Abstract
For more than 50 years, links between autoimmunity and lymphomas have been described based on human and animal studies. Over the last three decades, many studies have addressed specific hypotheses about these associations using population level data. This has been accomplished by assessing previous autoimmune history in case-control studies of patients with lymphoma (mainly non-Hodgkin lymphoma) and myeloma, and by following cohorts of patients with various autoimmune diseases for subsequent development of lymphoma and multiple myeloma. In this paper, we review our recently published series of association studies based on data from Scandinavia and from U.S. Veterans as well as other relevant findings. We also discuss what these associations have revealed about the mechanisms and pathways underlying both autoimmunity and lymphoma. Finally, we discuss the future directions involving a combination of population and molecular studies that are needed to better define underlying biological mechanisms.
I. Introduction
Lymphoid neoplasms include many different disease entities with distinct cells of origin, pathologies, risk factor profiles, and prognoses1 Immune dysregulation is thought to play a major role in lymphomagenesis as evidenced by the increased risk of certain lymphomas following organ transplant, infections, immunodeficiency states, and autoimmune conditions.2 Autoimmune diseases also comprise a broad variety of conditions characterized by dysregulation in various components of the immune response leading to loss of tolerance to self-antigens. The association of lymphoma and autoimmunity was recognized early on from case reports of autoimmune diseases preceding or co-occurring with lymphoma, and mouse strains showing association of autoimmune disease and lymphoma.3 Over the last three decades, there has been consistent evidence from population-based case-control and cohort studies that certain autoimmune diseases (especially rheumatoid arthritis (RA), Sjögren’s syndrome, and systemic lupus erythematosus (SLE) are associated with an increased risk of developing lymphoma.4 Explanations for these associations include the role of chronic immune stimulation, treatment for autoimmune disease, and shared genetic and/or environmental factors. A unifying model argues that both autoimmunity and lymphomas result from inhibitions (as a result of germline- and somatic mutations) of normal pathways that keep uncontrolled lymphocyte growth in check.5
Large population-based studies of lymphoma patients have revealed patterns of associations that suggest mechanisms for lymphomagenesis. However, studies have been limited by the rarity and heterogeneity of both autoimmune diseases and lymphomas. Additional challenges include the limitation of many studies to patients who were hospitalized due to autoimmune disease, latency of lymphoma development following autoimmune disease, the role of treatment for certain autoimmune diseases, and autoimmunity occurring as a complication of lymphomas.
In this report, we review the current state of knowledge relevant to the associations between autoimmune diseases and lymphomagenesis including our recent studies based on data from Scandinavia and from U.S. Veterans and other relevant literature as well as what these associations imply about the etiology of lymphomas. We also point out gaps in the literature and speculate about future directions for new studies.
II. Associations for specific lymphoid neoplasms
A. Study Designs
Population level associations between autoimmune diseases and lymphomas have been detected by two study designs. A number of studies have assembled cohorts of patients (often from hospital registries) with specific autoimmune diseases and then followed them for the occurrence of cancer using population cancer registries. For example, cohorts of patients with RA, SLE, and Sjögren’s syndrome have consistently shown an increased risk of developing non-Hodgkin lymphoma. A recent meta-analysis of published studies found the pooled odds ratios (OR’s) to be 3.9 (95%CI:2.5–5.9), for RA, 7.4 (95%CI:3.3–17.0) for SLE, and 18.8 (95%CI:9.5–37.3) for Sjögren’s syndrome.4 The advantage of this approach is that large samples of patients affected with autoimmune diseases can be studied although the lymphoma outcomes are rare. Similarly, case-control studies of lymphoma patients have shown an increased risk of lymphomas for individuals who reported a prior history of autoimmune disease. Case-control studies have the advantage of accruing larger numbers of well characterized cancer cases with the disadvantage being that some autoimmune diseases will be rare. Thus, both study designs will have limited power for some comparisons.
We have extended the case-control approach in a series of studies using population-based registry linkages in Sweden and Denmark.6–9 Our methodology has been described in detail in the separate studies. In brief, we assembled very large samples of cases of lymphomas and multiple myeloma from the central Cancer Registries, and then obtained controls from central Population Registries. Using Multigenerational databases, we ascertained first-degree relatives of cases and controls (Table 1). We then linked cases, controls and relatives to the hospital discharge registries and obtained all diagnoses of 32 autoimmune and related diseases. By taking this approach, we were able to survey risk of a large number of autoimmune diseases in very large cohorts of lymphoma cases compared to controls and to assess whether there was evidence of common familial risk of lymphoma and autoimmune diseases. Our large case samples gave us power to detect associations with rare conditions. We examined each condition separately using univariate regression models (Table 2). We also employed hierarchical regression models7, 10 that incorporate knowledge about similar biologic characteristics of autoimmune and related diseases: conditions with detectable autoantibodies and systemic involvement, conditions with detectable autoantibodies and organ involvement, and conditions without detectable autoantibodies. By using multivariate hierarchical regression models, we were able to study the impact of all autoimmune conditions simultaneously, while incorporating information at the group level. This model also corrects for correlations due to multiple autoimmune conditions in the same individual, eases the burden of multiple testing, and increases the precision of risk estimates for rare conditions. Finally, we applied this method to test for the effect of family history of an AI condition on risk of lymphoma. We have also applied a complementary approach to discharge diagnoses among 4 million U.S. Veterans admitted to almost 150 Veterans Administration (VA) hospitals from across the United States.11–13 The results of our studies are summarized below and in Table 2 (results of univariate logistic regression) along with the results of other relevant case-control studies.
Table 1.
