Abstract
Total disc replacement (TDR) clinical success has been reported to be related to the residual motion of the operated level. Thus, accurate measurement of TDR range of motion (ROM) is of utmost importance. One commonly used tool in measuring ROM is the Oxford Cobbometer. Little is known however on its accuracy (precision and bias) in measuring TDR angles. The aim of this study was to assess the ability of the Cobbometer to accurately measure radiographic TDR angles. An anatomically accurate synthetic L4–L5 motion segment was instrumented with a CHARITE artificial disc. The TDR angle and anatomical position between L4 and L5 was fixed to prohibit motion while the motion segment was radiographically imaged in various degrees of rotation and elevation, representing a sample of possible patient placement positions. An experienced observer made ten readings of the TDR angle using the Cobbometer at each different position. The Cobbometer readings were analyzed to determine measurement accuracy at each position. Furthermore, analysis of variance was used to study rotation and elevation of the motion segment as treatment factors. Cobbometer TDR angle measurements were most accurate (highest precision and lowest bias) at the centered position (95.5%), which placed the TDR directly inline with the x-ray beam source without any rotation. In contrast, the lowest accuracy (75.2%) was observed in the most rotated and off-centered view. A difference as high as 4° between readings at any individual position, and as high as 6° between all the positions was observed. Furthermore, the Cobbometer was unable to detect the expected trend in TDR angle projection with changing position. Although the Cobbometer has been reported to be reliable in different clinical applications, it lacks the needed accuracy to measure TDR angles and ROM. More accurate ROM measurement methods need to be developed to help surgeons and researchers assess radiological success of TDRs.
Keywords: Cobbometer, Total disc replacement, Precision and bias, Accuracy, Range of motion
Introduction
Total disc arthroplasty is an alternative to interbody fusion for the treatment of degenerative disc disease. However, unlike interboby fusion, the design of a total disc replacement (TDR) aims to provide the advantage of motion preservation at the operated level. With considerable (>5°) segmental flexion–extension range of motion (ROM), TDRs have been correlated to better clinical outcomes [7], and suggested to have reduced long-term risk in the development of radiographic adjacent level degeneration [8, 18]. Correct surgical placement of the TDR has been reported to be essential in achieving these improved clinical outcomes as well as flexion–extension ROM [3, 17]. Accurate post-operative measurement of TDR ROM is thus important in gauging both implant performance and surgical outcome.
The increasing use of TDRs has made measurement accuracy of TDR flexion–extension ROM a topic of interest. The Oxford Cobbometer is a commonly used tool in clinical practice to radiographically measure deformity and spinal ROM (Fig. 1). Using an intraclass correlation coefficient (ICC) analysis, the inter-observer (ICC ≥ 0.939) and intra-observer (ICC = 0.856–0.976) agreements for spinal deformity assessment using the Cobbometer have been shown to be reliable [19]. The authors of the study report a 2° absolute mean difference between readings and a ± 5.8° limit of agreement (± 2SD, 95%) improving on previous findings using the traditional Cobb method [2, 19]. Knowing that the Cobbometer is reliable in repeated readings as shown by the inter- and intra-observer agreements tells us only about its precision however, and not necessarily about its measurement bias. Further improvements in accuracy (i.e., increases in precision and reductions in bias) may be necessary when evaluating TDR ROM as this motion has been suggested to be less than that observed for the normal spine [5, 6].
Fig. 1.
The Oxford Cobbometer
Confidence in the clinical angle measurements made using the Oxford Cobbometer and advances in accuracy can only be expected following an understanding of both the precision and bias errors present in the measurement. This study aims to evaluate the ability of the Oxford Cobbometer, a commonly used clinical tool for TDR ROM measurements, to accurately detect known TDR angle deviations occurring as a result of variations in patient placement positions with respect to the x-ray beam source. To achieve this objective, both bias and precision errors are evaluated for TDR angle measurements made using the Oxford Cobbometer. Furthermore, a secondary goal of this study is to determine a Cobbometer based angular threshold that must be surpassed before one can be certain that TDR motion has occurred. A threshold is important for identifying with confidence that the angle differences measured between readings are indeed indicative of true TDR motion and not the result of obliquely imaged angle deviations resulting from variations in patient placement.
