Abstract
Background
The clinical relevance of detecting minority drug-resistant HIV-1 variants is uncertain.
Methods
To determine the effect of pre-existing minority non-nucleoside reverse transcriptase inhibitor (NNRTI)-resistant variants on the risk of virologic failure (VF), we reanalyzed a case-cohort substudy of efavirenz recipients in ACTG A5095. Minority K103N or Y181C populations were determined by allele-specific PCR (ASPCR) in subjects without NNRTI resistance by population sequencing. Weighted Cox proportional hazards models adjusted for recent adherence estimated the relative risk of VF in the presence of NNRTI-resistant minority variants.
Results
The evaluable case-cohort sample included 195 subjects from the randomly selected subcohort (51 with VF, 144 without failure [NF]), plus 127 of the remaining subjects with VF. Presence of minority K103N or Y181C mutations, or both, was detected in 8 (4.4%), 54 (29.5%) and 11 (6%), respectively, of 183 evaluable subjects in the random subcohort. Detection of minority Y181C mutants was associated with an increased risk of VF in the setting of recent adherence (HR=3.45, CI=1.90, 6.26), but not in non-adherent subjects (HR=1.39, CI=0.58, 3.29). Of note, 70% of subjects with minority Y181C achieved long-term viral suppression.
Conclusions
In adherent patients, pre-existing minority Y181C mutants more than tripled the risk of VF of first-line efavirenz-based ART.
Keywords: HIV-1, antiretroviral therapy, antiretroviral resistance, allele-specific PCR, minority variants, quasispecies
INTRODUCTION
Antiretroviral treatment guidelines recommend using the non-nucleoside reverse transcriptase inhibitor (NNRTI) efavirenz or a ritonavir-boosted protease inhibitor (PI), plus a fixed-dose combination of nucleoside or nucleotide reverse transcriptase inhibitors (NRTIs), for initial anti-HIV therapy [1, 2]. The efficacy of NNRTI-based regimens, however, is threatened in the presence of drug-resistant HIV-1 among newly infected or newly diagnosed persons [3, 4]. We previously showed that presence of pre-existing NNRTI-resistant mutants detected by population sequencing was associated with a 2.3-fold increased risk of virologic failure (VF) to first-line efavirenz-based antiretroviral therapy (ART) [5].
Antiretroviral drug resistance testing is recommended in HIV-1-infected subjects before starting ART to guide the selection of appropriate first-line regimens [2, 3]. Studies show that antiretroviral drug resistance testing is cost-effective [6], and improves the virologic, immunologic and clinical outcomes of ART [5, 7–10]. Current genotypic resistance assays, however, do not detect resistant viruses present in less than 15–20% of the viral population [11, 12]. New assays such as allele-specific real-time PCR (ASPCR) enable detection of low-abundance mutants with greater sensitivity [13–20]. Through preferential amplification of different allelic variants in real-time PCR conditions, ASPCR consistently detects mutants present in less than 0.1% of the virus population [14].
Relative to population sequencing of plasma viruses, ASPCR testing increases the detection of particular antiretroviral drug-resistance resistance mutations by 1.5- to 3-fold in different clinical settings [14, 15, 21, 22]. Whether drug-resistant mutants present at such low levels are associated with an increased risk of virologic failure of ART remains unresolved. We sought to address this question using ASPCR to detect selected NNRTI resistance mutations in pre-treatment plasma specimens from subjects in a case-cohort study of patients with and without VF in the efavirenz arms of AIDS Clinical Trials Group (ACTG) protocol A5095 [23, 24], a randomized trial of initial ART.
METHODS
Study Participants
The ACTG A5095 study (clinicaltrials.gov identifier: NCT00013520) was a randomized, controlled trial that compared the efficacy of efavirenz plus a fixed-dose combination of two or three nucleoside reverse transcriptase inhibitors (NRTIs) with that of a fixed-dose triple-nucleoside regimen in previously untreated HIV-1-infected subjects with plasma HIV-1 RNA level of 400 copies/mL or greater (Amplicor or UltraSensitive HIV-1 Monitor Assay version 1.0; Roche Molecular Systems, Branchburg, NJ) [23, 24]. For subjects meeting the criteria for virologic failure (2 consecutive measurements of HIV-1 RNA level ≥200 copies/mL, with the first measurement at least 16 weeks after study entry), population sequencing (TruGene; Siemens, Norwood, MA) of plasma viruses was performed from samples stored at the time of first virologic failure and at baseline.
Study design
A case-cohort study of ACTG A5095 was performed to determine the prevalence of NNRTI resistance and its impact on treatment outcome in the efavirenz-containing arms of this trial [5, 25]. The case-cohort sample consisted of a random sample (subcohort) stratified by, and drawn from, the efavirenz-containing arms of A5095, plus additional cases (virologic failures) that were not selected to be in the subcohort. The current report presents further analyses of the existing case-cohort study; the results of the relationship between mutations as detected by population sequencing and virologic failure for this cohort have been previously published. [5]
To identify pre-treatment minority K103N and Y181C variants, blinded pre-treatment plasma samples with no NNRTI resistance detected by population sequencing, were reanalyzed using ASPCR. The primary outcome measure for the case-cohort study was the occurrence of virologic failure; the primary variable of interest was presence or absence of minority K103N and/or Y181C variants in the pre-treatment samples. Minority variants were defined as variants detected by ASPCR, but not by population sequencing. Data on recent adherence, defined as not missing any doses over the past four days [27], were captured as part of A5095 while the subject was on randomized treatment at weeks 4, 12, and 24 and then every 24 weeks using a self-administered adherence questionnaire [26]. Given that non-adherence was associated with an increased risk of virologic failure in the main A5095 study [23], as-treated analyses in the current study were adjusted for recent self-reported adherence.
Detection of K103N and Y181C mutants using allele-specific PCR
Viral RNA was extracted from one milliliter of plasma (QIAamp Viral RNA Mini Kit, Valencia, CA) after centrifugation at 24000 x g for 1 hour at 4°C, and PCR-amplified. (Supplementary material) PCR reactions proceeded as previously published [14, 19]. Clinical specimens were analyzed in the same batch with serially diluted standards (range, 102 to 107 standard DNA copies). The percentage of HIV-1 sequences containing each mutation was calculated as: percent mutated sequences = 100 × (quantity of mutant sequences)/(quantity of total HIV-1 sequences). In addition to the sensitivity threshold for each ASPCR assay, we calculated a specific detection threshold for each sample, defined as the minimum proportion of variants that could be detected based on the subject’s plasma HIV-1 RNA level (pVL), the volume of plasma used in the RNA extraction (V), the fraction of the RNA elution volume used for cDNA synthesis (fe), and the assumed efficiencies of the RNA extraction (ERNAX) and cDNA synthesis (EcDNA).
