Abstract
While the clinical and neuropathological characterization of Alzheimer’s Disease (AD) is well defined, our understanding of the progression of pathologic mechanisms in AD remains unclear. Post-mortem brains from individuals who did not fulfill clinical criteria for AD may still demonstrate measurable levels of AD pathologies to suggest that they may have presented with clinical symptoms had they lived longer or are able to stave off disease progression. Comparison between such individuals and those clinically diagnosed and pathologically confirmed to have AD will be key in delineating AD pathogenesis and neuroprotection. In this study, we expression profiled laser capture microdissected non-tangle bearing neurons in 6 post-mortem brain regions that are differentially affected in the AD brain from 10 non-demented individuals demonstrating intermediate AD neuropathologies (NDAD; Braak stage of II through IV and CERAD rating of moderate to frequent) and evaluated this data against that from individuals who have been diagnosed with late onset AD as well as healthy elderly controls. We identified common statistically significant expression changes in both NDAD and AD brains that may establish a degenerative link between the two cohorts, in addition to NDAD specific transcriptomic changes. These findings pinpoint novel targets for developing earlier diagnostics and preventative therapies for AD prior to diagnosis of probable AD. We also provide this high-quality, low post-mortem interval (PMI), cell-specific, and region-specific NDAD/AD reference data set to the community as a public resource.
Keywords: Laser capture microdissection, Affymetrix microarrays, Expression profiling, Neuron, Transcriptomics
1. Introduction
With its increasing incidence, Alzheimer’s Disease (AD) has become a major concern for both the research community as well as the aging global population. Because identification of pathological markers is currently the only approach to confirming diagnosis, physicians and researchers have begun to focus on developing early diagnostic tools to allow for earlier preventative measures. One potential approach is to consider earlier stages of AD in which individuals do not demonstrate clinical criteria for AD dementia but may demonstrate intermediate levels of AD neuropathology (Braak stage of II, III, or IV with moderate to frequent neuritic plaques) evaluated post-mortemly. This characterization suggests that these individuals may have developed clinical AD symptoms had they lived longer, or are able to stave off disease progression. Evaluating such individuals compared to those who had been clinically diagnosed and histopathologically confirmed to have AD will help to elucidate the neuronal processes that may drive disease progression or neuroprotection. To begin to elucidate this putative relationship, we expression profiled laser capture microdissected non-tangle bearing cortical neurons from six functionally discrete post-mortem brain regions. These regions, which have been found to display differential susceptibilities to AD pathologies, were collected from 10 non-demented individuals that demonstrate intermediate levels of AD neuropathology (NDAD). This analysis builds upon the global neuronal expression resource (Liang et al., 2008) we have established focusing on healthy elderly controls and patients who had been diagnosed with late onset AD, and aims to provide a catalog of expression signatures that characterizes transcriptomic changes across control, NDAD, and AD brains.
The six regions profiled have differential susceptibilities to AD pathologies and include the entorhinal cortex (EC), hippocampus (HIP), middle temporal gyrus (MTG), posterior cingulate cortex (PC), superior frontal gyrus (SFG), and primary visual cortex (VCX). Based on analysis consolidating statistically significant gene expression changes in NDAD patients compared to controls and AD patients compared to controls, we have identified significant common expression changes in both NDAD and AD brains in addition to expression signatures that account for regional changes across NDAD and AD brains. These findings provide insight into pathogenic mechanisms that may link the progression from NDAD to AD in different parts of the human brain and also identifies novel targets for developing improved diagnostics and preventative therapeutics against AD.
2. Methods
2.1. Tissue collection
Brain samples were collected at two Alzheimer’s Disease Centers (Washington University and Sun Health Research Institute) from clinically classified non-demented individuals who demonstrate intermediate levels of AD pathologies (6 males and 4 females) with a mean age of 86.6±5.3. Individuals were matched as closely as possible for their mean age at death and gender. Subjects in this group have a Braak stage of II to IV with a CERAD neuritic plaque density of moderate or frequent. Tissue collection from healthy elderly control and AD samples was previously described (Liang et al., 2008; Liang et al., 2007). Samples were collected (mean post-mortem interval (PMI) of 2.5 h) from six brain regions that are either histopathologically or metabolically relevant to AD—these include the EC (BA 28 and 34), SFG (BA 10 and 11), HIP, VCX (BA 17), MTG (BA 21 and 37), and the PC (BA 23 and 31). Following dissection, samples were frozen, sectioned (8 µm), and fixed on glass slides.
Brain sections were stained with a combination of Thioflavin-S (Sigma; Dallas, TX) and 1% Neutral Red (Fisher Scientific; Chicago, IL) and pyramidal neurons were identified by their characteristic size, shape, and location within the region of interest, while tangles were identified by the fluorescence of Thioflavin-S staining. In the EC, the large stellate neurons lacking Thioflavin-S staining were collected from layer II and pyramidal cells lacking Thioflavin-S staining were collected from CA1 of the HIP. The CA1 region was selected for study because this area is the most affected and earliest affected region in the hippocampus in terms of tangle formation, and this region has already been expression profiled in neurologically healthy elderly individuals. In all other regions, cortical layer III pyramidal neurons lacking Thioflavin-S staining were collected (for all collected neurons, cell bodies were extracted). For each individual, approximately five hundred histopathologically normal pyramidal neurons were collected from the EC, HIP, MTG, PC, SFG, and VCX using LCM with the Arcturus Veritas Automated Laser Capture Microdissection System (Mountain View, CA). Cells were collected onto Arcturus CapSure Macro-LCM Caps and extracted according to the manufacturer’s protocol. Total RNA was isolated from the cell lysate using the Arcturus PicoPure RNA Isolation Kit with DNase I treatment using Qiagen’s RNase-free DNase Set (Valencia, CA).
2.2. Expression profiling
Expression profiling, hybridization, and array scanning was performed as previously described (Liang et al., 2008; Liang et al., 2007). Isolated total RNA from each sample of ~500 neurons was double round amplified, cleaned, and biotin-labeled using Affymetrix’s GeneChip Two-Cycle Target Labeling kit (Santa Clara, CA) with a T7 promoter and Ambion’s MEGAscript T7 High Yield Transcription kit (Austin, TX) as per manufacturer’s protocol. Amplified and labeled cRNA was quantitated on a spectrophotometer and run on a 1% TAE gel to check for an evenly distributed range of transcript sizes. Twenty micrograms of cRNA was fragmented to approximately 35–200 bp by alkaline treatment (200 mM Tris-acetate, pH 8.2, 500 mM KOAc, 150 mM MgOAc) and run on a 1% TAE gel to verify fragmentation. Separate hybridization cocktails were made using 15µg of fragmented cRNA from each sample as per Affymetrix’s protocol.
Two hundred microliters (containing 10µg of fragmented cRNA) of each cocktail was separately hybridized to an Affymetrix Human Genome U133 Plus 2.0 Array for 16h at 45°C in the Hybridization Oven 640. The Affymetrix Human Genome Arrays measure the expression of over 47,000 transcripts and variants, including 38,500 characterized human genes. Arrays were washed on Affymetrix’s upgraded GeneChip Fluidics Station 450 using a primary streptavidin phycoerythrin (SAPE) stain, subsequent biotinylated antibody stain, and secondary SAPE stain. Arrays were scanned on Affymetrix’s GeneChip Scanner 3000 7G with AutoLoader. Scanned images obtained by the Affymetrix GeneChip Operating Software (GCOS) v1.2 were used to extract raw signal intensity values per probe set on the array. MAS5.0 was used to calculate detection calls (absent, marginal, or present) and to scale all raw chip data to 150 to normalize signal intensities for inter-array comparisons. Reports generated by GCOS were reviewed for quality control—we looked for at least 20% present calls, a maximum 3′/5′ GAPDH ratio of 30.5, and a scaling factor under 11. Thirteen arrays that failed to pass these standards were not included in further analyses.
2.3. Pyramidal cell quality control
To ensure neuronal cell purity in the samples, expression of GFAP, an astrocyte cell marker, was evaluated. Five samples that had GFAP expression greater than 2 S.D. from the mean were removed from statistical analyses.
2.4. Statistical analysis
Data for samples from neurologically healthy elderly controls and AD-afflicted individuals were generated in previous studies (Liang et al., 2008; Liang et al., 2007). Microarray data files of the normal samples are available on the Gene Expression Omnibus (GEO) site at http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE5281 (project accession#GSE5281) and regional analyses are posted at http://www.tgen.org/neurogenomics/data/). A summary of the mean ages, gender numbers, and number of samples used for statistical analyses (across all groups) are shown in Table 1. As a metric of quality, R-squared values were calculated and averaged for each region within each sample group—these values are posted on the supplementary data site at http://www.tgen.org/neurogenomics/data.
Table 1.
Sample group information
| Control | NDAD | AD | |
|---|---|---|---|
| Mean age | 79.8 ± 9.1 | 86.6 ± 5.3 | 79.9 ± 6.9 |
| Gender | M: 10; F: 4 | M: 6; F: 4 | M: 15; F: 18 |
| EC (n) | 13 | 6 | 10 |
| HIP (n) | 13 | 6 | 10 |
| MTG (n) | 12 | 6 | 16 |
| PC (n) | 13 | 5 | 9 |
| SFG (n) | 11 | 6 | 23 |
| VCX (n) | 12 | 5 | 19 |
Sample sizes for each sample group and brain region are shown (n).
Direct comparisons between brains of neurologically healthy and NDAD brains were performed between all brain regions to analyze expression differences. For each analysis, genes that did not demonstrate at least approximately 10% present calls for each region-specific comparison were removed using Genespring GX 7.3 Expression Analysis software (Agilent Technologies; Palo Alto, CA). A two-tailed unpaired t-test, assuming unequal variances (with multiple testing corrections using the Benjamini and Hochberg False Discovery Rate (FDR)), was applied to each comparison in Excel to locate genes that are statistically significant in differentiating expression between healthy and NDAD brains: for each analysis, genes that had a maximum P-value of 0.01 were collected and those genes whose average NDAD signal and average control signal were both below a threshold of 150 were removed. Fold change values were determined by calculating the ratio between the average scaled expression signal (for all samples) for a gene from the NDAD sample region and the average scaled expression signal for the same gene from the normal samples.
Using this approach we identified sets of genes that were specifically up or down-regulated between normal and NDAD brains for each of the six brain regions-of-study. Maps for genes showing the greatest statistically significant (P < 0.01, corrected) changes in the NDAD versus controls analysis were assembled. For the EC, a minimum (increased or decreased) fold change of 6 was applied, for the HIP a 5.4-fold change, for the MTG an 6.2-fold change, for the PC a 4-fold change, for the SFG a 4.8-fold change, and for the VCX a 2.9-fold change. Heat maps for each brain region were created using GeneCluster v2.0 with no gene or sample clustering applied and are located on a supplementary data site at http://www.tgen.org/neurogenomics/data.
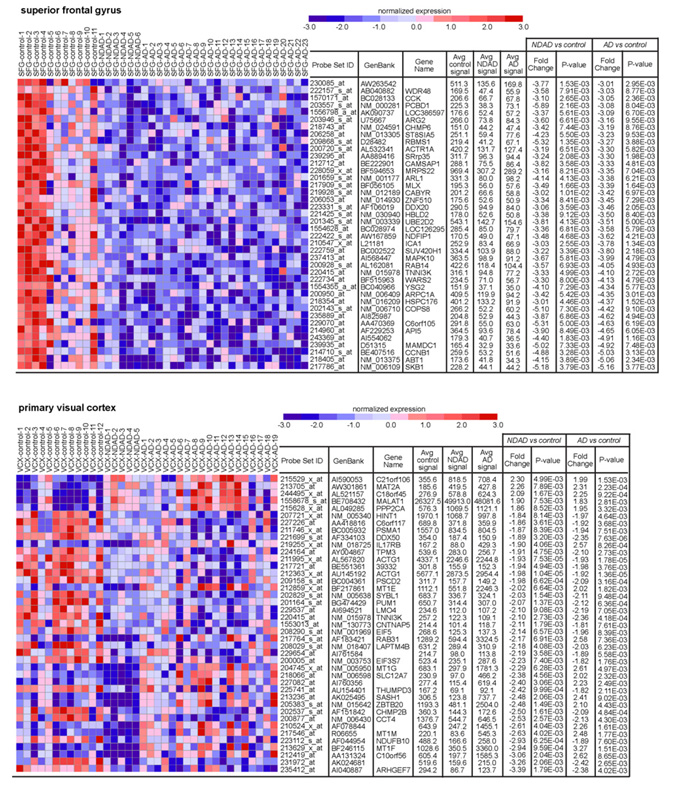
To find common statistically significant expression changes in AD and NDAD brains, each regional analysis (P < 0.01 with multiple testing corrections) for NDAD cases versus controls was compared against the parallel regional analysis for AD versus controls (Liang et al., 2008). Genes showing the greatest fold changes from the intersection lists were used to generate heat maps with GeneCluster v2.0 (Reich et al., 2004) (Fig. 1). For the EC, a minimum (increased or decreased) fold change of 5.0 was applied (for both the NDAD versus control analysis and AD versus control analysis), for the HIP a 4.3-fold change, for the MTG an 4.5-fold change, for the PC a 2.5-fold change, for the SFG a 3.0-fold change, and for the VCX a 1.8-fold change. To evaluate NDAD-specific alterations, genes showing statistically significant (P < 0.01 with corrections applied) expression changes only in the NDAD analyses, and not the AD analyses, were identified. Analyses are posted on the supplementary data site at http://www.tgen.org/neurogenomics/data/.
