Abstract
Exposure to secondhand tobacco smoke (SHS) has been linked to increased risk for a number of diseases, including lung cancer. The tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) is of particular interest due to its potency and its specificity in producing lung tumors in animals. The NNK metabolite 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) in urine is frequently used as a biomarker for exposure. Due to its long half-life (40-45 days), NNAL may provide a long-term, time-averaged measure of exposure. We developed a highly sensitive liquid chromatography – tandem mass spectrometry (LC-MS/MS) method for determination of NNAL in human urine. The method involves liquid-liquid extraction followed by conversion to the hexanoate ester derivative. This derivative facilitates separation from interfering urinary constituents by extraction and chromatography, and enhances detection with electrospray ionization mass spectrometry. The lower limit of quantitation is 0.25 pg/mL for 5 mL urine specimens. Applications to studies of people with a range of different SHS exposure levels is described.
INTRODUCTION
Tobacco and tobacco smoke contain numerous toxic substances, including about 70 carcinogens.1 More than 400,000 people in the US, and about 5,000,000 people worldwide die from tobacco-related diseases each year.2, 3 Most of these deaths occur in cigarette smokers, but other forms of tobacco use and exposure to secondhand smoke (SHS) are also significant causes of morbidity and mortality.4 The association between cigarette smoking and lung cancer has been known for many years, well documented and publicized initially in the 1964 Surgeon General’s Report.5 A number of epidemiological studies have demonstrated an increased risk of lung cancer in nonsmokers having long-term exposure to SHS.4, 6
Based on toxicology studies in animals, it has been proposed that polycyclic aromatic hydrocarbons (PAHs) and tobacco-specific nitrosamines (TSNAs) are the major lung carcinogens in tobacco smoke.7 The TSNA 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) has received particular interest due to its potency as a carcinogen and its specificity in producing lung tumors in laboratory animals.7, 8 NNK is specific to tobacco and tobacco smoke, formed from nicotine by oxidation and nitrosation during the curing process, as well as being formed pyrosynthetically from nicotine during smoking (Figure 1).8–10
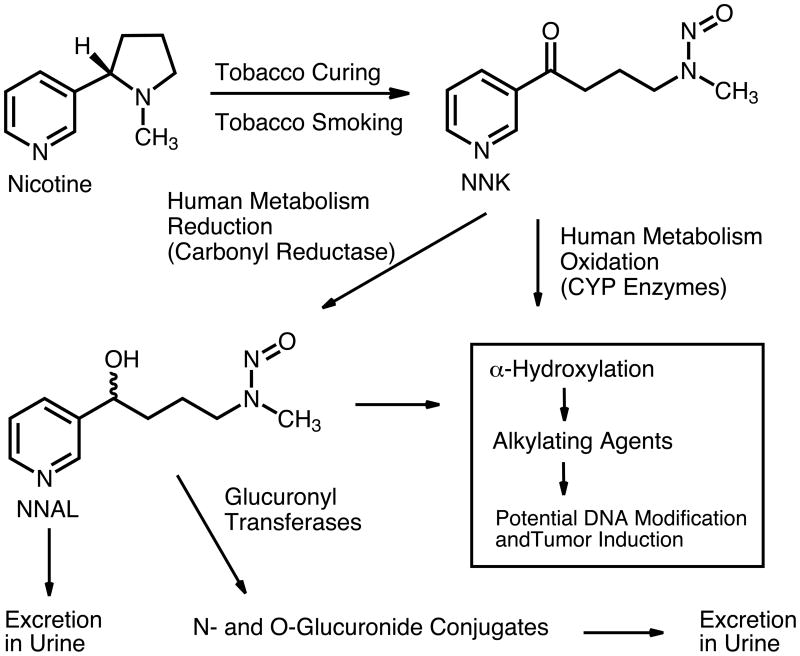
Figure 1.
Formation and metabolism of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK)
In humans and in laboratory animals, a major route of NNK metabolism is reduction of the keto group to give the secondary alcohol 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL (Figure 1). NNAL is further metabolized to N- and O-glucuronide conjugates, which are excreted in urine along with free NNAL.7, 8 A number of studies have documented the presence of NNAL and its glucuronides in urine of smokers and in urine of non-smokers exposed to SHS. Since these are quantitatively important metabolites of NNK, their determination in urine is of considerable utility in studies of human exposure to this tobacco-specific carcinogen.11, 12 In addition, the very long biologic half-live of NNK, 40–45 days,13 makes its metabolites useful as biomarkers for studies of long-term exposure to this carcinogen and to tobacco smoke in general. This is especially useful in studies of SHS exposure, in which exposure patterns are often irregular and the impact of exposure on disease outcomes occurs over a relatively long time period.
