Abstract
A retrospective cross-sectional study was designed to evaluate total sagittal spinal alignment in patients with lumbar disc herniation (LDH) and healthy subjects. Abnormal sagittal spinal alignment could cause persistent low back pain in lumbar disease. Previous studies analyzed sciatic scoliotic list in patients with lumbar disc herniation; but there is little or no information on the relationship between sagittal alignment and subjective findings. The study subjects were 61 LDH patients and 60 age-matched healthy subjects. Preoperative and 6-month postoperatively lateral whole-spine standing radiographs were assessed for the distance between C7 plumb line and posterior superior corner on the top margin of S1 sagittal vertical axis (SVA), lumbar lordotic angle between the top margin of the first lumbar vertebra and first sacral vertebra (L1S1), pelvic tilting angle (PA), and pelvic morphologic angle (PRS1). Subjective symptoms were evaluated by the Japanese Orthopedic Association (JOA) score for lower back pain (nine points). The mean SVA value of the LDH group (32.7 ± 46.5 mm, ± SD) was significantly larger than that of the control (2.5 ± 17.1 mm), while L1S1 was smaller (36.7 ± 14.5°) and PA was larger (25.1 ± 9.0°) in LDH than control group (49.0 ± 10.0° and 18.2 ± 6.0°, respectively). At 6 months after surgery, the malalignment recovered to almost the same level as the control group. SVA correlated with the subjective symptoms measured by the JOA score. Sagittal spinal alignment in LDH exhibits more anterior translation of the C7 plumb line, less lumbar lordosis, and a more vertical sacrum. Measurements of these spinal parameters allowed assessment of the pathophysiology of LDH.
Keywords: Sagittal spinal alignment, Lumbar disc herniation, Radicular pain
Introduction
Abnormal sagittal spinal alignment may cause persistent low back pain in patients with lumbar disease. Patients with lumbar disc herniation (LDH) accompanied by radicular pain sometimes present a forward-bending posture while walking. Previous studies analyzed sciatic scoliotic list in LDH [1, 2], although they did not quantify the relationship between sagittal alignment and the subjective findings. The present study investigated total sagittal spinal alignment and objective findings before and after surgery in LDH patients.
Materials and methods
The retrospective study comprised 61 patients (38 males and 23 females), aged from 20 to 49 years (mean, 32.7 years), who were diagnosed with LDH. The levels of herniated disc were L4-5 (n = 30) and L5-S1 (n = 31). All patients underwent a thorough preoperative clinical assessment followed by simple herniectomy at our facility from 2005 to 2007. We also included 60 normal subjects (39 males and 21 females) aged from 22 to 51 years who were free of LDH-related symptoms.
All subjects had lateral long cassette radiographs of the whole spine performed in the most stable and relaxed position while they were standing with their arms extended and their hands gently clasped in front of the trunk (clasped position) [3]. For each subject, lateral radiographs of the spine were taken using vertical film (35.4 × 83.7 cm2) with a constant distance between the subject and the radiographic source that included the use of a radio-opaque calibration tool.
