Abstract
Recently, medial patellofemoral ligament reconstruction has been emphasized for the treatment of patellar dislocation. This study compared the results of medial patellofemoral ligament reconstruction by adductor magnus tenodesis with distal patellar realignment in patients with recurrent patellar dislocation. Additionally, the development of patellofemoral osteoarthrosis was compared for these two procedures at a median 10-year followup. Between 1994 and 2000, 47 consecutive patients were treated for recurrent patellar dislocation by adductor magnus tenodesis (18 knees) or Roux-Goldthwait procedure (29 knees). Redislocations, subjective symptoms, and functional outcomes were evaluated. Magnetic resonance imaging was performed at followup. The incidence of patellar redislocation after surgery was 7% in the adductor magnus group and 14% in the Roux-Goldthwait group. Median Kujala scores were 88 for the adductor magnus group and 86 for the Roux-Goldthwait group. Magnetic resonance imaging revealed patellofemoral articular cartilage lesions in 22 knees (73.3%) at followup, including 14 (46.6%) with full-thickness cartilage loss. Radiographs revealed patellofemoral osteoarthritis in five patients in the Roux-Goldthwait group and in none of the patients in the adductor magnus group. Adductor magnus tenodesis is a reliable method to treat recurrent patellar dislocation. The medial patellofemoral ligament reconstruction seems to reduce the risk of osteoarthrosis compared with distal realignment surgery.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Acute lateral patellar dislocation may be followed by harmful sequelae such as recurrent dislocation and painful subluxation. Recurrent dislocation is defined as a patellar dislocation that occurs more than once, and subluxation can be described as symptomatic patellar displacement lateral to the rim of the lateral femoral condyle with spontaneous reduction [22]. In a recent prospective, randomized study [37], no benefit of initial surgery was seen for acute primary patellar dislocation. Instead, previous studies indicate operative treatment is better suited for prevention of recurrent dislocations. These studies also indicate that although surgery can prevent further dislocation and subluxation, it does not prevent patellofemoral pain [1, 43]. Furthermore, postoperatively, degenerative changes have been frequent in the patellofemoral joint, especially after distal realignment procedures [1, 5, 26, 33].
The medial patellofemoral ligament (MPFL) has been emphasized in publications on patellar dislocation since the early 1990s. Several studies [11, 40, 41] have investigated medial soft tissue structures in relation to the stability of the distal extensor mechanism. These studies show the MPFL, by contributing greater than 50% of the total force, is the major medial soft tissue restraint to prevent lateral displacement of the patella. A biomechanical investigation [21] on cadavers showed 50% of the lateral restraining force is provided by the MPFL alone, leading to the conclusion that other medial retinacular tissues play only a minor role. Other medial retinacular tissues affecting patellar stability are the superficial medial retinaculum and the medial patellotibial ligament. The function of the vastus medialis obliquus muscle is also to resist lateral patellar displacement, but its function as a passive stabilizer when the muscle is relaxed is inefficient [2, 5].
Previous studies have revealed a high incidence of MPFL ruptures in connection with acute patellar dislocations and MPFL abnormalities related to recurrent patellar dislocations [4, 17, 39, 44, 46]. It has been hypothesized that the failure to identify and correct incompetence of the MPFL at the site of disruption may contribute to recurrent instability [21]. In 1993, Avikainen et al. [6] described a method to reconstruct the MPFL by adductor magnus tenodesis. Their report on 14 patients, 10 with acute and four with recurrent patellar dislocations, showed good results for 12 patients in a 7-year followup, but absence of a control group was a limitation of the study. So far, no other studies have been published concerning this specific MPFL reconstruction technique. Although many repair or reconstructive techniques of the MPFL have been described [6, 14, 15, 17, 36, 40, 42, 47], the studies have lacked control groups and have reported only short- or midterm followup.
The primary aim of the current study was to compare the long-term results of MPFL reconstruction by adductor magnus tenodesis with distal patellar realignment surgery performed by the Roux-Goldthwait procedure in patients with recurrent patellar dislocation. The outcome measures for the study groups consisted of the redislocation rate, objective functional outcome as assessed by the Tegner activity scale, and subjective outcome as measured by the Kujala score. An additional aim of the study was to compare the development of radiographic signs of osteoarthrosis (OA) in the patellofemoral joint between MPFL reconstruction and distal realignment procedures as determined from plain radiographs and MRI at a median 10-year followup.
Materials and Methods
Using a computer search of the medical records of The Central Military Hospital, Helsinki, Finland, we identified all patients operated on for recurrent patellar dislocation at the hospital between 1994 and 2000. To be included, patients had to have at least two documented lateral dislocations of the patella followed by harmful patellofemoral complaints preventing the conscript from attending normal military service. The diagnosis of the recurrent lateral dislocations of the patella had to be based on physical examination by an orthopaedic surgeon (TV, HP) in The Central Military Hospital. Excluded from the study were patients with acute first-time patellar dislocation with few or no symptoms despite recurrent patellar dislocations (a conscript serving a full military service period without consideration of surgery) and patients whose data regarding previous dislocations were missing before surgery. Forty-seven consecutive conscripts diagnosed with recurrent patellar dislocation and who underwent MPFL reconstruction or a distal realignment procedure met the inclusion criterion. All 47 consecutive conscripts were male. Eighteen knees were treated by adductor magnus tenodesis as compared with 29 knees by the Roux-Goldthwait procedure. The median age at the time of surgery was 20.2 years (range, 19–22 years) in the adductor magnus group and 20.0 years (range, 19–24 years) in the Roux-Goldthwait group (p = 0.46). The minimum followups were 8 years (median, 10.1 years; range, 8–13 years) and 5 years (median, 7.0 years; range, 5–11 years) (p = 0.004), respectively. Fifteen of the 18 patients in the adductor magnus group and 21 of the 29 in the Roux-Goldthwait group were able to participate in the followups, at which their median ages were 30 years (range, 27–32 years) and 28 years (range, 24–33 years) (p = 0.08), respectively. The two study groups were comparable in terms of age and number of previous dislocations at baseline (Table 1). As a result of health requirements for military service, both groups consisted of healthy young adults with no preoperative OA characteristics. This gave us the opportunity to investigate the possible development of OA in the patellofemoral joint and to describe chondral lesions identified with MRI in relation to the surgical method of treatment.