Materials and methods
All of the Cobbometer measurements in this study were made on radiographic images granted from a previous computational study [10]. Complete procedural details of the computational study are presented elsewhere [10] and summarized here. An anatomically accurate synthetic L4–L5 motion segment was instrumented with a CHARITE artificial disc (DePuy Spine, Raynham, MA, USA). The instrumented motion segment was mounted to a frame allowing for independent rotation and elevation of the motion segment while holding the TDR angle and anatomical position between L4 and L5 fixed. The fixed motion segment was imaged at seven rotations (−15°, −10°, −5°, 0°, +5°, +10°, and +15°) and four elevations (0, −5, −10, and −15 cm) within the radiographic field of view, giving a total of 28 digital radiographs. The negative and positive rotations corresponded to turning and facing the anterior part of the motion segment toward the detecting plate or x-ray source, respectively.
Each of the 28 digital radiographs was measured using the Cobbometer, as would be done in clinical practice, on ten separate occasions, in random order, by a blinded experienced observer. The observer was instructed to use the external corners of the inferior and superior TDR endplates as landmarks for the angle measurements. A total of 280 angles were measured.
The resulting measurements are summarized using descriptive statistics. The term “trial angle” is used to identify the mean value of the ten repeated angle readings at each of the 28 imaged positions. The “absolute angle” is used to represent the mean of the 28 trial angles. Bias errors were determined by taking the difference between the mean Cobbometer angle (trial angle) measurements and the expected angles at each position. The expected (i.e., calibrated or true) angle at each position was determined using a high accuracy computational approach and a set of Steinmann pins instrumented on the same motion segment and seen on the 28 radiographs [10]. Furthermore, a t-test was employed to compare and identify significant differences between the clinical Cobbometer based angle measurements and the expected angles.
A precision interval for the Cobbometer measurements was determined at a 95% probability level. In addition, to provide an overall estimate of measurement error, a percent accuracy (A) for each position was determined using the following equation:
 |
where θ is the expected angle, and β is the angle measured using the Cobbometer. Finally, a two-way repeated measures analysis of variance (ANOVA) was utilized to study the interactions and average effects of rotation and elevation on the Cobbometer measured angles. Significance levels were categorized as extremely statistical significant (α = 0.001), highly statistical significant (α = 0.01), and statistically significant (α = 0.05).
Results
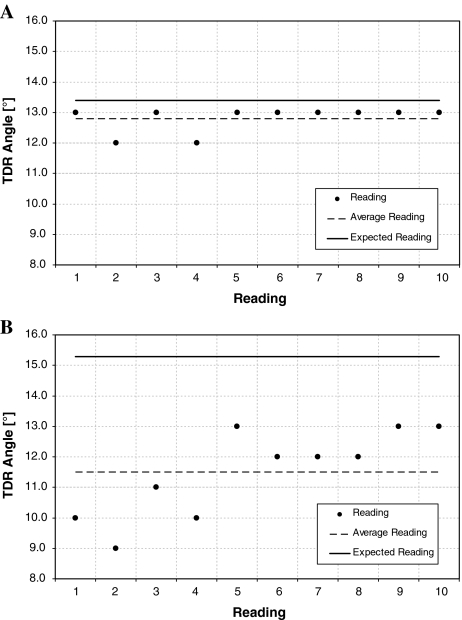
Cobbometer TDR angle measurements were most accurate (95.5%) at the centered position (0 cm,0°) which placed the TDR directly inline with the x-ray beam source (Table 1). Measurements at this position were also the most precise (± 1.0°, 95% probability) and had the least amount of bias (0.6°) (Fig. 2a). In contrast, Cobbometer measurements at the −15 cm, + 15° position had the lowest accuracy (75.2%), the least precision (± 3.2°, 95% probability), and highest magnitude of bias (3.8°) (Fig. 2b).
