Abstract
BACKGROUND
The best therapeutic strategy for patients with double-vessel coronary artery disease and proximal left anterior descending artery involvement (2VD + pLAD) is not clear.
OBJECTIVES
To compare the survival experience of a cohort of cardiac catheterization patients with 2VD + pLAD based on chosen therapeutic strategy (medical management versus percutaneous coronary intervention [PCI] versus coronary artery bypass graft surgery [CABG]).
METHODS
The authors identified and studied a total of 603 patients with 2VD + pLAD from all patients who underwent diagnostic coronary angiography in Alberta between January 1997 and May 1999. The primary end point was five-year survival from index catheterization for each of the treatment groups and from time of revascularization when the two revascularization strategies were compared.
RESULTS
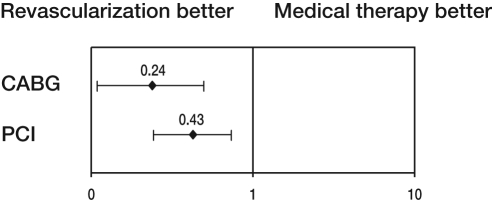
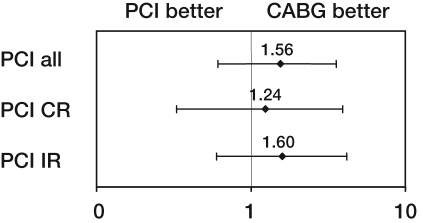
Risk-adjusted hazard ratios (HR) comparing cumulative five-year survival rates of patients treated medically, or with PCI or CABG indicated a survival benefit for patients treated with CABG (HR 0.24, 95% CI 0.11 to 0.54; P<0.001) and PCI (HR 0.43, 95% CI 0.24 to 0.77; P=0.003) compared with medical management. Meanwhile, a risk-adjusted comparison of revascularization strategies suggested a possible trend toward higher mortality for PCI-treated patients versus CABG-treated patients (HR 1.56, 95% CI 0.65 to 3.72; P=0.125).
CONCLUSIONS
The results of this registry-based observational study suggest a survival benefit from revascularization compared with medical management in patients with 2VD + pLAD. Furthermore, the authors found a trend toward better survival in CABG-treated patients compared with PCI-treated patients.
Keywords: Angioplasty, Coronary artery disease, Drugs, Surgery, Survival
Abstract
HISTORIQUE
On n’est pas certain de la meilleure stratégie thérapeutique pour les patients atteints d’une coronaropathie bitronculaire avec atteinte de l’artère descendante antérieure gauche proximale (C2T+DAGP).
OBJECTIFS
Comparer l’expérience de survie d’une cohorte de patients ayant subi un cathétérisme cardiaque avec C2T+DAGP d’après la stratégie thérapeutique choisie (prise en charge médicale, intervention coronaire percutanée [ICP] ou pontage aortocoronarien [PAC]).
MÉTHODOLOGIE
Les auteurs ont dépisté et étudié un total de 603 patients atteints d’une C2T+DAGP parmi l’ensemble des patients qui avaient subi une coronarographie diagnostique en Alberta entre janvier 1997 et mai 1999. Le paramètre ultime primaire était la survie cinq ans après le cathétérisme de référence dans chacun des groupes de traitement et à compter de la revascularisation lorsqu’on comparait les deux stratégies de revascularisation.
RÉSULTATS
Les risques relatifs rajustés (RRR) comparant les taux de survie au bout de cinq ans des patients traités par des médicaments, par ICP ou par PAC indiquent un avantage de survie chez les patients traités par PAC (RRR 0,24, 95 % IC 0,11 à 0,54; P<0,001) et par ICP (RRR 0,43, 95% IC 0,24 à 0,77; P=0,003) par rapport à la prise en charge médicale. De plus, une comparaison rajustée au risque des stratégies de revascularisation laisse supposer une tendance possible vers un taux de mortalité plus élevé chez les patients traités par ICP par rapport à ceux traités par PAC (RRR 1,56, 95 % IC 0,65 à 3,72; P=0,125).
CONCLUSIONS
Les résultats de cette étude d’observation de dossiers laissent supposer une meilleure survie après la revascularisation qu’à la prise en charge médicale chez les patients atteints d’une C2T+DAGP. De plus, les auteurs ont remarqué une tendance de meilleure survie chez les patients ayant subi une PAC par rapport à ceux traités par ICP.
The goals of therapeutic intervention for patients suffering from coronary artery disease (CAD) include symptomatic improvement, prevention of disease progression, and survival benefits. Achievement of these goals may be attempted through medical management (MM) or mechanical revascularization (either surgical or catheter-based). Patients with left main disease, triple-vessel disease (particularly with abnormal left ventricular function) and two-vessel disease (2VD) with involvement of the proximal left anterior descending (pLAD) artery have been shown to have a survival benefit following coronary artery bypass graft surgery (CABG) compared with MM. Randomized clinical trials (RCTs) of percutaneous coronary intervention (PCI) versus MM did not demonstrate a survival benefit in patients with predominantly single-vessel CAD (1–3), and there are very limited and mostly extrapolated data suggesting benefits of PCI treatment for patients with multivessel disease (4). RCTs comparing PCI and CABG for multivessel CAD did not demonstrate statistically significant survival differences (5–16), with the exception of patients with diabetes (17).
