Abstract
We investigated body vigilance, cardiac anxiety, and the mediating role of interoceptive fear on pain in patients with non-cardiac chest pain (NCCP; a syndrome of chest pain in the absence of identifiable organic etiology). Patients were more attentive to cardiac-congruent sensations than cardiac-incongruent sensations (e.g., gastrointestinal, cognitive dyscontrol; p's < .001). Patients with a DSM-IV Axis I anxiety or mood disorder were more body vigilant compared to patients who did not have a disorder (p's < .05). Patients with anxiety disorders were particularly vigilant to and fearful of cardiac sensations relative to patients without anxiety disorders. Latent variable path models examined the extent that interoceptive fear mediated the association between body vigilance and cardiac anxiety on chest pain. Within each model, diagnostic status, body vigilance, and cardiac anxiety were exogenous and predicted interoceptive fear that in turn predicted pain. Separate models examined body vigilance and cardiac anxiety, and both models fit the data well. Findings showed partial mediation for the body vigilance factor, and full mediation for the cardiac anxiety factor. Interoceptive fear played a mediating role in both models. The syndrome of NCCP may persist partly due to conscious hypervigilance to and fear of cardiac-congruent body sensations, particularly among anxious patients.
Keywords: Non-cardiac, chest pain, interoceptive, body vigilance, cardiac anxiety, mediation
Each year about 4.6 million people in the United States are evaluated by an urgent medical service because of symptoms suggestive of an acute cardiac syndrome (Burt, 1999), however, estimates suggest that only about one-quarter of these individuals receive a confirmed cardiac diagnosis (Pope, Ruthazer, Beshansky, Griffith, & Selker, 1998). Some individuals are relieved that their symptoms are not indicative of a medical or cardiac diagnosis. Yet, a significant number of these patients continue to experience chest pain, worry about their cardiac function, and experience disability similar to patients with coronary artery disease despite their apparently favorable prognosis (Eifert, Hodson, Tracey, Seville, & Gunsawardane, 1996). This syndrome of recurrent chest pain in the absence of identifiable organic etiology is non-cardiac chest pain (NCCP).
Data on the medical course of NCCP is mixed. Whereas some studies show a good prognosis for NCCP patients following a negative coronary angiography (Lichtlen, Bargheer, & Wenzlaff, 1995), other studies show a higher mortality rate than the normal population (Bodegard, Erikssen, Bjornholt, Thelle, & Erikssen, 2004) or a rate not different from those with cardiac chest pain (Eslick & Talley, 2008). Progress in understanding the syndrome of NCCP is slowed and complicated by the diagnostic classification of NCCP as a ‘diagnosis’ of exclusion (i.e., medical rule-outs) rather than diagnostic inclusion (White, 2007). Yet, longitudinal studies show that patients with NCCP experience chest pain from 1–11 years after the initial evaluation (Papanicolaou et al., 1986; Wielgosz et al., 1984), and nearly half of NCCP patients (44%–50%) continue to believe that they have a cardiac condition up to one-year after negative evaluations (Ockene, Shay, Alpert, Weiner, & Dalen, 1980; Potts & Bass, 1993).
In the absence of wholly satisfactory medical explanations for NCCP, researchers have tended to conceptualize NCCP from a biopsychosocial perspective. Early pioneering researchers asserted the importance of studying both affective and pain qualities in this syndrome (Beitman et al., 1987; Eifert, 1991), and several modern theoretical models of NCCP (Eifert, Zvolensky, & Lejuez, 2000; Mayou, 1998; White & Raffa, 2004) have been adapted from or share common features with empirically supported models of panic disorder and health anxiety. Affective components, such as worry and rumination, link NCCP theories to broader theories of anxiety and health anxiety. The relevance of theories of panic disorder applied to NCCP is partly due to the central role physical sensations play in the development and maintenance of the problem. The most influential models of panic disorder implicate physical sensations in the etiology and maintenance of panic (Barlow, 1988, 2002; Clark, 1986; Reiss, 1991). In Barlow’s model, for instance, individuals with panic disorder possess a biological vulnerability and a psychological vulnerability (i.e., a sense that events and emotions are uncontrollable and unpredictable). This vulnerability results in an inward shift of attention during arousal that contributes to developing anxious apprehension about experiencing additional attacks. Individuals with anxious apprehension about future attacks have a propensity to associate interoceptive cues with the first panic through conditioning (termed ‘learned alarms’). Somatic and cognitive cues may trigger future panic attacks. This model and other influential models propose that panic is triggered by bodily sensations that may be misinterpreted and posits an important role (or essential role, in some cases; Clark, 1986) for conscious appraisal of the sensations as dangerous (Schmidt & Woolaway-Bickel, 2006). Similar hypotheses with adaptations have been extended to hypochondriasis (Barsky, Cleary, Sarnie, & Ruskin, 1994; Kellner, 1986; Warwick & Salkovskis, 1990) or cardiac neurosis (Liebhart, 1976). Moreover, in their model of hypochondriasis, Warwick and Salkovskis (1990) indicate that if a patient’s anxiety about a disease elicits autonomic symptoms that coincide with the symptoms of the feared disease, then anxiety will escalate. In sum, theoretical models of NCCP are rooted in the broad, deep foundations of decades of research in anxiety and anxiety-related disorders and there is considerable clinical utility in applying these models to the study of the problem of NCCP.
