Abstract
Purpose
The aim of the study was to evaluate the effect of phosphorus-32 colloid ([32P]) intracavitary irradiation on the treatment of patients with cystic craniopharyngiomas.
Methods
Twenty patients with predominantly cystic craniopharyngiomas were admitted from 1981 to 2006. Eleven patients had [32P] intracavitary irradiation by stereotactic injection or Ommaya cyst instillation as the primary treatment, and the remaining nine had the same internal irradiation as an adjuvant treatment after tumor resection. A calculated irradiation dose of 400~500 Gy per once was delivered to the cyst wall.
Conclusion
The patients were followed up ranging from 36 to 336 months; no operative morbidity or mortality was found from [32P] intracavitary irradiation. Fourteen patients (70%) had tumor progression and required further two to four times intracavitary irradiation. All 20 cases achieved tumor shrinkage or stabilization with effective outcome 3–6 months after the last [32P] therapy. For patients with cystic craniopharyngioma, [32P] administration by stereo-tactic injection or Ommaya cyst instillation is a safe and helpful option, which could improve the life quality, prolong the life span, and enhance the survival rate of cystic craniopharyngioma patients.
Keywords: Craniopharyngioma, Intracavitary irradiation, 32P colloid, Stereotactic radiosurgery
Introduction
Craniopharyngiomas account for 5.6–15% of the intracranial tumors in children with peak incidence rates at the age of 5–14 years [1]. Despite the benign appearance, their clinical behavior is aggressive, causing serious morbidity by damaging the optic chiasm, the pituitary, and hypothalamic area [2]. Since Leksell and Liden had firstly reported a minimally invasive management strategy of intracavitary irradiation with radioisotopes (brachytherapy) in 1952 [3], several radiotherapeutic modalities have been advocated for treating craniopharyngiomas [4–8], and phosphorus-32 colloid ([32P]) has been considered as the optimal choice for treating cystic craniopharyngioma among the therapeutic radioactive isotopes in treating cystic brain tumor. However, previous studies demonstrated that the radiation dose (about 90–300 Gy) of [32P] was not adequate for effective treatment [5, 6], and the follow-up period of [32P] therapy did not exceed 12–23 years although it is not short [5, 8, 9]. Therefore, we suggested that increasing the radiation dose with multiple administration of [32P] would be a more effective alternative to the past treatment. In 1981, a 3-year-old girl with cystic craniopharyngioma was admitted to our hospital, and the patient underwent four times of [32P] intracavitary irradiation therapy during a 4-month period. Excellent response, with the shrinkage of the cyst and relaxation of the symptoms, was observed 6 months later after the fourth [32P] irradiation, and there was no obvious recurrence till 2009. She had celebrated her 31st birthday in March 2009. Encouraged by this successful case, from 1984 to 2006, we conducted intracavitary instillation of [32P] for 43 times to another 19 children suffering cystic craniopharyngiomas. This report summarizes the 3–28-year follow-up results of these 20 patients with pediatric cystic craniopharyngiomas.
Materials and methods
From 1981 to 2006, 20 children (12 boys and eight girls) were admitted to Xijing Hospital for primary treatment of craniopharyngioma. The diagnosis was all confirmed by computed tomography (CT) or magnetic resonance imaging (MRI) as having predominantly cystic craniopharyngiomas. Twelve boys aged between 1.7 and 9.0 (median 6.5)years, and eight girls aged between 3.1 and 7.5 (median 4.5)years at the time of diagnosis. The median volume of cysts of 20 cases was 28.7 ml (range 14.1 to 44.6 ml). Among them, nine cases were treated by neurosurgical subtotal resection plus [32P] treatment, and the other 11 patients received intracavitary [32P] radiotherapy followed by craniotomy but not tumor resection. The [32P] injection was performed via an Ommaya reservoir system that had been placed to the tumor cyst at craniotomy or a stereotactic injection technique (the later technique was only in the first case in 1981). Clinical characteristics are detailed in Table 1.
Table 1.
