Abstract
Guyon's canal at the wrist is not the common site of ulnar nerve compression. Ganglion, lipoma, anomalous tendon and muscles, trauma related to an occupation, arthritis, and carpal bone fracture can cause ulnar nerve compression at the wrist. However, ulnar nerve compression at Guyon's canal by vascular lesion is rare. Ulnar artery aneurysm, tortous ulnar artery, hemangioma, and thrombosis have been reported in the literature as vascular lesions. The authors experienced a case of ulnar nerve compression at Guyon's canal by an arteriovenous malformation (AVM) and the patient's symptom was improved after surgical resection. We can not easily predict vascular lesion as a cause of ulnar nerve compression at Guyon's canal. However, if there is not obvious etiology, we should consider vascular lesion as another possible etiology.
Keywords: Ulnar nerve, Arteriovenous malformation
INTRODUCTION
Guyon's canal, a fibro-osseous space within the proximal part of the hypothenar eminence between pisiform and hook of the hamate, was first described by Felix Guyon in 18611,2,4). It is covered proximally by the palmar carpal ligament and distally by the fibrous arch of the short palmar muscles4). In Guyon's canal, ulnar nerve is vulnerable to external compression and patient's clinical presentation is different according to the lesion involvement site1-3,4,11). Numerous lesions have been reported in the literature as causes of ulnar nerve compression at Guyon's canal but vascular lesion is rarely described in the literature4,5,7).
This report presents a rare case of ulnar nerve compression at Guyon's canal by an arteriovenous malformation (AVM).
CASE REPORT
A 60-year-old female presented with 2-year history of tingling sensation of fourth and fifth digit in her right hand. She had 5-year history of diabetes mellitus but the possibility of diabetic neuropathy was excluded by examination of Semmes-Weinstein monofilament test and vibration perception test in the diabetic department. Other past medical history was unremarkable. Clinical examination revealed paresthesia and hypesthesia of the fifth digit and medial region of the fourth digit. Hypothenar atrophy and weakness of the hypothenar muscles were not noticed.
Sensory conduction study of right ulnar nerve was normal, but motor conduction study of right ulnar nerve from the elbow and wrist to the abductor digiti minimi (ADM) muscle revealed a small amplitude. Needle electromyography (EMG) showed abnormal spontaneous activity in the right first dorsal interosseous (FDI) muscle. There was no abnormal spontaneous activity in the flexor carpi ulnaris. These electrophysiologic findings were consistent with ulnar nerve lesion at or around the wrist. Magnetic resonance imaging (MRI) was not performed because of strong suggestion of ulnar nerve compression at the wrist by clinical presentation and electrophysiological studies.
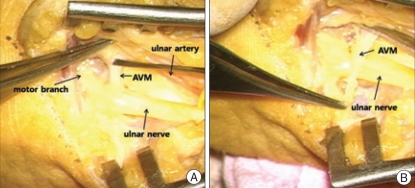
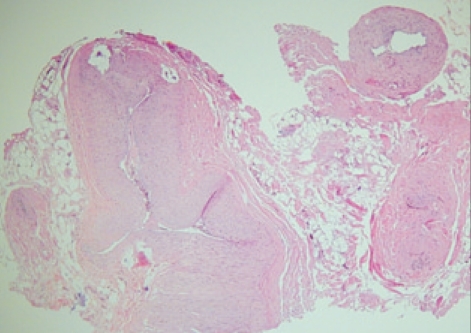
Under the diagnosis of ulnar nerve compression at the wrist, Guyon's canal decompression was carried out under general anesthesia. Under the microscopic magnification, ulnar nerve was compressed by an arteriovenous malformation originating from ulnar artery and vein and it was excised (Fig. 1). Histologic examination demonstrated the features of AVM (Fig. 2). After operation, the patient's symptom was improved immediately and she was discharged at the 3rd postoperative day. After 3 months postoperatively, repeated electrophysiologic examination revealed recovery of right ulnar nerve with increased amplitude of ADM muscle in motor conduction study.
Fig. 1.
Intraoperative photographs showing the ulnar nerve and anomalous vascular structure at Guyon's canal, (A) and the resection of arteriovenous malformation arising from the ulnar vessels crossing the ulnar nerve (B).
Fig. 2.
Photomicrograph demonstrating various sized arteries and veins (H & E stain, original magnification×200).
DISCUSSION
The most common site of ulnar nerve compression is the elbow3,8). Fibro-osseous space known as Guyon's canal at the wrist is rare site of ulnar nerve compression3,8). The etiology of ulnar nerve compression at the wrist includes ganglion, lipoma, vascular anomalies, carpal bone fractures, ulnar artery disease, anomalous tendon and muscles, and trauma related to an occupation1-5,7). Among them, ganglion is the most common cause3,5,7,11).
The symptom and signs are determined by the location of the lesion with respect to the various portion of the nerve1,3,9,10). Subsequently, knowledge of distal ulnar nerve is important. At Guyon's canal, ulnar nerve divides into a superficial sensory branch and a deep motor branch2,3). Superficial sensory branch supplies to the skin of the hypothenar eminence and the surface of the fifth digit and medial region of the fourth digit. Deep motor branch turn radially around the hook of hamate bone and pass under a fibro-tendinous arch called the pisoharmate hiatus, innervates to hypothenar muscles including ADM muscle, dorsal interossei, third and fourth lumbricals, adductor pollicis (AP), and the FDI muscles2,3).
