Abstract
UW Medicine teaching hospitals have seen a move from paper to electronic physician inpatient notes, after improving the availability of workstations, and wireless laptops and the technical infrastructure supporting the electronic medical record (EMR). The primary driver for the transition was to unify the medical record for all disciplines in one location. The main barrier faced was the time required to enter notes, which was addressed with data-rich templates tailored to rounding workflow, simplified login and other measures. After a 2-year transition, nearly all physician notes for hospitalized patients are now entered electronically, approximately 1500 physician notes per day. Remaining challenges include time for note entry, and the perception that notes may be more difficult to understand and to find within the EMR. In general, the transition from paper to electronic notes has been regarded as valuable to patient care and hospital operations.
Implementing an EMR system in a medical center often includes the intention to move from paper to electronic documentation of admission notes, progress notes, discharge summaries and other notes. In our hospitals, despite using computing systems to review results and imaging for 15 years, physicians only recently made the transition from writing notes in a paper chart to using the EMR to do so. Some hospitals in our city have made this transition, including the Veterans Administration hospital which did so a decade ago, but most have not. Because many hospitals in the USA are still using paper but may be considering electronic note entry, a description of our experience may be helpful. The purpose of this report is to describe what we believe to be the single most important step we took leading to physician adoption of electronic notes: our efforts to speed note entry.
Case description
This paper describes work conducted at the University of Washington Medical Center (UWMC), Harborview Medical Center (HMC) and the Seattle Cancer Care Alliance (SCCA). In 2007, UWMC had 390 beds, 72 ICU beds, and 18 120 admissions; HMC had 369 beds, 73 ICU beds, and 18 777 admissions. The SCCA has one hospital for adult patients, consisting of 18 beds. All three hospitals serve as teaching hospitals for the University of Washington. There are 792 active hospital medical staff at UWMC, 492 at HMC and 297 at SCCA. Across all hospitals, there are approximately 1000 residents and fellows, 826 medical students, 1610 full-time, and 1182 part-time nurses.
Our medical centers' leadership favored the transition to electronic physician notes because our medical record was fragmented among several computer systems and the paper chart. Notes by nurses, social workers, and other ancillary services were in one computing system, outpatient notes in another, and physician notes in the paper chart. From surveys, we learned that some physicians did not know how to access each of these systems, and so sometimes made decisions without important information that would have been available if notes by all disciplines were in a single location. There were other reasons also: improving the professional fee billing process, making notes available for quality of care review, and others.
Background
Our project was undertaken by the Medical Staff Documentation subgroup of the UW Medicine ORCA (EMR) project. It was overseen by a steering group consisting of hospital Medical Directors, the professional fee organization Chief Compliance Officer, and Patient Data Services (medical records) directors using weekly conference calls. The team comprised two nurse analysts, the CMIO, a programmer and a project manager. The project was formally chartered in July 2006 and completed in February 2007. Our goal was to move inpatient documentation from paper to electronic form, beginning at Harborview Medical Center and then UW Medical Center and Seattle Cancer Care Alliance. (Some notes such as detailed records of cardiac arrest management and records from other hospitals were entered on paper and scanned.)
Before undertaking the project, the main barrier voiced by physicians was concern that writing notes electronically would require more time than using paper templates.
Methods
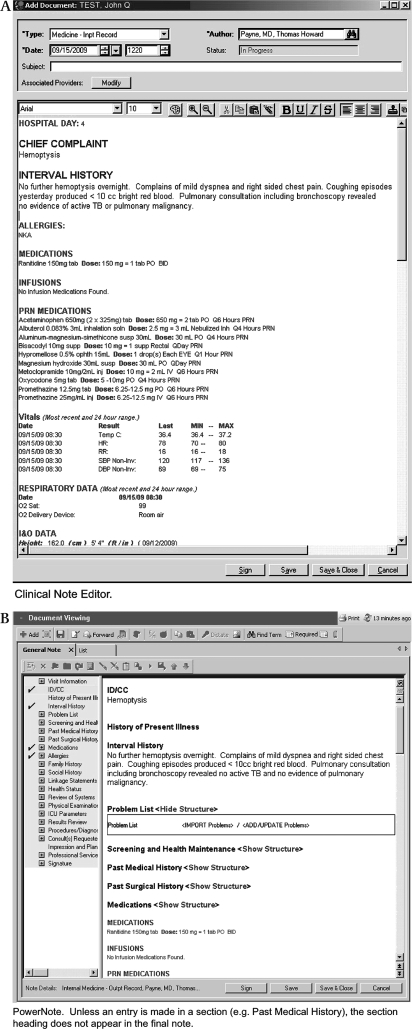
Between February and August of 2005, we began our transition by piloting directly entered notes on the inpatient Medicine teams at HMC, using PowerNote, a semiencoded note-entry application provided by our vendor (Cerner) in which both narrative text and encoded “clickable” elements are used to create the note. We delayed implementing other services until hardware and software limitations were addressed, including upgrading host hardware to improve performance and development of the “one button templates” described below. Surgical services were the next to adopt electronic notes. They used the narrative text Clinical Note Editor templates (figure 1) for nearly all progress notes. Clinical Note Editor, another note-entry application provided by our EMR vendor, uses a simple text editor similar to word-processing software. The rollout continued with a new inpatient service every 2 weeks, completing all three hospitals by February 2007, 2 years after our initial pilot. Most Medicine services subsequently moved to Clinical Note Editor templates.
