Abstract
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are widely used for the treatment of depression and anxious disorders. The observation that depression is an independent risk factor for cardiovascular mortality and morbidity in patients with ischemic heart disease, the assessment of the central role of serotonin in pathophysiological mechanisms of depression, and reports of cases of abnormal bleeding associated with antidepressant therapy have led to investigations of the influence of antidepressants on hemostasis markers. In this review, we summarize data regarding modifications of these markers, drawn from clinical studies and case reports. We observed an association between the type of antidepressant drug and the number of abnormal bleeding case reports, with or without modifications of hemostasis markers. Drugs with the highest degree of serotonin reuptake inhibition - fluoxetine, paroxetine, and sertraline - are more frequently associated with abnormal bleeding and modifications of hemostasis markers. The most frequent hemostatic abnormalities are decreased platelet aggregability and activity, and prolongation of bleeding time. Patients with a history of coagulation disorders, especially suspected or documented thrombocytopenia or platelet disorder, should be monitored in case of prescription of any serotonin reuptake inhibitor (SRI). Platelet dysfunction, coagulation disorder, and von Willebrand disease should be sought in any case of abnormal bleeding occurring during treatment with an SRI. Also, a non-SSRI antidepressant should be favored over an SSRI or an SRI in such a context. Considering the difficulty in performing platelet aggregation tests, which are the most sensitive in SRI-associated bleeding, and the low sensitivity of hemostasis tests when performed in case of uncomplicated bleeding in the general population, establishing guidelines for the assessment of SRI-associated bleeding complications remains a challenge.
Keywords: antidepressant, selective serotonin reuptake inhibitor, serotonin, hemostasis, hemostasis test, bleeding
Abstract
Los antidepresivos, especialmente los inhibidores selectivos de la recaptación de serotonina (ISRS), se utilizan frecuentemente en el tratamiento de la depresión y los trastornos de ansiedad. La consideración de la depresión como factor de riesgo independente que incide en una mayor mortalidad y morbilidad cardiovascular de pacientes con enfermedad cardiaca ischemica, así como la constatación del papel central de la serotonina en los mecanismos fisiopatológicos de la depresión, y el conocimiento de casos de hemorragias anormales producidas durante tratamientos con antidepresivos, han llevado a examinar el efecto de los antidepresivos sobre los medidores de hemostasis. Los fármacos con mayor grado de inhibición de la recaptación de serotonina - fluoxetina, paroxetina y sertralina - son los más frecuentemente asociados con hemorragias anormales y perturbaciones hemostáticas. Los trastornos hemostáticos más frecuentemente observados son la disminución de la aglutinación y de la actividad de las plaquetas, y la prolongación del tiempo de hemorragia. Generalmente, pacientes con antecedentes de trastornos de coagulación, en particular trombocitopenia o disturbio de las plaquetas ya diagnosticadas o sospechadas, deberían estar controlados si se les receta cualquier inhibidor de la recaptación de serotonina. En caso de hemorragias anormales durante un tratamiento con un inhibidor de la recaptación de serotonina (IRS), se debería proceder a la búsqueda de una disfunción de las plaquetas, una coagulopatia y la enfermedad de von Willebrand. Teniendo en cuenta la viabilidad de realizar las pruebas de aglutinación de las plaquetas, que son las más sensibles para casos de hemorragias asociadas con los IRS, y la baja sensibilidad de las pruebas de hemostasis hechas en caso de hemorragia no complicada en la población general, el desarrollo de criterios de guía para casos de hemorragia asociada con los IRS constituye todavía un importante desafío.
Abstract
Les antidépresseurs, particulièrement les inhibiteurs sélectifs de la recapture de la sérotonine (ISRS), sont largement utilisés dans le traitement des troubles dépressifs et anxieux. La mise en évidence du fait que la dépression est un facteur de risque indépendant pour une mortalité et une morbidité cardio-vasculaire accrue chez les patients souffrant de maladie cardiaque ischémique, celle du rôle central de la sérotonine (5-HT) dans les mécanismes physiopathologiques de la dépression, ainsi que la description de cas de saignements anormaux sous traitement antidépresseur, ont conduit à examiner l'influence des antidépresseurs sur les marqueurs de l'hémostase. Dans cet article, nous avons résumé les données concernant les variations de ces marqueurs à partir de cas et d'études cliniques. Nous avons observé une association entre le type d'antidépresseurs et le nombre de saignements anormaux avec ou sans modification des marqueurs de l'hémostase. Les molécules à haut degré d'inhibition de la recapture de la sérotonine, la fluoxétine, la paroxétine et la sertraline, sont le plus souvent associées à des saignements anormaux et des modifications des marqueurs de l'hémostase. Les anomalies hémostatiques le plus souvent observées sont une diminution de l'agrégabilité et de l'activité plaquettaires, ainsi qu'une prolongation du temps de saignement. De manière générale, les patients avec des antécédents de troubles de la coagulation, en particulier de thrombocytopénie ou de trouble plaquettaire connu ou suspecté, devraient faire l'objet d'une surveillance accrue en cas de prescription de n'importe quel inhibiteur de la recapture de la sérotonine (IRS). Une dysfonction plaquettaire, une coagulopathie et une maladie de Willebrand devraient être recherchées en cas de saignements anormaux au cours d'un traitement avec un IRS auquel on préférera un antidépresseur non IRS dans un tel contexte. Compte tenu de la difficulté de réalisation des tests d'agrégation plaquettaire, qui sont les tests les plus sensibles lors de saignements associés aux IRS, et de la faible sensibilité des tests de l'hémostase réalisés lors de saignements non compliqués dans la population générale, la mise en place de recommandations lors de saignements associés aux IRS reste un défi à relever.
Depression is considered to be an Independent risk factor for cardiovascular mortality and morbidity in patients with Ischemic heart disease (IHD).1,2The risk of cardiovascular disease is higher in Individuals suffering from depression,3 as is the risk of ischemic stroke.4 Among newly diagnosed patients with coronary heart disease, approximately one in five patients suffers from major depression, with a similar prevalence in patients recovering from acute myocardial infarction.5,6 The proposed mechanisms are either spurious, le, that depression predicts, but is not causally related to, cardiovascular heart disease morbidity and mortality (antidepressant cardiotoxicity, association with cardiac risk factors, sedentary lifestyle), or imply that depression may directly influence the course of cardiac heart disease (nonadherence to cardiac treatment and regimens, dysregulation of autonomic, neuroendocrine, and serotonergic systems).7
Serotonergic neurotransmission dysfunction has been investigated and observed in major depression.8,9 Various findings support the hypothesis that alterations in serotonergic neurons play a role in the pathophysiology of depression,10 and most antidepressants have a direct influence on serotonin (5-HT) transmission and levels. 5-HT is usually a vasodilator, becoming a vasoconstrictor when the endothelium is damaged.11 It is also involved in platelet aggregation. It is taken up from plasma and stored in platelet granules. Upon initiation of platelet aggregation, 5-HT is released into the blood and activates 5-HT2A receptors on the platelet membrane, which enhances the aggregation process. 5-HT per se is a weak activator, but dose-dependently enhances platelet activation induced by adenosine diphosphate (ADP) and, in particular, thrombin in whole blood.12 It also potentiates aggregation in the presence of epinephrine or collagen,13 and potentiates release reactions through a mechanism of amplification by an increase in free cytoplasmic intracellular calcium ion concentration. This induces a shape-change reaction of platelets, priming platelet surfaces for interactions with coagulation factors.14 5-HT may therefore be directly involved in increased cardiovascular mortality and morbidity in depressed patients.