The importance of CAD distribution has previously been demonstrated in nonrandomized trials (18,19). Involvement of the pLAD has been identified to be an important determinant of clinical outcomes in patients with multivessel CAD. Several registry studies comparing balloon angioplasty (percutaneous transluminal coronary angioplasty [PTCA]) and CABG showed a trend toward improved survival following surgical revascularization in this patient population (18–21). However, RCTs from the PCI era, which used stents and glycoprotein (GP) IIb/IIIa inhibitors, are conflicting. The Coronary Angioplasty with Stenting versus Coronary Bypass Surgery in patients with Multiple-Vessel Disease II (ERACI II) trial (22) and the Arterial Revascularization Therapies Study (ARTS) (23) demonstrated no significant difference in mortality between the two revascularization strategies, whereas the Stent or Surgery (SoS) trial (24) showed a survival benefit for CABG-treated patients.
The purpose of the present study was to compare the survival experience of cardiac catheterization patients with 2VD and pLAD (2VD + pLAD) patients based on a chosen therapeutic strategy (MM versus PCI versus CABG). Results are from the era of stenting and use of GP IIb/IIIa inhibitors.
METHODS
Data
All data were derived from the Alberta Provincial Program for Outcome Assessment in Coronary Heart disease (APPROACH). APPROACH is an ongoing prospective cohort study of all Alberta residents undergoing cardiac catheterization for CAD since 1995. The initiative has been described in detail elsewhere (25). In brief, this population-based multiple-year inception cohort database contains detailed information on sociodemographic characteristics, presence of risk factors and comorbidities, disease-specific variables, coronary catheterization results (Heartview software; Duke Medical Center, USA), postcatheterization referral decisions, records of actual revascularization and long-term outcomes, including survival and quality of life. Data from APPROACH are routinely supplemented and enhanced by merging the clinical registry data to administrative data records to supplement clinical information available on all patients. This data enhancement methodology has been validated and is also described in detail elsewhere (26). Patient survival and time from catheterization and/or revascularization until death were ascertained through semiannual linkage to Alberta Vital Statistics records.
Definitions
2VD + pLAD was defined as 70% or greater diameter stenosis of the pLAD and 50% or greater stenosis of either the left circumflex artery or the right coronary artery, determined visually by the cardiologist who performed the index diagnostic catheterization procedure between January 1997 and May 1999. The higher threshold of 70% was used for disease of the pLAD because it is the threshold above which many clinicians will propose revascularization. A cut-off point of 50% was used for other vessels because such lesions are recorded as potentially important CAD in the Heartview software and in the APPROACH database. Patients with single-vessel disease, triple-vessel disease or left main disease, and patients undergoing primary PCI because of ST segment elevation myocardial infarction were not included in this analysis. Patients were categorized into treatment groups according to the first treatment received (MM, PCI or CABG) within the first year of enrolment. The outcome of interest was mortality, and this was ascertained via linkage to data from the Alberta Bureau of Vital Statistics. The study follow-up extended to five years postcatheterization.
Analysis
Baseline comparisons of clinical characteristics across treatment groups were made by the χ2 test for categorical variables and by ANOVA for continuous variables. The Kaplan-Meier method was used to present unadjusted five-year survival rates from index catheterization for each of the treatment groups and from time of revascularization (PCI or CABG) when the two revascularization strategies were compared. Cox proportional hazard models were then used to determine risk-adjusted survival for clinical characteristics and comorbidities, and for each treatment group. These analyses were adjusted for age, sex, history of diabetes mellitus, hyperlipidemia, hypertension, serum creatinine level higher than 200 μmol/L, peripheral vascular disease, congestive heart failure, prior myocardial infarction, prior PCI, jeopardy scores (Duke, Bypass Angioplasty Revascularization Investigation [BARI] and APPROACH), as previously defined (27), as well as left ventricular ejection fraction. All these variables are routinely captured by the APPROACH database and are known to be associated with the adverse outcomes in patients with known CAD. Comorbid conditions were considered to be present if they were identified by the referring cardiologist or in the hospital record. The indication for the catheterization procedure (acute or recent myocardial infarction, unstable angina, stable angina or other) was also included. Risk-adjusted hazard ratios (HR) were calculated for the following treatment comparisons: CABG/MM, PCI/MM, CABG/PCI, CABG/PCI with complete revascularization and CABG/PCI with incomplete revascularization. Complete revascularization was defined as the successful treatment (residual stenosis of less than 50%) of all angiographically significant lesions (70% or greater diameter stenosis).
A multivariable analysis was also performed to control for the propensity (28) of being selected for either CABG or PCI compared with no revascularization. This was undertaken by conducting logistic regression analyses to model predictors of undergoing either CABG or PCI. The resulting models were used to calculate a probability and propensity of being selected for either CABG or PCI. The propensity scores were then included in the final multivariable analyses to assess the association between CABG and PCI with no revascularization.