Prevalence rates for anxiety disorders are elevated among patients who experience NCCP. DSM-IV anxiety and mood disorders are overrepresented among patients with NCCP (Mayou, 1998; White et al., 2008), particularly the occurrence of panic attacks (White, Ruhr, & Gervino, 2009). Although the occurrence of panic attacks alone does not indicate panic disorder, physical sensations appear play an essential role in the development and maintenance of this functional syndrome for some NCCP patients. Consistent with current theoretical models of NCCP, it may be that following an initial chest pain experience, patients with NCCP selectively monitor and are vigilant to their cardiac activity. If they perceive cardiac changes (e.g., acceleration, fluttering), they may misinterpret this as an indication of cardiac dysfunction (e.g., myocardial infarction, coronary heart disease). These cognitions elicit anxiety that may culminate in increased heart rate and possible panic. A similar type of feedback loop has been validated in the false heart rate paradigm as applied to panic (Ehlers, Margraf, Roth, Taylor, & Birbaumer, 1988). Although actual palpitations did not increase in the laboratory, patients with panic disorder who were provided with false feedback of heart rate acceleration reported greater subjective and physiological anxiety (Ehlers et al., 1988), with some exceptions (Antony et al., 1995).
Available research suggests that patients with NCCP are fearful of physical sensations, particularly cardiac sensations (Aikens, Michael, Levin, & Lowry, 1999). Aikens and colleagues (2001) found that NCCP patients report greater fear of cardiopulmonary symptoms compared to other physical sensations; as a result, these authors concluded support for their ‘differential specificity hypothesis’ that stated that NCCP patients were differentially fearful of cardiopulmonary sensations. Given the high rates of anxiety disorders in this population, however, it is unclear whether these results were perhaps due, in full or in part, to the high rates of anxiety disorders in this population rather than any differential specificity, per se. Research examining this competing hypothesis is needed. Moreover, fears for chest pain (compared to other sensations; e.g., stomach upset, dizziness) are heightened partly due to the public perception that chest pain is dangerous. Chest pain is often associated with coronary artery disease -- the leading cause of death and disability in the United States (American Heart Association, 2006) – and public health education campaigns designed to increase public awareness of cardiac risk factors and the implications of chest pain may have increased anxiety among some individuals. Research examining whether NCCP patients are consciously more vigilant to cardiopulmonary sensations than other bodily sensations is needed. It may be that attentional focus on specific pain sensations (e.g., chest pain) is associated with increased pain. Patients with NCCP display low pain thresholds for cardiac-related stress tests (Bradley, Richter, Scarinci, Haile, & Schan, 1992), and NCCP patients’ anxiety about pain may negatively impact peak metabolic output in the cardiac-related stress tests (Stein, White, Berman, Covino, & Gervino, 2009). Research is needed to examine the possibility that patients with NCCP exhibit elevated cardiac hypervigilance compared to other physical sensations, and to examine whether this elevation is due partly to the association between NCCP and psychiatric disorders, particularly anxiety disorders.
We investigated body vigilance, cardiac anxiety, and the possible mediating role of interoceptive fear in patients with NCCP. First, we aimed to clarify the role of body vigilance – the extent that patients consciously attend to physical sensations – in this sample of NCCP patients. We hypothesized that patients would be more vigilant to cardiopulmonary sensations than other bodily sensations. Next, building on the work of Aikens and colleagues (1999), we examined the extent to which body vigilance may differ for patients with and without comorbid anxiety disorders. This study extends previous work by examining both conscious vigilance to and fear of physical sensations (i.e., cardiac-congruent and incongruent). We aimed to extend previous work to examine whether NCCP patients were both more vigilant to and more fearful of cardiopulmonary sensations compared to other physical sensations, and whether this difference was associated with the presence of a comorbid anxiety disorder. It was hypothesized that patients with comorbid anxiety disorders would show more body vigilance to cardiac sensations than patients without comorbid anxiety disorders. We theorized that the syndrome of NCCP might persist partly due to hypervigilance to cardiac-congruent body sensations increasing symptom recognition, particularly among anxious patients. Finally, consistent with theoretical models of NCCP, we sought to examine the extent that fear of anxiety-related physical sensations (i.e., interoceptive fear) mediated the impact of body vigilance and cardiac anxiety on pain. We theorized that the possible link between body vigilance and chest pain in the syndrome of NCCP might persist partly because of interoceptive fears, especially among anxious patients.
Method
Participants
Participants were 231 patients seeking evaluation in the cardiology department of a large, university-affiliated medical center. Patients were eligible based on these inclusion criteria: a) At least 18 years of age, b) Chief complaint of chest pain or discomfort, c) Completion of cardiac evaluation including general physical exam and exercise tolerance test, d) Tests indicated no abnormalities during an exercise tolerance test, and e) English language fluency. To enhance generalizability, patients were excluded only if they had a current or lifetime cardiac diagnosis (e.g., CHD, myocardial infarction), or current or recent (last 6 months) uncontrolled severe medical (e.g., diabetes) or psychiatric illness (e.g., active psychosis). Two patients were excluded from the study for failure to meet inclusion criteria at a follow-up data point. A final sample of 229 patients participated in this study.
Gender distribution in this sample was nearly equal (56% women), and the average age was 50 years (SD = 10.3, range = 27 to 78). The sample was predominantly Caucasian (83%); the remainder self-identified as African-American (12%), Hispanic/Latino (3%), or other race (2%). Fifty-six percent of the sample reported their marital status as married, 17% as single, never married, 14% divorced, 7% cohabitating, 3% separated, or 3% widowed. The sample was well educated with most having a bachelor’s degree (62%) or more schooling; nearly all had a high school diploma or equivalent degree or greater (98%). Employment status was identified as fulltime position (58%), part-time position (15%), retired (12%), unemployed (7%), disability (5%), full-time homemaker (2%), or student (1%). Many patients in this sample reported their household income to be equal to or greater than $60,000 (56%), 11% reported household income at or below $15,000.