A relationship between depressive symptoms and increased platelet activity has been established in physically healthy depressed patients15-17 as well as in postmyocardial infarction (MI) depressed patients.8,18 The following mechanisms mediating platelet abnormalities observed in major depression have been proposed19: altered platelet function by increased plasma concentrations of 5-HT and epinephrine, affected platelet function by increased intraplatelet calcium mobilization, upregulation of 5-HT2A receptors or ot-adrenoreceptors, downregulation of 5-HT transporter number, altered second messenger signal transduction, or altered intraplatelet concentrations of monoamines and catecholamines.17
Thus, 5-HT probably plays a role in the pathophysiological mechanisms of depression as well as in primary hemostasis platelet activity, and this neurotransmitter might be a key element in the understanding of the relationship between depression and increased risk of cardiovascular disease. Amplification of platelet aggregation could be altered by antidepressants that inhibit serotonin reuptake, in particular selective 5-HT reuptake inhibitors (SSRIs), because of depletion or decrease in intraplatelet 5-HT levels. The purpose of this review of the literature is to summarize changes in hemostatic function observed during treatment by antidepressants.
We performed a MEDLINE search of the relevant literature, and reviewed prospective and retrospective studies, as well as case reports and reviews of literature related to bleeding side effects and hemostasis laboratory findings, associated with antidepressant treatment in the psychiatric population, in post-MI depressed patients, or in healthy volunteers.
The prothrombotic effect of typical and atypical antipsychotics, as well as the impaired platelet function and thrombocytopenia caused by the mood stabilizer valproate and the possible procoagulant effect of treatment by lithium, are not examined here.
Hemostasis
The process of hemostasis involves four principal stages: first, the initiation and formation of the platelet plug (also called primary hemostasis), second, the coagulation cascade, a series of enzymatic actions on proteins leading to clot formation; third, its termination by antithrombotic control mechanisms; and fourth, the removal of the clot by fibrinolysis. The coagulation cascade leads to formation of fibrin polymers which consolidate the platelet plug formed during primary hemostasis.20 Abnormalities in tests measuring the function of primary hemostasis and clotting cascade (coagulation) have been reported in case reports and cohort studies in patients treated with antidepressants.
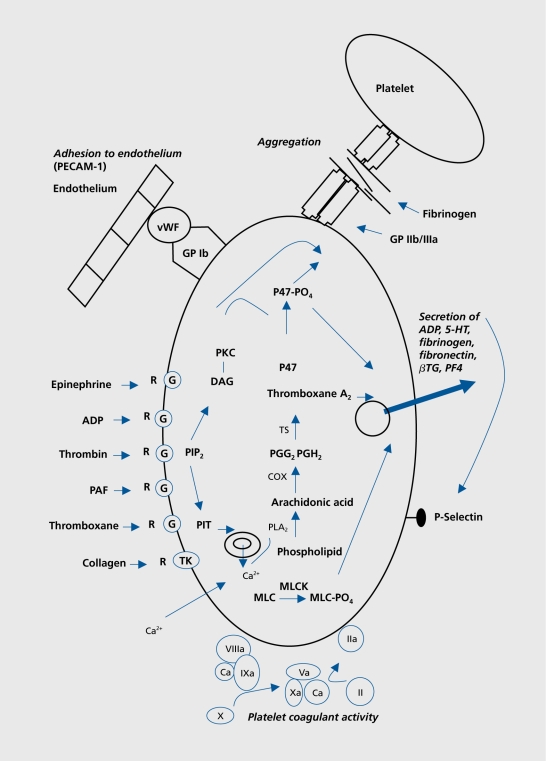
During primary hemostasis, the platelets form a plug at a site of injury in order to stop bleeding. This phase, which is the functional response of activated platelets, comprises four different processes: adhesion, aggregation, secretion, and procoagulant activity.21 During the vascular phase, vasoconstriction occurs and procoagulant (von Willebrand factor [vWF], tissue factor) as well as anticoagulant substances prostaglandin I2 [PGI2], thrombomodulin, urokinase, tissue plasminogen activator [tPA], antithrombin, nitric oxide [NO], and endotheliumderived relaxing factor [EDRF]) are secreted by the endothelium. The most potent platelet activators are collagen and thrombin, whereas ADP and epinephrine are weak activators. 5-HT itself is a weak platelet agonist, but it amplifies the effect of other platelet agonists.22 The process comprises successive steps, illustrating the central role of platelets (Figure 1):
Figure 1. Diagrammatic representation of primary hemostasis. 5-HT, serotonin; vWF, von Willebrand factor; ADP, adenosine diphosphate; βTG, β-thromboglobulin; PF4, platelet factor 4; MLC, myosine light chain; MLCK, myosine light chain kinase; PGG2, prostaglandin G2; PGH2, prostaglandin H2; PIP2 phosphatidylinositol 3,4-bisphosphate; PKC, protein kinase C; P47, pleckstrin phosphoprotein; TK, tyrosine kinase; PECAM, platelet endothelial cell adhesion molecule; DAG, diacylglycerol; COX, cyclo-oxygenase Adapted from ref 21: Colman RW, Clowes AW, George JN, et al. Hemostasis and Thrombosis: Basic Principles and Clinical Practice. Fifth ed. Philadelphia, Pa: Lippincott Williams and Wilkins; 2006. Copyright © Lippincott, Williams and Wilkins 2006.
Adhesion: Platelets change shape in response to activation, allowing adhesion to subendothelial matrix. This process is mediated by the binding of platelet surface receptor GPIb/IX/V complex to vWF. Binding of collagen to platelet collagen receptor GPIa/IIa also plays a role in platelet adhesion.
Aggregation: Both conformational and exposure changes in the GPIIb/IIIa on the platelet surface due to activation, result in binding of vWF and fibrinogen.
Secretion: Substances are secreted from platelet granules upon stimulation. ADP and 5-HT stimulate and recruit other platelets. Fibronectin stabilizes platelet aggregates. Secreted fibrinogen provides a source of fibrinogen at sites of endothelial injury in that present in the plasma. Thromboxane A2 (TXA2, from arachidonic acid [AA] release) stimulates platelet aggregation and causes vasoconstriction. Platelet-derived growth factor (PDGF) mediates tissue reparation.
Procoagulant activity: Exposure of procoagulant phospholipids and the subsequent assembly of the enzyme complexes on the platelet surface represent procoagulant activity.
Among others, the following laboratory tests explore primary hemostasis: platelet count, bleeding time, platelet function analyzer (PFA), platelet functional assessment, medullogram, and vWF (Table I). Normal values are not mentioned, since they are provided by the laboratory when these examinations are requested.
Table I. Laboratory tests of hemostasis. This list does not concern the third and fourth stages of hemostasis; the process is terminated by antithrombotic control mechanisms and fibrinolysis.
| Primary hemostasis | Coagulation cascade |
| Platelet count | Prothrombin time (extrinsic |
| pathway) | |
| Bleeding time | Partial thromboplastin time |
| (intrinsic pathway) | |
| Platelet function analyzer | Fibrinogen |
| Platelet functional assessment | Thrombin time |
| (Platelet aggregation) | |
| von Willebrand Factor | Coagulation factors |
| Inhibitors of coagulation | |
| (antithrombin, proteins C | |
| and S) |
The clotting cascade consists of the activation of various proenzymes to active enzymes, resulting in the formation of the red clot. Intrinsic and extrinsic pathways lead to activation of factor X which converts prothrombin to thrombin, the final enzyme of the clotting cascade, which in turns converts fibrinogen into an insoluble fibrin clot. Among others, the following laboratory tests examine the clotting cascade: prothrombin time (PT) and international normalized ratio (INR, extrinsic pathway), partial thromboplastin time (aPTT, intrinsic pathway), fibrinogen, thrombin time (TT), coagulation factors, and inhibitors of coagulation (antithrombin, proteins C and S, Table I).
Influence of antidepressant on hemostasis markers
Numerous prospective open comparative studies,9,16,23-34 randomized double-blind controlled trials,8,35-37 in vitro studies by incubation of the antidepressant compound,38-40 and case reports41-53 have pointed out changes in laboratory tests assessing function of primary hemostasis and clotting cascade.