Table 1.
Cobbometer measurement statistics at each of the 28 imaging positions
| Imaging position: height (cm), rotation (°) | Trial angle (°) | Precision interval (°) | Bias (°) | Accuracy (%) |
|---|---|---|---|---|
| 0, −15 | 11.9 | ±1.3 | 0.9 | 92.5 |
| 0, −10 | 12.0 | ±1.5 | 1.0 | 92.3 |
| 0, −5 | 12.3 | ±1.5 | 0.9 | 93.4 |
| 0,0 | 12.8 | ±1.0 | 0.6 | 95.5 |
| 0, + 5 | 12.5 | ±1.6 | 1.5 | 89.6 |
| 0, + 10 | 12.6 | ±1.2 | 1.9 | 86.8 |
| 0, + 15 | 12.5 | ±1.6 | 2.7 | 82.5 |
| −5, −15 | 11.7 | ±2.6 | 1.2 | 89.0 |
| −5, −10 | 11.6 | ±1.6 | 1.4 | 89.6 |
| −5, −5 | 12.3 | ±1.1 | 0.9 | 93.5 |
| −5,0 | 12.0 | ±1.8 | 1.6 | 88.5 |
| −5, + 5 | 11.7 | ±2.4 | 2.2 | 84.1 |
| −5, + 10 | 12.4 | ±1.6 | 2.1 | 85.4 |
| −5, + 15 | 12.1 | ±2.2 | 3.0 | 80.0 |
| −10, −15 | 12.1 | ±2.9 | 0.7 | 90.5 |
| −10, −10 | 11.9 | ±1.7 | 1.0 | 91.9 |
| −10, −5 | 11.7 | ±1.5 | 1.5 | 88.8 |
| −10,0 | 11.4 | ±1.9 | 2.1 | 84.3 |
| −10, + 5 | 11.9 | ±3.1 | 2.1 | 85.0 |
| −10, + 10 | 11.8 | ±3.0 | 2.7 | 81.4 |
| −10, + 15 | 11.9 | ±2.7 | 3.3 | 78.3 |
| −15, −15 | 11.0 | ±1.5 | 1.9 | 85.6 |
| −15, −10 | 11.4 | ±1.6 | 1.6 | 87.5 |
| −15, −5 | 11.4 | ±1.9 | 1.9 | 86.1 |
| −15,0 | 11.9 | ±2.2 | 1.6 | 88.0 |
| −15, + 5 | 11.3 | ±3.2 | 2.7 | 80.9 |
| −15, + 10 | 11.6 | ±2.9 | 2.9 | 79.9 |
| −15, + 15 | 11.5 | ±3.2 | 3.8 | 75.2 |
| Mean | 11.9 | ±2.0 | 1.8 | 86.6 |
Fig. 2.
a Graph showing both precision (± 1.0°) and bias (0.6°) for the ten repeated TDR angle readings at the 0 cm,0° imaging position. The Oxford Cobbometer was most accurate (95.5%) at this position. b Similar graph showing precision (± 3.2°) and bias (3.8°) for the −15 cm, + 15° imaging position. Readings at this position were the least accurate (75.2%)
A difference of 4° (largest range) between readings at an individual position was observed at the −5 cm, −15°; −10 cm, −15°; −15 cm, + 5°; and the −15 cm, + 15° positions (Table 2). In contrast, the least variation (smallest range) between readings was 1.0° at the 0 cm,0°; 0 cm, + 10°; and −5 cm, −5° positions (Fig. 3). Considering all of the 280 clinical angle measurements made using the Cobbometer on the motionless TDR radiographs, irrespective of position, the maximum and minimum readings were 15° and 9°, respectively, resulting in a 6° measurement variation.