Statistical methods
Based on the random subcohort, the prevalence of baseline minority K103N and/or Y181C mutants was estimated; the prevalence of each minority variant was compared between virologic failures and non-failures using the Fisher’s exact test. Using an exact test for homogeneity of odds ratios, the prevalence of Y181C mutants was compared between virologic failures and non-failures across the following subgroups: subjects with or without the K103N mutation, 4-drug or 3-drug EFV-based treatment, and screening HIV-1 RNA level. Summary statistics of the demographics of subjects in the random subcohort by pre-existing minority K103N and/or Y181C mutants, population resistance, or no NNRTI resistance are described, as well as for additional subjects with virologic failure. Weighted Cox proportional hazards models [29] were used to estimate the risk of virologic failure in the presence and absence of minority K103N and/or Y181C mutants at baseline among subjects without NNRTI resistance mutations by population sequencing. Unadjusted intent-to-treat and as-treated analyses showed similar results. Further as-treated analyses were adjusted for recent self-reported adherence; the presence of an interaction between recent self-reported adherence and baseline NNRTI resistance was examined. Such an interaction would imply a different impact of the presence of NNRTI resistance mutations at baseline dependent on recent adherence. Subjects without ASPCR results for either codon 103 or 181 were counted as missing unless otherwise specified. In a post-hoc analysis, all subjects with low-level Y181C mutants at baseline and experiencing virologic failure were evaluated for the presence of resistance by population sequencing at time of failure. A post-hoc analysis in the random cohort compared the mean change in viral load at day 14 on study from baseline in subjects with no NNRTI resistance mutations to subjects with low-abundant Y181C and to subjects with bulk resistance using the Wilcoxon rank sum test. All P-values and confidence intervals presented are nominal, unadjusted for multiple comparisons.
RESULTS
Case-cohort sample
Of the 220 randomly sampled subjects, 57 (26%) were cases (virologic failures) and 163 (74%) were controls (non-failures) (Figure 1). Eleven controls had less than 16 weeks of follow-up and therefore were not evaluable for the protocol-defined criteria for virologic failure; these subjects were excluded from analyses of virologic failure and were not assayed by ASPCR. Reasons for premature study discontinuation included loss to follow-up (5), unable to get to clinic (4), toxicity (1) and clinical event (1). The fully evaluable random cohort sample included 195 subjects with at least 16 weeks of follow-up of whom 12 were considered NNRTI-resistant by population sequencing and 183 had complete ASPCR results. Note, an additional 4 subjects had only ASPCR data for K103N or Y181C, but not both (2 and 2, respectively). One hundred twenty-seven additional failures were added to the random subcohort (7 NNRTI-resistant by population sequencing and 120 with complete ASPCR results). Overall, the total case-cohort sample included 322 subjects (178 failures and 144 non-failures).
Figure 1. Case-cohort design and subject disposition.
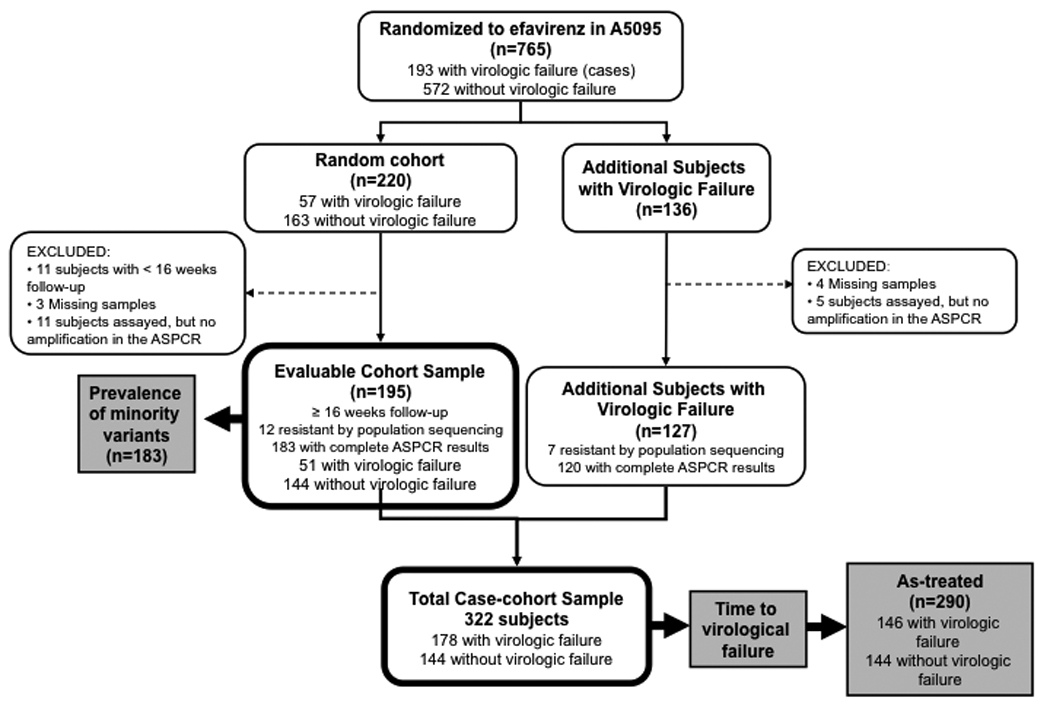
Subjects were excluded if they had no result for both minority variants. Subjects were considered to have incomplete data if they had a result for only one minority variant.
Allele-specific PCR
The detection threshold of the ASPCR was defined as more than 3 standard deviations above the mean of 20 repeated assays using the wild-type RT from pNL4-3 as a control target. Detection thresholds were: K103N (AAC) = 0.003%, K103N (AAT) = 0.001% and Y181C = 0.03%. The difference in real-time PCR threshold cycle values (ΔCt) between mutant and wild-type DNA equivalents was always > 17 cycles. Proportion measurements were linear down to at least 0.1% in all cases.
