Abstract
Racial and ethnic disparities in cardiovascular health care are well documented. Promising approaches to disparity reduction are increasingly described in literature published since 1995, but reports are fragmented by risk, condition, population, and setting. The authors conducted a systematic review of clinically oriented studies in communities of color that addressed hypertension, hyperlipidemia, physical inactivity, tobacco, and two major cardiovascular conditions, coronary artery disease and heart failure. Virtually no literature specifically addressed disparity reduction. The greatest focus has been African American populations, with relatively little work in Hispanic, Asian, and Native American populations. The authors found 62 interventions, 27 addressing hypertension, 9 lipids, 18 tobacco use, 8 physical inactivity, and 7 heart failure. Only 1 study specifically addressed postmyocardial infarction care. Data supporting the value of registries, multidisciplinary teams, and community outreach were found across several conditions. Interventions addressing care transitions, using telephonic outreach, and promoting medication access and adherence merit further exploration.
Keywords: cardiovascular disease, health disparities, interventions, quality improvement
Communities of color bear a disproportionate burden of ill health in the United States, with little improvement in overall mortality differentials during the past 40 years (R. S. Levine et al. 2001; Satcher et al. 2005). Cardiovascular disease accounts for 1.4 million deaths overall each year in the United States (Thom et al. 2006) and is the leading contributor to these differentials, with African Americans having two to three times the likelihood of dying from cardiovascular disease compared to whites at any given age (Mensah and Brown 2007).
These differentials in cardiovascular outcomes are thought to be partially attributable to disparities in cardiovascular disease prevention and treatment. Disparities in treatment are defined by the Institute of Medicine as ethnic/racial differences in treatment that are not justified by the underlying health conditions or treatment preferences of patients (Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care: Institute of Medicine 2002). Notable ethnic/racial disparities have been described in the diagnosis, management, and outcomes of many cardiac risk factors and conditions. Considerably less research has evaluated interventions designed to reduce those disparities. Fortunately, there is a growing literature describing interventions designed to improve care in communities of color. This later body of work may not directly address disparities reduction; however, interventions that are found to improve the health of patients of color may still prove valuable given the current situation in which African Americans and Hispanics receive poorer quality of care compared to whites for a broad range of core measures of health care quality (Agency for Healthcare Research and Quality 2006, fig. H1).
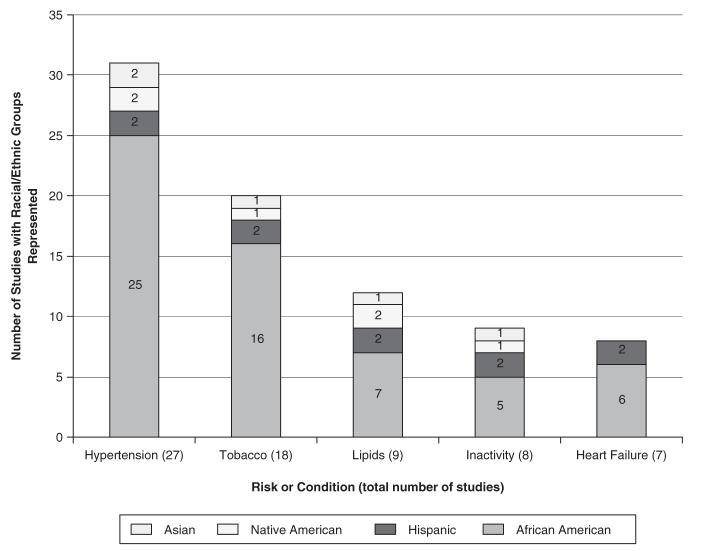
Figure 1.
Racial/Ethnic Representation in Studies
In the following section of this review, we briefly describe the disparities landscape for traditional vascular risk factors (hypertension, hyperlipidemia, physical inactivity, tobacco use) and for two cardiovascular conditions (coronary artery disease and heart failure [HF]) to provide the context for a systematic review of extant interventions.
Disparities in Vascular Risk Factors
It is important to realize that vascular risk factors vary in distribution by race, ethnicity, gender, and education, and this variation should influence the design and targeting of disparities reduction interventions (table 1). Hypertension in African Americans has earlier onset and greater prevalence, is harder to control, and is associated with far more end-organ damage (Bosworth et al. 2006; Gadegbeku, Lea, and Jamerson 2005). Fully half of the cardiovascular mortality disparity between whites and African Americans may be due to hypertension (Hicks et al. 2005; M. D. Wong et al. 2002), with African Americans having five times as many potentially preventable hospitalizations for hypertension compared to whites (Russo, Andrews, and Coffey 2006). Hypertension is also a great public health concern among other communities of color (Glover 2005; Ong et al. 2007; W. Wang et al. 2006).
Table 1.
Prevalence of Classical Vascular Risk Factors by Ethnicity/Race
| Risk Factor | White | African American | Mexican American/Hispanic | Native American | Asian Pacific Islander |
|---|---|---|---|---|---|
| Obesity (M/F)* | 30/31 | 31/51 | 29/39 | 33 | 6 |
| Hypertension for patients > 20 years of age (M/F)* | 33/32 | 43/47 | 29/31 | 24 | 16 |
| Prehypertension (F)† | 40 | 32 | 43 | 39 | — |
| Smoking prevalence (M/F)* | 24/20 | 24/17 | 19/11 | 37/29 | 18/5 |
| Diabetes: physician diagnosed (M/F)* | 7/6 | 11/13 | 11/11 | 16 | 8 |
| Prediabetes (M/F)* | 34/22 | 23/21 | 38/23 | — | — |
| Total cholesterol > 240 mg/dL (M/F)* | 16/18 | 45/42 | 16/14//26 | 26/29 | 27 |
| LDL cholesterol > 130 mg/dL (M/F)* | 32/34 | 32/30 | 39/31 | — | — |
| HDL cholesterol < 40 mg/dL (M/F)* | 26/9 | 16/7 | 34/15 | — | — |
| Physical inactivity (M/F)*‡ | 18/22 | 27/34 | 33/40 | 24/32 | 20/24 |
| Two or more cardiovascular risk factors§ | 35.5 | 48.7 | 39.6 | 46.7 | 25.9 |
| Treatment of both hypertension and lipids, where both present ∥ | 30.0 | 24.0 | 12.0 | — | — |
| Control of both hypertension and lipids, where both present ∥ | 11.0 | 6.5 | 0 | — | — |
| Metabolic syndrome (M/F)¶ | 35/39 | 20/35 | 43/52 | — | — |
Note: F = female; HDL = high-density lipoprotein; LDL = low-density lipoprotein; M = male.
Source:
Disparities in the prevalence and management of lipid abnormalities are also well described (Ma et al. 2005; Persell et al. 2005; Trivedi et al. 2005; M. L. Williams et al. 2002; Woodard, Kressin, and Petersen 2004). African Americans have lower rates of medication adherence and control relative to whites (Benner et al. 2002; L. T. Clark et al. 2006; Kaplan et al. 2004; M. L. Williams et al. 2002) even when insurance coverage is the same (Trivedi et al. 2006). Mexican Americans are less likely to be aware of or to be treated for dyslipidemia (Hertz, Unger, and Ferrario 2006).
Patterns of disparities in tobacco dependence differ from that of hypertension and hyperlipidemia. The prevalence of tobacco use in African Americans and whites is similar, with lower prevalence among Hispanic and Asian populations, but with smoking rates approaching 40%-50% in some populations of Native Americans and Alaskan natives. African Americans and Hispanics are less likely to be offered assistance with cessation (Houston et al. 2005; Lopez-Quintero, Crum, and Neumark 2006) and more likely to suffer higher rates of tobacco-related morbidity, including higher rates of lung cancer.
Physical inactivity is most prevalent in Hispanic and African American populations, especially among females. Differential rates of inactivity begin to manifest in childhood and widen during adolescence (Kimm et al. 2002), with pregnancy, tobacco use, and greater degrees of obesity further associated with inactivity (Genkinger et al. 2006). Overviews of correlates of physical inactivity in underserved populations have recently been published (Coble and Rhodes 2006; Yancey, Ory, and Davis 2006).
Differentials in Coronary Disease Procedures and Therapies
Differentials in the prevalence of cardiovascular conditions across racial and ethnic groups (table 2) might be attributed mainly to risk factor variation (Hozawa et al. 2007). However, the breadth and degree of racial and ethnic variations in access, management, and outcomes of established cardiovascular disease goes beyond that which can be explained by risk factor variation alone (Kindig and Thompson 2003; Mayberry, Mili, and Ofili 2000). Procedural differentials have been documented for nearly every area of cardiac diagnosis and care (Allison et al. 1996; Gauri et al. 2006; Hannan et al. 1999; Mickelson, Blum, and Geraci 1997; Peterson et al. 1994; Peterson et al. 1997; Pezzin, Keyl, and Green 2007; Schulman et al. 1999; K. A. Williams and Pokharna 2001; Yarzebski et al. 2004). Differentials in care persist even when the clinical appropriateness of the cardiac procedure (Epstein et al. 2003; Rathore et al. 2004; Vaccarino et al. 2005), socioeconomic status, and/or insurance are accounted for in analyses. As a related issue, communities of color tend to lag behind as new therapies are introduced (NCHS 2006; Sonel et al. 2005). Patient preference probably explains relatively little of the differentials in cardiac care (Gordon, Paterniti, and Wray 2004; Groeneveld et al. 2006; Kressin et al. 2004; Redberg 2005; Whittle et al. 1997).
Table 2.
Prevalence and Incidence of Vascular Conditions by Ethnicity/Race
| Condition | White | African American | Mexican American/Hispanic | Native American | Asian Pacific Islander |
|---|---|---|---|---|---|
| Cardiovascular disease, myocardial infarction or angina, %* | 6.2 | 6.2 | 6.9 | 11.2 | 4.7 |
| Coronary heart disease > 20 years of age (M/F), %† | 9.4/6.0 | 7.1/7.8 | 5.6/5.3 | 7.6 (18+) | 4.2 (18+) |
| Subclinical coronary artery calcification, %‡ | 70/45 | 52/37 | 57/35 | 59/42 | — |
| Congestive heart failure (M/F), %† | 2.8/2.1 | 2.7/3.3 | 2.1/1.9 | — | — |
| Stroke, years of potential life lost from stroke before age 75§ | 173.7 | 475.3 | 195.5 | 202.6 | 187.4 |
| Peripheral arterial disease in diabetes, %∥ | 8.5 | 9.5 | 5.0 | — | 6.4 |
| ESRD incidence (age- and sex-adjusted rates), per million¶ | 262 | 1,009 | — | 537 | 364 |
| Sudden cardiac death (M/F), per 100,000** | 205/138 | 207/141 | 119/147 | 133/77 | 112/67 |
| Premature (<65 years of age) cardiovascular mortality, % of deaths from heart disease^ | 14.7 | 31.5 | 23.5 | 36.0 | 21.1 |
Note: ESRD = end-stage renal disease; F = female; M = male.
Source:
Differences in residence and access to higher quality specialists (Ayanian et al. 2002; Fiscella and Franks 2006; Grimshaw et al. 2005; Konety, Vaughan Sarrazin, and Rosenthal 2005; LaVeist et al. 2003; Mehta et al. 2006) and health care organizations (Angelelli, Grabowski, and Mor 2006; Bach et al. 2004; Barnato et al. 2005; Doescher et al. 2001; Kressin 2005; Liu et al. 2006; Tonne et al. 2005; D. R. Williams and Collins 2001) are likely contributors to cardiac disparities. African Americans and Hispanics appear to receive vascular care at health care organizations that perform a lower volume of procedures and have higher risk-adjusted mortality after coronary artery bypass graft surgery (Trivedi, Sequist, and Ayanian 2006) and acute myocardial infarction (MI; Skinner et al. 2005).
Mortality and morbidity gaps appear to widen further in studies that look at longterm cardiovascular outcomes after hospitalizations or procedures (Bhandari et al. 2005; Chen et al. 2005; Horner et al. 2003; Konety, Vaughan Sarrazin, and Rosenthal 2005; Skinner et al. 2005; Spertus et al. 2005). This may be due, in part, to the fact that African Americans and Hispanics are 10%-40% less likely to receive outpatient secondary prevention therapies for cardiovascular disease (Ajani et al. 2006; Brown, Shepard, et al. 2005; Rathore et al. 2004; E. C. Schneider, Zaslavsky, and Epstein 2002; Virnig et al. 2002). Financial barriers are also much more likely in African American and Hispanic cardiac patients and are strongly associated with persistent angina and rehospitalization (Rahimi et al. 2007).
Disparities in HF
HF is the leading cause of medical admission in the Medicare population, and HF admission occurs significantly more in African Americans than whites, though the higher prevalence in African Americans is less clearly attributable to race once hypertension and other risk factors are controlled for (Brown, Haldeman, et al. 2005; He et al. 2001). Mortality after HF admission appears to be equal or lower in African Americans relative to whites (Agoston et al. 2004; Deswal et al. 2004; Thomas et al. 2005). However, once advanced left ventricular dysfunction develops, mortality in African Americans may be greater (Dries et al. 1999), and functional limitation in survivors appears relatively greater in African Americans (Vaccarino et al. 2002).
Nationally, inpatient quality of HF care appears similar between blacks and whites in some (Lafata et al. 2004; Rathore et al. 2003) but not all studies (Ahmed et al. 2003; Ayanian et al. 1999). When considering disparities in HF care, it is important to realize that the current understanding of the optimal treatment for HF for communities of color is evolving (Dries et al. 2002; Kahn and Sankar 2006; A. L. Taylor et al. 2004; Yancy et al. 2001).
New Contribution
The overall impression left by the preceding literature is that disparities in the quality of cardiovascular care exist, and they may partially explain disparities in cardiovascular outcomes. Disparities in cardiovascular care for communities of color have been attributed to factors such as limited access to care, limited health literacy, and education (Daumit et al. 1999; Fiscella and Franks 2004; Parker, Ratzan, and Lurie 2003; Sudore et al. 2006), delays in seeking cardiac care (Moser et al. 2006), inadequate cultural competency of providers (T. Fisher et al. 2007 [this issue]; R. L. Johnson et al. 2004; S. L. Taylor and Lurie 2004), provider stereotyping of communities of color (van Ryn et al. 2006), mistrust of the health care system by patients of color (Armstrong et al. 2006; Call et al. 2006; Jacobs et al. 2006; Price et al. 2005; Ranjit et al. 2007), and racism of providers (Fiscella and Williams 2004; Wyatt et al. 2003). Such factors are thought to operate synergistically (Mehta et al. 2006; D. R. Williams 2005).
While the preceding discussion might temper expectations of success, there is, in fact, a great deal of research that has been devoted to evaluating cardiovascular interventions for communities of color in the past decade, and some of this work has begun to bear fruit. The results of these interventions are often scattered in the cardiology, prevention, public health, and general medicine literature and typically are limited to a single cardiac risk factor or condition. A comprehensive review that brings together these interventions may help to identify flaws in the design of current studies, illustrate what risk factors and conditions have received limited attention, identify interventions that have shown particular promise, and provide direction for future research.
We set out to conduct such a review and bring together interventions addressing risk factor control (i.e., hypertension, hyperlipidemia, physical inactivity, tobacco use) and management of representative cardiovascular conditions (i.e., coronary artery disease and HF). We consider interventions specifically designed to reduce racial/ethnic disparities in care but also consider interventions designed simply to improve care in populations of color. We organize interventions by risk factors/conditions but also by the target of intervention (e.g., patient vs. provider/health care organization) using the conceptual model described earlier in the supplement (Chin et al. 2007 [this issue]).
Method of Literature Search, Quality Rating, and Abstraction
We searched multiple electronic databases (MEDLINE, the Cochrane Register of Controlled Trials, EMBASE, EPOC, Research and Developments Resource Base in CME, CINAHL) for evaluation studies of interventions published from 1995 to 2006 and designed to improve delivery of care addressing hypertension, lipid abnormalities, tobacco use, sedentary behavior, coronary artery disease, and HF for adult patients of color. Patients of communities of color were either the focus of studies, representing more than 50% of study subjects, or subgroups of larger trials, where data for ethnic/racial subgroups were specifically described. We required that interventions be based in North America and have a connection with a health care setting.
For the MEDLINE search, we used prespecified Medical Subject Headings (MeSH) and keywords to identify evaluation studies (Evaluation Studies, Clinical Trials [PT]) designed to address health care delivery (Health Services Accessibility, Delivery of Health Care, Integrated; Quality of Health Care) among communities of color (African Continental Ancestry Group; African Americans; Hispanic Americans; Mexican Americans; Indians, North American; Inuits; Asian Americans). This common search was systematically combined with searches using MeSH terms for each of the cardiac conditions—heart failure (Heart Failure, Congestive) and coronary artery disease (Myocardial Ischemia, Coronary Arteriosclerosis, Myocardial Revascularization, Coronary Artery Bypass)—and their related risk factors of smoking cessation (Tobacco Use Cessation, Smoking Cessation), sedentary behavior (Exercise), hypertension (Hypertension), and hyperlipidemia (Cholesterol). This generated six separate electronic searches. The details of non-MEDLINE searches are available by request.
We supplemented the search with a hand search of the past 2 years of issues from selected journals with a high likelihood of publishing interventions related to cardiovascular health (Academic Medicine, American Journal of Preventive Medicine, Archives of Pediatrics and Adolescent Health, Circulation, Ethnicity & Disease, Health Services Research, Journal of the American Medical Association, Journal of General Internal Medicine, Journal of Health Care for the Poor and Underserved, Journal of Transcultural Nursing, Medical Care, Milbank Quarterly, and New England Journal of Medicine). The hand search also included an examination of reference lists from initially identified trials and recent review articles on the topic of health disparities. The hand search was coordinated among all five authors.
We excluded reported interventions that were not connected to health care organizations, such as schools and churches, but did include community interventions with nurses and community health workers when they incorporated some degree of formal medical collaboration. We integrated multiple study designs including time series studies, before/after studies, nontraditional comparison studies, and controlled trials. The results of the initial electronic search and hand search for all six conditions identified 5,943 articles. Two authors independently reviewed the identified articles for possible inclusion; disagreements were resolved by consensus. A total of 382 studies met our initial inclusion criteria based on information in abstracts. After further review of full-length manuscripts, 62 studies were identified that met all inclusion criteria.
Data abstraction was conducted by four of the reviewers. All reviewers were given formal instruction on data abstraction. Using an abstraction form adapted from Zaza and colleagues (2000), we collected information on intervention characteristics, patient demographics, outcomes, results, and study duration. For each search we focused on specific processes of care of interest and documented baseline and follow-up. Studies were also rated on their quality, using a scale of study quality developed by Downs and Black (1998), intended for use with randomized and nonrandomized intervention studies. We utilized the first 26 criteria for this scale, which gave a maximum score of 27.
Results
Interventions to Reduce Racial and Ethnic Disparities
Interventions can be grouped in a number of different ways, including by mechanism, clinical setting, scope of intervention, specific vascular disease or risk factor, racial or ethnic group, and methodological parameters and quality (Committee on Quality Health Care in America: Institute of Medicine 2001; Horner et al. 2004; Kressin 2005; Matson Koffman et al. 2005; D. R. Williams and Neighbors 2001).
We grouped interventions by the vascular risk or condition they address and by the predominant target of the intervention: patient and family, provider and health care organizations, or multitarget interventions. We found 62 interventions in all, 27 addressing hypertension, 9 hyperlipidemia, 18 tobacco use, 8 physical inactivity, 1 post-MI care, and 7 HF, with some interventions addressing multiple targets (see figure 1).