Measures
Demographic and medical history
Demographic and medical history was assessed using a self-report questionnaire. Age, sex, race, marital status, and socioeconomic status were reported as well as general medical history (e.g., personal and family medical history, current medication use).
Psychiatric morbidity
The Anxiety Disorders Interview Schedule for the Diagnostic and Statistical Manual-4th edition (DSM-IV) (American Psychiatric Association, 1994) Lifetime Version (ADIS-IV-L) (Di Nardo, Brown, & Barlow, 1994) is a semi-structured diagnostic interview used to comprehensively evaluate DSM-IV anxiety, mood, somatoform, and substance use disorders and to screen for other major psychological disorders. Based on the interview results, diagnoses are evaluated both categorically (present or absent) and dimensionally (by clinical severity ratings and identification of principal diagnosis). All diagnoses are assigned a dimensional clinical severity rating (CSR) by the interviewer, which is scored on a “0” (no interference /distress) to “8” (extreme interference/distress) point scale reflecting the evaluator’s clinical judgment about the degree of interference and distress caused by the symptoms of a disorder. A CSR of four or greater indicates that the clinician evaluated the disorder to be present at a clinically significant level, whereas CSRs less than 4 indicate a subclinical disorder. The disorder with the highest CSR is the principal diagnosis that distinguishes it from other clinical and subclinical diagnoses that are additional diagnoses. The ADIS-IV-L has excellent reliability for DSM-IV anxiety and mood disorders (Brown, Campbell, Lehman, & Mancill, 2001). Diagnostic confidence ratings for this study ranged from 75% to 95% (M = 86%).
Chest pain
The Multidimensional Pain Inventory (MPI) (Kerns, Turk, & Rudy, 1985) is one of the most widely used measures of pain (Piotrowski, 1998), and studies have confirmed the adequacy of its psychometric properties (Kerns et al., 1985; Thompson, 1990). The MPI consists of 63-items that assess empirically derived scales that tap into three domains. The first domain examined assessed perceived pain intensity and the impact of pain on different aspects of patient’s lives. This domain consists of five subscales that measure 1) pain severity, 2) interference due to pain, 3) perceived control over pain and life events related to pain, 4) affective distress, and 5) support received from significant others. All items are rated on a 7-point Likert scale. Internal consistency ranged from 0.70 to 0.90, and test-retest coefficients range from 0.62 to 0.91 (Kerns et al., 1985). Internal consistencies for the scales used in this study were acceptable: MPI-Pain Severity (Cronbach’s α = .66) and MPI-Pain Interference (Cronbach’s α = 0.94). Chest pain history was assessed by anchored rating scales of the frequency, intensity, duration, and quality of their chest pain. Items were rated on Likert-type scales assessing frequency (0 = Never or rarely; 1 = Several times per day, 2 = Less than daily (every other day), 3 = About daily, 4 = About weekly, 5 = About monthly), intensity (1 = Not at all painful to 10 = Extremely painful), and duration (1 = A few seconds, 2 = Less than 5 minutes, 3 = 5–20 minutes, 4 = 21–60 minutes, 5 = More than one hour, 6 = About half the day, 7 = All day or longer, 8 = The pain is continuous, it does not stop. The context of chest pain onset and chest pain quality was also assessed.
Body Vigilance
The Body Vigilance Scale (BVS) (Schmidt, Lerew, & Trakowski, 1997) measures attention and sensitivity to interoceptive sensations. Patients completed the 4-items that assess total body vigilance as well as degree of attentional focus, perceived sensitivity to changes in bodily sensations, average time spent attending to sensations, and a separate composite rating of 15 bodily sensations (e.g., numbness, tingling, vision changes, nausea), for a total of 19-items. For example, patients rate the question “I am the kind of person who pays close attention to internal bodily sensations” on a 0 = Not at all like me to 10 = Extremely like me scale to assess attention to internal sensations. The BVS total scale has shown adequate reliability (Schmidt et al., 1997) and has been useful as an indicator of treatment response for panic disorder (Deacon & Abramowitz, 2006). Cronbach’s alpha in this study was .81. Domain-specific subscales were created for this study reflecting cardiopulmonary (.86), gastrointenstinal (.84), dissociative (.90), numbness (.92), and temperature (.76) related bodily sensations; adequate internal consistency was apparent on each subscale.
Emotional Distress
The Depression, Anxiety, Stress Scales (DASS) is a 42-item self-report measure consisting of three factor-analytically derived subscales that assess symptoms of depression, anxiety, and stress (Lovibond & Lovibond, 1995). Respondents indicate the extent that each statement applied to them over the past week on a 4-point Likert-type scale. The scales have good internal consistency, temporal stability, and convergent and discriminant validity in clinical (Brown, Chorpita, Korotitsch, & Barlow, 1997) and non-clinical samples (Lovibond & Lovibond, 1995). The measure was included here to evaluate whether patients completing questionnaires only differed systematically from those who completed the diagnostic interview and questionnaires on levels of emotional distress.
Interoceptive Fear
The Albany Panic and Phobia Questionnaire-revised (APPQ) is a 24-item questionnaire measuring situational, interoceptive, and social fear (Brown, White, & Barlow, 2005). This scale is a modification of the original scale (Rapee, Craske, & Barlow, 1994/1995). Patients rate how much fear they would expect to experience in certain activities and situations in the next week on a 0 (no fear) to 8 (extreme fear) Likert scale. The Interoceptive scale (APPQI), composed of five items measuring fear of activities that cause physical sensations (e.g., hiking on a hot day, exercising vigorously alone) was examined in this study. Evidence from clinical samples supports the reliability, factor structure, factor determinacy, and convergent and discriminant validity of the APPQ-R (Brown et al., 2005). Cronbach’s alpha was .89 in this study.