Baseline characteristics
As previously reported [5], the prevalence of pre-treatment NNRTI resistance by population sequencing in the randomly sampled subcohort was 5%; this included 6 subjects with K103N alone, 2 with K103N together with a second NNRTI resistance mutation (other than Y181C), 0 with Y181C alone, and 1 with both K103N and Y181C by population sequencing at baseline. Of the 183 subjects assayed for the presence of pre-existing low-abundance K103N and/or Y181C mutants using ASPCR, variants carrying the K103N, Y181C, or both were detected in 8 (4.4%), 54 (29.5%) and 11 (6%) subjects, respectively. Table 1 summarizes baseline demographics of the random subcohort by presence or absence of preexisting minority NNRTI resistance mutations, and for the additional subjects with virologic failure.
Table 1.
| Random Subcohort |
||||||||
|---|---|---|---|---|---|---|---|---|
| Resistance by ASPCR |
||||||||
| No NNRTI Resistance (n=110)c |
K103N only (n=8) |
Y181C only (n=54) |
Both K103N+Y181C (n=11) |
NNRTI Resistance by population sequencing (n=12)d |
All of Random Subcohort (n=195) |
Additional virologic failures (n=127) |
||
| Screening HIV-1 RNA | <100,000 copies/mL | 67 (61%) | 2 (25%) | 25 (46%) | 7 (64%) | 8 (67%) | 109 (56%) | 66 (52%) |
| Sex | Male | 82 (75%) | 8 (100%) | 47 (87%) | 9 (82%) | 11 (92%) | 157 (81%) | 105 (83%) |
| Age (yrs) | Mean (SD) | 36 (9) | 36 (8) | 40 (11) | 37 (10) | 37 (7) | 37 (10) | 37 (9) |
| Race/ethnicity | White Non-Hispanic | 48 (44%) | 4 (50%) | 23 (43%) | 4 (36%) | 8 (67%) | 87 (45%) | 46 (36%) |
| Black Non-Hispanic | 36 (33%) | 2 (25%) | 23 (43%) | 4 (36%) | 4 (33%) | 69 (35%) | 55 (43%) | |
| Hispanic (Regardless of Race) | 24 (22%) | 2 (25%) | 7 (13%) | 3 (27%) | 0 (0%) | 36 (18%) | 23 (18%) | |
| Othere | 2 (2%) | 0 (0%) | 1 (2%) | 0 (0%) | 0 (0%) | 3 (2%) | 3 (2%) | |
| IV drug history | Never | 95 (86%) | 6 (75%) | 46 (85%) | 8 (73%) | 7 (58%) | 162 (83%) | 112 (88%) |
| Currently/Previously | 15 (14%) | 2 (25%) | 8 (15%) | 3 (27%) | 5 (42%) | 33 (17%) | 15 (12%) | |
| HIV-1 RNA (log10cp/mL) | Mean (SD) | 4.85 (0.71) | 5.08 (0.93) | 4.94 (0.65) | 5.32 (0.47) | 4.65 (0.46) | 4.90 (0.69) | 4.94 (0.71) |
| CD4 Count (cells/mm3) | Median (Q1, Q3) | 204 (99, 322) | 74 (17,334) | 199 (44, 330) | 201 (46, 287) | 283 (208, 443) | 206 (65, 324) | 203 (75, 356) |
The case-cohort sample consisted of a random sample (Random subcohort) stratified by and drawn from the efavirenz-containing arms of the ACTG A5095 study, plus the additional cases (Additional virologic failures) that were not selected to be in the subcohort. The baseline characteristics of subjects included in the random subcohort are shown for the following groups: subjects without NNRTI resistance mutations detected by either population sequencing or ASPCR; those without NNRTI resistance detected by population sequencing but in whom ASPCR detected only K103N mutants (K103N only), only Y181C mutants (Y181C only) or both K103N and Y181C mutants (both K103N + Y181C); subjects in whom NNRTI resistance mutations were detected by population sequencing of plasma viruses, and for all subjects included in the random subcohort (All of Random Subcohort). Of note, subjects with NNRTI resistance mutations detected by population sequencing were not retested using ASPCR.
The table does not include subjects with less than 16 weeks of follow-up (n=11) or with missing (n=16) or incomplete (n=7) ASPCR results.
NNRTI, non-nucleoside reverse transcriptase inhibitor; ASPCR, allele-specific polymerase chain reaction
Population sequencing of plasma viruses
Other race/ethnicity category includes Asian, Pacific Islander, American Indian, Alaskan Native and unknown.
Levels of low-abundance drug-resistant mutants at baseline
Among subjects in the random subcohort in whom minority NNRTI-resistant variants were detected, the median (interquartile range) levels of mutants were: K103N, AAC allele= 0.012% (0.008%–0.116%); K103N, AAT allele= 0.013% (0.005%–0.053%); and Y181C=0.060% (0.048%–0.089%). Of note, the levels of Y181C and K103N mutants detected in individual samples were all below 1% (Figure 2 and data not shown).
Figure 2. Levels of minority Y181C mutants in the virus population.
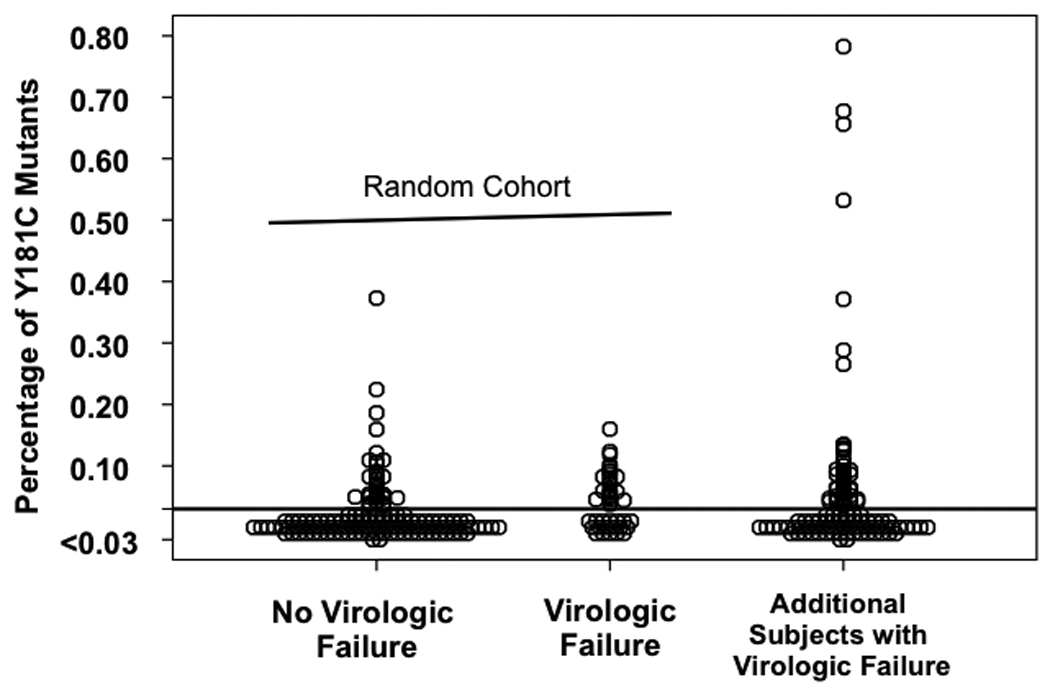
The horizontal line represents the sensitivity threshold of the allele-specific PCR assay for detecting Y181C mutants (0.03%). Circles represent the levels at which Y181C were found among each plasma sample. Each circle corresponds to one subject.