Hypertension Results
Patient and family interventions in hypertension
Of the 27 intervention studies concerning hypertension (table 3), 9 were focused on the behavior of patients or families, and these addressed nonpharmacologic approaches to hypertension including salt restriction (5), diet (2), exercise (1), and stress reduction (1), with some studies addressing multiple approaches. The Trial of Nonpharmacologic Interventions in the Elderly (TONE) evaluated the impact of a 4-month educational program led by a dietician among patients with hypertension under fair control on one medication. The intervention led to improvements in blood pressure (BP) with a reduction in the proportion of patients with average BP more than 150/90 mm Hg (59% of the intervention group compared to 73% of the control group; Appel et al. 2001).
Table 3.
Hypertension
| Reference | Design | Intervention | n, Follow-Up, Racial/Ethnic Composition | Setting | Results: Process and Patient Outcomes | Conclusion | Target | Quality Score |
|---|---|---|---|---|---|---|---|---|
| Ahluwalia 1996 | RCT | Reminder postcards sent to hypertensive patients | n = 107, 6 months, 95% AA | Urban hospital-based walk-in clinic | 45% in postcard group and 47% of controls followed up in 10 days (p = .93) | Follow-up in severe hypertensives was poor, and a mailed postcard reminder had no effect in a walk-in setting | Provider & care delivery | 16 |
| Appel 2001 | RCT | TONE: reduced Na intervention; initial individual session with dietician, 4-month intensive phase with weekly group meetings, 3-month extended phase with biweekly meetings, and a maintenance phase; periodic individual sessions | n = 681, 28 months, 23% AA in subgroup analysis | 1 of 4 TONE Clinical Centers | Primary outcome: 59% of reduced Na vs. 73% controls had BP > 150/90 (relative hazard ratio = 0.68); in AAs, the relative hazard ratio was 0.56 | A reduced Na intake is a broadly effective, nonpharmacologic therapy that can lower BP and control HTN in older individuals | Patient/family | 20 |
| Ard 2000 | Randomized modified crossover | Diet and exercise program included 1,000 kcal diet, culturally sensitive recipes, and address of exercise attitudes | n = 56, 8 weeks, 100% AA | Academic health center | Average weight loss 14.8 lb; BMI: 37.8 to 35.3 (p < .01); total cholesterol: 199 to 185 (p < .01); SBP and DBP decreased by 4.3 (p < .01), and 2.4 (p < .05); control group: no significant change | A culturally sensitive diet and exercise intervention can reduce BMI, cholesterol, and BP | Patient/family | 12 |
| Artinian 2001 | RCT | Nurse-managed HT plus usual care or nurse-managed CBM or usual care | n = 26, 3 months, 100% AA | Family community center in urban setting | HT and CBM group had significant drops (HT > CBM) in SBP and DBP at 3 months (p < .05); little change in usual-care group | Nurse case management and home/community monitoring can reduce BP | Provider & care delivery | 17 |
| Becker 2005 | RCT | Community-based multiple risk factor intervention on CV risk in black families with a history of premature coronary disease; CBC group received NP-led, community-based multicomponent education and management intervention compared to EPC | n = 364, 1 year, 100% AA | Primary care and nonclinical community sites | CBC group was two times more likely to achieve goal levels of LDL cholesterol and BP compared with the EPC group (95% CI: 1.11 to 4.20 and 1.39 to 3.88, respectively) | Multifaceted NP-directed community-based intervention can improve HTN, lipids, and tobacco cessation rates in a high-risk population | Provider & care delivery | 18 |
| Chisolm 2002 | RCT | Clinical pharmacist performing patient medication reviews, with emphasis on preventing or resolving medication-related problems and providing medication recommendations | n = 23, 1 year, 100% AA | Academic renal transplant clinic | Mean SBP significantly lower in the intervention group at second (138 vs. 169), third (136 vs. 165), and fourth (145 vs. 176) quarters of study (p < .05); mean DBP lower in intervention group at second (76 vs. 85) and fourth quarters of study (p < .05) | Pharmacist medication review and instruction improved BP control in renal transplant patients | Provider & care delivery | 21 |
| Erickson 1997 | RCT | Pharmacist preclinic counseling on HTN, drug and nondrug management, compliance, and recommendations to MD | n = 80, 5 months, 89% AA | Urban university-affiliated internal medicine clinic | Significant improvement in SBP 157 to 145 in intervention group only (p = .001); SF-36 physical functioning domain (p = .03) in intervention group without change in HTN-specific scale | Pharmacist education improved BP control in this setting | Provider & care delivery | 19 |
| Fedder 2003 | Retrospective comparison study | CHW impact on health care utilization of patients with DM with/without HTN | n = 117, 1 year, 100% AA | Urban Medicaid population | At 2 years, ER admissions decreased 53% (p = .02) | CHW-implemented HTN treatment program decreased emergency room use | Provider & care delivery | 10 |
| Haskell 2006 | RCT | Multifaceted disease management intervention using team case management | n = 148, 1 year, 89% minority (57% Hispanic, 11% Asian, 7% AA) | Urban community clinics serving low-income patients | Disease management produced clinically important decreases in selected risk factors compared with usual care, including systolic BP (p < .01) and LDL cholesterol (p < .03) | Disease management targeted at high-risk patients (24% had CAD, 64% had no health insurance) can improve HTN and lipids | Provider & care delivery | 21 |
| Hill 1999 | RCT | Nurse-CHW special (SI) educational-behavioral intervention, individualized counseling, monthly phone calls, home visit | n = 204, 12 months, 100% AA | Home and outpatient clinic at academic medical center | No significant differences in BP control | Nurse and CHW care consisting of multifaceted intervention did not improve BP control | Provider & care delivery | 18 |
| Hill 2003; Dennison 2007 | RCT | NP/CHW/MD educational-behavioral-pharmacologic vs. less intensive education referral | n = 309, 36 months, 100% AA | Home and outpatient clinic at academic medical center | At 36 months, SBP/DBP: -7.5/-10.1 (more intensive) vs. +3.4/-3.7 (less intensive), p = .001 and p = .005, respectively; LVM lower 274 g (more intensive) vs. 311 g (less intensive) (p = .004) | Combined nurse, CHW, MD behavioral pharmacological intervention improved BP control | Provider & care delivery | 21 |
| Jenkins 2006 | Pre/post study | General CV disease quality improvement | n = 2,860, 1 year 48% AA with subgroup analysis | Academic family practice clinic | Significant improvements occurred in BP control for all adults (OR = 1.44) and those with HTN (OR = 1.82); measures of total cholesterol (OR = 1.10) and HDL cholesterol (OR = 1.27) for all patients | Multifaceted intervention can improve process measures and CV outcomes | Provider & care delivery | 17 |
| Kokkinos 1995 | RCT | Moderate-intensity exercise plus BP medication or BP medication alone | n = 46, 32 weeks, 100% AA | Not mentioned | At 16 weeks, mean DBP decreased in exercise group (88 to 83 mm Hg) and increased in nonexercise group (88 to 90 mm Hg) (p = .002) | Effectiveness of moderately intense exercise extends to patients with severe HTN | Patient/family | 18 |
| Krieger 1999 | RCT | Enhanced tracking and follow-up services provided by CHWs to promote medical follow-up of persons with elevate BP | n = 421, 3 months, 79% AA | Urban community-based clinics | Follow-up visits were completed by 65.1% of intervention group vs. 46.7% of those in the usual-care group (p = .001) | Enhanced tracking and follow-up services by CHW improved compliance with follow-up visits | Provider & care delivery | 17 |
| Kumanyika 1999 | RCT | Nutrition program using food cards, audiotapes, and four classes vs. cards and nutrition guide | n = 255, 1 year, 100% AA | Community-based clinic affiliated with an academic medical center | Trend toward improvement but no significant difference in lipids and BP | Intensive nutrition intervention may improve lipid and BP control | Patient/family | 18 |
| Lenz 2004 | Comparative study, 2-year follow-up of RCT | NP-run or physician-run primary care practice | n = 406, 2 years, 93% Hispanic | Urban ambulatory primary care clinic | No statistically significant difference in SBP or DBP for NP vs. MD patients at 2-year follow-up | No difference between care provided by NPs and MDs | Provider & care delivery | 17 |
| Levine 2003 | RCT | Nurse-supervised indigenous CHWs deliver intervention with two different intensity levels to reduce BP | n = 817, 40 months, 100% AA | Urban community clinics | Singinficant decrease in SBP/DBP in both levels of intervention (p < 0.05); significant increase in the percentage with controlled high BP | Nurse-supervised CHW intervention in urban setting improved BP control | Provider & care delivery | 17 |
| Rogers 2001 | RCT | Home BP monitoring service and electronic reports provided weekly to the PCP and patient | n = 121, 11 weeks, 12.3% AA with subgroup analysis | University-affiliated primary care clinics | Among AA patients, MAP decreased by 9.6 mm Hg with home service and increased by 5.25 mm Hg in usual care (p = .047) | Telecommunication service was efficacious in reducing the mean arterial pressure of patients with established HTN | Provider & care delivery | 19 |
| Sanders 2002 | RCT | Chart-based reminder system for patients with HTN and DM | n = 320, 55% AA | Primary care practice of a Veterans Affairs Medical Center | Only 33% of visits resulted in medication change, although BP greater than guideline in 93% of patients | Chart reminder failed to improve MD compliance with the clinical guideline for HTN management in diabetics | Provider & care delivery | 17 |
| Schneider 2005 | RCT | TM vs. PMR vs. HE | n = 150, 1 year 100% AA | Urban community health center | TM group showed decreased BP 3-5 mm Hg and reduced BP medication relative to PMR (p = .001) and HE (p = .09) groups | A stress reduction approach, the Transcendental Mediation Program, may be useful as an adjunct in the treatment of HTN | Patient/family | 18 |
| Svetkey 1999; Bray 2004 | RCT | DASH: randomized controlled feeding study of (1) a diet rich in fruits and vegetables or (2) combination diet rich in fruits, vegetables, and low-fat dairy foods and reduced in saturated fat, total fat, and cholesterol (the DASH combination diet); weight and salt intake were held constant | n = 459, 8 weeks, 60% AA, 6% other minorities | Four academic medical centers | Combination diet: lowered SBP in all subgroups (p < .008), lowered DBP (p < .01) in all but two subgroups; combination diet lowered SBP significantly more in AA (6.8 mm Hg) than whites (3.0 mm Hg) | DASH combination diet may be an effective strategy for preventing and treating HTN in a broad cross-section of the population | Patient/family | 21 |
| Svetkey 2005; Appel 2003; Elmer 2006 | RCT | PREMIER, comprehensive lifestyle on diet, weight, lipids, BP; advice only vs. weight, exercise, EtOH, Na+ (established), vs. est + DASH | n = 810, 18 months, 34% AA with subgroup analysis | Four clinical centers | 18-month follow-up: diet and weight changed, BP marginally so; optimal BP 19% advice only, 30% in est, 35% in est + DASH | DASH modest supplemental help to established interventions; less of an effect with home meal preparation; BP effects greater in patients > 50; AA males and white males most responsive, AA females least | Patient/family | 22 |
| Tao 2003 | Pre/post study | Multidisciplinary HTN clinic: MDs, nurses, pharmacists, and nutritionists assessed and reinforced objectives tailored to individual needs | n = 50, 6 months, 94% AA | Public hospital-based clinic | 58% of patients achieved target BP at 6 months but 22% were lost to follow-up | Multidisciplinary clinic can improve BP control in patients with resistant HTN, at least for the short term | Provider & care delivery | 11 |
| Tobe 2006 | RCT | Home care nurse treatment using predefined HTN algorithm compared to RN home care visits (monitoring only) with MD treatment decisions | n = 95, 12 months, 100% Native American with DM and HTN | Home | SBP down 24 vs. 13.5 in control; albumin excretion no change | Home care nurse monitoring significantly improves SBP; algorithm-driven treatment by RNs provides additional DBP improvement | Provider & care delivery | 21 |
| TOHP Phase I and Phase II 1992, 1997; Kumanyika 2005 | RCT | Telephone-delivered dietary and behavioral change program led by dietitians, psychologists, and health conselors focused reducing Na intake | n = 2,382, 36 months, 18% AA with subgroup analysis | Nine academic medical centers | At 36 months I > C (weight loss, 1.3/0.9 mm Hg; Na reduction, 1.2/0.7 mm Hg; combined, 1.1/0.6 mm Hg) (p < .001), 21% Na reduction participants achieved the targeted level of Na excretion below 80 mmol/24 hr; no variation by race | Through 48 months, the incidence of HTN (140/90) was significantly less in each active intervention group than the usual-care group (average relative risks, 0.78-0.82); modest results with highly motivated and extensively counseled individuals; Na reduction sufficient to help population will be difficult to achieve without food supply changes | Patient/family | 18 |
| Vivian 2002 | RCT | Monthly meetings with a clinical pharmacist who changed drugs, adjusted doses, provided drug counseling, compared to usual MD care | n = 56, 6 months, 77% AA | Veterans Affairs Medical Center | BP < 140/90 attained in 81% of intervention group and 30% in usual care; patient satisfaction and adherence similar | Monthly pharmacist meeting with medication changes and dose adjustment improve BP control | Provider & care delivery | 20 |
| Walker 2000 | RCT | Programmed telephone calls with HTN messages | n = 83, 3 months, 100% AA | Home and outpatient clinic at an academic medical center | No significant improvements in HTN knowledge; SBP and DBP declined for both HTN and control (spiritual messages) | Programmed telephone calls do not improve HTN knowledge or medication adherence | Patient/family | 13 |
Note: AA = African American; BMI = body mass index; BP = blood pressure; C = control; CAD = coronary artery disease; CBC = community-based care; CBM = community-based monitoring; CHW = community health worker; CV = cardiovascular; DASH = Dietary Approaches to Stop Hypertension; DBP = diastolic blood pressure; DM = diabetes mellitus; EPC = enhanced primary care; ER = emergency room; HE = health education; HT = home telemonitoring; HTN = hypertension; I = intervention; LVM = left ventricular mass; MAP = mean arterial pressure; MD = medical doctor; Na = sodium; NP = nurse practitioner; PCP = primary care provider; PMR = progressive muscle relaxation; RCT = randomized controlled trial; RN = registered nurse; SBP = systolic blood pressure; SF = short form; TM = transcendental meditation; TOHP = Trials of Hypertension Prevention; TONE = Trial of Non-Pharmacologic Intervention in the Elderly.
The Trials of Hypertension Prevention (TOHP) studies of the 1990s explored multidisciplinary interventions on the diet and behavior of patients with diastolic BP of 80-89, with the involvement of dietitians, psychologists, and health counselors. Salt restriction, weight loss, and stress reduction were emphasized. At 36 months systolic pressure fell about 2 to 3 points in the diet and salt intervention groups (salt restriction alone, weight loss alone, and both combined). The incidence of formally diagnosed hypertension (>140/90) was significantly lower in the intervention groups (Stevens et al. 1993; TOHP 1992; TOHP2 1997), but in a later phase in a single center, only 21% of participants were able to achieve the target salt reduction (Kumanyika et al. 2005).
The Dietary Approaches to Stop Hypertension (DASH) diet held sodium and weight constant while testing a low-fat diet rich in fruits and vegetables in a hypertensive population (Appel et al. 1997). This intervention diet resulted in a daily intake of potassium nearly 3 g higher than in the control diet. This combination study diet was significantly more effective in the study’s 275 African American patients than for other ethnic/racial groups, reducing systolic BP by nearly 6.8 mm Hg (Svetkey et al. 1999). In a subsequent DASH-Sodium subgroup analysis, salt restriction was found to be especially effective in African American women (Bray et al. 2004). The PREMIER trial has been reported in several articles (Appel et al. 2003; Elmer et al. 2006; Svetkey et al. 2005) and compared a comprehensive lifestyle approach to established risk factors (weight, salt, alcohol, and exercise) to an intervention that added DASH diet counseling. It is important to note that the DASH diet was prepared in a research kitchen, while the PREMIER trial diet was prepared by patients in their homes. The PREMIER intervention marginally affected BP, with optimal BP achieved in 30% of those who received counseling that addressed established risk factors compared to 35% of those receiving this counseling plus the DASH diet counseling. Ard and colleagues studied a 1,000 kcal diet based on culturally targeted (T. Fisher et al. 2007) recipes, recipes that might appeal to the practices of African Americans, and found a 4-point fall in systolic pressure after 8 weeks (Ard, Rosati, and Oddone 2000), while a food card, audiotape, and group class approach did not significantly improve either BP or lipids (Kumanyika et al. 1999). Programmed telephone messages designed to improve hypertension knowledge and medication adherence also had no effect (Walker 2000).
R. H. Schneider and colleagues (1995) compared the effect of transcendental meditation in 127 African Americans with hypertension receiving care at an urban community health center. After a 3-month intervention, systolic BP fell about 5 points, and meditation patients had reduced requirements for BP medication relative to those in two control groups, one receiving progressive muscle relaxation and another receiving simple health education. Other studies have not supported an association between stress reduction and BP control (TOHP 1992).
Kokkinos and colleagues (1995) compared a program of moderate-intensity exercise combined with BP medication and a program of BP medication alone in 46 African American men followed for 16 weeks and demonstrated a 5-point improvement in diastolic BP.
In summary, for patient and family interventions, (1) sodium restriction yields important benefits, especially in African Americans, at least with use of study diets; (2) less evidence is available for the benefits of exercise, weight loss, and psychosocial interventions.
Provider and care delivery interventions in hypertension
Provider and care delivery interventions for hypertension have received more research attention than patient interventions. We found 18 interventions, many with overlapping multidisciplinary approaches in their design, including community-level components. The studies explored patient outreach (4), clinic reorganization (3), nurse interventions alone or in collaboration with community health workers (8), and pharmacist interventions (4). General clinic outreach produced mixed results. A postcard strategy was unsuccessful in encouraging follow-up appointments in an urban walk-in clinic (Ahluwalia, McNagny, and Kanuru 1996). By contrast, enhanced tracking and follow-up services by community health workers in 421 low-income patients (79% African American) improved clinic attendance from 47% to 65% compared to usual care (Krieger et al. 1999). Fedder and colleagues (2003) demonstrated a 50% reduction in emergency room visits after employing community health workers to work with a group of diabetic hypertensive patients. A small subgroup analysis in African Americans found a 9.6-mm Hg BP reduction associated with a home telephonic BP monitoring service that generated weekly electronic reports to the primary care physician and patient (Rogers et al. 2001).
Among health care organization interventions, chart-based reminders failed to improve physician adherence to hypertension guidelines in a Veterans Administration setting (Sanders and Satyvavolu 2002), while overall organizational change in a clinic’s approach to hypertension appeared to produce significant improvements in BP control in two other studies. In the first clinic reorganization study, a clinicwide program focused on improving the quality of care processes in cardiovascular disease was successful in an academic family practice clinic in the southeastern United States, for both white and African American patients (Jenkins et al. 2006). Likewise, a multidisciplinary intervention in the hypertension clinic of an urban public hospital provided individual therapeutic tailoring with doctors, pharmacists, nurses, and nutritionists. At 6 months 58% of patients achieved target BP, but sustaining the intervention proved challenging in this “safety-net” setting, with nearly a quarter of patients lost to follow-up (Tao et al. 2003).