Figure 1.
Example of partially written note using Clinical Note Editor (A) and PowerNote (B) demonstrating differences in the end user experience. Clinical Note Editor has a familiar text editor appearance. PowerNote has the ability to run macros, insert needed paragraph headings, and other features. Both permit automatic inclusion of patient-specific data such as current medication lists. The patient data in this figure are fictitious.
Initially, we developed templates using PowerNote. PowerNote templates enable the user to mix encoded elements in the Review of Systems, Physical Exam and elsewhere, with entry of narrative text in the History of Present Illness and elsewhere. A popular feature permitted a note to be copied into another note, modified and saved as a new note.
Most physician inpatient notes in our hospitals are daily progress notes. Physicians felt writing progress notes using PowerNote took substantially more time than using paper. To permit faster progress note entry, particularly for surgical services, we shifted to Clinical Note Editor. We created templates that include an outline of the note to be written, but most importantly when the template is opened a script loads the most recent medication list, allergies (drawn from our organizational “gold standard” location in the EMR), vital signs, and relevant laboratory results and other data. Laboratory results are displayed using popular “fishbone diagrams.” The electronic templates were designed to resemble paper progress note templates used in the past.1 Locations in the templates where the user is likely to type (eg, Chief Complaint, Interval History) are marked using an underscore to which the cursor quickly moves when the F3 function key is pressed. Some physicians manually copy portions of one note, such as the Assessment and Plan, into the next note, where it is modified to reflect changes and then signed. After the note has been written, it is reviewed and signed, and is immediately available for viewing in the medical record and accessible for coding. At the time the document is signed, the user may send it to another provider's Inbox, located within the EMR application, for review or signature. Training requirements for the Clinical Note Editor are lower than for PowerNote.
The fastest way to write notes is to select the patient from a system-generated patient list, and to configure the software to open the Clinical Note Editor default template when the user clicks an icon to start a new note. We refer to this process as a “one button template” which can be used to write notes while rounding. Following this process permits a review of the most recent laboratory and vital sign data at the time the note is being written, which saves additional time.
Both methods for entering notes permit use of system-wide templates to insert small amounts of text (eg, physician presence statements) and to create user-built templates using a feature called Auto-text. Notes created using either of these techniques, or by dictation, are viewable in the EMR in the same way. The same note-viewing screens also show scanned documents, such as records from an outside institution.
A representative from the billing and compliance department was actively involved in all phases of the implementation.
We measured the time required to enter notes using logs created during note entry. We used the difference between the time the note was started and final signing to determine note-entry time, which overestimates time required for some notes. User satisfaction was measured subjectively from comments by individuals and at committee meetings. The criterion for project success was whether nearly all notes written on inpatients by physicians were in the EMR as determined by chart audit, and that except in unusual circumstances, physicians did not have to look in the paper chart for notes.
Results
After project completion, physicians entered 1500 electronic notes for hospitalized patients in our three hospitals each day. Approximately 16% were entered by attending physicians, 58% by residents, 11% by mid-level practitioners, 7% by medical students, and 8% by fellows and others. These are divided among the note types shown in table 1.
Table 1.
Types of notes entered by physicians on a representative weekday
| Note type | No |
| Progress notes | 1073 |
| Admission notes | 66 |
| Procedure notes | 58 |
| Discharge summaries | 96 |
| Consultation notes | 101 |
| Other | 193 |
| Total | 1587 |
Note types are estimates because an admission note may be written using a progress note title.
We discovered that services have very different rounding and note-writing workflow. Trauma teams (Surgery, Neurosurgery, Orthopedics) round very quickly and sometimes write daily progress notes while rounding, usually starting at the uppermost floor of the hospital and working their way down to the operating room in the basement. These teams cover a large geographic area very quickly. They were supplied with laptop computers, and carts were placed at each stairwell entrance so that as the teams took the stairs from floor to floor, they would have a cart to use for the laptop while on that unit.