Fig. 1.
Common expression changes in NDAD and AD. Regional dendrograms of statistically significant genes (P< 0.01, corrected for multiple testing) demonstrating parallel expression changes are shown. Genes shown have the greatest changes in expression for both the NDAD vs. controls analysis and AD vs. controls analysis.
To identify expression patterns that account for the greatest amount of variance across disease states (healthy controls, NDAD, and AD) in each region, principle components analysis (PCA) was applied. PCA reduces a multi-dimensional data set to two dimensions by performing covariance analysis across the three sample groups. Genes showing at least ~10% present calls for each region were input into Genespring GX 7.3 for PCA analysis. For each region, three principle components were identified (the number of components is determined by the number of sample groups). The first component accounts for the greatest amount of variance across healthy control, NDAD, and AD brains, while the third component accounts for the least amount of variance. For each component, correlation values are measured for each gene in the input list—correlation values range from 0 to 1 with a value of 1 indicating that the gene has an identical expression signature to the specific component. Genes demonstrating a correlation value of 1 to component 1 for each region are listed in Table 5 and regional component graphs are shown in Fig. 2—the percentage of expression variance accounted for by each component is shown. Additional correlation data is listed on the supplementary data site.
Table 5.
Regional principal components analysis
| Brain region | Probe set ID | Genbank ID | Gene symbol | Brain region | Probe set ID | Genbank ID | Gene symbol |
|---|---|---|---|---|---|---|---|
| EC | 200766_at | NM 001909 | CTSD | MTG | 213347_x_at | AW132023 | RPS4X |
| EC | 204212_at | NM 005469 | ACOT8 | MTG | 232160_s_at | AL137262 | TNIP2 |
| EC | 227876_at | AW007189 | KIAA1688 | MTG | 225782_at | AW027333 | MSRB3 |
| EC | 218580_x_at | NM 017900 | AURKAIP1 | MTG | 212377_s_at | AU158495 | NOTCH2 |
| EC | 1558102_at | AK055438 | TM6SF1 | MTG | 228214_at | AW242286 | SOX6 |
| EC | 208977_x_at | BC004188 | TUBB2 | MTG | 226913_s_at | BF527050 | SOX8 |
| EC | 212085_at | AA916851 | SLC25A6 | MTG | 211962_s_at | BG250310 | ZFP36L1 |
| EC | 1555740_a_at | AF483549 | MRAP | MTG | 240648_at | AW104578 | LOC440728 |
| EC | 238528_at | AI361043 | UBR1 | MTG | 204906_at | BC002363 | RPS6KA2 |
| EC | 209914_s_at | AW149405 | NRXN1 | MTG | 212923_s_at | AK024828 | C6orf145 |
| EC | 204143_s_at | NM 017512 | ENOSF1 | PC | 226031_at | AA523733 | FLJ20097 |
| EC | 223319_at | AF272663 | GPHN | PC | 218877_s_at | NM 021820 | C6orf75 |
| EC | 210998_s_at | M77227 | HGF | PC | 206833_s_at | NM 001108 | ACYP2 |
| EC | 1567374_at | AJ011596 | PC | 238206_at | AI089319 | ||
| EC | 202192_s_at | NM 005890 | GAS7 | PC | 222975_s_at | AI423180 | CSDE1 |
| EC | 204120_s_at | NM 001123 | ADK | PC | 235195_at | BG109988 | FBXW2 |
| HIP | 217740_x_at | NM 000972 | RPL7A | PC | 240748_at | AI939338 | |
| HIP | 203865_s_at | NM 015833 | ADARB1 | PC | 208880_s_at | AB019219 | C20orf14 |
| HIP | 206491_s_at | NM 003827 | NAPA | PC | 201678_s_at | NM 020187 | DC12 |
| HIP | 206457_s_at | NM 000792 | DIO1 | PC | 217452_s_at | Y15014 | B3GALT2 |
| HIP | 227144_at | AA476916 | C22orf9 | PC | 222627_at | AK002205 | VPS54 |
| HIP | 222505_at | BF510801 | LMBR1 | PC | 53071_s_at | AI885411 | FLJ22222 |
| HIP | 201386_s_at | AF279891 | DHX15 | PC | 218125_s_at | NM 018246 | CCDC25 |
| HIP | 224606_at | BG250721 | KLF6 | PC | 213535_s_at | AA910614 | UBE2I |
| HIP | 217792_at | NM 014426 | SNX5 | PC | 222459_at | BG109865 | C1orf108 |
| HIP | 200822_x_at | NM 000365 | TPI1 | PC | 223093_at | T99215 | ANKH |
| HIP | 204701_s_at | NM 004809 | STOML1 | PC | 219248_at | NM 025264 | THUMPD2 |
| HIP | 203522_at | NM 005125 | CCS | PC | 226650_at | AI984061 | ZFAND2A |
| HIP | 225077_at | AA890703 | LOC283680 | PC | 225018_at | BF512188 | SPIRE1 |
| HIP | 223313_s_at | BC001207 | MAGED4 | PC | 214257_s_at | AA890010 | SEC22L1 |
| HIP | 202282_at | NM 004493 | HADH2 | PC | 218771_at | NM 018216 | PANK4 |
| HIP | 1568698_at | BC042563 | PC | 208826_x_at | U27143 | HINT1 | |
| HIP | 203081_at | NM 020248 | CTNNBIP1 | PC | 227797_x_at | AI652464 | DJ122O8.2 |
| HIP | 201155_s_at | NM 014874 | MFN2 | PC | 215093_at | U82671 | NSDHL |
| HIP | 209178_at | AF038391 | DHX38 | PC | 219288_at | NM 020685 | C3orf14 |
| HIP | 201956_s_at | NM 014236 | GNPAT | PC | 207573_x_at | NM 006476 | ATP5L |
| HIP | 200001_at | NM 001749 | CAPNS1 | SFG | 202936_s_at | NM 000346 | SOX9 |
| HIP | 234813_at | AB051477 | MGC3040 | SFG | 208623_s_at | J05021 | VIL2 |
| HIP | 201144_s_at | NM 004094 | EIF2S1 | SFG | 205608_s_at | U83508 | ANGPT1 |
| HIP | 222443_s_at | AF182415 | RBM8A | SFG | 224565_at | BE675516 | TncRNA |
| HIP | 227880_s_at | AW300965 | FAM11A | VCX | 1555876_at | BG290185 | |
| HIP | 216032_s_at | AF091085 | C20orf47 | VCX | 237931_at | AI732263 | |
| HIP | 200017_at | NM 002954 | RPS27A | VCX | 211384_s_at | D50855 | CASR |
| HIP | 1553101_a_at | NM 017758 | FLJ20308 | VCX | 210640_s_at | U63917 | GPR30 |
Genes correlating with component 1 (correlation = 1) for each regional analysis are listed.
Fig. 2.
Regional principal components analysis. Three principal components are shown for each region across healthy controls, NDAD brains, and AD brains (x-axis). The y-axis represents the logged normalized intensity value. The percentage of expression variance (across controls, NDAD, and AD brains) that each component accounts for is listed.
2.5. Data posting
MIAME-compliant microarray data files are located on the Gene Expression Omnibus (GEO) site at http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE5281 (project accession#GSE5281). Fold change and P-value data for each of the six regions across healthy control, NDAD, and AD brains are available online at: http://www.tgen.org/neurogenomics/data/. Posted lists show region-specific P-values and fold changes, and expression signals for genes that have at least approximately 10% present calls across regional samples with a maximum P-value of 0.01 with multiple testing corrections applied (no fold change thresholds have been applied on these lists).
2.6. RT-PCR validation of neuron-specific candidate genes
Total RNA was isolated from cortical grey matter from unprofiled MTG (controls: n = 9, NDAD cases: n = 8, AD cases: n = 9) and PC (controls: n = 8, NDAD cases: n = 8, AD cases: n = 11) frozen tissue using the RNAspin Mini kit (GE Healthcare Life Sciences; Piscataway, NJ) using manufacturers protocol modified by increasing initial volume of buffer RA1 to 500 µl to prevent subsequent column blockage. RNA quality was assessed on an Agilent 2100 Bioanalyzer (Santa Clara, CA) using Agilent RNA Nanochips. RIN numbers of 6.5 (range 6.5–9.0) and above were considered sufficient for this analysis. cDNA was generated using the Superscript First Strand Synthesis kit (Invitrogen; Carlsbad, CA) using 1 µg of total RNA in a 40 µl reaction. Quantitative RT-PCR was performed using Taqman primer/probe sets (Applied Biosystems; Foster City, CA) to amplify the following neuron-specific gene transcripts; MAP1B (microtubule-associated protein 1B; Hs00195485_m1), GRIA1 (glutamate receptor, ionotropic, AMPA 1; Hs00181348_m1) and GRIA3 (glutamate receptor, ionotropic, AMPA 3; Hs00241485_m1). Five assays for non-neuronal mRNA transcripts were performed, of which the first four are AD-related; APOE (apolipoprotein E; Hs0003037354_mH), APP (amyloid precursor protein; Hs00169098_m1), BACE1 (beta-site APP-cleaving enzyme 1; Hs00201573_m1), COX5B (cytochrome c oxidase subunit Vb; Hs00426948_m1) and MAP4 (microtubule-associated protein 4; Hs01104794_m1). Levels of β-Gluconuridase (GUSB 4333767F) mRNA were used for normalization of samples; this gene transcript did not show significant expression changes between AD and ND in the gene array analysis, and has been successfully employed for this purpose previously (Barrachina et al., 2006; Kuwano et al., 2006). qRT-PCR reactions were performed in 30 µl reactions using Taqman Gene Expression Master Mix (Applied Biosys-tems) according to manufacturers protocol on a BioRad iCycler IQ qPCR system (Hercules, CA). Threshold values were calculated using the maximum curvature approach. Ct values were used to calculate fold changes using the 2−ΔΔCt method (Livak and Schmittgen, 2001). Significance of observed changes was ascertained using the Student’s t-test.
3. Results and discussion
In this study, we gene expression profiled non-tangle bearing cortical neurons from the post-mortem brains of non-demented individuals who have been histopathologically confirmed to demonstrate intermediate pathologies associated with AD through Braak and CERAD staging. This study completes a high-quality expression data set that we have established to evaluate neuronal gene expression changes that characterize healthy elderly controls, non-demented individuals with intermediate AD neuropathology, and AD patients in different areas of the brain that are relevant to AD. By defining neuronal expression levels across healthy elderly individuals, NDAD individuals, and those diagnosed with late-onset AD, these findings provide insight into disease progression and the processes that may drive neurodegeneration or neuropro tection.