Eight interventions that utilized nursing personnel in care management had generally successful results (Artinian, Washington, and Templin 2001; Becker et al. 2005; Dennison et al. 2007; Haskell et al. 2006; Hill et al. 1999; Hill et al. 2003; Lenz et al. 2004; D. M. Levine et al. 2003; Tobe et al. 2006) with several of these combining nursing and community health personnel (Becker et al. 2005; Dennison et al. 2007; Hill et al. 1999; Hill et al. 2003; D. M. Levine et al. 2003). In a small pilot study of African American patients, a nurse telemonitoring program was compared to nurse-managed community-based monitoring with both interventions associated with 10-25-mm Hg improvements relative to usual care (Artinian, Washington, and Templin 2001). In a study addressing a Hispanic population, primary care patients were randomly assigned to either a nurse practitioner- or physician-managed practice in New York City. Equal outcomes in health status, physiologic measures, and patient satisfaction occurred for 2 years (Lenz et al. 2004). Hill and colleagues performed two studies specifically focused on urban, young African American men with hypertension. The first found no significant differences in BP control at 12 months (Hill et al. 1999). The second tested a nurse practitioner/community health worker/physician approach in 309 men followed for 4 years and showed a modest but significant improvement in BP control and a more robust improvement in left ventricular mass (Dennison et al. 2007; Hill et al. 2003). Nurses working with indigenous community health workers were also effective in improving BP control in one community academic health center partnership (D. M. Levine et al. 2003). A recent study used homecare nurses and predefined hypertension medication algorithms in 95 Canadian First Nation patients with both hypertension and diabetes. Systolic BP fell 24 points, though albumin excretion was not improved (Tobe et al. 2006).
Becker and colleagues (2005) and Haskell and colleagues (2006) both evaluated interventions designed to modify multiple cardiac risk factors. Becker and colleagues evaluated an intervention that deployed a nurse practitioner/community health worker in an attempt to address multiple cardiac risk factors in African American families with a history of premature coronary disease. Compared to enhanced primary care, community-based care resulted in a twofold better low-density lipoprotein (LDL) reduction and BP control and thus a substantial reduction in global coronary heart disease risk (Becker et al. 2005). Finally, Haskell and colleagues evaluated a multitarget intervention delivered by nurses and dieticians to a medically underserved, predominantly Hispanic population and demonstrated better BP and lipid control compared to a usual-care control population (Haskell et al. 2006).
The four pharmacist interventions varied in the degree to which pharmacists were involved in care. In addition to the study by Tao et al. discussed in the clinic reorganization section, a second study had pharmacy staff join residents in an internal medicine continuity clinic where they assessed side effects, patient beliefs, adherence, drug coverage, and hypertension knowledge. The authors demonstrated a 12-point drop in the intervention group, compared to 2 points in the control clinics (Erickson, Slaughter, and Halapy 1997). Vivian et al. reported a study from a Philadelphia Veterans Affairs program in which a pharmacist provided monthly counseling, drug changes, and dose adjustments. At the end of 6 months, 81% in the intervention group were controlled to <140/90 mm Hg compared to 30% of the physician usual-care group (Vivian 2002). Finally, a small study involving African American renal transplant patients demonstrated markedly better BP control when the clinical pharmacist was assigned to perform medication reviews and troubleshooting interactions and to provide recommendations (Chisholm et al. 2002).
In summary, (1) general clinic reorganization interventions appeared to produce promising results on BP control but were very few in number; (2) nurse-led interventions were common and produced beneficial effects on BP control; (3) pharmacist and community health worker interventions were generally effective, but the total number and size of studies were both small.
Hyperlipidemia Results
Patient and family interventions in lipids
Lipid interventions were the subject of nine studies, four of which focused on the patient and/or the family and five of which focused on the provider and/or the health care organization (table 4). Of the lipid interventions focused on the patient and/or family, two tested moderate-intensity aerobic exercise, one in African American men (Kokkinos et al. 1998) and another in 389 Mexican American women (Poston et al. 2001). Neither showed effects on lipid primary end points; attrition was high in the latter study, especially in younger and less educated women. Another trial explored diet in conjunction with increased activity. This randomized modified crossover trial of a 1,000 kcal diet with culturally tailored recipes and exercise attitude modification in African American patients demonstrated a modest drop in cholesterol from 199 to 185 mg/dL, with little change for controls (Ard, Rosati, and Oddone 2000). The remaining trial compared full instruction on cardiovascular nutrition to a self-help group and showed significant improvements in LDL cholesterol in both groups (Kumanyika et al. 1999).
Table 4.
Hyperlipidemia
| Reference | Design | Intervention | n, Follow-Up, Racial/Ethnic Composition | Setting | Results: Process and Patient Outcomes | Conclusion | Target | Quality Score |
|---|---|---|---|---|---|---|---|---|
| Ard 2000 | Randomized modified crossover | Diet and exercise program included 1,000 kcal diet, culturally sensitive recipes, and address of exercise attitudes | n = 56, 8 weeks, 100% AA | Academic health center | Average weight loss 14.8 lb; BMI: 37.8 to 35.3 (p < .01); total cholesterol: 199 to 185 (p < .01); SBP and DBP decreased by 4.3 (p < .01) and 2.4 (p < .05); control group: no significant change | A culturally sensitive diet and exercise intervention can reduce BMI, cholesterol, and BP | Patient/family | 12 |
| Becker 2005 | RCT | Community-based multiple risk factor intervention on CV risk in black families with a history of premature coronary disease; CBC group received NP-led, community-based multi-component education and management intervention compared to EPC | n = 364, 1 year, 100% AA | Primary care and nonclinical community sites | CBC group was two times more likely to achieve goal levels of LDL cholesterol and BP compared with the usual-care group (95% CI: 1.11 to 4.20 and 1.39 to 3.88, respectively) | Multifaceted NP-directed community-based intervention can improve HTN, lipids, and tobacco cessation rates in a high-risk population | Provider & care delivery | 18 |
| Burden 2002 | Pre/post study | Pharmacist-led lipid reduction with initial 1-hr visit and follow-up every 6 weeks until stable, then every 6-12 months; dietician visit; exercise encouraged | n = 74, 8 months, 100% Native Americans | Clinic at an Indian Health Services Hospital | 2.1 mg/dL increase in HDL (p = .01) | Pharmacist-directed lipid management resulted in modest improvement in HDL | Patient/family | 12 |
| Haskell 2006 | RCT | Multifaceted disease management intervention using team case management | n = 148, 1 year, 89% minority (57% Hispanic, 11% Asian, 7% AA) | Urban community clinics serving low-income patients | Disease management produced clinically important decreases in selected risk factors compared with usual care, including SBP (p < .01) and LDL cholesterol (p < .03) | Disease management targeted at high-risk patients (24% had CAD, 64% had no health insurance) can improve HTN and lipids | Provider & care delivery | 21 |
| Jenkins 2006 | Pre/post study | General CV disease quality improvement | n = 2,860, 1 year, 48% AA with subgroup analysis | Academic family practice clinic | Significant improvements occurred in BP control for all adults (OR = 1.44) and those with HTN (OR = 1.82); measures of total cholesterol (OR = 1.10) and HDL cholesterol (OR = 1.27) for all patients | Multifaceted intervention can improve process measures and CV outcomes | Provider & care delivery | 17 |
| Keyserling 1997 | RCT | 90-min tutorial, brief dietary assessment, and three 5-10-min diet counseling sessions by the primary care clinician; dietitian referral if LDL remained high at 4-month follow-up; clinician prompt to consider meds based on LDL at 7-months | n = 372, 7 months, 40% AA, 11% Native American | 21 rural and community health centers | 5.3 mg/dL greater reduction in total cholesterol for intervention group averaged over 1 year; increased rate of lipid medication use | Dietary intervention had minimal effect on lipid control in this low-income group | Provider & care delivery | 19 |
| Kokkinos 1998 | RCT | Moderate-intensity aerobic exercise for 20-50 min, 3 times/week for 16 weeks | n = 36, 16 weeks, 100% AA | Not mentioned | No change in lipids except HDL at 75% intensity (p = .003) | Low- to moderate-intensity aerobic exercise may not be enough to modify lipid profiles in patients with severe HTN, but increases in HDL suggest exercise intensity threshold | Provider & care delivery | 17 |
| Kumanyika 1999 | RCT | CV nutrition program using food cards, audiotapes, and four classes vs. cards and nutrition guide | n = 255, 1 year, 100% AA | Community-based clinic affiliated with an academic medical center | Trend toward improvement but no significant difference in lipids and BP | Intensive nutrition intervention may improve lipid and BP control | Provider & care delivery | 19 |
| Poston 2001 | RCT with block design | Culturally appropriate intervention: weekly 90-min meetings using individual-oriented, culturally tailored behavioral techniques and reading materials; wait-list control group did not receive intervention but were assessed at baseline and 6 and 12 months | n = 379, 12 months, 100% Mexican American women | Home and community centers | No difference in physical activity or cholesterol levels among the study participants; higher drop out rate in treatment group p < .001. | Culturally appropriate intevention consisting of weekly meetings, written materials, and behavioral techniques was not effective in increasing exercise or improving lipids in this challenging population | Patient/family | 19 |
Note: AA = African American; BMI = body mass index; BP = blood pressure; CAD = coronary artery disease; CBC = community-based care; CV = cardiovascular; DBP = diastolic blood pressure; EPC = enhanced primary care; HTN = hypertension; NP = nurse practitioner; SBP = systolic blood pressure.
Provider and health care organization interventions in lipids
Overall, five studies were identified, and these studies had mixed results. The first intervention asked primary care physicians to give 5- to 10-min dietary counseling sessions with referral to a local dietitian if the LDL cholesterol remained elevated and showed only modest short-term effects on cholesterol levels (Keyserling et al. 1997). In the second, a pharmacist intervention assessed a cardiovascular risk reduction program in a Native American population in New Mexico and demonstrated a statistically significant but clinically modest gain in HDL (Burden et al. 2002). The three remaining studies were multitarget cardiovascular risk factor interventions, all of which have been mentioned earlier in the section on hypertension, that successfully improved lipid levels (Becker et al. 2005; Haskell et al. 2006; Jenkins et al. 2006). The first intervention involved clinic reorganization (Jenkins et al. 2006), while the latter two involved nurses and or community health workers in care management (Becker et al. 2005; Haskell et al. 2006).
In summary, interventions designed to improve lipid levels in communities of color have had mixed results; however, several interventions intended to bring about overall improvements in cardiovascular risk factors via health care organization-level interventions or care management with nurses have successfully improved lipid levels.
Tobacco Results
In contrast to the literature on lipid lowering, studies specifically addressing tobacco use by communities of color were relatively common and of higher quality, with 13 of the 18 studies we identified being randomized controlled trials (table 5). Twelve of the studies evaluated interventions targeted at patients, all of which included counseling by a health care provider or health educator. Three studies targeted primarily health care provider behavior, and 3 studies were multicomponent, targeting both the patient and provider. In 14 studies African Americans made up the majority of the participants. Only 1 study had significant numbers of Hispanic participants, and only 1 study included Native Americans, despite their markedly higher prevalence of tobacco use relative to other racial and ethnic groups (table 1).
Table 5.
Tobacco Cessation
| Reference | Design | Intervention | n, Follow-Up, Racial/Ethnic Composition | Setting | Results: Process and Patient Outcomes | Conclusion | Target | Quality Score |
|---|---|---|---|---|---|---|---|---|
| Ahluwalia 1998 | RCT | Nicotine transdermal patch plus counseling vs. placebo | n = 410, 6 months, 100% AA smokers | Large urban hospital-based clinic | 6-month quit rates 17.1% with patch vs. 11.7% placebo; after adjustment, differences significant at 10 weeks (p = .04), but not at 6 months (p = .14) | Short-term quit rates are improved with the nicotine patch in AAs | Patient/family | 23 |
| Ahluwalia 1999 | RCT | Smoking as a vital sign stamp | n = 2,595, 4 months, 100% AA | Adult urban walk-in clinic | 78.4% intervention MDs vs. 45.6% control MDs asked about patient smoking; 39.9% intervention MDs advised quitting vs. 26.9% control MDs | Using smoking as a vital sign stamp; increased rates of asking, telling, and arranging follow-up for smoking cessation | Provider & care delivery | 22 |
| Allen 1998 | RCT | Tobacco cessation training session for residents | n (residents) = 158, 30% Asian, 45% AA, n (patients) = 1,086, 1 year, 100% AA | Public hospital-based clinic | No difference in quit rates at 1 year | Short focused educational intervention for providers is not adequate to increase quit rates | Provider & care delivery | 18 |
| Becker 2005 | RCT | Community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease; CBS group received NP-led, community-based multicomponent education and management intervention | n = 364, 1 year, 100% AA | Primary care and nonclinical community sites | The CBS group was two times more likely to achieve goal levels of LDL cholesterol and BP compared with the usual-care group (95% CI: 1.11 to 4.20 and 1.39 to 3.88, respectively) | Multifaceted NP-directed community-based intervention can improve HTN, lipids, and tobacco cessation rates in a high-risk population | Provider & care delivery | 18 |
| Curry 2003 | RCT | Motivational message from the child’s clinician, a guide, a 10-min motivational interview with a nurse or study interventionist, and up to three outreach phone counseling calls by interventionist in 3 months | n = 303, 1 year, 63% AA | 4 pediatric clinics serving an ethnically diverse low-income population | 1-year abstinence rates: 13.5% intervention vs. 6.9% control, adjusted OR = 2.77 | Pediatric clinic smoking cessation intervention has long-term benefits in socioeconomically disadvantaged sample of female smokers | Provider & care delivery | 20 |
| Davies 2005 | RCT | Bedside counseling format with follow-up contact postdischarge | n = 248, 6 months, 100% AA | Indident-care hospital | 40.0% intervention vs. 21.7% control patients progressed at least one stage in the transtheoretical model of change (p < .01) | Although this intervention did not show significant impact on cessation rates, it did increase smokers’ readiness to change their behavior | Provider & care delivery | 18 |
| Fisher 2005 | Pre/post study | Multidisciplinary committees developed participatory approaches to system change and promoted systematic implementation of smoking cessation interventions | n = 2 FQHCs intervention clinic with two comparison clinics; 2,600 and 3,900 patients overall in intervention clinics, mostly AA | Community health clinics and community | Documentation of smoking status or readiness to quit increased from 2% to 94%; rates advice to quit and providers offering assistance with quitting increased to 80%; quit rates not reported | Participatory, multidisciplinary approaches to systematically implement evidenced-based smoking cessation practices are effective in increasing documentation of smoking status and provision of advice | Provider & care delivery | 20 |
| Gemson 1995 | Cluster RCT | Multifaceted physician education intervention targeted at use of preventive care processes | n = 229, 6 months, 35% AA, 44% Asian | Inner-city municipal hospitals | Improved nutrition and exercise counseling rates with intervention group MDs per patient report (p < .05); trend toward increased rates of tobacco cessation counseling | Complex physician education and improved clinical support program can increase provision of preventive care | Provider & care delivery | 20 |
| Johnson 1997 | Nonrandomized controlled trial | DHS program: consisted of screening for tobacco use, culturally appropriate education material, provider- and staff-delivered counseling, and postcard follow-up | n = 601, 1 year, 100% Native Americans | 4 urban Indian Health Clinics | Abstinence rates higher in intervention group (7.1 vs. 4.9%), though no difference in quit rates validated by cotinine levels (6.7 vs. 6.8) | The DHS program may increase tobacco cessation rates in Native American smokers | Patient/family | 16 |
| Klerman 2001 | RCT | Augmented prenatal care, educational peer groups, longer and more frequent visits | n = 619 (46 smokers), mean intervention at week 11 of pregnancy, 100% AA | Medicaid-eligible OB clinic | 50% quit rate in the intervention group vs. 27% in control group; not statically significant; small number of patients | Tobacco cessation counseling embedded in an augmented prenatal care program may improve quit rates | Patient/family | 18 |
| Lillington 1995 | Pre/post study | Culturally specific counseling, self-help guide, booster postcard, and incentive contest | n = 555 pregnant women, 6-weeks postpartum, 53% AA and 43% Hispanic; four clinics (two intervention and two control) | 4 women, infant, and children clinics | 6 weeks postpartum abstinence rates: intervention vs. controls, 25% vs. 12% | Culturally specific counseling and materials resulted in significant quit rate in pregnant women | Patient/family | 22 |
| Lipkus 1999 | RCT comparing three interventions | Provider prompting intervention vs. provider prompting intervention plus printed material vs. provider prompting intervention plus printed material plus telephone counseling | n = 160, 16 months, 100% AA | Community health clinic | 21.8% of all participants quit; provider intervention vs. provider plus print material quit rate (32.7 vs. 13.2) (p <.05); no additional improvement with phone follow-up | Provider intervention plus print materials resulted in highest quit rate | Patient/family | 20 |
| Manfredi 1999 | Pre/post study | Multicomponent motivational smoking cessation intervention | n = 1,747, 8 weeks, 76% AA | 12 urban public health clinics | Quit rate in intervention vs. control group (14.5 vs. 7.7%) (p < .01) | This intervention, implemented by clinic personnel at routine visits, was effective | Patient/family | 20 |
| McBride 2002 | RCT | Enhanced usual care of BF; self-help manual nicotine patches; BF arm got genotyping GST3 gene (GSTM1) and health educator calls | n = 557, 1 year, 100% AA | Inner-city community health clinic | Smoking cessation was greater for the BF arm than the enhanced usualcare arm (19 vs. 10%, respectively) (p < .006) at 6 months but not at 12 months | Intervention showed short-term effectiveness when delivered as part of routine health care | Patient/family | 23 |
| Nevid 1997 | RCT | Clinic-based group program with culturally specific videotape with smoking related vignettes; control group received group self-help session | n = 93, 1 year, 100% Hispanic | Not mentioned | Intervention vs. control validated posttreatment abstinence rates (21 vs. 6%, p < .05); no difference in abstinence rates at 12-month follow-up | Intervention resulted in short-term increase in abstinence rates; no long-term improvements | Patient/family | 20 |
| Nollen 2006 | RCT | 2 × 2 design: nicotine gum or placebo and health education counseling or motivational interviewing | n = 755, 6 months, 100% AA | Urban community medical clinic | Health education recipients more than twice as likely to quit smoking at 6 months vs. motivational interviewing recipients (OR = 2.17%, CI = 1.38 to 3.41); older age and higher BMI also associated with higher quit rates | Knowledge of individual factors associated with quitting and directive, advice-oriented counseling may be effective facilitators in smoking cessation | Patient/family | 21 |
| Royce 1995 | Pre/post study | Brief clinician advice combined with socioculturally appropriate smoking cessation materials | n = 153, 7 months, 100% AA | Primary care clinic | Rates of cessation and cutting back by 50%; 21% quit rate in intervention group; an additional 27% decreased cigarette intake by at least 50% | Clinician advice combined with culturally appropriate materials decreased daily cigarette daily cigarette usage and increased cessation rates | Patient/family | 16 |
Note: AA = African American; BF = biomarker feedback; BMI = body mass index; BP = blood pressure; CBC = community-based care; DHS = Doctors Helping Smokers; FQHC = federally qualified health center; HTN = hypertension; LDL = low-density lipoprotein; MD = medical doctor; NP = nurse practitioner; RCT = randomized controlled trial.