Double-blind, randomized, placebo-controlled trials
In a randomized, double-blind, placebo-controlled, twoway crossover trial, Hergovich et al evaluated the potential inhibition of platelet function in 16 healthy male volunteers receiving paroxetine, 20 mg/d over 2 weeks. Paroxetine decreased intraplatelet 5-HT concentration by 83% and therefore prolonged closure time measured by PFA by 31% (in other terms inhibited the plug under shear stress). It also lowered platelet activation in response to thrombin receptor peptide, shown by an 8% decrease in the expression of the platelet activation marker CD63. No changes in plasma concentration of prothrombin fragment, vWF antigen, or soluble Pselectin were observed. This indicated no activation of coagulation, endothelium, or platelet in vivo, underlining a favorable risk:benefit ratio when the drug is used for rehabilitation of post-MI patients.35
In order to Investigate whether depressed post-MI patients have higher markers of platelet activation than nondepressed post-MI patients, and evaluate the effect of mirtazapine on platelet activation, Schins et al con? ducted a randomized, double-blind, placebo-controlled trial in 25 depressed post-MI patients receiving, for 8 weeks, either mirtazapine 30 to 45 mg or placebo. The control group consisted of nondepressed post-MI patients. The markers measured were plasma levels of pthromboglobulin (βTG), platelet factor 4 (PF4), soluble CD40 ligand (sCD40L), whole-blood, and intraplatelet 5-HT. Before treatment, only whole blood and intraplatelet 5-HT levels were significantly higher in depressed patients. Treatment with mirtazapine resulted in a nonsignificant decrease in βTG, PF4, and intraplatelet 5-HT level after 8 weeks. The authors underline the fact that mirtazapine, by lack of inhibitory effect on 5-HT reuptake, has not shown, in contrast with SSRIs, a potentiated risk of bleeding events, when given in combination with nonsteroidal antiinflammatory drugs (NSAIDs).54-56 Therefore, treatment of depressed post-MI patients with mirtazapine may be possible in patients susceptible to bleeding complications, according to the authors.8
In a randomized, double-blind, placebo-controlled trial, Serebruany et al assessed the release of platelet/endotheliai markers in 64 post-MI depressed patients treated with sertraline vs placebo. PF4, βTG, platelet/endothelial cell adhesion molecule-1, P-selectin, thromboxane B2 (TXB2), 6-ketoprostaglandin F1α, vascular cell adhesion molecule-1, and E-selectin were measured by enzymelinked immunosorbent assay (ELIS A). Treatment with sertraline was associated with substantially less release of these markers than treatment with placebo. These differences reached statistical significance for βTG at weeks 6 and 16 and for P-selectin at week 16. Repeatedmeasures ANOVA revealed a significant advantage for sertraline vs placebo for diminishing E-selectin and βTG concentrations across the entire treatment period. Despite previous broad use of aspirin and clopidogrel (though equally distributed between both groups), the authors underline the potential benefit of sertraline treatment of post-MI patients, because of decreased activation of platelets.36
Double-blind, randomized, comparative trial
Pollock et al investigated the influence of a 6-week paroxetine or nortriptyline treatment on platelet activation in 17 depressed patients with IHD, in a randomized double-blind trial. Baseline measurements of βTG and PF4 were significantly elevated in both groups before treatment, compared with those of healthy control subjects. In the paroxetine group, mean βTG and PF4 levels significantly decreased within 1 week of treatment and remained low at the 3- and 6-week measurements. In contrast, the nortriptyline group did not exhibit a significant decrease in βTG and PF4 levels after 1,3, and 6 weeks. A type II error for the nortriptyline group was not excluded; nor was the possible influence of the patient's clinical state on platelet activation. However, according to the authors, the reduction in platelet activation observed after only 1 week of paroxetine treatment is in favor of a pharmacologic effect.37
Prospective open comparative studies
Prospective open comparative studies, conducted in depressed patients, post-MI depressed patients, or healthy volunteers, with comparative measurements of various hemostasis parameters in a healthy control group or in subjects before treatment, demonstrated higher platelet activity in depressed or post-MI depressed patients in comparison with the control group, and/or decrease in platelet activity after antidepressant treatment.
Alvarez et al showed that untreated depressed patients have decreased numbers of platelet 5-HT transporter sites and increased levels of platelet inositol triphosphate (PIT), that treatment with both fluoxetine and clomipramine further reduces the density of these transporter sites (more marked in responders to treatment), accompanied by a dramatic decrease in plasma and platelet 5-HT levels, and that, in responders, PIT levels return to normal values.9
Markovitz et al showed a greater platelet secretory response to collagen in depressed patients than in healthy control subjects in baseline comparison measures. They then demonstrated a decrease in collagen-induced platelet secretion after treatment with sertraline for 6 weeks, most other platelet activation measures showing minimal change. These changes were, however, not related to improvement in the Beck Depression Inventory scores, but this finding might be limited by the short treatment duration. Thus, the decreased platelet activation after SSRI treatment could diminish the risk of coronary heart disease among depressed subjects, but the authors underline the need for studies in a large number of patients, placebo controls, and a longer follow-up period.24
In a study by Musselman et al, after 6 weeks of open-label treatment with paroxetine, a normalization of platelet activation occurred in patients with depression. This was shown by a significant decrease in PF4 and of the platelet monoclonal antibodies anti ligand-induced platelet binding site (LIBS) and GA6 (anti P-selectin). Before treatment, these markers were higher among depressed patients compared with the control group. The results of this study could be explained by recovery from depression. Thus, studies with placebo and/or psychotherapy are proposed by the authors as further investigation.25
A decrease in platelet response mediated by the 5-HT2A receptor following effective imipramine treatment was demonstrated by Gomez-Gil et al, shown by a significant decrease in 5-HT-amplified platelet aggregation to ADP, thus suggesting that desensitization or downregulation of platelet 5-HT2A receptor function could be linked to a therapeutic effect of some antidepressants.30
Comparing levels of plasma 5-HT and platelet 5-HT induced aggregation among depressed patients treated with either fluoxetine or amitriptyline and nontreated patients, Menys et al demonstrated a statistically significant decrease in both plasma 5-HT levels and 5-HT induced platelet aggregation, only with fluoxetine. This suggests a higher inhibition of platelet activity by SSRIs than tricyclic antidepressants, and therefore a more suitable treatment for depressed patients with cardiovascular disease.26
Laine-Cessac et al failed to demonstrate a significant effect of a 1-month fluoxetine treatment in 8 depressed patients, on the following primary hemostasis and coagulation tests: PT, aPTT, TT, fibrinogen, platelet count, bleeding time, platelet aggregation induced by ADP, AA, ristocetin, and collagen. The single statistically significant difference, in comparison with values before treatment, was found in a decreased velocity in platelet aggregation induced by epinephrine. The authors conclude that significant platelet dysfunction causing hemorrhagic diathesis is uncommon when fluoxetine is used at a dosage of 20 mg daily.27 However, methodological issues with this publication suggest a high risk of type II error.27
Lederbogen et al measured aPTT, vWF, fibrinogen, fibrin monomer, and prothrombin ratio (Quick) before and after treatment with either amitriptyline or paroxetine. Therapy was effective on depressive symptoms as measured by the Hamilton Depression scale in both groups, and ANOVA revealed prothrombin ratio to increase from start to end of treatment. No effect was seen on the other parameters. The authors conclude that changes observed in prothrombin ratio may be due to nutritional factors, and that bleeding associated with antidepressant therapy is probably not an extreme form of a general influence on the coagulation systems, but rather an idiosyncratic reaction.32