Table 1.
Patient characteristics in the study groups
| Characteristic | Adductor magnus (median; range) | Roux-Goldthwait (median; range) | All patients (median; range) |
|---|---|---|---|
| Number of patients | 18 | 29 | 47 |
| Number of patients at final followup | 15 | 21 | 36 |
| Age (years) at time of surgery | 20.2 (19–22) | 20.0 (19–24) | 20.0 (19–24) |
| Age at followup | 30.2 (27–32) | 28.0 (24–33) | 30.0 (24–33) |
| Previous dislocations (number) | 5 (2–10) | 5 (2–9) | 5 (2–10) |
| Previous dislocations treated operatively | 2 | 1 | 3 |
| Contralateral dislocations, number (%) | 5 (38) | 5 (24) | 10 (29) |
| Followup (years) | 10.1 (8–13) | 7.0 (5–11) | 10.0 (5–11) |
| Arthrosis on plain radiographs* Grade I or more severe |
0 | 0 | 0 |
* At the time of surgery, graded as I or more severe according to Ahlbäck [3].
All MPFL reconstructions by adductor magnus tenodesis were performed by one of the authors (TV), and all of the Roux-Goldthwait procedures were performed by another senior orthopaedic surgeon (OK). Because the surgeons took turns on duty, the choice of procedure depended on the available surgeon and his personal preference, and thus the patients were not randomized. The adductor magnus tenodesis operations were performed using the technique described by Avikainen et al. [6] (Figs. 1, 2). The distal part of the adductor magnus tendon was cut approximately 8 cm proximal to its distal insertion. The length of the adductor magnus tendon graft was defined by the distance from the insertion of the adductor magnus tendon at the medial femoral condyle to the medial edge of the patella. The graft then was fixed with nonresorbable sutures near the medial border of the patellar periosteum to reconstruct the MPFL. In the original study, Avikainen et al. [6] performed this surgery mainly on acute primary dislocations and reinserted the MPFL into the periosteum of the medial femoral epicondyle. In our study of recurrent dislocations, reinsertion of the MPFL was not done because an acute tear site of the MPFL could not be identified in any of the cases. After graft fixation, the incised retinaculum was duplicated, and the fascia, the subcutis, and the skin were closed in layers. Before closure, the reconstructed MPFL was checked by knee flexion from 0° to 90° to ensure adequate adductor magnus graft gliding over the femoral epicondyle. Postoperative immobilization included patellar orthosis with flexion limited to 60° in all patients with a median time of 3 weeks (range, 2–4 weeks). No limitations on weightbearing were set.
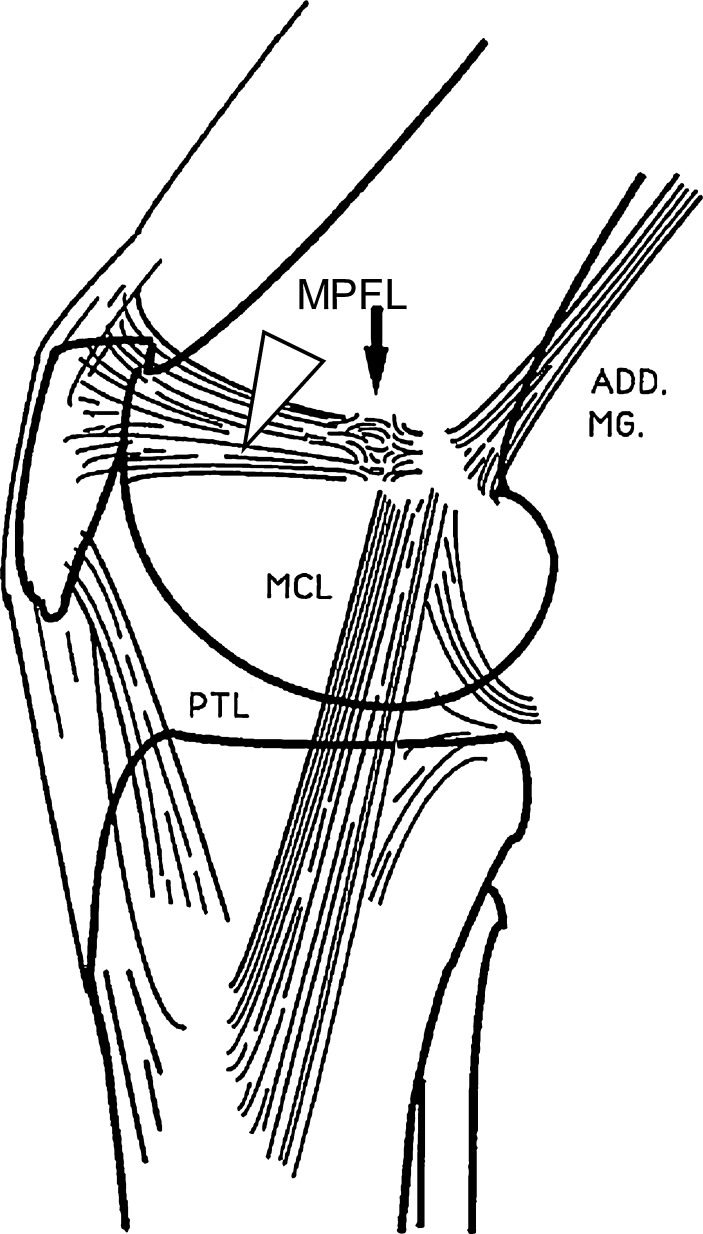
Fig. 1.