Studies varied in their approach to validating the presence of tobacco cessation and in their duration of follow-up. Studies with more scientifically rigorous (biochemically validated) and longer term (6 or 12 months) definitions of tobacco cessation tended to show smaller benefits in comparison to studies reporting shorter term and self-reported rates of tobacco cessation.
Patient and family interventions in tobacco
In this category of tobacco cessation interventions, two randomized double-blind placebo-controlled trials by Ahluwalia and colleagues explored the value of tobacco cessation medication use in African Americans (Ahluwalia, McNagny, and Clark 1998; Ahluwalia et al. 2002). The most effective intervention identified was a combination of eight counseling sessions combined with sustained-release bupropion and resulted in a cessation rate of 21% at 6 months (Ahluwalia et al. 2002). Participants in the transdermal nicotine patch study received written material and extensive education on proper use of the patch. Quit rates at 6 months were 17% for the patch group and 11.7% for the placebo group, though after adjustment for baseline differences these were not significantly different (Ahluwalia, McNagny, and Clark 1998). Pharmacologic interventions, especially when combined with counseling, appear to be the most effective interventions.
Apart from pharmacologic interventions, investigators have attempted to evaluate interventions that are linked to the community. Becker and colleagues evaluated a multicomponent community-based intervention to decrease cardiovascular risk of siblings of African American patients with premature cardiovascular disease (Becker et al. 2005). This complex study used a specialized community-based nonclinic site staffed by a nurse practitioner. Cessation medications were provided at no cost, as were written educational materials. At 1 year there was a 16% decrease in smoking in the intervention group and a 7% decrease in the control group.
Cessation interventions designed to be culturally competent have had mixed results. A study of hospitalized African American smokers, which included physician-delivered stage-specific advice, individualized counseling, self-help material tailored to African American smokers, and telephone follow-up, resulted in a significant advance in readiness to quit stage, but cessation rates were not reported (Davies et al. 2005). Nevid and Javier studied 93 Hispanic smokers, with the intervention group receiving a complex intervention involving two hour-long weekly group sessions led by Hispanic mental health workers, a culturally targeted video, and an assigned “buddy.” At 12 months the quit rates were the same in both groups, about 8% (Nevid and Javier 1997). McBride and colleagues assessed the effectiveness of adding information on a genetic biomarker linked to higher cancer risk in patients of African ancestry to culturally targeted cessation advice but found that this did not influence quit rates (McBride et al. 2002).
By contrast, Lipkus, Lyna, and Rimer (1999) evaluated a series of three interventions on quit rates and showed higher quit rates when health care provider prompts were combined with culturally targeted print materials. Royce and colleagues tested an intervention that included 2-3 hr of training in tobacco cessation for physicians and patient enrollment in a culturally targeted cessation program. This program used video and a series of incentive programs to encourage cessation and resulted in a 7-month quit rate of 21% (Royce et al. 1995). More recently, Nollen and associates completed a large study of African American light smokers that explored the value of a culturally targeted health educational intervention compared with motivational interviewing, with and without nicotine gum. Overall cotinine-verified quit rate was 15% at 6 months. Health education emphasizing the addictive nature of nicotine, health consequences of smoking, and concrete approaches to a quit plan and triggers were more than twice as effective as motivational interviewing. Low-income subjects had a reduced chance of success, with nicotine gum showing only a nonsignificant trend toward benefit (Nollen et al. 2006).
Finally, several interventions have specifically targeted young mothers and pregnant women with the added goal of improving the health of their children. One study evaluated an intervention targeted at mothers of young children. The intervention group received a motivational message from a health care provider, a quit smoking guide, and a 10-min motivational interview with a nurse or study coordinator. Self-reported abstinence rates at 1 year were 14% in the intervention group and 7% in the control group (Curry et al. 2003). Two additional studies looked at smoking cessation interventions targeted at pregnant women. A smoking cessation program embedded in a complex multidisciplinary program to decrease rates of low birth weight and preterm labor showed no significant difference in rates of quitting compared to usual care (Klerman et al. 2001). Another program that involved counseling, a self-help guide, a booster postcard, and an incentive contest targeted at pregnant African American and Hispanic women attending a Women, Infants, and Children Clinic showed a significant difference in abstinence rates at 6 weeks postpartum (25% intervention group vs. 12% control group; Lillington et al. 1995). Attempts were made to verify salivary cotinine levels but patient follow-up was poor. Women who continue to smoke despite being pregnant or having young children may be especially refractory to interventions aimed at cessation.
Provider and health care organization interventions in tobacco
Three studies of interventions to reduce tobacco use were directed primarily at individual providers; these focused interventions were largely ineffective. A randomized study by Allen, Pederson, and Leonard (1998) of an educational program for physician trainees designed to promote recognition and treatment of tobacco use in an urban public hospital clinic showed no significant improvement in quit rates, as verified by cotinine levels at 12 months. Another study that provided attendings and trainees with written materials and lectures did not improve rates of cessation counseling (Gemson et al. 1995). A study of adding smoking status as a vital sign increased the rates at which physician trainees asked about smoking, advised patients to quit, and arranged follow-up, but not their rate of offering advice on cessation techniques (Ahluwalia et al. 1999).
Compared to provider interventions, the multicomponent, clinicwide tobacco cessation programs had slightly more promising results, although this was not uniform across studies. Manfredi and colleagues evaluated a tobacco cessation program set in public health clinics in Chicago that consisted of provider-delivered advice and a signed contract, waiting room posters with a cessation message, a written booklet, and a patient-specific follow-up letter with or without a 15-min motivational counseling session. Quit rates at 5 to 8 weeks were 14.5% in the intervention clinics and 7.7% in the usual-care clinics (Manfredi et al. 1999). E. Fisher and colleagues evaluated a tobacco cessation program in the two federally qualified health centers in Saint Louis. The multicomponent program consisted of using smoking as a vital sign, electronic tracking of smokers, providing appropriate stage of quitting materials, training of and feedback to provider teams, medication cost reimbursement, and use of neighborhood resources. The clinic that offered the smoking cessation program showed increased documentation of smoking status and readiness to quit, though quit rates were not reported (E. Fisher et al. 2005). K. M. Johnson and colleagues studied the Doctors Helping Smokers program, which was implemented in two urban clinics serving Native Americans (K. M. Johnson et al. 1997). The program included screening all patients for tobacco use, alerts attached to charts, clinician-delivered smoking cessation messages, reinforcement delivered by staff, and phone follow-up by an outreach worker. Cotinine-verified 12-month quit rates were low and the same in both groups (6.7%).
In summary, (1) patient-directed pharmacologic interventions for smoking cessation have been shown in African Americans to be effective especially when combined with counseling; the same interventions have been less frequently studied in other minority groups. (2) Culturally targeted health education interventions have had mixed results, with heterogeneity in the study populations and interventions limiting the conclusions that can be drawn. (3) Clinicwide tobacco cessation programs may be more effective compared to isolated provider-targeted education programs.
Physical Inactivity Results
Eight studies described interventions to increase physical activity in communities of color (table 6). Of these studies, five included significant representation of African Americans (Banks-Wallace and Conn 2005; Gemson et al. 1995; Newton and Perri 2004; Rimmer et al. 2002; Yanek et al. 2001), two of Mexican Americans/Hispanics (Lorig, Ritter, and Gonzalez 2003; Poston et al. 2001), one of Alaskan Native/American Indians (Witmer et al. 2004), and one of Asian Americans (Gemson et al. 1995). Three of the eight studies were randomized controlled trials (Lorig, Ritter, and Gonzalez 2003; Poston et al. 2001; Yanek et al. 2001), and three were small pilot studies (Banks-Wallace and Conn 2005; Newton and Perri 2004; Witmer et al. 2004).
Table 6.
Physical Inactivity
| Reference | Design | Intervention | n, Follow-Up, Racial/Ethnic Composition | Setting | Results: Process and Patient Outcomes | Conclusion | Target | Quality Score |
|---|---|---|---|---|---|---|---|---|
| Banks-Wallace 2005 | RCT | 12-month intervention that included a 3-hr monthly group meeting (with behavioral counseling, some storytelling, and a 40-min interactive learning period) and a home-based walking component | n = 21, 6 months, 100% AA | Homes and community centers | At 6 months, mean steps/day increased by 37% from base-line in the entire group; this was only a trend toward statistical significance, probably related to small study size | Group intervention can have a positive impact on promoting walking in the African American population | Patient/family | 10 |
| Gemson 1995 | Cluster RCT | Multifaceted physician education intervention targeted at use of preventive care processes | n = 229, 6 months, 35% AA, 44% Asian | Improved nutrition and exercise counseling rates with intervention group MDs per patient report (p < .05); trend toward increased rates of tobacco cessation counseling | Complex physician education and improved clinical support program can increase provision of preventive care | Provider & care delivery | 20 | |
| Lorig 2003 | RCT for initial 4 months; then crossover of all study subjects to intervention group | 6-week peer-led intervention, audio exercise tape, illustrated booklet of the exercise routines, and audio relaxation tape | n = 551, 1 year, 50% Hispanic with cardiovascular risk factors | Community and home based | Improved health status, health behavior, and self-efficacy, as well as fewer emergency department visits (p < .05); at 1 year, the improvements maintained; significant improvement in physical activity at 4 months compared with baseline (p < .001); reduced number of ER visits at 4 months and 1 year | Peer-led education and exercise intervention reduced ER visits and increased physical activity | Patient/family | 22 |
| Newton 2004 | RCT | Standard behavioral counseling group (SB), culturally sensitive counseling (CS) group, physician advice comparison group (PA) | n = 60, 6 months, 100% AA | Home-based exercise promotion program | All three programs led to increases in self-reported physical activity; CS and SB showed higher increases in cardiovascular fit | Differences in fitness level did not differ significantly among all treatment groups; adherence was the same for all groups | Provider & care delivery | 22 |
| Poston 2001 | RCT with block design | Culturally appropriate intervention: weekly 90-min meetings using individual-oriented, culturally tailored behavioral techniques and reading materials; waitlist control group did not receive intervention but were assessed at baseline and 6 and 12 months | n = 379, 12 months, 100% Mexican American women | Home and community centers | No difference in physical activity among the study participants; higher drop-out rate in treatment than control group; not statistically significant at 6 months but significant at 12 months (p < .001) | Culturally appropriate intervention consisting of weekly meetings, written materials, and behavioral techniques was not effective in increasing exercise in this challenging population | Patient/family | 19 |
| Rimmer 2002 | Pre/post with control group | A 12-week structured exercise training program | n = 44 women, 12 weeks, 82% AA | Home and community health centers | Significant gain in cardiovascular function and strength (p < .001); improvement in some aspects of body composition; no change in flexibilityness vs. the PA group (SB vs. PA, p = .006; CS vs. PA, p = .034); CS had higher satisfaction | Free program with transport and motivation by phone calls helped increase participation and adherence; higher adherence among home-based group | Provider & care delivery | 19 |
| Witmer 2004 | RCT | Intervention group: 12 weekly 2-hr educational sessions taught by multidisciplinary team; educational materials were also used | n = 76, 12 months, 100% Alaskan Native/American Indian women | Anchorage Native Primary Care Center | Significant improvements in reported levels of physical activity among intervention participants (p < .04) | National initiatives invested in cardiovascular risk reduction must be tailored to specific populations and keep cultgural differences in mind | Patient/family | 17 |
| Yanek 2001 | RCT, block randomization | SBI: weigh in and group discussion including a 30-min moderate-intensity aerobic activity session; spiritual intervention: same as SBI with the addition of spiritual and church contextual components; self-help control intervention: reading materials | n = 529, 1 year, 100% AA women | Home, clinic, and church based | Self-help participants were significantly less likely to schedule appointemnts, keep scheduled appointments, or enroll in the program; spiritual and self-help participants were significantly more likely to return for follow-up than self-help patients; there was difference in weight loss (p < .0001), but not for energy expenditure | Intervention did improve a lot of the anthropometric measures at 1 year, but not physical activity; study emphasizes the importance of church and religion in the black community | Patient/family | 22 |
Note: AA = African American; ER = emergency room; MD = medical doctor; RCT = randomized controlled trial; SBI = standard behavioral intervention.
A variety of interventions utilized community-level components, including church-based interventions, home-based phone counseling and mail interventions, community-based group sessions utilizing motivational interviewing techniques (some incorporated cultural targeting), physician training in counseling, physician-assisted standard patient counseling, and self-motivation-based interventions. Most of the studies consisted of women only, with the exception of the studies by Newton and Lorig, which each had about 20% male subjects.
All of the studies had an intervention period of at least 3 months (Witmer et al. 2004) with the average follow-up period ranging between 6 and 12 months. In most of the studies, there was a high drop-out rate with reduced follow-up rates (32%-67%), with only one study recording a low (12%) drop-out rate (Poston et al. 2001). Three studies (Lorig, Ritter, and Gonzalez 2003; Newton and Perri 2004; Yanek et al. 2001) used general activity assessments such as the 7-day Physical Activity Recall questionnaire, with the remainder assessing walking behavior by self-report or pedometer readings.
The effectiveness of interventions was mixed. Four studies (Banks-Wallace and Conn 2005; Gemson et al. 1995; Poston et al. 2001; Yanek et al. 2001) found marginal or no statistically significant impact. Some of the studies that did not show a statistical difference cited intergroup contamination as a possible reason. For example, in the study conducted by Poston et al. (2001), the intervention group started off with statistically significant lower activity levels at baseline, suggesting randomization failure. Of note, interventions that incorporated culturally targeted and faith-based counseling themes did not appear to produce significant differences in physical activity in comparison to standard counseling methods (Newton and Perri 2004; Poston et al. 2001; Yanek et al. 2001). Physician education to improve exercise counseling was also ineffective (Gemson et al. 1995).
On the other hand, four studies demonstrated a positive effect on physical activity for patients of color (Lorig, Ritter, and Gonzalez 2003; Newton and Perri 2004; Rimmer et al. 2002; Witmer et al. 2004). Why these studies were successful while others were not is not entirely clear. Three of the interventions utilized nonphysician counselors in implementing behavioral education (Lorig, Ritter, and Gonzalez 2003; Newton and Perri 2004; Witmer et al. 2004); however, many of the previously described negative studies used similar intervention designs. The intervention by Lorig et al. is distinct in that the intervention was led by patient peers. That study is also notable for differences in patient behavior at the 1-year mark well after the intervention had ended at 6 weeks (Lorig, Ritter, and Gonzalez 2003). The study by Rimmer et al. (2002) evaluated a structured exercise training program in a majority African American population with chronic disease conditions and disabilities. All participants were able to adhere to the exercise program, and despite the patients’ disabilities, there were no side effects related to exercise. The authors cited removal of cost and transportation barriers and close followup by a highly motivated staff as reasons for the strong adherence.
In summary, interventions designed to increase physical activity have had mixed results and have been marked by high drop-out rates. While some study results are particularly promising, there are too few studies in this area to draw definitive conclusions regarding the ideal intervention to increase physical activity in communities of color.
Acute and Postacute Coronary Artery Disease Results
We found no interventions that directly addressed the care of acute coronary disease. We found only one study of post-MI care (Schneiderman et al. 2004). In this study, investigators evaluated a psychosocial intervention that attempted to address depression and low perceived social support among patients who had had recent MIs. Patients were followed for a mean of 2.4 years. The investigators found that there was a significant reduction in the outcome, cardiac death or nonfatal MI, among white men, but no such benefit for men or women of color (Schneiderman et al. 2004).
In summary, there are no studies describing attempts to improve acute coronary heart disease care. The one study of post-MI care of depression and social support was not effective in communities of color.
HF Results
Overall, seven reports met the review’s criteria of interventions to improve the quality of care for patients with HF (table 7). Most of these involved HF care management programs with multiple components including patient education, frequent phone follow-up, patient self-management skill development such as checking daily weights, and oversight by a cardiologist and/or the patient’s primary care provider. A key educational message consistent in most of the interventions was the early recognition of symptoms and signs of fluid overload and prompt adjustment of diuretic dose.
Table 7.
Congestive Heart Failure
| Reference | Design | Intervention | n, Follow-Up, Racial/Ethnic Composition | Setting | Results: Process and Patient Outcomes | Conclusion | Target | Quality Score |
|---|---|---|---|---|---|---|---|---|
| Artinian 2003 | RCT | Intervention group received usual care plus a Med-e Monitor device with electronic medication reminders; included daily reminders/assessment of medications and symptoms, while monitoring daily weight and BP | n = 18, 3 months, 65% AA class II-III CHF | CHF clinic of a Veterans Affairs Medical Center | Trend toward improved monitoring of daily weight (85% vs. 70%) and BP (81% vs. 51%) in intervention group as compared to control group; QOL improved in intervention group at 3 months (p = .006) | E-monitoring improved QOL, with trend toward improved self-monitoring | Provider & care delivery | 22 |
| Benatar 2003 | RCT | APN monitored recently discharged patients using transtelephonic home measuring (TTM) device to follow weight, BP, oxygenation, and heart rate or use of home nurse visits | n = 216, 12 months, 86% AA | Home | At 3 months, TTM group had fewer admissions at 13 vs. 24 for home visit group (p ≤ 0.001) and shorter lengths of stay at 49 vs. 105 days (p ≤ 0.001) | Cardiologist-guided computerized monitoring of patients with CHF reduces admission rates and length of stay | Provider & care delivery | 22 |
| DeWalt 2004 | Pre/post study | Patient education combined with frequent phone follow-up; patients given electronic scale to use for daily weights | n = 25, 3 months, 60% AA with low literacy | University internal medicine clinic | Proportion of patients reporting daily weights from 32% at baseline to 100% at 12 weeks; mean improvement on the MLwHF scale was 9.9 points over the 3-month trial (95% CI: 0.5 to 19.2); mean knowledge scores did not improve | E-monitoring improved QOL, with trend toward improved self-monitoring | Provider & care delivery | 16 |
| Naylor 2004 | RCT | A 3-month APN-directed discharge planning and home follow-up protocol | n = 239, 1 year, 36% AA (data reported for subgroup of AA patients; personal communication) | Hospital and home follow-up | Intervention patients had lower total number of CHF-related admissions (7 vs. 9) (p < .04) and lower CHF-related admission costs | Cardiologist-guided computerized monitoring of patients with CHF reduces admission rates and length of stay | Provider & care delivery | 24 |
| O’Connell 2001 | Pre/post study | Multidisciplinary case management program to reduce hospitalizations in indigent HF patients | n = 35, 1 year, 51% Hispanic | Academic teaching hospital-based clinic | Group A (2 hospital readmissions/year): 91% reduction in admissions (p < .001); Group B (difficult to manage): 100% reduction in admissions (p = .002) | Multidisciplinary case management was effective in reducing readmissions in patients with HF | Patient/family | 16 |
| Rich 1995, 1996 | RCT | Nurse-directed education program for patient and family, prescribed diet, social service consult, medication review, and intensive follow-up | n = 282, 90 days, 55% AA | Home | Intervention reduced HF admissions by 56.2% (p = .04) in subgroup; QOL improved in intervention group at 90 days (p = .001); 88% adherence intervention vs. 81% control (p = .003) | Nurse-directed multicomponent intervention can improve QOL, improve medication compliance, and reduce readmissions for HF patients | Patient/family | 22 |
| Sisk 2006 | RCT | RN-led case management including education, medication monitoring, and teaching of self-management skills coordinated with patient’s primary MD | n = 406, 12 months, 46% AA, 33% Hispanic | Four urban hospital-based clinics | Nurse management group had fewer hospitalizations compared to controls (143 vs. 180) and better functioning (39.9 vs. 36.3) on MLwHF | Case management delivered by RNs working with patient’s primary provider can improve outcomes | Patient/family | 23 |
Note: AA = African American; APN = advanced practice nurse; BP = blood pressure; CHF = congestive heart failure; HF = heart failure; MD = medical doctor; MLwHF = Minnesota Living with Heart Failure scale; QOL = quality of life; RCT = randomized controlled trial; RN = registered nurse.