All analyses were conducted using SPSS version 10.0 (SPSS Inc, USA).
RESULTS
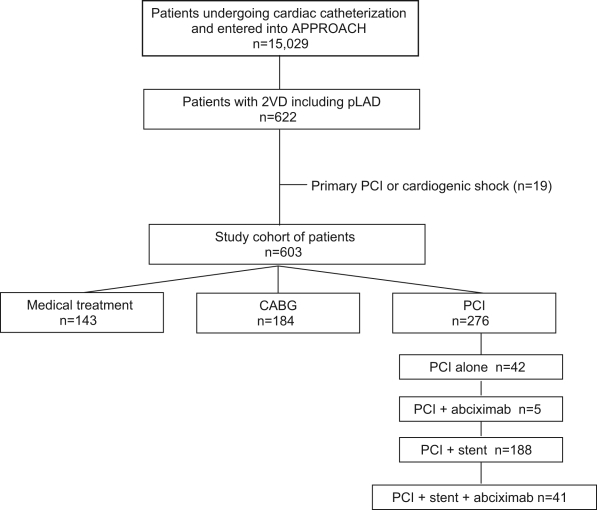
After application of the study inclusion criteria, 603 patients with 2VD + pLAD among all patients who underwent diagnostic coronary angiography in the province of Alberta between January 1997 and May 1999 were identified and studied (Figure 1). Of these patients, 143 were treated medically, 276 underwent PCI and 184 underwent CABG. The mean (± SD) time from index catheterization to catheter-based revascularization was 21±44 days and 70±74 days from index catheterization to surgery.
Figure 1.
Identification of patients with two-vessel coronary artery disease (2VD) with proximal left anterior descending artery involvement (pLAD) from the Alberta Provincial Program for Outcome Assessment in Coronary Heart disease (APPROACH) database. CABG Coronary artery bypass graft surgery; PCI Percutaneous coronary intervention
Clinical characteristics
Demographic and angiographic characteristics of the patient population are summarized in Table 1. MM patients were slightly older, more likely to have renal failure and peripheral vascular disease, and had better left ventricular ejection fraction than PCI- and/or CABG-treated patients. However, these differences did not reach statistical significance. On the other hand, patients undergoing CABG had larger amount of myocardium at risk (as measured by myocardial jeopardy scores) than MM patients and patients undergoing PCI.
TABLE 1.
Characteristics of patients treated with medical management, coronary artery bypass graft surgery (CABG) and percutaneous coronary intervention (PCI) (n=603)
| Clinical characteristics | Medical (n=143) | CABG (n=184) | PCI (n=276) | P |
|---|---|---|---|---|
| Age, years (mean) | 65.2 | 64.5 | 64.4 | 0.77 |
| Male sex, % | 78.3 | 77.2 | 78.3 | 0.96 |
| Pulmonary disease, % | 6.3 | 10.9 | 6.2 | 0.14 |
| Cerebrovascular disease, % | 4.2 | 6.0 | 5.8 | 0.74 |
| Creatinine >200 μmol/L, % | 5.6 | 1.6 | 2.5 | 0.09 |
| Congestive heart failure, % | 14.0 | 19.0 | 18.1 | 0.45 |
| Dialysis, % | 1.4 | 1.1 | 1.4 | 0.94 |
| Hypertension, % | 44.8 | 46.2 | 48.2 | 0.79 |
| Diabetes mellitus, % | 23.8 | 20.1 | 20.7 | 0.69 |
| Hyperlipidemia, % | 51.7 | 48.9 | 49.6 | 0.87 |
| Smoking, % | 36.6 | 31.5 | 34.7 | 0.62 |
| Malignancy, % | 1.4 | 3.8 | 2.9 | 0.43 |
| Liver/gastrointestinal disease, % | 2.1 | 3.8 | 3.6 | 0.64 |
| Prior myocardial infarction, % | 54.5 | 59.8 | 62.7 | 0.27 |
| Prior PTCA, % | 9.1 | 10.3 | 13.4 | 0.36 |
| Prior lytic therapy, % | 9.8 | 8.2 | 9.4 | 0.85 |
| Peripheral vascular disease, % | 7.0 | 4.3 | 6.2 | 0.56 |
| Clinical indications for catheterization, % | 0.30 | |||
| Stable angina | 32.9 | 31.0 | 27.2 | |
| Myocardial infarction | 30.8 | 38.6 | 41.3 | |
| Unstable angina | 30.1 | 26.1 | 23.9 | |
| Other | 6.3 | 4.3 | 7.6 | |
| Ejection fraction, % | 0.11 | |||
| >50 | 56.6 | 44.6 | 42.0 | |
| <30 | 7.0 | 8.2 | 9.4 | |
| 30–50 | 19.6 | 30.4 | 32.2 | |
| Ventriculogram not performed, % | 4.9 | 5.4 | 2.9 | |
| Ventriculogram missing, % | 11.9 | 11.4 | 13.4 | |