Cardiac Anxiety
Patients completed the 18-item Cardiac Anxiety Questionnaire (CAQ) which assesses fear of cardiac-related stimuli and sensations because of their perceived negative consequences (Eifert, Thompson et al., 2000). The CAQ consists of a total score and three subscales of Fear, Avoidance, and Attention associated with cardiac-focused anxiety. For example, patient rate the question “When I have chest discomfort or when my heart is beating fast, I worry that I may have a heart attack” on a 0 = Never to 4 = Always scale to assess their cardiac fear. The CAQ-Total Scale and the three subscale scores are computed as the mean of the relative frequency ratings for each of the 18 items. The CAQ-Total scale and the three subscales have been shown to have adequate reliability and convergent and divergent properties of the scale are promising (Eifert, Thompson et al., 2000). Reliability in this study was adequate for the total scale (Cronbach’s α = 0.86) and the three subscales (Fear = .81, Avoidance = .85, and Attention = .73), respectively.
Procedure
The Institutional Review Boards at Boston University and Beth Israel Deaconess Medical Center at Harvard Medical School approved this study. This study took place at a large, urban, university-affiliated cardiology department. All patients seeking evaluation for a chief complaint of chest pain who showed no evidence of electrocardiogram changes during an exercise tolerance test were eligible to participate. Clinical physiology technicians informed patients that their testing showed no abnormalities during the exercise tolerance test, and they invited patients to participate in a research study on medical and psychological factors that may cause chest pain. Research staff contacted patients by telephone to complete an eligibility screen based on inclusion and exclusion criteria. Eligible patients were invited to participate in a longitudinal study that included clinical interview and self-report questionnaires at four time points. Eligible patients participated in the process of informed consent, and patients read, signed, and dated the consent form. Patients were compensated $25 for participation at each time point of the study. All patients were encouraged to participate in both the interview and questionnaire, and patients were permitted to do either the questionnaire or the interview only. Patients completed the questionnaire and returned it to the research office in a pre-paid envelope. Trained clinical psychology doctoral students or a licensed psychologist conducted the clinical interviews.
Data Analyses
Data were analyzed using structural equation modeling with latent variables (Bollen, 1989). Separate analyses were conducted on measurement models that specified the relations between the observed variables (i.e., scores on the measures) and the latent variables they were believed to represent, and latent variable models that specified the pattern of relations among the latent variables. Within each model, analyses were based on 2–3 item parcels or subsets of items within each subscale. Items were matched based on their item-total correlations and then randomly assigned to parcels to facilitate uniform internal consistency. The fit of each model was examined based on several criteria including the comparative fit index (CFI), the Tucker-Lewis fit index (TLI), and the root mean square error of approximation (RMSEA) and its 90% confidence interval. Acceptable model fit was evaluated on the basis of several criteria including: CFI (> .90), TLI (> .90) (Bentler, 1992), and RMSEA (< .08, 90% CI < .08) (Browne & Cudeck, 1993). Multiple indices of model fit were used because they provide different information for evaluating model fit (e.g., absolute fit, fit adjusting for model parsimony, fit relative to a null model) and because they result in a more conservative and reliable evaluation of the model fit. Data were analyzed using Version 4.21 of Mplus (Muthén & Muthén, 1998–2007). One of its important features is a maximum likelihood estimation procedure that uses all cases within the data set, including those with missing data. This procedure uses the EM algorithm (Little & Schenker, 1995) to estimate means, variances and covariances among the manifest variables. This feature allowed model estimates to be calculated using all cases that provided data on some measures, but that may have had data missing on a specific scale. The EM algorithm is a preferred method of imputation largely because it uses an iterative process to improve the prediction of missing values as more missing data is imputed (Little & Schenker, 1995).
Results
Response Rate and Attrition
A total of 229 patients participated in this study: 147 patients completed the clinical interview, 113 patients completed the questionnaire battery and the clinical interview, 83 patients completed the questionnaire only, and 34 patients completed the interview only. Parametric and nonparametric tests revealed no significant differences on age, sex, ethnicity, education level, employment status, and income between the group completing the questionnaire only and the group completing the interview and questionnaire. The groups also did not differ on anxiety (DASS-Anxiety), depression (DASS-Depression), or stress (DASS-Stress). Chest pain severity (MPI-Severity) and interference (MPI-Interference) did not differ between groups either. The absence of differences between groups helps to ensure that no systematic selection bias influenced study participation.
Chest Pain Characteristics
Approximately one-half (55%) of patients had experienced chest pain for 6 months or longer, and 25% of patients reported pain for at least 1–6 months. Fifty-one percent of patients experienced episodes of chest pain at least weekly (10% experienced chest pain several times per day), and most patients (50%) described their pain as at moderate intense or greater. Overall, 60% of patients described a sudden chest pain onset, and most indicated that their pain was episodic in nature as compared to chronic or persistent pain. Most patients (63%) described their chest pain episodes as lasting less than 20 minutes each (Mode = 24%, "5 to 20 minutes"; followed by 22%, "less than 5 minutes"); 8% of patients reported that their chest pain typically lasted a full day or longer. The majority of the sample (73%) reported only mild interference from chest pain. Over 70% patients had one or two chest-pain related physician visits in the past year; 10% reported several chest-pain related physician visits in the past year. Self-reported pain scores on the MPI and the pain impact subscales (i.e., MPI-Pain Severity, MPI-Interference, MPI-Life Control, MPI-Affective Distress, and MPI-Support) were lower than most values reported in chronic pain samples (McCarberg & Wolf, 1999; Turk & Rudy, 1990). This group of patients with NCCP reported less pain severity and less life interference due to pain than that reported in other normative or chronic pain samples.