Table 2.
Largest and smallest angle measurement differences (range) between readings at individual imaging positions
| Imaging position: height (cm), rotation (°) | Maximum reading (°) | Minimum reading (°) | |
|---|---|---|---|
| Maximum range | |||
| 4° | −5, −15 | 14.0 | 10.0 |
| −10, −15 | 15.0 | 11.0 | |
| −15, + 5 | 13.0 | 9.0 | |
| −15, + 15 | 13.0 | 9.0 | |
| Minimum range | |||
| 1° | 0,0 | 13.0 | 12.0 |
| 0, + 10 | 13.0 | 12.0 | |
| −5, −5 | 13.0 | 12.0 | |
Fig. 3.
Digital radiographs illustrating the: a most accurate imaging position (0 cm, 0°) allowing for better precision in repeated TDR angle measurements as compared to: b the less accurate −15 cm, + 15° position showing an oblique view of the TDR making it more difficult to perform repeated readings of the same TDR angle
Comparing between the expected and clinically measured angles at each position using a t-test, extremely significant differences were identified in all but the following four positions: 0 cm, −5°; −5 cm, −15°; −10 cm, −15°; and −10 cm, −10°. The repeated readings at position 0 cm, −5° were found to be highly statistically significant, the readings at positions: −5 cm, −15° and −10 cm, −10° were statistically significantly, whereas the readings at position −10 cm, −15° were not significantly different. The expected angles showed a larger range and a different trend with changing position as compared to what could be detected using the clinical Cobbometer. This is exemplified at the 0-cm elevation with changing rotation in Fig. 4.
Fig. 4.
Expected and Cobbometer measured TDR angle trend with changing motion segment rotation at the 0 cm elevation
Both rotation and elevation of the motion segment were studied as treatment factors using a balanced design repeated measures two-way ANOVA. The clinical Cobbometer measurements showed elevation effects to be extremely statistically significant (P = 0.0001). Rotation (P = 0.344) and interaction (P = 0.622) effects were found to be insignificant. This finding leads to the conclusion that elevation of the motion segment can independently affect the value of the observed TDR angle.
Discussion
Accurate post-operative measurement of TDR ROM is important in assessing both implant performance and surgical outcome. Small amounts of TDR motion may considerably influence clinical outcome [6–8, 15]. TDR motion greater than 5° has been suggested to reduce the incidence of adjacent level degeneration [6–8]. Previous studies report on observer agreement statistics in TDR ROM measurements which tell us only about measurement precision [1, 14, 15]. This study aims to report on TDR angle measurement accuracy, analyzing both precision and bias errors, of the commonly used Oxford Cobbometer. Furthermore, we aim to establish a Cobbometer based threshold angle at which variations in patient placement with respect to the x-ray beam source during imaging, known to result in angle deviations during measurement, are not misinterpreted as TDR motion.
Findings from this study suggest that the Cobbometer may lack the accuracy to measure TDR angles and in turn ROM. Currently, it is common clinical practice for example, to center the x-ray beam at the mid-lumbar spine and not at the level of the arthroplasty. Our findings show that when the TDR is positioned below the centered position (e.g., at the −15 cm,0°), even without any motion segment rotation, Cobbometer measurement accuracy is reduced from 95.5 to 88.0% (see Table 1). Both of the constituent errors, precision and bias, are increased from ± 1.0° to ± 2.2°, and from 0.6° to 1.6°, respectively. In the worse case, when patient rotation is introduced (e.g., −15 cm,15°), the Cobbometer measurement accuracy is further reduced to 75.2% with decreasing precision (± 3.2°) and increasing bias (3.8°). At this position, the bias error exceeds the precision interval, and the Cobbometer is no longer capable of measuring the true angle. It is thus recommended from these findings, to aim at minimizing Cobbometer measurement error by placing the patient parallel to the plate with the beam centered not at the mid-lumbar spine, but at the level of the arthroplasty.