Berk et al studied 10 patients before and after treatment with fluoxetine. No changes in any index of platelet aggregation or coagulation were reported.33 Alderman et al were also unable to demonstrate any changes in primary hemostasis or coagulation parameters after use of fluoxetine or paroxetine for 28 days.28 This was also the case after a fluoxetine trial conducted by Bang et al.34
Interestingly, Tharmapathy et al observed that platelets from six or seven patients undergoing treatment with venlafaxine aggregated spontaneously during a routine centrifugation of platelet-rich plasma. Furthermore, increased baseline platelet activity as measured by P-selectin surface expression was observed during treatment compared with before treatment.29
In vitro studies
The in vitro effects of escalating concentrations of sertraline on human platelets were assessed by Serebruany et al, showing a dose-dependent inhibition of platelet aggregation induced by ADP, collagen, and thrombin, as well as decreased platelet surface expression of CD9, Pselectin, platelet endothelial cell adhesion molecule (PECAM)-I, and glycoproteins Ilb/IIIa and lb. The data from this study, showing a direct inhibitory effect on platelets of therapeutic concentrations of sertraline, suggest that it may account for a substantial portion of the association between depression and adverse outcomes of IHD by a thrombotic mechanism.39
Mohammad and Mason also demonstrated an inhibition of ADP-induced platelet aggregation by the tricyclics imipramine and amitriptyline.38
Case reports (no baseline values)
Among case reports of abnormal bleeding with antidepressant medication, some have revealed abnormalities in hemostasis tests. Alderman et al and De Maistre et al reported cases of abnormal bleeding associated with fluoxetine treatment, accompanied by a decrease in ADP, epinephrine, ristocetin, AA, collagen, and epinephrineinduced platelet aggregation, respectively, which were reversible after discontinuation of the drug (positive dechallenge).41,42
Ottervanger et al reported a decrease in epinephrineinduced platelet aggregation in a patient treated with paroxetine for 4 weeks.45
A decrease in ADP and ristocetin-induced platelet aggregation in a patient treated with fluoxetine was also reported by Evans et al. They also described an increase in bleeding time to more than 25 minutes, with positive dechallenge and rechallenge.46
Increased bleeding time with positive dechallenge was reported by Humphries et al in a patient treated for 2 years with fluoxetine, and by Calhoun and Calhoun for a patient treated for 10 weeks with sertraline.47,48 Ceylan and Alpsan-Omay also described the case of a patient treated with sertraline for 7 days, with prolonged bleeding time and prothrombin time, as well as a decrease in platelet count. All three parameters reversed after discontinuation (positive dechallenge).49
Low platelet count was also noted by Aranth and Lindberg and Leung and Shore in patients treated respectively with fluoxetine and fluvoxamine.43,44
Tham et al, Démet et al, and Tielens reported prolonged aPTT with venlafaxine, mirtazapine, and paroxetine respectively50,51,53 in the first two cases, values returned to normal range after discontinuation (positive dechallenge). Tham et al also reported a high antihemophilic factor VIII, whereas Démet et al showed a prolonged prothrombin time and increased INR.50,51
In contradiction with these findings, a case of diminished prothrombin time and aPTT was reported by Hardy and Sirois when trazodone was added to treatment with warfarin after mitral valve replacement, thus decreasing the efficiency of this treatment.52
Table II summarizes the discussed clinical studies on modification of hemostasis markers, while Table III summarizes the case reports.
Table II. Clinical studies on modifications of hemostasis markers. DB, double-blind; PC, placebo-controlled; POC, prospective open comparative study; PO, prospective open; CS,cross-sectional; DEP, depression; SS, statistically significant; MAB, monoclonal antibodies; NA, non-available; IHD, ischemic heart disease; βTG, β-thromboglobulin; PF4, platelet factor 4; ANOVA, analysis of variance; PECAM, platelet endothelial cell adhesion molecule; 5-HT, serotonin; CI, confidence interval; PIT, platelet inositol triphosphate; LIBS, ligand-induced platelet binding site; aPTT, partial thromblastin time; INR, international normalized ratio; TT, thrombin time; AA, arachidonic acid; ADP, adenosine diphosphate; PT, prothtrombin time .
| Type of study | Subjects | N° | Treatment | SS modifications of hemostasis markers | |
| Pollock et al, 200037 | Randomized, DB | DEP + IHD | 17 | Paroxetine or | Paroxetine: ↓ βTG (P<0.01), PF4 (P<0.001); |
| nortriptyline (6 weeks) | Nortriptyline: non-SS: ↓ PF4 | ||||
| Serebruany et al, 200336 | Randomized, | Post-MI DEP | 28 | Sertraline (16 weeks) | ↓ βTG (P=0.03), P-selectin (P=0.04), |
| DB, PC | DB, PC E-selectin and βTG (ANOVA); | ||||
| non-SS: ↓ PF4, PECAM-I | |||||
| Schins et al, 20048 | Randomized, | Post-MI DEP | 25/21 | Mirtazapine (8 weeks) | Non-SS: ↓ βTG, PF4, platelet 5-HT |
| DB, PC | vs non-DEP | ||||
| Hergovich et al, 200035 | Randomized, | Healthy | 16 | Paroxetine (2 weeks) | ↓ platelet 5-HT by 83% (CI95: 74-92), |
| DB, PC, CS/PO. | ↓ collagen/epinephrine induced platelet | ||||
| aggregation by 31% (CI95: 6-56), 1CD63 by 8% | |||||
| (CI95:4-12) | |||||
| Alvarez et al, 19999 | POC | DEP vs | 27/NA | Fluoxetine or | Fluoxetine: ↓ 5-HT plasma to 19% and |
| healthy | clomipramine | platelet to 23%, ↓ of PIT (P<0.02); | |||
| platelet to 23%, ↓ of PIT (P<0.02); | ↓ platelet paroxetine receptor (P=0.03) | ||||
| Clomipramine: ↓ 5-HT plasma to 8% and platelet | |||||
| to 40%, ↓ of PIT (P<0.0001); ↓ platelet paroxetine | |||||
| receptor (P=0.05) | |||||
| Markovitz et al, 200024 | POC | DEP vs | 17/21 | Sertraline (6 weeks) | ↓ collagen-induced platelet sécrétion |
| healthy | by 19.5% (P<0.05) | ||||
| Musselman et al, 200024 | POC | DEP vs | 15/12 | Paroxetine (6 weeks) | ↓ PF4 by 54%, platelet binding MAB |
| healthy | anti-LIBS by 48% (P=0.0007) and GA6 by 17% | ||||
| (P=0.02) (ie, ↓ activation) | |||||
| Gomez-Gil et al, 200430 | POC | DEP vs | 15/15 | Imipramine (145 days) | ↓ 5-HT induced platelet aggregation |
| healthy | (P=0.038) | ||||
| Piletz et al, 200016 | POC | DEP vs healthy | 19/17 | Bupropion (6-8 weeks) | No SS changes in P-selectin levels |
| Menys et al, 199626 | CS, POC | DEP vs | 33/13 | Fluoxetine or amitriptyline | Fluoxetine: ↓ plasma 5-HT (P<0.005), |
| non-treated | ↓ 5-HT induced aggregation; amitriptyline: | ||||
| no SS changes (P<0.05) | |||||
| Laine-Cessac et al, 199827 | PO | DEP | Fluoxetine | ↓ epinephrine-induced platelet aggregation (P<0.025) | |
| Alderman et al, 199628 | PO | DEP | 8 | Fluoxetine or | No SS changes of platelet aggregation, aPTT, |
| paroxetine (28 days) | PT, INR, platelet count | ||||
| Tharmopathy et al, 200029 | POC | DEP | 7 | Venlafaxine vs tricyclic Spontaneous platelet aggregation, | ↓ P-Selectin |
| Lederbogen étal, 200131,32 | POC | Dep | 49 | Amitriptyline or | Amitriptyline: ↓ prothrombin ratio |
| paroxetine (5 weeks) | (100.9%, P0.002); non-SS: ↓ platelet | ||||
| aggregation | |||||
| Paroxetine: ↓ prothrombin ratio (99.1%, P<0.002); | |||||
| non-SS: ↓ platelet aggregation | |||||
| Bang et al, 199133 | Prosp. op. | Healthy | 10 | Fluoxetine (4-6 weeks) | No SS changes in platelet aggregation |
| and coagulation factors | |||||
| Berk et al, 199534 | Prosp. op. | Dep | 10 | Fluoxetine | No SS changes in INR, aPTT, TT, bleeding time, |
| factors II, V, VII, VIII:C, IX, X, XI, XII, fibrinogen, | |||||
| platelet sensitivity to AA, collagen, ADP, epinephrine | |||||
| Serebruany et al, 200139 | In vitro | IHD vs healthy | 6/7 | Sertraline | ↓ platelet ADP-collagen-thrombin induced |
| aggregability, ↓ P-selectin, CD9, PECAM-I, | |||||
| glycoprotein llb/llla and Ib | |||||
| Mohammad et al, 197438 | In vitro | Healthy | NA | Imipramine or amitriptyline | ↓ ADP-induced platelet aggregation |
| Bondurant et al, 199840 | In vitro | Healthy | 5 | Fluoxetine | No SS changes in PT |
Table III. Case reports of modifications of hemostasis markers. AA, arachidonic acid; ADP, adenosine diphosphate; aPTT, partial thromboplastin time; INR, international normalized ratio .