The medial patellofemoral ligament (MPFL, arrowhead) attaches firmly to the femur just anterior to the medial epicondyle (arrow). The distal insertion of the adductor magnus tendon (ADD.MG.). (Reprinted with the permission of Lippincott Williams & Wilkins from Avikainen VJ, Nikku RK, Seppanen-Lehmonen TK. Adductor magnus tenodesis for patellar dislocation: technique and preliminary results. Clin Orthop Relat Res. 1993;297:12–16.)
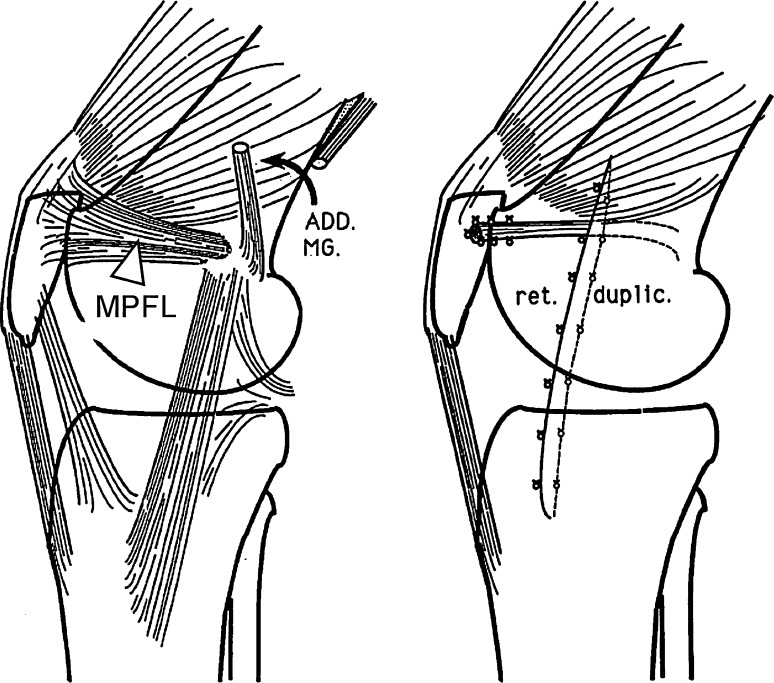
Fig. 2.
The distal part of the adductor magnus tendon (ADD.MG.) is cut approximately 8 cm proximal to its distal insertion. The graft is then fixed near the medial border of the patella to reconstruct the medial patellofemoral ligament (MPFL, arrowhead). (Reprinted with the permission of Lippincott Williams & Wilkins from Avikainen VJ, Nikku RK, Seppanen-Lehmonen TK. Adductor magnus tenodesis for patellar dislocation: technique and preliminary results. Clin Orthop Relat Res. 1993;297:12–16.)
The Roux-Goldthwait procedure followed the original technique [18]. The lateral half of the patellar tendon was transferred behind the medial half of the tendon, and the transferred lateral half was attached to the medial tibia to prevent lateral dislocation. After elevating a strip of the medial retinaculum, the lateral retinaculum was sectioned. The strip then was transferred into the opening in the lateral retinaculum and the medial incision was closed. Postoperative treatment included posterior splint or patellar orthosis immobilization for a median of 3 weeks (range, 2–4 weeks) with no limitations on weightbearing.
The followups were performed at a minimum of 5 years (median, 10.0 years; range, 5–11 years) postoperatively. The followup protocol consisted of a clinical examination and a systematic interview by the authors (PS, VM) with patellofemoral symptom scoring and assessment of the Tegner and Lysholm [48] activity level. In addition, plain radiographs and MR images of the surgically treated knee were taken, and questionnaires were used to record the number of redislocations and subsequent problems. For subjective symptoms and functional limitations, we used the patellofemoral rating scale by Kujala et al. [29] with a maximum possible score of 100 points (no symptoms); a score of 95 points or more was considered excellent, 94 to 85 good, 65 to 84 fair, and 64 or less as poor. The 100-mm visual analog scale (0 = no pain, 100 = most severe pain) was used to determine the patient’s subjective pain in the affected knee at followup. The institutional review board accepting this study was the Medical Ethics Committee of the institution and written consent was obtained from each patient.
Posteroanterior, lateral, and patellofemoral axial radiographs were taken preoperatively and at followup (Table 2). Axial Merchant [35] views with the knee at 45° flexion were used to analyze the medial and lateral facets of the patellofemoral joint. The radiographic parameters measured on the axial radiographs included the sulcus angle [7], lateral patellofemoral angle, and lateral patellar displacement as described by Laurin et al. [30]. Patellar height was measured on the lateral views as previously described by Insall and Salvati [23], which relates the length of the patellar tendon to the length of the patella. A patella alta was defined as a ratio greater than 1.0 according to Schlenzka and Schwesinger [45]. The severity of OA in the patellofemoral joint was assessed by plain radiographs by a senior, musculoskeletally specialized radiologist (MK) who was blinded to the type of surgical procedure and not involved with the surgery. Osteoarthrosis severity was graded from 0 to V by using the classification of Ahlbäck [3]: Grade 0 representing normal, Grade I joint narrowing, Grade II joint obliteration, and Grades III to V more severe destructive characteristics.