Lymphoproliferative malignancies studied (sample sizes)
| Cases (N) | Relatives of Cases (N) | Controls (N) | Relatives of Controls (N) | |
|---|---|---|---|---|
| NHL | 24,728 | 70,006 | 55,632 | 161,352 |
| HL | 7,476 | 23,136 | 18,573 | 63,027 |
| CLL | 7,764 | 17,991 | 16,658 | 39,388 |
| 8,406 | 22,490 | 16,543 | 44,436 |
Table 2.
| Disease | OR (95% CI) | ||||
|---|---|---|---|---|---|
| NHL | HL | CLL | MM | ||
| Systemic w/auto-antibodies | |||||
| Polymyositis/dermatomyositis | 1.3 (0.9–1.8) | 1.7 (0.9–3.4) | 1.6 (0.8–3.0) | 1.4 (.8–2.9) | |
| Rheumatoid arthritis | 1.6 (1.4–1.9) | 2.7 (1.9–4.0) | 1.0 (0.8–1.4) | 0.9 (.7–1.2) | |
| Sjögren’s syndrome | 11.7 (5.7–24) | 4 (p=.02) | 4.0 (0.99–15.8) | 0.8 (.2–4.1) | |
| Systemic lupus erythematosus | 3.3 (2.1–5.3) | 5.8 (2.2–15.1) | 0.8 (0.2–3.2) | 0.9 (.4–2.2) | |
| Systemic sclerosis | 2.0 (1.1–3.8) | 0.6 (.1–6.2) | 2.7 (0.9–8.7) | 0.5 (.2–1.6) | |
| Organ system w/auto-antibodies | |||||
| Addison’s disease | 0.4 (0.1–1.4) | 2.0 (.1–31.3) | 0 | 0.8 (.2–4.1) | |
| Amyotrophic lateral sclerosis | 0.6 (0.3–1.2) | 4 (p=.08) | 0.5 (0.1–2.6) | 0.3 (.1–1.0) | |
| Autoimmune hemolytic anemia | 5.0 (2.5–9.7) | 8.8 (.97–79.5) | 108.4 (15–784)* | 1.3 (.2–8.0) | |
| Chronic rheumatic heart disease | 0.8 (0.6–1.1) | 1.2 (0.5–2.9) | 0.55 (0.3–0.9) | 0.5 (.3–.8) | |
| Discoid lupus erythematosus | 4.1 (1.4–12) | 4 (p=.08) | 0 | 1.0 (.2–5.4) | |
| Grave’s disease | 0.8 (0.4–1.5) | 0.7 (0.2–2.5) | 0.5 (0.1–1.8) | 0.5 (.2–1.6) | |
| Hashimoto’s thyroiditis | 3.0 (1.2–7.5) | 2.0 (0.3–14.0) | 1.1 (0.2–5.9) | 1.5 (.3–6.7) | |
| Immune thrombocytopenic purpura | 2.4 (1.0–5.5) | 4 (p=0.002) | 2.2 (0.6–7.5) | 1.3 (.2–8.0) | |
| Diabetes mellitus type I | 0.4 (0.1–3.3) | 1.4 (0.4–5.5) | - | - | |
| Localized scleroderma | 2.1 (0.5–8.4) | - | - | - | |
| Lupoid hepatitis | 4 (p=.09) | 0 | - | - | |
| Multiple sclerosis | 0.6 (0.4–1.0) | 0.8 (0.3–2.4) | 0.8 (0.4–1.7) | .5 (.2–1.1) | |
| Myasthenia gravis | 2.3 (1.0–5.6) | 0 | 4.8 (0.4–53.) | 2.0 (.3–14.1) | |
| Pernicious anemia | 1.3 (0.9–2.0) | 0.4 (0.1–3.3) | 1.9 (1.2–3.2) | 3.3 (2.2–4.8) | |
| Polyarteritis nodosa | 5.8 (1.5–22) | 4 (p=.08) | 1.9 (0.1–31) | 1.0 (.2–5.4) | |
| Primary biliary cirrhosis | 1.2 (0.5–2.8) | 4 (p=.02) | 0.4 (0.05–3.6) | .9 (.2–3.3) | |
| Wegener’s granulomatosis | 0.8 (0.2–4.1) | 4 (p=.02) | 0 | .4 (.05–3.4) | |
| Auto-antibodies not detectable | |||||
| Ankylosing spondylitis | 1.1 (0.6–1.8) | 0.5 (0.1–2.2) | 1.4 (0.5–4.0) | 1.5 (.7–3.1) | |
| Behcet’s disease | 0 | - | - | - | |
| Chorea minor | - | - | - | - | |
| Crohn’s disease | 2.1 (1.3–3.2) | 1.5 (.6–3.7) | 0.4 (0.1–1.2) | 0.7 (.3–1.7) | |
| Polymyalgia rheumatica | 1.1 (0.8–1.5) | 2.9 (1.1–7.8) | 1.1 (0.6–1.8) | 1.8 (1.2–2.7) | |
| Psoriasis | 1.7 (1.2–2.4) | 1.8 (0.6–4.9) | 0.6 (0.3–1.1) | 1.4 (.8–2.2) | |
| Reiter’s disease | 1.0 (0.3–3.9) | 1.4 (0.1–15.6) | 0 | - | |
| Rheumatic fever | 1.0 (0.5–1.8) | 1.1 (0.3–4.2) | 0.7 (0.2–2.4) | 1.2 (.5–2.7) | |
| Sarcoidosis | 1.9 (1.3–2.7) | 14.1 (5.4–36.8) | 0.9 (0.4–2.1) | 1.4 (.7–2.8) | |
| Ulcerative colitis | 1.3 (0.8–1.9) | 0.8 (0.3–2.5) | 0.9 (0.4–1.9) | 1.2 (.7–2.1) | |
The majority of AIHA cases occurred within a year preceding CLL. If we eliminate these cases, the OR decreases to 47.4 (6.2–364.5).