| Diseased right coronary artery, % | 51.0 | 62.0 | 58.7 | 0.31 |
| Diseased left circumflex artery, % | 49.0 | 38.0 | 41.3 | 0.13 |
| Duke jeopardy score | 63.0 | 64.5 | 61.9 | 0.05 |
| BARI myocardial jeopardy score | 64.6 | 66.6 | 65.2 | |
| APPROACH lesion score | 64.6 | 69.0 | 65.8 | 0.05 |
APPROACH Alberta Provincial Program for Outcome Assessment in Coronary Heart disease; BARI Bypass Angioplasty Revascularization Investigation; PCTA Percutaneous transluminal coronary angioplasty
Survival
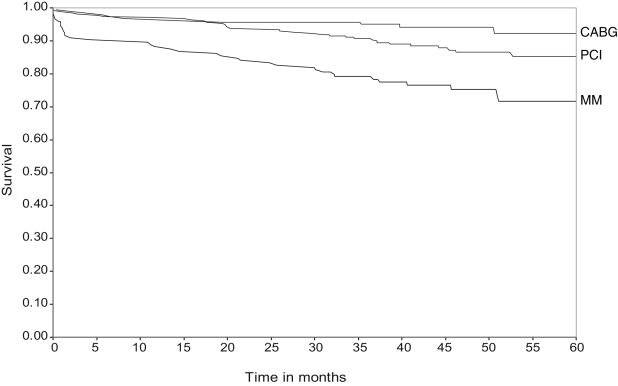
Overall, the unadjusted five-year cumulative survival from index angiographic procedure for the study population was 86.2%. The five-year survival rate for MM patients was 71.6%, while the corresponding rates for patients treated with PCI and CABG were 85.3% and 92.2%, respectively. There was a lower survival rate among MM patients than revascularized patients (MM versus PCI P=0.007 and MM versus CABG P<0.001) and better survival in patients undergoing CABG than PCI (P=0.037) (Figure 2).
Figure 2.
Kaplan-Meier plot showing survival from time of diagnostic catheterization. Medical management (MM) versus coronary artery bypass graft surgery (CABG) P<0.001; MM versus PCI P=0.007; CABG versus percutaneous coronary intervention (PCI) P=0.037
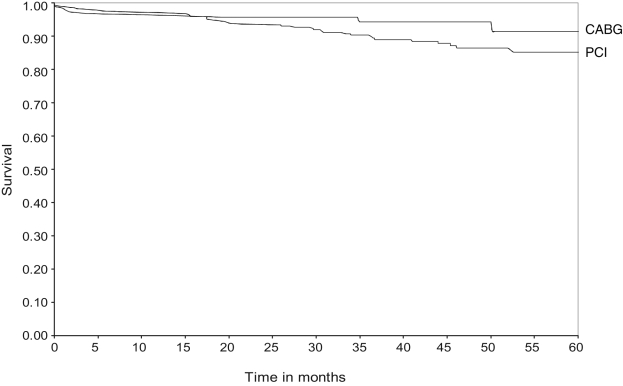
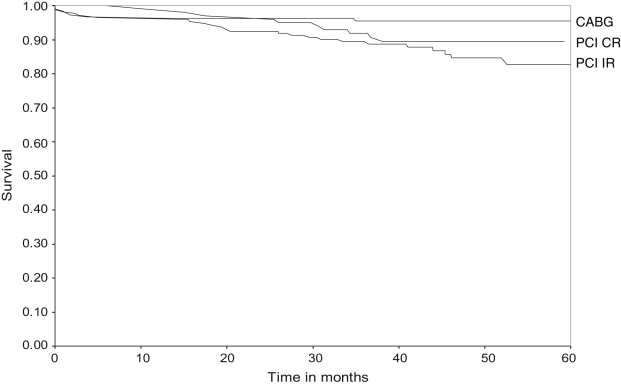
The five-year survival rate from the time of revascularization procedure was 91.5% for CABG-treated patients and 85.1% for PCI-treated patients (P=0.048) (Figure 3). Among PCI-treated patients, 100 (36.2%) were completely revascularized (all lesions with 70% or greater stenosis were successfully treated). The unadjusted survival rate of completely revascularized patients was similar to that of the CABG group (P=0.31). However, the survival rate of incompletely revascularized patients was significantly lower than that of patients undergoing CABG (P=0.027) (Figure 4).
Figure 3.
Kaplan-Meier plot showing survival from time of revascularization procedure. Coronary artery bypass graft surgery (CAGB) versus percutaneous coronary intervention (PCI) P=0.048
Figure 4.
Kaplan-Meier plot showing survival from time of revascularization procedure, with percutaneous coronary intervention (PCI)-treated patients separated into those with complete revascularization (CR) and incomplete revascularization (IR). Coronary artery bypass graft surgery (CABG) versus PCI CR P=0.31; CABG versus PCI IR P=0.027
Risk-adjusted analysis
Risk-adjusted HR comparing cumulative five-year survival rates of patients treated medically, interventionally (PCI) or surgically (CABG) indicated statistically significantly lower HR for the five-year mortality rate for treatment with CABG (HR 0.24, 95% CI 0.11 to 0.54; P<0.001) for PCI treatment (HR 0.43, 95% CI 0.24 to 0.77; P=0.003) compared with MM (Figure 5). Risk-adjusted analysis included age, sex, diabetes mellitus, hypertension, dyslipidemia, smoking, history of prior myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease and chronic renal failure.