Depending upon the brand and the smoking conditions, a cigarette delivers 50 – 220 ng NNK in the mainstream smoke, which is inhaled by the smoker8, 14–16 and 50 – 1440 ng in the sidestream smoke.6, 8, 12 This results in urine concentrations (total NNAL, free + glucuronide) ranging from about 50 to 3000 pg/mL, with means of about 400–600 pg/mL in habitual smokers.17 In non-smokers concentrations are much lower, from undetectable to about 100 pg/mL, with means ranging from 2 – 20 pg/L depending on the exposure levels.18 Measuring low parts per trillion levels of NNAL in a complex biological matrix such as urine presents a considerable analytical challenge. In the pioneering work by Hecht and colleagues, GC with a nitrosamine-selective detector (thermal energy analyzer, TEA) was used. This method required extraction of large volumes of urine (50–100 mL), purification of the extract using two preparative HPLC steps, and conversion of the secondary hydroxy group to a trimethylsilyl ether derivative prior to GC analysis using a thermal energy analyzer (TEA) detector.19 Recently, the method has been streamlined by simplifying the extraction procedure and replacing one of the HPLC purification steps with a solid-phase extraction.20 LC-MS/MS has been used to quantify NNAL in urine of smokers.21, 22 Recently, an LC-MS/MS method having sufficient sensitivity (detection limit of 3 pg/mL) to determine NNAL in urine of SHS exposed non-smokers was reported. This method utilizes molecularly imprinted polymer (MIP) columns for selective extraction of NNAL and removal of interfering urinary constituents.23
As part of studies on the biological consequences of SHS exposure, we required a method for determination of NNAL in urine of people with relatively low exposure levels. In addition, in some studies large volumes of urine were not available, which required a very sensitive method. In this report, we describe an LC-MS/MS method for quantitation of NNAL at sub-picogram per milliliter concentrations in 5 mL urine specimens. The method involves conversion of the hydroxy group of NNAL to the hexanoate ester derivative, which facilitates the removal of interfering urinary constituents and enhances detection using electrospray ionization mass spectrometry.
EXPERIMENTAL SECTION
Instrumentation
LC-MS/MS analyses were carried out with a Surveyor HPLC interfaced to a TSQ Quantum Ultra triple-stage quadrupole mass spectrometer (Thermo-Finnigan, San Jose, CA), with a heated electrospray ion source (HESI). An HSF5 column (2.1 X 150 mm, 5 μm, Supelco, Sigma-Aldrich, Saint Louis, Mo.) was used for the chromatography. Solvent evaporation was carried out using a Savant SpeedVac model SC210A (Thermo-Savant, Marietta, OH).
Chemicals
NNAL-d3 was a generous gift from Dr. Stephen Hecht, University of Minnesota. NNAL-d0 was obtained from Toronto Research Chemicals, North York, Ontario, Canada. HPLC grade methanol and water from Burdick and Jackson (Muskegon, MI) were used to prepare the LC mobile phase. HPLC grade toluene, 1-butanol, pentane and ethyl acetate from Fisher were used for extractions. Beta-glucuronidase type IXA from E. coli (3660 units/mg), hexanoic anhydride and 4-(dimethylamino)pyridine (DMAP)were purchased from Sigma-Aldrich (Saint Louis, Mo).
Preparation of Standards and Controls
A stock standard solution of NNAl-d0 was prepared in 12 mM HCl and stored frozen at -20°C. A 500 pg/mL solution of NNAl-d3 was prepared in 10% methanol containing 12 mM HCl. Pooled urine, collected over several days, (2 liter batches) from a non-smoker with no known SHS exposure was used to prepare the standards and QCs. Standards and controls were stored frozen at −20°C until use.
Sample Preparation
50 μL of 500 pg/mL NNAl-d3 internal standard solution was added to 5 mL urine samples, standards and QCs in 50 mL polypropylene centrifuge tubes (Fisherbrand) followed by brief vortex mixing. Sodium potassium phosphate buffer (0.5 mL of 2 M, pH 7) was added followed by the addition of 50 μL of 50 mg/mL glucuronidase dissolved in 0.1 M phosphate buffer. The samples were then incubated for 20–24 hours at 37°C to convert the NNAL glucuronides to free NNAL. (Using twice the enzyme concentration did not increase the measured amount of NNAL). Potassium carbonate(0.5 mL of 50% w/v) was added, andthe samples were extracted by vortex mixing for 5 min with 8 mL of toluene/1-butanol (70:30). The two phases were separated by centrifugation at 4000 X G for 5 minutes. After freezing the tubes in a dry ice-acetone bath, the organic upper layers were poured into 16X125 mm glass culture tubes containing 0.8 mL of 1 M H2SO4 . The tubes were then vortexed 5 min and centrifuged as described above. The aqueous layers were frozen with a dry ice-acetone bath, and the organic layers were poured off and discarded. The acidlayer was then washed with 5 mL of ethyl acetate/toluene (2:1) by vortex mixing 5 min. The tubes were centrifuged, the aqueous acid layers were frozen in a dry ice-acetone bath, and the upper wash layer was discarded. The acid phaseswere made basic with 0.8 mL of 50% (w/v) K2CO3 and extracted by vortex mixing 5 min with 4 mL of ethyl acetate/toluene (1:2). After centrifugation and freezing the aqueous layers the organic layers were transferred to 13X100 mm glass culture tubes. The organic extracts were then evaporated to dryness using the SpeedVac at high heat setting. Hexanoic anhydride (50 μL ) and 10 μL of 50 mg/mL 4-(dimethylamino)pyridine (DMAP) in toluene was then added to the dry extracts, the tubes were then tightly capped and heated at 70°C for 15 minutes. Saturated aqueous sodium bicarbonate (0.5 mL ) and 4 mL of 10% ethyl acetate in pentane were added, and the derivatives were extracted by vortex mixing, centrifugation, and freezing the aqueous layers. The organic layers were transferred to 13X100 mm tubes containing 0.5 mL of 1 M H2SO4 and the organic layers were discarded after vortexing, centrifuging and freezing. The acid layers were made basic with 0.5 mL of 50% (w/v) K2CO3 and then extracted with 4 ml of 10% ethyl acetate in pentane by vortex mixing, centrifugation, and freezing the aqueous layers. The organic layers were transferred to a new set of 13X100 mm tubes and evaporated using the SpeedVac at medium heat. The samples were reconstituted in 125 μL of 10% methanol containing 12 mM HCl and transferred to 300 μL polypropylene insert vials for analysis. Extraction efficiency was determined by spiking d0 and d3-NNAL into blank extract prior to evaporation and derivatization. A typical run consisted of 46 study samples plus 26 standards and QCs for a total of 72 samples. One analyst can carry out the enzyme incubation, extraction, and derivatization steps in 3 days, and the entire run, including LC-MS/MS analysis can be completed in a week.