In terms of the Cobbometer’s ability to detect the known trend in TDR angle deviations caused by variations in patient placement during imaging [10], the results form this study suggest that the Cobbometer, although shown to be a reliable tool in measuring fracture kyphosis [19], has limited sensitivity. The expected trend with changing position was not followed by the Cobbometer (see Fig. 4). Extremely statistically significant differences between the Cobbometer findings and the expected values were identified in most positions. Furthermore, the ANOVA findings from the Cobbometer measurements conclude that only elevation of the motion segment can independently affect the value of the observed TDR angle. In contrast, expected values have been found to be highly (elevation effects) and extremely (rotational effects) statistically significant without interaction, leading to the conclusion that both rotation and elevation can independently effect the TDR angles measured [10]. These findings suggest that further research is needed with an aim at developing newer measurement approaches/instruments that improve on the Cobbometer’s accuracy in making TDR angle measurements.
In terms of a threshold for motion, inherent radiographic Cobb angle measurement errors have lead studies to adapt a value as low as 2° between flexion–extension radiographs that must be surpassed before the occurrence of TDR motion [6]. Other studies however continue to report TDR flexion–extension ROM values even below this suggested 2° threshold [13, 17]. A recent study suggests that a threshold angle of at least 4.6° between flexion–extension radiographs must be measured before one can be certain that the ROM of the TDR is not 0 [15]. Furthermore, previous findings using the same motionless (by protocol, not by design) TDR as in the present study, have shown that variations in patient placement (rotation and elevation at the level of the arthroplasty) with respect to the radiographic beam source may lead to angle measurement inaccuracies and misinterpretations concerning TDR motion [10]. The authors, using a high accuracy computational based measurement method, report a threshold angle as high as 5.34°. Differences in TDR angle measurements below this threshold may be attributed to patient placement and may at times be incorrectly interpreted as TDR motion. Using a high accuracy computational based approach however, produces a lower end in the measurement error as compared to what can be expected in everyday clinical practice. Thus even the 4.6° threshold previously reported for the occurrence of motion may indeed be low [15].
The current study takes a more clinical approach, as compared to the aforementioned computational study, to address this issue by evaluating the accuracy of the commonly used Cobbometer in making TDR angle measurements. Based on the same sample of patient placement positions and using the same motionless TDR protocol, differences in Cobbometer readings were as high as 6° between the extreme maximum and minimum readings (see Table 2). This range, calculated by subtracting the TDR maximum and minimum angle readings from all the positions evaluated, prior to any averaging, presents the error range for the worse case scenario observed. Thus, these findings suggest that from one Cobbometer reading to another, even without any TDR motion, the observer may be mislead to believe that as much as 6° of motion has occurred. This observed motion, caused from limitations in instrumentation (Cobbometer), patient placement (rotation and elevation), and measurement method (TDR endplates) is reduced when looking at the maximum range for a single position. At a single position, the largest difference between the ten repeated readings was found to be 4.0°. This suggests that for a single reading (i.e., either the flexion or extension reading in a TDR ROM measurement) an error of as much as 4.0° may be observed. Caution should be taken however, when interpreting these findings. As mentioned previously, instrument (i.e., Cobbometer) bias may exceed its precision leading to inaccurate measurements and findings. Thus, in practice, the Cobbometer may be an inaccurate tool in measuring TDR angles.
Our study is limited to a single measurement method using the external corners of the inferior and superior TDR endplates as landmarks for the angle measurements. Other studies have looked at different radiographic methods for measurement of fracture kyphosis [11, 19], sagittal translation [20], and TDR ROM [1, 14]. In our case, the decision to use a Cobbometer was based on its simplicity, proven reliability [19], and frequent use in clinical practice. Our goal was to replicate TDR angle measurements as would be performed at a typical clinical setting.
Anterior–posterior translation was not tested since it would be equivalent to elevation the only difference being the orientation of the angle to be measured. Similarly sagittal rotation was not tested since angular measurements would be unaffected due to the divergent nature of the x-ray beam.