B. Non-Hodgkin lymphoma
We conducted a study of close to 25,000 cases of non-Hodgkin lymphomas (not including chronic lymphocytic leukemia) diagnosed in Denmark and Sweden, over 55,000 population-based matched controls, and their linkable first-degree relatives. Consistent with previous studies, a personal history of systemic autoimmune conditions was significantly associated with an increased risk of developing non-Hodgkin lymphoma (Table 2). Using the multivariate hierarchical model mentioned above, we found the ORs for separate autoimmune conditions to range from 1.6–5.4 and the overall odds ratio for the group of systemic autoimmune diseases was 2.6 (95%CI:1.7–4.1). A family history of a systemic autoimmune disease was associated with a 1.3-fold (95%CI:0.85–2.0) non-significant risk of non-Hodgkin lymphoma. Furthermore, in the univariate model, several other autoimmune conditions were associated with an elevated risk of non-Hodgkin lymphoma. We observed discoid lupus erythematosus, polyarteritis nodosa, Hashimoto thyroiditis, Crohn’s disease, psoriasis, and sarcoidosis to be associated with an excess non-Hodgkin lymphoma risk. Most of these associations were also found when we restricted the analysis to autoimmune conditions diagnosed 5 or more years before the non-Hodgkin lymphoma diagnosis, making it less likely that the associations were a result of detection bias or reverse causality. Although most of these associations had been previously reported, our study was unique in terms of its sample size, the simultaneous consideration of a large range of autoimmune conditions, and evaluation of the role of having a positive family history of autoimmune disease.
Because non-Hodgkin lymphomas include a collection of diverse lymphoma subtypes, it is important to define the pattern of associations between specific autoimmune diseases and non-Hodgkin lymphoma subtypes. In our study, we did not have detailed information regarding non-Hodgkin lymphoma subtypes. However, for a subset of cases we were able to classify the lymphomas into three major categories based on pathology codes: aggressive (primarily diffuse large B-cell lymphoma), indolent (primarily follicular lymphoma), and T-cell/anaplastic non-Hodgkin lymphomas. Based on this categorization, we found that the associations with systemic autoimmune diseases were stronger for aggressive non-Hodgkin lymphomas. A few recent studies14, 15 have examined autoimmune disease associations by specific lymphoma subtypes based on current WHO classifications.1 In one study, diffuse large B-cell lymphoma was strongly associated with prior RA, SLE, Sjögren’s syndrome, and celiac disease, while there were no associations with follicular lymphoma.15 A subsequent study showed that one particular subtype of diffuse large B-cell lymphomas (activated B-cell) was most strongly associated with RA16. If replicated in future studies, this could be of clinical relevance since the activated B-cell subtype has a poorer prognosis that the more common subtype of diffuse large B-cell lymphomas (germinal center subtype). A pooled analysis in the InterLymph consortium from 12 case-control studies found stronger risks of SLE, Sjögren’s syndrome, and hemolytic anemia in diffuse large B-cell lymphoma compared to follicular lymphoma (where only Sjögren’s syndrome was associated).14 A recent large study including more than 47,000 lymphoma and myeloma patients compared to controls was conducted using a SEER-Medicare database (Anderson et al, submitted). Although the study was limited to individuals over age 65, the large sample size makes this study extremely powerful for detecting risks involving rare conditions. As in the InterLymph study, RA, Sjögren’s syndrome, SLE, and systemic sclerosis were associated with risk of developing diffuse large B-cell lymphomas. For RA there was also a modest association with follicular lymphoma while Sjögren’s syndrome, SLE, celiac disease and pernicious anemia were associated with marginal zone lymphoma. Similarly, in the InterLymph analysis, SLE and Sjögren’s syndrome were associated with marginal zone lymphoma. Furthermore, in the InterLymph study psoriasis and celiac disease were associated with T-cell lymphoma. In the SEER-Medicare study, T-cell lymphoma was associated with RA, SLE, psoriasis, localized scleroderma, discoid lupus erythematosus, Crohn’s disease, and celiac disease
C. Waldenström’s macroglobulinemia and lymphoplasmacytic lymphoma
Waldenström’s macroglobulinemia and lymphoplasmacytic lymphoma are rare subtypes of non-Hodgkin lymphoma and, although not identical, are grouped together in the WHO classification.1 In a large case-control study of non-Hodgkin lymphomas, Smedby et al.15 examined subtypes and among 116 lymphoplasmacytic lymphoma patients, found a significant association with RA. We recently assessed the relationship of autoimmune diseases among 361 U.S. veterans subsequently affected with Waldenström’s macroglobulinemia and found that autoimmune conditions with autoantibodies (both systemic and those with organ involvement) were significantly associated with an increased risk for Waldenström’s macroglobulinemia.12 Specific conditions associated were RA, Sjögren’s syndrome, immune thrombocytopenic purpura, and Crohn’s disease. This pattern is similar to that seen in studies of combined non-Hodgkin lymphoma subtypes.
D. Chronic lymphocytic leukemia
Chronic lymphocytic leukemia (CLL) is classified as a subtype of non-Hodgkin lymphoma and is grouped together with small lymphocytic lymphoma (SLL) in the WHO classification.1 Our registry study of CLL involved 7764 patients, 16,658 matched controls, and first-degree relatives of patients (n = 17,991) and control subjects (n = 39,388) (Table 2)6. Autoimmune hemolytic anemia (AIHA) was strongly associated with CLL but this was only in the time period close to diagnosis which probably reflects the fact that autoimmune hemolytic anemia is often a complication of CLL and CLL is often indolent and not diagnosed in the early stages. The OR is overestimated in the Swedish study but is still substantially elevated if we consider AIHA diagnoses only one or more years before CLL diagnosis (see Table 2 footnote). In our VA study, the OR for AIHA one or more years before CLL was 3.9.13 Similarly, pernicious anemia was also associated with CLL, mainly in the first year after the hospital diagnosis. Chronic rheumatic heart disease was associated with a significantly decreased risk of CLL, particularly persons with a long latency (10+ years) between the 2 conditions. No effect of family history was seen. Smedby et al.15 found type I diabetes associated with CLL/SLL, an association also seen in a pooled InterLymph study. In the SEER-Medicare study, other than AIHA, no other condition was associated among 9171 CLL patients. CLL shows biological and clinical heterogeneity and it is possible that associations with autoimmune disease may be present for some subtype. It has recently been shown that a significant proportion of CLL patients carry stereotyped B-cell receptors suggesting that stimulation by a common antigen (possibly a self-antigen) is important in pathogenesis.17