Low-abundance K103N and/or Y181C mutants and virologic failure
Pre-existing low-abundance K103N mutants were detected less often than Y181C variants. K103N minority mutants were as frequent in non-failures as failures in the random subcohort with respect to Y181C minority mutants (Figure 3). Of the 185 subjects in the random subcohort, 58% of virologic failures compared to 29% of non-failures had low-abundance Y181C mutants at baseline (P=0.001). The relative prevalence of Y181C mutants in subjects with virologic failure compared to subjects without virologic failure was similar across subgroups defined by presence or absence of the K103N mutation, assignment to the 4-drug or 3-drug arm, and screening HIV-1 RNA level (Figure 3). In exploratory analyses, we were unable to define a threshold level of Y181C mutants that distinguished failures and non-failures with high sensitivity and specificity (not shown). A post-hoc analysis of the baseline characteristics of subjects with low-abundance Y181C mutants in the randomly sampled subcohort showed no differences between virologic failures and non-failures regarding screening HIV-1 RNA levels, CD4+ T-cell counts, or race/ethnicity (not shown). Note, these analyses include all subjects with results for the respective minority variant.
Figure 3. Prevalence of baseline minority K103N and Y181C mutants according to virologic outcome.
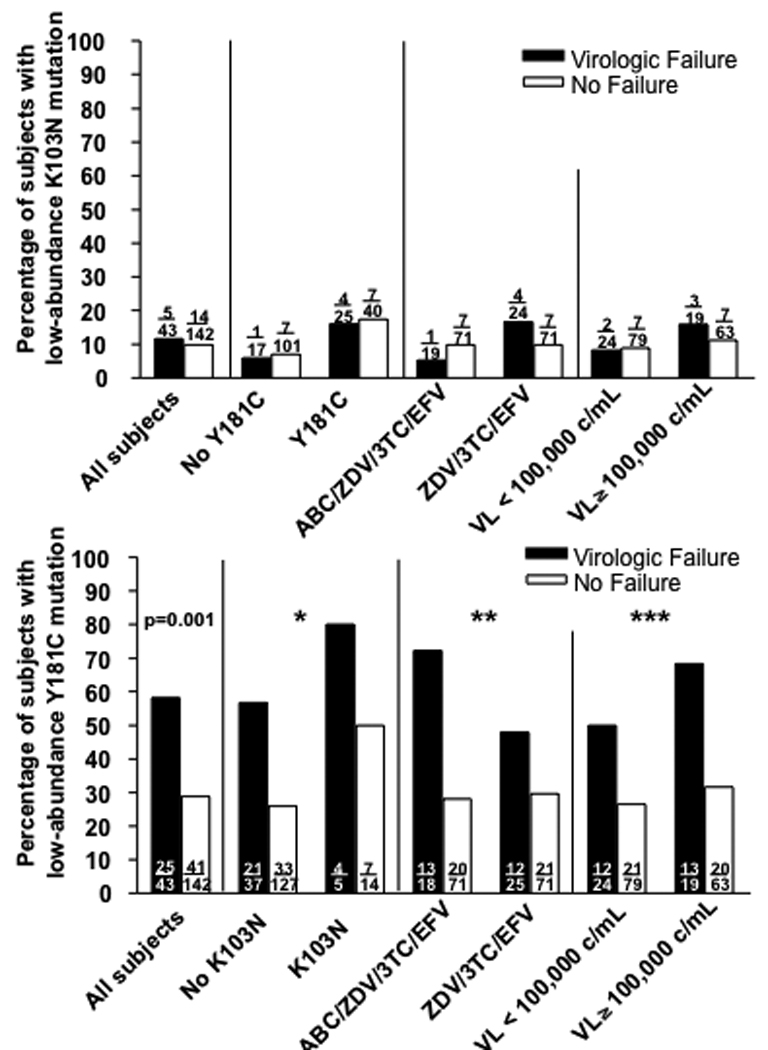
Figures show the proportion of subjects with and without virologic failure in whom low-abundance K103N (upper figure) and Y181C (lower figure) mutations were detected at baseline among those without NNRTI resistance by population sequencing in the random subcohort. The upper figure includes 2 subjects with a K103N result only and the lower figure includes 2 subjects with an Y181C result only; these subjects are excluded from all other analyses. Analyses were done overall; for subjects with the Y181C mutation detected by ASPCR (Y181C+) or not (No Y181C); for subjects with the K103N mutation detected by ASPCR (K103N+) or not (No K103N); for those receiving abacavir (ABC), zidovudine (ZDV), lamivudine (3TC) and efavirenz (EFV) or those receiving zidovudine (ZDV), lamivudine (3TC) and efavirenz (EFV); and for subjects with screening HIV-1 RNA levels (VL) greater than or equal to, or lower than 100,000 copies/mL. The prevalence of low-abundant K103N mutants among failures and non-failures was not significantly different overall (p-value not shown). P-value for difference in prevalence of low-abundant Y181C mutants among failures and non-failures overall is shown. Pinteraction values are based on exact test for homogeneity of odds ratios across subgroups. P-values are nominal and unadjusted for multiple comparisons.
* P interaction = 1.0; ** P interaction = 0.27; *** P Interaction = 0.71
An as-treated weighted Cox proportional hazards model adjusted for recent adherence showed a significantly increased risk of virologic failure for subjects with an NNRTI-resistant virus by population sequencing compared with those with wild-type virus by population sequencing and ASPCR (hazard ratio [HR]= 4.00, 95% confidence interval [CI]= 1.72, 9.09). Among subjects with wild-type HIV-1 by population sequencing, detection of low-abundance Y181C mutants by ASPCR was associated with an increased risk of virologic failure (HR=2.54, 95% CI= 1.53, 4.20). A significant association with the detection of minority K103N mutants and an increased risk of virologic failure was not detected (P=0.22), but the direction of the effect was similar (HR=1.58, 95% CI=0.76, 3.28). As seen in the study overall [23], subjects with recent non-adherence also had an increased risk of virologic failure compared with adherent subjects (HR=2.30, 95% CI=1.40, 3.78).