Characteristics of the craniopharyngioma patients (total number of patients=20)
| No. of patients (%) | |
|---|---|
| Characteristics of the craniopharyngioma patients | |
| Age at diagnosis (years) | 6.2±3.66 |
| Gender (male/female) | 12/8 |
| Tumor resection only | 0 |
| Brachytherapy with 32P only | 11 (55) |
| Tumor resection + brachytherapy | 9 (45) |
| Symptoms/signs before treatment | |
| Headache and vomiting | 20 (100) |
| Growth retardation | 15 (75) |
| Obesity | 12 (60) |
| Hypothyroidism | 15 (75) |
| Hypocortisolism | 14 (70) |
| Diabetes insipidus | 3 (15) |
Administration of [32P] and its dosimetry
The [32P] was provided by China Institute of Atomic Energy. In order to complete control the cyst, the therapy dose of [32P] activity was increased up to two to 2.5 times in this study compare with Loevinger's study [10]. According to the Table 1 of Taasan et al. [11], the corresponding volume (milliliters) of cyst was calculated by diameter (centimeters) measured with CT or MRI, and then the 32P activity of every case in this study was obtained. The activity of [32P] to be injected is in the range of 400–500 Gy per once.
Procedure of therapy
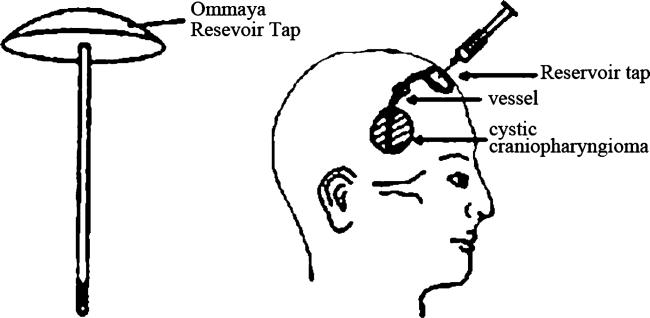
Firstly, the cyst fluid of patients was aspirated through the aspirate needle positioned in the tap of Ommaya reservoir, then the craniopharyngioma cyst was washed, and finally, [32P] (5.0~7.3 mCi/5–6 ml/each time) were given via the Ommaya reservoir system (Fig. 1). The patients were informed to turn over the head again and again to assume that [32P] inside the tumor cyst distributed uniformly. The characteristics of the craniopharyngioma patients and radiation times are detailed in Tables 1 and 2, respectively.
Fig. 1.
Pattern of Ommaya reservoir system
Table 2.
The intracavitary irradiation times with [32P]
| Times of [32P] instillation | No. of patients |
|---|---|
| Once | 6 |
| Twice | 5 |
| Three | 5 |
| Four | 4 |
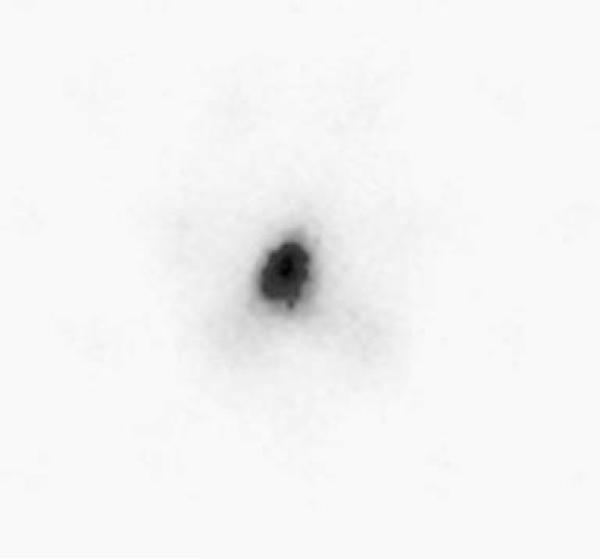
In order to determine whether there is any possible leakage of the [32P] to the outside of the target cyst, bremsstrahlung scanning of the target cyst was done by single photon emission computed tomography (SPECT) equipment in intervals up to the third day of postinstillation.
Clinical follow-up visit lasted for 36–336 months (median 47.7 months). The shrinkage of the cyst and relaxation of symptoms/signs were both taken into consideration for evaluating the effectiveness of the treatment. The efficacy was regarded as being “significantly effective” if the cyst size was considerably shrunk referred to the WHO standard [12] and symptoms/signs were alleviated obviously.