Four of the randomized controlled trials used interventions with specialized nurses and frequent phone follow-up to reduce rates of admission for HF (Benatar et al. 2003; Naylor et al. 2004; Rich et al. 1995; Sisk et al. 2006). Each of these interventions used nurse-led care management, patient education, and facilitated follow-up to identify early signs of fluid overload and implement medication changes, often over the phone. The four interventions varied in the exact nature of how vital signs of HF patients were ascertained and the extent to which other health care professionals were involved. Despite these differences, the interventions were largely successful in reducing rehospitalizations for HF. The study by Benatar and colleagues (2003) used transtelephonic home monitoring to measure such factors as weight and BP. Information was reviewed by trained nurses and adjustment of care plans were made by cardiologists and implemented by nurses. The study by Naylor and colleagues (2004), targeted at elderly patients, evaluated an advanced practice nurse-delivered program of education, frequent outpatient visits, and active assessment for early signs of volume overload. Rich and colleagues (1995) evaluated a multidisciplinary intervention that included intensive education and consultation with a geriatric cardiologist, dietician, and social worker. Patients were followed up with frequent home visits and telephone contacts. A recently published study by Sisk and colleagues (2006) evaluated a 12-month nurse-led program of dietary and medication counseling and education on the self-management of symptoms.
Two pre/postintervention studies evaluating nurse-led care management programs showed promising results. The first study was an evaluation of a nurse-led care management program for low-literacy patients that involved intensive education, frequent telephone follow-up, and telephone-based medication adjustment. The intervention group showed improvement in compliance with daily weights and the New York Heart Association class (DeWalt et al. 2004). The second study was conducted in a predominantly Latino population and evaluated an intervention also consisting of an educational component, care management by a nurse practitioner, and weekly follow-up. The intervention was associated with a marked reduction in hospitalization rates (O’Connell, Crawford, and Abrams 2001).
Apart from these nurse-led interventions, Artinian and colleagues (2003) evaluated a Web-based home-monitoring system that was designed to change self-care behaviors such as medication adherence, diet, and exercise. The study showed no significant difference in self-care behaviors, 6-min walk test, or functional class. Quality of life did improve in the monitoring group.
In summary, (1) HF care management programs have been found to decrease hospitalization rates; (2) successful care management programs have consisted of education, specialty nurse case management, frequent telephone follow-up with medication adjustment, and oversight by a specialist in HF and are best validated in patients with advanced HF; (3) the value of culturally tailored care and the importance of disease management in patients with mild to moderate HF remains to be demonstrated.
Discussion
In this systematic review, we describe cardiovascular interventions evaluated in populations of color since 1995. Despite thousands of studies bearing on the issue of cardiovascular racial and ethnic disparities, we found only 27 hypertension, 9 dyslipidemia, 18 tobacco use, 8 physical inactivity, 1 post-MI, and 7 HF studies formally testing interventions. Studies were often limited by small numbers, clinically modest gains, and short follow-up; demonstrations of sustainable improvement were decidedly the exception. Few interventions have been tested across the full range of cardiovascular conditions and spectrum of communities of color. Few interventions have been evaluated in multiple health care settings (Godfrey et al. 2003). Perhaps the most important limitation of the existing literature is that few studies have specifically tested interventions for their effectiveness in reducing ethnic/racial disparities in cardiovascular prevention and care. The vast majority of studies we identified during our systematic review were studies of interventions that have been carried out in communities of color without a white subpopulation for comparison. Despite this limitation, the strengths and weaknesses of these interventions will provide valuable lessons for future efforts to reduce cardiovascular disparities. Future efforts should also incorporate findings from the quality of care interventions that have, as of yet, solely been conducted in populations with a white majority.
Lessons Learned from the Current Cardiovascular Intervention Literature
Several overarching lessons emerged from our review of interventions, crossing all cardiovascular risk factors and conditions. First, interventions have been inconsistently studied across risk factors and conditions. The most heavily studied areas have been hypertension and tobacco use; attention to these areas is appropriate given their relative health burden. The most striking deficiency in the current literature is in the area of interventions to address acute or postacute coronary artery disease management, where disparities in care have been very well documented. This deficiency may be a reflection of the fact that designing interventions for acute coronary syndromes may simply require far more resources and planning on a scale that is far larger than interventions for risk factor or chronic disease management. Specialty societies have begun important work in this area (Roe 2004). The Robert Wood Johnson Program, Expecting Success, is an example of a large-scale multihospital initiative that will specifically target disparities in acute coronary disease management (http://www.expectingsuccess.org/index.html).
A second lesson learned has to do with the ideal approach to improving the management of cardiovascular risk factors in primary care practice. Our review suggests that interventions in primary care should consider organization-level interventions, such as clinic reorganization, rather than provider-level interventions that attempt to change physician prescribing behaviors. While high-quality primary care may facilitate cardiac risk reduction and access to specialty care, our review has found relatively little support for physician-focused programs. Physician awareness of key prescribing messages (sodium-restricted diets for hypertension; bupropion and nicotine replacement for smoking; aspirin, beta blocker, and statins for dyslipidemia and coronary artery disease) is necessary but not sufficient for effective translation, especially in vulnerable populations. Sustaining adherence to BP and lipid medication may fundamentally depend on ensuring access to care and prescription medication (Briesacher, Limcangco, and Gaskin 2003; Burke, Dunbar-Jacob, and Hill 1997; McDowell, Coleman, and Ferner 2006; Rehman et al. 2005; Sabatine et al. 2005; Schore, Brown, and Lavin 2003).
Health care organization-level interventions, such as practice reorganization, as a strategy in improving cardiovascular care has so far shown modest effects in fostering prescribing and behavior change in primary care practice. Results from such interventions may be difficult to extricate from the attention and enthusiasm that triggered the reorganization in the first place and require careful study (de Lusignan et al. 2004; Elley et al. 2003). Ongoing research in the Prescription for Change program funded by the Robert Wood Johnson Foundation and the Agency for Healthcare Research and Quality is exploring the value of adapting three existing models (the chronic care model, Rogers’ diffusion of innovation, and the Five A model) in ethnically diverse populations (Cifuentes et al. 2005). A robust set of “toolboxes” might be useful in allowing individual practices to adapt promising quality interventions to local patient populations and clinic organizational factors, something that has proved daunting even in fairly homogeneous patient populations (Shortell and Peck 2006; Solberg et al. 2000). Web-based updates in the prevalence of race- and ethnicity-specific risk factors (http://www.prevent.org; Satcher 2006) and the extent of health disparities (http://www.qualitytools.ahrq.gov/disparitiesreport) may help in the necessary business of setting prevention priorities for practices (Woolf and Stange 2006).
A third lesson learned has to do with the use of multidisciplinary health professional teams in improving cardiovascular risk factor and disease management among patients of color. Across the interventions in this review, management and outreach strategies involving nurses have shown relatively consistent effectiveness in communities of color and, by implication, may help to reduce health disparities. In our review, effectiveness of nursing interventions was best demonstrated for hypertension, HF, and several multitarget coronary artery disease prevention programs. This is consonant with other research suggesting that multicomponent nurse specialist-led intervention with physician collaboration appears most consistently effective in populations of color both in the United States and abroad (Denver et al. 2003) and in the general population (Salisbury and Fahey 2006).
In our review of interventions concerning communities of color, we found relatively few pharmacist-led interventions except in the areas of hypertension and hyperlipidemia (Fahey, Schroeder, and Ebrahim 2005), although they appeared to be relatively effective. In several studies excluded from this review because of inadequate representation by communities of color, pharmacist-led interventions have been found to improve lipid and BP levels (Lee, Grace, and Taylor 2006; Palmieri, Redline, and Morita 2005) and in one case have been found to reduce mortality rates in elderly patients (Wu et al. 2006). Such interventions deserve replication in communities of color in the United States.
Disease management has also been offered as a nurse- and sometimes pharmacist-based solution, given its potential to promote more systematic adherence to evidence-based guidelines and coordination of care between the inpatient and outpatient settings. However, this literature is heterogeneous in study population and intervention, has commonly involved managed care and for-profit settings, and has often had clinically modest effects, suggesting potential pitfalls in uncritically extrapolating this literature to disparities reduction (Ofman et al. 2004). An American Heart Association expert panel has recently published a taxonomy designed to improve the quality and comparability of disease management programs (Krumholz et al. 2006).
Potential Lessons from the General Population Intervention Literature for Specific Risk Factors and Conditions
Hypertension and diet
Hypertension remains a linchpin of efforts to reduce racial disparities in vascular disease (Yusuf 2006). Strategies to improve medication adherence have been recently reviewed, and assessing their usefulness in populations of color is a promising strategy (Hess et al. 2007; Kripalani, Yao, and Haynes 2007; T. J. Wang and Vasan 2005). Salt restriction and potassium supplementation may also have small but important benefits at the population level, especially in African American patients. Culturally targeted diets are likely to be of greater importance in the African American population. This is suggested by the lesser BP effects achieved by the PREMIER compared to DASH diets, which may well be attributed to the contrast between giving patients meals prepared in a research kitchen and teaching patients to follow a diet in their daily lives (Svetkey et al. 2005). In our review, the DASH and TONE studies as well as older literature (Brancati et al. 1996) suggest that potassium supplementation may be of value, especially in African American patients (Appel et al. 2006), with recent surveys suggesting that African Americans continue to consume more sodium and less potassium (Panel on Dietary Reference Intakes for Electrolytes and Water: Institute of Medicine 2004). While these dietary changes hold significant potential to reduce disparities in BP and thus cardiovascular disease (Cook et al. 2007; Erlinger et al. 2003), these changes may be difficult to achieve by individual patients without systemic changes in the available food supply (Dickinson et al. 2006; Kumanyika et al. 2005). Strategies to disseminate healthier culturally appealing food selection and preparation require further exploration (Pickering 2006).
Physical inactivity
Self-help or minimal assistance interventions are attractive because of their potential to influence broad segments of the population. Unfortunately, in our review, studies of self-help groups had higher drop-out rates and were at best modestly successful in increasing physical activity levels, compared with faith-based, culturally targeted, or physician-assisted counseling groups. Interventions directed at increasing the safety and acceptability of exercise in the community, interventions that target individuals across generations (Yancey, Ory, and Davis 2006), and programs addressing issues of “built environment” may hold greater promise for increasing physical activity (Mobley et al. 2006). Studies abroad have shown that primary care-delivered prescriptions for physical activity can increase patient activity and improve quality of life (Elley et al. 2003), but these studies have yet to be replicated in U.S. communities of color.
Coronary artery disease
Given the relative paucity of studies specifically examining coronary care for patients of color, studies of coronary artery disease quality improvement interventions in the general population offer important ideas for future interventions for patients of color (A. M. Clark et al. 2005). Adherence to protocol-driven care in acute coronary syndrome and acute MI within hospitals may help to enhance the quality of care for all patients (M. L. Williams, Hill, and Jackson 2006). A hospital-based discharge medicine program using statistical process control techniques was able to achieve appropriate cardiac medication-prescribing rates of more than 90% with an associated highly significant 21% reduction in 1-year mortality (Lappe et al. 2004). A computerized alert intervention incorporated academic detailing by inpatient pharmacists who responded to lab alerts of elevated troponins. This intervention increased the discharge provision of recommended secondary prevention medications (angiotensin-converting enzyme inhibitors, aspirin, beta blockers, and statins) in coronary artery disease patients (Bailey et al. 2007). A postoperative cardiac call from a nurse increased attendance to cardiac rehabilitation in Ontario from 50% to 78% (Harkness et al. 2005). Practice facilitators are health care professionals, often nurses with additional training, who assist primary care clinicians in research and quality improvement; they have shown great promise in Europe (Nagykaldi, Mold, and Aspy 2005). Given the significant degree of de facto segregation of cardiac care in the United States, disparities reduction strategies will need to benchmark, analyze, and address variations both within health care organizations (clinics, hospitals, and networks) and between health care organizations, looking for the clues and opportunities that better and worse performers can provide (Rumsfeld and Epstein 2006).
Limitations
Many of the studies we reviewed were of small sample size and confined to a single health care organization, limiting generalizability. Caution is warranted in drawing broad conclusions given the variability in the components of interventions and the intangibles of staff involvement and implementation. The review is retrospective, and publication bias in favor of successful interventions is likely, particularly given the complexity of modifying long-standing cardiac risk in vulnerable populations. Interventions that were exclusively community focused, such as faith- and school-based programs, were not addressed in this review, though some have rigorously shown positive effects in improving physical activity, weight loss, and BP control.
Conclusions
High-quality research specifically addressing reduction of cardiovascular racial and ethnic disparities is virtually nonexistent. Fortunately, there has been an accumulation of research addressing cardiac risk and conditions in vulnerable populations, and several broad themes have emerged. Interventions that have included organization-level interventions, such as multifactorial clinic reorganization and multidisciplinary teams, have had the most consistent success in improving the cardiovascular management of communities of color. Nurse-led interventions have shown greater effectiveness in general and may be more affordable in urban and rural settings with poorer physician supply.
Building on this existing literature, greater attention to cardiovascular disparities is sorely needed and should inform ongoing national efforts to improve cardiovascular care. There are accelerating national efforts to improve the quality of care for chronic conditions in the general population through methods such as the chronic care model (Bodenheimer, Wagner, and Grumbach 2002; Cifuentes et al. 2005; Solberg et al. 2006) and pay for performance (Grossbart 2006), but whether these strategies will prove useful in reducing health disparities remains largely untested (Chien et al. 2007 [this issue]; Lavizzo-Mourey and Jung 2005). To truly fulfill the promise of modern cardiovascular care, quality improvement efforts need to identify vulnerable populations, consider and document the presence of disparities, and when found, assess the value of clearly defined interventions in reducing them. This need is most apparent for the acute management of coronary artery disease, between-visit education and adherence (Benatar et al. 2003; Rogers et al. 2001; Wu et al. 2006), and for coordination of care (Coleman et al. 2006), areas that have thus far received relatively little attention in communities of color. Our hope is that the information gathered in this review will inform researchers, policy makers, and clinicians as they strive to reduce disparities and improve the quality of care for all.
Acknowledgments
This project was supported by the Robert Wood Johnson Foundation Finding Answers: Disparities Research for Change Program, the Department of Medicine at the University of Chicago, and the National Institute of Diabetes and Digestive and Kidney Diseases Diabetes Research and Training Center (P60 DK20595). Dr. Huang’s research is supported by a National Institutes of Health (NIH) Mentored Patient-Oriented Career Development Award (K23 AG021963). Ayana Chase’s research is supported through an NIH Short-Term Training: Health Professional Students program with Dr. Eugene Chang at the University of Chicago (T35 DK062419-20).