E. Hodgkin lymphoma
Table 2 shows our analyses of personal history of autoimmune conditions in 7476 Hodgkin lymphoma patients compared to controls.7 Several autoimmune conditions were strongly associated with Hodgkin lymphoma including RA, SLE, sarcoidosis, and immune thrombocytopenic purpura. The risk of Hodgkin lymphoma following Sjögren’s syndrome was elevated but the number of cases was small. In the hierarchical model, we found the overall odds ratio for systemic autoimmune diseases to be 2.7-fold (1.9–3.8) elevated. The risks were similar for young adult (age 15–44 years) and late onset (age >44 years) Hodgkin lymphoma. Associations of RA and SLE were significant 10 or more years prior to Hodgkin lymphoma diagnosis. A family history of sarcoidosis and ulcerative colitis were associated with Hodgkin lymphoma risk. The fact that both personal and family history of sarcoidosis was associated with risk of developing Hodgkin lymphoma suggests a role for shared susceptibility factors between the two diseases. Anderson et al (submitted) found increased risk for RA and SLE in Hodgkin lymphoma patients from the SEER-Medicare study. In addition they found significantly increased risk of Hodgkin lymphoma for localized scleroderma and discoid lupus erythematosus. Consistent with our results from Scandinavia, sarcoidosis was associated with a 3-fold risk with borderline significance. Increased risk of Hodgkin lymphoma as an outcome has been reported among RA18 and SLE cohorts. 19
F. Multiple myeloma
We reported that pernicious anemia and polymyalgia rheumatica were associated with multiple myeloma (MM), with the most prominent risks being within a year of autoimmune disease diagnosis (Table 2).8 Similar to CLL (see above), we found chronic rheumatic heart disease to be associated with a decreased risk of MM. No effect of family history of autoimmune disease was seen. Pernicious anemia was also associated with multiple myeloma in the SEER-Medicare study but no other conditions were associated. Some studies have found increased MM in RA patients20,18 but others have not.21,8 In our study of 4641 black and white U.S. veterans subsequently affected with MM, Brown et al. found MM associated with a prior history of all autoimmune disorders combined (RR=1.15, 1.02–1.28), all systemic autoimmune disorders diseases combined (RR=1.23, 1.09–1.40), and separate conditions, polymyositis/dermatomyositis, systemic sclerosis, autoimmune hemolytic anemia, pernicious anemia, and ankylosing spondylitis.11
G. Monoclonal gammopathy of undetermined significance
Multiple myeloma is usually preceded by the premalignant plasma-cell disorder monoclonal gammopathy of undetermined significance (MGUS). MGUS is defined by a monoclonal immunoglobulin concentrationin serum of 3 g per deciliter or less; the absence of lytic bone lesions, anemia, hypercalcemia, and renal insufficiency related to the proliferation of monoclonal plasma cells; and a proportion of plasma cells in the bone marrow of 10 percent or less.22 On average, MGUS progresses to multiple myeloma at a rate of 1 percent per year23 and those with an IgM MGUS progress more frequently to Waldenstrom’s macroglobulinemia.24 The U.S. Veteran’s study of Brown et al.11 ascertained 2046 patients with MGUS and found similar autoimmune disease associations as in the multiple myeloma sample from the same study. The risk for total autoimmune conditions was 1.67-fold (95%CI:1.47–1.90) increased. For total systemic autoimmune conditions, it was 1.78-fold (95%CI:1.54–206) elevated. This suggests that some autoimmune conditions may act as an early trigger in the pathway to multiple myeloma.
III. Mechanisms explaining association
A. Summary of findings
There is a general consistency in the literature in terms of the specificity of the associations between autoimmune conditions and lymphomas. Diffuse large B-cell lymphomas have been most strongly associated with systemic autoimmune diseases. Marginal zone lymphoma has been associated with both systemic and certain organ specific autoimmune conditions. In addition, mucosa associated lymphoid tissue (MALT) lymphomas have been found to arise following chronic inflammation due to autoimmune or infectious diseases. T-cell lymphomas have been associated with both systemic autoimmune diseases and certain organ specific autoimmune conditions. The more indolent lymphoma subtype, follicular lymphoma, has been only weakly associated with autoimmune disease and the same has been true for CLL which has not been associated with a prior history of systemic autoimmune diseases. In contrast, Waldenström’s macroglobulinemia, a typically indolent lymphoma subtype, has been associated with systemic autoimmune diseases. Hodgkin lymphoma, although considered to be considerably different in etiology, shows similar association with autoimmune diseases as other non-Hodgkin lymphomas. Associations of autoimmune diseases with multiple myeloma have not been consistently found.
B. Possible models
There are several possible mechanisms by which autoimmunity could be related to risk of developing lymphoma25. Dameshek and Schwartz26 originally described the similar proliferative processes of lymphocytes that characterized both autoimmunity and leukemia. In a recent review, Goodnow5 described the pathways and genes likely to be involved in both autoimmune diseases and lymphomas, emphasizing that both types of diseases result as a consequence of multistep processes that eliminate the checkpoints that inhibit uncontrolled B-cell growth, including uncontrolled growth of autoimmune lymphocytes. The multistep processes are likely to involve both inherited and somatic mutations of genes in these pathways. The most prominent example is the finding that somatic and germline Fas mutations are associated with both autoimmune diseases and lymphomas in mice and in humans. These mutations presumably interfere with apoptosis. A recent review article by Hansen et al.27 summarized possible mechanisms for progression of autoimmune diseases to lymphomas, including how specific dysregulation and hyperactivity of B-cells associated with autoimmune diseases and impaired T-cell function may lead to lymphomagenesis. For example, B-cell activating factor of the TNF family (BAFF) enhances survival of B-cells, and is found to be overexpressed in Sjögren’s syndrome, RA, SLE,28, 29 and lymphomas.29, 30 BAFF overexpression is also associated with syndromes similar to SLE and Sjögren’s syndrome in mice transgenic for BAFF. 31
In Figure 1, we show a more complete picture of the major immune-related factors thought to contribute to lymphomagenesis. As described above, autoimmunity may lead to both over-stimulation and defective apoptosis of B-cells. Secondary inflammation due to autoimmune stimulation can also promote these processes which is evident in the continuum of histological changes associated with Sjögren’s syndrome.27 Several infections have been associated with lymphoma development 2, 32–34 35, 36 and are likely to operate through some of the same pathways.
Figure 1.