3.1. Common expression changes in NDAD and AD brains
In order to identify common expression changes in NDAD and AD brains, we compared our data with our previous study in which we similarly profiled neurons from the brains of healthy elderly controls and individuals that have been clinically and histopathologically confirmed to have AD (Liang et al., 2008). Comparison of expression changes in NDAD versus control brains and AD versus control brains led to the identification of a significant overlap of genes demonstrating statistically significant (P < 0.01, corrected for multiple comparisons) expression changes within each regional analysis. In the EC, 1887 genes showed significant changes in both NDAD and AD brains compared to controls, 1892 genes demonstrated changes in the HIP of both NDAD and AD brains, 2755 genes in the MTG, 503 genes in the PC, 226 genes in the SFG, and 178 genes in the VCX. Interestingly, the SFG, a region that demonstrates metabolic changes associated with normal aging (Angelie et al., 2001; Convit et al., 2001; Ivancevic et al., 2000; Loessner et al., 1995; Moeller et al., 1996), and the VCX, a region found to be relatively spared from AD pathologies (Metsaars et al., 2003), showed the least amount of transcriptomic changes across healthy elderly, NDAD, and AD brains, while the greatest changes were found in brain regions that have increased susceptibilities to AD pathologies including neurofibrillary tangles (NFTs) (Bobinski et al., 1999; Bouras et al., 1994; Braak and Braak, 1992; de Leon et al., 1989; Du et al., 2003; Fox et al., 1996; Frisoni et al., 1999; Hyman et al., 1984) in the EC and HIP, and amyloid plaques (Braak and Braak, 1991; Mirra et al., 1991; Thal et al., 2002) and metabolic deficits (Blesa et al., 1996; Jack et al., 1998; Mielke et al., 1994, 1998; Small et al., 2000) in the MTG and PC. Dendrograms listing genes demonstrating the greatest expression changes in both NDAD and AD brains compared to controls for each region are shown in Fig. 1.
Due to the breadth of the data, we focused our attention on genes that have roles in mechanisms that have been previously implicated as being associated with AD to assess if these pathogenic pathways may be enacted in NDAD brains. These mechanisms include pathways leading to formation of NFTs and amyloid plaques, ubiquitin–proteasomal pathways, and pathways surrounding synaptic degeneration.
3.1.1. Common expression changes in NDAD and AD brains: tangle and plaque related pathways
With regards to pathological markers of AD, NFTs form as a result of intraneuronal aggregation of tau, while extracellular plaques form as a result of the aggregation of insoluble 40–42 amino acid long Abeta proteins. In the EC and MTG, decreased expression was identified for microtubule-associated protein tau (MAPT) across NDAD and AD brains (Table 2), while multiple probes in the HIP demonstrated both increased and decreased expression. Past studies have identified isoform specific (3-repeat and 4-repeat) tau expression in the temporal region (Conrad et al., 2007) and cerebellar cortex (Boutajangout et al., 2004), and in cholinergic basal forebrain and hippocampal CA1 neurons of AD brains (Ginsberg et al., 2006). However, the Affymetrix Human Genome U133 Plus 2.0 array does not specifically distinguish between 3-repeat and 4-repeat tau isoforms so that isoform-specific expression is not considered in this study. Even so, because of the presence of multiple probes targeted against MAPT, differences in expression changes between probes suggest that isoform-specific expression is present. In the HIP, 3 MAPT probes demonstrated significant opposite changes in expression levels in NDAD brains (Table 2). While 206401_s_at and 203928_x_at target the entire length of MAPT and demonstrate increased expression, 225379_at targets the 3′ untranslated region (UTR) and demonstrates decreased expression. Because 206401_s_at and 203928_x_at cover the entire MAPT gene, including alternatively spliced exons, their changes in expression may represent differential expression of different isoforms. Because 225379_at targets the 3′ UTR, this probe evaluates all variants and thus likely represents the net change in expression of MAPT. While isoform-specific expression changes have been identified in AD brains, past studies have not found changes in MAPT expression in post-mortem brain tissue (Goedert et al., 1989) and single cells in AD (Hemby et al., 2003). Another study evaluated gene expression differences in tangle bearing hippocampal CA1 neurons from AD brains compared to non-tangle bearing CA1 neurons in both AD brains and healthy brains and did not detect any expression changes of the 3-repeat and 4-repeat isoforms (Ginsberg et al., 2000). However, in this particular study, gene expression of non-tangle bearing neurons from AD and control brains defined the baseline of expression so that disease specific changes in healthy neurons are not evaluated. Despite these findings, we identified changes in MAPT expression between healthy neurons in NDAD brains and healthy neurons in control brains (to parallel greater expression changes in healthy neurons in AD brains compared to that in control brains). The primarily decreased net expression of MAPT across control, NDAD, and AD brains found here may demonstrate cellular efforts to inhibit aggregation of tau into NFTs at a timepoint prior to onset of measureable cognitive deficits.
Table 2.
Common expression changes in NDAD and AD brains: tangle and plaque pathway factors
| Probe set ID | Genbank ID | Gene symbol | Brain region | NDAD vs. control |
AD vs. control |
||
|---|---|---|---|---|---|---|---|
| Fold | P-value* | Fold | P-value* | ||||
| 203929_s_at | AI056359 | MAPT | EC | −2.32 | 2.41E−05 | −1.46 | 6.76E−03 |
| 206401_s_at | J03778 | MAPT | HIP | 2.73 | 7.86E−03 | 1.85 | 1.71E−02 |
| 203928_ x_at | AI870749 | MAPT | HIP | 2.48 | 5.15E−04 | 2.23 | 6.84E−04 |
| 225379_at | AA199717 | MAPT | HIP | −2.40 | 6.12E−05 | −2.15 | 1.35E−04 |
| 203930_s_at | NM 016835 | MAPT | MTG | −1.90 | 2.90E−02 | −1.99 | 1.81E−02 |
| 225379_at | AA199717 | MAPT | MTG | −2.00 | 7.44E−03 | −2.21 | 3.29E−03 |
| 226653_at | AB040910 | MARK1 | MTG | 2.51 | 2.76E−03 | 1.49 | 8.36E−03 |
| 239166_at | R98192 | MARK3 | EC | −3.75 | 1.47E−03 | −1.10 | 3.90E+00 |
| 202568_s_at | AI745639 | MARK3 | HIP | −2.08 | 2.24E−05 | −2.37 | 5.33E−06 |
| 202568_s_at | AI745639 | MARK3 | MTG | −1.61 | 2.76E−03 | −1.59 | 8.89E−04 |
| 55065_at | AL120554 | MARK4 | EC | −4.32 | 1.51E−05 | −2.39 | 2.44E−04 |
| 221560_at | AB049127 | MARK4 | EC | −5.07 | 1.44E−05 | −2.52 | 2.56E−04 |
| 204247_s_at | NM 004935 | CDK5 | EC | −2.49 | 1.21E−03 | −3.87 | 6.51E−06 |
| 204247_s_at | NM 004935 | CDK5 | HIP | −2.03 | 2.43E−03 | −1.91 | 4.62E−03 |
| 204247_s_at | NM 004935 | CDK5 | MTG | −2.49 | 2.95E−03 | −4.33 | 3.62E−04 |
| 209018_s_at | BF432478 | PINK1 | EC | −2.28 | 6.85E−05 | −1.89 | 3.60E−04 |
| 209019_s_at | AF316873 | PINK1 | HIP | −2.61 | 5.56E−04 | −2.23 | 6.52E−04 |
| 213922_at | AW294686 | TTBK2 | MTG | 4.66 | 8.02E−05 | 3.53 | 3.09E−06 |
| 213922_at | AW294686 | TTBK2 | HIP | 3.81 | 3.38E−04 | 3.52 | 1.17E−07 |
| 231086_at | BF939127 | BACE1 | EC | −1.98 | 4.40E−04 | −1.04 | 6.53E+00 |
| 222463_s_at | AF190725 | BACE1 | EC | −3.28 | 1.70E−04 | −1.66 | 1.49E−02 |
| 222462_s_at | AI653425 | BACE1 | EC | −3.06 | 1.94E−05 | −1.77 | 1.36E−03 |
| 222462_s_at | AI653425 | BACE1 | HIP | −1.47 | 6.26E−03 | −1.17 | 4.84E−01 |
| 217904_s_at | NM 012104 | BACE1 | HIP | −1.68 | 4.45E−03 | −1.93 | 3.77E−05 |
| 217904_s_at | NM 012104 | BACE1 | MTG | −1.75 | 9.56E−06 | −1.32 | 2.58E−03 |
| 203460_s_at | NM 007318 | PSEN1 | HIP | −1.92 | 5.33E−03 | −1.64 | 3.44E−02 |
| 226577_at | N49844 | PSEN1 | MTG | −2.06 | 3.95E−03 | −1.53 | 1.91E−02 |
| 203460_s_at | NM 007318 | PSEN1 | PC | −1.80 | 5.42E−03 | −2.30 | 4.05E−04 |
| 211373_s_at | U34349 | PSEN2 | MTG | −1.50 | 4.88E−03 | −1.89 | 4.25E−05 |
| 200602_at | NM 000484 | APP | HIP | 1.89 | 2.13E−04 | 2.14 | 3.55E−03 |
| 214953_s_at | X06989 | APP | MTG | 2.37 | 1.35E−03 | 1.12 | 1.44E+00 |
| 200602_at | NM 000484 | APP | MTG | 5.11 | 6.71E−04 | 3.09 | 8.20E−07 |
| 211277_x_at | BC004369 | APP | PC | 1.69 | 4.54E−04 | 3.01 | 2.05E−04 |
| 200602_at | NM 000484 | APP | PC | 2.11 | 1.87E−04 | 1.93 | 8.38E−04 |
Corrected P values are shown.
Cellular efforts to inhibit NFT formation may also be demonstrated by decreased expression of kinases that can phosphorylate tau—these include MAP/microtubule affinity-regulating kinases (MARK3, MARK4), cyclin-dependent kinase 5 (CDK5), PTEN-induced putative kinase 1 (PINK1), and tau tubulin kinase 2 (TTBK2) (Kitano-Takahashi et al., 2007) (Table 2). Along with decreases, increased expression for putative tau kinases were also identified (Table 2). The decreased expression of tau in certain regions along with altered expression of kinases that may phosphorylate tau suggests that neurons may be initiating responses to lessen or inhibit tangle formation at stages prior to detectable disease onset.
Evaluation of relevant factors in plaque formation pathways also led to the identification of altered expression of beta-secretase (BACE1), presenilins 1 and 2 (PSEN1, PSEN2), and APP (Table 2). Decreased expression was found for BACE1, the enzyme that makes the initial cleave in APP during sequential processing to generate Abeta proteins (Selkoe, 2001; Selkoe and Schenk, 2003; Sinha et al., 1999; Vassar et al., 1999; Yan et al., 1999), in NDAD and AD brains (compared to controls). In contrast, another study focusing on the temporal neocortex identified an absence of BACE expression changes between AD and control brains (Matsui et al., 2007)—this difference may be derived from the earlier degenerative timepoint considered in this study as well as the cellular specificity of this study. Furthermore, presenilins 1 and 2, components of the gamma secretase complex, showed decreased expression (Table 2). In contrast, in AD brains, PSEN1 demonstrated increased expression in the temporal neocortex (Matsui et al., 2007). Lastly, APP demonstrated increased expression (Table 2) to possibly correlate with the moderate to frequent CERAD ratings assigned for the profiled NDAD and AD brains. However, other studies have shown varied results regarding APP mRNA levels in AD brains. While one study identified increased levels of APP isoforms containing a Kunitz-type serine protease inhibitor domain in the cerebral cortices of AD brains (Preece et al., 2004), another study also identified this trend but did not find changes in overall levels of APP mRNA in the temporal neo-cortices of AD and control brains (Matsui et al., 2007). In contrast, Johnston et al. (1996) identified reductions in total APP mRNA levels in the mid-temporal cortices of AD brains. Although our APP expression findings contrast with these previous studies (and although we were unable to differentiate between APP mRNA isoforms on the Affymetrix array), it has been shown that APP expression differs greatly across subjects and thus may contribute to the differences found (Harrison et al., 1996; Oyama et al., 1991, 1993; Robinson et al., 1994). Additionally, as results from APP expression studies may differ, we considered both NDAD and AD cases and focused on neuron-specific regional expression to differentiate the findings presented here from whole tissue studies. The changes identified here suggest that common pathogenic or neuroprotective mechanisms are enacted in both NDAD and AD brains with regards to plaque formation. It is also particularly interesting to note the absence of significant expression alterations of NFT and plaque formation elements in the SFG and VCX, regions that are more spared from the hallmark AD pathologies.