References
- Agency for Healthcare Research and Quality . National healthcare disparities report. Department of Health and Human Services, Agency for Healthcare Research and Quality; Washington, DC: 2006. [Google Scholar]
- Agoston I, Cameron CS, Yao D, Dela Rosa A, Mann DL, Deswal A. Comparison of outcomes of white versus black patients hospitalized with heart failure and preserved ejection fraction. American Journal of Cardiology. 2004;94(8):1003–7. doi: 10.1016/j.amjcard.2004.06.054. [DOI] [PubMed] [Google Scholar]
- Ahluwalia JS, Gibson CA, Kenney RE, Wallace DD, Resnicow K. Smoking status as a vital sign. Journal of General Internal Medicine. 1999;14(7):402–8. doi: 10.1046/j.1525-1497.1999.09078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahluwalia JS, Harris KJ, Catley D, Okuyemi KS, Mayo MS. Sustained-release bupropion for smoking cessation in African Americans: A randomized controlled trial. Journal of the American Medical Association. 2002;288(4):468–74. doi: 10.1001/jama.288.4.468. [DOI] [PubMed] [Google Scholar]
- Ahluwalia JS, McNagny SE, Clark WS. Smoking cessation among inner-city African Americans using the nicotine transdermal patch. Journal of General Internal Medicine. 1998;13(1):1–8. doi: 10.1046/j.1525-1497.1998.00001.x. see comment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahluwalia JS, McNagny SE, Kanuru NK. A randomized trial to improve follow-up care in severe uncontrolled hypertensives at an inner-city walk-in clinic. Journal of Health Care for the Poor and Underserved. 1996;7(4):377–89. doi: 10.1353/hpu.2010.0216. [DOI] [PubMed] [Google Scholar]
- Ahmed A, Sims RV, Allman RM, DeLong JF, Aronow WS. Racial variations in cardiology care among hospitalized older heart failure patients. Heart Disease. 2003;5(1):8–14. doi: 10.1097/01.HDX.0000050408.07809.45. [DOI] [PubMed] [Google Scholar]
- Ajani UA, Ford ES, Greenland KJ, Giles WH, Mokdad AH. Aspirin use among U.S. adults behavioral risk factor surveillance system. American Journal of Preventive Medicine. 2006;30(1):74–77. doi: 10.1016/j.amepre.2005.08.042. [DOI] [PubMed] [Google Scholar]
- Allen B, Pederson LL, Leonard EH. Effectiveness of physicians-in-training counseling for smoking cessation in African Americans. Journal of the National Medical Association. 1998;90(10):597–604. [PMC free article] [PubMed] [Google Scholar]
- Allison JJ, Kiefe CI, Centor RM, Box JB, Farmer RM. Racial differences in the medical treatment of elderly Medicare patients with acute myocardial infarction. Journal of General Internal Medicine. 1996;11(12):736–43. doi: 10.1007/BF02598987. [DOI] [PubMed] [Google Scholar]
- Angelelli J, Grabowski DC, Mor V. Effect of educational level and minority status on nursing home choice after hospital discharge. American Journal of Public Health. 2006;96(7):1249–53. doi: 10.2105/AJPH.2005.062224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: A scientific statement from the American Heart Association. Hypertension. 2006;47(2):296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR. Effects of comprehensive lifestyle modification on blood pressure control: Main results of the PREMIER clinical trial. Journal of the American Medical Association. 2003;289(16):2083–93. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: Results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE) Archives of Internal Medicine. 2001;161(5):685–93. doi: 10.1001/archinte.161.5.685. [DOI] [PubMed] [Google Scholar]
- Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. New England Journal of Medicine. 1997;336(16):1117–24. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- Ard JD, Rosati R, Oddone EZ. Culturally-sensitive weight loss program produces significant reduction in weight, blood pressure, and cholesterol in eight weeks. Journal of the National Medical Association. 2000;92(11):515–23. [PMC free article] [PubMed] [Google Scholar]
- Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea JA. Distrust of the health care system and self-reported health in the United States. Journal of General Internal Medicine. 2006;21(4):292–97. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artinian NT, Harden JK, Kronenberg MW, Vander Wal JS, Daher E, Stephens Q, Bazzi RI. Pilot study of a Web-based compliance monitoring device for patients with congestive heart failure. Heart & Lung. 2003;32(4):226–33. doi: 10.1016/s0147-9563(03)00026-8. [DOI] [PubMed] [Google Scholar]
- Artinian NT, Washington OG, Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: A pilot study. Heart & Lung. 2001;30(3):191–99. doi: 10.1067/mhl.2001.112684. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Landrum MB, Guadagnoli E, Gaccione P. Specialty of ambulatory care physicians and mortality among elderly patients after myocardial infarction. New England Journal of Medicine. 2002;347(21):1678–86. doi: 10.1056/NEJMsa020080. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Weissman JS, Chasan-Taber S, Epstein AM. Quality of care by race and gender for congestive heart failure and pneumonia. Medical Care. 1999;37(12):1260–69. doi: 10.1097/00005650-199912000-00009. [DOI] [PubMed] [Google Scholar]
- Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. New England Journal of Medicine. 2004;351(6):575–84. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- Bailey TC, Noirot LA, Blickensderfer A, Rachmiel E, Schaiff R, Kessels A, Braverman A, Goldberg A, Waterman B, Dunagan WC. An intervention to improve secondary prevention of coronary heart disease. Archives of Internal Medicine. 2007;167(6):586–90. doi: 10.1001/archinte.167.6.586. [DOI] [PubMed] [Google Scholar]
- Banks-Wallace J, Conn V. Changes in steps per day over the course of a pilot walking intervention. ABNF Journal. 2005;16(2):28–32. [PubMed] [Google Scholar]
- Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Medical Care. 2005;43(4):308–19. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker DM, Yanek LR, Johnson WR, Jr., Garrett D, Moy TF, Reynolds SS, Blumenthal RS, Vaidya D, Becker LC. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation. 2005;111(10):1298–304. doi: 10.1161/01.CIR.0000157734.97351.B2. see comment. [DOI] [PubMed] [Google Scholar]
- Benatar D, Bondmass M, Ghitelman J, Avitall B. Outcomes of chronic heart failure. Archives of Internal Medicine. 2003;163(3):347–52. doi: 10.1001/archinte.163.3.347. [DOI] [PubMed] [Google Scholar]
- Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. Journal of the American Medical Association. 2002;288(4):455–61. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- Bhandari VK, Kushel M, Price L, Schillinger D. Racial disparities in outcomes of inpatient stroke rehabilitation. Archives of Physical Medicine and Rehabilitation. 2005;86(11):2081–86. doi: 10.1016/j.apmr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: The Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111(10):1313–20. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: The chronic care model, Part 2. Journal of the American Medical Association. 2002;288(15):1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, Oddone EZ. Racial differences in blood pressure control: Potential explanatory factors. American Journal of Medicine. 2006;119(1):70.e9–15. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- Brancati FL, Appel LJ, Seidler AJ, Whelton PK. Effect of potassium supplementation on blood pressure in African Americans on a low-potassium diet. A randomized, double-blind, placebo-controlled trial. Archives of Internal Medicine. 1996;156(1):61–67. [PubMed] [Google Scholar]
- Bray GA, Vollmer WM, Sacks FM, Obarzanek E, Svetkey LP, Appel LJ. A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: Results of the DASH-Sodium Trial. American Journal of Cardiology. 2004;94(2):222–27. doi: 10.1016/j.amjcard.2004.03.070. [DOI] [PubMed] [Google Scholar]
- Briesacher B, Limcangco R, Gaskin D. Racial and ethnic disparities in prescription coverage and medication use. Health Care Financing Review. 2003;25(2):63–76. [PMC free article] [PubMed] [Google Scholar]
- Brown DW, Haldeman GA, Croft JB, Giles WH, Mensah GA. Racial or ethnic differences in hospitalization for heart failure among elderly adults: Medicare, 1990 to 2000. American Heart Journal. 2005;150(3):448–54. doi: 10.1016/j.ahj.2004.11.010. [DOI] [PubMed] [Google Scholar]
- Brown DW, Shepard D, Giles WH, Greenlund KJ, Croft JB. Racial differences in the use of aspirin: An important tool for preventing heart disease and stroke. Ethnicity & Disease. 2005;15(4):620–26. [PubMed] [Google Scholar]
- Burden RW, Kumar RN, Phillips DL, Borrego ME, Galloway JM. Hyperlipidemia in Native Americans: Evaluation of lipid management through a cardiovascular risk reduction program. Journal of the American Pharmacists Association. 2002;42(4):652–55. doi: 10.1331/108658002763029634. [DOI] [PubMed] [Google Scholar]
- Burke LE, Dunbar-Jacob JM, Hill MN. Compliance with cardiovascular disease prevention strategies: A review of the research. Annals of Behavioral Medicine. 1997;19(3):239–63. doi: 10.1007/BF02892289. [DOI] [PubMed] [Google Scholar]
- Call KT, McAlpine DD, Johnson PJ, Beebe TJ, McRae JA, Song Y. Barriers to care among American Indians in public health care programs. Medical Care. 2006;44(6):595–600. doi: 10.1097/01.mlr.0000215901.37144.94. [DOI] [PubMed] [Google Scholar]
- Carnethon MR, Bertoni AG, Shea S, Greenland P, Ni H, Jacobs DR, Jr., Saad M, Liu K. Racial/ethnic differences in subclinical atherosclerosis among adults with diabetes: The multiethnic study of atherosclerosis. Diabetes Care. 2005;28(11):2768–70. doi: 10.2337/diacare.28.11.2768. [DOI] [PubMed] [Google Scholar]
- Chen MS, Bhatt DL, Chew DP, Moliterno DJ, Ellis SG, Topol EJ. Outcomes in African Americans and whites after percutaneous coronary intervention. American Journal of Medicine. 2005;118(9):1019–25. doi: 10.1016/j.amjmed.2004.12.035. [DOI] [PubMed] [Google Scholar]
- Chisholm MA, Mulloy LL, Jagadeesan M, Martin BC, DiPiro JT. Effect of clinical pharmacy services on the blood pressure of African-American renal transplant patients. Ethnicity & Disease. 2002;12(3):392–97. [PubMed] [Google Scholar]
- Cifuentes M, Fernald DH, Green LA, Niebauer LJ, Crabtree BF, Stange KC, Hassmiller SB. Prescription for health: Changing primary care practice to foster healthy behaviors. Annals of Family Medicine. 2005;3(suppl 2):S4–11. doi: 10.1370/afm.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: Secondary prevention programs for patients with coronary artery disease. Annals of Internal Medicine. 2005;143(9):659–72. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- Clark LT, Maki KC, Galant R, Maron DJ, Pearson TA, Davidson MH. Ethnic differences in achievement of cholesterol treatment goals. Results from the National Cholesterol Education Program Evaluation Project Utilizing Novel E-Technology II. Journal of General Internal Medicine. 2006;21(4):320–26. doi: 10.1111/j.1525-1497.2006.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coble JD, Rhodes RE. Physical activity and Native Americans: A review. American Journal of Preventive Medicine. 2006;31(1):36–46. doi: 10.1016/j.amepre.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine. 2006;166(17):1822–28. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- Committee on Quality Health Care in America: Institute of Medicine . Crossing the quality chasm: A new health system for the 21st century. National Academy Press; Washington, DC: 2001. [Google Scholar]
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care: Institute of Medicine . In: Unequal treatment: Confronting racial and ethnic disparities in health care. Smedley BD, Stith AY, Nelson AR, editors. National Academy Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: Observational follow-up of the Trials of Hypertension Prevention (TOHP) BMJ. 2007;334(7599):885. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry SJ, Ludman EJ, Graham E, Stout J, Grothaus L, Lozano P. Pediatric-based smoking cessation intervention for low-income women: A randomized trial. Archives of Pediatric and Adolescent Medicine. 2003;157(3):295–302. doi: 10.1001/archpedi.157.3.295. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Hermann JA, Coresh J, Powe NR. Use of cardiovascular procedures among black persons and white persons: A 7-year nationwide study in patients with renal disease. Annals of Internal Medicine. 1999;130(3):173–82. doi: 10.7326/0003-4819-130-3-199902020-00002. [DOI] [PubMed] [Google Scholar]
- Davies SL, Kohler CL, Fish L, Taylor BE, Foster GE, Annang L. Evaluation of an intervention for hospitalized African American smokers. American Journal of Health Behavior. 2005;29(3):228–39. doi: 10.5993/ajhb.29.3.4. [DOI] [PubMed] [Google Scholar]
- de Lusignan S, Hague N, Brown A, Majeed A. An educational intervention to improve data recording in the management of ischaemic heart disease in primary care. Journal of Public Health. 2004;26(1):34–37. doi: 10.1093/pubmed/fdh104. [DOI] [PubMed] [Google Scholar]
- Dennison CR, Post WS, Kim MT, Bone LR, Cohen D, Blumenthal RS, Rame JE, Roary MC, Levine DM, Hill MN. Underserved urban African American men: Hypertension trial outcomes and mortality during 5 years. American Journal of Hypertension. 2007;20(2):164–71. doi: 10.1016/j.amjhyper.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Denver EA, Barnard M, Woolfson RG, Earle KA. Management of uncontrolled hypertension in a nurse-led clinic compared with conventional care for patients with type 2 diabetes. Diabetes Care. 2003;26(8):2256–60. doi: 10.2337/diacare.26.8.2256. [DOI] [PubMed] [Google Scholar]
- Deswal A, Petersen NJ, Souchek J, Ashton CM, Wray NP. Impact of race on health care utilization and outcomes in veterans with congestive heart failure. Journal of the American College of Cardiology. 2004;43(5):778–84. doi: 10.1016/j.jacc.2003.10.033. [DOI] [PubMed] [Google Scholar]
- DeWalt DA, Pignone M, Malone R, Rawls C, Kosnar MC, George G, Bryant B, Rothman RL, Angel B. Development and pilot testing of a disease management program for low literacy patients with heart failure. Patient Education and Counseling. 2004;55(1):78–86. doi: 10.1016/j.pec.2003.06.002. [DOI] [PubMed] [Google Scholar]
- Dickinson HO, Nicolson DJ, Campbell F, Beyer FR, Mason J. Potassium supplementation for the management of primary hypertension in adults. Cochrane Database of Systematic Reviews. 2006;3 doi: 10.1002/14651858.CD004641.pub2. CD004641. [DOI] [PubMed] [Google Scholar]
- Doescher MP, Saver BG, Fiscella K, Franks P. Racial/ethnic inequities in continuity and site of care: Location, location, location. Health Services Research. 2001;36(6 pt 2):78–89. [PMC free article] [PubMed] [Google Scholar]
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health. 1998;52(6):377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction. New England Journal of Medicine. 1999;340(8):609–16. doi: 10.1056/NEJM199902253400804. [DOI] [PubMed] [Google Scholar]
- Dries DL, Strong MH, Cooper RS, Drazner MH. Efficacy of angiotensin-converting enzyme inhibition in reducing progression from asymptomatic left ventricular dysfunction to symptomatic heart failure in black and white patients. Journal of the American College of Cardiology. 2002;40(2):311–17. doi: 10.1016/s0735-1097(02)01943-5. [DOI] [PubMed] [Google Scholar]
- Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: Cluster randomised controlled trial. BMJ. 2003;326(7393):793. doi: 10.1136/bmj.326.7393.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmer PJ, Obarzanek E, Vollmer WM, Simons-Morton D, Stevens VJ, Young DR, Lin PH, Champagne C, Harsha DW, Svetkey LP, Ard J, Brantley PJ, Proschan MA, Erlinger TP, Appel LJ. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Annals of Internal Medicine. 2006;144(7):485–95. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- Epstein AM, Weissman JS, Schneider EC, Gatsonis C, Leape LL, Piana RN. Race and gender disparities in rates of cardiac revascularization: Do they reflect appropriate use of procedures or problems in quality of care? Medical Care. 2003;41(11):1240–55. doi: 10.1097/01.MLR.0000093423.38746.8C. [DOI] [PubMed] [Google Scholar]
- Erickson SR, Slaughter R, Halapy H. Pharmacists’ ability to influence outcomes of hypertension therapy. Pharmacotherapy. 1997;17(1):140–47. [PubMed] [Google Scholar]
- Erlinger TP, Vollmer WM, Svetkey LP, Appel LJ. The potential impact of nonpharmacologic population-wide blood pressure reduction on coronary heart disease events: Pronounced benefits in African-Americans and hypertensives. Preventive Medicine. 2003;37(4):327–33. doi: 10.1016/s0091-7435(03)00140-3. [DOI] [PubMed] [Google Scholar]
- Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database of Systematic Reviews. 2005;1 doi: 10.1002/14651858.CD005182. CD005182. [DOI] [PubMed] [Google Scholar]
- Fedder DO, Chang RJ, Curry S, Nichols G. The effectiveness of a community health worker outreach program on healthcare utilization of west Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethnicity & Disease. 2003;13(1):22–27. [PubMed] [Google Scholar]
- Fiscella K, Franks P. Should years of schooling be used to guide treatment of coronary risk factors? Annals of Family Medicine. 2004;2(5):469–73. doi: 10.1370/afm.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, Franks P. Does the content of primary care visits differ by the racial composition of physicians’ practices? American Journal of Medicine. 2006;119(4):348–53. doi: 10.1016/j.amjmed.2005.08.040. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: Implications for urban health care. Academic Medicine. 2004;79(12):1139–47. doi: 10.1097/00001888-200412000-00004. [DOI] [PubMed] [Google Scholar]
- Fisher E, Musick J, Scott C, Miller JP, Gram R, Richardson V, Clark J, Pachalla V. Improving clinic- and neighborhood-based smoking cessation services within federally qualified health centers serving low-income, minority neighborhoods. Nicotine & Tobacco Research. 2005;7(suppl 1):S45–56. doi: 10.1080/14622200500078105. [DOI] [PubMed] [Google Scholar]
- Fisher T, Burnet DL, Huang ES, Chin MH, Cagney K. Cultural leverage: Interventions utilizing culture to narrow racial disparities in health care. Medical Care Research and Review. 2007;64(5 Suppl):243S–282S. doi: 10.1177/1077558707305414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadegbeku CA, Lea JP, Jamerson KA. Update on disparities in the pathophysiology and management of hypertension: Focus on African Americans. Medical Clinics of North America. 2005;89(5):921–33. doi: 10.1016/j.mcna.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Gauri AJ, Davis A, Hong T, Burke MC, Knight BP. Disparities in the use of primary prevention and defibrillator therapy among blacks and women. American Journal of Medicine. 2006;119(2):e17–21. doi: 10.1016/j.amjmed.2005.08.021. 167. [DOI] [PubMed] [Google Scholar]
- Gemson DH, Ashford AR, Dickey LL, Raymore SH, Roberts JW, Ehrlich MH, Foster BG, Ganz ML, Moon-Howard J, Field LS, et al. Putting prevention into practice. Impact of a multifaceted physician education program on preventive services in the inner city. Archives of Internal Medicine. 1995;155(20):2210–16. doi: 10.1001/archinte.155.20.2210. [DOI] [PubMed] [Google Scholar]
- Genkinger JM, Jehn ML, Sapun M, Mabry I, Young DR. Does weight status influence perceptions of physical activity barriers among African-American women? Ethnicity & Disease. 2006;16(1):78–84. [PubMed] [Google Scholar]
- Glover MJ. Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999-2002. Morbidity and Mortality Weekly Report. 2005;54(1):7–9. [PubMed] [Google Scholar]
- Godfrey MM, Nelson EC, Wasson JH, Mohr JJ, Batalden PB. Microsystems in health care: Part 3. Planning patient-centered services. Joint Commission Journal on Quality and Patient Safety. 2003;29(4):159–70. doi: 10.1016/s1549-3741(03)29020-1. [DOI] [PubMed] [Google Scholar]
- Gordon HS, Paterniti DA, Wray NP. Race and patient refusal of invasive cardiac procedures. Journal of General Internal Medicine. 2004;19(9):962–66. doi: 10.1111/j.1525-1497.2004.30131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimshaw JM, Winkens RA, Shirran L, Cunningham C, Mayhew A, Thomas R, Fraser C. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database of Systematic Reviews. 2005;3 doi: 10.1002/14651858.CD005471. CD005471. [DOI] [PubMed] [Google Scholar]