Liquid Chromatography
The extracts (50 μL) were chromatographed with a methanol and water solvent system containing 10 mM ammonium formate at 0.333 mL/min using a linear gradient from 33% to 100% methanolic buffer over 11 minutes. The column was then held at 100% methanol for 1 minute and then ramped back to the initial conditions over 1 minute. Re-equilibration time was 7 minutes for a total run time of 20 minutes per sample.
Mass Spectrometry
The mass spectrometer was operated using electrospray ionization, in the positive ion mode. The ion source parameters were optimized by infusing a solution of the hexanoate ester derivative of NNAL into the ion source via a syringe pump. The vaporizer temperature was 372 °C, the heated capillary temperature was 265° C, the spray voltage was 3500 mV. Data was acquired in the selected reaction monitoring (SRM) mode. The transitions 308 to 84 and 311 to 87 at a collision energy of 20 eV were used for the hexanoate derivatives of NNAL and the internal standard, NNAL-d3, respectively. The mass resolution (FWHM) was set at 0.5 amu for both Q1 and Q3.
Data Analysis
The Finnigan XCalibur/LC Quan software was used to generate calibration curves (linear regression, 1/X weighting) and calculate concentrations using peak area ratios of analyte/internal standard. Two sets of 6 standards, spanning the range of 0.25 to 50 pg/mL were included in each run of 40–45 clinical samples. For studies of low-level SHS exposure, three sets of quality control specimens at 0, 0.5, 1.0 and 2.0 pg/mL were included. Analysis of spiked urine samples indicated that the method is linear to at least 500 pg/mL.
Clinical Samples
Urine specimens were obtained from nonsmokers participating in research studies, described elsewhere,24, 25 and were stored frozen at −20 °C prior to analysis.
RESULTS AND DISCUSSION
Method Development
Using LC-ESI-MS/MS methods similar to published methods,17, 21–23 we had previously been able to achieve a detection limit of 5 pg/mL for 3 mL urine specimens.26 However, some of our studies involved subjects with low-level exposure to SHS,24 and a method with higher sensitivity was required. The limiting factor was not instrument sensitivity, but rather trace amounts of co-eluting substances in the urine extracts. Attempts to separate these interfering substances chromatographically and with further MIP column purification23 of the liquid/liquid solvent extracts were unsuccessful.
NNAL is a moderately polar organic compound, and it occurred to us that by esterification of the hydroxy group, it could be converted to a relatively non-polar substance. Doing so might be expected to improve sensitivity in LC-MS/MS analysis for the following reasons: (1) A relatively non-polar substance could be partitioned between an aqueous phase and a non-polar organic solvent to remove many of the multitude of potentially interfering polar organic compounds present in urine. (2) The relatively non-polar ester derivative would be better retained on reverse-phase HPLC columns than the parent NNAL, and this could be a mechanism for separation of more polar, potentially interfering substances in the sample. (3) More efficient separation from other ionizable substances in urine, by extraction and chromatography, would be expected to reduce the extent of matrix suppression of ionization often occurring in electrospray ionization (ESI) of biological extracts.27–29 (4) Ionization efficiency of the ester derivative in an ESI source might be enhanced compared to NNAL, due to more efficient desolvation. The hydroxy group of NNAL would be expected to hydrogen bond strongly with the usual reverse-phase HPLC solvents water, methanol, and acetonitrile, but an ester would be expected to do so less avidly. (5) Increasing the mass by derivatization might be expected to increase selectivity in mass spectrometric detection, since potentially interfering substances in urine would be expected to have relatively low molecular weight. Consequently, we prepared the acetate and hexanoate derivatives, and evaluated them for sensitivity and specificity of detection in urine extracts.
