurance programs (95 percent CI=11.1–14.0 percent). Given current Medicaid enrollment, this corresponds to 3.0 million children per year (KFF 2003b). These data reiterate previous findings that public insurance programs experience rapid turnover. But now we can conclude that this turnover is not simply due to lost eligibility or acquiring other insurance. The annual drop-out rate of one-in-eight indicates that retention is a critical factor in the ongoing presence of millions of uninsured American children who are indeed eligible for public coverage.
Figure 1.
Descriptive Statistics for Medicaid/CHIP Disenrollment (1998–2001)
*Note: Subsample size in Panel 2 does not equal the precise fraction of the sample in Panel 1, due to the use of the CPS survey weights to calculate these statistics.
States vary considerably in their drop-out rates, from less than 5 percent to just over 25 percent. A simple F-test confirms that the state means are significantly different [F(50, 5500)=4.24, p<.01]. Table 1 presents drop-out rates by state, for all states with n≥50.5 The wide variation underscores the risk of generalizing from disenrollment studies of individual states.
Table 1.
Annual Drop-Out Rate by State*
| Alabama | 19.5% (6.2%, n=73) | Missouri | ** |
| Alaska | ** | Montana | 10.5% (4.5%, n=59) |
| Arizona | 15.1% (4.l%, n=135) | Nebraska | 0.9% (1.0%, n=55) |
| Arkansas | ** | Nevada | ** |
| California | 16.6% (2.2%, n=875) | New Hampshire | 0.0% (0.0%, n=50) |
| Colorado | ** | New Jersey | 7.8% (3.3%, n=106) |
| Connecticut | ** | New Mexico | 10.6% (3.2%, n=141) |
| Delaware | 10.2% (5.4%, n=85) | New York | 9.9% (1.7%, n=607) |
| District of Columbia | 8.7% (3.9%, n=80) | North Carolina | 17.9% (6.2%, n=99) |
| North Dakota | ** | ||
| Florida | 13.9% (3.9%, n=190) | Ohio | 3.2% (2.0%, n=128) |
| Georgia | 7.0% (3.9%, n=106) | Oklahoma | ** |
| Hawaii | 5.5% (3.4%, n=66) | Oregon | 7.2% (3.3%, n=65) |
| Idaho | 18.0% (6.3%, n=71) | Pennsylvania | 7.0% (2.9%, n=189) |
| Illinois | 13.9% (3.9%, n=219) | Rhode Island | ** |
| Indiana | 25.5% (10.2%, n=50) | South Carolina | 9.3% (6.0%, n=50) |
| Iowa | ** | South Dakota | ** |
| Kansas | ** | Tennessee | 12.4% (4.8%, n=79) |
| Kentucky | ** | Texas | 24.4% (3.7%, n=389) |
| Louisiana | 20.9% (6.7%, n=85) | Utah | ** |
| Maine | ** | Vermont | 5.2% (3.7%, n=71) |
| Maryland | ** | Virginia | ** |
| Massachusetts | 3.5% (1.6%, n=180) | Washington | 2.0% (2.1%, n=57) |
| Michigan | 5.6% (3.0%, n=192) | West Virginia | 13.8% (5.0%, n=100) |
| Minnesota | 10.1% (5.3%, n=66) | Wisconsin | 8.4% (4.8%, n=50) |
| Mississippi | 13.4% (6.7%, n=67) | Wyoming | 6.5% (3.4%, n=61) |
| National average=12.6% (0.8%, n=5,551) | |||
Standard error of the mean and subsample size reported in parentheses.
States with n<50 were omitted, since the sample sizes were too small to reliably report subsample means.
RISK FACTORS FOR DISENROLLMENT
To explore predictors of disenrollment, multivariate logistic regression was used. Three regression equations were specified, corresponding to the three distinct kinds of disenrollment—drop-out, acquiring other insurance, and lost eligibility. For Equation 1, the dependent variable was Drop-out, which equaled 1 for children who were no longer in Medicaid at the end of the year, and 0 for those still in the program. The sample excludes those who gained new insurance or lost eligibility during the year, so it only contains those who should—using the policy framework presented in this paper—have stayed enrolled. This yields a regression sample of 4,113 children. The independent variables are county/state parameters, as defined in the methods section, and individual/household demographic traits, listed below. Equation (1) is specified:
| (1) |
The Y's and Z's are fixed effects for the state and year, respectively. The year fixed effects filter out any secular trend due to changes in the economy or trends in health care costs. The state fixed effects filter out any time-invariant individual state idiosyncrasies not captured by the parameters incorporated in the model, such as charity care availability, stigma, and reenrollment outreach. Importantly, this specification means that the μ coefficients on state-level policies will not be affected by cross-sectional between-state variation, but only the effects of longitudinal within-state changes. State-year fixed effects were not included, as the use of 150 additional variables would almost certainly overfit the data.