Figure 5.
Risk-adjusted hazard risk ratio (with 95% CI) for revascularization procedures versus medical therapy. CABG Coronary artery bypass graft surgery; PCI Percutaneous coronary intervention
Additional analysis (considering the propensity to be selected for revascularization with CABG or PCI) had little or no effect on the adjusted HR for CABG (HR 0.24, 95% CI 0.11 to 0.55) or PCI (HR 0.44, 95% CI 0.24 to 0.79).
Meanwhile, a risk-adjusted comparison of revascularization strategies indicated a trend toward higher mortality for PCI-treated patients versus the CABG-treated patients, but this did not reach statistical significance (HR 1.56, 95% CI 0.65 to 3.72; P=0.125). Furthermore, risk-adjusted survival rates of completely and incompletely revascularized patients were not statistically different compared with CABG-treated patients (Figure 6).
Figure 6.
Risk-adjusted hazard ratio (with 95% CI) for death in the percutaneous coronary intervention (PCI) group compared with the coronary artery bypass graft surgery (CABG) group. CR Complete revascularization; IR Incomplete revascularization
DISCUSSION
Our registry-based study demonstrated an association between revascularization treatments (PCI or CABG) and a better survival rate compared with MM in patients with 2VD + pLAD in the era of bare metal stents and GP IIb/IIIa inhibitors. Our results also showed no statistically significant difference in risk-adjusted survival following surgical versus catheter-based revascularization (PCI) in this patient population, though outcomes tended to be better after CABG, particularly compared with PCI patients who did not have complete revascularization by the catheter-based intervention.
In the absence of large RCTs comparing all three therapeutic modalities (MM, PCI and CABG) in multivessel CAD, clinical decisions are made on the basis of the Medicine, Angioplasty, or Surgery Study II (MASS II) (12), as well as trials comparing MM with CABG, MM with PCI or CABG, and PCI with CABG. The groups of patients who benefit most from CABG compared with MM or PCI have been well defined (4). However, for some patients with CAD, such as those with multivessel disease and pLAD, the optimal therapeutic strategy has not been clearly defined, because the results of early and more recent registry trials (18–21), as well as published RCTs (5–17,22–24), are conflicting.
MM versus PCI
Early RCTs of PTCA versus MM did not demonstrate a survival benefit in patients with predominantly single-vessel CAD (1–3). Unfortunately, there are no RCTs directly comparing PTCA or PCI with MM in patients with multivessel CAD. Recent guidelines (4) are based on extrapolation of data from a trial comparing MM with one of the revascularization strategies, either surgical or catheter-based (29), and there are very limited and predominantly extrapolated data suggesting benefits of PCI treatment for patients with multivessel disease (4).
Our data demonstrated survival benefits of catheter-based revascularization compared with MM in patients with 2VD + pLAD in the era of stents and GP IIb/IIIa inhibitors. These data extend our knowledge regarding the most appropriate treatment strategy for specific population(s) of patients with CAD, especially with regard to the survival benefit of catheter-based revascularization compared with MM. Prior registry studies (17,20) showed improved long-term outcomes following PTCA compared with MM in specific patient populations. The Emory-Coronary Artery Surgery Study (CASS) (20) demonstrated a survival advantage in patients with impaired left ventricular function (ejection fraction lower than 50%) and two-vessel disease who were treated with PCI compared with MM. However, the subgroup of patients with pLAD did not demonstrate a significant survival difference. Data from the Duke registry are suggestive of PTCA superiority in long-term outcomes, compared with MM, in a low-risk stratum of CAD patients (17). The major concern about the results of all of these aforementioned registry trials and studies is their nonrandomized nature.
MM versus CABG
Our data support the current recommendations (4) for surgical revascularization of patients with 2VD + pLAD. The findings presented here therefore provide further evidence from a ‘usual care’ context in support of the guideline recommendations.
PCI versus CABG
RCTs comparing PCI and CABG for multivessel CAD did not demonstrate a statistically significant survival difference (5–16), with the exception of patients with diabetes (17).