3.1.2. Common expression changes in NDAD and AD brains: ubiquitin–proteasomal pathways
The toxicity of protein aggregates in the form of NFTs and plaques may also be related to changes or deficits in the ubiquitin–proteasomal pathway, a primary avenue for protein degradation. Across NDAD and AD brains and across all profiled regions, elements in the ubiquitin–proteasomal pathway showed both up-regulated and down-regulated expression with the lowest number of affected elements in the SFG and VCX. Altered expression was identified for ubiquitins (UBB, UBC), ubiquitin-conjugating enzymes (UBE1C, UBE1DC1, UBE2D2, UBE2D3, UBE2H, UBE2I, UBE2J1, UBE2L3, UBE2R2), ubiquitin specific peptidases (USP1, USP2, USP4, USP6-8, USP10, USP11, USP16, USP21, USP22, USP31, USP33, USP34, USP36, USP37, USP42, USP46-48, USP50, USP53, USP54), and proteasomal sub-units (PSMA1, PSMA5-7, PSMB1-7, PSMB10, PSMC1-3, PSMC5, PSMD1, PSMD4, PSMD11). The EC, SFG, and VCX showed solely decreased expression in NDAD and AD brains, while the HIP, MTG, and PC showed both increased and decreased expression for different subunits. Such dysregulated expression of ubiquitin–proteasomal pathway components indicates that this pathway is altered in NDAD and AD brains and may represent neuroprotective or pathogenic efforts (particularly with regards to the formation of plaques and tangles) that may begin at NDAD stages and potentially progress to AD.
3.1.3. Common expression changes in NDAD and AD brains: loss of synaptic connections
Another characteristic marker of AD is brain atrophy and loss of synaptic connections. To assess relevant expression changes that may affect such degeneration, we evaluated genes encoding synaptic proteins. These proteins include synaptosomal-associated protein, 25kDa (SNAP25), syntaxins (STX), synapsins (SYN), synap-tobrevins (vesicle-associated membrane protein; VAMP), synaptogyrins (SYNGR), and synaptotagmins (SYT) (refer to Table 3). SNAP-25, STX, and VAMP make up the SNARE complex, whose assembly allows for synaptic exocytosis (Sollner et al., 1993) and thus influences inter-neuronal communications. SYNs are phosphoproteins that help to regulate neurotransmitter release (Hackett et al., 1990; Hilfiker et al., 1998; Jovanovic et al., 2001, 2000; Li et al., 1995; Llinas et al., 1985, 1991; Rosahl et al., 1995) and also may have roles in establishing synaptic contacts. Finally, SYNGRs are suggested to be involved in vesicle exocytosis and membrane trafficking (Belizaire et al., 2004; Janz et al., 1999; Sugita et al., 1999), while SYTs are synaptic vesicle proteins that act as calcium sensors to support fast exocytosis and neurotransmitter release (Saraswati et al., 2007). Both up-regulated and down-regulated expression was identified for these synaptic factors (Table 3) to indicate drastic changes in demand for these proteins. In addition, increased expression of SYNs has been found to be correlated with establishing synaptic contacts (Ferreira et al., 2000; Lohmann et al., 1978; Melloni and DeGennaro, 1994) to suggest that the increased and decreased expression seen in this study may be correlated with a loss and establishment of synaptic contacts in NDAD brains. Such changes in contacts may ultimately lead to deficits in synaptic functions if contacts are not properly re-established.
Table 3.
Common expression changes in NDAD and AD brains: synaptic factors
| Probe set ID | Genbank ID | Gene symbol | Brain region | NDAD vs. control |
AD vs. control |
||
|---|---|---|---|---|---|---|---|
| Fold | P-value* | Fold | P-value* | ||||
| 1556629_a_at | AI806346 | SNAP25 | EC | −3.26 | 1.46E−06 | −2.52 | 7.50E−06 |
| 1556629_a_at | AI806346 | SNAP25 | HIP | 2.15 | 6.30E−03 | 2.15 | 8.46E−05 |
| 202507_s_at | L19760 | SNAP25 | MTG | −4.07 | 1.02E−03 | −14.27 | 2.04E−04 |
| 202508_s_at | NM 003081 | SNAP25 | VCX | 1.90 | 7.75E−04 | −1.28 | 3.33E−01 |
| 204729_s_at | NM 004603 | STX1A | HIP | −1.60 | 5.85E−03 | −1.72 | 5.18E−03 |
| 204729_s_at | NM 004603 | STX1A | MTG | −1.69 | 5.35E−03 | −2.45 | 9.18E−05 |
| 209238_at | BE966922 | STX3A | HIP | −1.54 | 3.66E−03 | −1.76 | 1.62E−03 |
| 230691_at | R85929 | STX1B2 | EC | −4.95 | 4.85E−07 | −3.49 | 1.49E−06 |
| 212799_at | BE217875 | STX6 | MTG | 1.60 | 6.86E−03 | 1.02 | 1.83E+01 |
| 204690_at | NM 004853 | STX8 | MTG | −3.06 | 4.38E−04 | −3.10 | 4.36E−04 |
| 204690_at | NM 004853 | STX8 | HIP | −2.12 | 6.93E−04 | −2.99 | 1.59E−05 |
| 212625_at | NM 003765 | STX10 | EC | −2.24 | 1.90E−04 | 1.09 | 2.15E+00 |
| 212625_at | NM 003765 | STX10 | MTG | −2.09 | 4.99E−04 | −1.33 | 1.11E−01 |
| 221499_s_at | AK026970 | STX16 | VCX | −1.79 | 1.01E−02 | 1.04 | 6.87E+00 |
| 222708_s_at | AW014619 | STX17 | VCX | −2.20 | 8.86E−03 | −1.55 | 1.47E−03 |
| 228091_at | AI800609 | STX17 | HIP | 1.50 | 3.34E−03 | 1.21 | 3.74E−01 |
| 228091_at | AI800609 | STX17 | MTG | 1.61 | 2.03E−03 | 1.20 | 4.33E−01 |
| 222708_s_at | AW014619 | STX17 | PC | −2.45 | 1.74E−04 | −1.40 | 1.61E−01 |
| 222708_s_at | AW014619 | STX17 | SFG | −3.11 | 3.94E−03 | −2.30 | 1.14E−02 |
| 218763_at | NM 016930 | STX18 | HIP | −2.18 | 2.51E−05 | −2.34 | 2.20E−05 |
| 218763_at | NM 016930 | STX18 | MTG | −2.65 | 2.02E−05 | −1.67 | 1.99E−04 |
| 218763_at | NM 016930 | STX18 | PC | −1.46 | 8.63E−03 | −1.23 | 9.62E−01 |
| 221914_at | H19843 | SYN1 | EC | −7.49 | 1.85E−05 | −4.92 | 4.04E−05 |
| 210247_at | AW139618 | SYN2 | EC | −3.11 | 2.34E−04 | −3.31 | 1.79E−04 |
| 206322_at | NM 003490 | SYN3 | EC | −2.52 | 7.56E−05 | −3.35 | 4.12E−06 |
| 221914_at | H19843 | SYN1 | HIP | −2.12 | 2.71E−04 | −1.40 | 7.55E−02 |
| 221914_at | H19843 | SYN1 | MTG | −1.63 | 8.53E−03 | −2.48 | 1.41E−04 |
| 221914_at | H19843 | SYN1 | PC | −1.77 | 3.77E−03 | −1.35 | 2.55E−01 |
| 229039_at | BE220333 | SYN2 | HIP | −2.01 | 5.17E−03 | −3.09 | 1.59E−04 |
| 210315_at | AF077737 | SYN2 | HIP | 1.84 | 4.85E−03 | 1.80 | 1.10E−02 |
| 206322_at | NM 003490 | SYN3 | HIP | 5.74 | 8.18E−03 | 6.36 | 2.38E−03 |
| 206322_at | NM 003490 | SYN3 | MTG | 3.37 | 5.28E−03 | 2.04 | 7.24E−02 |
| 204287_at | NM 004711 | SYNGR1 | EC | −1.95 | 2.95E−04 | −2.65 | 2.16E−05 |
| 205691_at | NM 004209 | SYNGR3 | EC | −2.37 | 2.06E−03 | −4.73 | 1.15E−04 |
| 203999_at | AV731490 | SYT1 | MTG | −1.54 | 2.47E−03 | −3.93 | 9.17E−10 |
| 223901_at | AL136594 | SYT3 | EC | −2.04 | 8.15E−04 | −2.40 | 1.50E−04 |
| 223901_at | AL136594 | SYT3 | MTG | −2.01 | 3.08E−03 | −1.94 | 2.47E−03 |
| 206162_x_at | NM 003180 | SYT5 | EC | −3.42 | 9.06E−05 | −2.70 | 2.80E−04 |
| 244227_at | AI863338 | SYT6 | EC | −2.83 | 1.47E−03 | 1.75 | 6.87E−02 |
| 244227_at | AI863338 | SYT6 | SFG | −2.49 | 2.84E−03 | −1.06 | 1.13E+01 |
| 232677_at | AU146128 | SYT11 | EC | −4.22 | 3.62E−04 | −1.78 | 2.27E−02 |
| 209198_s_at | BC004291 | SYT11 | VCX | 1.24 | 8.14E−03 | 1.05 | 4.00E+00 |
| 228072_at | AK024280 | SYT12 | EC | −3.53 | 2.73E−04 | −1.82 | 1.07E−02 |
| 226086_at | AB037848 | SYT13 | HIP | −2.77 | 1.87E−04 | −2.28 | 1.64E−04 |
| 205613_at | NM 016524 | SYT17 | EC | −3.87 | 6.19E−04 | −2.24 | 5.66E−03 |
| 205613_at | NM 016524 | SYT17 | MTG | −1.94 | 7.35E−03 | 1.09 | 1.86E+00 |
| 205613_at | NM 016524 | SYT17 | VCX | −2.66 | 4.87E−04 | 1.67 | 6.60E−03 |
| 213326_at | AU150319 | VAMP1 | VCX | 1.52 | 2.61E−04 | −1.38 | 8.47E−02 |
| 201556_s_at | BC002737 | VAMP2 | EC | −4.27 | 2.82E−05 | −1.63 | 1.62E−02 |
| 214792_x_at | AI955119 | VAMP2 | EC | −6.32 | 1.18E−05 | −1.65 | 3.07E−02 |
| 201556_s_at | BC002737 | VAMP2 | SFG | −2.94 | 8.11E−03 | −3.78 | 4.04E−03 |
| 201336_at | BC003570 | VAMP3 | HIP | −2.02 | 1.18E−03 | −1.36 | 2.88E−01 |
| 201336_at | BC003570 | VAMP3 | MTG | −2.21 | 1.06E−03 | 1.12 | 1.82E+00 |
| 201336_at | BC003570 | VAMP3 | PC | −1.76 | 7.18E−03 | −1.25 | 1.14E+00 |
| 213480_at | AF052100 | VAMP4 | MTG | 1.96 | 1.93E−04 | 1.28 | 1.39E−01 |
| 213480_at | AF052100 | VAMP4 | VCX | 1.54 | 2.40E−03 | −1.40 | 3.66E−02 |
Corrected P values are shown.
3.2. Unique expression changes in NDAD brains
In addition to significant common expression changes in NDAD brains and AD brains compared to controls, unique statistically significant (P < 0.01, corrected) expression changes in NDAD brains (and absent or not significant in AD brains) were also identified. Pathway analysis using MetaCore GeneGo identified processes that contain these uniquely expressed genes. Data for these genes and all processes for each regional analysis are located on the supplementary data site. Interestingly, learning and/or memory processes were found to be affected in the EC, HIP, MTG, PC, and SFG of NDAD brains. Down-regulated genes from these processes include APOE, CHST10 (carbohydrate sulfotransferase 10), CTNND2 (catenin, delta 2), EGR1 (early growth response 1), ABI2 (Abl interactor 2), FYN (FYN oncogene), GM2A (GM2 ganglioside activator), PRKCB1 (protein kinase C, beta 1), PTN (pleiotrophin), S100B (S100 calcium binding protein, beta), and SHC3 (SHC transforming protein 3) (refer to Table 4). Up-regulated genes from learning and/or memory processes include ABI2, EFNB2 (ephrin-B2), MAPT, GRM7 (glutamate receptor, metabotropic 7), LAMB1 (laminin, beta 1), PRKACB (protein kinase, cAMP-dependent, catalytic, beta), and VDAC3 (voltage-dependent anion channel 3). While the NDAD patients did not meet clinical criteria for dementia, these transcriptomic changes precede stages during which dementia symptoms are detectable and may represent compensatory efforts targeted against onset of cognitive deficits. These learning/memory genes may thus represent novel factors to consider in developing earlier diagnostics and treatments.
Table 4.