Table 2.
Postoperative radiographs
| Measure | Adductor magnus (median; range) | Roux-Goldthwait (median; range) | Normal value |
|---|---|---|---|
| Sulcus angle | 145 (125–166) | 141 (131–150) | < 150° |
| Lateral patellar angle | 0 (−8 to +10) | 4 (−2 to +10) | Horizontally or laterally |
| Lateral patellar displacement | 3 (0 to 7) | 3 (−1 to +7) | > 0 mm |
| Insall-Salvati index | 1.36 (1.04–1.75) | 1.26 (0.96– 1.47) | ≤ 1.0 |
In addition, at followup, MRI was performed to determine the locality and severity of possible cartilage defects in the patellofemoral joint. Magnetic resonance imaging was performed on 30 of the 36 patients at followup; two patients in the adductor magnus and four patients in the Roux-Goldthwait group were unable to have MRI and plain radiography. All MR images were obtained using a 1.0-Tesla MRI scanner (Signa Horizon; GE Medical Systems, Milwaukee, WI). A knee coil with a field of view of 10 to 16 cm was used. Slice thickness was 3 mm to 4 mm with a 0.5-mm or 1.0-mm intersection gap. Sagittal proton density spin-echo (SE) sequence images with fat suppression (repetition time/echo time = 3400 ms/17 ms, with two signals averaged and a 256 × 256 [516] matrix) and sagittal T1-weighted SE sequence images (680/11, with two signals averaged and a 256 × 256 [512] matrix) were obtained. T2-weighted fast SE sequences with fat saturation were obtained axially (2560/85, with two signals averaged and a 256 × 256 [512] matrix) and coronally (4000–4600/72–90, with two signals averaged and a 256 × 256 [512] matrix), and the combination of the axial and coronal planes was used to provide sufficient coverage of the articular surfaces and a high sensitivity and specificity for chondral defects [8].
All MR images were reviewed by a senior, musculoskeletally specialized radiologist (MK) who was not involved with the surgery and was blinded to the type of surgical procedure. Chondral lesions were classified according to their depth using the numeric grading system developed by the International Cartilage Repair Society (ICRS) and described by Brittberg and Winalski [9]. Grade I lesions were excluded as a result of the difficulties in differentiating these lesions from normal (ICRS Grade 0) cartilage by MRI [9]. Because previous studies have shown MRI is unreliable in detecting superficial lesions (softening) [13, 16, 27], only Graded II to IV lesions were documented to avoid false-positive MRI findings. ICRS Grade II describes articular cartilage defects extending down to less than 50% of cartilage depth, Grade III extending deeper than 50% of cartilage depth, and Grade IV are defects with full-thickness articular cartilage loss.
The Kruskal-Wallis test was used to test differences in the continuous skewed data (Kujala scores, Tegner levels) and the independent samples t-test in the continuous unskewed data (age, followup time, visual analog scale) between the groups. Differences in the two-way tables were determined with the Pearson chi square test (redislocations, subluxations, OA variables). Significance was set at p ≤ 0.05. The software package SPSS 14.0.1 for Windows (SPSS Inc, Chicago, IL) was used for statistical analysis.
Results
The redislocation rate was relatively low in both of the study groups. There was one redislocation (one of 15 [6.7%]) in the MPFL reconstruction group treated by adductor magnus tenodesis and three redislocations (three of 21 [14.3%]) in the comparison group treated by the Roux-Goldthwait distal realignment procedure (p = 0.52). Painful subluxations and patellofemoral reoperations resulting from patellar instability were similarly infrequent in both groups. The reoperation rate for redislocations was 7% (one of 15) in the adductor magnus group and 14% (three of 21) in the Roux-Goldthwait group (p = 0.68) (Table 3).
Table 3.
Results of the followups
| Study parameter | Adductor magnus (median; range) | Roux-Goldthwait (median; range) | Statistical value (p) |
|---|---|---|---|
| Redislocation, number (% ) | 1 (6.7%) | 3 (14.3%) | 0.52 |
| Kujala score (maximum 100 points) | 88.0 (57–100) | 86.0 (58–100) | 0.68 |
| Excellent (95–100 points), number | 4 | 5 | |
| Good (85–94 points), number | 6 | 7 | |
| Fair (65–84 points), number | 4 | 6 | |
| Poor (64 or less points), number | 1 | 3 | |
| Visual analog scale (0–100 mm) | 10 (0–50) | 10 (0–60) | 0.51 |
| Tegner activity level (1–10) | 4 (2–8) | 5 (2–7) | 0.55 |
| Control MRI | 13 | 17 | |
| Painful subluxations | 2 | 2 | |
| Chondral lesions* on MRI | 10/13 | 12/17 | 0.20 |
| Full-thickness† articular cartilage loss | 7/13 | 7/17 | 0.11 |
| Reoperation | 2 | 3 | 0.93 |
| Arthrosis on native radiographs‡ Grade I or more severe | 0 | 5 | 0.04 |
The overall outcomes, subjective and functional, were good in both groups. The median Kujala score for subjective symptoms and functional outcome in the adductor magnus group was 88 points (range, 57–100) and in the comparison group 86 points (range, 58–100) (p = 0.68). The median Tegner activity scores were 4 (range, 2–8) and 5 (range, 2–7) (p = 0.55), respectively. Two patients in both groups experienced painful patellar subluxations, and one patient in the adductor magnus group underwent reoperation resulting from painful subluxations during the followup period. In the adductor magnus group, difficulties in squatting and going down stairs were less common than in the Roux-Goldthwait group (Table 4), but the differences were not statistically significant. Clinical examination, including assessment of range of motion (values 141 [range, 130–155] and 144 [range, 135–155], respectively), did not reveal any significant differences between the groups.