Further modeling suggested an interaction between baseline presence of low-abundance Y181C mutants and recent adherence (P=0.08), showing that in the presence of recent non-adherence, the effect of minority Y181C was diminished (Figure 4). Among adherent subjects, the presence of minority Y181C by ASPCR had an increased risk of virologic failure compared to those that were sensitive by both population sequencing and ASPCR (HR=3.45, 95% CI= 1.90, 6.26; P<0.001); among non-adherent subjects, the presence of minority Y181C did not show a significantly increased risk of virologic failure (HR=1.39, 95% CI= 0.58, 3.29, P=0.46). Similar results were obtained when repeating this analysis using the presence of any minority variant (either K103N or Y181C) (data not shown).
Figure 4. Effect of Y181C in the presence of recent adherence (adjusted for presence of minority of K103N by ASPCR).
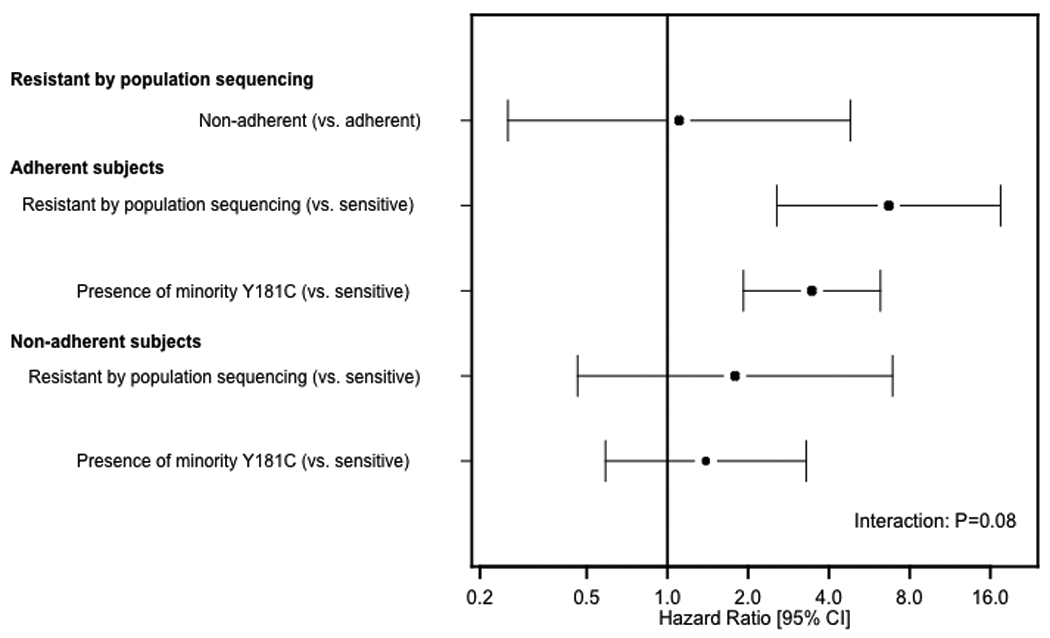
As-treated weighted Cox proportional hazards model of time to virologic failure; Adherent, adequate recent self-reported adherence to therapy; Sensitive, no evidence of non-nucleoside reverse transcriptase inhibitors (NNRTI) resistance mutations by population sequencing and by allele-specific PCR (ASPCR); 95% CI, 95% confidence interval.
NNRTI resistance mutations at virologic failure
Sixty-five subjects with low-abundance Y181C mutants at baseline experienced virologic failure and had a viral genotype (by population sequencing) available at the time of virologic failure. No resistance mutations were detected in 27 (41.5%), K103N was detected in 25 (38.5%), Y181C in 5 (7.7%) and K101E in 4 (6.2%); 2 of these 4 [3.1%] also had the K103N mutation (Table 2).
Table 2.
Resistance mutations in HIV reverse transcriptase identified by population sequencing at the time of virologic failure among subjects with Y181C at baseline identified by ASPCR
| Resistance mutations | Number of subjects |
|---|---|
| Nonea | 27 |
| K103N | 11 |
| M184V,K103N | 6 |
| Y181C | 3 |
| M184V | 2 |
| D67N,K70R,M184V,K101E,G190A | 1 |
| D67N,M184V,K103N,P225H | 1 |
| K101E | 1 |
| K101Q,K103N | 1 |
| K103N,P225H | 1 |
| K65R,M184V,K103N,P225H | 1 |
| L100I,K101E,K103N | 1 |
| M184I,K103N | 1 |
| M184V,K101E,K103N | 1 |
| M184V,K103N,M230L | 1 |
| M184V,K219Q | 1 |
| M184V,V179D | 1 |
| V118I | 1 |
| Y181C,V108I | 1 |
| Y181C,G190S | 1 |
| Y188C,G190S | 1 |
| TOTAL | 65 |
Absence of resistance mutations by population sequencing.
Low-abundant K103N and/or Y181C mutants and viral dynamics
Following these observations we chose to examine whether low-abundant Y181C mutants impacted initial declines (to day 14) in HIV-1 RNA level upon treatment initiation. To avoid bias from over-sampling of virologic failures, these analyses were limited to the random cohort. Among subjects in the random cohort with available sequencing and day 14 viral load data, the mean change in viral load at day 14 on study from baseline was not significantly different between subjects with low-abundant Y181C and subjects with no NNRTI resistance mutations (P=0.97); a significantly smaller mean change in viral load at day 14 from baseline was detected in subjects with bulk resistance (mean change=−1.53 log 10copies/mL) as compared to subjects with no NNRTI resistance mutations (mean change=−2.06 log 10copies/mL) (difference: 0.52, 95% CI=0.13,0.91 copies/mL, P=0.01).