Psychiatric Comorbidity
Overall, the prevalence of patients having any current Axis I diagnosis was 44% (White et al., 2008). The prevalence of any anxiety disorder or any mood disorder in this sample was 41% and 13%, respectively. An additional 34% (n = 49) and 4.8% (n = 7) of patients were diagnosed with at least one subclinical anxiety or mood disorder. In total, over 75% of the sample was diagnosed with at least one clinical or subclinical Axis I disorder. Among those patients with at least one clinical diagnosis, the frequency of diagnoses assigned ranged from 1–5 diagnoses, and the average number of anxiety and mood disorder diagnoses was 1.78 anxiety disorders (SD = 1.7) and 0.3 (SD = 0.44) mood disorders. Social phobia (16%), specific phobia (14%), generalized anxiety disorder (13%), and panic disorder (12%) were the most common current anxiety disorders diagnosed present in this sample. A total of 6% were assigned a diagnosis of anxiety disorder not otherwise specified (NOS) because they showed prominent anxiety or anxiety-related avoidance that did not meet criteria for any specific anxiety disorder. A total of 13% of the sample were diagnosed with depressive disorders. Of these, 8% of the sample met criteria for major depressive disorder, 5% met criteria for dysthymic disorder, and just over 3% were diagnosed with a mood disorder NOS. Undifferentiated somatoform disorder was evident in 6.8% of the sample, and alcohol or substance abuse was diagnosed in 5% of the sample. Clinically significant hypochondriasis was diagnosed in only two patients. The remainder of the sample (25%) did not report or exhibit clinical or subclinical symptoms of any Axis I disorder; 56% of patients did not have any clinically significant Axis I disorders. A detailed report of DSM-IV Axis I psychiatric disorders is reported separately (White et al., 2008).
Vigilance to Cardiopulmonary Sensations
To investigate whether patients with NCCP are more consciously vigilant to cardiopulmonary sensations relative to other physical sensations, we used multiple paired samples t-tests (df = 189) to compare cardiopulmonary scores with the scores of each of the other factors (i.e., Gastrointestinal, Dissociative, Numbness, Heat); corrected alpha using Bonferroni correction adjusted p value = .0125. As expected, cardiopulmonary vigilance was significantly elevated relative to all other forms of body vigilance: gastrointestinal (t = 13.1, p < .001; d = .94), dissociative (t = 4.4, p < .001; d = .32), numbness (t = 13.8, p < .001, d = 1.0), and heat (t = 15.2, p < .001, d = 1.1). Results show that NCCP patients are more vigilant to cardiopulmonary sensations compared to other bodily sensations.
Psychiatric Comorbidity and Body Vigilance
A series of one-way ANOVAs examined the association between presence of a DSM-IV Axis I psychiatric disorder and body vigilance. As hypothesized, patients with any Axis I morbidity reported increased body vigilance for all somatic domains (F’s 1.5 – 10, p’s < .05) except heat vigilance (BVS-Heat). Patients with any Axis I morbidity also reported more body vigilance overall, F (1,103) = 12.5, p < .01, d = .66), and increased attention, sensitivity to body changes, body scanning, and symptom vigilance, F’s = 7.8 – 10.6, p’s < .01. More specifically, patients with an Axis I anxiety disorder reported increased body vigilance overall (F (1,106) = 4.4, p < .05, d = .40) and increased symptom attention (F (1,108) = 5.4, p < .05, d = .44). These results show that NCCP patients with comorbid anxiety disorders differed from NCCP patients without anxiety disorders in their report of cardiorespiratory symptom vigilance (all p’s < .05).
Relations Among Variables
Prior to examining the theoretical models, the measurement model representing the relations between the measures and the latent factors was examined (see Figure 1). Analyses of the 4-factor measurement model indicated that the solution fit the data well, χ2 (21, N = 149) = 33.3, p < .05, CFI = .97, TLI = .95, RMSEA = .063 (.012/.101), variance explained = 53%. Loadings representing relations between the observed variables and the four latent factors were all significant at p < .001, with standardized values all greater than .50. Correlations among the latent factors were all significant at p < .01. Factor determinacies (i.e., validity coefficients reflecting the correlation between factor score estimates and their respective factors) were computed on the factor scores. All three factors evidenced good levels of determinacy, range .87–.98, based on > .80 guideline (Grice, 2001). Items reflecting attention to bodily sensations were evident on two scales (i.e., CAQ-Attention, BVS-Attention). To ensure that the cardiac anxiety factor represented anxiety-based concerns not related to attentional processes, the cardiac anxiety factor was represented only by the heart-focused fear and avoidance scales but not the attentional scale of the CAQ that was evident in the item-scale content overlap.
Figure 1.
Initial Measurement model representing relations between observed variables and latent factors. Rectangles represent observed variables, ovals represent latent factors, and solid lines with arrows represent relations among the observed variables and latent factors. Inspection of the item-scale content and factor loadings, the items reflecting attention to heart-related sensations were evident on two scales (i.e., CAQ-Attention, BVS-Attention). To ensure that the theoretical construct of cardiac anxiety represented concerns reflected cardiac anxiety and related behaviors and not attentional processes, the Cardiac Anxiety Factor was represented by cardiac worry and avoidance.
Latent Variable Path Models
Latent variable path models were used to examine the hypotheses regarding the extent to which interoceptive fear mediated the impact of bodily vigilance and cardiac anxiety on chest pain. Within each model, diagnostic status, bodily vigilance, and cardiac anxiety were considered exogenous variables that predicted interoceptive fear, which in turn predicted pain. Exogenous variables in structural models are specified to be measured without error. In this model, the covariances among observed independent variables are estimated as the sample values. Separate models for body vigilance and cardiac anxiety were examined. Psychiatric disorder status was included in each model to examine the association of psychiatric status with the interoceptive fear and pain factors.