Unique expression changes in NDAD brains
| Probe set ID | Genbank ID | Gene symbol | Brain region | NDAD vs. control |
|
|---|---|---|---|---|---|
| Fold | P-value* | ||||
| 225112_at | AA058571 | ABI2 | HIP | 1.33 | 5.12E−03 |
| 225098_at | BF245400 | ABI2 | HIP | 2.27 | 2.41E−04 |
| 225098_at | BF245400 | ABI2 | MTG | 1.70 | 3.66E−05 |
| 203381_s_at | N33009 | APOE | EC | −3.45 | 5.18E−03 |
| 203382_s_at | NM 000041 | APOE | EC | −4.35 | 6.54E−04 |
| 212884_x_at | AI358867 | APOE | EC | −5.01 | 1.46E−04 |
| 203382_s_at | NM 000041 | APOE | HIP | −2.40 | 3.82E−03 |
| 212884_x_at | AI358867 | APOE | HIP | −2.26 | 1.23E−03 |
| 203381_s_at | N33009 | APOE | HIP | −5.05 | 5.36E−04 |
| 203381_s_at | N33009 | APOE | MTG | −2.75 | 9.06E−04 |
| 203382_s_at | NM 000041 | APOE | MTG | −3.00 | 1.44E−04 |
| 212884_x_at | AI358867 | APOE | MTG | −2.58 | 2.07E−05 |
| 212884_x_at | AI358867 | APOE | PC | −2.02 | 2.40E−03 |
| 203381_s_at | N33009 | APOE | PC | −2.47 | 1.52E−03 |
| 204065_at | NM 004854 | CHST10 | HIP | −1.95 | 5.45E−03 |
| 209618_at | U96136 | CTNND2 | HIP | −1.71 | 2.92E−03 |
| 209618_at | U96136 | CTNND2 | MTG | −1.64 | 5.90E−03 |
| 202668_at | BF001670 | EFNB2 | HIP | 1.97 | 1.86E−03 |
| 227404_s_at | AI459194 | EGR1 | EC | −2.07 | 1.04E−03 |
| 201693_s_at | AV733950 | EGR1 | EC | −3.14 | 1.60E−04 |
| 227404_s_at | AI459194 | EGR1 | PC | −1.99 | 2.52E−03 |
| 216033_s_at | S74774 | FYN | EC | −3.26 | 6.07E−03 |
| 210105_s_at | M14333 | FYN | EC | −3.04 | 4.41E−07 |
| 216033_s_at | S74774 | FYN | HIP | −2.73 | 6.50E−03 |
| 216033_s_at | S74774 | FYN | MTG | −2.85 | 2.20E−03 |
| 212737_at | AL513583 | GM2A | EC | −2.43 | 5.07E−03 |
| 212737_at | AL513583 | GM2A | MTG | −1.69 | 7.63E−03 |
| 35820_at | M76477 | GM2A | MTG | −1.98 | 5.17E−03 |
| 212737_at | AL513583 | GM2A | PC | −1.78 | 3.97E−03 |
| 207548_at | NM 000844 | GRM7 | MTG | 1.79 | 8.18E−05 |
| 236437_at | N30158 | LAMB1 | MTG | 2.53 | 1.82E−04 |
| 206401_s_at | J03778 | MAPT | HIP | 2.73 | 7.86E−03 |
| 203928_x_at | AI870749 | MAPT | HIP | 2.48 | 5.15E−04 |
| 225379_at | AA199717 | MAPT | HIP | −2.40 | 6.12E−05 |
| 225379_at | AA199717 | MAPT | MTG | −2.00 | 7.44E−03 |
| 203928_x_at | AI870749 | MAPT | MTG | 2.16 | 8.61E−04 |
| 203928_x_at | AI870749 | MAPT | PC | 1.90 | 4.89E−03 |
| 202742_s_at | NM 002731 | PRKACB | MTG | 3.74 | 7.08E−05 |
| 227817_at | R51324 | PRKCB1 | EC | −2.54 | 7.99E−04 |
| 228795_at | AI523569 | PRKCB1 | EC | −2.08 | 4.55E−04 |
| 209465_x_at | AL565812 | PTN | EC | −2.16 | 1.48E−03 |
| 209466_x_at | M57399 | PTN | EC | −3.87 | 8.75E−04 |
| 211737_x_at | BC005916 | PTN | EC | −4.55 | 1.68E−04 |
| 211737_x_at | BC005916 | PTN | PC | −2.22 | 4.62E−03 |
| 209466_x_at | M57399 | PTN | PC | −2.51 | 2.51E−03 |
| 209465_x_at | AL565812 | PTN | SFG | −2.79 | 1.00E−03 |
| 209686_at | BC001766 | S100B | PC | −2.46 | 4.52E−04 |
| 206330_s_at | NM 016848 | SHC3 | HIP | −1.72 | 9.61E−04 |
| 208845_at | BC002456 | VDAC3 | MTG | 1.57 | 6.31E−03 |
Corrected P values are shown.
Regional analysis of unique expression changes also identified additional affected pathways including cell communication (in the EC), neuron recognition (EC), neurite development (EC), cell organization and biogenesis (EC, HIP, PC, VCX), synaptic transmission (HIP, PC), regulation of neurotransmitter levels (HIP), intracellular transport (HIP, MTG, PC, VCX), smooth ER calcium ion homeostasis (MTG), neurophysiological process (PC), and negative regulation of apoptosis (SFG). Interestingly, in the VCX, the region found to be most spared from AD pathologies, the majority of the top processes include metabolic (protein, primary, cellular, macromolecule) and biosynthesis pathways, which may lend insight into earlier events that may influence this region’s protection from plaque and tangle formation. While the implications for these process-specific changes are not clear, this analysis provides evidence of specific changes in NDAD brains apart from AD brains that may define an early timepoint in neurodegeneration.
3.3. Regional expression variance across sample groups
To consider a more global perspective of expression changes across the control, NDAD, and AD sample groups, principle components analysis (PCA) was applied for each region. This analysis evaluates expression levels across all three sample groups and pinpoints expression patterns (also referred to as components) that account for the greatest amount of expression variance across these groups. The components identified from this analysis, along with the percentage of variance accounted for by each component, are shown in Fig. 2. Those genes that demonstrate a signature identical to the first component (with a correlation value of 1), and thus demonstrate the greatest expression changes across the three sample groups, are listed in Table 5. Briefly, for the EC, HIP, and PC, component 1 for each of these regions demonstrates an overall decrease in expression levels across control, NDAD, and AD brains. In contrast, for the MTG, SFG, and VCX, component 1 for these regions demonstrates an increase in expression levels across control, NDAD, and AD brains.
Evaluation of the genes accounting for the greatest amount of expression changes within each region and across the three sample groups led to the identification of potentially biologically relevant factors in AD pathogenesis. The first is cathepsin D (CTSD), a gene that has been suggested to demonstrate a genetic association with AD risk and pathogenesis (Davidson et al., 2006; Mariani et al., 2006; Papassotiropoulos et al., 2000) and which codes for a protease that may cleave apoE to generate fragments found in plaques (Zhou et al., 2006). CTSD, correlating with component 1 in the EC, demonstrates a decrease in expression starting from control brains, to NDAD brains, and to AD brains—this trend may represent neuroprotective efforts to inhibit plaque formation. Genes coding for enzymes that have primary roles in the ubiquitin–proteasomal pathway also demonstrated this downward trend across healthy brains to NDAD brains and to AD brains. These genes include UBR1 (ubiquitin protein ligase E3) which correlates with EC component 1 and UBE2I (ubiquitin-conjugating enzyme E2I), which correlates with PC component 1. These UBR1/UBE2I signatures suggest that their degradative pathways may be operating at lower levels in NDAD brains and more so in AD brains. Such down-regulation may represent a weakening of the ubiquitin–proteasomal system to ultimately allow buildup of NFTs. Also correlating with EC component 1 is neurexin 1 (NRXN1), whose transcripts can be alternatively spliced to generate alpha or beta isoforms. Interestingly, beta-neurexins interact with neuroligins to form and stabilize synapses (Benson et al., 2001; Scheiffele, 2003; Waites et al., 2005) so that the decreasing levels of expression shown by EC component 1 parallels characteristic loss of synaptic connections in AD brains and potentially in NDAD brains to a lesser extent.
PCA analysis of HIP also identified a number of interesting genes that correlate with component 1 in this region. First is CCS (copper chaperone for superoxide dismutase), which binds copper and complexes with and activates superoxide dismutase 1 (SOD1) (Brown et al., 2004; Culotta et al., 1997; Furukawa et al., 2004; Rae et al., 2001; Rothstein et al., 1999; Schmidt et al., 1999), an enzyme responsible for destroying free radicals. As AD pathogenesis is suggested to be influenced by oxidative stress resulting from free radicals (Markesbery, 1997), the expression signature for component 1 indicates a decrease in expression of CCS from healthy control brains to NDAD brains and to AD brains. This gradual decrease may demonstrate weakened neuronal efforts directed at fighting free radical toxicity in NDAD and AD brains. Second is ABAD (3-hydroxyacyl-CoA dehydro-genase type II), which has been found to be up-regulated in affected neurons in AD (Yan et al., 1997) and has been found to link Abeta to mitochondrial toxicity in AD (Lustbader et al., 2004). While HIP component 1 indicates a decrease in expression in NDAD and AD brains compared to controls, this finding correlates with our profiling of non-tangle bearing neurons. Also correlating with HIP component 1 is CAPNS1 (calpain, small subunit 1), which codes for a subunit common to all calpains. Increased activity of calpain has been suggested to be involved in AD development due to its association with perturbed calcium homeostasis (LaFerla, 2002; Mattson and Chan, 2003; Nixon, 2003; Vanderklish and Bahr, 2000). Thus, across NDAD and AD brains, the decreased expression of CAPNS1 may represent neuroprotective efforts enacted in healthy neurons of NDAD and AD brains.
Overall, PCA analysis identifies the expression trends within each region profiled and provides a general overview of region-specific transcriptomic changes that may be associated with disease progression. In the EC, HIP, and PC, significant down-regulation of gene expression is prevalent across control, NDAD, and AD brains, whereas in the MTG, SFG, and VCX, significant up-regulation of gene expression is seen. While further studies are necessary to decipher the implications of these changes, it is apparent that region-specific transcriptomic changes occur across brains of healthy elderly individuals, non-demented individuals with intermediate AD neuropathology, and clinically diagnosed AD patients with AD neuropathology, and may be key in understanding the timeline of AD pathogenesis.
3.4. RT-PCR validation of selected genes
To validate gene expression changes in NDAD brains, we performed RT-PCR on unprofiled fresh frozen brain sections from additional healthy elderly controls, NDAD cases, and AD cases. Based on the NDAD analyses, genes were selected for validation based on statistical significance (P < 0.05, corrected), relevance to AD, and availability of brain tissue. Based on these criteria, GRIA1, GRIA3, MAP1B, APOE, APP, BACE1, COX5B, and MAP4 were evaluated in the MTG and APOE, APP, BACE1, COX5B, and MAP4 were evaluated in the PC. Results from RT-PCR analysis, along with the respective array data, are shown in Table 6 and Fig. 3.
Table 6.
