Abstract
Background
Adenoidectomy, surgical removal of the adenoids, is a common ENT operation worldwide in children with otitis media. A systematic review on the effectiveness of adenoidectomy in this specific group has not previously been performed.
Objectives
To assess the effectiveness of adenoidectomy versus non‐surgical management or tympanostomy tubes in children with otitis media.
Search methods
We searched the Cochrane Ear, Nose and Throat Disorders Group Trials Register; the Cochrane Central Register of Controlled Trials (CENTRAL); PubMed; EMBASE; CINAHL; Web of Science; BIOSIS Previews; Cambridge Scientific Abstracts; mRCT and additional sources for published and unpublished trials. The date of the most recent search was 30 March 2009.
Selection criteria
Randomised controlled trials comparing adenoidectomy, with or without tympanostomy tubes, versus non‐surgical management or tympanostomy tubes only in children with otitis media. The primary outcome studied was the proportion of time with otitis media with effusion (OME). Secondary outcomes were mean number of episodes, mean number of days per episode and per year, and proportion of children with either acute otitis media (AOM) or otitis media with effusion (OME), as well as mean hearing level. Tertiary outcome measures included atrophy of the tympanic membrane, tympanosclerosis, retraction of the pars tensa and pars flaccid and cholesteatoma.
Data collection and analysis
Two authors assessed trial quality and extracted data independently.
Main results
Fourteen randomised controlled trials (2712 children) studying the effectiveness of adenoidectomy in children with otitis media were evaluated. Most of these trials were too heterogeneous to pool in a meta‐analysis. Loss to follow up varied from 0% to 63% after two years.
Adenoidectomy in combination with a unilateral tympanostomy tube has a beneficial effect on the resolution of OME (risk difference (RD) 22% (95% CI 12% to 32%) and 29% (95% CI 19% to 39%) for the non‐operated ear at six and 12 months, respectively (n = 3 trials)) and a very small (< 5 dB) effect on hearing, compared to a unilateral tympanostomy tube only. The results of studies of adenoidectomy with or without myringotomy versus non‐surgical treatment or myringotomy only, and those of adenoidectomy in combination with bilateral tympanostomy tubes versus bilateral tympanostomy tubes only, also showed a small beneficial effect of adenoidectomy on the resolution of the effusion. The latter results could not be pooled due to large heterogeneity of the trials.
Regarding AOM, the results of none of the trials including this outcome indicate a significant beneficial effect of adenoidectomy. The trials were too heterogeneous to pool in a meta‐analysis.
The effects of adenoidectomy on changes of the tympanic membrane or cholesteatoma have not been studied.
Authors' conclusions
Our review shows a significant benefit of adenoidectomy as far as the resolution of middle ear effusion in children with OME is concerned. However, the benefit to hearing is small and the effects on changes in the tympanic membrane are unknown. The risks of operating should be weighed against these potential benefits.
The absence of a significant benefit of adenoidectomy on AOM suggests that routine surgery for this indication is not warranted.
Keywords: Child, Humans, Adenoidectomy, Adenoidectomy/methods, Hearing Loss, Hearing Loss/surgery, Middle Ear Ventilation, Otitis Media, Otitis Media/surgery, Otitis Media with Effusion, Otitis Media with Effusion/surgery, Randomized Controlled Trials as Topic, Tympanic Membrane, Tympanic Membrane/surgery
Plain language summary
Adenoidectomy for recurrent or chronic middle ear disease in children
Both acute and chronic middle ear infections (acute otitis media and chronic otitis media with effusion or 'glue ear') are very common in children. Adenoidectomy is a surgical procedure to remove the adenoids and is often performed in these children as it is thought to prevent these problems.
Our review, which includes 14 studies and 2712 children, shows that adenoidectomy is effective in getting rid of middle ear fluid ('glue') but does not have a significant effect on acute otitis media or the child's hearing.
Background
Incidence
Adenoidectomy is one of the most frequently performed surgical procedures in children in Western countries. Annual adenoidectomy rates, however, differ between countries, from 127/10,000 children per year in Belgium, 101/10,000 children per year in the Netherlands and 39/10,000 children per year in England to 24/10,000 and 17/10,000 children per year in the United States and Canada, respectively (Schilder 2004).
Adenoidectomy
Indications for adenoidectomy include recurrent episodes of acute otitis media (AOM) and persistent otitis media with effusion (OME). The operation involves removing the adenoids ‐ a nasopharyngeal reservoir of potential respiratory pathogens and a potential cause of obstruction of the nasal airway. As such, Eustachian tube function is thought to improve.
Evidence for adenoidectomy
At present the effectiveness of adenoidectomy in children with otitis media remains uncertain and practice is experience‐based rather than evidence‐based. Some surgeons prefer to perform adenoidectomy in these children, whereas others do not. In previous systematic reviews for The Cochrane Library the effectiveness of 1) grommets (ventilation tubes) for recurrent acute otitis media in children (McDonald 2008) and 2) grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children (Lous 2005) and 3) tonsillectomy or adeno‐tonsillectomy versus non‐surgical treatment for chronic/recurrent acute tonsillitis (Burton 2009) have all been assessed. For adenoidectomy in children with otitis media no such review is available. This study therefore provides a comprehensive systematic review and meta‐analysis of randomised controlled trials evaluating the effectiveness of adenoidectomy in children with otitis media.
Objectives
To assess the effectiveness of adenoidectomy compared with non‐surgical management in children up to 18 years of age with otitis media.
Methods
Criteria for considering studies for this review
Types of studies
We considered all identified randomised controlled trials of adenoidectomy for otitis media compared with non‐surgical treatment or tympanostomy tubes alone for inclusion in this review. We included trials in which the method of randomisation was not specified in detail, but we excluded quasi‐randomised trials (e.g. allocation by date of birth or record number).
Studies had to have a follow up of at least six months. Studies with a follow up of six to 12 months were reported separately from those with a follow up of 12 months or more.
Desirable time points of outcome assessment were six months, 12 months, 24 months and 36 months.
Types of participants
Children up to 18 years of age diagnosed with otitis media.
Types of interventions
To evaluate the effects of adenoidectomy we compared the following interventions:
adenoidectomy (with or without myringotomy) versus non‐surgical treatment or myringotomy only;
adenoidectomy with unilateral tympanostomy tube versus unilateral tympanostomy tube only (in studies of this type it is the ear without the tympanostomy tube that is evaluated to study the effect of adenoidectomy);
adenoidectomy with bilateral tympanostomy tubes versus bilateral tympanostomy tubes only.
Non‐surgical management included watchful waiting and medical treatment including antibiotics (intermittent and long‐term), steroids, antihistamines and analgesics.
Types of outcome measures
Primary outcomes
The primary outcome measure was the proportion of time with effusion, diagnosed with and without tympanometry.
Secondary outcomes
Secondary outcomes are as follows.
-
Acute otitis media (AOM).
Number of episodes per year.
Number of days per episode and per year.
Proportion of children with recurrent episodes.
Otitis media with effusion (OME).
Number of episodes per year.
Number of days per episode and per year.
Proportion of children with recurrent episodes.
Mean hearing level.
Definitions of secondary outcome measures
AOM and OME were defined according to the definitions issued by the American Association of Family Physicians (AAFP) and the American Academy of Pediatrics (AAP).
For AOM this is: acute onset of signs and symptoms, the presence of middle ear effusion (bulging of the tympanic membrane, or limited or absent mobility of the tympanic membrane, or air‐fluid level behind the tympanic membrane, or otorrhoea), and signs and symptoms of middle ear inflammation (distinct erythema of the tympanic membrane or distinct otalgia (AAFP 2009a).
For OME this is: presence of fluid in the middle ear, without signs and symptoms of acute ear infection as diagnosed by (pneumatic) otoscopy or tympanometry (AAFP 2009b).
Recurrent was defined as the patient having three or more episodes of OME or AOM in a period of six months, or four or more episodes in a period of 12 months (Rosenfeld 2000).
Tertiary outcome measures
Tertiary outcome measures include:
the proportion of children with atrophy of the tympanic membrane;
the proportion of children with tympanosclerosis of the tympanic membrane;
the proportion of children with retraction of the pars tensa and pars flaccida;
the proportion of children with cholesteatoma.
Search methods for identification of studies
We conducted systematic searches for randomised controlled trials on the effectiveness of adenoidectomy in children up to 18 years of age with otitis media. There were no language, publication year or publication status restrictions. We contacted original authors for clarification and further data if trial reports were unclear and arranged translations of papers where necessary. The date of the last search was 30 March 2009.
Electronic searches
We searched the following databases from their inception: the Cochrane Ear, Nose and Throat Disorders Group Trials Register; the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library Issue 1, 2009); PubMed; EMBASE; CINAHL; LILACS; KoreaMed; IndMed; PakMediNet; CAB Abstracts; Web of Science; BIOSIS Previews; CNKI; mRCT (Current Controlled Trials); ClinicalTrials.gov; ICTRP (International Clinical Trials Registry Platform); ClinicalStudyResults.org and Google.
We modelled subject strategies for databases on the search strategy designed for CENTRAL. Where appropriate, we combined subject strategies with adaptations of the highly sensitive search strategy designed by the Cochrane Collaboration for identifying randomised controlled trials and controlled clinical trials (as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1, Box 6.4.b. (Handbook 2008)). Search strategies for major databases including CENTRAL are provided in Appendix 1.
Searching other resources
We checked the reference lists of identified publications for additional trials. We searched PubMed; TRIPdatabase; NHS Evidence ‐ ENT and Audiology and Google to retrieve existing systematic reviews possibly relevant to this systematic review, in order to search their reference lists for additional trials. We scanned abstracts of conference proceedings via the Cochrane Ear, Nose and Throat Disorders Group Trials Register and CENTRAL.
Data collection and analysis
We conducted the review according to the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions 5.0.1 (Handbook 2008).
Selection of studies
Two review authors (MvdA, EH) scanned the abstracts to identify relevant randomised controlled trials. The same two authors obtained and reviewed the full texts of these articles. We assessed the eligibility of the trials independently and resolved any differences in opinion by discussion between the two authors. Reasons for exclusion of potentially relevant studies are given in the 'Characteristics of excluded studies' table.
Data extraction and management
Two review authors (MvdA, EH) also performed data extraction independently, followed by a consensus conference to resolve differences. We extracted the following data from each study: total number of children in each trial, description of participants (mean age, country of origin, inclusion and exclusion criteria, allergy status, adenoid size), follow‐up time in months, description of intervention and control therapy, number of patients per intervention group, primary and secondary outcomes, the use of tympanometry as an objective outcome measure and the authors' conclusion.
Assessment of risk of bias in included studies
Two authors (MvdA, CB) assessed the quality of all included trials independently using the Cochrane Collaboration’s tool for assessing risk of bias ('Risk of bias' table, Cochrane Handbook for Systematic Reviews of Interventions, chapter 5 (Handbook 2008)). Six specific domains were addressed, i.e. sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and ‘other biases’. By answering pre‐specified questions we reported the execution of the study and judged the risk of bias for each domain. The outcome for each domain was either 1) yes, a high risk, 2) no, a low risk or 3) an unknown or unclear risk of bias. We resolved disagreement by discussion (MvdA, CB, MR).
We planned to assess publication bias with a scatter plot (funnel plot) of the log rate ratios (x‐axis) versus precision defined as 1/standard error (y‐axis) (Handbook 2008).
Data synthesis
We used RevMan version 5.0 (RevMan 2008) to carry out the meta‐analyses for comparable trials and outcomes.
For continuous outcomes (i.e. number of episodes, number of days per episode, number of days per year, and mean hearing loss) we calculated standard mean differences (SMD) and their corresponding 95% confidence intervals (CI).
For dichotomous outcomes we measured the estimates of effect as risk differences (RD) with their corresponding 95% confidence intervals. Risk differences were calculated using: (proportion of children with outcome present in adenoidectomy group) ‐ (proportion of children with outcome present in control group).
If heterogeneity was low (I2 < 25%) we calculated the summary weighted risk differences and 95% confidence intervals (random‐effects model) by the Mantel‐Haenszel method, which weighs studies by the number of events in the control group, using the Cochrane statistical package in RevMan (version 5.0).
We planned to perform sensitivity analyses excluding the studies with the lowest methodological quality according to the Cochrane Collaboration's risk of bias assessment, and by including and excluding studies using tympanometry as an objective measure in the diagnosis of OME, to investigate whether these factors influenced the final outcome. We intended to perform subgroup analyses for age groups and adenoid size. Ultimately this was impossible because the original papers did not report the effects for these subgroups separately. Data allowing, we hope to include sensitivity and subgroup analyses in future updates of this review.
Results
Description of studies
Results of the search
Our search of CENTRAL, PubMed, EMBASE and other databases retrieved a total of 204 articles. We first sifted the articles by title/abstract and this left us 31 articles to read in full text. A total of 14 studies (n = 2712 children) were included in this review. No additional trials were identified by checking the bibliographies of the selected trials and reviews, nor by contacting the first or corresponding author of the eligible trials. One study by Sagnelli et al (Sagnelli 1990) could not be retrieved.
We excluded eleven of the publications because the same data are presented in more recent articles included in this review (Black 1986; Gates 1988; Gates 1989; Maw 1983; Maw 1985a; Maw 1985b; Maw 1987; Maw 1988; Maw 1993; Maw 1994a; Maw 1994b). Publications which focused on the intervention adenotonsillectomy were also excluded except for those in which a separate analysis for adenoidectomy was performed (Paradise 1999). Reasons for exclusion are described in the 'Characteristics of excluded studies' table.
Included studies
The included studies used a wide range of interventions and outcome measures. Therefore studies will be described by type of intervention. The 'Characteristics of included studies' table shows the characteristics in summary. The inclusion and exclusion criteria for participants of all included trials in this review are shown in Appendix 2.