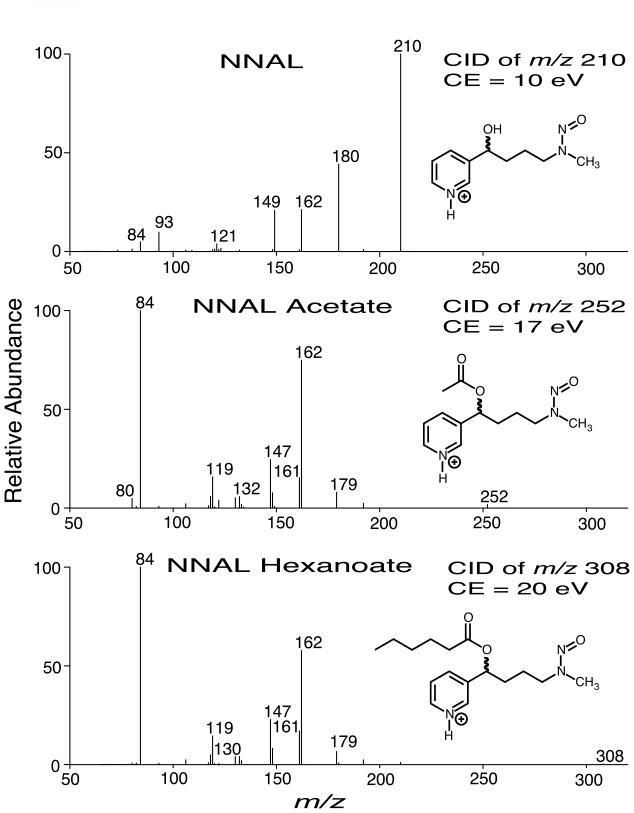
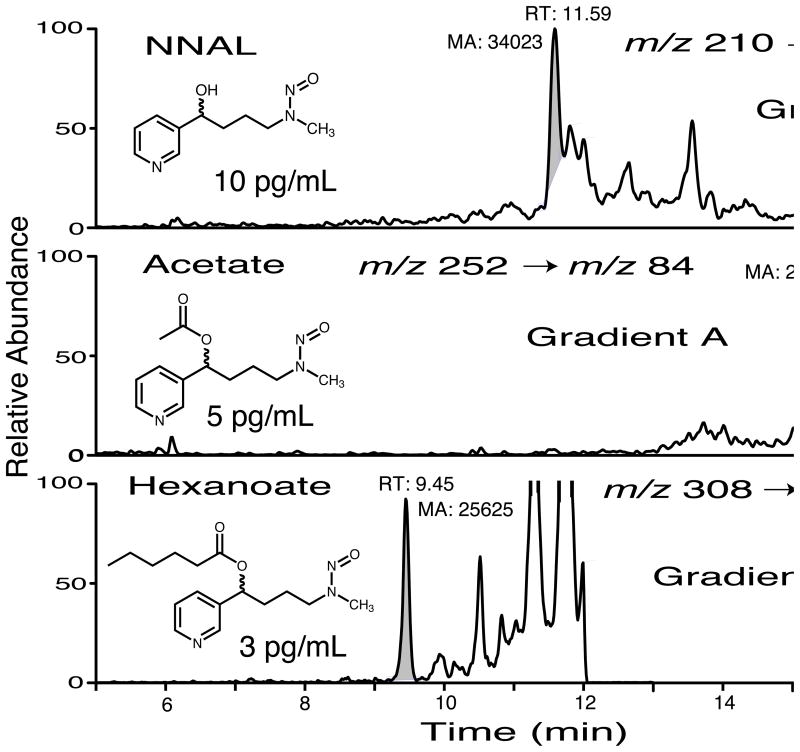
ESI was used, and the most abundant ion transitions of each derivative (Figure 2) were evaluated in the selected reaction monitoring (SRM) mode. HPLC separation was carried out using a gradient of water – methanol with ammonium formate (pH ~ 6) buffer. Both derivatives provided better sensitivity than underivatized NNAL, but the hexanoate was by far the best, presumably owing to its much lower polarity, facilitating chromatographic separation from co-extracted substances in urine, as well as more efficient desolvation in the electrospray ion source. Depending on the mobile phase composition, the ESI response was 1.5 to 2.3 times greater for the hexanoate derivative than for underivatized NNAL, with the response for the acetate derivative between the two. Not surprisingly, the differences were greater under conditions of gradient elution, in which the hexanoate derivative eluted with a lower percentage of water in the mobile phase than the acetate or underivatized NNAL (Table 1). These data support the notion that these less polar derivatives bind less avidly to water and methanol, facilitating desolvation and increasing transmission of ions into the mass spectrometer. However, the most important factor affecting sensitivity was separation from interfering urinary constituents, since the intrinsic ESI response was not the factor limiting the sensitivity of the method (Figure 3). By comparing spiked urine to aqueous standards, suppression of ionization was estimated to be about 25%. Of the SRM transitions evaluated, m/z 308 to m/z 84 of the hexanoate derivative provided the best selectivity in terms of minimizing interference by urinary constituents. Although a confirmation ion would be an advantage, none of the alternative product ions we investigated had enough specificity for detection in urine below about 3 pg/mL, and unfortunately, most of our study samples had concentrations below this.
Figure 2.