Equation (2) replaces “drop-out” with “acquiring new health insurance” as the dependent variable, and equation (3) replaces “drop-out” with “lost Medicaid/CHIP eligibility.” A child who both lost eligibility and acquired new insurance would thus have a “1” for the dependent variables in both equations (2) and (3). The right-hand side of the regressions was unchanged from equation (1). But unlike equation (1), the sample for these analyses included the full sample from the descriptive statistics—all children who were in Medicaid/CHIP in Year 1 of the survey.
State and County Factors Affecting Disenrollment
Table 2 displays the multivariate results.6 The upper half of the table summarizes the associations between disenrollment and Medicaid policies. Starting with equation (1), the only policy that was a statistically significant predictor of drop-out was the physician reimbursement rate. Increased reimbursement—and therefore wider access to care for enrollees, and more incentive for providers to keep patients enrolled—led to significantly less drop-out. The odds ratio (OR) indicates that a $1 increase in reimbursement (which represents a 2.4 percent increase from the median rate of $42.12) was associated with a 5.8 percent decrease in the drop-out rate.7 This reflects a highly elastic response, indicating that cutting reimbursement rates may save program funds but will do so at the expense of children who are much more likely to become uninsured.
Table 2.
Demographic and Policy Predictors of Disenrollment
| Variable | Equation 1: Drop-Out Odds Ratio† | Equation 2: New Insurance Odds Ratio† | Equation 3: Lost Eligibility Odds Ratio† |
|---|---|---|---|
| State and county parameters | |||
| MCO penetration | 1.007 (.007) | 1.008* (.004) | 1.002 (.007) |
| Reimbursement rate | 0.93*** (.03) | 0.99 (.02) | 0.99 (.02) |
| Frequent recertification | 1.14 (.57) | 1.23 (.47) | 0.60 (.31) |
| Face-to-face interview | 1.59 (.73) | 0.99 (.33) | 1.32 (.60) |
| Individual and household traits | |||
| Age | |||
| 0–1 | 1.37 (.30) | 1.05 (.19) | 0.58* (.18) |
| 2–5 | 0.97 (.15) | 1.05 (.13) | 1.06 (.19) |
| 6–12 | 0.99 (.12) | 1.01 (.11) | 1.16 (.18) |
| >12 | 1.00 (—) | 1.00 (—) | 1.00 (—) |
| Parents education | |||
| No high school diploma | 0.69 (.24) | 0.47*** (.11) | 0.41*** (.13) |
| HS graduate, no college | 0.90 (.31) | 0.61** (.14) | 0.69 (.20) |
| Some college | 0.94 (.34) | 1.00 (.23) | 0.84 (.25) |
| College graduate | 1.00 (—) | 1.00 (—) | 1.00 (—) |
| Race | |||
| Native American | 0.44 (.23) | 1.65 (.63) | 0.60 (.35) |
| Black | 1.09 (.23) | 0.88 (.13) | 0.51*** (.13) |
| Asian | 0.90 (.53) | 1.67 (.57) | 1.54 (.71) |
| White | 1.00 (—) | 1.00 (—) | 1.00 (—) |
| Other demographics | |||
| Male | 0.78*** (.08) | 1.01 (.08) | 1.12 (.14) |
| Urban | 0.94 (.20) | 1.09 (.18) | 1.09 (.24) |
| Latino household head | 1.28 (.29) | 0.85 (.14) | 0.77 (.20) |
| Sibling on Medicaid | 0.51*** (.07) | 0.61*** (.07) | 0.46*** (.07) |
| Sample size | n=4,113 | n=5,551 | n=5,496 |
Notes:Standard errors in parentheses.
p<.10,
p<.05,
p<.01.