| Treatment | Subject | Modifications of hemostasis markers | Dechallenge | Bleeding | |
| Alderman et al, 199241 | Fluoxetine | 49-year-old man | ↓ ADP-epinephrine-ristocetin-AA- | + | |
| (4 days) | collagen-induced platelet aggregation | ||||
| De Maistre et al, 200242 | Fluoxetine | 78-year-old woman | ↓ Epinephrine-induced | + | Intraperitoneal |
| (1-year) | platelet aggregation | hematoma | |||
| Aranth et Lindberg, | Fluoxetine | 40-year-old woman | Platelet count= 131 g/L | - | Ecchymoses |
| 199243 | 60 mg (2 months) | ||||
| Leung et Shore, | Fluvoxamine | 38-year-old man | Platelet count =142 g/L | - | Epistaxis, |
| 199644 | 200 mg | ecchymoses | |||
| Ottervanger et al, | Paroxetine | 27-year-old woman | ↓ Epinephrine-induced | - | Ecchymoses |
| 199445 | 20 mg (4 weeks) | platelet aggregation | |||
| Evans et al, 199146 | Fluoxetine | 33-year-old man | ↓ ADP-ristocetin-induced platelet | + and | Subdural |
| 20 mg | aggregation; bleeding time > 25 min, | rechallenge + | hematomas | ||
| Humphries et al, | Fluoxetine | 44-year-old woman | Bleeding time > 11.5 min. | + | Petechiae |
| 199047 | 20 mg (2-years) | ||||
| Calhoun et Calhoun, | Sertraline | 16-year-old woman | Bleeding time >12.5 min. | + | Ecchymoses |
| 199648 | 50 mg (10 weeks) | ||||
| Ceylan et Alpsan- | Sertraline | 43-year-old woman | Bleeding time =11 min.; | + | Hemoptysis, |
| Omay, 200549 | 50 mg (7 days) | PT =20 sec; platelet count =30 g/L | macroscopic | ||
| hematuria | |||||
| Tham et al, 199950 | Venlafaxine | 47-year-old woman | aPTT =89 sec; high antihemophilic | + | Ecchymoses |
| 75 mg (2.5 months) | factor VIII C antibodies, titre =190 BU/mL | ||||
| Démet et al, 200551 | Mirtazapine | 54-year-old woman | PT =22 sec; INR =2.56; aPTT =34 sec | + | Ecchymoses |
| 30 mg (10 months) | |||||
| Hardy et Sirois, 198652 | Trazodone | 40-year-old woman | TP =14 sec (before trazodone =20 sec); | - | |
| 300 mg (5 weeks) | aPTT = 36 sec (before trazodone =44 sec) | ||||
| + Warfarin | |||||
| Tielens, 199753 | Paroxetine | 33-year-old woman | aPTT=41 sec | - | Bruises, excessive |
| 40 mg (2 weeks) | menstrual blood |
Discussion
In this review, we have presented the modifications of hemostasis markers caused by antidepressants. The most frequent modifications are decreased platelet aggregability and activity, and prolongation of bleeding time (primary hemostasis); they are more likely to occur with antidepressants such as fluoxetine, sertraline, or paroxetine. Other antidepressants such as venlafaxine, fluvoxamine, amitriptyline, imipramine, and even mirtazapine, can also influence hemostasis. Modifications of platelet count, as well as PT and PTT (coagulation cascade) are much less frequent. It is not known whether there might be laboratory modifications in the last two stages of hemostasis, ie, the termination by antithrombotic control mechanisms and the removal of the clot by fibrinolysis.
Antidepressants that inhibit platelet reuptake of 5-HT cause a platelet 5-HT depletion. This can inhibit 5-HTinduced platelet aggregation amplification. Patients suffering from bleeding complications during antidepressant treatment may have a mild pre-existing platelet disorder or a modified platelet serotonergic response amplified by depletion of 5-HT stocks57; autoimmune mechanisms may also be involved.50
Different types of studies were performed, from case reports to epidemiological studies and prospective laboratory studies comparing subjects and controls receiving antidepressants. These studies did not lead to the same conclusions.
A causal association between use of antidepressants, especially SSRIs, and abnormal bleeding or need for transfusion during surgical procedures has been found in retrospective studies.54-56,58-61 The main observation concerns a relationship between the type of antidepressant drug and the risk of bleeding complications. The risk of upper gastrointestinal bleeding was twice as high for SSRIs than for other antidepressant drugs.55 The risk of upper gastrointestinal bleeding in elderly and depressed patients increased with antidepressants having the greatest extent of inhibition of 5-HT reuptake.56 Similarly, a significant association between the degree of 5-HT reuptake Inhibition by antidepressants and the risk of hospital admission for abnormal bleeding as primary diagnosis was found.59 in these studies, antidepressants were classified according to their degree of 5-HT reuptake Inhibition according to pharmacological studies.62,63 Blood transfusion require? ments during surgery was Increased for SRI antidepressant users compared with nonusers, which was not the case for nonserotonerglc antidepressant users.60 Upper gastrointestinal bleeding risk was found to be 12.2 times greater than expected when there was a concomitant use of SSRIs and NSAIDs.54
In the prospective laboratory studies mentioned, the results are heterogenous. Indeed, some studies found changes in given laboratory tests which were normal in other studies. Some studies failed to show any modlflca? tion in measured hemostasis markers.28,33,34 Otherwise, decrease in platelet/plasma 5-HT level and diminution of 5-HT-lnduced aggregation are the markers which were more often modified upon antldepresslve treatment, in line with the central role of this neurotransmitter in primary hemostasis.9,26,30 Thus, prospective studies clearly Indicate that antidepressants modify primary hemostasis. However, the configuration and the extent of these changes remains unspecified.
Most case reports of abnormal bleeding associated with the use of antidepressants that have failed to demonstrate perturbations in hemostasis concern the use of antidepressants with high degree of Inhibition of 5-HT reuptake,45,57,64,76 or, to a lesser extent, antidepressants with a mild degree of Inhibition of 5-HT reuptake.77,80 This was also the case for abnormal bleeding case reports with perturbation of hemostasis markers. In accordance with classification of antidepressants by their degree of 5-HT reuptake Inhibition, the drugs most frequently associated with abnormal bleeding are the SSRIs fluoxetine, sertra? line and paroxetine, thus confirming that 5-HT may directly be involved in the pathophysiology of bleeding side effects in patients undergoing antidepressant treatment, and may therefore be a more potent platelet activator in vivo than in vitro. Interestingly, in those case reports where coagulation markers were measured, about half of the patients showed no modification of hemostasis markers. This is coherent with the observa? tion that hemostasis tests, when performed in the general population, in cases of uncomplicated bleeding such as bruising, have a low sensitivity, ie, show normal results.