The use of a motion segment without the surrounding tissue and body mass presents an additional limitation. Our findings however, suggest that the Cobbometer may be an inaccurate way to measure TDR angles, a conclusion which would be further amplified with a reduction in radiographic imaging quality that may follow with the added body mass.
In summary, since measurement of ROM is important in assessing the success of TDRs, it is crucial to aim at minimizing Cobbometer measurement error by placing the patient parallel to the plate with the beam centered not at the mid-lumbar spine, but at the level of the arthroplasty. This may be difficult to do in practice however. Even if the patient is optimally placed, rotational malposition of the TDR itself may cause decreases in measurement accuracy. Furthermore, maintaining a comparable TDR alignment in flexion and extension views may be especially difficult. We must thus aim at developing newer three-dimensional measurement approaches/instruments that improve TDR angle measurement accuracy. Radiostereometric analysis (RSA) may be a way forward. RSA involves implantation of tantalum markers to analyze implant and joint micro-motion and has been shown to be accurate [4, 9, 12, 16, 21]. Further work is needed to evaluate this technology for use in TDR ROM measurements. Presently, clinicians should be aware of the inherent limitations in Cobbometer radiographic TDR angle measurements, especially when measurements show a small TDR ROM.
Acknowledgment
The Département de l’Appareil Locomoteur receives financial support in the form of a research grant from DePuy Spine, Inc., Raynham, Massachusetts, United States.
References
- 1.Cakir B, Richter M, Puhl W, Schmidt R. Reliability of motion measurements after total disc replacement: the spike and the fin method. Eur Spine J. 2006;15:165–173. doi: 10.1007/s00586-005-0942-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carman DL, Browne RH, Birch JG. Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. J Bone Joint Surg Am. 1990;72:328–333. [PubMed] [Google Scholar]
- 3.Freeman BJ, Davenport J. Total disc replacement in the lumbar spine: a systematic review of the literature. Eur Spine J. 2006;15(Suppl 3):S439–S447. doi: 10.1007/s00586-006-0186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garling EH, Kaptein BL, Geleijns K, Nelissen RG, Valstar ER. Marker configuration model-based Roentgen fluoroscopic analysis. J Biomech. 2005;38:893–901. doi: 10.1016/j.jbiomech.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 5.Hayes MA, Howard TC, Gruel CR, Kopta JA. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine. 1989;14:327–331. doi: 10.1097/00007632-198903000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Huang RC, Girardi FP, Cammisa FP, Jr, Tropiano P, Marnay T. Long-term flexion-extension range of motion of the prodisc total disc replacement. J Spinal Disord Tech. 2003;16:435–440. doi: 10.1097/00024720-200310000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Huang RC, Girardi FP, Cammisa FP, Jr, Lim MR, Tropiano P, Marnay T. Correlation between range of motion and outcome after lumbar total disc replacement: 8.6-year follow-up. Spine. 2005;30:1407–1411. doi: 10.1097/01.brs.0000166528.67425.0e. [DOI] [PubMed] [Google Scholar]