Product ion spectra of NNAL, NNAL acetate, and NNAL hexanoate.
Table 1.
Comparison of ESI sensitivity for NNAL, NNAL acetate, and NNAL hexanoate with different HPLC mobile phase compositions.
| Analyte | Isocratica % of NNALd | Fast gradientb % of NNALd | Slow gradientc % of NNALd |
|---|---|---|---|
| NNAL | 100 | 100 | 100 |
| NNAL Acetate | 113 | 154 | 112 |
| NNAL Hexanoate | 154 | 212 | 231 |
10 mM ammonium formate in 90:10 methanol/water.
Linear gradient of 10 mM ammonium formate, 100% aqueous changing to 100% methanolic over 2 min followed by 6 min methanolic.
Gradient described in Experimental Section used for urine sample analyses.
Peak areas as percent of the peak area for NNAL.
Figure 3.
Chromatograms of urine extracts containing NNAL, NNAL acetate, and NNAL hexanoate. Mobile phase (10 mM ammonium formate in methanol-water), column, and flow rate as described in experimental section. A was a linear gradient from 10% methanol to 70% methanol over 15 minutes; B was a linear gradient from 33% methanol to 100% methanol over 11 minutes.
A liquid-liquid extraction/derivatization procedure was devised to (1) utilize acid-base partitioning of the weakly basic NNAL, which has pyridine ring, to remove neutral and acidic substances; (2) esterify the hydroxy group with hexanoic anhydride to provide the hexanoate derivative; (3) remove excess hexanoic anhydride and other remaining neutral and acidic substances by acid-base partitioning, and (4) a final extraction with a solvent of low polarity (90–10 pentane – ethyl acetate) followed by evaporation and reconstitution in HPLC mobile phase. The efficiency of extraction was determined by spiking urine with both NNAL-d0 and NNAL-d3 and comparing the peak areas with urine extracts spiked prior to the derivatization step. The extraction recovery was about 60%.
Method validation
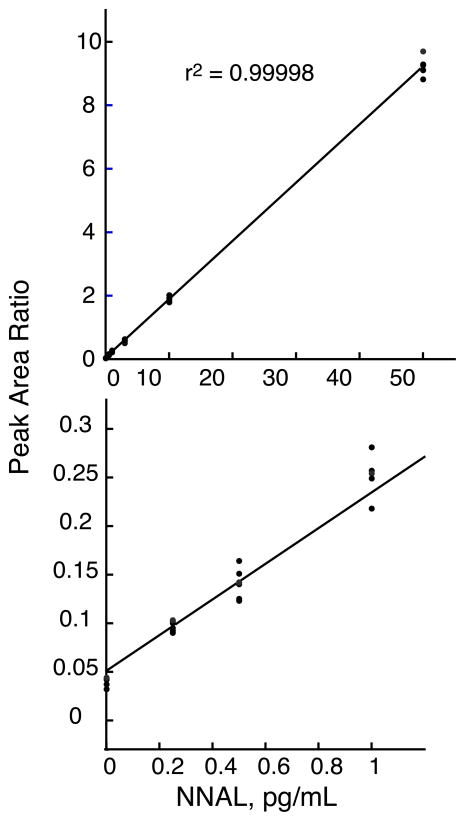
Standard curves were linear from 0.25 to 50 pg/mL with typical r2 values > 0.99 using linear regression with 1/x weighting. A standard curve constructed from means of six replicates is presented in Figure 4. Precision, accuracy, and lower limit of quantitation were determined by analyzing urine from a non-smoker, who had no known exposure to SHS, spiked with NNAL. Over the range of 0.25 pg/mL to 50 pg/mL, precision ranged from 3.2 – 15.0 % (percent coefficient of variation, CV) and accuracy ranged from 88.0-107.1 % (percent of expected) (Tables 2 and 3). Using the criteria of Shah et al, the lower limit of quantitation (LLOQ) was determined to be 0.25 pg/mL.30 Determining the limit of detection (LOD) in urine is complicated by the ubiquitous presence of tobacco smoke residues in the environment, and consequently nearly everyone will have at least a minute exposure to the precursor substance NNK. Therefore, truly NNAL-free urine may be hard to verify, and it may be not be possible to distinguish NNAL from a co-eluting substance with the same product ion. Consequently, we investigated the LOD by extracting, derivatizing, and analyzing standards prepared in 0.01 N HCl. The blank value was positive, as the intercept of the standard curve indicated. A 5 mL 0.0625 pg/mL standard prepared in 0.01 N HCl, following extraction, derivatization, and injection of an aliquot gave rise to a peak with about twice the peak area of a corresponding peak in the blank. We also estimated the instrument sensitivity by injecting known amounts of NNAL hexanoate. Injecting an aliquot of a methanol solution containing 62.5 attomoles of NNAL hexanoate (which would correspond to about 13 femtograms of NNAL) resulted in a peak of about twice the area of a corresponding peak in the methanol blank.
Figure 4.
Calibration curve for NNAL in urine. Six replicates at each concentration, linear regression, 1/x weighting. Lower panel is expanded scale for range of 0-1 pg/mL.
Table 2.