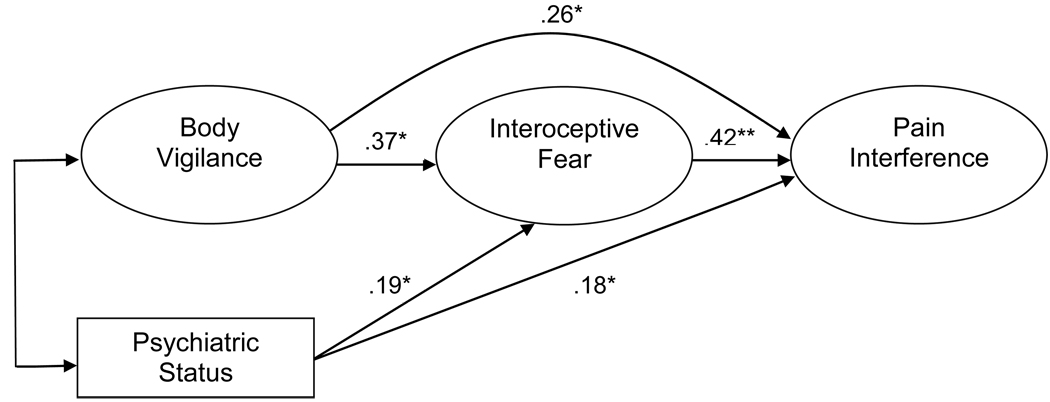
The analysis of the body vigilance model indicated that the model provided a good fit to the data, χ2 (15, N = 149) = 39.3, p >.05, CFI = .96, TLI = .93, RMSEA = .07 (.00/.13), variance explained = 61%. All factor indicators loaded significantly onto their respective factor (at p < .05), and all standardized factor loadings in the final solution were greater than .18. The fit of this model was not significantly different from the fit of the unconstrained baseline model indicating that constraining the model did not result in a decrement in model fit with the additional parameter constraints of the latent variable path model. Examination of modification indices resulted in improved model fit with the addition of one correlated error term between an indicator of the interoceptive fear and an indicator of the chest pain factor. Analysis of the cardiac anxiety factor model also provided an adequate fit to the data, χ2 (15, N = 149) = 31.5, p < .05, CFI = .95, TLI = .91, RMSEA = .08 (.04/.13), variance explained = 57%. Similar to the body vigilance model, the latent variable path model for cardiac anxiety fit the data equally well compared to the baseline model (i.e., uncontrained measurement model) despite the additional constraints in the latent variable model. For each model, the association between interoceptive fear with chest pain was significant with standardized path coefficients of .42 and .37, respectively. Paths linking each of the factors representing body vigilance and cardiac anxiety to the interoceptive fear factor were also significant. The cardiac anxiety factor had the strongest association with the interoceptive fear factor with a standardized coefficient of .67 compared to .37 for the body vigilance factor. The body vigilance factor also had a significant direct effect on pain (β = .26), however, the cardiac anxiety factor did not have a direct effect on pain after controlling for interoceptive fear (p > .05). These findings are consistent with partial mediation (Baron & Kenny, 1986) for the body vigilance factor and full mediation for the cardiac anxiety factor. That is, body vigilance had both a direct and indirect association with chest pain; however, cardiac anxiety had an indirect association with chest pain that was fully mediated by interoceptive fear. In sum, interoceptive fear played a strong mediating role for both body vigilance and cardiac anxiety in this sample.
Discussion
Theories have posited a central role for body vigilance (i.e., conscious attention directed at internal physical sensations) in the development and persistence of NCCP (Eifert, 1992; Mayou, 1998; White & Raffa, 2004). In this study, we examined body vigilance by the rate and pattern of conscious monitoring and evaluation of internal sensations in patients with NCCP. We hypothesized that patients would be more vigilant to cardiac-congruent sensations (e.g., heart palpitations, chest discomfort) than other bodily sensations that were cardiac-incongruent (e.g., stomach upset, nausea, faintness, dizziness, numbness). Consistent with expectations, NCCP patients in this study displayed hypervigilance for cardiac-related symptoms compared to non-cardiac symptom domains. These results reinforce theoretical models of NCCP that propose the syndrome is associated with an exaggerated vigilance to cardiac-specific symptoms. Consistent with past research on differential fear in NCCP patients (Aikens, Zvolensky, & Eifert, 2001), this study extended this literature to reveal that NCCP patients may also be prone to differential body vigilance for cardiopulmonary sensations.