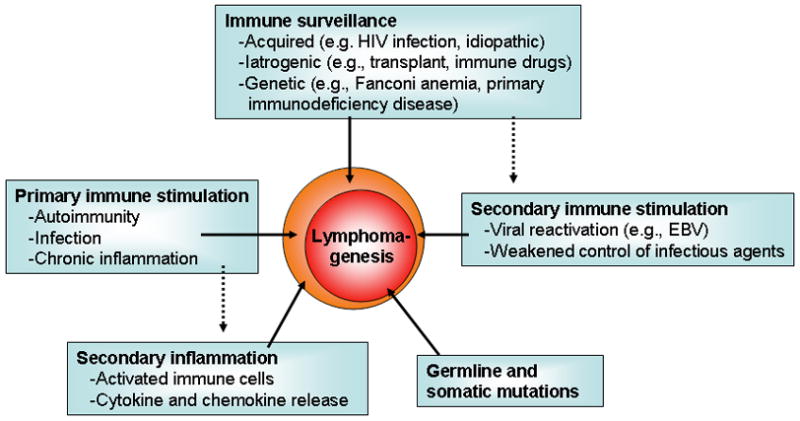
Immune-related factors and their role in lymphomagenesis
In addition to various types of extrinsic factors, genetic factors likely play a role in lymphomagenesis and autoimmunity. There are substantial data demonstrating heritability of autoimmune diseases (e.g.37–40) and lymphomas,41 respectively. Based on these observations, it has been suggested that there could be some inherited mutations causing susceptibility to both autoimmune diseases and lymphomas. One way to test for this hypothesis would be to look for familial aggregation of both autoimmune diseases and lymphomas in families. However, our previous large population-based case-control studies found that family history of autoimmune disease was generally not a predictor of lymphoma risk.6–9 Similarly, a prior study of relatives of RA patients did not find an increased risk of lymphoma.42 While rare mutations (such as those described in the Fas gene) might lead to familial syndromes involving both autoimmunity and lymphoma, common gene mutations or polymorphisms are unlikely to play a prominent role in explaining association.
It is possible that autoimmune disease therapy plays a role in the development of subsequent lymphoma. However, the literature of lymphoma risk following autoimmune therapies (such as methotrexate and TNF-alpha blocking agents) is inconclusive.43–45 Spontaneous lymphoma regression has been reported in RA patients following removal of immunosuppressive therapy, and with methotrexate (MTX) withdrawal used as a primary intervention46, 47 At the same time, it has been reported that lymphomas developing following transplant are more likely to be of more aggressive subtypes, which has been proposed to be attributed to the level of immunosuppression and resulting infection caused by re-activation of Epstein-Barr virus (EBV).48 Overall, the literature on the role of immunosuppression and EBV in RA-related lymphomas is inconsistent 42, 44, 46, 49 One large study found the rate of EBV positivity to be higher in RA associated LPD than in sporadic LPD but no different between MTX and non-MTX LPD in RA patients.50 ew biological therapies blocking TNF-alpha are potent and have advanced the management of RA patients and those with other autoimmune conditions and recent studies have shown monocolonal antibody therapy (such as anti-CD20: “rituximab”) to be effective for treatment of RA.51 Since rituximab is also a treatment for lymphoma, one would not expect an increased risk for subsequent lymphoma development. Nonetheless, careful evaluation at the initiation of the treatment as well as long-term surveillance of the patients receiving different treatments for autoimmune disease will be necessary
IV. Limitations and Future Directions
Our studies and others in the field have yielded new information about the nature of the association between autoimmune diseases and lymphomagenesis. However, some limitations should be noted. The definition of which diseases are autoimmune will likely change over time as our understanding of these processes improves. Given the heterogeneity of both autoimmune diseases and lymphomas, there are many ways that the associations can be analyzed and it is hard to avoid conducting many statistical tests. Our studies and others relied on diagnoses from hospital registries so the numbers will not reflect individuals who were only treated as outpatients and were never hospitalized. In addition, the autoimmune diagnoses were not validated from medical records and the earliest data of diagnosis is not known. Similarly, diagnoses of autoimmune diseases in case-control studies are often based on personal reports.
Autoimmune rheumatic features may occur in the course of lymphoproliferative malignancies, sometimes being the first sign of the malignancy. For these reasons, most studies eliminate the first year after autoimmune diagnosis to minimize the influence of detection bias and reverse causality. In our studies, we attempted to reduce the effects of such paraneoplastic syndromes by excluding the year preceding diagnosis and studied any remaining effect by performing a latency analysis (1–4 years and 5+ years). For example, most of the observed association between AIHA and lymphomas may be a paraneoplastic syndrome, reflected in the the pronounced risk observed within less than five years preceding non-Hodgkin lymphoma and CLL in our studies. This is particularly relevant for CLL where CLL cells have been shown to function as erythrocyte protein antigen presenting cells presumably triggering the autoimmune process against erythrocytes.52, 53 Since CLL and some other lymphomas (like Waldenström’s macroglobulinemia) typically are indolent, it may be hard to determine whether the autoimmune disease preceded the malignancy. Alternatively, it could be that immune-related disorders are reflections of a preceding precursor state on the pathway to full-blown malignancy. A recent small study showed that lymphocytes with a CLL phenotype could be detected by immunophenotyping at a higher rate in AIHA and ITP patients than in normal individuals suggesting that the CLL precursor stage may predispose to AIHA.54 The excess of non-Hodgkin lymphoma and Hodgkin lymphoma after sarcoidosis was highest during this short term period (1–4 years) and thus may partly be due to diagnostic misclassification, if a lymphoma is misinterpreted as a sarcoid granuloma.
Future large studies will be needed that incorporate molecular and laboratory components to validate the diagnoses and produce more biologically homogenous groupings of autoimmune disorders, to examine lymphoma risks using the WHO or even further improved classifications, and to investigate prospectively the natural history and pathogenesis of autoimmune disorders in individuals who subsequently develop lymphomas. For example, studies have identified molecular markers in Sjögren’s syndrome that predict progression to lymphoma.55 The role of autoimmunity on subsequent prognosis and survival of lymphoma needs to be better defined as this may have clinical implications for the treatment of lymphoma patients with autoimmune conditions. In addition to expanding our understanding of etiology and pathogenesis lymphomas, such efforts will help to improve clinical lymphoma management by leading to more informed risk assessments of novel autoimmune drugs which might play roles in lymphomagenesis.