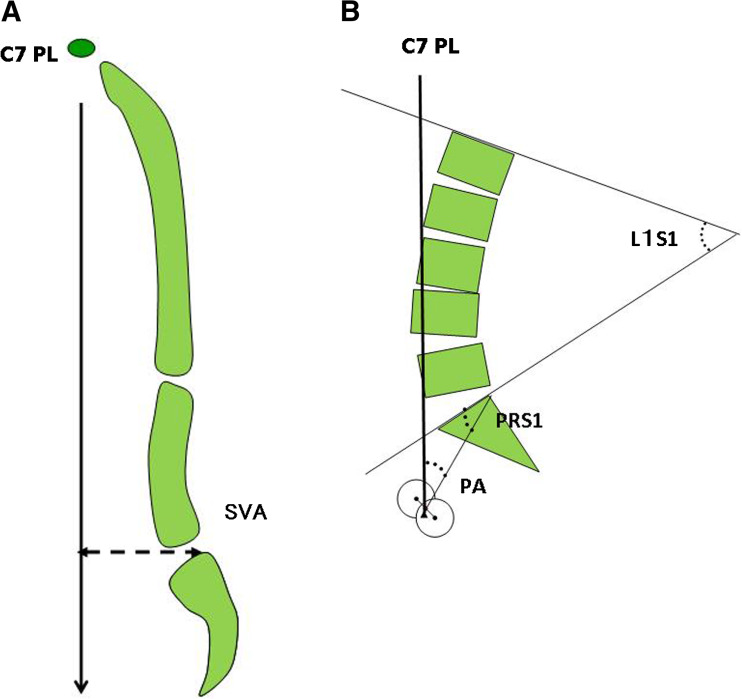
The following parameters were measured on the lateral whole spine standing radiographs a few days before and 6 months after surgery as described by Jackson et al. [4]: distance between the C7 plumb line and the posterior corner of the sacrum (sagittal vertical axis, SVA) (Fig. 1a); angle between the upper margin of the first lumbar vertebra and the first sacral vertebra (L1S1) as a lumbar lordosis; pelvic tilting angle (PA); and, pelvic morphological angle (PRS1) (Fig. 1b). PA corresponds to the angle between the line connecting the posterior corner of the sacrum to the bicoxofemoral axis and the vertical plane, and is considered as a pelvic positional parameter. PRS1 is the angle between the line paralleling sacral surface and the hip axis, and is a morphological constant taken as an independent measure of the pelvic spatial orientation [4, 5]. These parameters were compared between the LDH and control groups.
Fig. 1.
Measurements of (a) SVA and (b) lumbopelvic balance. C7 PL C7 plumb line; SVA sagittal vertical axis (mm); L1S1 L1S1 angle; PA pelvic tilt angle; PRS1 pelvic morphological angle
Subjective symptoms (low back pain, leg pain, and gait disturbance) were evaluated using the Japanese Orthopedic Association criteria (JOA score) for low back pain (three points each with a total of nine points) [6]. The subjective symptoms were measured immediately before and 6 months after surgery.
Values were expressed as mean ± standard deviation (SD). The measurements were tabulated and analyzed using Excel (Microsoft, Redmond, WA). Differences between groups were examined for statistical significance using Student’s t-test or the Mann–Whitney U-test. Correlations between two variables were analyzed by Pearson’s correlation coefficient or Spearman’s rank-correlation coefficient. P values less than 0.05 were considered statistically significant.
Results
The mean SVA and PA values for the LDH group (32.7 ± 46.5 mm and 25.1 ± 9.0°, respectively) were significantly larger than those of the control group (2.5 ± 17.1 mm and 18.2 ± 6.0°, respectively), while L1S1 was smaller (36.7 ± 14.5°) in LDH patients than in controls (49.0 ± 10.0°) (Table 1). PRS1 was not significantly different between the two groups (Table 1). The Pearson’s correlation coefficients of the LDH and control groups were 0.44 and 0.08 between SVA and L1S1, –0.47 and –0.33 between L1S1 and PA, and 0.39 and 0.21 between PA and SVA, respectively.
Table 1.