Consistent with our predictions, presence of psychiatric comorbidity was associated with increased body vigilance among patients with NCCP. Patients with comorbid anxiety and depressive disorders were more sensitive to changes in bodily sensations, engaged in more body scanning, and endorsed more symptom vigilance overall compared to individuals without these disorders. Similarly, patients with psychiatric disorders were more vigilant to cardiorespiratory symptoms relative to other body symptoms, and this was not the case among patients without any comorbid psychiatric disorders. Our results are consistent with prior literature showing that anxiety and depression are associated with more symptom reporting in medical patients (Katon, Lin, & Kroenke, 2007) and with more physical symptoms in patients with medically unexplained physical symptoms (Henningsen, Zimmermann, & Sattel, 2003). Based on our small-to-moderate effect sizes, however, it seems unlikely that the body symptoms are solely due to the physical expression of a concurrent anxiety and/or depressive disorder. It may be that patients with psychiatric disorders experience elevated bodily vigilance partly as a partly as a consequence of their disorder status. For instance, the internal focus of attention (commonly termed interoceptive sensitivity) that is more likely among patients with anxiety and depression may increase their odds of noticing physiological changes. As such, it may be that body vigilance is part of a sequence of events – body vigilance may lead to increased autonomic arousal, an increased likelihood of increased likelihood of perceiving threatening interoceptive symptoms, and in turn, these symptoms may increase attentional focus on bodily pain cues, particularly chest pain symptoms. On the other hand, it cannot be ruled out that NCCP patients suffer from lower pain thresholds (Bradley et al., 1992), particularly among those with psychiatric disorders. Also, the measures of chest pain reported herein were self-report and represent patients’ perception of their chest pain. It is possible that among patients who also experience panic attacks, there is some shared overlap between the patients’ report of chest pain and their symptoms of panic attacks or an anxiety disorder, particularly panic disorder. Distinguishing the somatic symptoms from the emotional disorder is a challenge in many functional pain syndromes (e.g., fibromyalgia, irritable bowel syndrome). Research is needed to make clear the possible construct overlap between the chest pain symptoms and the emotions in this anxious pain population, including the role that subclinical or limited symptom panic attacks may play.
Finally, we examined body vigilance, cardiac anxiety, and the possible mediating role of interoceptive fear on chest pain. Partly consistent with hypotheses, results showed that higher body vigilance was associated with increased chest pain and impairment and this association was partially mediated by interoceptive fear. In other words, the influence of body vigilance on chest pain was partly diminished after accounting for interoceptive fear. In addition, our results showed that the impact of cardiac anxiety on pain was fully mediated by interoceptive fear. Considerable research has shown that the syndrome of NCCP can be persistent in some patients (Potts & Bass, 1993; Wielgosz et al., 1984), and our data suggest that conscious attention to body sensations, particularly those sensations that are perceived as threatening or fearful (i.e., cardiopulmonary sensations), is associated with increased chest pain and impairment. Our findings are consistent with research conducted in the laboratory showing that conscious attention is associated with increased pain (Arntz, Dreessen, & Merckelbach, 1991) – however, the influence of body vigilance on chest pain was partly diminished after accounting for the mediating effect of interoceptive fear. It may be that consciously attending to bodily sensations is associated with anxious cognitive processing, particularly in patients who may be prone to heart-focused worry, and as a result, chest pain may be one physical manifestation of this affective state. Patients with NCCP may feel a wide range of somatic sensations but may selectively attend to (and report) only those bodily sensations that are perceived as threatening because of their presumed cardiovascular significance (e.g., chest pain, shortness of breath, palpitations). As a result, these patients may be vigilant to only feared sensations relating to their heart. This may help to explain why many of these patients screen negative for full blown panic attacks (i.e., they do not endorse 4 or more symptoms) (Beitman, Kushner, Lamberti, & Mukerji, 1990; White et al., 2009).
Interpretive caveats and directions for future research merit consideration. First and most importantly, this was a within-subjects study and did not include a comparison or control group. As a result, it is not possible to examine whether the results pertain uniquely to patients with NCCP. It is possible that these findings could apply to other community samples or groups of patients. The syndrome of NCCP occurs in patients with coronary artery disease, and these findings are generalizable to patients with NCCP who receive a negative medical evaluation and who show no abnormalities during an exercise tolerance test. At first blush, it may appear somewhat surprising that our sample consists of nearly equal numbers of males and females in this study on psychiatric comorbidity in NCCP. However, our study was not complicated by the selection parameters (i.e., pre-screening criteria) and referral patterns evident in past research that may led to biased age and sex distributions and psychiatric comorbidity estimates. Our results are generalizable to white, non-Hispanic, educated patients seeking evaluation in from a cardiovascular specialist for chest pain. Exercise tolerance testing has excellent reliability and predictive validity (Goldschlager, Selzer, & Cohn, 1976), and our laboratory has demonstrated excellent sensitivity and specificity (84% and 95%, respectively); for a more detailed discussion, please see guidelines (Gibbons et al., 1997). Future research that examines how the syndrome of NCCP differs in patients with and without disease (i.e., coronary artery disease), particularly how body vigilance for threatening physical sensations may function for groups of differing risk profiles (i.e., CAD-high risk versus minimal or low risk, personal family history significant for cardiac disease). Second, the results presented here are cross-sectional, and longitudinal studies that disentangle if body vigilance and psychiatric morbidity relate to long-term risk in NCCP patients are needed. At present, we are following up this sample and a second sample of patients using a prospective design. Longitudinal studies with more diverse samples are needed to examine alternative models over time. For instance, equivalent models cannot be distinguished in terms of overall fit (McCallum, Wegener, Uchino, & Fabriger, 1993), however, there may be other substantially meaningful alternative models that are plausible (e.g., cardiac anxiety may mediate the association between interoceptive fear and chest pain). Third, our study alluded to autonomic dysregulation in patients with NCCP, however, this study did not examine biomarkers of autonomic dysregulation (e.g., cortisol, heart rate variability, and baroreflex sensitivity). Future research examining the bidirectional pathways underlying how the negative emotions of depression and anxiety influence pain in this patient group is needed.