Acknowledgments
This research was supported by the Intramural Research Program of the National Cancer Institute, National Institutes of Health. We thank Dr. Wyndham Wilson (NCI/NIH), for valuable scientific input and help in creating Figure 1.
Footnotes
The authors have no conflict of interest to declare.
References
- 1.Jaffe ES, Harris NL, Stein H, Vardiman JW. Pathology and genetics of tumours of haematopoietic and lymphoid tissues. Lyon Oxford: IARC Press; Oxford University Press (distributor); 2001. [Google Scholar]
- 2.Alexander DD, Mink PJ, Adami HO, Chang ET, Cole P, Mandel JS, Trichopoulos D. The non-Hodgkin lymphomas: a review of the epidemiologic literature. Int J Cancer. 2007(120 Suppl 12):1–39. doi: 10.1002/ijc.22719. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17405121. [DOI] [PubMed]
- 3.Mellors RC. Autoimmune disease in NZB-Bl mice. II. Autoimmunity and malignant lymphoma. Blood. 1966;27(4):435–48. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=5327005. [PubMed]
- 4.Zintzaras E, Voulgarelis M, Moutsopoulos HM. The risk of lymphoma development in autoimmune diseases: a meta-analysis. Arch Intern Med. 2005;165(20):2337–44. doi: 10.1001/archinte.165.20.2337. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16287762. [DOI] [PubMed]
- 5.Goodnow CC. Multistep pathogenesis of autoimmune disease. Cell. 2007;130(1):25–35. doi: 10.1016/j.cell.2007.06.033. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17632054. [DOI] [PubMed]
- 6.Landgren O, Engels EA, Caporaso NE, Gridley G, Mellemkjaer L, Hemminki K, Linet MS, Goldin LR. Patterns of autoimmunity and subsequent chronic lymphocytic leukemia in Nordic countries. Blood. 2006b;108(1):292–6. doi: 10.1182/blood-2005-11-4620. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16527887. [DOI] [PMC free article] [PubMed]
- 7.Landgren O, Engels EA, Pfeiffer RM, Gridley G, Mellemkjaer L, Olsen JH, Kerstann KF, Wheeler W, Hemminki K, Linet MS, Goldin LR. Autoimmunity and susceptibility to Hodgkin lymphoma: a population-based case-control study in Scandinavia. J Natl Cancer Inst. 2006;98(18):1321–30. doi: 10.1093/jnci/djj361. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt= [DOI] [PubMed]
- 8.Landgren O, Linet MS, McMaster ML, Gridley G, Hemminki K, Goldin LR. Familial characteristics of autoimmune and hematologic disorders in 8,406 multiple myeloma patients: a population-based case-control study. Int J Cancer. 2006a;118(12):3095–8. doi: 10.1002/ijc.21745. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt= [DOI] [PubMed]
- 9.Mellemkjaer L, Pfeiffer RM, Engels EA, Gridley G, Wheeler W, Hemminki K, Olsen JH, Dreyer L, Linet MS, Goldin LR, Landgren O. Autoimmune disease in individuals and close family members and susceptibility to non-Hodgkin’s lymphoma. Arthritis Rheum. 2008;58(3):657–66. doi: 10.1002/art.23267. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18311836. [DOI] [PubMed]
- 10.Witte JS, Greenland S, Kim LL, Arab L. Multilevel modeling in epidemiology with GLIMMIX. Epidemiology. 2000;11(6):684–8. doi: 10.1097/00001648-200011000-00012. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11055630. [DOI] [PubMed]
- 11.Brown LM, Gridley G, Check D, Landgren O. Risk of multiple myeloma and monoclonal gammopathy of undetermined significance among white and black male United States veterans with prior autoimmune, infectious, inflammatory, and allergic disorders. Blood. 2008;111(7):3388–94. doi: 10.1182/blood-2007-10-121285. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18239085. [DOI] [PMC free article] [PubMed]
- 12.Koshiol J, Gridley G, Engels EA, McMaster ML, Landgren O. Chronic immune stimulation and subsequent Waldenstrom macroglobulinemia. Arch Intern Med. 2008;168(17):1903–9. doi: 10.1001/archinternmed.2008.4. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18809818. [DOI] [PMC free article] [PubMed]
- 13.Landgren O, Gridley G, Check D, Caporaso NE, Morris Brown L. Acquired immune-related and inflammatory conditions and subsequent chronic lymphocytic leukaemia. Br J Haematol. 2007;139(5):791–8. doi: 10.1111/j.1365-2141.2007.06859.x. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17941950. [DOI] [PubMed]
- 14.Ekstrom Smedby K, Vajdic CM, Falster M, Engels EA, Martinez-Maza O, Turner J, Hjalgrim H, Vineis P, Seniori Costantini A, Bracci PM, Holly EA, Willett E, et al. Autoimmune disorders and risk of non-Hodgkin lymphoma subtypes: a pooled analysis within the InterLymph Consortium. Blood. 2008;111(8):4029–38. doi: 10.1182/blood-2007-10-119974. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18263783. [DOI] [PMC free article] [PubMed]
- 15.Smedby KE, Hjalgrim H, Askling J, Chang ET, Gregersen H, Porwit-MacDonald A, Sundstrom C, Akerman M, Melbye M, Glimelius B, Adami HO. Autoimmune and chronic inflammatory disorders and risk of non-Hodgkin lymphoma by subtype. J Natl Cancer Inst. 2006;98(1):51–60. doi: 10.1093/jnci/djj004. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16391371. [DOI] [PubMed]
- 16.Baecklund E, Backlin C, Iliadou A, Granath F, Ekbom A, Amini RM, Feltelius N, Enblad G, Sundstrom C, Klareskog L, Askling J, Rosenquist R. Characteristics of diffuse large B cell lymphomas in rheumatoid arthritis. Arthritis Rheum. 2006;54(12):3774–81. doi: 10.1002/art.22277. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17133544. [DOI] [PubMed]