DISCUSSION
Detection of pre-existing minority Y181C mutants encoding NNRTI resistance was associated with a more than 3-fold increased risk of virological failure to initial ART with efavirenz-based regimens in ART-naive HIV-1-infected subjects in the presence of perfect adherence. The increased risk persisted across subjects with diverse baseline characteristics, including those with plasma HIV-1 RNA levels greater than or equal to, or less than 100,000 copies/mL; the risk magnitude was considerable and clinically relevant. Importantly, the impact of the presence of low-abundance Y181C mutants on the risk of virologic failure was diminished among non-adherent subjects. These findings confirm the importance of pre-existing resistant viruses present as minority members of the viral quasispecies in determining the virologic outcome of ART, particularly in the case of drugs with a low genetic barrier to resistance. They also underscore the clinical need for improving the sensitivity of genotypic drug resistance assays.
Mutations Y181C and K103N were chosen for the ASPCR analysis because they are the most frequent NNRTI resistance mutations found after virological failure to nevirapine and efavirenz. Minority Y181C and K103N mutants were detected by ASPCR in nearly 40% of subjects with wildtype virus by standard genotypic testing. This prevalence represented an almost 9-fold increase in the detection of primary NNRTI resistance when the results of ASPCR plus population sequencing (44%) were compared to population sequencing alone (5%).
In the current study, we did not detect an association with the presence of low-abundance K103N mutants and increased risk of virologic failure. This observation contrasts with previous studies, including our own finding in the same study population of a significantly increased risk of virologic failure when K103N was detected by population sequencing. However, this discrepancy may be attributable to the relatively small number of subjects with low-abundance K103N mutants identified by ASPCR.
It is noteworthy that all of the mutants identified by ASPCR in our study were present at levels below 1%. Although these low levels could represent underestimation due to polymorphisms at the primer binding sites in the target sequences, it would be surprising if this were the case in every subject tested. A more likely explanation is that Y181C and K103N mutants present at higher levels had already been identified by population sequencing, since samples from those subjects were not retested by ASPCR. This interpretation is consistent with data generated by ultradeep pyrosequencing [22], which found that NNRTI-resistant mutants were either present at relatively high levels (>20%, and thus detectable by population sequencing) or at low levels (generally below 1%–5%). These findings suggest that ultrasensitive resistance assays should have sufficient sensitivity to detect variants present at less than 1%–5% of the plasma virus population.
Our study extends the findings of two earlier studies. A retrospective case-control analysis from the U.S. Centers for Diseases Control and Prevention (CDC) applied a modified ASPCR technique to baseline samples drawn from two clinical trials of efavirenz-containing first-line regimens [33]. Presence of minority mutations at RT codons 103, 181 or 184 was associated with an 11-fold increased odds of virological failure, but these mutations were detected in only a small number of subjects (7/95 with virologic failure and 2/221 with virologic suppression). The contribution of each individual mutation to the risk of virologic failure could not be assessed.
Analysis of baseline resistance by ultradeep pyrosequencing in the Flexible Initial Retrovirus Suppressive Therapies (FIRST) study, which compared initial ART strategies including an NNRTI, PI or both [34] found that pre-existing minority NNRTI-resistant variants more than tripled the hazard of virological failure in ART-naive subjects starting NNRTI-based therapy [22]. Similarly, all 4 subjects in the PI arm in whom PI-resistant minority variants were detected experienced virologic failure, but the numbers were too small to show a statistically significant increase in the risk of virologic failure.
The clinical application of ASPCR or any other resistance assay requires a precise refinement of thresholds that identify subjects at greatest risk of virologic failure. We were unable to define a threshold level of mutants that distinguished between subjects with virologic failure and subjects without virologic failure with high sensitivity and specificity. Although subjects with minority Y181C variants were at greater risk of virologic failure, 70% of these subjects nevertheless achieved long-term viral suppression on their initial efavirenz-based regimen. In post-hoc exploratory analyses, we were unable to identify factors that explained this difference. The high sensitivity of ASPCR may capture natural fluctuations within the quasispecies over time that are not necessarily clinically significant. Conversely, the other two studies addressing the clinical relevance of minority variants used higher thresholds for detecting minor variants. Because the modified ASPCR method used in the CDC study [33] was designed to detect mutant viruses above the natural quasispecies frequency of each mutation, the actual threshold for detecting the K103N and Y181C mutants was 0.9% and 1.0%, respectively, which is at least two orders of magnitude higher than with our approach. Indeed, the clonal frequencies of the resistant variants in the CDC study ranged between 0.6% and 12.5%, suggesting a lower sensitivity of the ASPCR method used by the CDC, relative to ours. Similarly, due to the error rate of pyrosequencing, the cut-off for detecting minority variants in the FIRST study [22] was established at 1%. Whereas the CDC and the FIRST studies could have missed clinically relevant minority mutants, a number of minority mutants detected in our study did not contribute to virologic failure during the study period. Determining the optimum threshold to maximize sensitivity and specificity requires analysis of a larger number of samples than available in studies performed to date.
Although the presence of pre-existing low-abundance Y181C mutants was associated with a greater risk of virologic failure, other EFV resistance mutations were more commonly found at the time of virologic failure. Similar results were obtained in the FIRST study [22]. It is possible that presence of the Y181C mutants was a marker for presence of other, undetected NNRTI mutants that emerged under efavirenz selection. Alternatively, the low-level EFV resistance conferred by Y181C could have allowed ongoing virus replication that led, in turn, to the later accumulation of other NNRTI resistance mutations such as K103N or G190S. Persistence of Y181C might have been selected against by the coadministration of zidovudine, since Y181C increases HIV-1 susceptibility to that drug [32]. Because we did not attempt to detect minority NRTI-resistant variants at baseline, we cannot fully rule out that preexistence of some of such variants (e.g. M184V) could have influenced the risk of virological failure.
In conclusion, low-abundance NNRTI-resistant variants significantly increased the risk of virologic failure to initial antiretroviral therapy with efavirenz among adherent subjects; these minority mutants did not add to the risk of failure with non-adherence. More sensitive resistance assays could improve the clinical management of HIV-infected subjects. The clinical application of such assays, however, will require further technical developments, a better understanding of the role of low-abundance resistant variants in different clinical scenarios and, refinement of assay thresholds that identify patients at greatest risk of virologic failure.
Supplementary Material
ACKNOWLEDGMENTS
We thank the 33 participating AIDS Clinical Trials Units, the A5095 study team members and the study subjects for their contributions to this work. We also thank Danielle Smith (Massachusetts General Hospital), Russell Young (University of Colorado Health Sciences Center), Lorraine Sutton (Vanderbilt University), J. Darrell Darren Hazelwood (University of Alabama, Birmingham) and Leslie Petch (University of North Carolina at Chapel Hill) performed HIV-1 genotyping assays for ACTG A5095.