- Groeneveld PW, Sonnad SS, Lee AK, Asch DA, Shea JE. Racial differences in attitudes toward innovative medical technology. Journal of General Internal Medicine. 2006;21(6):559–63. doi: 10.1111/j.1525-1497.2006.00453.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossbart SR. What’s the return? Assessing the effect of “pay-for-performance” initiatives on the quality of care delivery. Medical Care Research Review. 2006;63(1 suppl):S29S–48. doi: 10.1177/1077558705283643. [DOI] [PubMed] [Google Scholar]
- Hannan EL, van Ryn M, Burke J, Stone D, Kumar D, Arani D, Pierce W, Rafii S, Sanborn TA, Sharma S, Slater J, DeBuono BA. Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Medical Care. 1999;37(1):68–77. doi: 10.1097/00005650-199901000-00010. [DOI] [PubMed] [Google Scholar]
- Harkness K, Smith KM, Taraba L, Mackenzie CL, Gunn E, Arthur HM. Effect of a postoperative telephone intervention on attendance at intake for cardiac rehabilitation after coronary artery bypass graft surgery. Heart & Lung. 2005;34(3):179–86. doi: 10.1016/j.hrtlng.2004.07.010. [DOI] [PubMed] [Google Scholar]
- Harris C, Ayala C, Dai S, Croft JB. Disparities in deaths from stroke among persons aged <75 years—United States, 2002. Morbidity and Mortality Weekly Report. 2005;54(19):477–81. [PubMed] [Google Scholar]
- Haskell WL, Berra K, Arias E, Christopherson D, Clark A, George J, Hyde S, Klieman L, Myll J. Multifactor cardiovascular disease risk reduction in medically underserved, high-risk patients. American Journal of Cardiology. 2006;98(11):1472–79. doi: 10.1016/j.amjcard.2006.06.049. [DOI] [PubMed] [Google Scholar]
- Hayes DK. Racial/ethnic and socioeconomic disparities in multiple risk factors for heart disease and stroke—United States, 2003. Morbidity and Mortality Weekly Report. 2005;54(5):113–17. [PubMed] [Google Scholar]
- He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Archives of Internal Medicine. 2001;161(7):996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- Hertz RP, Unger AN, Ferrario CM. Diabetes, hypertension, and dyslipidemia in Mexican Americans and non-Hispanic whites. American Journal of Preventive Medicine. 2006;30(2):103–10. doi: 10.1016/j.amepre.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Hess PL, Reingold JS, Jones J, Fellman MA, Knowles P, Ravenell JE, Kim S, Raju J, Ruger E, Clark S, Okoro C, Ogunji O, Knowles P, Leonard D, Wilson RP, Haley RW, Ferdinand KC, Freeman A, Victor RG. Barbershops as hypertension detection, referral, and follow-up centers for black men. Hypertension. 2007;49(5):1040–46. doi: 10.1161/HYPERTENSIONAHA.106.080432. [DOI] [PubMed] [Google Scholar]
- Hicks LS, Shaykevich S, Bates DW, Ayanian JZ. Determinants of racial/ethnic differences in blood pressure management among hypertensive patients. BMC Cardiovascular Disorders. 2005;5(1):16. doi: 10.1186/1471-2261-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men: Recruitment, follow-up, and outcomes. American Journal of Hypertension. 1999;12(6):548–54. doi: 10.1016/s0895-7061(99)00007-2. [DOI] [PubMed] [Google Scholar]
- Hill MN, Han H-R, Dennison CR, Kim MT, Roary MC, Blumenthal RS, Bone LR, Levine DM, Post WS. Hypertension care and control in underserved urban African American men: Behavioral and physiologic outcomes at 36 months. American Journal of Hypertension. 2003;16(11 pt 1):906–13. doi: 10.1016/s0895-7061(03)01034-3. [DOI] [PubMed] [Google Scholar]
- Horner RD, Salazar W, Geiger HJ, Bullock K, Corbie-Smith G, Cornog M, Flores G. Changing healthcare professionals’ behaviors to eliminate disparities in healthcare: What do we know? How might we proceed? American Journal of Managed Care. 2004;10(spec no):SP12–19. [PubMed] [Google Scholar]
- Horner RD, Swanson JW, Bosworth HB, Matchar DB. Effects of race and poverty on the process and outcome of inpatient rehabilitation services among stroke patients. Stroke. 2003;34(4):1027–31. doi: 10.1161/01.STR.0000060028.60365.5D. [DOI] [PubMed] [Google Scholar]
- Houston TK, Scarinci IC, Person SD, Greene PG. Patient smoking cessation advice by health care providers: The role of ethnicity, socioeconomic status, and health. American Journal of Public Health. 2005;95(6):1056–61. doi: 10.2105/AJPH.2004.039909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hozawa A, Folsom AR, Sharrett AR, Chambless LE. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: Comparison of African American with white subjects—Atherosclerosis Risk in Communities Study. Archives of Internal Medicine. 2007;167(6):573–79. doi: 10.1001/archinte.167.6.573. [DOI] [PubMed] [Google Scholar]
- Hsia J, Margolis KL, Eaton CB, Wenger NK, Allison M, Wu L, LaCroix AZ, Black HR. Prehypertension and cardiovascular disease risk in the Women’s Health Initiative. Circulation. 2007;115(7):855–60. doi: 10.1161/CIRCULATIONAHA.106.656850. [DOI] [PubMed] [Google Scholar]
- Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. Journal of General Internal Medicine. 2006;21(6):642–47. doi: 10.1111/j.1525-1497.2006.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins RG, Ornstein SM, Nietert PJ, Klockars SJ, Thiedke C. Quality improvement for prevention of cardiovascular disease and stroke in an academic family medicine center: Do racial differences in outcome exist? Ethnicity & Disease. 2006;16(1):132–37. [PubMed] [Google Scholar]
- Johnson KM, Lando HA, Schmid LS, Solberg LI. The GAINS project: Outcome of smoking cessation strategies in four urban Native American clinics. Giving American Indians No-smoking Strategies. Addictive Behaviors. 1997;22(2):207–18. doi: 10.1016/s0306-4603(96)00015-9. [DOI] [PubMed] [Google Scholar]
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. American Journal of Public Health. 2004;94(12):2084–90. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn J, Sankar P. Being specific about race-specific medicine. Health Affairs (Millwood) 2006;25(5):375–77. doi: 10.1377/hlthaff.25.w375. [DOI] [PubMed] [Google Scholar]
- Kaplan RC, Bhalodkar NC, Brown EJ, Jr., White J, Brown DL. Race, ethnicity, and sociocultural characteristics predict noncompliance with lipid-lowering medications. Preventive Medicine. 2004;39(6):1249–55. doi: 10.1016/j.ypmed.2004.04.041. [DOI] [PubMed] [Google Scholar]
- Keyserling TC, Ammerman AS, Davis CE, Mok MC, Garrett J, Simpson R., Jr. A randomized controlled trial of a physician-directed treatment program for low-income patients with high blood cholesterol: The Southeast Cholesterol Project. Archives of Family Medicine. 1997;6(2):135–45. doi: 10.1001/archfami.6.2.135. [DOI] [PubMed] [Google Scholar]
- Kimm SY, Glynn NW, Kriska AM, Barton BA, Kronsberg SS, Daniels SR, Crawford PB, Sabry ZI, Liu K. Decline in physical activity in black girls and white girls during adolescence. New England Journal of Medicine. 2002;347(10):709–15. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- Kindig DA, Thompson GE. The right to equal treatment: An action plan to end racial and ethnic disparities in clinical diagnosis and treatment in the United States. Physicians for Human Rights; Boston: 2003. [Google Scholar]
- Klerman LV, Ramey SL, Goldenberg RL, Marbury S, Hou J, Cliver SP. A randomized trial of augmented prenatal care for multiple-risk, Medicaid-eligible African American women. American Journal of Public Health. 2001;91(1):105–11. doi: 10.2105/ajph.91.1.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokkinos PF, Narayan P, Colleran JA, Pittaras A, Notargiacomo A, Reda D, Papademetriou V. Effects of regular exercise on blood pressure and left ventricular hypertrophy in African-American men with severe hypertension. New England Journal of Medicine. 1995;333(22):1462–67. doi: 10.1056/NEJM199511303332204. [DOI] [PubMed] [Google Scholar]
- Kokkinos PF, Narayan P, Colleran J, Fletcher RD, Lakshman R, Papademetriou V. Effects of moderate intensity exercise on serum lipids in African-American men with severe systemic hypertension. American Journal of Cardiology. 1998;81(6):732–35. doi: 10.1016/s0002-9149(97)01020-5. [DOI] [PubMed] [Google Scholar]
- Konety SH, Vaughan Sarrazin MS, Rosenthal GE. Patient and hospital differences underlying racial variation in outcomes after coronary artery bypass graft surgery. Circulation. 2005;111(10):1210–16. doi: 10.1161/01.CIR.0000157728.49918.9F. [DOI] [PubMed] [Google Scholar]
- Kressin NR. Separate but not equal: The consequences of segregated health care. Circulation. 2005;112(17):2582–84. doi: 10.1161/CIRCULATIONAHA.105.577635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kressin NR, Chang BH, Whittle J, Peterson ED, Clark JA, Rosen AK, Orner M, Collins TC, Alley LG, Petersen LA. Racial differences in cardiac catheterization as a function of patients’ beliefs. American Journal of Public Health. 2004;94(12):2091–97. doi: 10.2105/ajph.94.12.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J, Collier C, Song L, Martin D. Linking community-based blood pressure measurement to clinical care: A randomized controlled trial of outreach and tracking by community health workers. American Journal of Public Health. 1999;89(6):856–61. doi: 10.2105/ajph.89.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: A systematic review. Archives of Internal Medicine. 2007;167(6):540–50. doi: 10.1001/archinte.167.6.540. [DOI] [PubMed] [Google Scholar]
- Kruger AJ. Trends in leisure-time physical inactivity by age, sex, and race/ethnicity—United States, 1994-2004. Morbidity and Mortality Weekly Report. 2005;54(39):991–94. [PubMed] [Google Scholar]
- Krumholz HM, Currie PM, Riegel B, Phillips CO, Peterson ED, Smith R, Yancy CW, Faxon DP. A taxonomy for disease management: A scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation. 2006;114(13):1432–45. doi: 10.1161/CIRCULATIONAHA.106.177322. [DOI] [PubMed] [Google Scholar]
- Kumanyika SK, Adams-Campbell L, Van Horn B, Ten Have TR, Treu JA, Askov E, Williams J, Achterberg C, Zaghloul S, Monsegu D, Bright M, Stoy DB, Malone-Jackson M, Mooney D, Deiling S, Caulfield J. Outcomes of a cardiovascular nutrition counseling program in African-Americans with elevated blood pressure or cholesterol level. Journal of the American Dietetic Association. 1999;99(11):1380–91. doi: 10.1016/S0002-8223(99)00336-3. [DOI] [PubMed] [Google Scholar]
- Kumanyika SK, Cook NR, Cutler JA, Belden L, Brewer A, Cohen JD, Hebert PR, Lasser VI, Raines J, Raczynski J, Shepek L, Diller L, Whelton PK, Yamamoto M. Sodium reduction for hypertension prevention in overweight adults: Further results from the Trials of Hypertension Prevention Phase II. Journal of Human Hypertension. 2005;19(1):33–45. doi: 10.1038/sj.jhh.1001774. [DOI] [PubMed] [Google Scholar]
- Lafata JE, Pladevall M, Divine G, Ayoub M, Philbin EF. Are there race/ethnicity differences in outpatient congestive heart failure management, hospital use, and mortality among an insured population? Medical Care. 2004;42(7):680–89. doi: 10.1097/01.mlr.0000129903.12843.fc. [DOI] [PubMed] [Google Scholar]
- Lappe JM, Muhlestein JB, Lappe DL, Badger RS, Bair TL, Brockman R, French TK, Hofmann LC, Horne BD, Kralick-Goldberg S, Nicponski N, Orton JA, Pearson RR, Renlund DG, Rimmasch H, Roberts C, Anderson JL. Improvements in 1-year cardiovascular clinical outcomes associated with a hospital-based discharge medication program. Annals of Internal Medicine. 2004;141(6):446–53. doi: 10.7326/0003-4819-141-6-200409210-00010. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Arthur M, Morgan A, Plantholt S, Rubinstein M. Explaining racial differences in receipt of coronary angiography: The role of physician referral and physician specialty. Medical Care Research Review. 2003;60(4):453–67. doi: 10.1177/1077558703255685. discussion 496-508. [DOI] [PubMed] [Google Scholar]
- Lavizzo-Mourey R, Jung M. Fighting unequal treatment: The Robert Wood Johnson Foundation and a quality-improvement approach to disparities. Circulation. 2005;111(10):1208–9. doi: 10.1161/01.CIR.0000157739.93631.EB. [DOI] [PubMed] [Google Scholar]
- Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: A randomized controlled trial. Journal of the American Medical Association. 2006;296(21):2563–71. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- Lenz ER, Mundinger MO, Kane RL, Hopkins SC, Lin SX. Primary care outcomes in patients treated by nurse practitioners or physicians: Two-year follow-up. Medical Care Research Review. 2004;61(3):332–51. doi: 10.1177/1077558704266821. [DOI] [PubMed] [Google Scholar]
- Levine DM, Bone LR, Hill MN, Stallings R, Gelber AC, Barker A, Harris EC, Zeger SL, Felix-Aaron KL, Clark JM. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African-American population. Ethnicity & Disease. 2003;13(3):354–61. see comment. [PubMed] [Google Scholar]
- Levine RS, Foster JE, Fullilove RE, Fullilove MT, Briggs NC, Hull PC, Husaini BA, Hennekens CH. Black-white inequalities in mortality and life expectancy, 1933-1999: Implications for healthy people 2010. Public Health Reports. 2001;116(5):474–83. doi: 10.1093/phr/116.5.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillington L, Royce J, Novak D, Ruvalcaba M, Chlebowski R. Evaluation of a smoking cessation program for pregnant minority women. Cancer Practice. 1995;3(3):157–63. [PubMed] [Google Scholar]
- Lipkus IM, Lyna PR, Rimer BK. Using tailored interventions to enhance smoking cessation among African-Americans at a community health center. Nicotine & Tobacco Research. 1999;1(1):77–85. doi: 10.1080/14622299050011181. [DOI] [PubMed] [Google Scholar]
- Liu JH, Zingmond DS, McGory ML, SooHoo NF, Ettner SL, Brook RH, Ko CY. Disparities in the utilization of high-volume hospitals for complex surgery. Journal of the American Medical Association. 2006;296(16):1973–80. doi: 10.1001/jama.296.16.1973. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Crum RM, Neumark YD. Racial/ethnic disparities in report of physician-provided smoking cessation advice: Analysis of the 2000 National Health Interview Survey. American Journal of Public Health. 2006;96(12):2235–39. doi: 10.2105/AJPH.2005.071035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, Gonzalez VM. Hispanic chronic disease self-management: A randomized community-based outcome trial. Nursing Research. 2003;52(6):361–69. doi: 10.1097/00006199-200311000-00003. [DOI] [PubMed] [Google Scholar]
- Ma J, Sehgal NL, Ayanian JZ, Stafford RS. National trends in statin use by coronary heart disease risk category. PLoS Medicine. 2005;2(5):e123. doi: 10.1371/journal.pmed.0020123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfredi C, Crittenden KS, Warnecke R, Engler J, Cho YI, Shaligram C. Evaluation of a motivational smoking cessation intervention for women in public health clinics. Preventive Medicine. 1999;28(1):51–60. doi: 10.1006/pmed.1998.0377. [DOI] [PubMed] [Google Scholar]
- Matson Koffman DM, Goetzel RZ, Anwuri VV, Shore KK, Orenstein D, LaPier T. Heart healthy and stroke free: Successful business strategies to prevent cardiovascular disease. American Journal of Preventive Medicine. 2005;29(5 suppl 1):113–21. doi: 10.1016/j.amepre.2005.07.017. [DOI] [PubMed] [Google Scholar]
- Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Medical Care Research Review. 2000;57(suppl 1):108–45. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- McBride CM, Bepler G, Lipkus IM, Lyna P, Samsa G, Albright J, Datta S, Rimer BK. Incorporating genetic susceptibility feedback into a smoking cessation program for African-American smokers with low income. Cancer Epidemiology, Biomarkers & Prevention. 2002;11(6):521–28. [PubMed] [Google Scholar]
- McDowell SE, Coleman JJ, Ferner RE. Systematic review and meta-analysis of ethnic differences in risks of adverse reactions to drugs used in cardiovascular medicine. BMJ. 2006;332(7551):1177–81. doi: 10.1136/bmj.38803.528113.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta RH, Marks D, Califf RM, Sohn S, Pieper KS, Van de Werf F, Peterson ED, Ohman EM, White HD, Topol EJ, Granger CB. Differences in the clinical features and outcomes in African Americans and whites with myocardial infarction. American Journal of Medicine. 2006;119(1):e1–8. doi: 10.1016/j.amjmed.2005.07.043. 70. [DOI] [PubMed] [Google Scholar]
- Mensah GA, Brown DW. An overview of cardiovascular disease burden in the United States. Health Affairs (Millwood) 2007;26(1):38–48. doi: 10.1377/hlthaff.26.1.38. [DOI] [PubMed] [Google Scholar]
- Mickelson JK, Blum CM, Geraci JM. Acute myocardial infarction: Clinical characteristics, management and outcome in a metropolitan Veterans Affairs Medical Center teaching hospital. Journal of the American College of Cardiology. 1997;29(5):915–25. doi: 10.1016/s0735-1097(97)00034-x. [DOI] [PubMed] [Google Scholar]
- Mobley LR, Root ED, Finkelstein EA, Khavjou O, Farris RP, Will JC. Environment, obesity, and cardiovascular disease risk in low-income women. American Journal of Preventive Medicine. 2006;30(4):327–32. doi: 10.1016/j.amepre.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, Mensah GA, Morris DL, Pancioli AM, Riegel B, Zerwic JJ. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: A scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114(2):168–82. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- Nagykaldi Z, Mold JW, Aspy CB. Practice facilitators: A review of the literature. Family Medicine. 2005;37(8):581–88. [PubMed] [Google Scholar]
- Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society. 2004;52(5):675–84. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- NCHS QuickStats: Use of stents among hospitalized patients undergoing coronary angioplasty, by race—United States. Morbidity and Mortality Weekly Report. 2006;2003;54(12):309. [Google Scholar]
- Nevid JS, Javier RA. Preliminary investigation of a culturally specific smoking cessation intervention for Hispanic smokers. American Journal of Health Promotion. 1997;11(3):198–207. doi: 10.4278/0890-1171-11.3.198. [DOI] [PubMed] [Google Scholar]
- Newton RL, Jr., Perri MG. A randomized pilot trial of exercise promotion in sedentary African-American adults. Ethnicity & Disease. 2004;14(4):548–57. [PubMed] [Google Scholar]
- Nollen NL, Mayo MS, Sanderson Cox L, Okuyemi KS, Choi WS, Kaur H, Ahluwalia JS. Predictors of quitting among African American light smokers enrolled in a randomized, placebo-controlled trial. Journal of General Internal Medicine. 2006;21(6):590–95. doi: 10.1111/j.1525-1497.2006.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connell AM, Crawford MH, Abrams J. Heart failure disease management in an indigent population. American Heart Journal. 2001;141(2):254–58. doi: 10.1067/mhj.2001.111956. [DOI] [PubMed] [Google Scholar]
- Ofman JJ, Badamgarav E, Henning JM, Knight K, Gano AD, Jr., Levan RK, Gur-Arie S, Richards MS, Hasselblad V, Weingarten SR. Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. American Journal of Medicine. 2004;117(3):182–92. doi: 10.1016/j.amjmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- Oh SS. Disparities in premature deaths from heart disease—50 states and the District of Columbia, 2001. Morbidity and Mortality Weekly Report. 2004;53(6):121–25. [PubMed] [Google Scholar]
- Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- Palmieri J, Redline S, Morita R. Goal attainment in patients referred to a telephone-based dyslipidemia program. American Journal of Health System Pharmacy. 2005;62(15):1586–91. doi: 10.2146/ajhp040343. [DOI] [PubMed] [Google Scholar]
- Panel on Dietary Reference Intakes for Electrolytes and Water: Institute of Medicine . Dietary reference intakes: Water, potassium, sodium chloride, and sulfate. 1st ed National Academy Press; Washington, DC: 2004. [Google Scholar]
- Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Archives of Internal Medicine. 2003;163(4):427–36. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker RM, Ratzan SC, Lurie N. Health literacy: A policy challenge for advancing high-quality health care. Health Affairs (Millwood) 2003;22(4):147–53. doi: 10.1377/hlthaff.22.4.147. [DOI] [PubMed] [Google Scholar]
- Persell SD, Maviglia SM, Bates DW, Ayanian JZ. Ambulatory hypercholesterolemia management in patients with atherosclerosis. Gender and race differences in processes and outcomes. Journal of General Internal Medicine. 2005;20(2):123–30. doi: 10.1111/j.1525-1497.2005.40155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary-revascularization procedures. Are the differences real? Do they matter? New England Journal of Medicine. 1997;336(7):480–86. doi: 10.1056/NEJM199702133360706. [DOI] [PubMed] [Google Scholar]
- Peterson ED, Wright SM, Daley J, Thibault GE. Racial variation in cardiac procedure use and survival following acute myocardial infarction in the Department of Veterans Affairs. Journal of the American Medical Association. 1994;271(15):1175–80. [PubMed] [Google Scholar]