- 17.Stamatopoulos K, Belessi C, Moreno C, Boudjograh M, Guida G, Smilevska T, Belhoul L, Stella S, Stavroyianni N, Crespo M, Hadzidimitriou A, Sutton L, et al. Over 20% of patients with chronic lymphocytic leukemia carry stereotyped receptors: Pathogenetic implications and clinical correlations. Blood. 2007;109(1):259–70. doi: 10.1182/blood-2006-03-012948. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16985177. [DOI] [PubMed]
- 18.Mellemkjaer L, Linet MS, Gridley G, Frisch M, Moller H, Olsen JH. Rheumatoid arthritis and cancer risk. Eur J Cancer. 1996;32A(10):1753–7. doi: 10.1016/0959-8049(96)00210-9. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=8983286. [DOI] [PubMed]
- 19.Bernatsky S, Ramsey-Goldman R, Isenberg D, Rahman A, Dooley MA, Sibley J, Boivin JF, Joseph L, Armitage J, Zoma A, Clarke A. Hodgkin’s lymphoma in systemic lupus erythematosus. Rheumatology (Oxford) 2007;46(5):830–2. doi: 10.1093/rheumatology/kel444. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17255135. [DOI] [PubMed]
- 20.Thomas E, Brewster DH, Black RJ, Macfarlane GJ. Risk of malignancy among patients with rheumatic conditions. Int J Cancer. 2000;88(3):497–502. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11054684. [PubMed]
- 21.Gridley G, McLaughlin JK, Ekbom A, Klareskog L, Adami HO, Hacker DG, Hoover R, Fraumeni JF., Jr Incidence of cancer among patients with rheumatoid arthritis. J Natl Cancer Inst. 1993;85(4):307–11. doi: 10.1093/jnci/85.4.307. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=8426374. [DOI] [PubMed]
- 22.Rajkumar SV. MGUS and Smoldering Multiple Myeloma: Update on Pathogenesis, Natural History, and Management. Hematology Am Soc Hematol Educ Program. 2005:340–5. doi: 10.1182/asheducation-2005.1.340. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16304401. [DOI] [PubMed]
- 23.Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF, Melton LJ., 3rd A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med. 2002;346(8):564–9. doi: 10.1056/NEJMoa01133202. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11856795. [DOI] [PubMed]
- 24.Kyle RA, Therneau TM, Rajkumar SV, Remstein ED, Offord JR, Larson DR, Plevak MF, Melton LJ., 3rd Long-term follow-up of IgM monoclonal gammopathy of undetermined significance. Blood. 2003;102(10):3759–64. doi: 10.1182/blood-2003-03-0801. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12881316. [DOI] [PubMed]
- 25.Mackay IR, Rose NR. Autoimmunity and lymphoma: tribulations of B cells. Nat Immunol. 2001;2(9):793–5. doi: 10.1038/ni0901-793. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11526388. [DOI] [PubMed]
- 26.Dameshek W, Schwartz RS. Leukemia and auto-immunization- some possible relationships. Blood. 1959;14:1151–8. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=13813891. [PubMed]
- 27.Hansen A, Lipsky PE, Dorner T. B-cell lymphoproliferation in chronic inflammatory rheumatic diseases. Nat Clin Pract Rheumatol. 2007;3(10):561–9. doi: 10.1038/ncprheum0620. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17906611. [DOI] [PubMed]
- 28.Youinou P. Editorial: Is BAFF the murderer in lupus? Lupus. 2008;17(7):613–4. doi: 10.1177/0961203308092164. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18625632. [DOI] [PubMed]
- 29.Tangye SG, Bryant VL, Cuss AK, Good KL. BAFF, APRIL and human B cell disorders. Semin Immunol. 2006;18(5):305–17. doi: 10.1016/j.smim.2006.04.004. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16916610. [DOI] [PubMed]
- 30.Mackay F, Tangye SG. The role of the BAFF/APRIL system in B cell homeostasis and lymphoid cancers. Curr Opin Pharmacol. 2004;4(4):347–54. doi: 10.1016/j.coph.2004.02.009. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15251127. [DOI] [PubMed]
- 31.Groom J, Kalled SL, Cutler AH, Olson C, Woodcock SA, Schneider P, Tschopp J, Cachero TG, Batten M, Wheway J, Mauri D, Cavill D, et al. Association of BAFF/BLyS overexpression and altered B cell differentiation with Sjogren’s syndrome. J Clin Invest. 2002;109(1):59–68. doi: 10.1172/JCI14121. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11781351. [DOI] [PMC free article] [PubMed]
- 32.Giordano TP, Henderson L, Landgren O, Chiao EY, Kramer JR, El-Serag H, Engels EA. Risk of non-Hodgkin lymphoma and lymphoproliferative precursor diseases in US veterans with hepatitis C virus. Jama. 2007;297(18):2010–7. doi: 10.1001/jama.297.18.2010. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17488966. [DOI] [PubMed]
- 33.Landgren O, Rapkin JS, Caporaso NE, Mellemkjaer L, Gridley G, Goldin LR, Engels EA. Respiratory tract infections and subsequent risk of chronic lymphocytic leukemia. Blood. 2007;109(5):2198–201. doi: 10.1182/blood-2006-08-044008. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17082317. [DOI] [PMC free article] [PubMed]
- 34.Landgren O, Rapkin JS, Mellemkjaer L, Gridley G, Goldin LR, Engels EA. Respiratory tract infections in the pathway to multiple myeloma: a population-based study in Scandinavia. Haematologica. 2006;91(12):1697–700. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17145609. [PubMed]
- 35.Engels EA. Infectious agents as causes of non-Hodgkin lymphoma. Cancer Epidemiol Biomarkers Prev. 2007;16(3):401–4. doi: 10.1158/1055-9965.EPI-06-1056. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17337646. [DOI] [PubMed]
- 36.Engels EA, Chatterjee N, Cerhan JR, Davis S, Cozen W, Severson RK, Whitby D, Colt JS, Hartge P. Hepatitis C virus infection and non-Hodgkin lymphoma: results of the NCI-SEER multi-center case-control study. Int J Cancer. 2004;111(1):76–80. doi: 10.1002/ijc.20021. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15185346. [DOI] [PubMed]