Within-run precision and accuracy for determination of NNAL in urinea
| Added Amount (pg/mL) | Measured Mean (pg/mL) | Accuracy (Percent of Expected) | Precision CV (%) |
|---|---|---|---|
| 0 | < LLOQ | __ | 12.3b |
| 0.25 | 0.24 | 95.2 | 12.6 |
| 0.50 | 0.47 | 94.1 | 12.5 |
| 1.00 | 1.08 | 107.9 | 10.2 |
| 3.00 | 2.87 | 95.8 | 8.3 |
| 10.00 | 10.10 | 101.0 | 4.2 |
| 50.00 | 49.99 | 100.0 | 3.2 |
Six replicate analyses of urine from a non-smoker with no known SHS exposure spiked with NNAL.
For blank urine, precision is based on the area ratios of peak corresponding to analyte/peak of internal standard.
Table 3.
Between-run precision and accuracy for determination of NNAL in urinea
| Added Amount (pg/mL) | Measured Mean (pg/mL) | Accuracy (Percent of Expected) | Precision CV (%) |
|---|---|---|---|
| 0.50 | 0.487 | 97.4 | 15.0 |
| 1.00 | 0.950 | 95.0 | 8.8 |
| 2.00 | 1.76 | 88.0 | 4.4 |
Seven replicate analyses (three different runs) of urine from a non-smoker with no known SHS exposure spiked with NNAL.
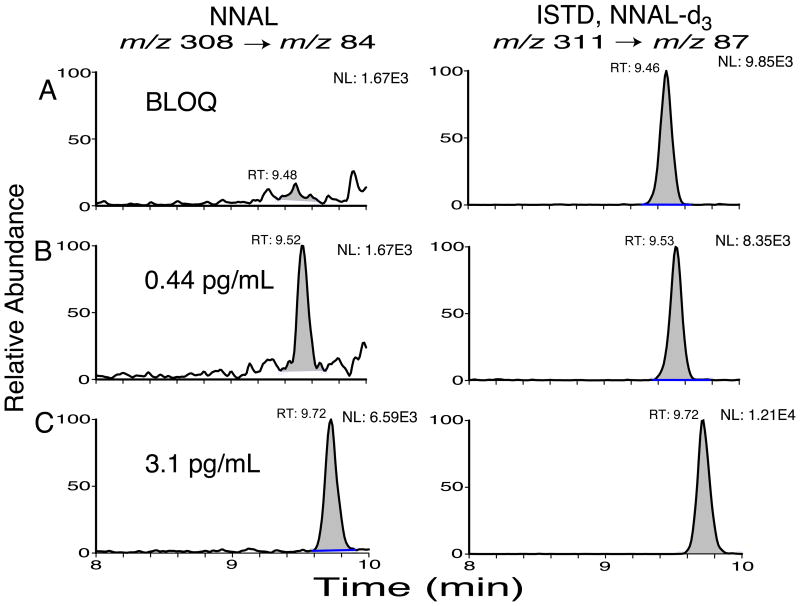
Specificity was determined by analyzing urine samples from 8 non-smokers with no known SHS exposure. All had NNAL concentrations below the limit of quantitation of 0.25 pg/mL. A urine specimen from a person reporting a brief exposure to SHS 17 hr prior to the sample collection had a concentration of 0.99 pg/mL. Chromatograms of urine extracts from three people with varying levels of SHS exposure are presented in Figure 5.
Figure 5.
Chromatograms of non-smokers’ urine extracts. A, person with little or no SHS exposure; B, subject in study of SHS exposure in people with chronic obstructive pulmonary disease;24 C, college student after SHS exposure in a bar.25
Application of the Method
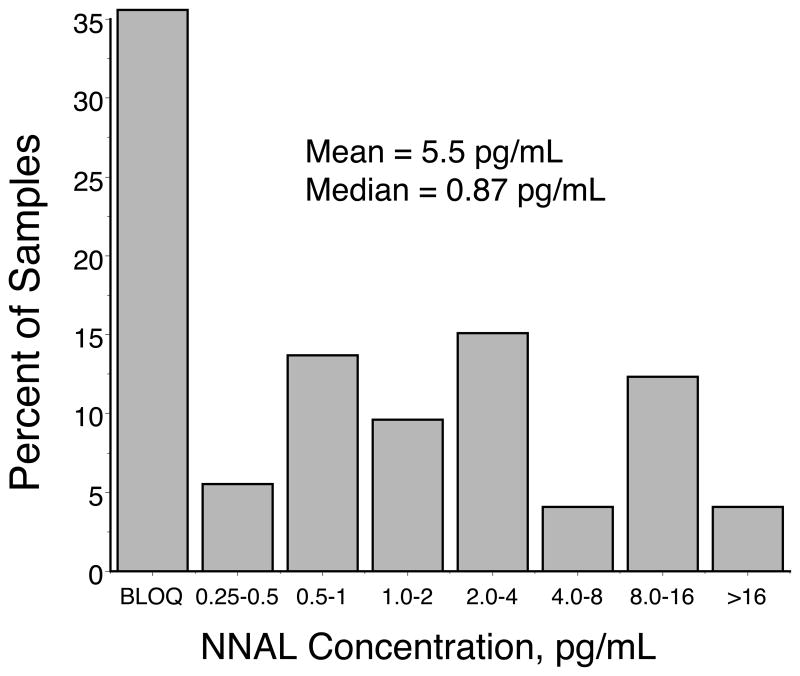
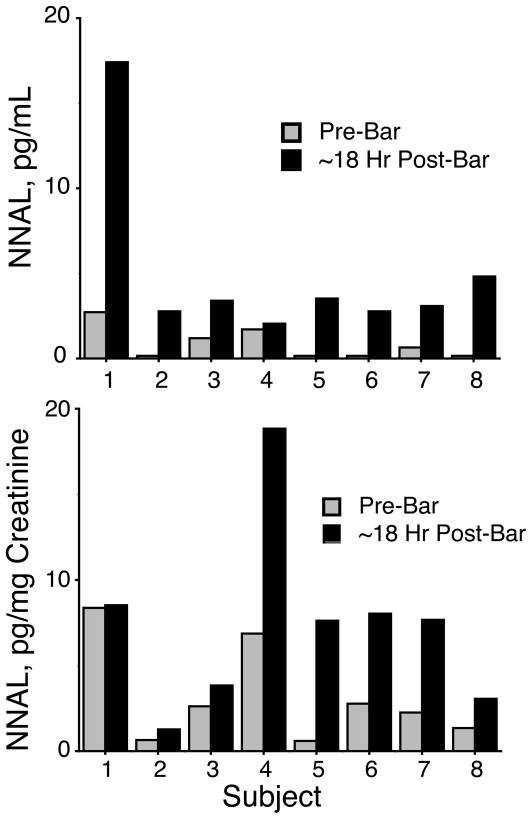
Urine specimens from 73 non-smoking research subjects who suffered from chronic obstructive pulmonary disease24 (COPD) were analyzed for NNAL. Concentrations ranged from below the LOQ (26 subjects) to 153 pg/mL, with a mean of 5.5 pg/mL, and median of 0.87 pg/mL. (Figure 6). The mean is similar to that reported by other investigators for non-smokers.18 We also analyzed urine samples from 8 non-smoking college students before and after they spent 6 hours in smoking-allowed bars. In all 8 subjects, concentrations of NNAL in urine collected approximately 16 hours after entering the bar were higher than those from samples collected prior to entering the bar (Figure 7).