Managed care penetration was not a significant predictor of drop-out. Meanwhile, the OR's for the two administrative hassle variables also did not differ significantly from 1.0, although both point estimates suggest that more restrictive recertification procedures are associated with higher drop-out, as we would expect. A longer study period with more within-state variation in these policies would be a more powerful test of these effects.
Turning to equation (2), high Medicaid managed care penetration was a significant predictor of acquiring other insurance (90 percent of which was private coverage). This effect could plausibly be due to two influences of high managed care penetration. First, families with the means to acquire other insurance may be more likely to do so when Medicaid requires them to join managed care plans. Second, areas with high Medicaid managed care penetration may also have high managed care penetration in the private sector; if this leads to cheaper premiums, we may simply be detecting that families are more likely to acquire other insurance if private coverage is cheaper in their geographical region. Lastly, equation (3) shows no significant policy predictors of lost eligibility—which is reassuring, since we would not expect any of these parameters to exert a direct effect on a given family's eligibility status.
Individual and Household Factors Affecting Disenrollment
Table 2 also presents the results for individual and household traits. The strongest predictor of drop-out was whether a child had a sibling in public insurance. Children with a sibling in Medicaid or CHIP were 39 percent less likely to drop out than those without siblings in either program.7 This makes sense given our conceptual framework: the total cost of re-enrollment for a given family is relatively fixed, regardless of the number of children being enrolled (assuming no premiums), while the marginal benefit of recertification should go up as the same reenrollment process leads to coverage for more children. Additionally, siblings in the program may lead to more frequent outreach attempts, either by the state or by providers.
Provider outreach may also explain the fact that boys appear to be significantly less likely to drop out—17.4 percent less likely—than girls.7 Epidemiological studies show that boys are more likely to be hospitalized than girls for injuries or asthma, two common pediatric morbidities (Chen et al. 2003; Spady et al. 2004). More generally, all-cause morbidity and health care utilization tend to be higher among boys than girls (Rajmil et al. 1999; Kaneko et al. 2000; Wells 2000). If the clinical encounter often serves as the means of reenrollment, then children who receive more frequent medical care will be more likely to stay enrolled.
Race and ethnicity were not significant predictors of drop-out, but African-American children were 45 percent less likely to lose eligibility than white children, a statistically significant result.7 These findings counter the results of a previous study of New Jersey's CHIP (Miller and Phillips 2002), but are in line with a Florida Medicaid study (Shulman 2003) that found higher disenrollment among whites than blacks. It appears that race is not affecting disenrollment via drop-out, but instead through differential income mobility. Similarly, parental education was not a significant predictor of drop-out, but children with more educated parents were significantly more likely to lose eligibility or acquire new health insurance. Children whose parents had not graduated from high school were 54 percent less likely to lose eligibility and 43 percent less likely to acquire other insurance than those whose parents were college graduates.7 As with race, these results probably reflect the relative income and job mobility of these different groups.
Age does not appear to be a significant predictor of drop-out. But, infants are significantly less likely to lose eligibility—38 percent less likely compared to older children.7 The protective effect of age likely results from the more generous eligibility standards for infants in many states. This result is in keeping with previous findings that CHIP disenrollment is higher among older children (Miller and Phillips 2002; Shenkman et al. 2002)—and suggests that this age-related disenrollment is largely due to lost eligibility, rather than drop-out.
DISCUSSION AND POLICY IMPLICATIONS
The descriptive statistics on disenrollment present two key findings. First, during the study period (1998–2001), Medicaid and CHIP were significantly affected by turnover, as 28 percent of children in the programs were no longer enrolled 12 months later. Second, much of this turnover was undesirable from a policy perspective, as 45 percent of children leaving the program did so despite having no other form of health insurance and remaining eligible. This means that 1 in 8 children in Medicaid and CHIP dropped out each year into the ranks of the uninsured, despite still being eligible. This translates into 3.0 million children annually, nearly one-third of all uninsured children in the U.S. in 2000 (KFF 2002). Clearly, Medicaid retention poses a critical policy problem. Drop-out rates varied significantly across states, indicating that there is ample room for improvement in much of the country. Although this study did not examine adults, these findings suggest that adult drop-out from Medicaid may also be a problem. As U.S. policymakers debate ways to extend coverage to the uninsured, the issue of drop-out must be addressed. Otherwise, Medicaid and CHIP will continue to be plagued by—in the words of Hill and Lutzky (2002)—“a hole in the bucket.” In the meantime, children who drop out will suffer more inconsistent care and worse health outcomes, and if some of them do eventually re-enroll, it will come at a greater cost than if they had remained steadily enrolled (Ku and Ross 2002).