RT-PCR validation of selected genes
| Probe set ID | Gene name | GenBankID | MTG-array data |
MTG-RT-PCR data |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NDAD/control |
AD/control |
Normalized fold |
NDAD/control fold change |
NDAD/control t-test P-value |
AD/control fold change |
AD/control t-test P-value |
|||||||
| Fold change | Corrected P-value | Fold change | Corrected P-value | Control | NDAD | AD | |||||||
| 209793_at | GRIA1 | AL567302 | −1.42 | 3.44E−02 | −2.57 | 2.86E−06 | 1.00 | 0.26 | 0.39 | −3.85 | 3.61E−04 | −2.56 | 6.88E−03 |
| 208032_s_at | GRIA3 | NM_000828 | 2.04 | 1.19E−02 | −1.27 | 3.36E−01 | 1.00 | 0.53 | 0.37 | −1.89 | 4.93E−02 | −2.70 | 1.63E−02 |
| 217565_at | GRIA3 | BF110551 | 3.21 | 7.79E−03 | 1.19 | 2.16E+00 | |||||||
| 206730_at | GRIA3 | NM_007325 | 3.67 | 1.85E−04 | 1.82 | 3.34E−02 | |||||||
| 1569290_s_at | GRIA3 | BC032004 | 2.15 | 1.10E−04 | −1.32 | 1.44E+00 | |||||||
| 214577_at | MAP1B | BG164365 | 2.45 | 4.30E−03 | 1.76 | 1.71E−01 | 1.00 | 0.84 | 0.43 | −1.19 | 3.85E−01 | −2.33 | 5.46E−03 |
| 212233_at | MAP1B | AL523076 | −2.27 | 1.07E−05 | −4.27 | 2.21E−07 | |||||||
| 203381_s_at | APOE | N33009 | −2.75 | 9.06E−04 | 1.89 | 2.34E−02 | 1.00 | 0.59 | 0.54 | −1.69 | 2.55E−04 | −1.85 | 2.47E−03 |
| 203382_s_at | APOE | NM_000041 | −3.00 | 1.44E−04 | 1.53 | 1.08E−02 | |||||||
| 212884_x_at | APOE | AI358867 | −2.58 | 2.07E−05 | 1.80 | 8.77E−04 | |||||||
| 214953_s_at | APP | X06989 | 2.37 | 1.35E−03 | 1.12 | 1.44E+00 | 1.00 | 0.47 | 0.45 | −2.13 | 1.59E−03 | −2.22 | 6.40E−03 |
| 200602_at | APP | NM_000484 | 5.11 | 6.71E−04 | 3.09 | 8.20E−07 | |||||||
| 231086_at | BACE1 | BF939127 | −1.47 | 4.08E−02 | −1.26 | 3.27E−01 | 1.00 | 0.38 | 0.55 | −2.63 | 3.51E−03 | −1.82 | 3.96E−02 |
| 217904_s_at | BACE1 | NM_012104 | −1.75 | 9.56E−06 | −1.32 | 2.58E−03 | |||||||
| 213736_at | COX5B | AI557312 | −4.20 | 9.44E−04 | −4.43 | 9.31E−04 | 1.00 | 0.30 | 0.43 | −3.33 | 1.05E−06 | −2.33 | 4.39E−03 |
| 211025_x_at | COX5B | BC006229 | −2.97 | 6.05E−04 | −3.34 | 3.64E−04 | |||||||
| 202343_x_at | COX5B | NM_001862 | −2.75 | 1.72E−04 | −2.94 | 1.35E−04 | |||||||
| 213735_s_at | COX5B | AI557312 | −2.03 | 8.57E−05 | −2.21 | 2.25E−05 | |||||||
| 212567_s_at | MAP4 | AL523310 | −1.80 | 1.75E−02 | 2.40 | 1.60E−03 | 1.00 | 0.56 | 0.7 | −1.79 | 3.54E−03 | −1.43 | 2.68E−02 |
| 33850_at | MAP4 | W28892 | −1.70 | 9.05E−03 | 2.50 | 3.75E−03 | |||||||
| Probe set ID | Gene name | GenBank ID | PC-array data |
PC-RT-PCR data |
|||||||||
| NDAD/control |
AD/control |
Normalized fold |
NDAD/control fold change |
NDAD/control t-test P-value |
AD/control fold change |
AD/control t-test P-value |
|||||||
| Fold change | Corrected P-value | Fold change | Corrected P-value | Control | NDAD | AD | |||||||
| 203381_s_at | APOE | N33009 | −2.47 | 1.52E−03 | −2.57 | 7.47E−04 | 1.00 | 0.64 | 0.73 | −1.56 | 2.35E−03 | −1.37 | 1.47E−02 |
| 203382_s_at | APOE | NM_000041 | −1.94 | 2.35E−02 | −1.25 | 8.31E−01 | |||||||
| 212884_x_at | APOE | AI358867 | −2.02 | 2.40E−03 | −1.22 | 5.71E−01 | |||||||
| 211277_x_at | APP | BC004369 | 1.69 | 4.54E−04 | 3.01 | 2.05E−04 | 1.00 | 0.51 | 0.74 | −1.96 | 9.95E−03 | −1.35 | 1.33E−01 |
| 200602_at | APP | NM_000484 | 2.11 | 1.87E−04 | 1.93 | 8.38E−04 | |||||||
| 222462_s _at | BACE1 | AI653425 | −1.34 | 3.96E−02 | −1.17 | 9.87E−01 | 1.00 | 0.40 | 0.56 | −2.50 | 2.58E−02 | −1.79 | 5.22E−02 |
| 222463_s _at | BACE1 | AF190725 | −2.05 | 1.62E−04 | −1.16 | 1.12E+00 | |||||||
| 231086_at | BACE1 | BF939127 | −1.57 | 3.81E−03 | −1.35 | 3.27E−01 | |||||||
| 211025_x_at | COX5B | BC006229 | −2.08 | 2.39E−03 | −3.68 | 1.55E−05 | 1.00 | 0.32 | 0.68 | −3.13 | 2.22E−06 | −1.47 | 2.84E−02 |
| 202343_x_at | COX5B | NM_001862 | −2.18 | 3.87E−03 | −4.08 | 1.44E−05 | |||||||
| 235066_at | MAP4 | AI078534 | 1.75 | 2.89E−02 | −2.17 | 3.05E−02 | 1.00 | 0.60 | 0.84 | −1.67 | 3.96E−04 | −1.19 | 3.06E−01 |
RT-PCR validation data for the MTG and PC of unprofiled controls, NDAD cases, and AD cases are shown. Corresponding microarray expression data are also listed.
Fig. 3.
RT-PCR validation of selected genes. RT-PCR validation of expression changes identified from array analysis was performed on unprofiled MTG (controls: n = 9, NDAD: n = 8, AD: n = 9) and PC (controls: n = 8, NDAD: n = 8, AD: n = 11) samples. RT-PCR data, along with respective array data, are shown (quantitative data is listed in Table 6). Fold values normalized to controls are shown on the y-axis and genes are listed on the x-axis.
In the MTG, RT-PCR data validated expression changes in NDAD brains compared to healthy elderly control brains for GRIA1, APOE, BACE1, COX5B, and MAP4 (all demon-strated decreased expression in NDAD brains compared to controls). Non-significant changes were identified for MAP1B and opposite (down-regulated) changes were found for APP. Furthermore, RT-PCR analysis of AD MTG samples compared to control samples validated down-regulated expression changes for GRIA1, MAP1B, and COX5B. In the PC, RT-PCR data also validated expression changes in NDAD brains compared to controls for APOE, BACE1, and COX5B (these genes all showed down-regulated expression in NDAD brains compared to controls), while opposite changes were identified for APP and MAP4. Along with the NDAD validation, RT-PCR also validated down-regulated AD versus control expression changes in the PC for APOE and COX5B, while APP and MAP4 demonstrated non-significant changes. This RT-PCR data provides independent validation of the majority of expression changes of relevant genes selected from array analysis of the MTG and PC.
4. Summary
In this study, we expression profiled non-tangle bearing neurons from the post-mortem brains of non-demented individuals who demonstrated median levels of AD pathologies in the brain. The findings we present here build upon our previous study in which we similarly evaluated neurons from healthy elderly control brains and AD brains, and provide molecular information about an earlier state during AD pathogenesis. Significant overlapping expression changes were identified in both NDAD and AD brains compared to controls and may thus define a timeline of AD pathogenesis for which factors involved in formation of AD pathologies already demonstrate expression changes in NDAD brains. Overall,we have generated a high-quality, low PMI, novel expression data set that defines the neuronal tran-scriptome in healthy elderly, NDAD, and AD brains. This resource will help to elucidate AD pathogenesis and identifies novel targets for developing improved diagnostics and therapeutics against AD. Lastly, we provide this data set to the scientific community as a public resource.
Supplementary Material
Acknowledgements
We would like to thank Nick Lehmans (Translational Genomics Research Institute) for help in setting up the supplementary data site, Lucia Sue (Sun Health Research Institute) for help with obtaining neuropathological data, and Elizabeth Salomon (Translational Genomics Research Institute) for assistance with GEO data posting. We would also like to thank the National Institute on Aging’s Alzheimer’s Disease Centers program and the National Alzheimer’s Coordinating Center for help in obtaining samples for analysis.
This project was funded by grants from: the National Institute on Aging (#K01AG024079 to TD; 1-RO1-AG023193 to DAS; RO1-5U24NS051872 to DAS (NIH Neuroscience Microarray Consortium); P30 AG19610 to EMR; P50 AG05681 to JCM; P01 AG03991 to JCM; AG05128 for the Duke University ADC), the National Alzheimer’s Coordinating Center (U01AG016976), the Arizona Alzheimer’s Research Center (to EMR) under a collaborative agreement from the National Institute on Aging, and the State of Arizona to the Arizona Parkinson’s Disease Center (Arizona Biomedical Research Commission contract 0011).
Footnotes
Conflict of interest statement
The authors state that there are no actual or potential conflicts of interest.
Contributor Information
Winnie S. Liang, Email: wliang@tgen.org.
Travis Dunckley, Email: tdunckley@tgen.org.
Thomas G. Beach, Email: thomas.beach@sunhealth.org.
Andrew Grover, Email: andrew.grover@sunhealth.org.
Diego Mastroeni, Email: diego.mastroeni@sunhealth.org.
Richard J. Caselli, Email: caselli.richard@mayo.edu.
Walter A. Kukull, Email: kukull@u.washington.edu.
John C. Morris, Email: morrisj@abraxas.wustl.edu.
Christine M. Hulette, Email: hulet001@mc.duke.edu.
Eric M. Reiman, Email: eric.reiman@bannerhealth.com.
Joseph Rogers, Email: joseph.rogers@sunhealth.org.
Dietrich A. Stephan, Email: dstephan@tgen.org.