Figure 6.
Distribution of NNAL concentrations in urine of 73 Research Subjects with chronic obstructive pulmonary disease.24 BLOQ = below limit of quantitation.
Figure 7.
Concentrations of NNAL in urine of 8 college students prior to and after spending 6 hours in smoking-allowed bars.25 In the lower panel concentrations are normalized to creatinine to adjust for differences in urinary flow.
CONCLUSION
A method for determination of the tobacco-specific carcinogen biomarker NNAL in human urine at sub-picogram per milliliter concentrations has been developed. Key to the success of this method was conversion of the analyte to a relatively non-polar derivative, which facilitates removal of interfering substances in the sample matrix by chromatography and by the extraction procedure, and enhances detection by electrospray ionization mass spectrometry. This method appears to be the most sensitive method yet reported for determination of NNAL in urine. Applicability of the method to determination of NNAL in urine of humans exposed to low levels of secondhand tobacco smoke has been demonstrated. Although derivatization adds extra steps to the sample preparation procedure, conversion of hydrophilic analytes to more hydrophobic derivatives has the potential to greatly improve the sensitivity and specificity of ESI mass spectrometric analyses.
Acknowledgments
The authors thank Margaret Wilson, who carried out much of the development work for the extraction procedure, Yan Chen and Kefei Wang of Thermo-Fisher Corporation for providing the heated ESI source used in these studies, and Marc Olmsted for editorial assistance. Financial support from the Flight Attendant Medical Research Institute, The National Institutes of Health (DA012393, CA78603, DA02277) and the California Tobacco Related Disease Research Program (10RT-0215) is gratefully acknowledged.