The treatment protocol and procedure described above have been approved by the ethical committee of Fourth Military Medical University.
Results
There was no mortality or morbidity in 20 patients with [32P] intracavitary irradiation. The symptoms and signs of most patients were alleviated obviously within 3–6 months after therapy. Their treatment results are summarized in Tables 3 and 4.
Table 3.
Assessment of the pituitary hormones pre- and posttherapy in patients with craniopharyngioma (abnormal no./total no. in measurement)
| GH deficiency | ACTH deficiency | TSH deficiency | Hyperprolactinemia | |
|---|---|---|---|---|
| Pretherapy | 14/20 (70%) | 14/18 (78%) | 15/20 (75%) | 7/20 (35%) |
| Posttherapy | 14/20 (70%) | 11/18 (61%) | 10/20 (50%) | 10/20 (50%) |
Table 4.
Results of intracystic therapy with [32P]
| Symptoms/signs before treatment (n) | Symptoms and signs at follow-up after the last therapy |
|||
|---|---|---|---|---|
| No change | Alleviated | Absent | Worsening | |
| Headache and vomiting (20) | 0 | 5 | 15 | 0 |
| Visual disturbances (20) | 5 | 13 | 1 | 1 |
| Growth retardation(15) | 0 | 10 | 5 | 0 |
| Diabetes insipidus (3) | 1 | 2 | 0 | 0 |
| Obesity (12) | 10 | 1 | 1 | 0 |
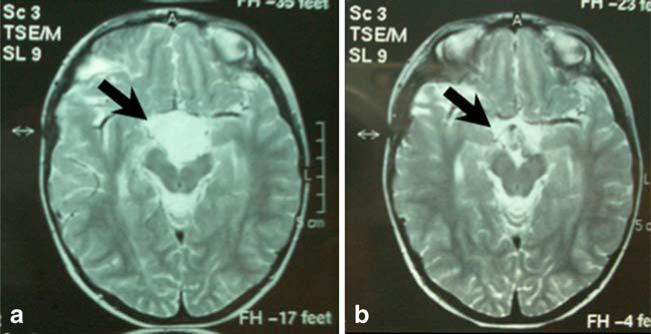
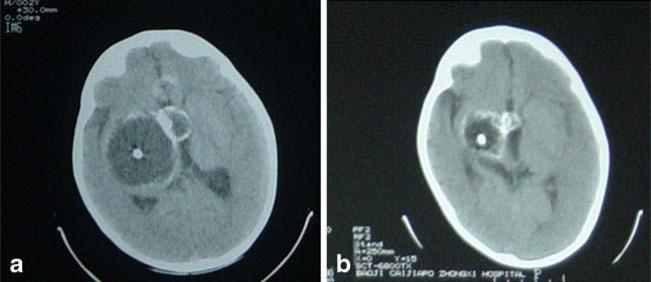
During a median follow-up of 47.7 months, out of 20 cases, 18 (90%) of the cysts decreased more than 50% in size, and the mean of maximum diameter of cyst decreased from 3.8 cm before treatment to 1.2 cm (13 cases) or 1.8 cm (five cases), respectively. For example, case 2 and case 3 were indicated considerable shrinkage after 6 months of last [32P] therapy with MRI as shown in Figs. 2 and 3. Both target cysts were positive by bremsstrahlung SPECT scanning; however, no bremsstrahlung image was detected outside the target cyst up to the third day of [32P] postinstillation (Fig. 4).
Fig. 2.
Case 2: MRI of cystic craniopharyngioma in a 5-year-old boy before (a cyst diameter≈3.8 cm) and after (b cyst diameter≈1.2 cm) [32P] treatment
Fig. 3.
Case 3: MRI of cystic craniopharyngioma in a 1.7-year-old boy before (a cyst diameter≈4.4 cm) and after (b cyst diameter≈1.5 cm) [32P] treatment
Fig. 4.