1) Adenoidectomy with or without myringotomy versus non‐surgical treatment or myringotomy only.
2) Adenoidectomy with unilateral tympanostomy tube versus a unilateral tympanostomy tube only; non‐operated ear examined for comparison.
3) Adenoidectomy with bilateral tympanostomy tubes versus bilateral tympanostomy tubes only.
A summary of outcomes reported per study can be found in Table 1.
1. Summary of outcomes reported per study.
| Intervention failure | Recovery time in months | Change in frequency | Time to first recurrence | Mean number of AOM episodes | Mean number of OME episodes | Proportion of time with otitis media | Proportion time with AOM | Proportion of time with OME | Resolution of effusion | Mean hearing loss | Time with hearing loss > 20 dB | Tympanogram type | Mean number of days with earache | Mean number of days with rhinitis | Mean number of days with fever | Number of episodes of otorrhoea | Proportion of time with otorrhoea | Number of days with otorrhoea | Mean number of doctor visits | Mean number of antibiotic prescriptions | Mean number of days with antimicrobial treatment | Number of re‐treatments or myringotomy or TT procedures | |
| Koivunen 2004 | X | X | X | X | X | X | X | ||||||||||||||||
| Paradise 1999 | X | X | X | X | X | ||||||||||||||||||
| Paradise 1990 | X | X | X | X | X | X | |||||||||||||||||
| Gates 1987 | X | X | X | X | |||||||||||||||||||
| Fiellau‐Nikolajsen 1980 | X | X | |||||||||||||||||||||
| Rynnel‐Dagöö 1978 | X | ||||||||||||||||||||||
| Dempster 1993 | X | X | |||||||||||||||||||||
| Black 1990 | X | X | |||||||||||||||||||||
| Maw 1986 | X | X | |||||||||||||||||||||
| Casselbrant 2009 | X | X | X | X | |||||||||||||||||||
| Hammarén‐Malmi 2005 | X | ||||||||||||||||||||||
| Nguyen 2004 | X | ||||||||||||||||||||||
| Mattila 2003 | X | X | |||||||||||||||||||||
| Gates 1987 | X | X | X | X | |||||||||||||||||||
| Roydhouse 1980 | X |
AOM = acute otitis media OME = otitis media with effusion TT = tympanostomy tube
Adenoidectomy (with or without myringotomy) versus non‐surgical treatment or myringotomy only
Koivunen 2004 reported on 180 children aged 10 months to two years with at least three episodes of acute otitis media during the previous six months. They were randomly allocated to 1) adenoidectomy (n = 60), 2) chemoprophylaxis (n = 60) or 3) placebo (n = 60). The primary outcome was intervention failure in the first six months, which was defined as two or more episodes of acute otitis media in two months or at least three in six months, or middle ear effusion for at least two months. Secondary outcomes were mean number of 1) episodes of acute otitis media, 2) visits to a doctor, 3) antibiotic prescriptions and 4) days with symptoms (rhinitis, earache, fever). Follow up was two years.
Paradise 1999 reported on 304 children aged three to 15 years with recurrent acute otitis media or persistent otitis media with effusion. They were randomly allocated to 1) adenoidectomy (n = 100), 2) adenotonsillectomy (n = 103) or 3) the control group (n = 101). The primary outcome was the mean number of episodes of acute otitis media measured at 12, 24 and 36 months. Secondary outcomes were estimated proportion of time with acute otitis media, mean number of days with ear pain, mean number of days with antimicrobial treatment and the number of myringotomy and tympanostomy tube procedures. Follow up was three years.
Paradise 1990 reported on 99 children aged one to 15 years with recurrent acute otitis media after tympanostomy tube extrusion. They were randomly allocated to 1) adenoidectomy (n = 52) or 2) the control group (n = 47). The primary outcome was the proportion of time with otitis media and the number of episodes of otitis media with effusion. The secondary outcome measures were the number of tympanostomy tube procedures, the number of episodes of otorrhoea, and the numbers of days, respectively, on which ear pain occurred and antimicrobial treatment was received. Follow up was three years.
Gates 1987 reported on 491 children aged four to eight years with chronic effusion. They were randomly allocated to 1) bilateral myringotomy (n = 107), 2) bilateral tympanostomy tubes (n = 129), 3) adenoidectomy and bilateral myringotomy (n = 130) and 4) adenoidectomy and bilateral tympanostomy tubes (n = 125). Primary outcomes were time with effusion and time with hearing loss > 20 dB. Secondary outcome measures were median days to first recurrence of OME and number of surgical re‐treatments. Follow up was two years.
Fiellau‐Nikolajsen 1980 screened 463 three‐year‐old children with recurrent or persistent OME by tympanometry and otoscopy. Forty‐two children with an abnormal tympanogram, i.e. type B or C1/C2 for at least six months, were included in the trial. The children were randomly assigned to 1) myringotomy with adenoidectomy (n = 20) or to 2) myringotomy without adenoidectomy (n = 22). Primary outcome was type of tympanogram (A, C1, C2 or B). Secondary outcome was recovery time in months. Follow up was six months.
Rynnel‐Dagöö 1978 reported on 105 children aged less than 12 years with recurrent serous and purulent otitis media, frequent upper airway infections and nasal obstruction. After randomisation 29 children were excluded for various reasons, i.e. 76 children remained for analysis: 37 in the adenoidectomy group and 39 in the control group. Outcomes were change (better, deteriorated or unchanged) in frequency of common colds, purulent or serous otitis media and nasal obstruction. The follow up was two years.
In summary, the selected studies differed regarding the inclusion criteria and the outcomes measured.
Adenoidectomy with a unilateral tympanostomy tube versus a unilateral tympanostomy tube only; non‐operated ear examined for comparison
Dempster 1993 reported on 78 children, aged three to 12 years with bilateral otitis media with effusion based on otoscopy, an air bone gap > 15 dB, hearing levels > 25 dB HL and a type B tympanogram in both ears at two examinations with an interval of 12 weeks. The children were randomly assigned to 1) adenoidectomy with unilateral tube insertion (n = 37) or 2) unilateral tube insertion (n = 35). The primary outcomes were resolution of otitis media and improvement in hearing recorded at six and 12 months postoperatively by a validated otoscopist, tympanometry and pure‐tone audiometry. Follow up was one year.
Black 1990 reported on 149 children aged four to nine years with bilateral otitis media with effusion. All children were randomly assigned to 1) adenoidectomy with bilateral myringotomy and unilateral tympanostomy tube insertion (n = 37), 2) adenoidectomy with unilateral tympanostomy tube insertion (n = 38), 3) bilateral myringotomy and unilateral tympanostomy tube insertion (n = 37) and 4) unilateral tympanostomy tube insertion (n = 37). Outcome measures were mean hearing loss (dB) of the three worst heard frequencies between 250 Hz and 4000 Hz, resolution of effusion and parental views on their child's progress. Follow up was two years.
Maw 1986 reported on 150 children aged two to nine years with bilateral OME, subjective hearing loss, a mean hearing loss of > 25 dB and tympanograms other than type A, for at least three months. The children were randomised to 1) adenotonsillectomy (n = 47), 2) adenoidectomy (n = 47) or 3) neither (n = 56). Furthermore, all children received a tympanostomy tube in either the left or right ear by random allocation. Outcomes were resolution of effusion based on otoscopy and tympanometry. Pure tone audiometry was also performed. Follow up was one year.
In summary, inclusion criteria and outcome measures of the included studies were comparable.
Adenoidectomy with bilateral tympanostomy tubes versus bilateral tympanostomy tubes only
Casselbrant 2009 reported on 98 children aged 24 months to 47 months with bilateral or unilateral middle ear effusion. They were randomly assigned to 1) myringotomy and tympanostomy tube insertion (n = 32), 2) adenoidectomy with myringotomy and tympanostomy tube insertion (n = 32) or 3) adenoidectomy with myringotomy alone (n = 34). The primary outcome was percentage of time with middle ear effusion. Secondary outcomes were episodes of AOM, otorrhoea and OME, time to first recurrence, number of surgical procedures, treatment failures, complications and treatment sequelae. Follow up was 3 years.
Hammarén‐Malmi 2005 reported on 217 children aged one to four years with recurrent acute otitis media (162 children) or persistent otitis media with effusion (55 children) examined for at least six to eight weeks. They were randomly assigned to 1) adenoidectomy with insertion of bilateral tympanostomy tubes (n = 109) or 2) bilateral tympanostomy tube insertion without adenoidectomy (n = 108). The outcome was the mean number of otitis media episodes. Follow up was one year.
Nguyen 2004 reported on 72 patients aged 18 months to 18 years with recurrent acute otitis media and/or otitis media with effusion causing a conductive hearing loss > 30 dB. The children were randomly assigned to 1) bilateral tympanostomy tube insertion with adenoidectomy (n = 23) or 2) bilateral tympanostomy tube insertion without adenoidectomy (n = 40). The outcome measure was the rate of treatment failure (recurrence of AOM, persistent OME or reinsertion of ventilation tubes). Follow up was one year.
Mattila 2003 included 137 children aged one to two years out of 2497 children who were participating in a pneumococcal vaccine study (the Finnish Otitis Media Vaccine Trial). All included children experienced recurrent episodes of acute otitis media (with or without effusion); more than three to five events of AOM during the last six months, or four to six events during the last year. The children were randomly allocated to 1) bilateral tympanostomy tubes (n = 63) and 2) bilateral tympanostomy tubes and adenoidectomy (n = 74). Primary outcomes were the rate of all acute otitis media episodes (per person‐year) and the rates of acute otitis media episodes caused by S pneumonia, H influenza and M catarrhalis. The secondary outcome measure was the number of days with otorrhoea. Follow up was one year.
Gates 1987 reported on 491 children aged four to eight years with chronic effusion. They were randomly allocated to 1) bilateral myringotomy (n = 107), 2) bilateral tympanostomy tubes (n = 129), 3) adenoidectomy and bilateral myringotomy (n = 130) and 4) adenoidectomy and bilateral tympanostomy tubes (n = 125). Primary outcomes were time with effusion and time with hearing loss > 20 dB. Secondary outcome measures were median days to first recurrence of OME and number of surgical re‐treatments. Follow up was two years.
Roydhouse 1980 assessed 169 children aged two to 14 years with OME for at least two months. The 100 eligible children were randomly assigned to 1) bilateral tympanostomy tubes with adenoidectomy (n = 50) or 2) bilateral tympanostomy tubes without adenoidectomy (n = 50). The outcome measure was presence or absence of effusion. Absence of effusion was defined as type A or C1/C2 tympanogram or tympanostomy tubes in situ. Follow up was three years.
In summary, the included studies differed regarding the inclusion criteria and outcome measures.
Risk of bias in included studies
Figure 1 and Figure 2 show the results of the quality assessment according to the Cochrane Collaboration’s tool for assessing risk of bias. Figure 1 shows the judgements about each methodological quality item presented as percentages across all included trials; Figure 2 shows the judgements for each included trial separately.
1.
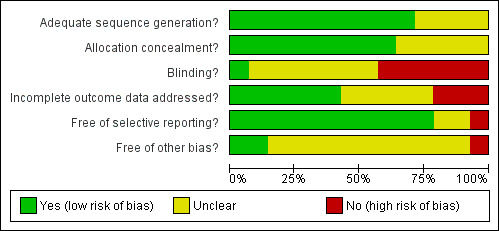
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
2.
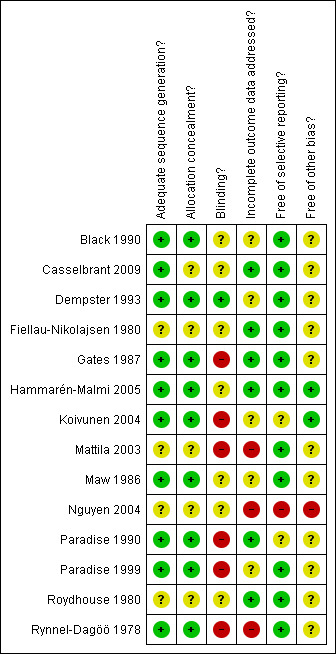
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Sequence generation and allocation concealment
In four out of 14 studies (29%) the risk of bias for sequence generation was classified as unclear (Fiellau‐Nikolajsen 1980; Mattila 2003; Nguyen 2004; Roydhouse 1980). In five out of 14 studies (36%) allocation concealment was classified as unclear (Casselbrant 2009; Fiellau‐Nikolajsen 1980; Mattila 2003; Nguyen 2004; Roydhouse 1980). The reasons are reported in the 'Risk of bias' tables under 'Characteristics of included studies'. Ten out of the 14 studies (71%) had a low risk of bias for sequence generation (Black 1990; Casselbrant 2009; Dempster 1993; Gates 1987; Hammarén‐Malmi 2005; Koivunen 2004; Maw 1986, Paradise 1990; Paradise 1999; Rynnel‐Dagöö 1978) and nine out of 14 studies (64%) had a low risk of bias for allocation concealment (Black 1990; Dempster 1993; Gates 1987; Hammarén‐Malmi 2005; Koivunen 2004; Maw 1986; Paradise 1990; Paradise 1999; Rynnel‐Dagöö 1978).
Blinding
Seven out of 14 studies (50%) had a high risk of bias for blinding (Gates 1987; Koivunen 2004; Mattila 2003; Nguyen 2004; Paradise 1990; Paradise 1999; Rynnel‐Dagöö 1978). In six out of 14 studies (43%) the risk of bias for blinding was unclear (Black 1990; Casselbrant 2009; Fiellau‐Nikolajsen 1980; Hammarén‐Malmi 2005; Maw 1986; Roydhouse 1980). Blinding was performed for the outcome assessor of the primary outcome in one study (7%) (Dempster 1993).