Table 4.
Subjective assessment and functional knee limitations shown as proportions (%)
| Study parameter | Adductor magnus | Roux-Goldthwait | Subjective result |
|---|---|---|---|
| Stairs (%) | 87% | 56% | Normal |
| 13% | 31% | Pain going down stairs | |
| 0% | 13% | Always painful | |
| Running (%) | 60% | 50% | No difficulties |
| 33% | 38% | 0–2 km without pain | |
| 7% | 12% | Pain from the start; severe pain during running | |
| Squatting (%) | 67% | 31% | Normal |
| 20% | 69% | Painful when repeated | |
| 13% | 0% | Always painful or unable to squat | |
| Pain | 33% | 38% | None |
| 60% | 56% | Slight; interferes with sleep | |
| 7% | 6% | Occasionally severe |
Radiographic signs of OA were more frequent among patients treated with the Roux-Goldthwait procedure (p = 0.04) (Table 3). In this group, five patients had OA (at least Ahlbäck Grade I) in the patellofemoral joint compared with none in the adductor magnus group. Osteoarthritis was not seen in the patellofemoral joint on plain radiographs at the time of surgery. Likewise, the tibiofemoral joint was graded as normal in all of the cases. Regarding the tibiofemoral joint, at followup, none of the patients in either group had chondral lesions on MRI (Grade II or severe), and the native radiographs were graded as normal (Ahlbäck Grade 0) for all patients.
Distributions of the chondral lesions showed no statistically significant differences between the groups (Table 5). In the adductor magnus group, 10 of the 13 knees had at least Grade II chondral lesions in the patellofemoral joint. In the Roux-Goldthwait group, 12 of the 17 knees had at least Grade II chondral lesions (p = 0.20). Seven patients with severe, full-thickness Grade IV cartilage lesions either in the patellar or femoral articular surfaces were found in each group (Tables 3, 5). In the Roux-Goldthwait group, we noted the patients with full-thickness articular cartilage loss on MRI also had severe OA deformities on the native radiographs (Figs. 3, 4). In the adductor magnus group, full-thickness articular cartilage lesions also were detected, even in as much as 50% of the patients, yet none had an excessively large surface of articular cartilage loss on both sides of the patellofemoral joint to cause OA deformities.
Table 5.
Distribution of articular cartilage lesions* in the patellofemoral joint at followup†
| Method | Medial patella Grades II–III | Medial patella Grade IV | Lateral patella Grades II–III | Lateral patella Grade IV | Lateral femoral condyle Grades II–III | Lateral femoral condyle Grade IV | Medial femoral condyle Grades II–IV |
|---|---|---|---|---|---|---|---|
| Adductor magnus | 3 (23%) | 7 (54%) | 2 (15%) | 6 (46%) | 3 (23%) | 1 (8%) | 1 (8%) |
| Roux-Goldthwait | 6 (35%) | 5 (29%) | 1 (6%) | 4 (24%) | 2 (12%) | 1 (6%) | 0 |
* Chondral lesions were classified according to their depth using the numeric grading system developed by the International Cartilage Repair Society [9]; nearly normal Grade I lesions were excluded as a result of the insensitivity of MRI detection [9]; †shown as number of patients and as proportions.
Fig. 3A–B.
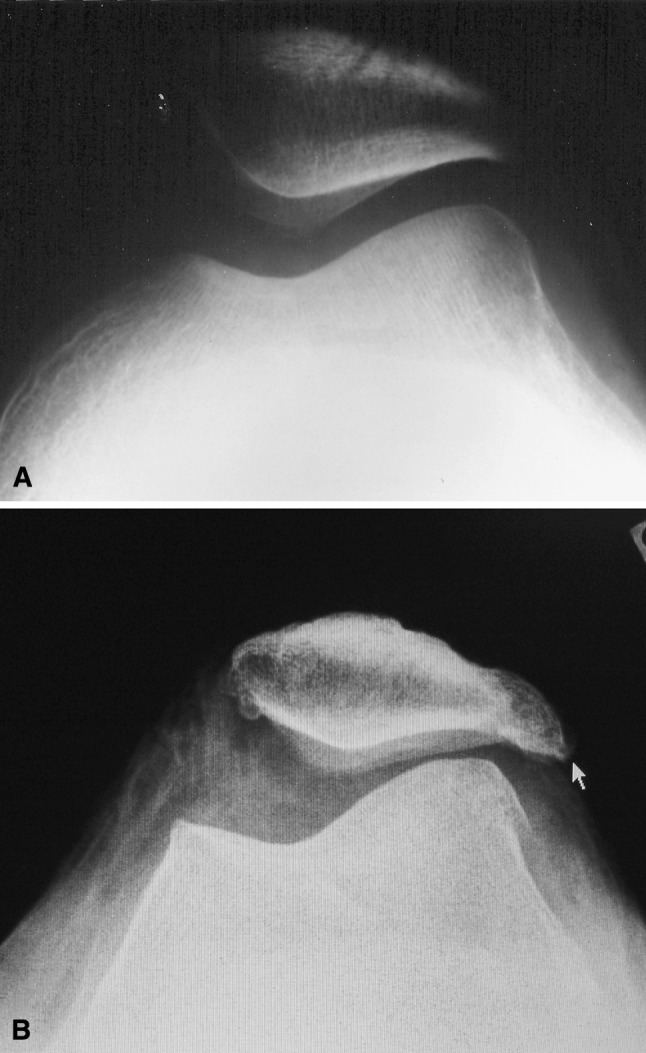
Plain axial radiographs show the patellofemoral joint (A) before surgery and (B) 10 years after surgery with patellofemoral osteoarthritis. The 29-year-old patient had more than one redislocation after surgery.