The majority of these RCTs did not, however, include sufficient numbers of patients with high-risk features, such as diabetes mellitus, impaired left ventricular dysfunction or multivessel disease with pLAD. We specifically studied the subgroup of patients suffering from 2VD + pLAD. This patient population is one of the most controversial, from an outcome perspective. Early registry studies comparing PTCA and CABG showed a trend toward improved survival following surgical revascularization in this patient population (17–21). However, RCTs from the PCI era, which used stents and GP IIb/IIIa inhibitors, are conflicting. The ERACI II (22) and ARTS (23) trials demonstrated no significant difference in mortality between the two revascularization strategies, but the SoS trial (24) showed a survival benefit for CABG. Furthermore, recently published registry data from Cleveland, Ohio (30), focusing on high-risk patients with multivessel CAD undergoing coronary revascularization (either PCI or CABG) demonstrated improved survival in patients undergoing surgical revascularization. Although the Cleveland registry data included a large number of patients with pLAD, post hoc analyses were primarily focused on patients with diabetes mellitus and impaired left ventricular function. Our unadjusted results suggest better survival outcomes in surgically revascularized patients with 2VD + pLAD (91.5% versus 85.1% survival rate for CABG and PCI, respectively; P=0.048). In this regard, our observation was similar to recently published data from a statewide New York cardiac procedures registry (31). However, when we retrospectively analyzed the data based on completeness of revascularization, defined as successful revascularization of both involved coronary arteries (pLAD and the second lesion) by PCI, completely revascularized patients had similar survival rates to CABG-treated patients, while the survival rates of incompletely revascularized patients were significantly lower (P=0.027) (Figure 4). When a risk-adjusted analysis was performed to account for differences in the baseline characteristics presented in Tables 1 and 2, however, there was no statistically significant difference in survival between CABG- and PCI-treated patients. These results are complementary to previously published randomized comparisons of complete and incomplete PCI versus CABG (32), which demonstrated a non-significant trend toward an improved five-year survival rate in CABG patients. However, it should be noted that in our study population, stents were used in 83% of patients, abciximab was used relatively infrequently (17% of patients), and drug-eluting stents were not used at all. As such, it should be acknowledged that future increases in the use of these innovations in PCI care may lead to better PCI outcomes.
Early mortality in the MM group
Our analysis demonstrated significant early mortality in the MM group. This may simply be the result of the greater burden of CAD and comorbidities in this patient group. However, as previously demonstrated by Thompson et al (33), the so-called ‘medical treatment group’ in such observational studies comprises patients receiving medical therapy as planned initially, as well as patients receiving medical therapy despite an earlier proposal that they undergo revascularization with either PCI or CABG. Patients who received MM at variance with the proposal for revascularization had the highest mortality of all patients in the study (33). Similarly, in our study, the MM group had the poorest survival. We do not have information on the initial recommendations regarding revascularization treatment for these patients and, thus, cannot differentiate between patients who received MM as a chosen therapy and patients whose initial planned treatment was revascularization but for whom intervening factors led to a change in the management plan (eg, new clinical events or a late personal decision to forego revascularization). In this regard, it should be acknowledged that early deaths in the MM group may reflect the occurrence of undesirable clinical events while patients were actually waiting for a previously planned revascularization procedure that, in the end, did not occur.
Study limitations
The major limitation of our study is its nonrandomized nature. Even though our risk-adjusted analysis dealt with all measured and available variables affecting survival in this CAD population, it is impossible to capture all factors involved in the decision making process that happened at the time of catheterization by the heterogeneous pool of physicians involved in the care of these patients. Furthermore, despite the availability of jeopardy scores, we cannot ensure that all patients were suitable for revascularization, and it is therefore possible that patients not suitable for revascularization were treated medically, which might have been, at least in part, responsible for the survival rate differences. A second limitation is that we were unable to describe the details and quality of MM that patients in each treatment group received at the time of discharge and during the follow-up period. Another limitation is that our database (APPROACH) does not contain data on completeness of surgical revascularization (CABG); we were thus unable to compare the outcomes of patients with complete versus incomplete surgical revascularization. Finally, because of the five-year follow-up, the longer-term life expectancy implications of our findings are not entirely clear.
CONCLUSIONS
Our data suggest that in the era of stents and GP IIb/IIIa inhibitors, revascularization is associated with better outcomes than MM alone in patients with 2VD + pLAD. The results of the present registry-based study also demonstrated survival benefits of PCI compared with MM. We did not find any statistically significant differences in five-year survival rates between CABG and PCI, although a trend toward better survival in CABG-treated patients was observed.
Footnotes
FUNDING: Dr Knudtson receives partial support from the Libin Trust Fund. Dr Ghali is supported by the Government of Canada Research Chair in Health Services Research program and by a Health Scholar Award from the Alberta Heritage Foundation for Medical Research (Edmonton, Alberta). Ms Galbraith is supported by a Canadian Cardiovascular Outcomes Research Team (www.ccort.ca) student fellowship, funded by an operating grant from the Canadian Institutes of Health Research, and by the Heart and Stroke Foundation and Tomorrow’s Research Cardiovascular Health Professionals (TORCH) (www.torch.ca) student fellowship. APPROACH was funded in 1995 by the W Garfield Weston Foundation and has received ongoing support from Merck Frosst Canada Inc, Monsanto Canada Inc/Searle, Eli Lilly Canada Inc, Guidant Corporation, Boston Scientific Ltd, Roche Ltd, Johnson & Johnson Inc, Cordis and the Province Wide Services Advisory Committee of Alberta Health and Wellness.