Incomplete outcome data
There was a high risk of bias for incomplete outcome data in three out of 14 studies (21%) (Mattila 2003; Nguyen 2004; Rynnel‐Dagöö 1978). The risk of bias was unclear in five studies (36%) (Black 1990; Dempster 1993; Koivunen 2004; Maw 1986; Paradise 1999) and low in six studies (43%) (Casselbrant 2009; Fiellau‐Nikolajsen 1980; Gates 1987; Hammarén‐Malmi 2005; Paradise 1990; Roydhouse 1980).
Selective outcome reporting
One study (7%) had a high risk of selective outcome reporting (Nguyen 2004). In two studies (14%) the risk of bias was unclear (Koivunen 2004; Paradise 1990). Eleven studies (79%) had a low risk of bias for selective outcome reporting (Black 1990; Casselbrant 2009; Dempster 1993; Fiellau‐Nikolajsen 1980; Gates 1987; Hammarén‐Malmi 2005; Maw 1986; Paradise 1999; Roydhouse 1980; Rynnel‐Dagöö 1978).
Other sources of bias
One study (7%) had a high risk of bias for other sources of bias (Nguyen 2004). In ten studies (71%) the risk of bias was unclear (Black 1990; Casselbrant 2009; Dempster 1993; Gates 1987; Fiellau‐Nikolajsen 1980; Mattila 2003; Maw 1986; Paradise 1999; Roydhouse 1980; Rynnel‐Dagöö 1978) and in three low (21%) (Hammarén‐Malmi 2005; Koivunen 2004; Paradise 1990).
Effects of interventions
Adenoidectomy (with or without myringotomy) versus non‐surgical treatment or myringotomy only
Koivunen 2004 showed that 26 children (43%) in the adenoidectomy group still had otitis media at six months and 43 children (76%) at 24 months. In the control group these numbers were 32 children (58%) at six months and 41 (79%) at 24 months. The corresponding difference rates, are ‐15% (95% confidence interval (CI) ‐3 to 33) and ‐3% (95% CI ‐13 to 19) at six and 24 months, respectively.
Differences at six months were calculated for the mean number of acute otitis media (AOM) episodes (0; 95% CI ‐0.4 to 0.4), sick child visits (0.6; 95% CI ‐0.3 to 1.5), antimicrobial prescriptions (‐0.1; 95% CI ‐0.6 to 0.5), days with earache (‐0.3; 95% CI ‐1.6 to 1.0) and days with fever (1.6; 95% CI ‐4.5 to 1.2).
Paradise 1999 reported that the mean rate of AOM episodes (> 10 days) during the first year was 1.8 per subject in the adenoidectomy group and 2.1 per subject in the control group. After two and three years the episode rates were 1.7 versus 1.2 and 1.3 versus 1.5, respectively.
The difference between the groups in percentage of subjects without AOM episodes was 9.6% (95% CI ‐5.1% to 24.4%) after one year; ‐10.9% (95% CI ‐28.0% to 6.2%) after two years; and ‐0.9% (95% CI ‐22.0% to 20.3%) after three years.
The mean number of days with earache per subject in the adenoidectomy and control group was 7.0 versus 8.1, 6.8 versus 6.8, and 5.4 versus 6.1 in the first, second and third year, respectively.
The number of days that subjects were treated with antibiotics was 50.2 versus 61.9, 44.6 versus 44.0, and 46.1 versus 42.1 in the first, second and third year, respectively. Since no standard deviations were reported we could not calculate standardised mean differences.
Paradise 1990 reported a mean proportion of time with otitis media during the first year of 15% in the adenoidectomy group and 27.4% in the control group. After two years this was 18% versus 27.2% respectively. The difference between the groups in proportion of time with otitis media was ‐12.2% (95% CI ‐31.4 to 6.9) after one year and ‐10.4% (95% CI ‐31.4 to 10.6) after two years. The mean number of episodes of otitis media with effusion in the adenoidectomy group and the control group was 1.06 versus 1.45, 1.09 versus 1.67, and 0.89 versus 0.87 in the first, second and third follow‐up year respectively
The number of tympanostomy tube procedures per subject in the adenoidectomy and the control group were 0.13 versus 0.29, 0.13 versus 0.26, and 0.08 versus 0.13 in the first, second and third year, respectively. The number of secondary otorrhoea episodes per subject in the adenoidectomy and the control group was 0.13 versus 0.13, 0.09 versus 0.04, and 0.05 versus 0.07 in the first, second and third year, respectively. The mean number of days with earache per subject was 3.99 versus 4.54, 4.21 versus 4.28, and 3.94 versus 5.08 in the first, second and third year, respectively. The mean number of days with antimicrobial treatment was 30.7 versus 43.2, 28.6 versus 45.3, and 30.8 versus 25.8 in the first, second and third year, respectively.
Gates 1987 reported that the mean time with effusion (± SD) in the myringotomy with adenoidectomy group was 0.302 (± 0.250) and in the myringotomy group 0.491 (± 0.252). The corresponding standardised mean difference (SMD) is ‐0.76 (95% CI ‐1.02 to ‐0.49).
The mean time with hearing loss > 20 dB (SD) for the better ear was 0.078 (± 0.131) in the myringotomy with adenoidectomy group and 0.186 (± 0.195) in the myringotomy group. The standardised mean difference (SMD) is ‐0.66 (95% CI ‐0.93 to ‐0.40). For the poorer ear these numbers were 0.220 (± 0.239) and 0.375 (± 0.253), respectively. The standardised mean difference (SMD) is ‐0.65 (95% CI ‐0.91 to ‐0.39).
Fiellau‐Nikolajsen 1980 showed that 68% of the children in the adenoidectomy group had normal ears (type A tympanogram) compared to 52% in the control group after six months of follow up. The risk differences (RD) were 15% (95% CI ‐5% to 36%) for a type A tympanogram and ‐2% (95% CI ‐30% to 26%) for recovery of effusion.
Rynnel‐Dagöö 1978 found an overall improvement regarding the frequency of common colds and otitis media in both the adenoidectomy and control group, but no difference was found between intervention groups.
Improvement in episodes of purulent otitis media, meaning a reduction in number of more than two episodes of illness, was found in 47% versus 49% after 12 months, and in 46% versus 52% after 24 months in the adenoidectomy and control group, respectively. The risk differences were ‐1% (95% CI ‐24% to 21%) and ‐6% (95% CI ‐30% to 18%).
Improvement in episodes of serous otitis media, defined as a change from existing to non‐existing serous secretion, was found in 19% versus 30% after 12 months, and in 31% versus 30% after 24 months in the adenoidectomy and control group, respectively. The risk differences were ‐10% (95% CI ‐30% to 9%) and 1% (95% CI ‐21% to 23%).
Three trials reported similar outcomes (Koivunen 2004; Paradise 1990; Paradise 1999), i.e. mean number of AOM episodes, mean number of antimicrobial prescriptions and mean number of days with earache, but the inclusion criteria and time of follow‐up measurements differed. Therefore, we could not perform a meta‐analysis.
Adenoidectomy with a unilateral tympanostomy tube versus a unilateral tympanostomy tube only; non‐operated ear examined for comparison
Meta‐analysis could be performed for the following.
1) Resolution of OME based on otoscopy.
Dempster 1993 (at six and 12 months).
Maw 1986 (at six and 12 months).
2) Resolution of OME measured by tympanometry.
Dempster 1993 (at six and 12 months).
Black 1990 (at seven weeks, six, 12 and 24 months).
Maw 1986 (at six and 12 months).
Resolution of OME based on otoscopy
Dempster reported that in 49% of the children in the adenoidectomy group the effusion had resolved after six months. In the control group this percentage was 26%. The risk difference was 23% (95% CI 1% to 45%).
Maw 1986 reported that the effusion had resolved in 49% of the children in the adenoidectomy group after six months. In the control group this was 17%. The risk difference was 31% (95% CI 11% to 51%).
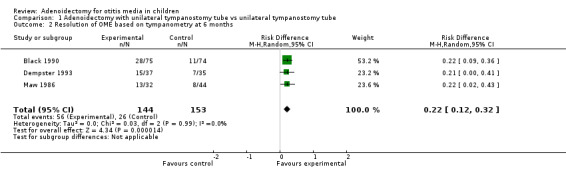
Analysis 1.1 shows no heterogeneity (I2 value 0%) between the two studies when considering number of children with resolution of OME by otoscopy at six months. The overall risk difference is 27% (95% CI 13% to 42%) (Figure 3).
1.1. Analysis.
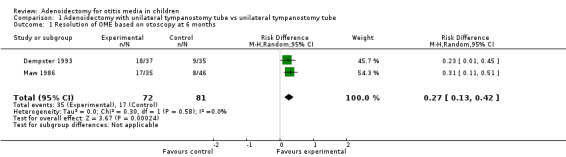
Comparison 1 Adenoidectomy with unilateral tympanostomy tube vs unilateral tympanostomy tube, Outcome 1 Resolution of OME based on otoscopy at 6 months.
3.
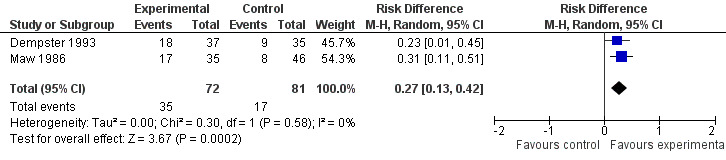
Forest plot of comparison: 1 Adenoidectomy with unilateral tympanostomy tube vs a unilateral tympanostomy tubes, outcome: 1.1 Resolution of OME based on otoscopy at 6 months.
The analysis considering this outcome at 12 months showed a high heterogeneity (I2 > 50%), suggesting that these trials differ too much to pool into a meta‐analysis.
Dempster 1993 showed 54% resolution of OME in the adenoidectomy group and 37% in the control group after 12 months. The risk difference was 17% (95% CI ‐6% to 40%).
Maw 1986 reported that in 69.4% of the children the effusion had resolved in the adenoidectomy group after 12 months. In the control group this percentage was 27.7%. The risk difference was 42% (95% CI 22% to 62%).
Resolution of OME measured by tympanometry
Dempster 1993 reported resolution of effusion in 41% of the children in the adenoidectomy group after six months compared to 20% in the control group. The risk difference was 21% (95% CI 0% to 41%). After 12 months the effusion had resolved in 51% of the children in the adenoidectomy group versus 31% of the control group. The risk difference was 20% (95% CI ‐2% to 42%).
Black 1990 reported resolution of effusion in 37% of the children in the adenoidectomy group versus 15% in the control group after six months. The risk difference was 22% (95% CI 9% to 36%). After 12 months the effusion had resolved in 41% of the children in the adenoidectomy group versus 9% in the control group. The risk difference was 32% (95% CI 19% to 45%).
Maw 1986 reported resolution of effusion in 41% of the children in the adenoidectomy group after six months compared to 18% of the control group. The risk difference was 22% (95% CI 2% to 43%). After 12 months the effusion had resolved in 58% of the children in the adenoidectomy group versus 28% in the control group. The risk difference was 30% (95% CI 8% to 52%).
According to Analysis 1.2 there is no heterogeneity (I2 value 0%) between studies when resolution of OME measured by tympanometry is considered at six months. The overall risk difference (RD) is 22% (95% CI 12% to 32%) (Figure 4).
1.2. Analysis.
Comparison 1 Adenoidectomy with unilateral tympanostomy tube vs unilateral tympanostomy tube, Outcome 2 Resolution of OME based on tympanometry at 6 months.
4.
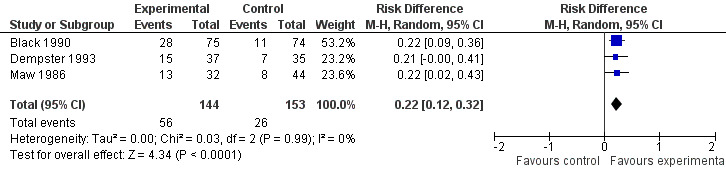
Forest plot of comparison: 1 Adenoidectomy with unilateral tympanostomy tube vs a unilateral tympanostomy tubes, outcome: 1.2 Resolution of OME based on tympanometry at 6 months.
According to Analysis 1.3 there is no heterogeneity (I2 value 0%) between studies when resolution of OME measured by tympanometry is considered at 12 months. The overall risk difference (RD) is 29% (95% CI 19% to 39%) (Figure 5).
1.3. Analysis.
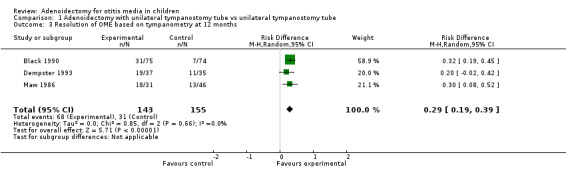
Comparison 1 Adenoidectomy with unilateral tympanostomy tube vs unilateral tympanostomy tube, Outcome 3 Resolution of OME based on tympanometry at 12 months.
5.
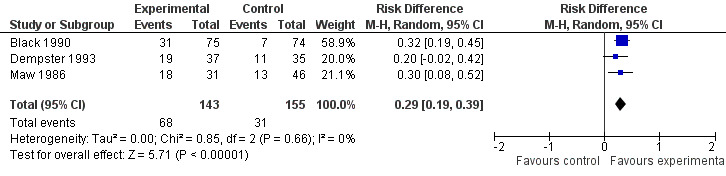
Forest plot of comparison: 1 Adenoidectomy with unilateral tympanostomy tube vs a unilateral tympanostomy tubes, outcome: 1.3 Resolution of OME based on tympanometry at 12 months.
Hearing loss (air conduction measured in dB HL) in children with OME
The analysis considering this outcome showed high heterogeneity (I2 > 50%), so these trials differ too much to pool into a meta‐analysis.