Fig. 4.

An MR image shows a severe patellofemoral articular cartilage defect (small arrow) and osteoarthrosis deformities (large arrows) in a 29-year-old patient 9 years after surgery.
Discussion
Our study is the first to explore the long-term results of MPFL reconstruction compared with distal realignment surgery. In the adductor magnus group, only one patellar redislocation occurred during the median followup of 10.1 years, which we consider a good result. The patients who underwent distal realignment surgery were treated by the Roux-Goldthwait procedure, which is considered a reliable method for treatment of recurrent patellar dislocation [10, 25, 28, 34]. Overall good long-term results were achieved in both groups after operatively treated recurrent patellar dislocation, the redislocation rate being 11% (four of 36). No statistically significant differences were found between the groups with the exception of OA seen on the plain radiographs of the Roux-Goldthwait group.
Recurrent patellofemoral subluxation or dislocation seems to predispose to development of patellofemoral OA. Magnetic resonance images at followup showed full-thickness articular cartilage loss in 14 patients (47%), and 73% of the patients had at least Grade II chondral lesions. Based on our findings, early signs of OA of the patellofemoral joint can be seen on MRI at the age of 30 years in patients with patellar dislocations. Of our 35 patients, there were five patients (14%) with OA visible on plain radiographs as well, all in the Roux-Goldthwait group. Previously published data of patients with OA changes after operatively treated patellar dislocation have shown proportions between 4% and 70% [5, 12, 19, 24, 33]. However, these studies have included a wide range of patients with ages up to 50 to 60 years, suggesting OA may have been caused by factors other than patellar dislocation. In the current study, although the median followup for the adductor magnus group was 3 years longer than in the Roux-Goldthwait group, no OA was seen on plain radiographs after the adductor magnus tenodesis. In the Roux-Goldthwait group, patients who had severe chondral lesions also had larger surfaces of articular cartilage loss compared with the adductor magnus group, which were observable as OA on plain radiographs. It might be that the MPFL reconstruction technique prevented additional deterioration of articular cartilage lesions and initiation of OA deformities.
Strengths of the study included homogeneity of the patients, all being young, healthy male adults, which resulted in good comparability between the groups. The median followup for the adductor magnus group was 10.1 years, which is longer than in the previously published study of adductor magnus tenodesis [6]. Furthermore, no previous studies have focused on the long-term MRI characteristics of OA after patellar dislocation. The limitation of our study was the lack of female gender and a nonoperative control group, which would have produced additional evidence regarding the potential benefits of MPFL reconstruction. The Roux-Goldthwait procedure may be performed less commonly now than previously, but as a result of the relatively long followup, this limitation is obvious.
Based on Kujala scores, both of the surgical procedures used in the current study resulted in good functional outcomes (median 88 in the adductor magnus group and 86 in the Roux-Goldthwait group). In the original publication of Kujala et al. [29], the mean score among patellar dislocators was only 62 points and 68 points for patellar subluxations. Maenpaa and Lehto described mean Kujala scores ranging from 74 to 82 points in their 100 patients with nonoperatively treated patellar dislocations in a followup study (average, 13 years) [32]. Previous studies describing several promising MPFL reconstructive techniques with followups are summarized [6, 14, 15, 40, 47] (Table 6). So far, only one study on MPFL reconstruction techniques has exceeded followup of 10 years [40]. The current study, however, reported a median Kujala score of 88 for the adductor magnus tenodesis procedure in a 10.1-year followup and is the only followup study on MPFL reconstruction technique with a comparison group reported.
Table 6.
Results of prior studies using medial patellofemoral ligament reconstructive techniques for patellar dislocations
| Study and year | Number of cases (age range*) | Controls | Followup (years) | Result (score) | Graft type | Osteoarthrosis evaluated at followup (result) |
|---|---|---|---|---|---|---|
| Drez et al. [14], 2001 | 19 (5–51 years) | None | 2.6 | 88 (Kujala) | Hamstring tendon | Not evaluated |
| Ellera Gomes et al. [15], 1992 | 30 (unknown) | None | 3.3 | (83% improved) | Polyester ligament | Not evaluated |
| Steensen et al. [47], 2005 | 14 (unknown) | None | 3.1 | (redislocations: none) | Quadriceps tendon | Not evaluated |
| Nomura et al. [40], 2007† | 24 (7–24 years) | None | 11.9 | 94 (Kujala) | Polyester tape | 1 moderate, 23 none-mild |
| Avikainen et al. [6], 1993 | 14 (15–27 years) | None | 7 | 84 (Lysholm) | Adductor Magnus tendon | Not evaluated |
| Current study | 15 (19–24 years) | 21‡ | 10.1 | 88 (Kujala) | Adductor Magnus tendon | None in study group; 5 in controls |
* Age at the time of surgery; †the longest followup study of several medial patellofemoral ligament studies by Nomura et al.; ‡distal realignment procedure.
In young adults, concomitant factors such as degenerative tibiofemoral arthrosis have a lesser impact on the outcome of the surgery, which may partly explain the overall good results seen in this study. Nonetheless, the overall findings of this 10-year median followup suggest a superior outcome compared with previous studies with similar or longer followups [26, 31, 32]. An obvious limitation of the previous studies has been the wide subject age range, from teenagers to people in their late 60s. Although our study was not randomized, development of OA characteristics as seen on native radiographs seemed to differ between these two surgical techniques. Furthermore, our findings suggest MPFL reconstructive surgery may prevent deterioration of patellofemoral OA as compared with the Roux-Goldthwait method, although this result was not confirmed by the Kujala scores. However, there is some evidence that the severity of patellofemoral OA and patellofemoral scoring do not correlate very well [20, 38].