Funding/Support: This work was supported by NIH grants AI38858 and AI068636 (AIDS Clinical Trials Group Central Grant), AI069419, AI051966, AI069472, AI069452, RR024996; subcontracts from grants AI38858 and AI06836 with the Virology Support Laboratories at Massachusetts General Hospital, the University of Alabama, the University of North Carolina, and Vanderbilt University; the Birmingham Veterans Affairs Medical Center; and the Harvard University and University of Alabama at Birmingham and the University of North Carolina at Chapel Hill Centers for AIDS Research (AI060354, AI027767, and AI50410). Dr. Paredes was awarded the “La Caixa” Grant for Post-Graduate Studies, Caixa de Pensions de Barcelona, “La Caixa”, Spain. Bristol-Myers Squibb and GlaxoSmithKline provided drug for this study as well as financial support for plasma HIV-1 RNA determinations.
Footnotes
Clinical Trials Registration: clinicaltrials.gov Identifier: NCT00013520
Financial Disclosures:
Dr. Paredes reports having received research grants (awarded to the irsiCaixa Foundation) from Boehringer-Ingelheim, Monogram, Pfizer, and Merck; and received speaker honoraria from Siemens Medical Solutions. Dr. Shikuma reports having had affiliations with or financial involvement with Boehringer-Ingelheim, Bristol-Myers Squibb, Gilead, and GlaxoSmithKline. Dr. Johnson reports serving as a consultant to and/or having received grant support from Bayer, Bristol-Myers Squibb and GlaxoSmithKline. Dr. Fiscus reports having received speaker honoraria from Gen-Probe and Abbott Molecular and receiving kits from Gen-Probe, Abbott Molecular, and Perkin-Elmer. Dr. D’Aquila reports having received grant support from Bristol-Myers Squibb and being a consultant to Boehringer-Ingleheim and GlaxoSmithKline. Dr. Gulick reports having received research grants (awarded to Cornell University) from Merck, Pfizer, Schering and Tibotec; served as an ad hoc consultant to Boehringer-Ingelheim, Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Merck, Pathway, Pfizer, Progenics, Schering, Tibotec, and Virostatics; and serving as DSMB Chair for Koronis. Dr. Kuritzkes reports having served as a consultant for and received speaker's fees and/or research support from Boehringer-Ingelheim, Bristol-Myers Squibb, and GlaxoSmithKline; and served as a consultant for and received research support from Bayer and Siemens. Dr. Ribaudo served on the DSMB for Koronis. Ms. Lalama and Dr. Schackman had no financial disclosures to report.
Previous Presentation: Presented in part at the 15th Conference on Retroviruses and Opportunistic Infections, February 3–6, 2008, Boston, MA, Abstract 83.
REFERENCES
- 1.Hammer SM, Eron JJ, Jr, Reiss P, et al. Antiretroviral treatment of adult HIV infection: 2008 recommendations of the International AIDS Society-USA panel. JAMA. 2008;300:555–570. doi: 10.1001/jama.300.5.555. [DOI] [PubMed] [Google Scholar]
- 2. [January 29, 2008];DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents: Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. 2008 Available at http://www.aidsinfo.nih.gov.
- 3.Hirsch MS, Gunthard HF, Schapiro JM, et al. Antiretroviral drug resistance testing in adult HIV-1 infection: 2008 recommendations of an International AIDS Society-USA panel. Clin Infect Dis. 2008;47:266–285. doi: 10.1086/589297. [DOI] [PubMed] [Google Scholar]
- 4.Kozal MJ, Hullsiek KH, Macarthur RD, et al. The Incidence of HIV drug resistance and its impact on progression of HIV disease among antiretroviral-naive participants started on three different antiretroviral therapy strategies. HIV Clin Trials. 2007;8:357–370. doi: 10.1310/hct0806-357. [DOI] [PubMed] [Google Scholar]
- 5.Kuritzkes DR, Lalama CM, Ribaudo HJ, et al. Preexisting resistance to nonnucleoside reverse-transcriptase inhibitors predicts virologic failure of an efavirenz-based regimen in treatment-naive HIV-1-infected subjects. J Infect Dis. 2008;197:867–870. doi: 10.1086/528802. [DOI] [PubMed] [Google Scholar]
- 6.Sax PE, Islam R, Walensky RP, et al. Should resistance testing be performed for treatment-naive HIV-infected patients? A cost-effectiveness analysis. Clin Infect Dis. 2005;41:1316–1323. doi: 10.1086/496984. [DOI] [PubMed] [Google Scholar]
- 7.Vray M, Meynard JL, Dalban C, et al. Predictors of the virological response to a change in the antiretroviral treatment regimen in HIV-1-infected patients enrolled in a randomized trial comparing genotyping, phenotyping and standard of care (Narval trial, ANRS 088) Antivir Ther. 2003;8:427–434. doi: 10.1177/135965350300800510. [DOI] [PubMed] [Google Scholar]
- 8.Tural C, Ruiz L, Holtzer C, et al. Clinical utility of HIV-1 genotyping and expert advice: the Havana trial. Aids. 2002;16:209–218. doi: 10.1097/00002030-200201250-00010. [DOI] [PubMed] [Google Scholar]
- 9.Baxter JD, Mayers DL, Wentworth DN, et al. A randomized study of antiretroviral management based on plasma genotypic antiretroviral resistance testing in patients failing therapy. CPCRA 046 Study Team for the Terry Beirn Community Programs for Clinical Research on AIDS. Aids. 2000;14:F83–F93. doi: 10.1097/00002030-200006160-00001. [DOI] [PubMed] [Google Scholar]
- 10.Harrigan PR, Hertogs K, Verbiest W, et al. Baseline HIV drug resistance profile predicts response to ritonavir-saquinavir protease inhibitor therapy in a community setting. Aids. 1999;13:1863–1871. doi: 10.1097/00002030-199910010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Brun-Vezinet F, Costagliola D, Khaled MA, et al. Clinically validated genotype analysis: guiding principles and statistical concerns. Antivir Ther. 2004;9:465–478. [PubMed] [Google Scholar]