Multivariate analysis highlights several groups that are more likely to leave the program, albeit for different reasons. Girls and children without any siblings in public insurance were significantly more likely to drop out and become uninsured, despite continuing eligibility. Meanwhile, non-black children, children with more educated parents, and older children were more likely to lose eligibility or acquire other health insurance.
At the state level, the findings present a strong word of caution to would-be budget cutters who hope to save money by cutting provider reimbursement rates. The evidence strongly suggests that this policy will increase the rate of children leaving Medicaid and CHIP to become uninsured. As for making the recertification process more intensive—either more frequent or requiring a face-to-face interview—the results were inconclusive, but suggest that these changes may exacerbate drop-out. While budget pressures may make these kinds of policies a necessity, they should not be undertaken with the misguided notion that they will not affect the extent of insurance coverage among disadvantaged populations.
On the other hand, the results indicate that one popular solution for improving retention does not address the core of the problem. The 12-month continuous eligibility rule, which keeps an individual enrolled for 1 year following initial enrollment regardless of changes in family status or income, has been adopted by over a dozen states (Ross and Cox 2000; Irvin et al. 2001). But this rule will not help the vast majority of Medicaid and CHIP drop-outs who are still eligible. As shown in Figure 1, only 4 percent of disenrollees became uninsured due to lost eligibility, while 45 percent became uninsured despite still being eligible simply by failing to recertify. In addition, continuous eligibility may also direct money to households that are no longer as needy as when they initially enrolled.
So what can be done? The unifying feature of several predictors of drop-out—other siblings in Medicaid, gender, and provider reimbursement—appears to be the frequency of clinical encounters, suggesting that providers are the key intermediaries in keeping children enrolled. Thus, a simple first step would be for states to commit to maintaining (or even raising) current physician reimbursement rates, and tie them to a reasonable cost-of-living index over time to prevent inflation from eroding their value.
A more comprehensive solution would be passive re-enrollment, under which children remain enrolled as long as their families do not report any changes in status. Passive re-enrollment would not keep children covered if their circumstances improve significantly, but it would prevent children in need from dropping out simply because their parents failed to recertify. Incidentally, it would also reduce administrative costs. This approach is not foreign to the current system, since most states already require families to update the welfare office during the year (even prior to their redetermination period) if their circumstances change. The proposed reform would simply make this approach the only method of eligibility redetermination. The major drawback of this policy—keeping some children enrolled who are no longer eligible—is far outweighed by the magnitude of the drop-out problem: again, 45 percent of disenrollees dropped out, but only 16 percent lost eligibility (most of whom ended up with private coverage anyway).
Of course, this study has several limitations. The CPS was used for this analysis because it offers a large nationally representative sample, is released in a timely manner that enables analysis of more recent years, and allows for state-by-state analysis to ascertain the effects of Medicaid policy variation. But it also has several disadvantages. First, the CPS for this period combines CHIP and Medicaid into one category, preventing analysis of the programs' differences. Second, the CPS enables only a 2-year longitudinal analysis; thus, it cannot provide information on the average duration of enrollment or how often drop-outs re-enrolled later on. These are important issues that future research using other data could explore.
Third, Medicaid eligibility is typically based on the previous month's income, so using annual income introduces measurement error. Imputed eligibility from annual income has been used in similar Medicaid analyses (Cutler and Gruber 1996) but may generate bias in estimating retention. If many children lost eligibility due to large changes in monthly income shortly before the survey, they may have falsely appeared eligible based on annual income. Income dynamics for this group, however, make it unlikely that this phenomenon could bias the drop-out estimate significantly.8 A similar phenomenon could have occurred with children who were eligible based on medical need or disability. Children who qualified due to medical status in Year 1 but not in Year 2, without any underlying change in imputed income eligibility, would be falsely labeled “drop-outs,” when they in fact had lost eligibility. But, again, this could not explain much of the estimated drop-out, since the vast majority of children in Medicaid qualify based on income, not disability (KFF 2003b). So, while the drop-out estimate may be upwardly biased by using annual income, there is still ample evidence that drop-out is a significant problem.