Dempster 1993 reported a mean air conduction HL of 18.0 dB (± 13.0) versus 21.1 dB (± 11.7) at six months, and 15.6 dB (± 8.4) versus 18.4 dB (± 10.6) at 12 months in the adenoidectomy and control group, respectively. The standardised mean differences (SMD) were ‐0.25 dB (95% CI ‐0.71 to 0.22) and ‐0.29 dB (95% CI ‐0.76 to 0.17), respectively.
Black 1990 reported only treatment group comparisons of change in mean audiometry scores (dB). Differences of 4.3 dB (95% CI ‐1.4 to 9.9) and 4.3 dB (95% CI ‐3.1 to 11.6) were found between the group with adenoidectomy and the group without adenoidectomy after six and 12 months, respectively.
Maw 1986 reported a mean air conduction HL of 20.4 dB (± 11.27) versus 36.5 dB (± 11.87) at six months, and 19.7 dB (± 10.36) versus 27.4 dB (± 12.13) after 12 months in the adenoidectomy and control group, respectively. The standardised mean differences (SMD) were ‐1.37 dB (95% CI ‐1.87 to ‐0.88) and ‐0.67 dB (95% CI ‐1.12 to ‐0.22).
Adenoidectomy with bilateral tympanostomy tubes versus bilateral tympanostomy tubes
Casselbrant 2009 reported the percentage of time with middle ear effusion of 18% in the adenoidectomy group and 12% in the control group during the first 18 months. After three years this was 21% and 19%, respectively. The difference in proportion of time was 6% (95% CI ‐12 to 24) after 18 months and 2% (95% CI ‐19 to 23) after 36 months.
After 18 months the number of episodes of AOM was seven and six in the adenoidectomy and the control group, respectively. The risk difference is 5% (95% CI ‐22 to 32). After 36 months the number of AOM episodes was 17 and 21 in the adenoidectomy and the control group. The risk difference is ‐18% (95% CI ‐37 to 1).
Hammarén‐Malmi 2005 reported a mean number of otitis media episodes of 1.73 (SD ± 1.8) in the tympanostomy tube with adenoidectomy group versus 1.44 (SD ± 1.5) in the tympanostomy tubes group. The standardised mean difference (SMD) was 0.17 (95% CI ‐0.11 to 0.45).
Nguyen 2004 reported 21.7% failures in the PET (pressure equalisation tubes) with adenoidectomy group and 42.5% failures in the PET group, with a risk difference (RD) of ‐21% (95% CI ‐44% to 2%) regarding treatment failure.
Mattila 2003 reported 2.05 episodes of acute otitis media per person‐year in the tympanostomy tubes with adenoidectomy group and 2.40 in the tympanostomy tubes group. Since no standard deviations were reported, we could not calculate standardised mean differences (SMD). The estimate efficacy, determined as 1 minus the RR adjusted for vaccination status, sex, number of siblings, and the preoperative number of otitis media episodes, of adenoidectomy with tympanostomy tubes versus tympanostomy tubes was 0.19 (95% CI ‐0.14 to 0.43).
Gates 1987 reported the mean time with effusion (± SD) in the tympanostomy tubes with adenoidectomy group was 0.258 (± 0.212) and in the tympanostomy tubes group 0.349 (± 0.235). The corresponding standardised mean difference (SMD) is ‐0.40 (95% CI ‐0.65 to ‐0.15).
The mean time with hearing loss > 20 dB (± SD) for the better ear was 0.065 (± 0.116) in the tympanostomy tubes with adenoidectomy group and 0.101 (± 0.141) in the tympanostomy tubes group. The standardised mean difference (SMD) is ‐0.23 (95% CI ‐0.48 to 0.02). For the poorer ear these numbers were 0.224 (± 0.221) and 0.304 (± 0.227), respectively. The standardised mean difference (SMD) is ‐0.35 (95% CI ‐0.60 to ‐0.11).
Roydhouse 1980 reported that 18% and 23% of all ears had effusion at 12 months in the tympanostomy tubes with adenoidectomy group and tympanostomy tubes group, respectively. These numbers were 15% and 18% after 24 months in both intervention groups, respectively. The risk differences were ‐5% (95% CI ‐8% to 17%) and ‐3% (95% CI ‐10% to 15%).
The trials were too heterogeneous to pool into a meta‐analysis.
Subgroup and sensitivity analysis
Since all three studies included in the meta‐analysis (Black 1990; Dempster 1993; Maw 1986) were of high quality and all used the best available non‐invasive objective diagnostic test for OME (tympanometry) as an objective outcome measure, sensitivity analysis excluding studies of either low quality or those not using tympanometry as an objective outcome measure was not possible.
For the other studies pooling was impossible and the outcome measures differed too much to perform sensitivity analysis. Due to the lack of data in the included studies concerning age, adenoid size and allergic rhinitis, factors that may modify the effect of adenoidectomy, it was not possible to perform subgroup analyses.
Complications and adverse effects
Five studies (Dempster 1993; Gates 1987; Koivunen 2004; Paradise 1999; Rynnel‐Dagöö 1978) reported information about postoperative complications. Gates 1987 reported on one child with recurring haemorrhage; Paradise 1999 reported on one patient with incipient malignant hyperthermia, one with postoperative pneumonia and two with transient postoperative velopharyngeal insufficiency. No haemorrhage occurred. In the studies by Koivunen 2004, Dempster 1993 and Rynnel‐Dagöö 1978 no complications occurred.
Discussion
Summary of main results
The most important findings are the 22% (95% CI 12% to 32%) and 29% (95% CI 19% to 39%) risk differences at six months and 12 months for children with persistent otitis media with effusion (OME) in the three pooled trials that compared adenoidectomy with unilateral tympanostomy tubes versus a unilateral tympanostomy tube alone, in which the non‐operated ears were used as the comparator.
The trials comparing adenoidectomy with or without myringotomy versus non‐surgical treatment or myringotomy alone, and adenoidectomy with bilateral tympanostomy tubes versus bilateral tympanostomy tubes alone, are more difficult to interpret because they include a heterogeneous patient population: some children had primarily recurrent acute otitis media (AOM), some had only OME and some had a combination of the two. Nevertheless, the effect of adenoidectomy on both AOM and hearing appears to be small and non‐significant.
The effects of adenoidectomy on changes of the tympanic membrane or cholesteatoma were not reported in any of the included trials.
Potential biases in the review process
During the review process potential biases were identified both in the individual trials and in the review process itself.
In only four trials a power analysis was provided and adequate numbers included (Black 1990; Dempster 1993; Gates 1987; Koivunen 2004). As the other trials included relatively few patients, their power may have been too low, leading to either a type I or type II error.
Loss to follow up was significant in most studies. This can be associated with either good or poor outcome. In three trials children were excluded after randomisation, which may have led to residual confounding (Mattila 2003; Paradise 1999; Rynnel‐Dagöö 1978).
Eight studies were analysed per protocol and no data were available to perform intention‐to‐treat analyses (Black 1990; Dempster 1993; Hammarén‐Malmi 2005; Mattila 2003; Maw 1986; Nguyen 2004; Paradise 1999; Rynnel‐Dagöö 1978). Per protocol analyses in which children who change groups are excluded may underestimate the treatment effect. In surgical trials only children in the watchful waiting group with severe complaints can change treatment group, whereas children in the surgical group who may experience similarly severe complaints cannot change treatment group. Analysing children on the basis of time spent in a treatment arm may over or underestimate the treatment effect.
Information bias may be considerable since trials on adenoidectomy, like most surgical trials, cannot be performed in a true double‐blind fashion. Such bias will overestimate the effect of the intervention.
All three studies included in the meta‐analysis for 'adenoidectomy with a unilateral tympanostomy tube versus unilateral tympanostomy tube only; non‐operated ear examined for comparison' (Black 1990; Dempster 1993; Maw 1986) randomised which ear (left or right) would receive the tympanostomy tube. Eustachian tube function has been shown to vary greatly between ears in individuals (Heerbeek 2003), therefore the validity of a paired organ design for otitis media may be limited.
Generalisability of the trials can be questioned since only a very small proportion of the eligible children undergoing adenoidectomy were included in the trials.
Due to the large variety of outcome measures used it was not possible to make a funnel plot to explore publication bias.
Due to the lack of data on factors that may modify the effect of adenoidectomy, such as age, adenoid size or allergic rhinitis, it was not possible to perform subgroup analyses and identify children that may benefit more or less from the operation.
The authors of this review were not blinded to authorship and origin of the included studies, since they knew most of the literature before embarking on this review.
Lastly, we could not include the results of the TARGET trial (TARGET), the largest and highest quality study to date on the effectiveness of adenoidectomy and tympanostomy tubes in children with otitis media with effusion, as the results have not yet been published. We expect to be able to include these results in the next update of this review.
Authors' conclusions
Implications for practice.
Our review shows a significant benefit of adenoidectomy as far as the resolution of middle ear effusion in children with otitis media with effusion (OME) is concerned. However, the benefit to hearing is small and the effects on changes in the tympanic membrane are unknown. The risks of operating should be weighed against these potential benefits.
The absence of a significant benefit of adenoidectomy for acute otitis media (AOM) suggests that routine surgery for this indication is not warranted.
Implications for research.
There is a need for good quality evidence on the effectiveness of adenoidectomy in children with otitis media. An individual patient data meta‐analysis, pooling the original data of trials performed in this area, could identify the subgroups that will benefit most from adenoidectomy.
What's new
| Date | Event | Description |
|---|---|---|
| 16 February 2010 | Amended | Declarations of interest updated. |
History
Protocol first published: Issue 2, 2009 Review first published: Issue 1, 2010
| Date | Event | Description |
|---|---|---|
| 28 April 2009 | Amended | Contact details updated. |
Acknowledgements
We acknowledge the work of Mohammed Attrach in the early stages of the protocol.
Appendices
Appendix 1. Search strategies for electronic databases
| CENTRAL | PubMed | EMBASE (Ovid) |
| #1 MeSH descriptor Adenoidectomy explode all trees #2 MeSH descriptor Adenoids explode all trees with qualifier: SU #3 adenoidectom* or adenotonsillectom* or adenotonsilectom* or adeno NEXT tonsillectomy* or adeno NEXT tonsilectom* #4 (#1 OR #2 OR #3) #5 MeSH descriptor Adenoids explode all trees #6 adenoid* or adenotonsil* #7 (#5 OR #6) #8 MeSH descriptor Surgical Procedures, Operative explode all trees #9 (surg*:ti or operat*:ti or excis*:ti or extract*:ti or remov*:ti or dissect*:ti or ablat*:ti or coblat*:ti or laser*:ti) #10 (#8 OR #9) #11 (#7 AND #10) #12 (#4 OR #11) #13 (nose OR nasal) NEAR (symptom* OR discharg* OR secret* OR obstruct*) #14 rhinorrhea OR rhinorrhoea #15 MeSH descriptor Nasal Obstruction explode all trees #16 airway* AND obstruct* #17 breath* AND impair* #18 MeSH descriptor Otitis Media explode all trees #19 middle NEXT ear NEXT (infect* OR inflam* OR disease*) #20 otitis OR aom OR ome #21 glue AND ear #22 (#13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21) #23 (#12 AND #22) | #1 "Adenoidectomy"[Mesh] #2 "Adenoids/surgery"[Mesh] #3 adenoidectom* [tiab] OR adenotonsillectom* [tiab] OR adenotonsilectom* [tiab] OR "adeno tonsillectomy" [tiab] OR "adeno tonsilectom" [tiab] #4 #1 OR #2 OR #3 #5 "Adenoids"/ [Mesh] #6 adenoid* [tiab] OR adenotonsil* [tiab] #7 #5 OR #6 #8 "Surgical Procedures, Operative"[Mesh] #9 "surgery"[Subheading] #10 surg* [tiab] OR operat* [tiab] OR excis* [tiab] OR extract* [tiab] OR remov* [tiab] OR dissect* [tiab] OR ablat* [tiab] OR coblat* [tiab] OR laser* [tiab] #11 #8 OR #9 OR #10 #12 #7 AND #11 #13 #4 OR #12 #14 (nose [tiab] OR nasal [tiab]) AND (symptom* [tiab] OR discharg* [tiab] OR secret* [tiab] OR obstruct* [tiab]) #15 rhinorrhea [tiab] OR rhinorrhoea [tiab] #16 "Nasal Obstruction"[Mesh] #17 airway* [tiab] AND obstruct* [tiab] #18 breath* [tiab] AND impair* [tiab] #19 "Otitis Media"[Mesh] #20 middle [tiab] AND ear [tiab] AND (infect* [tiab] OR inflam* [tiab] OR disease* [tiab]) #21 otitis [tiab] OR aom [tiab] OR ome [tiab] #22 glue [tiab] AND ear [tiab] #23 #14 OR #15 OR #16 | 1 adenoidectomy/ 2 (adenoidectom* or adenotonsillectom* or adenotonsilectom* or "adeno tonsillectomy*" or "adeno tonsilectom*").tw. 3 1 or 2 4 *Adenoid/ 5 (adenoid* or adenotonsil*).ti. 6 4 or 5 7 (surg* or operat* or excis* or extract* or remov* or dissect* or ablat* or coblat* or laser*).ti. 8 exp *Surgery/ 9 8 or 7 10 6 and 9 11 3 or 10 12 nose obstruction/ or rhinorrhea/ 13 *airway obstruction/ or *upper respiratory tract obstruction/ 14 ((nose or nasal) and (symptom* or discharg* or obstruct* or secret*)).tw. 15 (rhinorrhea or rhinorrhoea).tw. 16 (airway* and obstruct*).tw. 17 (breath* and impair*).tw. 18 exp Middle Ear Disease/ 19 (middle and ear and (infect* or inflamm* or disease*)).tw. 20 (otitis or aom or raom or ome).tw. 21 (glue and ear).tw. 22 21 or 17 or 12 or 20 or 15 or 14 or 18 or 13 or 16 or 19 23 22 and 11 |
| CINAHL (EBSCO) | Web of Science | BIOSIS Previews/CAB Abstracts (Ovid) |