References
- Angelie E, Bonmartin A, Boudraa A, Gonnaud PM, Mallet JJ, Sappey-Marinier D. Regional differences and metabolic changes in normal aging of the human brain: proton MR spectroscopic imaging study. Am. J. Neuroradiol. 2001;22(1):119–127. [PMC free article] [PubMed] [Google Scholar]
- Barrachina M, Castano E, Ferrer I. TaqMan PCR assay in the control of RNA normalization in human post-mortem brain tissue. Neu-rochem. Int. 2006;49(3):276–284. doi: 10.1016/j.neuint.2006.01.018. [DOI] [PubMed] [Google Scholar]
- Belizaire R, Komanduri C, Wooten K, Chen M, Thaller C, Janz R. Characterization of synaptogyrin 3 as a new synaptic vesicle protein. J. Comp. Neurol. 2004;470(3):266–281. doi: 10.1002/cne.20008. [DOI] [PubMed] [Google Scholar]
- Benson DL, Colman DR, Huntley GW. Molecules, maps and synapse specificity. Nat. Rev. Neurosci. 2001;2(12):899–909. doi: 10.1038/35104078. [DOI] [PubMed] [Google Scholar]
- Blesa R, Mohr E, Miletich RS, Hildebrand K, Sampson M, Chase TN. Cerebral metabolic changes in Alzheimer’s disease: neu-robehavioral patterns. Dementia. 1996;7(5):239–245. doi: 10.1159/000106886. [DOI] [PubMed] [Google Scholar]
- Bobinski M, de Leon MJ, Convit A, De Santi S, Wegiel J, Tarshish CY, Saint Louis LA, Wisniewski HM. MRI of entorhinal cortex in mild Alzheimer’s disease. Lancet. 1999;353(9146):38–40. doi: 10.1016/s0140-6736(05)74869-8. [DOI] [PubMed] [Google Scholar]
- Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH. Regional distribution of neurofibrillary tangles and senile plaques in the cerebral cortex of elderly patients: a quantitative evaluation of a one-year autopsy population from a geriatric hospital. Cereb. Cortex. 1994;4(2):138–150. doi: 10.1093/cercor/4.2.138. [DOI] [PubMed] [Google Scholar]
- Boutajangout A, Boom A, Leroy K, Brion JP. Expression of tau mRNA and soluble tau isoforms in affected and non-affected brain areas in Alzheimer’s disease. FEBS Lett. 2004;576(1–2):183–189. doi: 10.1016/j.febslet.2004.09.011. [DOI] [PubMed] [Google Scholar]
- Braak H, Braak E. The human entorhinal cortex: normal morphology and lamina-specific pathology in various diseases. Neurosci. Res. 1992;15(1–2):6–31. doi: 10.1016/0168-0102(92)90014-4. [DOI] [PubMed] [Google Scholar]
- Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. (Berl.) 1991;82(4):239–259. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- Brown NM, Torres AS, Doan PE, O’Halloran TV. Oxygen and the copper chaperone CCS regulate posttranslational activation of Cu, Zn superoxide dismutase. Proc. Natl. Acad. Sci. U.S.A. 2004;101(15):5518–5523. doi: 10.1073/pnas.0401175101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad C, Zhu J, Conrad C, Schoenfeld D, Fang Z, Ingelsson M, Stamm S, Church G, Hyman BT. Single molecule profiling of tau gene expression in Alzheimer’s disease. J. Neurochem. 2007;103(3):1228–1236. doi: 10.1111/j.1471-4159.2007.04857.x. [DOI] [PubMed] [Google Scholar]
- Convit A, Wolf OT, de Leon MJ, Patalinjug M, Kandil E, Caraos C, Scherer A, Saint Louis LA, Cancro R. Volumetric analysis of the pre-frontal regions: findings in aging and schizophrenia. Psychiatry Res. 2001;107(2):61–73. doi: 10.1016/s0925-4927(01)00097-x. [DOI] [PubMed] [Google Scholar]
- Culotta VC, Klomp LW, Strain J, Casareno RL, Krems B, Gitlin JD. The copper chaperone for superoxide dismutase. J. Biol. Chem. 1997;272(38):23469–23472. doi: 10.1074/jbc.272.38.23469. [DOI] [PubMed] [Google Scholar]
- Davidson Y, Gibbons L, Pritchard A, Hardicre J, Wren J, Tian J, Shi J, Stopford C, Julien C, Thompson J, Payton A, Thaker U, Hayes AJ, Iwatsubo T, Pickering-Brown SM, Pendleton N, Horan MA, Burns A, Purandare N, Lendon CL, Neary D, Snowden JS, Mann DM. Genetic associations between cathepsin D exon 2 C → T polymorphism and Alzheimer’s disease, and pathological correlations with genotype. J. Neurol. Neurosurg. Psychiatry. 2006;77(4):515–517. doi: 10.1136/jnnp.2005.063917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leon MJ, George AE, Stylopoulos LA, Smith G, Miller DC. Early marker for Alzheimer’s disease: the atrophic hippocampus. Lancet. 1989;2(8664):672–673. doi: 10.1016/s0140-6736(89)90911-2. [DOI] [PubMed] [Google Scholar]
- Du AT, Schuff N, Zhu XP, Jagust WJ, Miller BL, Reed BR, Kramer JH, Mungas D, Yaffe K, Chui HC, Weiner MW. Atrophy rates of entorhinal cortex in AD and normal aging. Neurology. 2003;60(3):481–486. doi: 10.1212/01.wnl.0000044400.11317.ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira A, Kao HT, Feng J, Rapoport M, Greengard P. Synapsin III: developmental expression, subcellular localization, and role in axon formation. J. Neurosci. 2000;20(10):3736–3744. doi: 10.1523/JNEUROSCI.20-10-03736.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox NC, Warrington EK, Stevens JM, Rossor MN. Atrophy of the hippocampal formation in early familial Alzheimer’s disease. A longitudinal MRI study of at-risk members of a family with an amyloid precursor protein 717Val-Gly mutation. Ann. N.Y. Acad. Sci. 1996;777:226–232. doi: 10.1111/j.1749-6632.1996.tb34423.x. [DOI] [PubMed] [Google Scholar]
- Frisoni GB, Laakso MP, Beltramello A, Geroldi C, Bianchetti A, Soininen H, Trabucchi M. Hippocampal and entorhinal cortex atrophy in frontotemporal dementia and Alzheimer’s disease. Neurology. 1999;52(1):91–100. doi: 10.1212/wnl.52.1.91. [DOI] [PubMed] [Google Scholar]
- Furukawa Y, Torres AS, O’Halloran TV. Oxygen-induced maturation of SOD1: a key role for disulfide formation by the copper chaperone CCS. Embo J. 2004;23(14):2872–2881. doi: 10.1038/sj.emboj.7600276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsberg SD, Che S, Counts SE, Mufson EJ. Shift in the ratio of three-repeat tau and four-repeat tau mRNAs in individual cholinergic basal forebrain neurons in mild cognitive impairment and Alzheimer’s disease. J. Neurochem. 2006;96(5):1401–1408. doi: 10.1111/j.1471-4159.2005.03641.x. [DOI] [PubMed] [Google Scholar]
- Ginsberg SD, Hemby SE, Lee VM, Eberwine JH, Trojanowski JQ. Expression profile of transcripts in Alzheimer’s disease tangle-bearing CA1 neurons. Ann. Neurol. 2000;48(1):77–87. [PubMed] [Google Scholar]
- Goedert M, Spillantini MG, Jakes R, Rutherford D, Crowther RA. Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron. 1989;3(4):519–526. doi: 10.1016/0896-6273(89)90210-9. [DOI] [PubMed] [Google Scholar]
- Hackett JT, Cochran SL, Greenfield LJ, Jr, Brosius DC, Ueda T. Synapsin I injected presynaptically into goldfish mauthner axons reduces quantal synaptic transmission. J. Neurophysiol. 1990;63(4):701–706. doi: 10.1152/jn.1990.63.4.701. [DOI] [PubMed] [Google Scholar]
- Harrison PJ, Wighton-Benn WH, Heffernan JM, Sanders MW, Pearson RC. Amyloid precursor protein mRNAs in Alzheimer’s disease. Neurodegeneration. 1996;5(4):409–415. doi: 10.1006/neur.1996.0055. [DOI] [PubMed] [Google Scholar]
- Hemby SE, Trojanowski JQ, Ginsberg SD. Neuron-specific age-related decreases in dopamine receptor subtype mRNAs. J. Comp. Neurol. 2003;456(2):176–183. doi: 10.1002/cne.10525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilfiker S, Schweizer FE, Kao HT, Czernik AJ, Greengard P, Augustine GJ. Two sites of action for synapsin domain E in regulating neurotransmitter release. Nat. Neurosci. 1998;1(1):29–35. doi: 10.1038/229. [DOI] [PubMed] [Google Scholar]
- Hyman BT, Van Hoesen GW, Damasio AR, Barnes CL. Alzheimer’s disease: cell-specific pathology isolates the hippocampal formation. Science. 1984;225(4667):1168–1170. doi: 10.1126/science.6474172. [DOI] [PubMed] [Google Scholar]
- Ivancevic V, Alavi A, Souder E, Mozley PD, Gur RE, Benard F, Munz DL. Regional cerebral glucose metabolism in healthy volunteers determined by fluordeoxyglucose positron emission tomography: appearance and variance in the transaxial, coronal, and sagittal planes. Clin. Nucl. Med. 2000;25(8):596–602. doi: 10.1097/00003072-200008000-00005. [DOI] [PubMed] [Google Scholar]
- Jack CR, Jr, Petersen RC, Xu Y, O’Brien PC, Smith GE, Ivnik RJ, Tangalos EG, Kokmen E. Rate of medial temporal lobe atrophy in typical aging and Alzheimer’s disease. Neurology. 1998;51(4):993–999. doi: 10.1212/wnl.51.4.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz R, Sudhof TC, Hammer RE, Unni V, Siegelbaum SA, Bol-shakov VY. Essential roles in synaptic plasticity for synaptogyrin I and synaptophysin I. Neuron. 1999;24(3):687–700. doi: 10.1016/s0896-6273(00)81122-8. [DOI] [PubMed] [Google Scholar]
- Johnston JA, Norgren S, Ravid R, Wasco W, Winblad B, Lannfelt L, Cowburn RF. Quantification of APP and APLP2 mRNA in APOE genotyped Alzheimer’s disease brains. Brain Res. Mol. Brain Res. 1996;43(1–2):85–95. doi: 10.1016/s0169-328x(96)00161-1. [DOI] [PubMed] [Google Scholar]
- Jovanovic JN, Czernik AJ, Fienberg AA, Greengard P, Sihra TS. Synapsins as mediators of BDNF-enhanced neurotransmitter release. Nat. Neurosci. 2000;3(4):323–329. doi: 10.1038/73888. [DOI] [PubMed] [Google Scholar]
- Jovanovic JN, Sihra TS, Nairn AC, Hemmings HC, Jr, Greengard P, Czernik AJ. Opposing changes in phosphorylation of specific sites in synapsin I during Ca2+-dependent glutamate release in isolated nerve terminals. J. Neurosci. 2001;21(20):7944–7953. doi: 10.1523/JNEUROSCI.21-20-07944.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitano-Takahashi M, Morita H, Kondo S, Tomizawa K, Kato R, Tanio M, Shirota Y, Takahashi H, Sugio S, Kohno T. Expression, purification and crystallization ofahuman tau-tubulin kinase 2 that phos-phorylates tau protein. Acta Crystallogr. Sect. F: Struct. Biol. Cryst. Commun. 2007;63(Pt 7):602–604. doi: 10.1107/S1744309107028783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuwano R, Miyashita A, Arai H, Asada T, Imagawa M, Shoji M, Higuchi S, Urakami K, Kakita A, Takahashi H, Tsukie T, Toyabe S, Akazawa K, Kanazawa I, Ihara Y. Dynamin-binding protein gene on chromosome 10q is associated with late-onset Alzheimer’s disease. Hum. Mol. Genet. 2006;15(13):2170–2182. doi: 10.1093/hmg/ddl142. [DOI] [PubMed] [Google Scholar]
- LaFerla FM. Calcium dyshomeostasis and intracellular signalling in Alzheimer’s disease. Nat. Rev. Neurosci. 2002;3(11):862–872. doi: 10.1038/nrn960. [DOI] [PubMed] [Google Scholar]
- Li L, Chin LS, Shupliakov O, Brodin L, Sihra TS, Hvalby O, Jensen V, Zheng D, McNamara JO, Greengard P, Andersen P. Impairment of synaptic vesicle clustering and of synaptic transmission, and increased seizure propensity, in synapsin I-deficient mice. Proc. Natl. Acad. Sci. U.S.A. 1995;92(20):9235–9239. doi: 10.1073/pnas.92.20.9235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang WS, Dunckley T, Beach TG, Grover A, Mastroeni D, Ramsey K, Caselli RJ, Kukull WA, McKeel D, Morris JC, Hulette CM, Schmechel D, Reiman EM, Rogers J, Stephan DA. Altered neuronal gene expression in brain regions differentially affected by Alzheimer’s Disease: a reference data set. Physiol. Genomics. 2008 doi: 10.1152/physiolgenomics.00242.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang WS, Dunckley T, Beach TG, Grover A, Mastroeni D, Walker DG, Caselli RJ, Kukull WA, McKeel D, Morris JC, Hulette C, Schmechel D, Alexander GE, Reiman EM, Rogers J, Stephan DA. Gene expression profiles in anatomically and functionally distinct regions of the normal aged human brain. Physiol. Genomics. 2007;28(3):311–322. doi: 10.1152/physiolgenomics.00208.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- Llinas R, Gruner JA, Sugimori M, McGuinness TL, Greengard P. Regulation by synapsin I and Ca(2+)-calmodulin-dependent protein kinase II of the transmitter release in squid giant synapse. J. Physiol. 1991;436:257–282. doi: 10.1113/jphysiol.1991.sp018549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llinas R, McGuinness TL, Leonard CS, Sugimori M, Greengard P. Intraterminal injection of synapsin I or calcium/calmodulin-dependent protein kinase II alters neurotransmitter release at the squid giant synapse. Proc. Natl. Acad. Sci. U.S.A. 1985;82(9):3035–3039. doi: 10.1073/pnas.82.9.3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loessner A, Alavi A, Lewandrowski KU, Mozley D, Souder E, Gur RE. Regional cerebral function determined by FDG-PET in healthy volunteers: normal patterns and changes with age. J. Nucl. Med. 1995;36(7):1141–1149. [PubMed] [Google Scholar]