REFERENCES
- 1.Hartigan PM, Giacomini JC, Folland ED, Parisi AF. Two- to three-year follow-up of patients with single-vessel coronary artery disease randomized to PTCA or medical therapy (results of a VA cooperative study). Veterans Affairs Cooperative Studies Program ACME Investigators. Angioplasty Compared to Medicine. Am J Caridol. 1998;82:1445–50. doi: 10.1016/s0002-9149(98)00685-7. [DOI] [PubMed] [Google Scholar]
- 2.RITA-2 trial participants. Coronary angioplasty versus medical therapy for angina: The second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet. 1997;350:461–8. [PubMed] [Google Scholar]
- 3.Pitt B, Waters D, Brown WV, et al. Aggressive lipid-lowering therapy compared with angioplasty in stable coronary artery disease. Atorvastatin versus Revascularization Treatment Investigators. N Engl J Med. 1999;341:70–6. doi: 10.1056/NEJM199907083410202. [DOI] [PubMed] [Google Scholar]
- 4.Gibbons RJ, Abrams J, Chatterjee K, et al. American College of Cardiology; American Heart Association Task Force on Practice Guidelines. Committee on the Management of Patients With Chronic Stable Angina. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina – summary article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina) Circulation. 2003;107:149–58. doi: 10.1161/01.cir.0000047041.66447.29. [DOI] [PubMed] [Google Scholar]
- 5.Coronary angioplasty versus coronary artery bypass surgery: The Randomized Intervention Treatment of Angina (RITA) trial. Lancet. 1993;341:573–80. [PubMed] [Google Scholar]
- 6.CABRI Trial Participants. First-year results of CABRI (Coronary Angioplasty versus Bypass Revascularisation Investigation) Lancet. 1995;346:1179–84. [PubMed] [Google Scholar]
- 7.The Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med. 1996;335:217–25. doi: 10.1056/NEJM199607253350401. (Erratum in 1997;336:147) [DOI] [PubMed] [Google Scholar]
- 8.Hamm CW, Reimers J, Ischinger T, Rupprecht HJ, Berger J, Bleifeld W. A randomized study of coronary angioplasty compared with bypass surgery in patients with symptomatic multivessel coronary disease. German Angioplasty Bypass Surgery Investigation (GABI) N Engl J Med. 1994;331:1037–43. doi: 10.1056/NEJM199410203311601. [DOI] [PubMed] [Google Scholar]
- 9.Henderson RA, Pocock SJ, Sharp SJ, et al. Long-term results of RITA-1 trial: Clinical and cost comparisons of coronary angioplasty and coronary-artery bypass grafting. Randomised Intervention Treatment of Angina. Lancet. 1998;352:1419–25. doi: 10.1016/s0140-6736(98)03358-3. [DOI] [PubMed] [Google Scholar]
- 10.King SB, III, Lembo NJ, Weintraub WS, et al. A randomized trial comparing coronary angioplasty with coronary bypass surgery. Emory Angioplasty versus Surgery Trial (EAST) N Engl J Med. 1994;331:1044–50. doi: 10.1056/NEJM199410203311602. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez A, Boullon F, Perez-Baliño N, Paviotti C, Liprandi MI, Palacios IF. Argentine randomized trial of percutaneous transluminal coronary angioplasty versus coronary artery bypass surgery in multivessel disease (ERACI): In-hospital results and 1-year follow-up. ERACI Group. J Am Coll Cardiol. 1993;22:1060–7. doi: 10.1016/0735-1097(93)90416-x. [DOI] [PubMed] [Google Scholar]
- 12.Favarato D, Hueb W, Gersh BJ, et al. First Year Follow-Up of MASS II Study. Relative cost comparison of treatments for coronary artery disease: The First Year Follow-Up of MASS II Study. Circulation. 2003;108(Suppl 1):II21–3. doi: 10.1161/01.cir.0000087381.98299.7b. [DOI] [PubMed] [Google Scholar]
- 13.Serruys PW, Unger F, Sousa JE, et al. Arterial Revascularization Therapies Study Group. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344:1117–24. doi: 10.1056/NEJM200104123441502. [DOI] [PubMed] [Google Scholar]
- 14.Morrison DA, Sethi G, Sacks J, et al. Angina With Extremely Serious Operative Mortality Evaluation (AWESOME) Percutaneous coronary intervention versus coronary artery bypass graft surgery for patients with medically refractory myocardial ischemia and risk factors for adverse outcomes with bypass: A multicenter, randomized trial. Investigators of the Department of Veterans Affairs Cooperative Study #385, the Angina With Extremely Serious Operative Mortality Evaluation (AWESOME) J Am Coll Cardiol. 2001;38:143–9. doi: 10.1016/s0735-1097(01)01366-3. [DOI] [PubMed] [Google Scholar]
- 15.Seven-year outcome in the Bypass Angioplasty Revascularization Investigation (BARI) by treatment and diabetic status. J Am Coll Cardiol. 2000;35:1122–9. doi: 10.1016/s0735-1097(00)00533-7. [DOI] [PubMed] [Google Scholar]
- 16.Hannan EL, Racz MJ, McCallister BD, et al. A comparison of three-year survival after coronary artery bypass graft surgery and percutaneous transluminal coronary angioplasty. J Am Coll Cardiol. 1999;33:63–72. doi: 10.1016/s0735-1097(98)00540-3. [DOI] [PubMed] [Google Scholar]