| S1 (MH "Adenoidectomy") S2 (MH "Adenoids/SU") S3 adenoidectom* or adenotonsillectom* or adenotonsilectom* or "adeno tonsillectomy*" or "adeno tonsilectom*" S4 (MM "Adenoids") S5 TI adenoid* or adenotonsil* S6 TI surg* or operat* or excis* or extract* or remov* or dissect* or ablat* or coblat* or laser* S7 (MH "Surgery, Operative") S8 S6 or S7 S9 S4 or S5 S10 S8 and S9 S11 S1 or S2 or S3 or S10 | #1 TS=(adenoidectom* or adenotonsillectom* or adenotonsilectom* or "adeno tonsillectomy*" or "adeno tonsilectom*") #2 TI=(adenoid* or adenotonsil*) #3 TI=(surg* or operat* or excis* or extract* or remov* or dissect* or ablat* or coblat* or laser*) #4 #2 AND #3 #5 #1 OR #4 #6 TS=((nose or nasal) and (symptom* or discharg* or obstruct* or secret*)) #7 TS=(rhinorrhea or rhinorrhoea) #8 TS=(airway* and obstruct*) #9 TS=(breath* and impair*) #10 TS=(middle and ear and (infect* or inflamm* or disease*)) #11 TS=(otitis or aom or raom or ome) #12 TS=(glue and ear) #13 #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 #14 #5 AND #13 | 1 (adenoidectom* or adenotonsillectom* or adenotonsilectom* or "adeno tonsillectomy*" or "adeno tonsilectom*").tw. 2 (adenoid* or adenotonsil*).ti. 3 (surg* or operat* or excis* or extract* or remov* or dissect* or ablat* or coblat* or laser*).ti. 4 ((nose or nasal) and (symptom* or discharg* or obstruct* or secret*)).tw. 5 (rhinorrhea or rhinorrhoea).tw. 6 (airway* and obstruct*).tw. 7 (breath* and impair*).tw. 8 (middle and ear and (infect* or inflamm* or disease*)).tw. 9 (otitis or aom or raom or ome).tw. 10 (glue and ear).tw. 11 3 and 2 12 11 or 1 13 8 or 6 or 4 or 7 or 10 or 9 or 5 14 13 and 12 |
Appendix 2. Inclusion and exclusion criteria of studies included in this review
| Author | Inclusion criteria | Exclusion criteria |
| Black 1990 | Children with an operation indication for glue ear (secretory otitis media) based on the clinical judgement of the otolaryngologist | Children who had previous operations on their tonsils, adenoids or ears. Children with evidence of cleft palate or any sensorineural deafness. Children with conditions other than glue ear, such as gross nasal obstruction (where also adenoidectomy is indicated). |
| Casselbrant 2009 | Children aged 24 to 47 months, with a history of bilateral middle ear effusion (MEE) for at least 3 months, unilateral for 6 months or longer, or unilateral for 3 months after extrusion of one tympanostomy tube with the other still in place and patent, and who had completed a 10‐day course of a broad spectrum antimicrobial agent within the past month | Children with previous tonsillectomy and/or adenoidectomy, previous ear surgery other than tympanocentesis or myringotomy with or without tube insertion; history of seizure disorder, diabetes mellitus, asthma requiring daily medication, or any health condition that would make entry potentially disadvantageous to the child; medical conditions with predisposition for MEE, such as cleft plate, Down's syndrome, congenital malformations of the ear; cholesteatoma or chronic mastoiditis; severe retraction pockets; acute or chronic diffuse external otitis; perforation of the tympanic membrane; intracranial or intratemporal complications of MEE; upper respiratory obstruction attributable to tonsil or adenoid enlargement or both with cor pulmonale, sleep apnoea or severe dysphagia; conductive hearing loss attributable to destructive changes in the middle ear; sensorineural hearing loss; distance from CHP that would make follow up difficult. |
| Dempster 1993 | Otoscopic evidence of bilateral otitis media with effusion with a pure tone air conduction thresholds average over 0.5, 1 and 2 kHz of > 25 dB HL, and with an air bone gap over 0.5, 1 and 2 kHz of >25 dB, and a type B tympanogram | Children with previous adenoidectomy or aural surgery, or additional symptoms requiring surgical intervention, e.g. recurrent sore throat, or children with a cleft palate |
| Fiellau‐Nikolajsen 1980 | Persistent or recurrent secretory otitis media and tubal dysfunction at 3‐years old. Abnormal (type B, C1 or C2) tympanograms must be present at the 4 preoperative follow‐up points (duration preoperative follow‐up time was 7 months). | Parents refusal to operate on their children, cholesteatoma, previous operation for cleft palate |
| Gates 1987 | Bilateral chronic effusion diagnosed by otoscopists | Children with a history of previous tonsil or adenoid surgery, placement of TT (within 2 years), or cleft palate, or children with any severe chronic illness, were excluded. Also children with advanced or irreversible structural damage of the tympanum (such as cholesteatoma, perforation, atelectasis) were excluded. |
| Hammarén‐Malmi 2005 | Children with recurrent AOM (> 3 episodes of AOM during the preceding 6 months or > 5 episodes of AOM during the preceding 12 months) or a suspicion of chronic OME as judged by examination with a pneumatic otoscope | Previous adenotonsillar surgery or placement of tympanostomy tubes. Children with asthma, cleft palate, or diabetes or children who were judged to require prompt removal of adenoids because of obstructive symptoms resulting in continues mouth breathing or sleep apnoea, were excluded. |
| Koivunen 2004 | 3 or more episodes of acute otitis media in the last 6 months | Previously performed adenoidectomy or tympanostomy tube placement, cranial anomalies, documented immunological disorders and ongoing antimicrobial chemoprophylaxis |
| Mattila 2003 | 3 to 5 events of acute otitis media during the last 6 months or 4 to 6 events of acute otitis media during the last year | Nothing known about exclusion criteria |
| Maw 1986 | 1) Persistent subjective hearing difficulty 2) Pneumatic otoscopic confirmation of bilateral effusions 3) Symmetrical audiometric hearing loss, in excess of 25 dB at one or more frequencies 4) Impedance measurements not showing a peak A type of curve | 1) Resolution of effusions in 1 or both ears during 3 months preoperative follow up 2) Upper airway obstruction from gross adenoidal hyperplasia 3) Parents refusal of randomisation 4) Reappraisal of audiometric data, either because the loss was asymmetrical or because superadded sensorineural loss 5) Loss to preoperative follow up 6) At operation because either ear proved to be dry at myringotomy or because the contralateral ear was suspected to be dry |
| Nguyen 2004 | Children who required PET insertion as their first surgical treatment of OM with the following indications: 1) Recurrent OM with more than 3 episodes during the preceding 6 months or more than 4 during the preceding 12 months 2) OM with effusion persisting for more than 3 months or producing a conducting hearing loss > 30 dB with a type B tympanogram or 3) Both |
1) Previous PET insertion 2) Down's syndrome 3) Craniofacial anomalies such as cleft palate 4) Immune deficiency 5) Bleeding disorders 6) Ciliary dyskinesia 7) A follow‐up period of less than 6 months |
| Paradise 1990 | 1) A history of persistent and/or recurrent otitis media 2) To have thereafter received tympanostomy‐tube placement in one or both ears on one or more occasions, and to have 3) developed, after extrusion and within the year that preceded enrolment, one or more additional, well‐documented episodes of either suppurative (acute) otitis media or non‐suppurative (acute) otitis media. | Children with overt or submucous palatal clefts |
| Paradise 1999 | 1) At least 3 episodes of AOM during the preceding 6 months, or at least 4 episodes during the preceding 12 months including at least 1 episode during the preceding 6 months, with at least 1 of the episodes having been documented with recorded description of symptoms and tympanic membrane findings or confirmed by tympanometry or myringotomy; or 2) Middle ear effusion in one or both ears extending over at least 180 days during the preceding year and documented by at least 2 clinical observations at least 6 months apart, the most recent by a study‐team clinician and/or confirmed by tympanometry | Children with overt or submucous palatal clefts and children who have undergone previous tympanostomy tube placement |
| Roydhouse 1980 | Children with OME diagnosed on clinical grounds and with impedance audiometry | Children with a primary bias towards recurrent tonsillitis were not taken into this study |
| Rynnel‐Dagöö 1978 | Recurrent serous/purulent otitis media, frequent upper airway infections and nasal obstruction | Cases of severe nasal obstruction, previous operation performed, refused operation by parents, cases of recurring adenoids, diabetes or administrative mishaps |
Data and analyses
Comparison 1. Adenoidectomy with unilateral tympanostomy tube vs unilateral tympanostomy tube.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Resolution of OME based on otoscopy at 6 months | 2 | 153 | Risk Difference (M‐H, Random, 95% CI) | 0.27 [0.13, 0.42] |
| 2 Resolution of OME based on tympanometry at 6 months | 3 | 297 | Risk Difference (M‐H, Random, 95% CI) | 0.22 [0.12, 0.32] |
| 3 Resolution of OME based on tympanometry at 12 months | 3 | 298 | Risk Difference (M‐H, Random, 95% CI) | 0.29 [0.19, 0.39] |
Characteristics of studies
Characteristics of included studies [author‐defined order]
Black 1990.
| Methods | RCT | |
| Participants | 149 children aged 4 to 9 years with bilateral OME | |
| Interventions | Adenoidectomy with bilateral myringotomy (n = 37), adenoidectomy with a unilateral tube (n = 38), bilateral myringotomy (n = 37) and a unilateral tube (n = 37) | |
| Outcomes | Measured at 7 weeks, 6, 12 and 24 months:
|
|
| Notes | 15% of the children were lost to follow up after 12 months follow up and 39% after 24 months 48 children (32%) underwent further surgery during 24 months follow up Children who had undergone adenoidectomy were less likely to have further surgery (19% versus 45%) No intention‐to‐treat method was used for analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote 1: “we randomly divided the children in to one of four groups” “Randomisation between the right ear and the left ear for grommet insertion was also carried out” Quote 2: “Instructions about the treatment allocated were contained in sealed numbered envelopes. The contents of the envelopes were determined with a table of random numbers.” |
| Allocation concealment? | Low risk | Quote 1: “we randomly divided the children in to one of four groups” “Randomisation between the right ear and the left ear for grommet insertion was also carried out” Quote 2: “Instructions about the treatment allocated were contained in sealed numbered envelopes. The contents of the envelopes were determined with a table of random numbers.” |
| Blinding? All outcomes | Unclear risk | Quote: “The audiometricians were blind to treatment the children had received.” Comment: no information is provided about blinding of the otolaryngologist who retrieved the remaining data. Probably not since it is a surgical trial. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Quote 1: “Audiometric data were not obtained on every occasion in 22 children and therefore these children were omitted from the analysis.” Quote 2: “The data were initially analysed without taking into account any loss to follow up. The results are shown in table IV (raw data).” |
| Free of selective reporting? | Low risk | Comment: the main outcome measures 1) mean hearing loss (dB), 2) results of impedance tympanometry and 3) parental views on their child’s progress are reported |
| Free of other bias? | Unclear risk | Quote: “The only important methodological problem was the higher than predicted number of children who we were unable to follow up for two years. The principal reason for this was the clinicians dissatisfaction with a child’s progress, which they believed warranted further surgical intervention.” |
Casselbrant 2009.
| Methods | RCT | |
| Participants | 98 children aged 24 to 47 months, with a history of bilateral middle ear effusion (MEE) for at least 3 months, unilateral for 6 months or longer or unilateral for 3 months after extrusion of a tympanostomy tube, unresponsive to recent antibiotic. | |
| Interventions | 1) Myringotomy and tympanostomy tubes, 2) adenoidectomy, myringotomy and tympanostomy tube, 3) adenoidectomy and myringotomy | |
| Outcomes | Measured at 18 months and 36 months:
|
|
| Notes | Analysed with 'intention‐to‐treat' principle If MEE persisted bilaterally for 4 consecutive months or cumulatively for 6 of the previous 12 months, or unilateral MEE for 6 consecutive months or cumulatively for 8 months in the past 12 months, myringotomy and tympanostomy tube placement was performed in all children irrespective of initial random assignment and adenoidectomy was recommended to children initially randomised to myringotomy and tympanostomy tube placement. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "The children were randomly assigned within strata to defined by age (..), nasal obstruction (...), and previous history of M&T into one of three treatment groups (...). Children with one functioning tympanostomy tube were assigned to one of two treatment groups". Comment: the randomisation method was not specifically mentioned; one can assume that the randomisation was computer generated, since this was stratified. |
| Allocation concealment? | Unclear risk | Comment: no information provided |
| Blinding? All outcomes | Unclear risk | Comment: no information provided |
| Incomplete outcome data addressed? All outcomes | Low risk | Comment: the study was terminated before the number of the estimated sample size was reached due to low accrual rate and ending of the funding period. The length of follow up was equal in all three groups. For the analysis of 18 and 36 months only those children with full follow up were analysed. |
| Free of selective reporting? | Low risk | Comment: all reported outcome measures are reported on |
| Free of other bias? | Unclear risk | Comment: no information provided |
Dempster 1993.