JOA scores and spinal parameters in control and LDH groups
| Control subjects | LDH patients | ||
|---|---|---|---|
| Before surgery | 6 months after surgery | ||
| n | 26 | 61 | – |
| Gender (male/female) | 15/11 | 38/23 | – |
| Age (years) | 22–51 (32.7) | 20–49 (32.7) | – |
| JOA* | – | 3.5 ± 1.7 | 7.6 ± 0.8 |
| SVA (mm)* | 1.5 ± 17.7 | 32.7 ± 46.5 | 6.7 ± 27.7 |
| L1S1 (º)* | 49.0 ± 10.0 | 36.7 ± 14.5 | 44.8 ± 10.8 |
| PA(º)* | 18.0 ± 6.0 | 25.1 ± 9.0 | 21.3 ± 7.0 |
| PRS1º* | 36.6 ± 10.4 | 36.5 ± 8.9 | 36.3 ± 7.4 |
* Values are expressed as mean ± SD
Six months after surgery, the LDH patients showed significant recovery according to the subjectively based JOA score, as well as the reduced SVA and PA, and larger L1S1 values compared to the preoperative scores and values. Data analyzed at 6 months postoperatively were closer to the control values (Table 1).
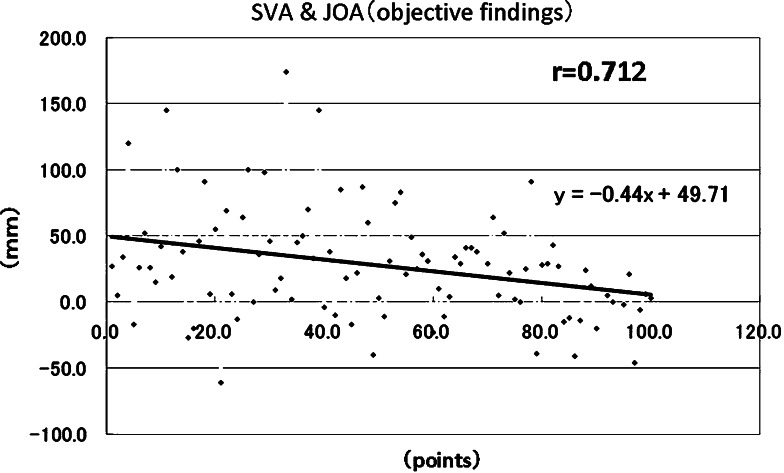
With regard to the relationship between abnormal posture and subjective findings, SVA and L1S1 correlated with various subjective symptoms determined by the JOA score (r = 0.49 and 0.38, respectively), whereas PA did not correlate with the JOA score (r = 0.02, Fig. 2).
Fig. 2.
Correlation between SVA and subjective symptoms measured by the JOA score (nine points) in patients with lumbar disc herniation
Discussion
Several studies have analyzed spino-pelvic alignment in the general population [3, 7], aging populations [5, 8], and patients with lumbar degenerative disease [9–11]. It is well known that patients with LDH sometimes present with a forward-bending posture while walking. The sciatic scoliotic list in LDH patients has also been investigated [1, 2]. However, the relationship between sagittal spinal alignment and sciatic pain has not been quantified in detail [12, 13].
The present study demonstrated that LDH patients and controls were significantly different in anterior translation of the C7 plumb line, loss of lumbar lordosis, and decrease in sacral slope. The loss of lumbar lordosis in LDH is not likely to be due to severe structural deformity. Rather, it may be secondary to segmental discopathy or small loss of disc height, a postural change secondary to an analgesic response to avoid posterior disc hyperpression, or foraminal stenosis due to a herniated disc [12]. The observed lumbar lordotic changes might also correspond to a rotation of the pelvis around the coxofemoral joints by contraction of the hip extensor muscles [13]. Biomechanically, the loss of lordosis would result in anterior displacement of the C7 plumb line as well as a more vertical pelvic tilt (i.e., increase in PA) to compensate for the anterior translation of the gravitational axis [10]. The correlations among parameters found in this study concord with that conclusion.
On the other hand, the pelvic morphologic angle (PRS1) in LDH patients was not significantly different from the control, a finding similar to the results of other studies [12, 14]. Previous studies suggested the association between the PRS1 and lumbar degenerative diseases [10, 12, 13]. The smaller PRS1 angle sometimes appear with the onset of certain lumbar degenerative disease. It is possible that the mechanism of LDH is different from other lumbar degenerative diseases.