Case 2: The bremsstrahlung scanning of cystic craniopharyngioma in a 5-year-old boy treated with intracavitary [32P] in intervals up to the third day of postinstillation: It is never presented the bremsstrahlung image outside the target cyst
Discussion
Cystic craniopharyngiomas are frequently considered inoperable due to extensive local attachment of cyst wall to adjacent vital structures, and it was easy for the surgeon to lose contact with the extremely thin sinus cyst wall, which later resulted in tumor recurrence. So today, there are strong advocated of good local control for both radical surgical resection and limited surgery followed by postoperative radiotherapy [13, 14]. When a patient presents with a purely cystic craniopharyngioma, the management options include the stereotactic placement of a catheter to allow repeated aspiration and furthermore intracystic irradiation with radionuclide (32P or 90Y, etc.) [5, 7, 15, 16]. In 1952, Leksell and Liden reported the effects of intracavitary irradiation for craniopharyngioma primarily [3]. Up to now, more than thousand craniopharyngioma patients were treated by radiosurgery and radionuclide intracavitary irradiation methods. Although there have been no controlled comparative studies, the latter approach offers the maximum chance of local control with minimal morbidity and has become the preferred treatment method in many countries [1]. Intracavitary irradiation is a minimally invasive management strategy of instillation of radionuclide (such as [32P]) into cystic craniopharyngioma, which could deliver higher dose of radiation directly into the inner surface of the cyst than to tumor's adjacent tissue offered by conventional external beam radiotherapy. The beneficial effect is achieved through destruction of the secretory epithelial lining, causing elimination of fluid production and cyst shrinkage. In view of the reduced surgical morbidity and mortality, the brachytherapy became an attractive management option for predominantly cystic (and particularly monocystic) tumors [1].
The severity of symptoms and signs in children patients is directly related to the tumor's size, position, and affected area, but no age-related differences were found. The main symptoms and signs result from the increased intracranial pressure, abnormal neural and/or mental behavior, visual disturbance, and disturbance of endocrine function due to hypopituitarism. The 20 cases reported in this paper complained all but not very severe symptoms and signs (Table 1); this may be mainly due to the patients’ young age (1.7–9.0 years old) and hence smaller tumor size.
In previous reports [5, 6, 16, 17], the dose delivered to target cyst was within the range of 90–300 Gy. In order to enhance the therapeutic efficiency, the radiation dose in our studies was increased to 400–500 Gy. In addition, we arranged two to four times (5.0~7.3 mCi/5–6 ml/each time) instillation of [32P] to cyst of 14 cases (Table 2), so the total radioactivity of [32P] injected was within the range of 10–20 mCi in this group. In the present cases, there was no development of adverse reactions or any damages. Because [32P] is a pure beta-emitting radionuclide with an ideal mean energy of 0.69 MeV, the maximum range of these beta particles in soft tissue is 7.9 mm, and less than 50% of the given dose penetrates beyond 0.8 mm [5]. Even with these ideal physical characteristics of the [32P] source, critical and radiosensitive structures, such as optic chiasm and cavernous sinus, etc., should be monitored intensively during the treatment planning stage in order to prevent accidental overdosage.
Prognosis and quality of life
Our results presented that the predominant therapeutic efficiency may be due to the addition of radiation doses and multiple instillation of [32P]. Since there has been no method for “complete cure of craniopharyngiomas”, current treatment methods can only shrink the size of the tumor and alleviate the symptoms. The survival prognosis of patients treated by [32P] brachytherapy for craniopharyngioma is favorable, and the overall survival rate is up to 95% at 5 years [18] and 10-year survival rate is approximately 80% in children [17]. Our report demonstrated a 5-year survival rate of approximately 100% in children with craniopharyngioma.
However, with the progress of neurosurgery and nuclear medicine treatment methods, it is expected that the recurrence rate should be reduced and survival period extended. Smaller solid craniopharyngiomas are usually treated by γ or X knife therapy, whereas for large solid craniopharyngiomas, the 125I particle knife therapy is often used. The latter method is a brachytherapy that makes use of the released radiation from inserted 125I particles. Considering that any surgery has high risk factor [19] and approximately 60% of craniopharyngiomas occur in the form of a single large cyst [20], intracyst injection of [32P] for treating cystic craniopharyngiomas has been widely accepted today [21, 22]. Although surgeons also rely on the [32P] therapy to treat cystic brain tumor, there has been no any systematic study with large samples comparing [32P] therapy alone with combined treatment by surgery first and followed by [32P].