Lastly, the CPS is thought to undercount Medicaid enrollment, perhaps due to respondent confusion about the program or stigma (Lewis and Ellwood 1997). However, this should not bias the analysis, since the sample is restricted to children who reported Medicaid coverage in Year 1 (“reporters”). Any children whose parents failed to indicate that they were in Medicaid (“non-reporters”) are simply excluded from the study. There is no reason to think that reporters in Year 1 would become non-reporters in Year 2, so the analysis is unlikely to mistake non-reporting for drop-out. This exclusion will not bias the results, unless non-reporters have significantly different rates of Medicaid drop-out. If non-reporters differ from reporters—due to less of an understanding of Medicaid or greater sensitivity to stigma—they are probably even more likely to drop out. Thus, if the undercount does cause systematic bias, it likely produces an artificially low drop-out estimate. Concerns about undercount are also mitigated by the fact that this study's disenrollment estimate was in the same ballpark as previous estimates from other data.
In terms of the multivariate analysis, the primary limitation is that none of these relationships has been shown to be causal. Nonetheless, the strong associations between drop-out, provider reimbursement, and likely indicators of clinical contact suggest that there is much room for policy reforms to help maintain the coverage of the 47 million Americans in Medicaid, as well as expand coverage to the roughly 45 million Americans who currently have no health insurance at all.
Acknowledgments
This study was conducted while the author received funding from the National Science Foundation and the PASTEUR program at Harvard Medical School. Many thanks are due to Kathy Swartz, Joe Newhouse, and David Cutler for reading through drafts and offering helpful advice. Also, I am grateful for the advice and suggestions of Bob Blendon, Sheldon Danziger, Marilyn Ellwood, Melissa Wachterman, and three anonymous reviewers. Thanks are also due to Charles Nelson at the Census Bureau for answering technical questions about the CPS, and to countless information and policy officials at welfare offices across the country for providing data on enrollment procedures, eligibility, and managed care. Any remaining errors are, of course, solely my responsibility.
Footnotes
The 2001 CPS data are from the initial unexpanded file released on the FERRET system, which initially had incorrect weights. The corrected weights were downloaded after they were revised in December 2001. Insurance status was coded for according to CPS guidelines, and is available at http://www.census.gov/hhes/hlthins/hlthinsvar.html.
Matching only on household and personal ID numbers results in roughly 20 percent of files being clearly mismatched. Thus, any file indicating a change in age by more than two years or a change in sex was dropped from the sample.
Year of enactment of policy changes was assigned based on the closest March to the date of change.
County-level penetration was not available for all subjects, for two reasons: (1) The CPS only records respondents' county of residence for larger counties. (2) Not all states keep county-level MCO data. Overall, county MCO penetration was available for 40 percent of the sample (but for 86 percent of respondents living in CPS-labeled counties). Remaining values were derived as follows: For counties not listed in the CPS, a penetration rate for the non–CPS-listed counties was calculated when possible. For states without county MCO data, HCFA state averages were used.
Table 1 focuses specifically on “drop-out,” not disenrollment more generally.
Standard errors were adjusted for the non-independence of observations by clustering at the household level, and the regression used CPS household weights. Several smaller states perfectly predicted the dependent variables in Equations 1 and 3 (i.e., Drop-out=0 percent or Lost-Elig=0 percent), so observations from these states had to be dropped from the samples for the respective regressions (two states with n=60 from Equation 1; one state with n=55 from Equation 3). A regression without the fixed effects was run to check the effect of the dropped observations on the household and individual predictors; the significant coefficients were all unchanged from the results in Table 2.
All probabilities in this section are derived from OR's using the method of recycled predictions, in which the sample-wide average probability of drop-out is predicted using the regression coefficients, as the variable of interest takes on different values (Greene 2003, p. 668). For instance, the predicted baseline drop-out rate was 17.1 percent, and it fell to 16.1 percent with a sample-wide $1 reimbursement increase, equivalent to a relative decrease in drop-out of 5.8 percent.