The platelet aggregation tests are the most sensitive tests when modifications of hemostasis markers are suspected during treatment with antidepressants; however, they are time-consuming or, unfortunately, not performed in routine laboratory studies. Furthermore, these tests sometimes give negative results because of genetic factors, leading to the absence of platelet aggregation. This is explained by inherited differences in platelet aggregation (PAR)-l thrombin receptor levels, and may be clinically relevant for subjects at increased risk of bleeding.81
Several pertinent questions remain about the clinical relevance of hemostasis modifications by antidepressants. Should antidepressants be contraindicated in patients receiving anticoagulation treatment, or suffering from gastric ulcer, from von Willebrand disease, or from hemo? philia? Should hemostasis tests be performed in all patients treated with SSRIs and undergoing surgery?82
What is the correct course to take in case of abnormal bleeding in a patient treated with an antidepressant? in our opinion, the above questions are highly relevant to clinical practice, but it remains difficult to provide straightforward answers for several reasons. In most of the publications mentioned, the authors propose no guidelines for SRI? or SSRI-associated bleeding complications, arguing that complementary investigations are still requested. Members of hematological societies are best equipped to establish guidelines on the above issues. Such guidelines will help clinicians. In the meantime, we can nevertheless propose the following general comments. In case of abnormal bleeding in a patient treated with an SSRI, the pharmacological treatment should be stopped, and replaced if needed by a non-SSRI antidepressant. Patients with a medical history of coagulation disorders, especially suspected or documented thrombo? cytopenia or platelet disorder, should be monitored in case of prescription of any SRI. Platelet dysfunction, coagulation disorders, and von Willebrand disease (characterized by prolongation of bleeding time combined with decreased factor VIII procoagulant activity) should be sought in case of abnormal bleeding occurring during treatment with any SRI. Platelet aggregation measurement by PFA is the most sensitive laboratory test in these situations, and should be considered if hemostasis tests are requested, for example before surgery. Non-SSRI antidepressants should be preferred to SSRIs or SRIs in cases of von Willebrand disease, hemophilia, gastric ulcer, and anticoagulation treatment.
Selected abbreviations and acronyms
- 5-HT
5-hydroxytryptamine (serotonin)
- AA
arachidonic acid
- ADP
adenosine diphosphate
- aPTT
partial thromboplastin time
- βTG
β-thromboglobulin
- IHD
ischémie heart disease
- INR
international normalized ratio
- MI
myocardial infarction
- NSAID
nonsteroidal anti-inflammatory drug
- PDGF
platelet-derived growth factor
- PF4
platelet factor 4
- PFA
platelet function analyzer
- PIT
platelet inositol triphosphate
- PT
prothrombin time (Quick)
- SRI
serotonin reuptake inhibitor
- SSRI
sélective serotonin reuptake inhibitor
- TT
thrombin time
- TXA2
thromboxane A2
- vWF
von Willebrand factor
Contributor Information
Demian Halperin, Clinical Psychopharmacology Unit, Geneva University Hospitals, Geneva, Switzerland.
Guido Reber, Hemostasis unit, Geneva University Hospitals, Geneva, Switzerland.
REFERENCES
- 1.Bush DE., Ziegelstein RC., Tayback M., et al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol. 2001;88:337–341. doi: 10.1016/s0002-9149(01)01675-7. [DOI] [PubMed] [Google Scholar]
- 2.Barefoot JC., SchroII M. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation. 1996;93:1976–1980. doi: 10.1161/01.cir.93.11.1976. [DOI] [PubMed] [Google Scholar]
- 3.Penninx BW., Beekman AT., Honig A., et al. Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry. 2001;58:221–227. doi: 10.1001/archpsyc.58.3.221. [DOI] [PubMed] [Google Scholar]
- 4.Ohira T., Iso H., Satoh S., et al. Prospective study of depressive symptoms and risk of stroke among Japanese. Stroke. 2001;32:903–908. doi: 10.1161/01.str.32.4.903. [DOI] [PubMed] [Google Scholar]
- 5.Carney RM., Freedland KE., Rich MW., Jaffe AS. Depression as a risk factor for cardiac events in established coronary heart disease: a review of possible mechanisms. Ann Behav Med. 1995;17:142–149. doi: 10.1007/BF02895063. [DOI] [PubMed] [Google Scholar]
- 6.Glassman AH., Shapiro PA. Depression and the course of coronary heart disease. Am J Psychiatry. 1998;155:104–111. doi: 10.1176/ajp.155.1.4. [DOI] [PubMed] [Google Scholar]
- 7.Carney RM., Freedland KE., Miller GE., Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- 8.Schins A., Hamulyak K., Scharpe P., et al. Whole blood serotonin and platelet activation in depressed post-myocardial infarction patients. Life Sci. 2004;24;76:637–650. doi: 10.1016/j.lfs.2004.04.060. [DOI] [PubMed] [Google Scholar]
- 9.Alvarez JC., Gluck D., Arnulf I., et al. Decreased platelet serotonin transporter sites and increased platelet inositol triphosphate levels in patients with unipolar depression: effects of clomipramine and fluoxetine. Clin Pharmacol Ther. 1999;66:617–624. doi: 10.1053/cp.1999.v66.103402001. [DOI] [PubMed] [Google Scholar]
- 10.Owens MJ., Nemeroff CB. Role of serotonin in the pathophysiology of depression: focus on the serotonin transporter. Clin Chem. 1994;40:288–295. [PubMed] [Google Scholar]
- 11.Golino P., Piscione F., Willerson JT., et al. Divergent effects of serotonin on coronary-artery dimensions and blood flow in patients with coronary atherosclerosis and control patients. N Engl J Med. 1991;324:641–648. doi: 10.1056/NEJM199103073241001. [DOI] [PubMed] [Google Scholar]
- 12.Li N., Wallen NH., Ladjevardi M., Hjemdahl P. Effects of serotonin on platelet activation in whole blood. Blood Coagul Fibrinolysis. 1997;8:517–523. doi: 10.1097/00001721-199711000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Skop BP., Brown TM. Potential vascular and bleeding complications of treatment with selective serotonin reuptake inhibitors. Psychosomatics. 1996;37:12–16. doi: 10.1016/S0033-3182(96)71592-X. [DOI] [PubMed] [Google Scholar]
- 14.Troy GC. An overview of hemostasis. Vet Clin North Am Small Anim Pract. 1988;18:5–20. doi: 10.1016/s0195-5616(88)50003-7. [DOI] [PubMed] [Google Scholar]
- 15.Schins A., Honig A., Crijns H., Baur L., Hamulyak K. Increased coronary events in depressed cardiovascular patients: 5-HT2A receptor as missing link? Psychosom Med. 2003;65:729–777. doi: 10.1097/01.psy.0000088596.42029.10. [DOI] [PubMed] [Google Scholar]
- 16.Piletz JE., Zhu H., Madakasira S., et al. Elevated P-Selectin on platelets in depression: response to. bupropion. J Psych iatr Res. 2000;34:397–404. doi: 10.1016/s0022-3956(00)00034-0. [DOI] [PubMed] [Google Scholar]
- 17.Musselman DL., Tomer A., Manatunga AK., et al. Exaggerated platelet reactivity in major depression. Am J Psych ia try. 1996;153:1313–1317. doi: 10.1176/ajp.153.10.1313. [DOI] [PubMed] [Google Scholar]