Adductor magnus tenodesis is a reliable option for treatment of patellar instability. It seems to restore MPFL function adequately, resulting in a low recurrence rate and only few symptoms in a median followup of 10 years. One of the important findings of the current study was the presence of OA characteristics in most of the patients as shown by MRI at followup. Full-thickness patellofemoral articular cartilage defects were detected in almost 50% of the patients. On plain radiographs, there were considerably more patients with visible OA in the Roux-Goldthwait group than in the adductor magnus tenodesis group. The MPFL reconstruction technique by adductor magnus tenodesis prevented initiation of OA deformities as compared with distal realignment surgery. However, the diverse techniques for MPFL repair or reconstruction deserve additional investigation to ascertain their potential advantages over more traditional techniques. Owing to OA seen at the age of 30 years in patients with patellar dislocation, more knowledge regarding the risk factors and preventive methods for patellar dislocation is required.
Acknowledgments
We gratefully acknowledge the surgical expertise of Olli Kiviluoto, MD, PhD (Central Military Hospital, Helsinki, Finland) and the radiologic expertise of Martti Kiuru, MD, PhD (Central Military Hospital, Helsinki, Finland). We thank Marja Vajaranta (University of Tampere, Tampere, Finland) for editing the language.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aglietti P, Buzzi R, De Biase P, Giron F. Surgical treatment of recurrent dislocation of the patella. Clin Orthop Relat Res. 1994;308:8–17. [PubMed] [Google Scholar]
- 2.Aglietti P, Pisaneschi A, De Biase P. Recurrent dislocation of patella: three kinds of surgical treatment. Ital J Orthop Traumatol. 1992;18:25–36. doi: 10.1007/BF02620424. [DOI] [PubMed] [Google Scholar]
- 3.Ahlbäck S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Suppl. 1968;277:7–72. [PubMed] [Google Scholar]
- 4.Ahmad CS, Stein BE, Matuz D, Henry JH. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation: a review of eight cases. Am J Sports Med. 2000;28:804–810. doi: 10.1177/03635465000280060701. [DOI] [PubMed] [Google Scholar]
- 5.Arnbjornsson A, Egund N, Rydling O, Stockerup R, Ryd L. The natural history of recurrent dislocation of the patella: long-term results of conservative and operative treatment. J Bone Joint Surg Br. 1992;74:140–142. doi: 10.1302/0301-620X.74B1.1732244. [DOI] [PubMed] [Google Scholar]
- 6.Avikainen VJ, Nikku RK, Seppanen-Lehmonen TK. Adductor magnus tenodesis for patellar dislocation: technique and preliminary results. Clin Orthop Relat Res. 1993;297:12–16. [PubMed] [Google Scholar]
- 7.Brattstroem H. Shape of the intercondylar groove normally and in recurrent dislocation of patella: a clinical and x-ray-anatomical investigation. Acta Orthop Scand Suppl. 1964;68(suppl 68):1–148. [PubMed] [Google Scholar]
- 8.Bredella MA, Tirman PF, Peterfy CG, Zarlingo M, Feller JF, Bost FW, Belzer JP, Wischer TK, Genant HK. Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol. 1999;172:1073–1080. doi: 10.2214/ajr.172.4.10587150. [DOI] [PubMed] [Google Scholar]
- 9.Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85(suppl 2):58–69. doi: 10.2106/00004623-200300002-00008. [DOI] [PubMed] [Google Scholar]
- 10.Chrisman OD, Snook GA, Wilson TC. A long-term prospective study of the Hauser and Roux-Goldthwait procedures for recurrent patellar dislocation. Clin Orthop Relat Res. 1979;144:27–30. [PubMed] [Google Scholar]
- 11.Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Crosby EB, Insall J. Recurrent dislocation of the patella: relation of treatment to osteoarthritis. J Bone Joint Surg Am. 1976;58:9–13. [PubMed] [Google Scholar]
- 13.Disler DG, McCauley TR, Kelman CG, Fuchs MD, Ratner LM, Wirth CR, Hospodar PP. Fat-suppressed three-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: comparison with standard MR imaging and arthroscopy. AJR Am J Roentgenol. 1996;167:127–132. doi: 10.2214/ajr.167.1.8659356. [DOI] [PubMed] [Google Scholar]
- 14.Drez D, Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 15.Ellera Gomes JL. Medial patellofemoral ligament reconstruction for recurrent dislocation of the patella: a preliminary report. Arthroscopy. 1992;8:335–340. doi: 10.1016/0749-8063(92)90064-i. [DOI] [PubMed] [Google Scholar]
- 16.Gagliardi JA, Chung EM, Chandnani VP, Kesling KL, Christensen KP, Null RN, Radvany MG, Hansen MF. Detection and staging of chondromalacia patellae: relative efficacies of conventional MR imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol. 1994;163:629–636. doi: 10.2214/ajr.163.3.8079858. [DOI] [PubMed] [Google Scholar]
- 17.Garth WP, Jr, DiChristina DG, Holt G. Delayed proximal repair and distal realignment after patellar dislocation. Clin Orthop Relat Res. 2000;377:132–144. doi: 10.1097/00003086-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Goldthwait JE, Goldthwait JE. Slipping or recurrent dislocation of the patella: with the report of eleven cases. American Journal of Orthopedic Surgery, Vol 1, pp 293–308, 1903. J Bone Joint Surg Am. 1903;2003:2489. [PubMed] [Google Scholar]
- 19.Hampson WG, Hill P. Late results of transfer of the tibial tubercle for recurrent dislocation of the patella. J Bone Joint Surg Br. 1975;57:209–213. [PubMed] [Google Scholar]