According to anatomical location, Shea and McClain classified ulnar nerve lesion into three types9). Type I is the motor and sensory abnormalities with the lesion of Guyon's canal or proximal to it (30%). Type II is the motor abnormalities with weakness of the intrinsic muscle (52%). Type III is the sensory abnormalities on the palmar surface of the hypothenar eminence and in the fourth and fifth digit (18%). Recently, Wu et al.10) suggested reclassification of ulnar nerve lesion into five types clinicoanatomically. Type I is a mixed motor and sensory neuropathy with the lesion just proximal or within the proximal end of Guyon's canal. Type II is a pure sensory neuropathy, with only the lesion of sensory branch. Type III is a pure motor neuropathy, with the lesion of deep motor branch just distal to the superficial sensory branch but proximal to the branch supplying the hypothenar muscles. Type IV is a pure motor neuropathy with sparing of hypothenar muscles with the lesion distal to the origin of both the superficial branch and the branch going to the hypothenar muscles. Type V is a pure distal motor neuropathy with the lesion affect only the branches to the FDI and AP muscles. Our case corresponds to type I by Shea and McClain classification and type I by Wu classification.
Under clinical suspicion, electrophysiologic studies are essential to confirm of diagnosis and location of ulnar nerve compression1,8). If the symptom and physical findings are uncertain, magnetic resonance imaging (MRI) can be used as an another diagnostic tool1,3).
Although many causative lesions of ulnar nerve compression at the Guyon's canal have been reported in the literature, vascular lesion is rare. Some authors have reported ulnar artery aneurysm, tortous ulnar artery, hemangioma, and thrombosis as vascular lesion of ulnar nerve compression at wrist4,5,11). Ozdemir et al.7) reported ulnar nerve compression by an AVM, it was similar with our case. In their report, ulnar nerve edema by chronic pressure, alteration of microcirculation, ischemia, and fibrosis of ulnar nerve was proposed as pathomechanism.
CONCLUSION
We report a rare case of ulnar nerve compression at Guyon's canal by an AVM. Although many etiologies may cause ulnar nerve compression at the wrist, vascular lesion should be considered as another possible etiology.
References
- 1.Aguiar PH, Bor-Seng-Shu E, Gomes-Pinto F, Almeida-Leme RJ, Freitas AB, Martins RS, et al. Surgical management of Guyon's canal syndrome, an ulnar nerve entrapment at the wrist : report of two cases. Arq Neuropsiquiatr. 2001;59:106–111. doi: 10.1590/s0004-282x2001000100022. [DOI] [PubMed] [Google Scholar]
- 2.Bozkurt MC, Tagil SM, Ozçakar L, Ersoy M, Tekdemir I. Anatomical variations as potential risk factors for ulnar tunnel syndrome : a cadaveric study. Clin Anat. 2005;18:274–280. doi: 10.1002/ca.20107. [DOI] [PubMed] [Google Scholar]
- 3.Erkin G, Uysal H, Keles I, Aybay C, Ozel S. Acute ulnar neuropathy at the wrist : a case report and review of the literature. Rheumatol Int. 2006;27:191–196. doi: 10.1007/s00296-006-0166-8. [DOI] [PubMed] [Google Scholar]
- 4.Jose RM, Bragg T, Srivastava S. Ulnar nerve compression in Guyon's canal in the presence of a tortuous ulnar artery. J Hand Surg Br. 2006;31:200–202. doi: 10.1016/j.jhsb.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Koch H, Haas F, Pierer G. Ulnar nerve compression in Guyon's canal due to a haemangioma of the ulnar artery. J Hand Surg Br. 1998;23:242–244. doi: 10.1016/s0266-7681(98)80185-x. [DOI] [PubMed] [Google Scholar]
- 6.Lindsey JT, Watumull D. Anatomic study of the ulnar nerve and related vascular anatomy at Guyon's canal : a practical classification system. J Hand Surg Am. 1996;21:626–633. doi: 10.1016/S0363-5023(96)80016-5. [DOI] [PubMed] [Google Scholar]
- 7.Ozdemir O, Calisaneller T, Altinors N. Compression of the ulnar nerve in Guyon's canal by an arteriovenous malformation. J Hand Surg Eur. 2007;32:600–601. doi: 10.1016/J.JHSE.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Papathanasiou ES, Loizides A, Panayiotou P, Papacostas SS, Kleopa KA. Ulnar neuropathy at Guyon's canal : electrophysiological and surgical findings. Electromyogr Clin Neurophysiol. 2005;45:87–92. [PubMed] [Google Scholar]
- 9.Shea JD, McClain EJ. Ulnar-nerve compression syndromes at and below the wrist. J Bone Joint Surg Am. 1969;51:1095–1103. [PubMed] [Google Scholar]
- 10.Wu JS, Morris JD, Hogan GR. Ulnar neuropathy at the wrist : case report and review of literature. Arch Phys Med Rehabil. 1985;66:785–788. [PubMed] [Google Scholar]
- 11.Yoshii S, Ikeda K, Murakami H. Ulnar nerve compression secondary to ulnar artery true aneurysm at Guyon's canal. J Neurosurg Sci. 1999;43:295–297. [PubMed] [Google Scholar]