| Methods | RCT | |
| Participants | 78 children aged 3 to 12 years with bilateral OME associated with hearing loss | |
| Interventions | Adenoidectomy with unilateral tube (n = 37), unilateral tube (n = 35) | |
| Outcomes | Measured at 6 and 12 months:
|
|
| Notes | 6 children (8%) were lost to follow up after 12 months follow up No re‐treatments occurred No intention‐to‐treat method was used for analysis No immediate postoperative complications were reported by surgeons |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “These 78 children were then (...) randomly allocated by a serially numbered envelope system. (...) The ears in each child were then randomly allocated by a similar process to have no ear surgery or to have a unilateral Shah grommet inserted following a radial myringotomy with aspiration of fluid” |
| Allocation concealment? | Low risk | Quote: “These 78 children were then (...) randomly allocated by a serially numbered envelope system. (...) The ears in each child were then randomly allocated by a similar process to have no ear surgery or to have a unilateral Shah grommet inserted following a radial myringotomy with aspiration of fluid” |
| Blinding? All outcomes | Low risk | Quote: “At six and 12 months post‐surgery, the presence or absence or otitis media in the non‐grommeted ear was recorded by the validated otoscopist who was blinded as to whether adenoidectomy had been performed and by tympanometry.” |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Quote: “(...) parents of 78 of them agreed to participate. Six children defaulted either at the six or 12 month assessment visits, leaving 72 children with complete clinical, audiometric and tympanometric data for the pre‐operative and these post‐operative visits.” Comment: these 6 children seem to be evenly distributed over both groups, however it is unclear whether they are clinically similar to the 72 children analysed |
| Free of selective reporting? | Low risk | Quote: “(...) the effect of adenoidectomy on resolution of otitis media with effusion, (..) the effect on the hearing of grommet insertion alone, adenoidectomy alone, and of adenoidectomy with grommet insertion could be assessed". Comment: all outcome measures are reported on |
| Free of other bias? | Unclear risk | Comment: each group consisted of a small number of children |
Fiellau‐Nikolajsen 1980.
| Methods | RCT | |
| Participants | 42 children aged 3 years with persistent or recurrent OME | |
| Interventions | Myringotomy with adenoidectomy (n = 20), myringotomy only (n = 22) | |
| Outcomes | Measured at 1, 3 and 6 months:
|
|
| Notes | No children were lost to follow up Intention‐to‐treat method was used for analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: “The children were divided by randomized, blind allocation (...).” Comment: no information provided on randomisation process |
| Allocation concealment? | Unclear risk | Quote: “The children were divided by randomized, blind allocation (...).” Comment: no information provided on randomisation process |
| Blinding? All outcomes | Unclear risk | Quote: “The children were divided by randomized, blind allocation (?).” Comment: no further information provided who was blinded (parents, outcome assessor?), however tympanometry was used as an objective measure to asses the primary outcome |
| Incomplete outcome data addressed? All outcomes | Low risk | Comment: all 42 children included in the trial are reported on and shown in the outcome tables |
| Free of selective reporting? | Low risk | Comment: the results of the pure tone audiometry and otomicroscopy at 1, 3 and 6 months postoperatively are reported on in Table 3 |
| Free of other bias? | Unclear risk | Comment: each group consisted of a small number of children |
Gates 1987.
| Methods | RCT | |
| Participants | 491 children aged 4 to 8 years with persistent bilateral OME | |
| Interventions | Bilateral myringotomy (n = 107), tympanostomy tubes (n = 129), bilateral myringotomy with adenoidectomy (n = 130), tympanostomy tubes with adenoidectomy (n = 125) | |
| Outcomes | Measured until 24 months:
|
|
| Notes | 17% of the children were lost to follow up after 12 months and 63% after 24 months follow up Surgical re‐treatment occurred and reported as an outcome Intention‐to‐treat method was used for analysis Complications: 1 patient had recurring haemorrhage |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote 1: “(...) the child was assigned by the statistician (who used tables of random numbers) to one of the four groups (..).” Quote 2: ”Randomization was done in blocks of 16 with each stratum to ensure even distribution of patients within the four groups across time.” |
| Allocation concealment? | Low risk | Quote 1: “(...) the child was assigned by the statistician (who used tables of random numbers) to one of the four groups (..).” Quote 2: "Randomization was done in blocks of 16 with each stratum to ensure even distribution of patients within the four groups across time." |
| Blinding? All outcomes | High risk | Quote: “An otolaryngologist in the study advised parents about the known advantages and disadvantages of the assigned treatment.” |
| Incomplete outcome data addressed? All outcomes | Low risk | Quote: “Eighty‐seven patients who were randomly assigned were not included in the analysis because they did not have an operation; the effusion cleared in 46 of them and parents of 41 refused to allow surgical treatment. These children were distributed equally across treatment groups and did not differ in any clinically important way from the other 491.” |
| Free of selective reporting? | Low risk | Quote: “The outcome measures, established a priori, were time with effusion, time with abnormal hearing, time to first recurrence of effusion, and number of surgical retreatments.” Comment: all outcome measures are reported in the results section |
| Free of other bias? | Unclear risk | Quote: “A potential source of bias is the six‐week period between observations. Thus, it is possible that the duration of effusion, time to first recurrence, and tube‐retention time were overestimated and that the number of recurrent effusions and the time to first recurrence after the tubes fell out were underestimated. Since the follow‐up procedures were applied uniformly to all groups, it is unlikely that this source of bias influenced the conclusions” Quote 2: “Entry into Group 1 was closed in November 1983 because of increased morbidity.” Comment: it is unclear how this information was obtained and what consequences it had for the objectivity of the following data collection |
Hammarén‐Malmi 2005.
| Methods | RCT | |
| Participants | 217 children aged 1 to 4 years with recurrent AOM or persistent OME | |
| Interventions | Tympanostomy tubes with adenoidectomy (n = 109), tympanostomy tubes (n = 108) | |
| Outcomes | Measured at 12 months:
|
|
| Notes | 19 children (9%) were lost to follow up after 12 months follow up 18 children (8%) underwent reinsertion of tympanostomy tubes No intention‐to‐treat‐method was used; patients who did not receive intervention as allocated were excluded from analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “These children were randomised in blocks of 8” |
| Allocation concealment? | Low risk | Quote: “These children were randomised in blocks of 8” |
| Blinding? All outcomes | Unclear risk | Comment: no information provided. Could be possible. |
| Incomplete outcome data addressed? All outcomes | Low risk | Quote: “The two randomisation groups were similar at the end of the follow‐up? (Table 1)” |
| Free of selective reporting? | Low risk | Quote: “The outcome measure was the number of otitis media episodes.” Comment: this is reported |
| Free of other bias? | Low risk | Comment: not including the data of 4 children in the tympanostomy‐only treatment arm who underwent adenoidectomy for recurrent otitis media did not influence the final outcome |
Koivunen 2004.
| Methods | RCT | |
| Participants | 180 children aged 10 months to 2 years with recurrent AOM | |
| Interventions | Adenoidectomy (n = 60), chemoprophylaxis (n = 60), placebo (n = 60) | |
| Outcomes | Primary outcome measured at 12 and 24 months:
Secondary outcomes measured until intervention failure, drop‐out, or 6 months of follow up, whichever came first:
|
|
| Notes | Duration of an episode is not described Follow up 24 months; 34 children (28%) were lost to follow up in the non‐adenoidectomy groups and 2 children (3%) were lost to follow up in the adenoidectomy group after 24 months follow up At the beginning of the study 12 children in the adenoidectomy group concurrently received tympanostomy tubes. During follow up 23 children (13%) (6 adenoidectomy, 6 chemoprophylaxis, 11 placebo) received tympanostomy tubes because of persistent middle ear fluid Intention‐to‐treat method was used for analysis No complications in the adenoidectomy procedures were reported by surgeons |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “We randomly assigned children to receive..(...) We performed block randomisation with a block size of six using numbered containers so that allocation was concealed from the investigator.” |
| Allocation concealment? | Low risk | Quote: “We performed block randomisation with a block size of six using numbered containers so that allocation was concealed from the investigator.” |
| Blinding? All outcomes | High risk | Quote: ”The sulfafurazole and placebo suspensions were given in a double blind fashion.” Comment: blinding for adenoidectomy vs. placebo was not possible. Outcome measures are subjective. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Quote: “Children in the sulfafurazole and placebo groups discontinued intervention and received anther prophylaxis more often than children in the adenoidectomy group (fig.1).” Comment: 1 child was lost to follow up in the adenoidectomy group, whereas 15 and 14 children were lost to follow up in the sulfafurazole and placebo group respectively. However, intention‐to‐treat analysis with all 180 randomised children was performed. |
| Free of selective reporting? | Unclear risk | Comment: all outcome measures are presented. The primary outcome in Table 2 and the secondary outcome measures in Table 3. |
| Free of other bias? | Low risk | Quote 1: “However, as the children in the placebo group and sulfafurazole groups discontinued the allocated intervention more often than the children in the adenoidectomy group (...), and as these children may have had more severe otitis media, this could have caused some bias by weakening the true effect of adenoidectomy.” Quote 2: “There are two other important sources of bias that may have diminished the true effect of the treatments: firstly, the use of symptom diaries to collect the outcome, and, secondly, the possibility of misdiagnoses". Comment: 12 children in the adenoidectomy group also received tympanostomy tubes |
Mattila 2003.
| Methods | A prospective trial with a randomised and non‐randomised arm; the randomised arm only was evaluated | |
| Participants | 137 children aged 1 to 2 years with recurrent AOM | |
| Interventions | Tympanostomy tubes (n = 63), tympanostomy tubes with adenoidectomy (n = 74) | |
| Outcomes | Measured until 24 months, per person‐year:
|
|
| Notes | All children received a pneumococcal vaccine (PncCRM or PncOMPC) before entering the trial 3 children (2%) were lost to follow up after 24 months follow up No intention‐to‐treat method was used for analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: “(...) he or she was randomized into 1 of 2 treatment groups.” Comment: no information provided |
| Allocation concealment? | Unclear risk | Quote: “The allocated treatment was not exposed to the parents or to the operation surgeon before the study was introduced and explained to the parents. If the parents showed willingness to participate, the randomly allocated treatment was revealed to them. At this point the parents were given the chance to not participate. (?) those children whose parents gave written consent were enrolled in the randomized trial (..).” |
| Blinding? All outcomes | High risk | Quote: “If the parents showed willingness to participate, the randomly allocated treatment was revealed to them. At this point the parents were given the chance to not participate.” |
| Incomplete outcome data addressed? All outcomes | High risk | Quote: “Of the 306 children randomized, 137 were enrolled in the trial. Of those enrolled, 63 were assigned to be treated with tympanostomy tubes (39% of the 162 randomized to have tympanostomy only) and 74 were assigned to be treated with concurrent tympanostomy tube placement and adenoidectomy (51% of the 144 children randomized to have concurrent tympanostomy and adenoidectomy).” |
| Free of selective reporting? | Low risk | Quote: “The main outcome measures were the rate of all acute otitis media episodes and the rates of otitis media episodes caused by S pneumoniae, H influenzae and M Catarrhalis. The secondary outcome measure was the number of days with otorrhea (?).” Comment: all these outcomes are reported |
| Free of other bias? | Unclear risk | Quote 1: “Thus, the design of the trial was unconventional in that the eligible children were randomized before the study subjects were enrolled.” Comment: baseline values between study groups are not equal for number of siblings and vaccination status Quote 2: “Thus, in the analysis the 5 children were transferred from the tympanostomy group to the tympanostomy and adenoidectomy group at the time of adenoidectomy." |
Maw 1986.
| Methods | RCT | |
| Participants | 150 children aged 2 to 9 years with persistent bilateral OME | |
| Interventions | Adenotonsillectomy with unilateral tube (n = 47), adenoidectomy with unilateral tube (n = 47), unilateral tube (n = 56) | |
| Outcomes | Measured at 6 and 12 months:
|
|
| Notes | 15 children (10%) were lost to follow up after 24 months follow up 12 children (26%) in the adenoidectomy group and 30 children (54%) in the control group had re‐insertion of tympanostomy tubes Method of analysis was unknown |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "From tables of random numbers the children were allocated (...)." |
| Allocation concealment? | Low risk | Quote: "From tables of random numbers the children were allocated (...)." |
| Blinding? All outcomes | Unclear risk | Quote: "Post operatively clinical otoscopic examinations were done in standard fashion by the same observer, who did not look at the case notes beforehand and was not aware of the operative subgroup." |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Quote: “13 cases were excluded at operation, either because an ear proved to be dry at myringotomy or because the contralateral ear was suspected to be dry.” Comment: however, 150 children were randomised and reported on in the baseline table Quote 2: “2 cases were excluded before six months because of gross nasal obstruction requiring adenoidectomy.” |
| Free of selective reporting? | Low risk | Comment: otoscopic and audiometric findings and tympanometric peak ‐ no peak conversion are reported |
| Free of other bias? | Unclear risk | Quote: "(..) of those having adenoidectomy 12 (26%) had 16 reinsertions; and in the no‐surgery group 30 (54%) had 47 reinsertions. (..) the difference between surgery and no‐surgery is significant at the 1% level." |
Nguyen 2004.
| Methods | RCT | |
| Participants | 72 patients aged 18 months to 18 years with recurrent AOM or OME | |
| Interventions | Tympanostomy tubes (n = 40), tympanostomy tubes with adenoidectomy (n = 23) | |
| Outcomes | Measured at 12 months:
|
|
| Notes | 9 children (12%) were lost to follow up after 12 months follow up Nothing known about re‐treatments Incidences of OM related to patient noncompliance with water‐protection (i.e. swimming‐related) were excluded from final analysis. No intention‐to‐treat method was used for analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: “patients were randomised to two groups.” |
| Allocation concealment? | Unclear risk | Comment: no information provided |
| Blinding? All outcomes | Unclear risk | Comment: no information provided |
| Incomplete outcome data addressed? All outcomes | High risk | Quote 1: “Two patients were not included in the final analysis because their adenoids were found to be completely obstructing their nasopharynx and subsequently underwent adenoidectomy.” Quote 2: “Seven patients did not complete the study because of incomplete follow‐up of less than 12 months. Of these seven patients, 5 (71%) were randomized to the experimental group.“ Comment: experimental group is tympanostomy tubes and adenoidectomy Comment: these 9 children were excluded from all analyses |
| Free of selective reporting? | High risk | Quote: “Selective demographic and clinical characteristics of patients in each subgroup are summarised in Table 1.” Comment: only the mean age, percentage of males, and the degree of adenoid hypertrophy in percentage are mentioned. No absolute numbers, therefore it is unclear whether this is data on 72 or 63 children. It is also unlikely that these are the only baseline data. Quote 2: “Incidences of otitis media related to patient non‐compliance with water protection were excluded from the final analysis.” |
| Free of other bias? | High risk | Quote 1: "For ethical reasons, patients found to have adenoids completely obstructing their nasopharynx underwent adenoidectomy, despite their initial randomisation.” Comment: randomisation did not successfully create two equal groups. Age and degree of adenoid hypertrophy differed between the two groups (Table 1). Comment: follow‐up data were obtained by retrospectively filled out questionnaires at least every 6 months. This could have lead to recall bias. |
Paradise 1990.