Based on our experience, we would recommend the following good practices: Firstly, resect the craniopharyngiomas and then perform intracystic injection of [32P] via Ommaya reservoir. The latter treatment is an internal radiation method; therefore, the radioactivity of [32P] should be carefully selected in order to achieve a safe yet effective treatment and also reduce the occurrence of radiation accidents. This method is less invasive, effective, safe, economical, and easy to perform and thus can be conducted at the outpatient department by a qualified nuclear medicine doctor.
We recommend that intracavitary irradiation therapy using [32P] should be the primary method of treating monocystic craniopharyngioma. In the future, to popularize earlier application of stereotactic techniques may further reduce the unacceptable morbidity and mortality associated with radical surgical resection of craniopharyngioma.
Acknowledgments
The authors acknowledge the cooperation and assistance of Professor Weiping Liu and Professor Yi Wang, Department of Neurosurgery, Xijing Hospital, Fourth Military Medical University.
Footnotes
Rong Zhao and Jinglan Deng contributed equally to this work.
Contributor Information
Rong Zhao, Department of Nuclear Medicine, Xijing Hospital, Fourth Military Medical University, Xi'an, Shaanxi 710032, China.
Jinglan Deng, Department of Nuclear Medicine, Xijing Hospital, Fourth Military Medical University, Xi'an, Shaanxi 710032, China.
Xiaoyan Liang, Department of Nuclear Medicine, Xijing Hospital, Fourth Military Medical University, Xi'an, Shaanxi 710032, China.
Jin Zeng, Department of Nuclear Medicine, Xijing Hospital, Fourth Military Medical University, Xi'an, Shaanxi 710032, China.
Xiaoyuan Chen, Department of Radiology, School of Medicine, Stanford University, Stanford, CA, USA.
Jing Wang, Department of Nuclear Medicine, Xijing Hospital, Fourth Military Medical University, Xi'an, Shaanxi 710032, China wangjing@fmmu.edu.cn.
References
- 1.Karavitaki N, Cudlip S, Adams CBT, Wass JAH. Craniopharyngiomas. Endo Rev. 2006;27:371–397. doi: 10.1210/er.2006-0002. [DOI] [PubMed] [Google Scholar]
- 2.Dekkers OM, Biermasz NR, Smit JWA, Groot LE, Roelfsema F, Romijn JA, Pereira AM. Quality of life in treated adult craniopharyngioma patients. Eur Journal of Endocrinol. 2006;154:483–489. doi: 10.1530/eje.1.02114. [DOI] [PubMed] [Google Scholar]
- 3.Leksell L, Liden K. 32P radiation in the treatment of craniopharyngiomas. J Neurooncol. 1952;56:69–78. [Google Scholar]
- 4.Richmond IL, Wara WM, Wilson CB. Role of radiation therapy in the management of craniopharyngiomas in children. Neurosurgery. 1980;6:513–517. doi: 10.1227/00006123-198005000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Kobayashi T, Kageyama N, Ohara K. Internal irradiation for cystic craniopharyngioma. J Neurosurg. 1981;55:896–903. doi: 10.3171/jns.1981.55.6.0896. [DOI] [PubMed] [Google Scholar]
- 6.Lunsford LD, Gumerman L, Levine G. Stereotactic intracavitary irradiation of cystic neoplasms of the brain. Appl Neurophysiol. 1985;48:146–150. doi: 10.1159/000101118. [DOI] [PubMed] [Google Scholar]
- 7.Tian Z. Stereotactic intracavitary irradiation of large cystic craniopharyngiomas. J Clin Neurosci. 1997;4:161–162. doi: 10.1016/s0967-5868(97)90066-7. [DOI] [PubMed] [Google Scholar]