- Lohmann SM, Ueda T, Greengard P. Ontogeny of synaptic phos-phoproteins in brain. Proc. Natl. Acad. Sci. U.S.A. 1978;75(8):4037–4041. doi: 10.1073/pnas.75.8.4037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustbader JW, Cirilli M, Lin C, Xu HW, Takuma K, Wang N, Caspersen C, Chen X, Pollak S, Chaney M, Trinchese F, Liu S, Gunn-Moore F, Lue LF, Walker DG, Kuppusamy P, Zewier ZL, Arancio O, Stern D, Yan SS, Wu H. ABAD directly links Abeta to mitochondrial toxicity in Alzheimer’s disease. Science. 2004;304(5669):448–452. doi: 10.1126/science.1091230. [DOI] [PubMed] [Google Scholar]
- Mariani E, Seripa D, Ingegni T, Nocentini G, Mangialasche F, Ercolani S, Cherubini A, Metastasio A, Pilotto A, Senin U, Mecocci P. Interaction of CTSD and A2M polymorphisms in the risk for Alzheimer’s disease. J. Neurol. Sci. 2006;247(2):187–191. doi: 10.1016/j.jns.2006.05.043. [DOI] [PubMed] [Google Scholar]
- Markesbery WR. Oxidative stress hypothesis in Alzheimer’s disease. Free Radic. Biol. Med. 1997;23(1):134–147. doi: 10.1016/s0891-5849(96)00629-6. [DOI] [PubMed] [Google Scholar]
- Matsui T, Ingelsson M, Fukumoto H, Ramasamy K, Kowa H, Frosch MP, Irizarry MC, Hyman BT. Expression of APP pathway mRNAs and proteins in Alzheimer’s disease. Brain Res. 2007;1161:116–123. doi: 10.1016/j.brainres.2007.05.050. [DOI] [PubMed] [Google Scholar]
- Mattson MP, Chan SL. Neuronal and glial calcium signaling in Alzheimer’s disease. Cell Calcium. 2003;34(4–5):385–397. doi: 10.1016/s0143-4160(03)00128-3. [DOI] [PubMed] [Google Scholar]
- Melloni RH, Jr, DeGennaro LJ. Temporal onset of synapsin I gene expression coincides with neuronal differentiation during the development of the nervous system. J. Comp. Neurol. 1994;342(3):449–462. doi: 10.1002/cne.903420311. [DOI] [PubMed] [Google Scholar]
- Metsaars WP, Hauw JJ, van Welsem ME, Duyckaerts C. A grading system of Alzheimer disease lesions in neocortical areas. Neurobiol. Aging. 2003;24(4):563–572. doi: 10.1016/s0197-4580(02)00134-3. [DOI] [PubMed] [Google Scholar]
- Mielke R, Herholz K, Grond M, Kessler J, Heiss WD. Clinical deterioration in probable Alzheimer’s disease correlates with progressive metabolic impairment of association areas. Dementia. 1994;5(1):36–41. doi: 10.1159/000106692. [DOI] [PubMed] [Google Scholar]
- Mielke R, Kessler J, Szelies B, Herholz K, Wienhard K, Heiss WD. Normal and pathological aging—findings of positron-emission-tomography. J. Neural. Transm. 1998;105(8–9):821–837. doi: 10.1007/s007020050097. [DOI] [PubMed] [Google Scholar]
- Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM, Vogel FS, Hughes JP, van Belle G, Berg L. The consortium to establish a registry for Alzheimer’s Disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology. 1991;41(4):479–486. doi: 10.1212/wnl.41.4.479. [DOI] [PubMed] [Google Scholar]
- Moeller JR, Ishikawa T, Dhawan V, Spetsieris P, Mandel F, Alexander GE, Grady C, Pietrini P, Eidelberg D. The metabolic topography of normal aging. J. Cereb. Blood Flow Metab. 1996;16(3):385–398. doi: 10.1097/00004647-199605000-00005. [DOI] [PubMed] [Google Scholar]
- Nixon RA. The calpains in aging and aging-related diseases. Ageing Res. Rev. 2003;2(4):407–418. doi: 10.1016/s1568-1637(03)00029-1. [DOI] [PubMed] [Google Scholar]
- Oyama F, Shimada H, Oyama R, Titani K, Ihara Y. Beta-amyloid protein precursor and tau mRNA levels versus beta-amyloid plaque and neurofibrillary tangles in the aged human brain. J. Neurochem. 1993;60(5):1658–1664. doi: 10.1111/j.1471-4159.1993.tb13388.x. [DOI] [PubMed] [Google Scholar]
- Oyama F, Shimada H, Oyama R, Titani K, Ihara Y. Differential expression of beta amyloid protein precursor (APP) and tau mRNA in the aged human brain: individual variability and correlation between APP-751 and four-repeat tau. J. Neuropathol. Exp. Neurol. 1991;50(5):560–578. doi: 10.1097/00005072-199109000-00004. [DOI] [PubMed] [Google Scholar]
- Papassotiropoulos A, Bagli M, Kurz A, Kornhuber J, Forstl H, Maier W, Pauls J, Lautenschlager N, Heun R. A genetic variation of cathepsin D is a major risk factor for Alzheimer’s disease. Ann. Neurol. 2000;47(3):399–403. [PubMed] [Google Scholar]
- Preece P, Virley DJ, Costandi M, Coombes R, Moss SJ, Mudge AW, Jazin E, Cairns NJ. Amyloid precursor protein mRNA levels in Alzheimer’s disease brain. Brain Res. Mol. Brain Res. 2004;122(1):1–9. doi: 10.1016/j.molbrainres.2003.08.022. [DOI] [PubMed] [Google Scholar]
- Rae TD, Torres AS, Pufahl RA, O’Halloran TV. Mechanism of Cu, Zn-superoxide dismutase activation by the human metallochaperone hCCS. J. Biol. Chem. 2001;276(7):5166–5176. doi: 10.1074/jbc.M008005200. [DOI] [PubMed] [Google Scholar]
- Reich M, Ohm K, Angelo M, Tamayo P, Mesirov JP. GeneClus-ter 2.0: an advanced toolset for bioarray analysis. Bioinformatics. 2004;20(11):1797–1798. doi: 10.1093/bioinformatics/bth138. [DOI] [PubMed] [Google Scholar]
- Robinson CA, Clark AW, Parhad IM, Fung TS, Bou SS. Gene expression in Alzheimer neocortex as a function of age and pathologic severity. Neurobiol. Aging. 1994;15(6):681–690. doi: 10.1016/0197-4580(94)90049-3. [DOI] [PubMed] [Google Scholar]
- Rosahl TW, Spillane D, Missler M, Herz J, Selig DK, Wolff JR, Hammer RE, Malenka RC, Sudhof TC. Essential functions of synapsins I and II in synaptic vesicle regulation. Nature. 1995;375(6531):488–493. doi: 10.1038/375488a0. [DOI] [PubMed] [Google Scholar]
- Rothstein JD, Dykes-Hoberg M, Corson LB, Becker M, Cleveland DW, Price DL, Culotta VC, Wong PC. The copper chaperone CCS is abundant in neurons and astrocytes in human and rodent brain. J. Neurochem. 1999;72(1):422–429. doi: 10.1046/j.1471-4159.1999.0720422.x. [DOI] [PubMed] [Google Scholar]
- Saraswati S, Adolfsen B, Littleton JT. Characterization of the role of the Synaptotagmin family as calcium sensors in facilitation and asynchronous neurotransmitter release. Proc. Natl. Acad. Sci. U.S.A. 2007;104(35):14122–14127. doi: 10.1073/pnas.0706711104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheiffele P. Cell-cell signaling during synapse formation in the CNS. Annu. Rev. Neurosci. 2003;26:485–508. doi: 10.1146/annurev.neuro.26.043002.094940. [DOI] [PubMed] [Google Scholar]
- Schmidt PJ, Rae TD, Pufahl RA, Hamma T, Strain J, O’Halloran TV, Culotta VC. Multiple protein domains contribute to the action of the copper chaperone for superoxide dismutase. J. Biol. Chem. 1999;274(34):23719–23725. doi: 10.1074/jbc.274.34.23719. [DOI] [PubMed] [Google Scholar]
- Selkoe DJ. Alzheimer’s disease: genes, proteins, and therapy. Physiol. Rev. 2001;81(2):741–766. doi: 10.1152/physrev.2001.81.2.741. [DOI] [PubMed] [Google Scholar]
- Selkoe DJ, Schenk D. Alzheimer’s disease: molecular understanding predicts amyloid-based therapeutics. Annu. Rev. Pharmacol. Toxicol. 2003;43:545–584. doi: 10.1146/annurev.pharmtox.43.100901.140248. [DOI] [PubMed] [Google Scholar]
- Sinha S, Anderson JP, Barbour R, Basi GS, Caccavello R, Davis D, Doan M, Dovey HF, Frigon N, Hong J, Jacobson-Croak K, Jewett N, Keim P, Knops J, Lieberburg I, Power M, Tan H, Tatsuno G, Tung J, Schenk D, Seubert P, Suomensaari SM, Wang S, Walker D, Zhao J, McConlogue L, John V. Purification and cloning of amyloid precursor protein beta-secretase from human brain. Nature. 1999;402(6761):537–540. doi: 10.1038/990114. [DOI] [PubMed] [Google Scholar]
- Small GW, Ercoli LM, Silverman DH, Huang SC, Komo S, Bookheimer SY, Lavretsky H, Miller K, Siddarth P, Rasgon NL, Mazziotta JC, Saxena S, Wu HM, Mega MS, Cummings JL, Saunders AM, Pericak-Vance MA, Roses AD, Barrio JR, Phelps ME. Cerebral metabolic and cognitive decline in persons at genetic risk for Alzheimer’s disease. Proc. Natl. Acad. Sci. U.S.A. 2000;97(11):6037–6042. doi: 10.1073/pnas.090106797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sollner T, Whiteheart SW, Brunner M, Erdjument-Bromage H, Geromanos S, Tempst P, Rothman JE. SNAP receptors implicated in vesicle targeting and fusion. Nature. 1993;362(6418):318–324. doi: 10.1038/362318a0. [DOI] [PubMed] [Google Scholar]
- Sugita S, Janz R, Sudhof TC. Synaptogyrins regulate Ca2+-dependent exocytosis in PC12 cells. J. Biol. Chem. 1999;274(27):18893–18901. doi: 10.1074/jbc.274.27.18893. [DOI] [PubMed] [Google Scholar]
- Thal DR, Rub U, Orantes M, Braak H. Phases of A beta-deposition in the human brain and its relevance for the development of AD. Neurology. 2002;58(12):1791–1800. doi: 10.1212/wnl.58.12.1791. [DOI] [PubMed] [Google Scholar]
- Vanderklish PW, Bahr BA. The pathogenic activation of calpain: a marker and mediator of cellular toxicity and disease states. Int. J. Exp. Pathol. 2000;81(5):323–339. doi: 10.1111/j.1365-2613.2000.00169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassar R, Bennett BD, Babu-Khan S, Kahn S, Mendiaz EA, Denis P, Teplow DB, Ross S, Amarante P, Loeloff R, Luo Y, Fisher S, Fuller J, Edenson S, Lile J, Jarosinski MA, Biere AL, Curran E, Burgess T, Louis JC, Collins F, Treanor J, Rogers G, Citron M. Beta-secretase cleavage of Alzheimer’s amyloid precursor protein by the transmembrane aspartic protease BACE. Science. 1999;286(5440):735–741. doi: 10.1126/science.286.5440.735. [DOI] [PubMed] [Google Scholar]
- Waites CL, Craig AM, Garner CC. Mechanisms of vertebrate synaptogenesis. Annu. Rev. Neurosci. 2005;28:251–274. doi: 10.1146/annurev.neuro.27.070203.144336. [DOI] [PubMed] [Google Scholar]
- Yan R, Bienkowski MJ, Shuck ME, Miao H, Tory MC, Pauley AM, Brashier JR, Stratman NC, Mathews WR, Buhl AE, Carter DB, Tomasselli AG, Parodi LA, Heinrikson RL, Gurney ME. Membrane-anchored aspartyl protease with Alzheimer’s disease beta-secretase activity. Nature. 1999;402(6761):533–537. doi: 10.1038/990107. [DOI] [PubMed] [Google Scholar]
- Yan SD, Fu J, Soto C, Chen X, Zhu H, Al-Mohanna F, Collison K, Zhu A, Stern E, Saido T, Tohyama M, Ogawa S, Roher A, Stern D. An intracellular protein that binds amyloid-beta peptide and mediates neurotoxicity in Alzheimer’s disease. Nature. 1997;389(6652):689–695. doi: 10.1038/39522. [DOI] [PubMed] [Google Scholar]
- Zhou W, Scott SA, Shelton SB, Crutcher KA. Cathepsin D-mediated proteolysis of apolipoprotein E: possible role in Alzheimer’s disease. Neuroscience. 2006;143(3):689–701. doi: 10.1016/j.neuroscience.2006.08.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.