Medicine teams (General Medicine, Cardiology, Oncology, Geriatrics) spent more time rounding and gathering data for the daily progress note. These teams more commonly used desk workstations for note entry, which they usually entered after rounds. All services except for the Bone Marrow Transplant Service found the additional speed of the Clinical Note Editor progress notes to be an advantage and adopted it for progress note entry. The Bone Marrow Transplant Service found the structure and encoded data elements to be more important than speed for progress notes. A comparison of features for PowerNote and Clinical Note Editor is shown in table 2.
Table 2.
Comparison of PowerNote and Clinical Note Editor features and their importance to physician users
| Feature | Clinical Note Editor | PowerNote | Importance to physician user |
| Time required to write note | Less time | More time | ++++ |
| Clicks to launch new note | 1 | 3–4 | +++ |
| Copy forward entire note | Harder | Simpler | ++ |
| Automatic inclusion of prespecified patient data | Possible | Possible | ++ |
| Ability to select data for inclusion in note (eg, specific labs) | Harder | Simpler | ++ |
| Training requirement | Less time | More time | ++ |
| Ease of editing notes | Simpler | Harder | ++ |
| Simplicity of title assignment | Simpler | Harder | + |
| Send to attending for cosign | Possible | Possible | + |
| Template sophistication | Simpler | Richer | + |
| Ability to run macros | Not possible | Possible | + |
| Encoded data | None | Some | +/− |
| Ability to query for reports | Not yet possible | Possible | +/− |
This table is the assessment of the authors based on informal user feedback. Copy forward means beginning a new one using a previous note's text. Template sophistication indicates features such as gender-specific template content, conditional appearance of selectable choices and other features. Simplicity of title assignment means the number of steps required to assign the correct note title by which the note is displayed in the electronic medical record.
++++, very important; +/−, less important.
Using timing logs, we found that some physicians wrote and signed notes for uncomplicated patients within 2 min; comparable notes using PowerNotes take longer, though we have not quantified the difference. Our impression from many conversations with physicians and committee feedback was that the time required to write electronic notes, while longer than desired, was acceptable to them and that using the Clinical Note Editor for progress notes was faster than PowerNotes. Our impression from informal feedback from many physicians is that our physicians judge that availability of all notes made additional work to enter electronic notes worthwhile. (Since our project team is regularly in contact on the wards with housestaff and attending physicians, we continuously hear their comments and suggestions.) Non-random sampling of inpatient charts showed that, with few exceptions, physicians now use the EMR to write notes and not the paper chart; by this criterion, our project was successful. Physicians observe that many notes have duplicated Plan sections from one day to the next, and contain long lists of medications and other data that make it more difficult to find the most important sections of the note. We are addressing this by continual review and adjustment of templates by small workgroups with approval by our Health Information Management committees.
Discussion
In a recent survey, only 12% of US hospitals had instituted electronic physicians' notes across all clinical units.2 Direct note entry by care providers is likely very low in office practice, since EMR penetration is low in this setting. Hospitals have higher adoption rates of EMRs. A 2006 national survey of US hospitals indicated that 64% of hospitals EMRs had access to medical history and medical records, and 32% of hospitals had “fully implemented” systems. The criteria used and survey responses did not indicate if electronic physician documentation was a part of the record.3
In addition, there is limited literature on the experience of individual institutions on implementing computerized physician documentation in hospitals. Some of the most extensive experience with direct physician entry has taken place in the Veterans Health Administration. In the Intermountain Healthcare System, 68% of ambulatory care physicians in the Intermountain Healthcare System entered some data in the EMR.4 Our group has also reported on our initial experiences with physician documentation on the Medicine service.5 There have been extensive reports on the challenges and opportunities introduced with computerized physician documentation.3 6 7 8
Nearly all physicians in our hospitals appreciate improved legibility of inpatient records, their accessibility from any location and the new comprehensiveness of the medical record achieved when notes from all services are contained within it. Additional advantages became clear over time: the ability to standardize documentation using templates, protection from note loss, instantaneous availability of electronic notes to billing personnel, communication with physicians who are not on the ward at the time by forwarding notes, ease with which attending physicians can “link” to notes written by trainees, and others. In our case, past fragmentation of the medical record between notes by nurses, physical therapists, physicians and others was largely solved when all adopted the same electronic medical record.