Gottschalk (1997) reports that nearly 70 percent of Americans in the lowest quintile of earnings in 1974 were still in that quintile 12 months later, and Bradbury and Katz (2002) found that mobility in the 1990s was even less than in previous decades. Even if we use 70 percent of the estimate found in this study as a lower bound on drop-out versus lost eligibility, this still leaves 2.1 million children dropping out each year, despite remaining eligible and uninsured.
References
- American Academy of Pediatrics . Medicaid Reimbursement Survey. Elk Grove Village, IL: American Academy of Pediatrics; 1998/1999, 2001. [Google Scholar]
- American Federation of Teachers . Interstate Cost of Living Index. Washington, DC: American Federation of Teachers; 1998. [Google Scholar]
- American Health Line (AHL) 2002a. “Budget Deficits Force States to Reduce Health Services.” [Accessed on October 7, 2002 http://nationaljournal.com/pubs/healthline/
- American Health Line (AHL) 2002b. “Governor Races: AHL Rounds Up Results—Tennessee.” [Accessed on November 6, 2002 http://nationaljournal.com/pubs/healthline/
- Bradbury K, Katz J. “Women's Labor Market Involvement and Family Income Mobility When Marriages End.”. New England Economic Review. 2002;4Q:41–74. [Google Scholar]
- Broaddus M, Blaney S, Dude A, Guyer J, Ku L, Peterson J. Expanding Family Coverage: States' Medicaid Eligibility Policies for Working Families in the Year 2000. Washington, DC: Center on Budget and Policy Priorities; 2002. [Google Scholar]
- Bureau of Labor Statistics (BLS) 2003. “Consumer Price Indices” [accessed on July 20, 2003]. Available at http://www.bls.gov/cpi/
- Burstin HR, Swartz K, O'Neil AC, Orav EJ, Brennan TA. “The Effect of Change of Health Insurance on Access to Care.”. Inquiry. 1998;35(4):389–97. [PubMed] [Google Scholar]
- Centers for Medicaid and Medicare Services (CMS) 2002. “Medicaid Eligibility” [accessed on December 15, 2002]. Available at http://www.cms.hhs.gov/medicaid/eligibility/criteria.asp.
- Chen Y, Stewart P, Johansen H, McRae L, Taylor G. “Sex Differences in Hospitalization Due to Asthma in Relation to Age.”. Journal of Clinical Epidemiology. 2003;56(2):180–7. doi: 10.1016/s0895-4356(02)00593-0. [DOI] [PubMed] [Google Scholar]
- Cutler D, Gruber J. “Does Public Insurance Crowd Out Private Insurance?”. Quarterly Journal of Economics. 1996;111(2):391–430. [Google Scholar]
- Dick AW, Allison RA, Haber SG, Brach C, Shenkman E. “Consequences of States' Policies for SCHIP Disenrollment.”. Health Care Financing Review. 2002;23(3):65–88. [PMC free article] [PubMed] [Google Scholar]
- Ellwood M, Lewis K. On and Off Medicaid: Enrollment Patterns for California and Florida in 1995. Washington, DC: Urban Institute; 1999. [Google Scholar]
- Gottschalk P. “Inequality, Income Growth and Mobility: The Basic Facts.”. Journal of Economic Perspectives. 1997;11(2):21–40. [Google Scholar]
- Greene WH. Econometric Analysis. 5th ed. Upper Saddle River, NJ: Prentice-Hall; 2003. [Google Scholar]
- Health Care Financing Administration (HCFA) Medicaid Managed Care, State Enrollment. Washington, DC: Health Care Financing Administration; 1998–2000. [Google Scholar]
- Hill I, Lutzky AW. Is There a Hole in the Bucket? Understanding SCHIP Retention. Washington, DC: Urban Institute; 2003. [Google Scholar]
- Irvin C, Peikes D, Trenholm C, Khan N. Discontinuous Coverage in Medicaid and the Implications of 12-Month Continuous Coverage for Children. Cambridge, MA: Mathematica Policy Research; 2001. [Google Scholar]
- Kaiser Family Foundation (KFF) Children's Health: Why Health Insurance Matters. Menlo Park, CA: Kaiser Commission on Medicaid and the Uninsured; 2002. [Google Scholar]
- Kaiser Family Foundation (KFF) State Budget Constraints: The Impact on Medicaid. Menlo Park, CA: Kaiser Commission on Medicaid and the Uninsured; 2003a. [Google Scholar]