- 8.Lunsford LD, Pollock BE, Kondziolka DS, Levine G, Flickinger JC. Stereotactic options in the management of craniopharyngioma. Pediatr Neurosurg. 1994;21(Suppl l):90–97. doi: 10.1159/000120868. [DOI] [PubMed] [Google Scholar]
- 9.Backlund E-O, Axelsson B, Bergstrand C-G, Eriksson A-L, Norén G, Ribbesjö E, Rähn T, Schnell P-O, Tallstedt L, Sääf M, Thorén M. Treatment of craniopharyngiomas—the stereotactic approach in a ten to twenty three years’ perspective. Acta Neurochir (Wien) 1989;99:11–19. doi: 10.1007/BF01407771. [DOI] [PubMed] [Google Scholar]
- 10.Loevinger R, Tapha EM, Brownell GL. Discrete radioisotope sources. 1. Beta-radiation. In: Hine GJ, Brownell GL, editors. Radiation dosimetry. Academic; New York: 1956. pp. 694–754. [Google Scholar]
- 11.Taasan V, Shapiro B, Taren JA, Beierwaltes WH, McKeever P, Wahl RL, Carey JE, Petry N, Mallette S. Phosphorus-32 therapy of cystic grade IV astrocytomas: technique and preliminary application. J Nucl Med. 1985;26:1335–1338. [PubMed] [Google Scholar]
- 12.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, Van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. JNCI. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 13.Habrand JL, Saran F, Alapetite C, Noel G, El Boustany R, Grill J. Radiation therapy in the management of craniopharyngioma: current concepts and future developments. J Pediatr Endocrinol Metab. 2006;19(Suppl 1):389–394. [PubMed] [Google Scholar]
- 14.Kalapurakal JA. Radiation therapy in the management of pediatric craniopharyngiomas—a review. Childs Nerv Syst. 2005;21:808–816. doi: 10.1007/s00381-005-1188-3. [DOI] [PubMed] [Google Scholar]
- 15.Pollock BE, Lunsford LD, Kondziolka D, Levine G, Flickinger JC. Phosphorus-32 intracavitary irradiation of cystic craniopharyngiomas: current technique and long-term results. Int J Radiat Oncol Biol Phys. 1995;33:437–446. doi: 10.1016/0360-3016(95)00175-X. [DOI] [PubMed] [Google Scholar]
- 16.Albright AL, Hadjipanayis CG, Lunsford LD, Kondziolka D, Pollack IF, Adelson PD. Individualized treatment of pediatric craniopharyngiomas. Childs Nerv Syst. 2005;21:649–654. doi: 10.1007/s00381-005-1185-6. [DOI] [PubMed] [Google Scholar]
- 17.Hasegawa T, Kondziolka D, Hadjipanayis CG, Lunsford LD. Management of cystic craniopharyngiomas with phosphorus-32 intracavitary irradiation. Neurosurgery. 2004;54:813–822. doi: 10.1227/01.neu.0000114262.30035.af. [DOI] [PubMed] [Google Scholar]
- 18.Fisher PG, Jenab J, Gopldthwaite PT, Tihan T, Wharam MD, Foer DR, Burger PC. Outcomes and failure patterns in childhood craniopharyngiomas. Childs Nerv Syst. 1998;14:558–563. doi: 10.1007/s003810050272. [DOI] [PubMed] [Google Scholar]
- 19.Lyen KR, Grant DB. Endocrine function, morbidity, and mortality after surgery for craniopharyngioma. Arch Dis Child. 1982;57:837–841. doi: 10.1136/adc.57.11.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar PP, Good RR, Skultety FM, Jones EO, Chu WK. Retreatment of recurrent cystic craniopharyngioma with chromic phosphorus P 32. J Natl Med Assoc. 1986;78(542–543):547–549. [PMC free article] [PubMed] [Google Scholar]
- 21.Sadeghi M, Moradi S, Shahzadi S, Pourbeigi H. Dosimetry of (32)P radiocolloid for treatment of cystic craniopharyngioma. Appl Radiat Isot. 2007;65:519–523. doi: 10.1016/j.apradiso.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 22.Shahzadi S, Sharifi G, Andalibi R, Zali A, Ali-Asgari A. Management of cystic craniopharyngiomas with intracavitary irradiation with 32P. Arch Iranian Med. 2008;11:30–34. [PubMed] [Google Scholar]