Barriers, and how we addressed them
Despite numerous advantages, there are barriers that delay transition from paper to electronic notes. Chief among these is the time required to enter notes. We strove to reduce time required to enter notes in several ways. We used templates tailored to rounding workflow to insert information physicians want included in their notes such as current medication lists, recent laboratory results and other data, and used graphical conventions to display these data that physicians prefer. We made it possible to invoke these templates with a single mouse click. This proved successful for the busiest services such as Orthopedics. We modeled these note templates on versions created in a heavily used rounding report and sign-out application which created PDF templates that were printed, completed and filed in the paper chart by most services.1 We are not aware of any published data comparing the time required to enter electronic notes compared with paper notes, and are working to gather comparative data.
Numerous disadvantages to electronic notes have been described.9 10 Among them are concern that electronic notes are more difficult to read and understand than handwritten notes, and inappropriate copying and pasting. Distinctive handwriting, ink color, circling for emphasis, and other marks make handwritten notes different from those written with electronic applications. The labor of handwriting encouraged brevity, whereas electronic templates containing detailed medication lists, laboratory results, and copied/pasted reports both lengthened notes, and sometimes reduced their ability to rapidly convey meaning. Despite efforts to train our community to write brief notes,11 this remains a concern and challenge for us. We are developing a training curriculum for medical students and residents to improve note quality and readability. Along with other institutions, we are exploring development of a search capability to simplify a search of the growing number of notes in each patient's record.
Physicians also feel it is harder to find the note of interest among many daily notes created. Searching for an Infectious Disease consult note after a 2-week hospitalization is now more difficult than it had been with a clear Physician Note section in a paper chart, where characteristic penmanship of the consultant could be identified by rapidly flipping through the paper chart. Though we developed strategies to help—specialized note titles,12 screens showing multiple note attributes on a single row and others—increased numbers of notes within the EMR make the search more difficult. Another concern is the perception that the quality and readability of many notes have declined. To our knowledge, there is no generally accepted index of note quality, but the opinion of many physicians is that we need to make notes more readable. By moving from semiencoded to narrative text notes, we have accepted the limitations on what can be extracted from the notes that contain few encoded data for automated review and quality assessment. We are experimenting with the use of natural language processing to address this.
Our transition from paper to electronic physician inpatient notes required approximately 2 years and followed substantial efforts to improve the availability of workstations and wireless laptops for entry and review of notes, speed of note entry, as well as the technical infrastructure supporting the EMR. In general, the transition from paper to electronic notes has been regarded as valuable to patient care and hospital operations.
Acknowledgments
We would like to thank UW Medicine housestaff and faculty and our EMR team, for their support of this project, and S Barnhart and R Hodge, for their generous contributions of time, support and leadership.
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Van Eaton EG, Horvath KD, Lober WB, et al. Organizing the transfer of patient care information: The development of a computerized resident sign-out system. Surgery 2004;136:5–13 [DOI] [PubMed] [Google Scholar]
- 2.Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in US hospitals. N Engl J Med 2009;360:1628–38 [DOI] [PubMed] [Google Scholar]
- 3.American Hospital Association Continued progress: hospital use of information technology. Chicago: American Hospital Association, 2007 [Google Scholar]
- 4.Clayton PD, Naus SP, Bowes WA, 3rd, et al. Physician use of electronic medical records: issues and successes with direct data entry and physician productivity. AMIA Annu Symp Proc 2005:141–5 [PMC free article] [PubMed] [Google Scholar]
- 5.Payne TH, Perkins M, Kalus R, et al. The transition to electronic documentation on a teaching hospital medical service. AMIA Annu Symp Proc 2006:629–33 [PMC free article] [PubMed] [Google Scholar]
- 6.Davidson SJ, Zwemer FL, Jr, Nathanson LA, et al. Where's the beef? The promise and the reality of clinical documentation. Acad Emerg Med 2004;11:1127–34 [DOI] [PubMed] [Google Scholar]
- 7.O'Donnell H, Kaushal R, Siegler E, et al. Physicians attitudes towards copy and pasting in electronic note writing. AMIA Annu Symp Proc 2008:1073. [PubMed] [Google Scholar]
- 8.Embi PJ, Yackel TR, Logan JR, et al. Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians. J Am Med Inform Assoc 2004;11:300–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartzband P, Groopman J. Off the record—avoiding the pitfalls of going electronic. N Engl J Med 2008;358:1656–8 [DOI] [PubMed] [Google Scholar]
- 10.Hirschtick RE. Copy-and-paste. JAMA 2006;295:2335–6 [DOI] [PubMed] [Google Scholar]
- 11.Payne TH, Hirschmann JV, Helbig S. Elements of electronic note style. J AHIMA 2003;74:68,70. [PubMed] [Google Scholar]
- 12.Payne TH, Kalus R, Zehner J. Evolution and use of a note classification scheme in an electronic medical record. AMIA Annu Symp Proc 2005:599–603 [PMC free article] [PubMed] [Google Scholar]