- Pezzin LE, Keyl PM, Green GB. Disparities in the emergency department evaluation of chest pain patients. Academic Emergency Medicine. 2007;14(2):149–56. doi: 10.1197/j.aem.2006.08.020. [DOI] [PubMed] [Google Scholar]
- Pickering TG. New guidelines on diet and blood pressure. Hypertension. 2006;47(2):135–36. doi: 10.1161/01.HYP.0000202417.57909.26. [DOI] [PubMed] [Google Scholar]
- Poston WS, II, Haddock CK, Olvera NE, Suminski RR, Reeves RS, Dunn JK, Hanis CL, Foreyt JP. Evaluation of a culturally appropriate intervention to increase physical activity. American Journal of Health Behavior. 2001;25(4):396–406. doi: 10.5993/ajhb.25.4.5. [DOI] [PubMed] [Google Scholar]
- Prevalence of Heart Disease—United States, 2005. Morbidity and Mortality Weekly Report. 2007;56(6):113–18. [PubMed] [Google Scholar]
- Price EG, Beach MC, Gary TL, Robinson KA, Gozu A, Palacio A, Smarth C, Jenckes M, Feuerstein C, Bass EB, Powe NR, Cooper LA. A systematic review of the methodological rigor of studies evaluating cultural competence training of health professionals. Academic Medicine. 2005;80(6):578–86. doi: 10.1097/00001888-200506000-00013. [DOI] [PubMed] [Google Scholar]
- Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. Journal of the American Medical Association. 2007;297(10):1063–72. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- Ranjit N, Diez-Roux AV, Shea S, Cushman M, Seeman T, Jackson SA, Ni H. Psychosocial factors and inflammation in the multi-ethnic study of atherosclerosis. Archives of Internal Medicine. 2007;167(2):174–81. doi: 10.1001/archinte.167.2.174. [DOI] [PubMed] [Google Scholar]
- Rathore SS, Foody JM, Wang Y, Smith GL, Herrin J, Masoudi FA, Wolfe P, Havranek EP, Ordin DL, Krumholz HM. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. Journal of the American Medical Association. 2003;289(19):2517–24. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- Rathore SS, Masoudi FA, Havranek EP, Krumholz HM. Regional variations in racial differences in the treatment of elderly patients hospitalized with acute myocardial infarction. American Journal of Medicine. 2004;117(11):811–22. doi: 10.1016/j.amjmed.2004.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redberg RF. Gender, race, and cardiac care: Why the differences? Journal of the American College of Cardiology. 2005;46(10):1852–54. doi: 10.1016/j.jacc.2005.07.043. [DOI] [PubMed] [Google Scholar]
- Rehman SU, Hutchison FN, Hendrix K, Okonofua EC, Egan BM. Ethnic differences in blood pressure control among men at Veterans Affairs clinics and other health care sites. Archives of Internal Medicine. 2005;165(9):1041–47. doi: 10.1001/archinte.165.9.1041. [DOI] [PubMed] [Google Scholar]
- Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. New England Journal of Medicine. 1995;333(18):1190–95. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- Rimmer JH, Nicola T, Riley B, Creviston T. Exercise training for African Americans with disabilities residing in difficult social environments. American Journal of Preventive Medicine. 2002;23(4):290–95. doi: 10.1016/s0749-3797(02)00517-2. [DOI] [PubMed] [Google Scholar]
- Roe MT. Success stories: How hospitals are improving care. American Heart Journal. 2004;148(5 Suppl):S52–5. doi: 10.1016/j.ahj.2004.09.017. [DOI] [PubMed] [Google Scholar]
- Rogers MA, Small D, Buchan DA, Butch CA, Stewart CM, Krenzer BE, Husovsky HL. Home monitoring service improves mean arterial pressure in patients with essential hypertension. A randomized, controlled trial. Annals of Internal Medicine. 2001;134(11):1024–32. doi: 10.7326/0003-4819-134-11-200106050-00008. [DOI] [PubMed] [Google Scholar]
- Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, Haase N, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell CJ, Roger V, Rumsfeld J, Sorlie P, Steinberger J, Thom T, Wasserthiel-Smoller S, Hong Y. Heart disease and stroke statistics—2007 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- Royce JM, Ashford A, Resnicow K, Freeman HP, Caesar AA, Orlandi MA. Physician- and nurse-assisted smoking cessation in Harlem. Journal of the National Medical Association. 1995;87(4):291–300. [PMC free article] [PubMed] [Google Scholar]
- Rumsfeld JS, Epstein AJ. Racial disparities in cardiovascular procedure outcomes: Turn down the volume. Journal of the American College of Cardiology. 2006;47(2):425–26. doi: 10.1016/j.jacc.2005.10.025. [DOI] [PubMed] [Google Scholar]
- Russo CA, Andrews RM, Coffey RM. Racial and ethnic disparities in potentially preventable hospitalizations. ARHQ; Rockville, MD: 2006. 2003. [PubMed] [Google Scholar]
- Sabatine MS, Blake GJ, Drazner MH, Morrow DA, Scirica BM, Murphy SA, McCabe CH, Weintraub WS, Gibson CM, Cannon CP. Influence of race on death and ischemic complications in patients with non-ST-elevation acute coronary syndromes despite modern, protocol-guided treatment. Circulation. 2005;111(10):1217–24. doi: 10.1161/01.CIR.0000157733.50479.B9. [DOI] [PubMed] [Google Scholar]
- Salisbury C, Fahey T. Overcoming clinical inertia in the management of hypertension. Canadian Medical Association Journal. 2006;174(9):1285–86. doi: 10.1503/cmaj.060243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders KM, Satyvavolu A. Improving blood pressure control in diabetes: Limitations of a clinical reminder in influencing physician behavior. Journal of Continuing Education in the Health Professions. 2002;22(1):23–32. doi: 10.1002/chp.1340220104. [DOI] [PubMed] [Google Scholar]
- Satcher D. Priorities among effective clinical preventive services: A commentary. American Journal of Preventive Medicine. 2006;31(1):97–98. doi: 10.1016/j.amepre.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Satcher D, Fryer GE, Jr., McCann J, Troutman A, Woolf SH, Rust G. What if we were equal? A comparison of the black-white mortality gap in 1960 and 2000. Health Affairs (Millwood) 2005;24(2):459–64. doi: 10.1377/hlthaff.24.2.459. [DOI] [PubMed] [Google Scholar]
- Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in Medicare managed care. Journal of the American Medical Association. 2002;287(10):1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- Schneider RH, Staggers F, Alxander CN, Sheppard W, Rainforth M, Kondwani K, Smith S, King CG. A randomised controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26(5):820–27. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- Schneiderman N, Saab PG, Catellier DJ, Powell LH, DeBusk RF, Williams RB, Carney RM, Raczynski JM, Cowan MJ, Berkman LF, Kaufmann PG. Psychosocial treatment within sex by ethnicity subgroups in the Enhancing Recovery in Coronary Heart Disease clinical trial. Psychosomatic Medicine. 2004;66(4):475–83. doi: 10.1097/01.psy.0000133217.96180.e8. [DOI] [PubMed] [Google Scholar]
- Schore J, Brown R, Lavin B. Racial disparities in prescription drug use among dually eligible beneficiaries. Health Care Financing Review. 2003;25(2):77–90. [PMC free article] [PubMed] [Google Scholar]
- Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dube R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Escarce JJ. The effect of race and sex on physicians’ recommendations for cardiac catheterization. New England Journal of Medicine. 1999;340(8):618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Peck WA. Enhancing the potential of quality improvement organizations to improve quality of care. Annals of Internal Medicine. 2006;145(5):388–89. doi: 10.7326/0003-4819-145-5-200609050-00138. [DOI] [PubMed] [Google Scholar]
- Sisk JE, Hebert PL, Horowitz CR, McLaughlin MA, Wang JJ, Chassin MR. Effects of nurse management on the quality of heart failure care in minority communities: A randomized trial. Annals of Internal Medicine. 2006;145(4):273–83. doi: 10.7326/0003-4819-145-4-200608150-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112(17):2634–41. doi: 10.1161/CIRCULATIONAHA.105.543231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg LI, Crain AL, Sperl-Hillen JM, Hroscikoski MC, Engebretson KI, O’Connor PJ. Care quality and implementation of the chronic care model: A quantitative study. Annals of Family Medicine. 2006;4(4):310–16. doi: 10.1370/afm.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg LI, Kottke TE, Brekke ML, Magnan S, Davidson G, Calomeni CA, Conn SA, Amundson GM, Nelson AF. Failure of a continuous quality improvement intervention to increase the delivery of preventive services. A randomized trial. Effective Clinical Practice. 2000;3(3):105–15. [PubMed] [Google Scholar]
- Sonel AF, Good CB, Mulgund J, Roe MT, Gibler WB, Smith SC, Jr., Cohen MG, Pollack CV, Jr., Ohman EM, Peterson ED. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes: Insights from CRUSADE (Can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the ACC/AHA guidelines?) Circulation. 2005;111(10):1225–32. doi: 10.1161/01.CIR.0000157732.03358.64. [DOI] [PubMed] [Google Scholar]
- Spertus JA, Nerella R, Kettlekamp R, House J, Marso S, Borkon AM, Rumsfeld JS. Risk of restenosis and health status outcomes for patients undergoing percutaneous coronary intervention versus coronary artery bypass graft surgery. Circulation. 2005;111(6):768–73. doi: 10.1161/01.CIR.0000155242.70417.60. [DOI] [PubMed] [Google Scholar]
- Stevens VJ, Corrigan SA, Obarzanek E, Bernauer E, Cook NR, Hebert P, Mattfeldt-Beman M, Oberman A, Sugars C, Dalcin AT, et al. Weight loss intervention in phase 1 of the Trials of Hypertension Prevention. The TOHP Collaborative Research Group. Archives of Internal Medicine. 1993;153(7):849–58. [PubMed] [Google Scholar]
- Sudore RL, Mehta KM, Simonsick EM, Harris TB, Newman AB, Satterfield S, Rosano C, Rooks RN, Rubin SM, Ayonayon HN, Yaffe K. Limited literacy in older people and disparities in health and healthcare access. Journal of the American Geriatrics Society. 2006;54(5):770–76. doi: 10.1111/j.1532-5415.2006.00691.x. [DOI] [PubMed] [Google Scholar]
- Svetkey LP, Erlinger TP, Vollmer WM, Feldstein A, Cooper LS, Appel LJ, Ard JD, Elmer PJ, Harsha D, Stevens VJ. Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. Journal of Human Hypertension. 2005;19(1):21–31. doi: 10.1038/sj.jhh.1001770. [DOI] [PubMed] [Google Scholar]
- Svetkey LP, Simons-Morton D, Vollmer WM, Appel LJ, Conlin PR, Ryan DH, Ard J, Kennedy BM. Effects of dietary patterns on blood pressure: Subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Archives of Internal Medicine. 1999;159(3):285–93. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- Tao LS, Hart P, Edwards E, Evans AT, Whitaker E, Smith P. Treatment of difficult-to-control blood pressure in a multidisciplinary clinic at a public hospital. Journal of the National Medical Association. 2003;95(4):263–69. [PMC free article] [PubMed] [Google Scholar]
- Taylor AL, Ziesche S, Yancy C, Carson P, D’Agostino R, Jr., Ferdinand K, Taylor M, Adams K, Sabolinski M, Worcel M, Cohn JN. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. New England Journal of Medicine. 2004;351(20):2049–57. doi: 10.1056/NEJMoa042934. [DOI] [PubMed] [Google Scholar]
- Taylor SL, Lurie N. The role of culturally competent communication in reducing ethnic and racial healthcare disparities. American Journal of Managed Care. 2004;10(spec no):SP1–4. [PubMed] [Google Scholar]
- Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O’Donnell C, Kittner S, Lloyd-Jones D, Goff DC, Jr., Hong Y, Adams R, Friday G, Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P, Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P. Heart disease and stroke statistics—2006 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113(6):e85–151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- Thomas KL, East MA, Velazquez EJ, Tuttle RH, Shaw LK, O’Connor CM, Peterson ED. Outcomes by race and etiology of patients with left ventricular systolic dysfunction. American Journal of Cardiology. 2005;96(7):956–63. doi: 10.1016/j.amjcard.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Tobe SW, Pylypchuk G, Wentworth J, Kiss A, Szalai JP, Perkins N, Hartman S, Ironstand L, Hoppe J. Effect of nurse-directed hypertension treatment among First Nations people with existing hypertension and diabetes mellitus: The Diabetes Risk Evaluation and Microalbuminuria (DREAM 3) randomized controlled trial. Canadian Medical Association Journal. 2006;174(9):1267–71. doi: 10.1503/cmaj.050030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TOHP The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. Journal of the American Medical Association. 1992;267(9):1213–20. doi: 10.1001/jama.1992.03480090061028. [DOI] [PubMed] [Google Scholar]
- TOHP2. The Trials of Hypertension Prevention Collaborative Research Group Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, Phase II. Archives of Internal Medicine. 1997;157(6):657–67. [PubMed] [Google Scholar]
- Tonne C, Schwartz J, Mittleman M, Melly S, Suh H, Goldberg R. Long-term survival after acute myocardial infarction is lower in more deprived neighborhoods. Circulation. 2005;111(23):3063–70. doi: 10.1161/CIRCULATIONAHA.104.496174. [DOI] [PubMed] [Google Scholar]
- Trivedi AN, Sequist TD, Ayanian JZ. Impact of hospital volume on racial disparities in cardiovascular procedure mortality. Journal of the American College of Cardiology. 2006;47(2):417–24. doi: 10.1016/j.jacc.2005.08.068. [DOI] [PubMed] [Google Scholar]
- Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. New England Journal of Medicine. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Relationship between quality of care and racial disparities in Medicare health plans. Journal of the American Medical Association. 2006;296(16):1998–2004. doi: 10.1001/jama.296.16.1998. [DOI] [PubMed] [Google Scholar]
- U.S. Renal Data System . USRDS 2006 Annual Data Report: Atlas of end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: 2006. [Google Scholar]
- Vaccarino V, Gahbauer E, Kasl SV, Charpentier PA, Acampora D, Krumholz HM. Differences between African Americans and whites in the outcome of heart failure: Evidence for a greater functional decline in African Americans. American Heart Journal. 2002;143(6):1058–67. doi: 10.1067/mhj.2002.122123. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, Manhapra A, Mallik S, Krumholz HM. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. New England Journal of Medicine. 2005;353(7):671–82. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M, Burgess D, Malat J, Griffin J. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. American Journal of Public Health. 2006;96(2):351–57. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virnig BA, Lurie N, Huang Z, Musgrave D, McBean AM, Dowd B. Racial variation in quality of care among Medicare+Choice enrollees. Health Affairs (Millwood) 2002;21(6):224–30. doi: 10.1377/hlthaff.21.6.224. [DOI] [PubMed] [Google Scholar]
- Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22(12):1533–40. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]
- Walker CC. An educational intervention for hypertension management in older African Americans. Ethnicity & Disease. 2000;10(2):165–74. [PubMed] [Google Scholar]
- Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation. 2005;112(11):1651–62. doi: 10.1161/CIRCULATIONAHA.104.490599. [DOI] [PubMed] [Google Scholar]
- Wang W, Lee ET, Fabsitz RR, Devereux R, Best L, Welty TK, Howard BV. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: The Strong Heart Study. Hypertension. 2006;47(3):403–9. doi: 10.1161/01.HYP.0000200710.29498.80. [DOI] [PubMed] [Google Scholar]
- Whittle J, Conigliaro J, Good CB, Joswiak M. Do patient preferences contribute to racial differences in cardiovascular procedure use? Journal of General Internal Medicine. 1997;12(5):267–73. doi: 10.1046/j.1525-1497.1997.012005267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR. The health of U.S. racial and ethnic populations. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60(spec no 2):53–62. doi: 10.1093/geronb/60.special_issue_2.s53. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Report. 2001;116(5):404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors H. Racism, discrimination and hypertension: Evidence and needed research. Ethnicity & Disease. 2001;11(4):800–16. [PubMed] [Google Scholar]
- Williams KA, Pokharna HK. Racial disparities in cardiovascular health care: Unfulfilled exSPECTations? Journal of Nuclear Cardiology. 2001;8(5):626–29. doi: 10.1067/mnc.2001.118066. [DOI] [PubMed] [Google Scholar]
- Williams ML, Hill G, Jackson M. The impact of an acute myocardial infarction guideline and pathway on racial outcomes at a university hospital. Ethnicity & Disease. 2006;16(3):653–58. [PubMed] [Google Scholar]
- Williams ML, Morris MT, II, Ahmad U, Yousseff M, Li W, Ertel N, VANJHCS Research Group. Veterans Affairs of New Jersey Healthcare System Racial differences in compliance with NCEP-II recommendations for secondary prevention at a Veterans Affairs medical center. Ethnicity & Disease. 2002;12(1):S1-58–62. [PubMed] [Google Scholar]
- Witmer JM, Hensel MR, Holck PS, Ammerman AS, Will JC. Heart disease prevention for Alaska Native women: A review of pilot study findings. Journal of Womens Health (Larchmt) 2004;13(5):569–78. doi: 10.1089/1540999041280981. [DOI] [PubMed] [Google Scholar]
- Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. New England Journal of Medicine. 2002;347(20):1585–92. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- Wong ND, Lopez V, Tang S, Williams GR. Prevalence, treatment, and control of combined hypertension and hypercholesterolemia in the United States. American Journal of Cardiology. 2006;98(2):204–8. doi: 10.1016/j.amjcard.2006.01.079. [DOI] [PubMed] [Google Scholar]
- Woodard LD, Kressin NR, Petersen LA. Is lipid-lowering therapy underused by African Americans at high risk of coronary heart disease within the VA health care system? American Journal of Public Health. 2004;94(12):2112–17. doi: 10.2105/ajph.94.12.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Stange KC. A sense of priorities for the healthcare commons. American Journal of Preventive Medicine. 2006;31(1):99–102. doi: 10.1016/j.amepre.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Wu JY, Leung WY, Chang S, Lee B, Zee B, Tong PC, Chan JC. Effectiveness of telephone counselling by a pharmacist in reducing mortality in patients receiving polypharmacy: Randomised controlled trial. BMJ. 2006;333(7567):522. doi: 10.1136/bmj.38905.447118.2F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt SB, Williams DR, Calvin R, Henderson FC, Walker ER, Winters K. Racism and cardiovascular disease in African Americans. American Journal of the Medical Sciences. 2003;325(6):315–31. doi: 10.1097/00000441-200306000-00003. [DOI] [PubMed] [Google Scholar]
- Yancey AK, Ory MG, Davis SM. Dissemination of physical activity promotion interventions in underserved populations. American Journal of Preventive Medicine. 2006;31(4S):82–91. doi: 10.1016/j.amepre.2006.06.020. [DOI] [PubMed] [Google Scholar]
- Yancy CW, Fowler MB, Colucci WS, Gilbert EM, Bristow MR, Cohn JN, Lukas MA, Young ST, Packer M. Race and the response to adrenergic blockade with carvedilol in patients with chronic heart failure. New England Journal of Medicine. 2001;344(18):1358–65. doi: 10.1056/NEJM200105033441803. [DOI] [PubMed] [Google Scholar]
- Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project Joy: Faith based cardiovascular health promotion for African American women. Public Health Reports. 2001;116(suppl 1):68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarzebski J, Bujor CF, Lessard D, Gore JM, Goldberg RJ. Recent and temporal trends (1975 to 1999) in the treatment, hospital, and long-term outcomes of Hispanic and non-Hispanic white patients hospitalized with acute myocardial infarction: A population-based perspective. American Heart Journal. 2004;147(4):690–97. doi: 10.1016/j.ahj.2003.10.023. [DOI] [PubMed] [Google Scholar]
- Yusuf S. Preventing vascular events due to elevated blood pressure. Circulation. 2006;113(18):2166–68. doi: 10.1161/CIRCULATIONAHA.106.620757. [DOI] [PubMed] [Google Scholar]
- Zaza S, Wright-De Aguero LK, Briss PA, Truman BI, Hopkins DP, Hennessy MH, Sosin DM, Anderson L, Carande-Kulis VG, Teutsch SM, Pappaioanou M. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Task Force on Community Preventive Services. American Journal of Preventive Medicine. 2000;18(1 suppl):44–74. doi: 10.1016/s0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- Zheng ZJ. State-specific mortality from sudden cardiac death—United States, 1999. Morbidity and Mortality Weekly Report. 2002;51(6):123–26. [PubMed] [Google Scholar]