- 8.Huang RC, Tropiano P, Marnay T, Girardi FP, Lim MR, Cammisa FP., Jr Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine. 2006;J6:242–247. doi: 10.1016/j.spinee.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Ioppolo J, Borlin N, Bragdon C, Li M, Price R, Wood D, Malchau H, Nivbrant B. Validation of a low-dose hybrid RSA and fluoroscopy technique: determination of accuracy, bias and precision. J Biomech. 2007;40:686–692. doi: 10.1016/j.jbiomech.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Kosmopoulos V, McManus J, Schizas C (2007) Consequences of patient position in the radiographic measurement of artificial disc replacement angles. Eur Spine J doi: 10.1007/s00586–007-0486-8 [DOI] [PMC free article] [PubMed]
- 11.Kuklo TR, Polly DW, Owens BD, Zeidman SM, Chang AS, Klemme WR. Measurement of thoracic and lumbar fracture kyphosis: evaluation of intraobserver, interobserver, and technique variability. Spine. 2001;26:61–65. doi: 10.1097/00007632-200101010-00012. [DOI] [PubMed] [Google Scholar]
- 12.Lawrie DF, Downing MR, Ashcroft GP, Gibson PH. Insertion of tantalum beads in RSA of the hip: variations in incidence of extra-osseous beads with insertion site. Acta Orthop Scand. 2003;74:404–407. doi: 10.1080/00016470310017695. [DOI] [PubMed] [Google Scholar]
- 13.Lemaire JP, Carrier H, Sariali El-H, Skalli W, Lavaste F (2005) Clinical and radiological outcomes with the Charite artificial disc: a 10-year minimum follow-up.[erratum appears in J Spinal Disord Tech. 2006 Feb;19(1):76 Note: Sari Ali, El-Hadi [corrected to Sariali, El-hadi]]. J Spinal Disord Tech 18:353–359 [DOI] [PubMed]
- 14.Lim MR, Girardi FP, Zhang K, Huang RC, Peterson MG, Cammisa FP., Jr Measurement of total disc replacement radiographic range of motion: a comparison of two techniques. J Spinal Disord Tech. 2005;18:252–256. [PubMed] [Google Scholar]
- 15.Lim MR, Loder RT, Huang RC, Lyman S, Zhang K, Sama A, Papadopoulos EC, Warner K, Girardi FP, Cammisa FP., Jr Measurement error of lumbar total disc replacement range of motion. Spine. 2006;31:E291–E297. doi: 10.1097/01.brs.0000216452.54421.ea. [DOI] [PubMed] [Google Scholar]
- 16.Lind B, Zoega B, Anderson PA. A radiostereometric analysis of the Bryan cervical disc prosthesis. Spine. 2007;32:885–890. doi: 10.1097/01.brs.0000259925.11230.dd. [DOI] [PubMed] [Google Scholar]
- 17.McAfee PC, Cunningham B, Holsapple G, Adams K, Blumenthal S, Guyer RD, Dmietriev A, Maxwell JH, Regan JJ, Isaza J. A prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcomes. Spine. 2005;30:1576–1583. doi: 10.1097/01.brs.0000170561.25636.1c. [DOI] [PubMed] [Google Scholar]
- 18.El-H Sariali, Lemaire JP, Pascal-Mousselard H, Carrier H, Skalli W. In vivo study of the kinematics in axial rotation of the lumbar spine after total intervertebral disc replacement: long-term results: a 10–14 years follow up evaluation. Eur Spine J. 2006;15:1501–1510. doi: 10.1007/s00586-005-0016-5. [DOI] [PubMed] [Google Scholar]
- 19.Seel EH, Verrill CL, Mehta RL, Davies EM. Measurement of fracture kyphosis with the Oxford Cobbometer: intra- and interobserver reliabilities and comparison with other techniques. Spine. 2005;30:964–968. doi: 10.1097/01.brs.0000158952.43914.fb. [DOI] [PubMed] [Google Scholar]
- 20.Shaffer WO, Spratt KF, Weinstein J, Lehmann TR, Goel V. 1990 Volvo Award in clinical sciences. The consistency and accuracy of roentgenograms for measuring sagittal translation in the lumbar vertebral motion segment. An experimental model. Spine. 1990;15:741–750. doi: 10.1097/00007632-199008010-00003. [DOI] [PubMed] [Google Scholar]
- 21.Yuan X, Ryd L, Tanner KE, Lidgren L. Roentgen single-plane photogrammetric analysis (RSPA). A new approach to the study of musculoskeletal movement. J Bone Joint Surg Br. 2002;84:908–914. doi: 10.1302/0301-620X.84B6.11146. [DOI] [PubMed] [Google Scholar]