- 12.Grant RM, Kuritzkes DR, Johnson VA, et al. Accuracy of the TRUGENE HIV-1 genotyping kit. J Clin Microbiol. 2003;41:1586–1593. doi: 10.1128/JCM.41.4.1586-1593.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Margulies M, Egholm M, Altman WE, et al. Genome sequencing in microfabricated high-density picolitre reactors. Nature. 2005;437:376–380. doi: 10.1038/nature03959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paredes R, Marconi VC, Campbell TB, Kuritzkes DR. Systematic evaluation of allele-specific real-time PCR for the detection of minor HIV-1 variants with pol and env resistance mutations. J Virol Methods. 2007 doi: 10.1016/j.jviromet.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Metzner KJ, Rauch P, Walter H, et al. Detection of minor populations of drug-resistant HIV-1 in acute seroconverters. Aids. 2005;19:1819–1825. doi: 10.1097/01.aids.0000189878.97480.ed. [DOI] [PubMed] [Google Scholar]
- 16.Lecossier D, Shulman NS, Morand-Joubert L, et al. Detection of minority populations of HIV-1 expressing the K103N resistance mutation in patients failing nevirapine. J Acquir Immune Defic Syndr. 2005;38:37–42. doi: 10.1097/00126334-200501010-00007. [DOI] [PubMed] [Google Scholar]
- 17.Dykes C, Najjar J, Bosch RJ, et al. Detection of drug-resistant minority variants of HIV-1 during virologic failure of indinavir, lamivudine, and zidovudine. J Infect Dis. 2004;189:1091–1096. doi: 10.1086/382033. [DOI] [PubMed] [Google Scholar]
- 18.Charpentier C, Dwyer DE, Mammano F, Lecossier D, Clavel F, Hance AJ. Role of minority populations of human immunodeficiency virus type 1 in the evolution of viral resistance to protease inhibitors. J Virol. 2004;78:4234–4247. doi: 10.1128/JVI.78.8.4234-4247.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palmer S, Boltz V, Martinson N, et al. Persistence of nevirapine-resistant HIV-1 in women after single-dose nevirapine therapy for prevention of maternal-to-fetal HIV-1 transmission. Proc Natl Acad Sci U S A. 2006;103:7094–7099. doi: 10.1073/pnas.0602033103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cai F, Chen H, Hicks CB, Bartlett JA, Zhu J, Gao F. Detection of minor drug-resistant populations by parallel allele-specific sequencing. Nat Methods. 2007;4:123–125. doi: 10.1038/nmeth995. [DOI] [PubMed] [Google Scholar]
- 21.Paredes R, Cheng I, Kuritzkes DR, Tuomala RE. High prevalence of primary lamivudine and nelfinavir resistance in HIV-1-infected pregnant women in the United States, 1998–2004. Aids. 2007;21:2103–2106. doi: 10.1097/QAD.0b013e3282ef3822. [DOI] [PubMed] [Google Scholar]
- 22.Simen BB, Huppler Hullsiek K, Novak RM, et al. 16th International HIV Drug Resistance Workshop. West Indies: Barbados; 2007. Prevalence of Low Abundance Drug Resistant Variants by Ultra-Deep Sequencing in Chronically HIV-Infected Antiretroviral (ARV) Naive Patients and the Impact on Virologic Outcomes. [Google Scholar]
- 23.Gulick RM, Ribaudo HJ, Shikuma CM, et al. Triple-nucleoside regimens versus efavirenz-containing regimens for the initial treatment of HIV-1 infection. N Engl J Med. 2004;350:1850–1861. doi: 10.1056/NEJMoa031772. [DOI] [PubMed] [Google Scholar]
- 24.Ribaudo HJ, Kuritzkes DR, Gulick RM. A comparison of three initial antiretroviral AIDS regimens. N Engl J Med. 2007;357:1056–1057. doi: 10.1056/NEJMc070207. [DOI] [PubMed] [Google Scholar]
- 25.Prentice RL. Opportunities for enhancing efficiency and reducing cost in large scale disease prevention trials: a statistical perspective. Stat Med. 1990;9:161–170. doi: 10.1002/sim.4780090123. discussion 170-2. [DOI] [PubMed] [Google Scholar]
- 26.Chesney MA, Ickovics JR, Chambers DB, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12:255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 27.Schackman BR, Ribaudo HJ, Krambrink A, Hughes V, Kuritzkes DR, Gulick RM. Racial differences in virologic failure associated with adherence and quality of life on efavirenz-containing regimens for initial HIV therapy: results of ACTG A5095. J Acquir Immune Defic Syndr. 2007;46:547–554. doi: 10.1097/qai.0b013e31815ac499. [DOI] [PubMed] [Google Scholar]
- 28.Lin HJ, Tanwandee T, Hollinger FB. Improved methods for quantification of human immunodeficiency virus type 1 RNA and hepatitis C virus RNA in blood using spin column technology and chemiluminescent assays of PCR products. J Med Virol. 1997;51:56–63. [PubMed] [Google Scholar]
- 29.Barlow WE, Ichikawa L, Rosner D, Izumi S. Analysis of case-cohort designs. J Clin Epidemiol. 1999;52:1165–1172. doi: 10.1016/s0895-4356(99)00102-x. [DOI] [PubMed] [Google Scholar]
- 30.Havlir D, McLaughlin MM, Richman DD. A pilot study to evaluate the development of resistance to nevirapine in asymptomatic human immunodeficiency virus-infected patients with CD4 cell counts of > 500/mm3: AIDS Clinical Trials Group Protocol 208. J Infect Dis. 1995;172:1379–1383. doi: 10.1093/infdis/172.5.1379. [DOI] [PubMed] [Google Scholar]
- 31.Havlir DV, Eastman S, Gamst A, Richman DD. Nevirapine-resistant human immunodeficiency virus: kinetics of replication and estimated prevalence in untreated patients. J Virol. 1996;70:7894–7899. doi: 10.1128/jvi.70.11.7894-7899.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richman DD, Havlir D, Corbeil J, et al. Nevirapine resistance mutations of human immunodeficiency virus type 1 selected during therapy. J Virol. 1994;68:1660–1666. doi: 10.1128/jvi.68.3.1660-1666.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson JA, Li JF, Wei X, et al. Minority HIV-1 drug resistance mutations are present in antiretroviral treatment-naive populations and associate with reduced treatment efficacy. PLoS Med. 2008;5:e158. doi: 10.1371/journal.pmed.0050158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.MacArthur RD, Novak RM, Peng G, et al. A comparison of three highly active antiretroviral treatment strategies consisting of non-nucleoside reverse transcriptase inhibitors, protease inhibitors, or both in the presence of nucleoside reverse transcriptase inhibitors as initial therapy (CPCRA 058 FIRST Study): a long-term randomised trial. Lancet. 2006;368:2125–2135. doi: 10.1016/S0140-6736(06)69861-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