With regard to the control group, the relation between spinal alignment and SVA is independent. However, in the LDH group at baseline (before operation), the SVA was affected by spinal parameters. This could be interpreted that patients with LDH exhibit lack of spinal compensation to changes in spinal alignment and that such ability recovers after surgery.
The present study also identified a correlation between SVA and L1S1 with the JOA score. Particularly in cases with progressive anterior translation of the C7 plumb line, the subjective findings (i.e., JOA score) were severe and the spinal alignment showed less lumbar lordosis and more vertical tilt of the pelvic bone. Recovery of the abnormal posture was noted within 6 months after surgery, together with improvement in the subjective symptoms on the JOA score.
We conclude that in patients with LDH, sagittal balance might be affected by sciatic stimulation and tonic contraction of the surrounding lumbopelvic muscles.
These abnormal parameters are mainly based on protective mechanisms designed to avoid sciatic pain. Such protective mechanisms have also been described in patients with degenerative spinal stenosis [12]. The abnormal translation of SVA and the abnormal posterior pelvic rotation are probably related to mechanisms that avoid increased tension of painful sciatic nerve. After surgery, hip extension followed by reduced sciatic nerve tension seems to allow recovery of SVA and pelvic anterior rotation.
Conclusion
Sagittal spinal alignment of LDH exhibits a more anterior translation of C7 plumb line, less lordosis, and a more vertical sacrum. Analysis of spinal posture and clinical symptoms showed correlation of SVA and L1S1 with subjective symptoms measured by the JOA score. Quantitative assessment of spinal alignment provides a better understanding of the pathophysiology of LDH.
Acknowledgments
The authors thank Dr. F.G. Issa (www.word-medex.com.au) for careful reading and editing of the manuscript.
References
- 1.Matsui H, Ohmori K, Kanamori M, Ishihara H, Tsuji H. Significance of sciatic scoliotic list in operated patients with lumbar disc herniation. Spine. 1998;23:338–342. doi: 10.1097/00007632-199802010-00010. [DOI] [PubMed] [Google Scholar]
- 2.Suk KS, Lee HM, Moon SH, Kim NH. Lumbosacral scoliotic list by lumbar disc herniation. Spine. 2001;26:667–671. doi: 10.1097/00007632-200103150-00023. [DOI] [PubMed] [Google Scholar]
- 3.Matsuoka H, Komagata M, Nishiyama M, Imakiire A. Radiographic assessment of sagittal spinal alignment to correlate standards classified by age and low back pain. J Tokyo Med Univ. 2004;62:64–71. [Google Scholar]
- 4.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine. 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 5.Kobayashi T, Atsuta Y, Matsuno T, Takeda N. A longitudinal study of congruent sagittal spinal alignment in adult cohort. Spine. 2004;29:671–676. doi: 10.1097/01.BRS.0000115127.51758.A2. [DOI] [PubMed] [Google Scholar]
- 6.Izumida S, Inoue S. Assessment of treatment for low back pain. J Jpn Orthop Assoc. 1986;60:391–394. [Google Scholar]
- 7.Gelb DE, Lenke LG, Bridwell KH, Blanke K, MacEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]
- 8.Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis: clinical, radiological and epidemiological studies. Spine. 1998;13:1317–1326. doi: 10.1097/00007632-198811000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Rober B, Hansen S, Saillant G, Maurs L, Trabelsi R. Sagittal alignment in lumbosacral fusion relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Legaye J, Duval-Beaupere G, Hecquet J, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am. 1983;65-A:768–772. [PubMed] [Google Scholar]
- 12.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvic–spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007;16:1459–1467. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurology. 2007;61:981–986. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 14.Rajnics P, Templier A, Skalli W, Lavaste F, Illes T. The importance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop. 2002;26:104–108. doi: 10.1007/s00264-001-0317-1. [DOI] [PMC free article] [PubMed] [Google Scholar]