- 17.Jones RH, Kesler K, Phillips HR, III, et al. Long-term survival benefits of coronary artery bypass grafting and percutaneous transluminal angioplasty in patients with coronary artery disease. J Thorac Cardiovasc Surg. 1996;111:1013–25. doi: 10.1016/s0022-5223(96)70378-1. [DOI] [PubMed] [Google Scholar]
- 18.Favaloro RG. Critical analysis of coronary artery bypass graft surgery: A 30-year journey. J Am Coll Cardiol. 1998;31(Suppl B):1B–63B. doi: 10.1016/s0735-1097(97)00559-7. [DOI] [PubMed] [Google Scholar]
- 19.Mark DB, Nelson CL, Califf RM, et al. Continuing evolution of therapy for coronary artery disease. Initial results from the era of coronary angioplasty. Circulation. 1994;89:2015–25. doi: 10.1161/01.cir.89.5.2015. [DOI] [PubMed] [Google Scholar]
- 20.Ellis SG, Fisher L, Dushman-Ellis S, et al. Comparison of coronary angioplasty with medical treatment for single- and double-vessel coronary disease with left anterior descending coronary involvement: Long-term outcome based on an Emory-CASS registry study. Am Heart J. 1989;118:208–20. doi: 10.1016/0002-8703(89)90178-6. [DOI] [PubMed] [Google Scholar]
- 21.Kurbaan AS, Rickards AF, Ilsley CD, Foale RA, Sigwart U, Bowker TJ Coronary Angioplasty versus Bypass Revascularisation Investigation. Relation between coronary artery disease, baseline clinical variables, revascularization mode, and mortality. CABRI Participants. Coronary Angioplasty vs. Bypass Revascularisation Investigation. Am J Cardiol. 2000;86:938–42. doi: 10.1016/s0002-9149(00)01126-7. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez A, Bernardi V, Navia J, et al. Argentine Randomized Study: Coronary Angioplasty with Stenting versus Coronary Bypass Surgery in patients with Multiple-Vessel Disease (ERACI II): 30-day and one-year follow-up results. ERACI II Investigators. J Am Coll Cardiol. 2001;37:51–8. doi: 10.1016/s0735-1097(00)01052-4. (Erratum in 2001;37:973–4) [DOI] [PubMed] [Google Scholar]
- 23.Serruys PW, Unger F, Sousa JE, et al. Arterial Revascularization Therapies Study Group. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344:1117–24. doi: 10.1056/NEJM200104123441502. [DOI] [PubMed] [Google Scholar]
- 24.SoS Investigators. Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): A randomised controlled trial. Lancet. 2002;360:965–70. doi: 10.1016/S0140-6736(02)11078-6. [DOI] [PubMed] [Google Scholar]
- 25.Ghali WA, Knudtson ML. Overview of the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease. On behalf of the APPROACH Investigators. Can J Cardiol. 2000;16:1225–30. [PubMed] [Google Scholar]
- 26.Norris CM, Ghali WA, Knudtson ML, Naylor CD, Saunders LD. Dealing with missing data in observational health care outcome analyses. J Clin Epi. 2000;53:377–83. doi: 10.1016/s0895-4356(99)00181-x. [DOI] [PubMed] [Google Scholar]
- 27.Graham MM, Faris PD, Ghali WA, et al. APPROACH Investigators (Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease. Validation of three myocardial jeopardy scores in a population-based cardiac catheterization cohort. Am Heart J. 2001;142:254–61. doi: 10.1067/mhj.2001.116481. [DOI] [PubMed] [Google Scholar]
- 28.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–63. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 29.Davies RF, Goldberg AD, Forman S, et al. Asymptomatic Cardiac Ischemia Pilot (ACIP) study two-year follow-up: Outcomes of patients randomized to initial strategies of medical therapy versus revascularization. Circulation. 1997;95:2037–43. doi: 10.1161/01.cir.95.8.2037. [DOI] [PubMed] [Google Scholar]
- 30.Brener SJ, Lytle BW, Casserly IP, Schneider JP, Topol EJ, Lauer MS. Propensity analysis of long-term survival after surgical or percutaneous revascularization in patients with multivessel coronary artery disease and high-risk features. Circulation. 2004;109:2290–5. doi: 10.1161/01.CIR.0000126826.58526.14. [DOI] [PubMed] [Google Scholar]
- 31.Hannan EL, Racz MJ, Walford G, et al. Long-term outcomes of coronary-artery bypass grafting versus stent implantation. N Engl J Med. 2005;352:2174–83. doi: 10.1056/NEJMoa040316. [DOI] [PubMed] [Google Scholar]
- 32.Bourassa MG, Kip KE, Jacobs AK, et al. Is a strategy of intended incomplete percutaneous transluminal coronary angioplasty revascularization acceptable in nondiabetic patients who are candidates for coronary artery bypass graft surgery? The Bypass Angioplasty Revascularization Investigation (BARI) J Am Coll Cardiol. 1999;33:1627–36. doi: 10.1016/s0735-1097(99)00077-7. [DOI] [PubMed] [Google Scholar]
- 33.Thompson CR, Humphries KH, Gao M, et al. Canadian Cardiovascular Outcomes Research Team. Revascularization use and survival outcomes after cardiac catheterization in British Columbia and Alberta. Can J Cardiol. 2004;20:1417–23. [PubMed] [Google Scholar]