- Kaiser Family Foundation (KFF) The Medicaid Program at a Glance. Menlo Park, CA: Kaiser Commission on Medicaid and the Uninsured; 2003b. [Google Scholar]
- Kaneko K, Tokita A, Shimizu T, Yashamiro Y. “Gender and Disease in Japan.”. Acta Paediatrica. 2000;89:500. doi: 10.1080/080352500750028311. [DOI] [PubMed] [Google Scholar]
- Kenney G, Haley J. Why Aren't More Uninsured Children Enrolled in Medicaid or SCHIP? Washington, DC: Urban Institute; 2001. [Google Scholar]
- Kogan MD, Alexander GR, Teitelbaum MA, Jack BW, Kotelchuck M, Pappas G. “The Effect of Gaps in Health Insurance on Continuity of a Regular Source of Care among Preschool-aged Children in the United States.”. Journal of the American Medical Association. 1995;274(18):1429–35. [PubMed] [Google Scholar]
- Ku L, Ross DC. Staying Covered: The Importance of Retaining Health Insurance for Low-Income Families. Washington, DC: Center on Budget and Policy Priorities; 2002. [Google Scholar]
- Lewis K, Ellwood M. Children's Health Insurance Patterns: A Review of the Literature. Cambridge, MA: Mathematica Policy Research, Inc; 1997. [Google Scholar]
- Miller JE, Phillips JA. Does Context Affect SCHIP Disenrollment? Findings from a Multilevel Analysis. Chicago: Joint Center for Poverty Research; 2002. [Google Scholar]
- National Governors Association . Maternal and Child Health Update. Washington, DC: NGA Center for Best Practices; 1998, 1999, 2000, 2001. [Google Scholar]
- Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. “Health Insurance and Access to Primary Care for Children.”. New England Journal of Medicine. 1998;338(8):513–9. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- Perry M, Kannel S, Riley T, Pernice C. What Parents Say: Why Eligible Children Lose SCHIP. Portland, ME: National Academy for State Health Policy; 2001. [Google Scholar]
- Rajmil L, Fernandez E, Salas T, Barba G, Raspall F, Vila C, Segura A, Plasencia A. “Gender Differences in Children's Hospitalization in Catalonia: Another Inequality?”. Acta Paediatrica. 1999;88:990–7. doi: 10.1080/08035259950168504. [DOI] [PubMed] [Google Scholar]
- Rosenbach M, Ellwood M, Czajka J, Irvin C, Coupe W, Quinn B. Implementation of the State Children's Health Insurance Program: Momentum Is Increasing after a Modest Start. Cambridge, MA: Mathematica Policy Research, Inc.; 2001. [Google Scholar]
- Ross DC, Cox L. Making It Simple: Medicaid for Children and CHIP Income Eligibility Guidelines and Enrollment Procedures. Menlo Park, CA: Kaiser Family Foundation; 2000. [Google Scholar]
- Shenkman E, Vogel B, Boyett J, Naff R. “Disenrollment and Re-Enrollment Patterns in a CHIP.”. Health Care Financing Review. 2002;23(3):47–63. [PMC free article] [PubMed] [Google Scholar]
- Shi L, Samuels ME, Pease M, Bailey P, Corley E. “Patient Characteristics Associated with Hospitalizations for Ambulatory Care Sensitive Conditions in South Carolina.”. Southern Medical Journal. 1999;92(10):989–98. doi: 10.1097/00007611-199910000-00009. [DOI] [PubMed] [Google Scholar]
- Shulman S. Evaluating Infant Utilization and Retention under Medicaid Managed Care. Cambridge, MA: Harvard University; 2003. (unpublished dissertation) [Google Scholar]
- Spady DW, Saunders DL, Schopflocher DP, Svenson LW. “Patterns of Injury in Children: A Population-Based Approach.”. Pediatrics. 2004;113(3):522–9. doi: 10.1542/peds.113.3.522. [DOI] [PubMed] [Google Scholar]
- Stata Corporation . Stata 7 Statistical Software. College Station, TX: Stata Corporation; 2001. [Google Scholar]
- Wells JCK. “Natural Selection and Sex Differences in Morbidity and Mortality in Early Life.”. Journal of Theoretical Biology. 2000;202:65–76. doi: 10.1006/jtbi.1999.1044. [DOI] [PubMed] [Google Scholar]