| Methods | Two parallel randomised clinical trials; one‐arm RCT only valued | |
| Participants | 99 children aged 1 to 15 years with either recurrent AOM or persistent OME after tympanostomy tube extrusion | |
| Interventions | Adenoidectomy (n = 52), control group (n = 47) | |
| Outcomes | Measured at 12, 24 and 36 months:
|
|
| Notes | 13% of the children were lost to follow up after 12 months, 27% after 24 months and 47% after 36 months follow up Children with OME at inclusion who did not respond to antibiotic therapy underwent tympanostomy tube placement In the adenoidectomy group 1 child underwent repeat adenoidectomy, in the control group 17 children underwent adenoidectomy The data were analysed in 2 modes: per protocol (i.e. the children who switched treatment arm or were lost to follow up without completing the full year were not analysed for the whole year outcomes) and intention‐to‐treat for the primary outcome measure |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "The 99 of these children whose parents gave consent were assigned randomly." Comment: probably done since other similar trial reports “separate computer generated random number lists were used for the assignments” |
| Allocation concealment? | Low risk | Comment: no information provided, probably done since other similar trial reports “separate computer generated random number lists were used for the assignments”. |
| Blinding? All outcomes | High risk | Comment: no information provided, probably not done since it is a surgical intervention trial However, tympanometry was performed during most visits to objectively confirm the primary outcome measure |
| Incomplete outcome data addressed? All outcomes | Low risk | Quote 1: "Not included in the tables are data derived from experiences of less than a full year in an assigned treatment group that resulted from either failure to complete the year or a change in treatment group." Quote 2: "An alternative 'intention‐to‐treat analysis', (...) gave closely similar results." |
| Free of selective reporting? | Unclear risk | Quote: "(...) not included in the tables are data derived from experiences of less than a full year in an assigned treatment group that resulted from either failure to complete the year or a change in treatment group." |
| Free of other bias? | Unclear risk | Comment: no information provided. For all children to start the trial without OME, children with OME at assignment received antibiotic therapy. This occurred more often in the control group. However, data collection for the adenoidectomy group started later than the control group. |
Paradise 1999.
| Methods | Two parallel randomised clinical trials; 3‐way trial only valued | |
| Participants | 304 children aged 3 to 15 years with either recurrent AOM or persistent OME | |
| Interventions | Adenoidectomy (n = 100), adenotonsillectomy (n = 103), control group (n = 101) | |
| Outcomes | Measured at 12, 24 and 36 months:
|
|
| Notes | 23% of the children were lost to follow up after 12 months, 34% after 24 months and 47% after 36 months follow up 11 children (4%) had insertion of tympanostomy tubes during follow up The author noted data were analysed in 2 modes, published data not according intention‐to‐treat method |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “The children were then assigned randomly (...). Separate, computer generated random number lists were used for the assignments.” |
| Allocation concealment? | Low risk | Quote: “The children were then assigned randomly (...). Separate, computer generated random number lists were used for the assignments.” |
| Blinding? All outcomes | High risk | Comment: no information provided, probably not done since it is a surgical intervention trial However, tympanometry was performed during most visits to objectively confirm the primary outcome measure |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Quote: “304 were eligible for the 3‐way trial. (..) A total of 47 subjects assigned to surgical treatment groups were withdrawn from the trials without undergoing surgery, in some instances because the parents lacked insurance coverage. (..) Four subjects assigned to control status were also withdrawn. To conserve resources, these 51 withdrawn subjects were discharged from the study. (..) Accordingly, follow‐up data were available for 266 children in the 3‐way trial.” Comment: it is possible that the children withdrawn from the study with a lower socio‐economic status have a higher risk of AOM and OME. This might possibly have influenced the outcome. Intention‐to‐treat analysis was performed for the primary outcome measure |
| Free of selective reporting? | Low risk | Quote: “Data concerning the remaining outcome measures are summarized in table 4.” |
| Free of other bias? | Unclear risk | Comment: no information provided. For all children to start the trial without OME, children with OME at assignment received antibiotic therapy. This occurred more often in the control group. However, data collection for the adenoidectomy group started later than the control group. |
Roydhouse 1980.
| Methods | RCT | |
| Participants | 169 children aged 2 to 14 years with persistent OME | |
| Interventions | Tympanostomy tubes with adenoidectomy (n = 50), tympanostomy tubes (n = 50), control group (n = 69) | |
| Outcomes | Measured at 12, 24 and 36 months:
|
|
| Notes | 5 children (3%) were lost to follow up after 12 months, 22 children (13%) after 24 months and 38 (22%) after 36 months follow up 24 children (53%) required repeat insertions in the adenoidectomy group and 31 children (62%) in control group “Children without effusion” were defined as children with type A or type C tympanograms, children who had tympanostomy tubes in place or children who had persistent perforations following extrusion of the tube |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Group A includes those cases who by random selection underwent adenoidectomy and insertion of aeration tubes." Comment: no information provided |
| Allocation concealment? | Unclear risk | Quote: “Group A includes those cases who by random selection underwent adenoidectomy and insertion of aeration tubes.“ Comment: no information provided |
| Blinding? All outcomes | Unclear risk | Comment: no information provided |
| Incomplete outcome data addressed? All outcomes | Low risk | Comment: all information is provided for all patients still included per year. The reasons for loss to follow up are reported and equal in both groups. |
| Free of selective reporting? | Low risk | Comment: all outcomes are reported. Extra outcomes reported are number of relapses and the relation to adenoid size. |
| Free of other bias? | Unclear risk | Comment: no information provided |
Rynnel‐Dagöö 1978.
| Methods | Prospective controlled study | |
| Participants | 105 children aged less than 12 years with recurrent AOM/OME, frequent upper airway infections and nasal obstruction | |
| Interventions | Adenoidectomy (n = 37), control group (n = 39) | |
| Outcomes | Measured at 12 and 24 months:
|
|
| Notes | 11% of the children were lost to follow up (8% in the adenoidectomy group and 13% in the control group) after 24 months follow up 35% of the children in the adenoidectomy group and 56% of the children in the control group had insertion of tympanostomy tubes. When those children still had tubes at the end of the trial they were excluded for analysis (8% in the adenoidectomy group and 3% in the control group) No intention‐to‐treat‐method was used for analysis No complications were reported by surgeons |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: “All children (...) received a number between 0‐105 randomly acquired by casting of lots. Children with even numbers came to belong to the adenoidectomy group and those with odd numbers to the control group.” |
| Allocation concealment? | Low risk | Quote: “All children (...) received a number between 0‐105 randomly acquired by casting of lots. Children with even numbers came to belong to the adenoidectomy group and those with odd numbers to the control group.” |
| Blinding? All outcomes | High risk | Quote: “(..) we were naturally aware of whether the children belonged to the A‐ or C‐group.” |
| Incomplete outcome data addressed? All outcomes | High risk | Quote: “Twenty‐nine children were omitted for reasons shown in Table 1, leaving 76 children to participate in the investigation.” Comment: these children were excluded after randomisation. The most common reasons were severe nasal obstruction and administrative mishaps. It is unclear whether the 29 omitted children were otherwise clinically similar to the 76 children included in the study. |
| Free of selective reporting? | Low risk | Comment: all outcomes are reported on (nasopharyngeal flora, improvement, unchanged or deterioration in episodes of common colds, purulent otitis media, serous otitis media, and nasal obstruction) |
| Free of other bias? | Unclear risk | Quote 1: “(...) data concerning frequency of illnesses were obtained retrospectively by interviews with the parents.” Comment: each group consisted of a small number of children |
AOM = acute otitis media MEE = middle ear effusion OME = otitis media with effusion RCT = randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Black 1986 | Same study as Black 1990; first 100 children were analysed No additional data were published |
| Bulman 1984 | Allocation: not concealed Participants: selection of patients not restricted by clear boundaries; not all had bilateral OME and bilateral similar deafness. Preoperative middle ear effusion only measured for 6 weeks. Outcome measures: ‘Adenoidectomy only’ versus ‘Control’ are the only two groups that can be compared; 15 versus 14 patients were allocated to those groups. Overall, results of the different intervention groups are impossible to differentiate. |
| Fiellau‐Nikolajsen 1982 | Same study as Fiellau‐Nikolajsen 1980 |
| Gates 1988 | Same study as Gates 1987 |
| Gates 1989 | Same study as Gates 1987. Outcome measures: results are specified on adenoid size (in our study this is not an outcome). |
| Marshak 1980 | Allocation: non‐randomised controlled study |
| Maw 1983 | Same study as Maw 1986 |
| Maw 1985a | Same study as Maw 1986 |
| Maw 1985b | Same study as Maw 1986 |
| Maw 1987 | Same study as Maw 1986 |
| Maw 1988 | Same study as Maw 1986 |
| Maw 1993 | This study was excluded because data from the adenoidectomy group could not be analysed separately from those undergoing adenotonsillectomy. The authors combined the adenoidectomy group and the adenotonsillectomy group because in the study Maw 1986 adenotonsillectomy appeared to have no additional benefit compared to adenoidectomy alone. |
| Maw 1994a | Same study as Maw 1993, long‐term effect |
| Maw 1994b | Same study as Maw 1986 |
| Widemar 1982 | Allocation: randomisation process (used date of birth to randomise) Same study as Widemar 1985. The first year follow up of 44 children is presented. |
| Widemar 1985 | Allocation: randomisation process (used date of birth to randomise) Participants: only data from 59 children were used for analysis because 19 children were excluded after randomisation Intervention: a total of 13 and 22 tympanostomy tubes were inserted in groups A and C, respectively. They excluded the children that still had unilateral or bilateral tubes at the time of comparison. |
OME = otitis media with effusion
Characteristics of ongoing studies [ordered by study ID]
FATA.
| Trial name or title | FATA: Food Allergy ‐ Tubes ‐ Adenoids trial |
| Methods | RCT |
| Participants | Children up to 4 years of age, with otoscopic and tympanometric signs of OME for 3 months or more, with lack of improvement after antibiotics for 3 months, with > 3 episodes of AOM in the preceding 6 months or > 5 in the preceding 12 months, bilateral conductive hearing loss of 15 dB or more and without previous adenotonsillar surgery or tympanostomy tube placement, or inhalent allergies including asthma |
| Interventions | 1) Bilateral myringotomy with tympanostomy tubes 2) Bilateral myringotomy with tympanostomy tubes and food allergy testing and management 2) Bilateral myringotomy with tympanostomy tubes, adenoidectomy and food allergy testing and management |
| Outcomes | Number of otitis media episodes |
| Starting date | 1 October 2008 |
| Contact information | Y. Paik, Department of Otolaryngology ‐ Head and Neck Surgery, University Hospital, Columbia, Missouri, United States, 65212 PaikY@health.missouri.edu |
| Notes | — |
NOA.
| Trial name or title | NOA: Netherlands Adenoidectomy Study |
| Methods | RCT, follow up of 2 years |
| Participants | 111 children aged 1 to 6 years selected for adenoidectomy, with or without myringotomy, because of recurrent or chronic upper respiratory tract infections (common colds, rhinosinusitis) |
| Interventions | 1) Adenoidectomy, with or without myringotomy, within 6 weeks 2) Watchful waiting strategy |
| Outcomes | Primary outcome measure:
Secondary outcome measures:
|
| Starting date | 1 April 2007 |
| Contact information | A. Schilder, Department of Otorhinolaryngology & Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht, Netherlands |
| Notes | — |
TARGET.
| Trial name or title | TARGET: trial of alternative regimens in glue ear treatment ‐ effectiveness of surgery for otitis media with effusion in 3.5 to 7‐year olds using multiple developmental and economic measures combined with classical clinical measures |
| Methods | RCT |
| Participants | Children aged 3.5 to 7 years without previous ear or adenoid surgery, with B+B or B+C2 tympanograms and a bilateral average hearing threshold > 20 dB and an air‐bone gap > 10 dB HL |
| Interventions | 1) Ventilation tube insertion alone 2) Ventilation tube insertion plus adenoidectomy 3) Observation + medical management |
| Outcomes | Clinical measures ‐ otoscopy, audiometry, tympanometry and questionnaire measures, (hearing and predictive factors, general health, economic impact, behavioural assessment and quality of life |
| Starting date | 1 April 1994 |
| Contact information | M. Haggard, Institute of Hearing Research, Nottingham, UK |
| Notes | — |
Differences between protocol and review
This review is based on the protocol 'Adenoidectomy for recurrent or chronic nasal symptoms and middle ear disease in children up to 18 years of age' (van den Aardweg 2009). After finalising the first draft of the review in which we combined recurrent or chronic nasal symptoms and middle ear disease, there was a general consensus that the review would benefit from being split into two separate reviews; one looking at the effects of adenoidectomy on nasal symptoms (van den Aardweg 2010) and the other at the effect of otitis media (this review).
Further, some minor changes from the protocol have been carried out in this review. Quasi‐randomised trials are explicitly excluded because they have an increased risk of selection bias. The diagnosis of the participating children is more clearly described, i.e. "diagnosed with otitis media" has been added to "children up to 18 years of age". Finally, both the comparisons and the definition of non‐surgical management in the 'Types of interventions' section have been defined more clearly.