- 37.Anaya JM, Delgado-Vega AM, Castiblanco J. Genetic basis of Sjogren’s syndrome. How strong is the evidence? Clin Dev Immunol. 2006;13(2–4):209–22. doi: 10.1080/17402520600876911. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17162364. [DOI] [PMC free article] [PubMed]
- 38.Anaya JM, Gomez L, Castiblanco J. Is there a common genetic basis for autoimmune diseases? Clin Dev Immunol. 2006;13(2–4):185–95. doi: 10.1080/17402520600876762. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17162361. [DOI] [PMC free article] [PubMed]
- 39.Bowes J, Barton A. Recent advances in the genetics of RA susceptibility. Rheumatology (Oxford) 2008;47(4):399–402. doi: 10.1093/rheumatology/ken005. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18263596. [DOI] [PubMed]
- 40.Harley JB, Kelly JA, Kaufman KM. Unraveling the genetics of systemic lupus erythematosus. Springer Semin Immunopathol. 2006;28(2):119–30. doi: 10.1007/s00281-006-0040-5. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17021721. [DOI] [PubMed]
- 41.Goldin LR, Caporaso NE. Family studies in chronic lymphocytic leukaemia and other lymphoproliferative tumours. Br J Haematol. 2007;139(5):774–9. doi: 10.1111/j.1365-2141.2007.06810.x. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18021091. [DOI] [PubMed]
- 42.Ekstrom K, Hjalgrim H, Brandt L, Baecklund E, Klareskog L, Ekbom A, Askling J. Risk of malignant lymphomas in patients with rheumatoid arthritis and in their first-degree relatives. Arthritis Rheum. 2003;48(4):963–70. doi: 10.1002/art.10939. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12687538. [DOI] [PubMed]
- 43.Hakulinen T, Isomaki H, Knekt P. Rheumatoid arthritis and cancer studies based on linking nationwide registries in Finland. Am J Med. 1985;78(1A):29–32. doi: 10.1016/0002-9343(85)90242-6. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=3970037. [DOI] [PubMed]
- 44.Mariette X, Cazals-Hatem D, Warszawki J, Liote F, Balandraud N, Sibilia J. Lymphomas in rheumatoid arthritis patients treated with methotrexate: a 3-year prospective study in France. Blood. 2002;99(11):3909–15. doi: 10.1182/blood.v99.11.3909. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12010788. [DOI] [PubMed]
- 45.Toussirot E, Wendling D. The use of TNF-alpha blocking agents in rheumatoid arthritis: an update. Expert Opin Pharmacother. 2007;8(13):2089–107. doi: 10.1517/14656566.8.13.2089. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17714062. [DOI] [PubMed]
- 46.Salloum E, Cooper DL, Howe G, Lacy J, Tallini G, Crouch J, Schultz M, Murren J. Spontaneous regression of lymphoproliferative disorders in patients treated with methotrexate for rheumatoid arthritis and other rheumatic diseases. J Clin Oncol. 1996;14(6):1943–9. doi: 10.1200/JCO.1996.14.6.1943. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=8656264. [DOI] [PubMed]
- 47.Usman AR, Yunus MB. Non-Hodgkin’s lymphoma in patients with rheumatoid arthritis treated with low dose methotrexate. J Rheumatol. 1996;23(6):1095–7. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=8782146. [PubMed]
- 48.Nalesnik MA, Jaffe R, Starzl TE, Demetris AJ, Porter K, Burnham JA, Makowka L, Ho M, Locker J. The pathology of posttransplant lymphoproliferative disorders occurring in the setting of cyclosporine A-prednisone immunosuppression. Am J Pathol. 1988;133(1):173–92. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=2845789. [PMC free article] [PubMed]
- 49.Dawson TM, Starkebaum G, Wood BL, Willkens RF, Gown AM. Epstein-Barr virus, methotrexate, and lymphoma in patients with rheumatoid arthritis and primary Sjogren’s syndrome: case series. J Rheumatol. 2001;28(1):47–53. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11196542. [PubMed]
- 50.Hoshida Y, Xu JX, Fujita S, Nakamichi I, Ikeda J, Tomita Y, Nakatsuka S, Tamaru J, Iizuka A, Takeuchi T, Aozasa K. Lymphoproliferative disorders in rheumatoid arthritis: clinicopathological analysis of 76 cases in relation to methotrexate medication. J Rheumatol. 2007;34(2):322–31. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17117491. [PubMed]
- 51.Mease PJ. B cell-targeted therapy in autoimmune disease: rationale, mechanisms, and clinical application. J Rheumatol. 2008;35(7):1245–55. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18609733. [PubMed]
- 52.Galletti J, Canones C, Morande P, Borge M, Oppezzo P, Geffner J, Bezares R, Gamberale R, Giordano M. Chronic lymphocytic leukemia cells bind and present the erythrocyte protein band 3: possible role as initiators of autoimmune hemolytic anemia. J Immunol. 2008;181(5):3674–83. doi: 10.4049/jimmunol.181.5.3674. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18714043. [DOI] [PubMed]
- 53.Hall AM, Vickers MA, McLeod E, Barker RN. Rh autoantigen presentation to helper T cells in chronic lymphocytic leukemia by malignant B cells. Blood. 2005;105(5):2007–15. doi: 10.1182/blood-2003-10-3563. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15284121. [DOI] [PubMed]
- 54.Mittal S, Blaylock MG, Culligan DJ, Barker RN, Vickers MA. A high rate of CLL phenotype lymphocytes in autoimmune hemolytic anemia and immune thrombocytopenic purpura. Haematologica. 2008;93(1):151–2. doi: 10.3324/haematol.11822. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18166805. [DOI] [PubMed]
- 55.Voulgarelis M, Skopouli FN. Clinical, immunologic, and molecular factors predicting lymphoma development in Sjogren’s syndrome patients. Clin Rev Allergy Immunol. 2007;32(3):265–74. doi: 10.1007/s12016-007-8001-x. Available from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17992593. [DOI] [PubMed]