References
- 1.Hoffmann D, Hoffmann I, El-Bayoumy K. Chem Res Toxicol. 2001;14:767–790. doi: 10.1021/tx000260u. [DOI] [PubMed] [Google Scholar]
- 2.MMWR Morb Mortal Wkly Rep. 2005;54:625–628. [PubMed] [Google Scholar]
- 3.Benowitz NL. Clin Pharmacol Ther. 2008;83:531–541. doi: 10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- 4.Department of Health and Human Services, P. H. S. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. DHHS (CDC) Publication No. 87-8398. US Government Printing Office; Washington DC: 2006. [Google Scholar]
- 5.Public Health Service Publication No. 1103. U.S. Department of Health and Human Services; Bethesda, Maryland: 1964. Smoking and Health: A report of the Advisory Committee to the Surgeon General. [Google Scholar]
- 6.International Council for Research on Cancer . IARC Sci Publ. 2004. p. 83. [Google Scholar]
- 7.Hecht SS. Chem Res Toxicol. 1998;11:559–603. doi: 10.1021/tx980005y. [DOI] [PubMed] [Google Scholar]
- 8.Hecht SS, Tricker AR. In: Analytical Determination of Nicotine and Related Compounds and Their Metabolites. Gorrod JW, Jacob P III, editors. Elsevier; Amsterdam: 1999. pp. 421–488. [Google Scholar]
- 9.Hecht SS, Chen CB, Ornaf RM, Jacobs E, Adams JD, Hoffmann D. J Org Chem. 1978;43:72–76. doi: 10.1021/jo00395a017. [DOI] [PubMed] [Google Scholar]
- 10.Adams JD, Lee SJ, Hoffmann D. Carcinogenesis. 1984;5:221–223. doi: 10.1093/carcin/5.2.221. [DOI] [PubMed] [Google Scholar]
- 11.Hecht SS. Carcinogenesis. 2002;23:907–922. doi: 10.1093/carcin/23.6.907. [DOI] [PubMed] [Google Scholar]
- 12.Hecht SS. Tob Control. 2004;13(Suppl 1):i48–56. doi: 10.1136/tc.2002.002816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hecht SS, Carmella SG, Chen M, Dor Koch JF, Miller AT, Murphy SE, Jensen JA, Zimmerman CL, Hatsukami DK. Cancer Res. 1999;59:590–596. [PubMed] [Google Scholar]
- 14.Wu W, Ashley DL, Watson CH. Anal Chem. 2003;75:4827–4832. doi: 10.1021/ac030135y. [DOI] [PubMed] [Google Scholar]
- 15.Harris JE. Public Health Rep. 2001;116:336–343. doi: 10.1093/phr/116.4.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wagner KA, Finkel NH, Fossett JE, Gillman IG. Anal Chem. 2005;77:1001–1006. doi: 10.1021/ac048887v. [DOI] [PubMed] [Google Scholar]
- 17.Hecht SS, Carmella SG, Murphy SE, Riley WT, Le C, Luo X, Mooney M, Hatsukami DK. Cancer Epidemiol Biomarkers Prev. 2007;16:1567–1572. doi: 10.1158/1055-9965.EPI-07-0227. [DOI] [PubMed] [Google Scholar]
- 18.Hecht SS. Prev Med. 2006;43:256–260. doi: 10.1016/j.ypmed.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 19.Hecht SS, Carmella SG, Murphy SE, Akerkar S, Brunnemann KD, Hoffmann D. N Engl J Med. 1993;329:1543–1546. doi: 10.1056/NEJM199311183292105. [DOI] [PubMed] [Google Scholar]
- 20.Carmella SG, Han S, Fristad A, Yang Y, Hecht SS. Cancer Epidemiol Biomarkers Prev. 2003;12:1257–1261. [PubMed] [Google Scholar]
- 21.Byrd GD, Ogden MW. J Mass Spectrom. 2003;38:98–107. doi: 10.1002/jms.406. [DOI] [PubMed] [Google Scholar]
- 22.Pan J, Song Q, Shi H, King M, Junga H, Zhou S, Naidong W. Rapid Commun Mass Spectrom. 2004;18:2549–2557. doi: 10.1002/rcm.1656. [DOI] [PubMed] [Google Scholar]
- 23.Xia Y, McGuffey JE, Bhattacharyya S, Sellergren B, Yilmaz E, Wang L, Bernert JT. Anal Chem. 2005;77:7639–7645. doi: 10.1021/ac058027u. [DOI] [PubMed] [Google Scholar]
- 24.Eisner MD, Balmes J, Yelin EH, Katz PP, Hammond SK, Benowitz N, Blanc PD. BMC Pulm Med. 2006;6:12. doi: 10.1186/1471-2466-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Repace J, Hughes E, Benowitz N. Nicotine Tob Res. 2006;8:701–711. doi: 10.1080/14622200600792696. [DOI] [PubMed] [Google Scholar]
- 26.Benowitz NL, Hall SM, Stewart S, Wilson M, Dempsey D, Jacob P., 3rd Cancer Epidemiol Biomarkers Prev. 2007;16:2479–2485. doi: 10.1158/1055-9965.EPI-07-0393. [DOI] [PubMed] [Google Scholar]
- 27.Matuszewski BK, Constanzer ML, Chavez-Eng CM. Anal Chem. 1998;70:882–889. doi: 10.1021/ac971078+. [DOI] [PubMed] [Google Scholar]
- 28.Jacob P, 3rd, Wilson M, Yu L, Mendelson J, Jones RT. Anal Chem. 2002;74:5290–5296. doi: 10.1021/ac020101a. [DOI] [PubMed] [Google Scholar]
- 29.Liang HR, Foltz RL, Meng M, Bennett P. Rapid Commun Mass Spectrom. 2003;17:2815–2821. doi: 10.1002/rcm.1268. [DOI] [PubMed] [Google Scholar]
- 30.Shah VP, Midha KK, Findlay JW, Hill HM, Hulse JD, McGilveray IJ, McKay G, Miller KJ, Patnaik RN, Powell ML, Tonelli A, Viswanathan CT, Yacobi A. Pharm Res. 2000;17:1551–1557. doi: 10.1023/a:1007669411738. [DOI] [PubMed] [Google Scholar]