Contributions of authors
Maaike van den Aardweg was lead author, selected eligible studies, assessed trial quality, performed data extraction, analysed and interpreted the data, drafted and revised the review and approved the final content.
Anne Schilder initiated the review, revised the review and approved the final content.
Ellen Herkert selected eligible studies, performed data extraction, analysed and interpreted the data, drafted the review and approved the final content.
Chantal Boonacker assessed trial quality, analysed the data, revised the review and approved the final content.
Maroeska Rovers initiated the review, analysed and interpreted the data, revised the review and approved the final content.
Sources of support
Internal sources
Department of Otorhinolaryngology, University Medical Center Utrecht, Netherlands.
Julius Center for Health Services and Primary Health Care, University Medical Center Utrecht, Netherlands.
External sources
ZonMw (Netherlands Organisation for Health Research and Development), Netherlands.
Declarations of interest
At the time of publication Chantal Boonacker and Maaike van den Aardweg were involved in a Nederlands Onderzoek Adenotomie (NOA) trial entitled 'A RCT on the effectiveness of adenoidectomy in children with recurrent or chronic upper respiratory tract infections' (see 'Characteristics of ongoing studies').
Maroeska Rovers and Anne Schilder have participated in workshops and educational activities on otitis media for GlaxoSmithKline.
Edited (no change to conclusions)
References
References to studies included in this review
Black 1990 {published data only}
- Black NA, Sanderson CF, Freeland AP, Vessey MP. A randomised controlled trial of surgery for glue ear. BMJ 1990;300(6739):1551‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Casselbrant 2009 {published data only}
- Casselbrant ML, Mandel EM, Rockette HE, Kurs‐Lasky M, Fall PA, Bluestone CD. Adenoidectomy for otitis media with effusion in 2‐3‐year‐old children. International Journal of Pediatric Otorhinolaryngology 2009;Oct 9:[Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dempster 1993 {published data only}
- Dempster JH, Browning GG, Gatehouse SG. A randomized study of the surgical management of children with persistent otitis media with effusion associated with a hearing impairment. Journal of Laryngology and Otology 1993;107(4):284‐9. [DOI] [PubMed] [Google Scholar]
Fiellau‐Nikolajsen 1980 {published data only}
- Fiellau‐Nikolajsen M, Falbe‐Hansen J, Knudstrup P. Adenoidectomy for middle ear disorders: a randomized controlled trial. Clinical Otolaryngology and Allied Sciences 1980;5(5):323‐7. [DOI] [PubMed] [Google Scholar]
Gates 1987 {published data only}
- Gates GA, Avery CA, Prihoda TJ, Cooper JC. Effectiveness of adenoidectomy and tympanostomy tubes in the treatment of chronic otitis media with effusion. New England Journal of Medicine 1987;317(23):1444‐51. [DOI] [PubMed] [Google Scholar]
Hammarén‐Malmi 2005 {published data only}
- Hammarén‐Malmi S, Saxen H, Tarkkanen J, Mattila PS. Adenoidectomy does not significantly reduce the incidence of otitis media in conjunction with the insertion of tympanostomy tubes in children who are younger than 4 years: a randomized trial. Pediatrics 2005;116(1):185‐9. [DOI] [PubMed] [Google Scholar]
Koivunen 2004 {published data only}
- Koivunen P, Uhari M, Luotonen J, Kristo A, Raski R, Pokka T, et al. Adenoidectomy versus chemoprophylaxis and placebo for recurrent acute otitis media in children aged under 2 years: randomised controlled trial. BMJ 2004;328(7438):487. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mattila 2003 {published data only}
- Mattila PS, Joki‐Erkkila VP, Kilpi T, Jokinen J, Herva E, Puhakka H. Prevention of otitis media by adenoidectomy in children younger than 2 years. Archives of Otolaryngology ‐ Head and Neck Surgery 2003;129(2):163‐8. [DOI] [PubMed] [Google Scholar]
Maw 1986 {published data only}
- Maw AR, Herod F. Otoscopic, impedance, and audiometric findings in glue ear treated by adenoidectomy and tonsillectomy. A prospective randomised study. Lancet 1986;1(8495):1399‐402. [DOI] [PubMed] [Google Scholar]
Nguyen 2004 {published data only}
- Nguyen LH, Manoukian JJ, Yoskovitch A, Al Sebeih KH. Adenoidectomy: selection criteria for surgical cases of otitis media. Laryngoscope 2004;114(5):863‐6. [DOI] [PubMed] [Google Scholar]
Paradise 1990 {published data only}
- Paradise JL, Bluestone CD, Rogers KD, Taylor FH, Colborn DK, Bachman RZ, et al. Efficacy of adenoidectomy for recurrent otitis media in children previously treated with tympanostomy‐tube placement. Results of parallel randomized and nonrandomized trials. JAMA 1990;263(15):2066‐73. [PubMed] [Google Scholar]
Paradise 1999 {published data only}
- Paradise JL, Bluestone CD, Colborn DK, Bernard BS, Smith CG, Rockette HE, et al. Adenoidectomy and adenotonsillectomy for recurrent acute otitis media: parallel randomized clinical trials in children not previously treated with tympanostomy tubes. JAMA 1999;282(10):945‐53. [DOI] [PubMed] [Google Scholar]
Roydhouse 1980 {published data only}
- Roydhouse N. Adenoidectomy for otitis media with mucoid effusion. Annals of Otology, Rhinology, and Laryngology. Supplement 1980;89(3 Part 2):312‐5. [DOI] [PubMed] [Google Scholar]
Rynnel‐Dagöö 1978 {published data only}
- Rynnel‐Dagöö B, Ahlbom A, Schiratzki H. Effects of adenoidectomy: a controlled two‐year follow‐up. Annals of Otology, Rhinology and Laryngology 1978;87(2 Part 1):272‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Black 1986 {published data only}
- Black N, Crowther J, Freeland A. The effectiveness of adenoidectomy in the treatment of glue ear: a randomized controlled trial. Clinical Otolaryngology and Allied Sciences 1986;11(3):149‐55. [DOI] [PubMed] [Google Scholar]
Bulman 1984 {published data only}
- Bulman CH, Brook SJ, Berry MG. A prospective randomized trial of adenoidectomy vs grommet insertion in the treatment of glue ear. Clinical Otolaryngology and Allied Sciences 1984;9(2):67‐75. [DOI] [PubMed] [Google Scholar]
Fiellau‐Nikolajsen 1982 {published data only}
- Fiellau‐Nikolajsen M, Hojslet PE, Felding JU. Adenoidectomy for Eustachian tube dysfunction: long‐term results from a randomized controlled trial. Acta Oto‐Laryngologica. Supplement 1982;386:129‐31. [Google Scholar]
Gates 1988 {published data only}
- Gates GA, Avery CA, Prihoda TJ. Effect of adenoidectomy upon children with chronic otitis media with effusion. Laryngoscope 1988;98(1):58‐63. [DOI] [PubMed] [Google Scholar]
Gates 1989 {published data only}
- Gates GA, Avery CA, Cooper JC Jr, Prihoda TJ. Chronic secretory otitis media: effects of surgical management. Acta Oto‐Laryngologica. Supplement 1989;138:2‐32. [DOI] [PubMed] [Google Scholar]
Marshak 1980 {published data only}
- Marshak G, Neriah ZB. Adenoidectomy versus tympanostomy in chronic secretory otitis media. Annals of Otology, Rhinology, and Laryngology. Supplement 1980;89(3 Part 2):316‐8. [DOI] [PubMed] [Google Scholar]
Maw 1983 {published data only}
- Maw AR. Chronic otitis media with effusion (glue ear) and adenotonsillectomy: prospective randomised controlled study. British Medical Journal (Clinical Research Ed) 1983;287(6405):1586‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maw 1985a {published data only}
- Maw AR. The long term effect of adenoidectomy on established otitis media with effusion in children. Auris Nasus Larynx 1985;12(Suppl 1):S234‐6. [DOI] [PubMed] [Google Scholar]
Maw 1985b {published data only}
- Maw AR. Factors affecting adenoidectomy for otitis media with effusion (glue ear). Journal of the Royal Society of Medicine 1985;78(12):1014‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maw 1987 {published data only}
- Maw AR. The effectiveness of adenoidectomy in the treatment of glue ear: a randomized controlled trial. Clinical Otolaryngology and Allied Sciences 1987;12(2):155‐6. [DOI] [PubMed] [Google Scholar]
Maw 1988 {published data only}
- Maw AR, Parker A. Surgery of the tonsils and adenoids in relation to secretory otitis media in children. Acta Oto‐Laryngologica. Supplement 1988;454:202‐7. [DOI] [PubMed] [Google Scholar]
Maw 1993 {published data only}
- Maw AR, Bawden R. Spontaneous resolution of severe chronic glue ear in children and the effect of adenoidectomy, tonsillectomy, and insertion of ventilation tubes (grommets). BMJ 1993;306(6880):756‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maw 1994a {published data only}
- Maw AR, Bawden R. The long term outcome of secretory otitis media in children and the effects of surgical treatment: a ten year study. Acta Oto‐Rhino‐Laryngologica Belgica 1994;48(4):317‐24. [PubMed] [Google Scholar]
Maw 1994b {published data only}
- Maw AR, Bawden R. Does adenoidectomy have an adjuvant effect on ventilation tube insertion and thus reduce the need for re‐treatment?. Clinical Otolaryngology and Allied Sciences 1994;19(4):340‐3. [DOI] [PubMed] [Google Scholar]
Widemar 1982 {published data only}
- Widemar L, Rynnel‐Dagöö B, Schiratzki H, Svensson C. The effect of adenoidectomy on secretory otitis media. Acta Oto‐Laryngologica. Supplement 1982;386:132‐3. [DOI] [PubMed] [Google Scholar]
Widemar 1985 {published data only}
- Widemar L, Svensson C, Rynnel‐Dagöö B, Schiratzki H. The effect of adenoidectomy on secretory otitis media: a 2‐year controlled prospective study. Clinical Otolaryngology & Allied Sciences 1985;10(6):345‐50. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
FATA {published data only}
- Paik Y. Food Allergy ‐ Tubes ‐ Adenoids (FATA) Trial. http://clinicaltrials.gov/ct2/show/NCT00736112. [NCT00736112]
NOA {published data only}
- Schilder A. NOA (Nederlands Onderzoek Adenotomie). Effectiveness of adenoidectomy in children with recurrent upper respiratory tract infections. Nederlands Trial Register (http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=968). [NTR968]
TARGET {published data only}
- Haggard M. TARGET. Trial of alternative regimens in glue ear treatment ‐ effectiveness of surgery for otitis media with effusion in 3.5‐7 year olds using multiple developmental and economic measures combined with classical clinical measures. http://www.controlled‐trials.com/ISRCTN35793977/. [ISRCTN35793977]
Additional references
AAFP 2009a
- American Academy of Family Physicians. Diagnosis and management of acute otitis media. www.aafp.org/online/en/home/clinical/clinicalrecs/aom.html (accessed February 2009).
AAFP 2009b
- American Academy of Family Physicians. Otitis media with effusion. www.aafp.org/online/en/home/clinical/clinicalrecs/otitismedia.html (accessed February 2009).
Burton 2009
- Burton MJ, Glasziou PP. Tonsillectomy or adeno‐tonsillectomy versus non‐surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database of Systematic Reviews 2009, Issue 1. [Art. No.: CD001802. DOI: 10.1002/14651858.CD001802.pub2] [DOI] [PubMed] [Google Scholar]
Handbook 2008
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Heerbeek 2003
- Heerbeek N, Akkerman AE, Ingels KJ, Engel JA, Zielhuis GA. Left‐right differences in Eustachian tube function in children with ventilation tubes. International Journal of Pediatric Otorhinolaryngology 2003;67(8):861‐6. [DOI] [PubMed] [Google Scholar]
Lous 2005
- Lous J, Burton MJ, Felding JU, Ovesen T, Rovers MM, Williamson I. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database of Systematic Reviews 2005, Issue 1. [Art. No.: CD001801. DOI: 10.1002/14651858.CD001801] [DOI] [PubMed] [Google Scholar]
McDonald 2008
- McDonald S, Langton Hewer CD, Nunez DA. Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database of Systematic Reviews 2008, Issue 4. [Art. No.: CD004741. DOI: 10.1002/14651858.CD004741.pub2] [DOI] [PubMed] [Google Scholar]
RevMan 2008 [Computer program]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2008.
Rosenfeld 2000
- Rosenfeld RM, Bluestone CD. Chapter 18: Pathogenesis of otitis media. Evidence‐based otitis media. 2nd Edition. Hamilton: BC Decker, 2000:292. [Google Scholar]
Sagnelli 1990
- Sagnelli M, Marzullo C, Pollastrini L, Marullo MN. Secretory otitis media: current aspects and therapeutic role of adenoidectomy. Medicina‐Firenze 1990;10(1):16‐22. [PubMed] [Google Scholar]
Schilder 2004
- Schilder AGM, Lok W, Rovers MM. International perspectives on management of acute otitis media: a qualitative review. International Journal of Pediatric Otorhinolaryngology 2004;68(1):29‐36. [DOI] [PubMed] [Google Scholar]
van den Aardweg 2009
- Aardweg MTA, Schilder AGM, Herkert E, Boonacker CWB, Rovers M. Adenoidectomy for recurrent or chronic nasal symptoms and middle ear disease in children up to 18 years of age. Cochrane Database of Systematic Reviews 2009, Issue 2. [Art. No.: CD007810. DOI: 10.1002/14651858.CD007810] [Google Scholar]
van den Aardweg 2010
- Aardweg MTA, Schilder AGM, Herkert E, Boonacker CWB, Rovers MM. Adenoidectomy for recurrent or chronic nasal symptoms in children. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI] [PMC free article] [PubMed] [Google Scholar]