- 20.Han I, Chang CB, Lee S, Lee MC, Seong SC, Kim TK. Correlation of the condition of the patellar articular cartilage and patellofemoral symptoms and function in osteoarthritic patients undergoing total knee arthroplasty. J Bone Joint Surg Br. 2005;87:1081–1084. doi: 10.1302/0301-620X.87B8.16209. [DOI] [PubMed] [Google Scholar]
- 21.Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174–182. doi: 10.1097/00003086-199804000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Hughston JC. Subluxation of the patella. J Bone Joint Surg Am. 1968;50:1003–1026. [PubMed] [Google Scholar]
- 23.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 24.Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y. Roentgenographic and clinical findings of patellofemoral osteoarthrosis: with special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res. 1990;252:190–197. [PubMed] [Google Scholar]
- 25.Jalovaara P, Seppanen-Lehmonen T, Lindholm RV. Krogius and Roux-Goldthwait operations for recurrent patellar dislocation. Acta Orthop Belg. 1988;54:380–383. [PubMed] [Google Scholar]
- 26.Juliusson R, Markhede G. A modified Hauser procedure for recurrent dislocation of the patella: a long-term follow-up study with special reference to osteoarthritis. Arch Orthop Trauma Surg. 1984;103:42–46. doi: 10.1007/BF00451317. [DOI] [PubMed] [Google Scholar]
- 27.Kawahara Y, Uetani M, Nakahara N, Doiguchi Y, Nishiguchi M, Futagawa S, Kinoshita Y, Hayashi K. Fast spin-echo MR of the articular cartilage in the osteoarthrotic knee: correlation of MR and arthroscopic findings. Acta Radiol. 1998;39:120–125. doi: 10.1080/02841859809172164. [DOI] [PubMed] [Google Scholar]
- 28.Koskinen SK, Rantanen JP, Nelimarkka OI, Kujala UM. Effect of Elmslie-Trillat and Roux-Goldthwait procedures on patellofemoral relationships and symptoms in patients with patellar dislocations. Am J Knee Surg. 1998;11:167–173. [PubMed] [Google Scholar]
- 29.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 30.Laurin CA, Dussault R, Levesque HP. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res. 1979;144:16–26. [PubMed] [Google Scholar]
- 31.Maenpaa H, Huhtala H, Lehto MU. Recurrence after patellar dislocation: redislocation in 37/75 patients followed for 6–24 years. Acta Orthop Scand. 1997;68:424–426. doi: 10.3109/17453679708996255. [DOI] [PubMed] [Google Scholar]
- 32.Maenpaa H, Lehto MU. Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med. 1997;25:213–217. doi: 10.1177/036354659702500213. [DOI] [PubMed] [Google Scholar]
- 33.Maenpaa H, Lehto MU. Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res. 1997;339:156–162. doi: 10.1097/00003086-199706000-00021. [DOI] [PubMed] [Google Scholar]
- 34.Marcacci M, Zaffagnini S, Iacono F, Visani A, Petitto A, Neri NP. Results in the treatment of recurrent dislocation of the patella after 30 years’ follow-up. Knee Surg Sports Traumatol Arthrosc. 1995;3:163–166. doi: 10.1007/BF01565476. [DOI] [PubMed] [Google Scholar]
- 35.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 36.Muneta T, Sekiya I, Tsuchiya M, Shinomiya K. A technique for reconstruction of the medial patellofemoral ligament. Clin Orthop Relat Res. 1999;359:151–155. doi: 10.1097/00003086-199902000-00016. [DOI] [PubMed] [Google Scholar]
- 37.Nikku R, Nietosvaara Y, Aalto K, Kallio PE. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76:699–704. doi: 10.1080/17453670510041790. [DOI] [PubMed] [Google Scholar]
- 38.Niskanen RO, Paavilainen PJ, Jaakkola M, Korkala OL. Poor correlation of clinical signs with patellar cartilaginous changes. Arthroscopy. 2001;17:307–310. doi: 10.1053/jars.2001.21240. [DOI] [PubMed] [Google Scholar]
- 39.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23:260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35:1851–1858. doi: 10.1177/0363546507306161. [DOI] [PubMed] [Google Scholar]
- 41.Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13:510–515. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 42.Nomura E, Inoue M, Osada N. Augmented repair of avulsion-tear type medial patellofemoral ligament injury in acute patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2005;13:346–351. doi: 10.1007/s00167-004-0544-2. [DOI] [PubMed] [Google Scholar]
- 43.Rantanen J, Paananen M. Modified Hauser operation for patellar instability: immediate mobilization of 35 knees, a 5–8 year follow-up study. Acta Orthop Scand. 1996;67:455–458. doi: 10.3109/17453679608996667. [DOI] [PubMed] [Google Scholar]
- 44.Sanders TG, Morrison WB, Singleton BA, Miller MD, Cornum KG. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr. 2001;25:957–962. doi: 10.1097/00004728-200111000-00021. [DOI] [PubMed] [Google Scholar]
- 45.Schlenzka D, Schwesinger G. The height of the patella: an anatomical study. Eur J Radiol. 1990;11:19–21. doi: 10.1016/0720-048X(90)90097-U. [DOI] [PubMed] [Google Scholar]
- 46.Spritzer CE, Courneya DL, Burk DL, Jr, Garrett WE, Strong JA. Medial retinacular complex injury in acute patellar dislocation: MR findings and surgical implications. AJR Am J Roentgenol. 1997;168:117–122. doi: 10.2214/ajr.168.1.8976933. [DOI] [PubMed] [Google Scholar]
- 47.Steensen RN, Dopirak RM, Maurus PB. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy. 2005;21:365–370. doi: 10.1016/j.arthro.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 48.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]