- 18.Laghrissi-Thode F., Wagner WR., Pollock BG., Johnson PC., Finkel MS. Elevated platelet factor 4 and p-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biol Psychiatry. 1997;42:290–295. doi: 10.1016/S0006-3223(96)00345-9. [DOI] [PubMed] [Google Scholar]
- 19.Nemeroff CB., Musselman DL. Are platelets the link between depression and ischemic heart disease? Am Heart J. 2000;140 (4 suppl):57–62. doi: 10.1067/mhj.2000.109978. [DOI] [PubMed] [Google Scholar]
- 20.Leung Lawrence LK. Overview of hemostasis. Available at: www.uptodate.com. Accessed November 2006 [Google Scholar]
- 21.Colman RW., Clowes AW., George JN., et al. Hemostasis and Thrombosis: Basic Principles and Clinical Practice. Fifth ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2006 [Google Scholar]
- 22.De Clerck F. The role of serotonin in thrombogenesis. Clin Physiol Biochem. 1990;8(suppl 3):40–49. [PubMed] [Google Scholar]
- 23.Butler J., Leonard BE. The platelet serotonergic system in depression and following sertraline treatment. Int Clin Psychopharmacol. 1988;3:343–347. doi: 10.1097/00004850-198810000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Markovitz JH., Shuster JL., Chitwood WS., May RS., Tolbert LC. Platelet activation in depression and effects of sertraline treatment: an open-label study. Am J Psychiatry. 2000;157:1006–1008. doi: 10.1176/appi.ajp.157.6.1006. [DOI] [PubMed] [Google Scholar]
- 25.Musselman DL., Marzec UM., Manatunga A., et al. Platelet reactivity in depressed patients treated with paroxetine: preliminary findings. Arch Gen Psychiatry. 2000;57:875–882. doi: 10.1001/archpsyc.57.9.875. [DOI] [PubMed] [Google Scholar]
- 26.Menys VC., Smith CC., Lewins P., Farmer RD., Noble Ml. Platelet 5-hydroxytryptamine is decreased in a preliminary group of depressed patients receiving the 5-hydroxytryptamine re-uptake inhibiting drug fluoxetine. Clin Sci (Lond). 996;91:87–92. doi: 10.1042/cs0910087. [DOI] [PubMed] [Google Scholar]
- 27.Laine-Cessac P., Shoaay I., Garre JB., Glaud V., Turcant A., Allain P. Study of haemostasis in depressive patients treated with fluoxetine. Pharmacoepidemiol Drug Saf. 1998;7(suppl 1):S54–S57. doi: 10.1002/(sici)1099-1557(199808)7:1+<s54::aid-pds345>3.3.co;2-q. [DOI] [PubMed] [Google Scholar]
- 28.Alderman CP., Seshadri P., Ben-Tovim Dl. Effects of serotonin reuptake inhibitors on hemostasis. Ann Pharmacother. 1996;30:1232–1234. doi: 10.1177/106002809603001103. [DOI] [PubMed] [Google Scholar]
- 29.Tharmapathy P., Selheim F., Odegaard K., Lund A., Holmsen H. Venlafaxine treatment stimulates blood platelet activity. J Clin Psychopharmacol. 2000;20:589–590. doi: 10.1097/00004714-200010000-00023. [DOI] [PubMed] [Google Scholar]
- 30.Gomez-Gil E., Gasto C., Carretero M., et al. Decrease of the platelet 5HT2A receptor function by long-term imipramine treatment in endogenous depression. Hum Psychopharmacol. 2004;19:251–258. doi: 10.1002/hup.583. [DOI] [PubMed] [Google Scholar]
- 31.Lederbogen F., Gilles M., Maras A., et al. Increased platelet aggregability in major depression? Psychiatry Res. 2001;24:255–261. doi: 10.1016/s0165-1781(01)00259-1. [DOI] [PubMed] [Google Scholar]
- 32.Lederbogen F., Weber B., Colla M., Heuser H., Deuschle M., Dempfle CE. Antidepressant treatment and global tests of coagulation and fibrinolysis. J Clin Psychiatry. 2001;62:2. doi: 10.4088/jcp.v62n0210g. [DOI] [PubMed] [Google Scholar]
- 33.Berk M., Jacobson BF., Hurly E. Fluoxetine and hemostatic function: a pilot study. J Clin Psychiatry. 1995;56:14–16. [PubMed] [Google Scholar]
- 34.Bang NU. Acquired abnormalities of platelet function [letter]. N Engl J Med. 1991;324:1672. doi: 10.1056/NEJM199106063242313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hergovich N., Aigner M., Eichler HG., Entlicher J., Drucker C., Jilma B. Paroxetine decreases platelet serotonin storage and platelet function in human beings. Clin Pharmacol Ther. 2000;68:435–442. doi: 10.1067/mcp.2000.110456. [DOI] [PubMed] [Google Scholar]
- 36.Serebruany VL., Glassman AH., Malinin AI., et al. Endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) platelet substudy. Circulation. 2003;108:939–944. doi: 10.1161/01.CIR.0000085163.21752.0A. [DOI] [PubMed] [Google Scholar]
- 37.Pollock BG., Laghrissi-Thode F., Wagner WR. Evaluation of platelet activation in depressed patients with ischemic heart disease after paroxetine or nortriptyline treatment. J Clin Psychopharmacol. 2000;20:137–140. doi: 10.1097/00004714-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Mohammad SF., Mason RG. Inhibition of human platelet-collagen adhesion reaction by amitriptyline and impramine. Proc Soc Exp Biol Med. 1974;145:1106–1113. doi: 10.3181/00379727-145-37962. [DOI] [PubMed] [Google Scholar]
- 39.Serebruany VL., Gurbel PA., O'Connor CM. Platelet inhibition by sertraline and N-desmethylsertraline: a possible missing link between depression, coronary events, and mortality benefits of selective serotonin reuptake inhibitors. Pharmacol Res. 2001;43:453–462. doi: 10.1006/phrs.2001.0817. [DOI] [PubMed] [Google Scholar]
- 40.Bondurant T., Darrell MJ., El Asyouty S., et al. Effect of fluoxetine on prothrombin time. Psychosomatics. 1998;39:296–298. doi: 10.1016/s0033-3182(98)71350-7. [DOI] [PubMed] [Google Scholar]
- 41.Alderman CP., Moritz CK., Ben-Tovim Dl. Abnormal platelet aggregation associated with fluoxetine therapy. Ann Pharmacother. 1992;26:1517–1519. doi: 10.1177/106002809202601205. [DOI] [PubMed] [Google Scholar]
- 42.De Maistre E., Allart C., Lecompte T., Bollaert PE. Severe bleeding associated with use of low molecular weight heparin and selective serotonin reuptake inhibitors. Am J Med. 2002;113:530–532. doi: 10.1016/s0002-9343(02)01239-1. [DOI] [PubMed] [Google Scholar]
- 43.Aranth J., Lindberg C. Bleeding, a side effect of fluoxetine. Am J Psychiatry. 1992;149:412. doi: 10.1176/ajp.149.3.412a. [DOI] [PubMed] [Google Scholar]
- 44.Leung M., Shore R. Fluvoxamine-associated bleeding. Can J Psychiatry. 1996;41:604–605. doi: 10.1177/070674379604100919. [DOI] [PubMed] [Google Scholar]
- 45.Ottervanger JP., Strieker BH., Huls J., Weeda JN. Bleeding attributed to the intake of paroxetine. Am J Psychiatry. 1994;151:781–782. doi: 10.1176/ajp.151.5.781. [DOI] [PubMed] [Google Scholar]
- 46.Evans TG., Buys SS., Rodgers GM. Acquired abnormalities of platelet function [letter]. N Engl J Med. 1991;324:1671. doi: 10.1056/NEJM199106063242313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Humphries JE., Wheby MS., Vandenberg SR. Fluoxetine and the bleeding time. Arch Pathol Lab Med. 1990;114:727–728. [PubMed] [Google Scholar]
- 48.Calhoun JW., Calhoun DD. Prolonged bleeding time in a patient treated with sertraline. Am J Psychiatry. 1996;153:443. doi: 10.1176/ajp.153.3.443a. [DOI] [PubMed] [Google Scholar]
- 49.Ceylan ME., Alpsan-Omay MH. Bleeding induced by SSRIs. Eur Psychiatry. 2005;20:570–571. doi: 10.1016/j.eurpsy.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 50.Tham CJ., Trew M., Brager N. Abnormal clotting and production of factor VIII inhibitor in a patient treated with venlafaxine. Can J Psychiatry. 1999;44:923–924. [PubMed] [Google Scholar]
- 51.Demet MM., Mizrak S., Esen-Danaci A. Mirtazapine-induced arthralgia and coagulopathy: a case report. J Clin Psychopharmacol. 2005;25:395–396. doi: 10.1097/01.jcp.0000169622.53066.5d. [DOI] [PubMed] [Google Scholar]
- 52.Hardy JL., Sirois A. Reduction of prothrombin and partial thromboplastin times with trazodone. CMAJ. 1986 15;135:1372. [PMC free article] [PubMed] [Google Scholar]
- 53.Tielens JA. Vitamin C for paroxetine - and fluvoxamine - associated bleeding. Am J Psychiatry. 1997; 154:883–884. doi: 10.1176/ajp.154.6.883b. [DOI] [PubMed] [Google Scholar]
- 54.Dalton SO., Johansen C., Mellemkjoer L., Norgard B., Sorensen HT., Olsen JH. Use of selective serotonin reuptake inhibitors and risk of upper gastrointestinal tract bleeding. Arch Intern Med. 2003;163:59–64. doi: 10.1001/archinte.163.1.59. [DOI] [PubMed] [Google Scholar]
- 55.de Abajo FJ., Garcia Rodriguez LA., Montera D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319:1106–1109. doi: 10.1136/bmj.319.7217.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Walraven C., Mamdani MM., Wells PS., Williams JL. Inhibition of serotonin reuptake by antidepressants and upper gastrointestinal bleeding in elderly patients: retrospective cohort study. BMJ. 2001;323:1–6. doi: 10.1136/bmj.323.7314.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pai VB., Kelly MW. Bruising associated with the use of fluoxetine. Ann Pharmacother. 1996;30:786–788. doi: 10.1177/106002809603000716. [DOI] [PubMed] [Google Scholar]
- 58.Layton D., Clark DW., Pearce GL., Shakir SA. Is there an association between selective serotonin reuptake inhibitors and risk of abnormal bleeding? Eur J Clin Pharmacol. 2001;57:167–176. doi: 10.1007/s002280100263. [DOI] [PubMed] [Google Scholar]
- 59.Meijer WE., Heerdink ER., Nolen WA., Herings RM., Leufkens HG., Egberts AC. Association of risk of abnormal bleeding with degree of serotonin reuptake inhibition by antidepressants. Arch Intern Med. 2004;164:2367–2370. doi: 10.1001/archinte.164.21.2367. [DOI] [PubMed] [Google Scholar]
- 60.Movig KL., Janssen MW., de Waal Malefijt J., Kabel PJ., Leufkens HG., Egberts AC. Relationship of serotonergic antidepressants and need for blood transfusion in orthopedic surgical patients. Arch Intern Med. 2003;163:2354–2358. doi: 10.1001/archinte.163.19.2354. [DOI] [PubMed] [Google Scholar]
- 61.Tata LJ., Fortun PJ., Hubbard RB., et al. Does concurrent prescription of selective serotonin reuptake inhibitors and non-steroidal anti-inflammatory drugs substantially increase the risk of upper gastrointestinal bleeding? Aliment Pharmacol Ther. 2005;22:175–181. doi: 10.1111/j.1365-2036.2005.02543.x. [DOI] [PubMed] [Google Scholar]
- 62.Tatsumi M., Groshan K., Blakely RD., Rîchelson E. Pharmacological profile of antidepressants and related compounds at human monoamine transporters. Eur J Pharmacol. 1997;340:249–258. doi: 10.1016/s0014-2999(97)01393-9. [DOI] [PubMed] [Google Scholar]
- 63.Richelson E. Pharmacology of antidepressants: clinical relevance of effects on neurotransmitter systems and their receptors. In: Den Boer JA, Westenberg HGM, eds. Antidepressants: Selectivity or Multiplicity. Amsterdam, the Netherlands: Benecke NI; 2001:43–60. [Google Scholar]
- 64.Nelva A., Guy C., Tardy-Poncet B., et al. . Syndromes hémorragiques sous antidépresseurs inhibiteurs sélectifs de la recapture de la serotonine (ISRS). A propos de sept cas et revue de la littérature. Rev Méd Interne. 2000;21:152–160. doi: 10.1016/s0248-8663(00)88244-2. [DOI] [PubMed] [Google Scholar]
- 65.Vandel P., Vandel S., Kantelip JP. SSRI-induced bleeding: two case reports. Thérapie. 2001;56:445–447. [PubMed] [Google Scholar]
- 66.Wilmhurst PT., Kumar AV. Subhyaloid haemorrhage with fluoxetine. Eye. 1996;10:141–50. doi: 10.1038/eye.1996.26. [DOI] [PubMed] [Google Scholar]
- 67.Gunzberger DW., Martinez D. Adverse vascular effects associated with fluoxetine. Am J Psychiatry. 1992;149:1751. doi: 10.1176/ajp.149.12.1751a. [DOI] [PubMed] [Google Scholar]
- 68.Yaryura-Tobias JA., Kirschen H., Niman P., Mosberg HJ. Fluoxetine and bleeding in obsessive-compulsive disorder. Am J Psychiatry. 1991;148:949. doi: 10.1176/ajp.148.7.949b. [DOI] [PubMed] [Google Scholar]
- 69.Mhanna MJ., Bennet JB., Izatt SD. Potential fluoxetine chloride (Prozac) toxicity in a newborn. Pediatrics. 1997;100:158–159. doi: 10.1542/peds.100.1.158. [DOI] [PubMed] [Google Scholar]
- 70.Smith M., Robinson D. Sertraline and vaginal bleeding: a possible association [letter]. J Am Geriatr Soc. 2002;50:200–201. doi: 10.1046/j.1532-5415.2002.50032.x. [DOI] [PubMed] [Google Scholar]
- 71.Lake MB., Birmaher B., Wassick S., Mathos K., Yelovich AK. Bleeding and selective serotonine reuptake inhibitors in childhood and adolescence. J Child Adolesc Psychopharmacol. 2000; 10:35–38. doi: 10.1089/cap.2000.10.35. [DOI] [PubMed] [Google Scholar]
- 72.Shen W., Swartz C., Calhoun J. Is inhibition of nitric oxide synthase a mechanism for SSRI-induced bleeding? [letter]. Psychosomatics. 1999;40:268–289. doi: 10.1016/S0033-3182(99)71248-X. [DOI] [PubMed] [Google Scholar]
- 73.Holzer L., Halfon O. Sertraline and gastrointestinal bleeding in an adolescent girl. J Child Adolesc Psychopharmacol. 2006;16:1–2. doi: 10.1089/cap.2006.16.1. [DOI] [PubMed] [Google Scholar]
- 74.Cooper TA., Valcour VG., Gibbons RB., O'Brien-Falls K. Spontaneous ecchymoses due to paroxetine administration. Am J Med. 1998;104:197–198. doi: 10.1016/s0002-9343(97)00399-9. [DOI] [PubMed] [Google Scholar]
- 75.Duijvestijn YC., Kalmeijer MD., Passier AL., Dahlem P., Smiers F. Neonatal intraventricular haemorrhage associated with maternal use of paroxetine. Br J Clin Pharmacol. 2003;56:581–582. doi: 10.1046/j.1365-2125.2003.01906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Berg C., Couturier F., Grass F., Aujoulat O., Guillard D., Stoeckel C. Saignements sous inhibiteurs spécifiques de la recapture de la sérotonine: à propos d'un cas clinique. Thérapie. 2001;56:65–67. [PubMed] [Google Scholar]
- 77.Kohn S., Labbate LA. Venlafaxine and ecchymoses. Can J Psychiatry. 1997;42:91. doi: 10.1177/070674379704200126. [DOI] [PubMed] [Google Scholar]
- 78.Linnebur SA., Saseen JJ., Pace WD. Venlafaxine-associated vaginal bleeding. Pharmacotherapy. 2002;22:652–655. doi: 10.1592/phco.22.8.652.33219. [DOI] [PubMed] [Google Scholar]
- 79.Rubell EB. Does imipramine (Tofranil) cause oral bleeding? Pediatrics. 1969;43:144–145. [PubMed] [Google Scholar]
- 80.Benazzi F. Hemorrhages during escitalopram- venlafaxine-mirtazapine combination treatment of depression. Can J Psychiatry. 2005;50:184. doi: 10.1177/070674370505000314. [DOI] [PubMed] [Google Scholar]
- 81.Dupont A., Fontana P., Bachelot-Loza C., et al. An intronic polymorphism in the PAR-1 gene is associated with platelet receptor density and the response to SFLLRN. Blood. 2003;101:1833–1840. doi: 10.1182/blood-2002-07-2149. [DOI] [PubMed] [Google Scholar]
- 82.Sewnath ME., van Hillegersberg R., Koopman MM., Levi MM., Gouma DJ. Increased perioperative blood loss during treatment with paroxetine. Ned Tijdschr Geneeskd. 2002;146:1800–1802. [PubMed] [Google Scholar]