The syndrome of NCCP has long been frustrating for the medical community – and research examining the risk and resilience factors associated with the pain and persistence of this syndrome is still in the early stages. These findings show that an important subgroup of patients with NCCP show an exaggerated attention to cardiac-congruent sensations, particularly those with psychiatric comorbidity. It remains unclear if the cardiac-congruent hypervigilance and fear identified herein translates to an increase in long-term cardiovascular risk – perhaps through reduced cardioprotective behaviors (i.e., exercise, physical exertion) and/or increased risk behaviors (e.g., sedentary behaviors, social withdrawal; White, 2007). Clinical research examining disease-related risk in this patient group is necessary and timely, particularly because existing data regarding medical outcomes for these patients show a mixed prognosis (Bodegard et al., 2004; Eslick & Talley, 2008; Lichtlen et al., 1995). Research that examines the risk and resilience factors that contribute to the syndrome of NCCP will serve as a foundation upon which to begin to identify they best ways to intervene for each individual.
Figure 2.
Combined cross-sectional latent variable path model representing hypothesized relations among body vigilance, interoceptive fear, and chest pain. The rectangle represents an observed variable, the ovals represent latent factors, and the solid lines with arrows represent relations among the observed variables and latent factors. To decrease the complexity of the figure, the figure does not show indicator variables for latent factors, paths that were not significant, disturbance terms, or relations between observed variables and latent variables.
Acknowledgments
Grants from the National Institutes of Health, National Institute of Mental Health (MH63185) and the University of Missouri-Saint Louis (University Research Award, awarded to Kamila White) supported this research and the preparation of this manuscript. The contents herein are solely the responsibility of the author and do not necessarily represent the view of the funding sources.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kamila S. White, University of Missouri-Saint Louis
Jennifer M. Craft, University of Missouri-Saint Louis
Ernest V. Gervino, Beth Israel Deaconess Medical Center, Harvard Medical School
References
- Aikens JE, Michael E, Levin T, Lowry E. The role of cardioprotective avoidance beliefs in noncardiac chest pain and associated emergency department utilization. Journal of Clinical Psychology in Medical Settings. 1999;6:317–332. [Google Scholar]
- Aikens JE, Zvolensky MJ, Eifert GH. Differential fear of cardiopulmonary sensations in emergency room noncardiac chest pain patients. Journal of Behavioral Medicine. 2001;24:155–167. doi: 10.1023/a:1010710614626. [DOI] [PubMed] [Google Scholar]
- American Heart Association. Heart and stroke statistical update. Dallas, TX: 2006. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: Author; 1994. [Google Scholar]
- Antony M, Brown TA, Craske MG, Barlow DH, Mitchell WB, Meadows E. Accuracy of heart beat perception in panic disorder, social phobic, and non-anxious subjects. Journal of Anxiety Disorders. 1995;9:355–371. [Google Scholar]
- Arntz A, Dreessen L, Merckelbach H. Attention, not anxiety, influences pain. Behaviour Research and Therapy. 1991;29:41–50. doi: 10.1016/s0005-7967(09)80006-5. [DOI] [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford Press; 1988. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barsky AJ, Cleary PD, Sarnie MK, Ruskin JN. Panic disorder, palpitations, and the awareness of cardiac activity. Journal of Nervous and Mental Disease. 1994;182:63–71. doi: 10.1097/00005053-199402000-00001. [DOI] [PubMed] [Google Scholar]
- Beitman BD, Basha I, Flaker G, DeRosear L, Mukerji V, Trombka L, et al. Atypical or nonanginal chest pain. Panic disorder or coronary artery disease? Archives of Internal Medicine. 1987;147:1548–1552. [PubMed] [Google Scholar]
- Beitman BD, Kushner MG, Lamberti JW, Mukerji V. Panic disorder without fear in patients with angiographically normal coronary arteries. Journal of Nervous and Mental Disease. 1990;178:307–312. doi: 10.1097/00005053-199005000-00005. [DOI] [PubMed] [Google Scholar]
- Bentler PM. On the fit of models to covariances and methodology to the Bulletin. Psychological Bulletin. 1992;112:400–404. doi: 10.1037/0033-2909.112.3.400. [DOI] [PubMed] [Google Scholar]
- Bodegard J, Erikssen G, Bjornholt JV, Thelle D, Erikssen J. Possible angina detected by the WHO angina questionnaire in apparently healthy men with a normal exercise ECG: coronary heart disease or not? A 26 year follow up study. Heart. 2004;90:627–632. doi: 10.1136/hrt.2003.012542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York, NY: John Wiley and Sons; 1989. [Google Scholar]
- Bradley LA, Richter JE, Scarinci IC, Haile JM, Schan CA. Psychosocial and psychophysical assessments of patients with unexplained chest pain. The American Journal of Medicine. 1992;92:65–73. doi: 10.1016/0002-9343(92)80059-9. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Mancill R. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch B, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- Brown TA, White KS, Barlow DH. A psychometric reanalysis of the Albany Panic and Phobia Questionnaire. Behaviour Research and Therapy. 2005;43:337–355. doi: 10.1016/j.brat.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage Publications; 1993. pp. 136–162. [Google Scholar]
- Burt CW. Summary statistics for acute cardiac ischemia and chest pain visits to United States EDs. 1995–1999. American Journal of Emergency Medicine. 1999;17:552–559. doi: 10.1016/s0735-6757(99)90195-x. [DOI] [PubMed] [Google Scholar]
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Deacon B, Abramowitz J. A pilot study of two-day cognitive-behavioral therapy for panic disorder. Behaviour Research and Therapy. 2006;44:807–817. doi: 10.1016/j.brat.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety disorders interview schedule for DSM-IV: Lifetime version. San Antonio, TX: Oxford University Press; 1994. [Google Scholar]
- Ehlers A, Margraf J, Roth WT, Taylor CB, Birbaumer N. Anxiety induced by false heart rate feedback in patients with panic disorder. Behaviour Research and Therapy. 1988;26:1–11. doi: 10.1016/0005-7967(88)90028-9. [DOI] [PubMed] [Google Scholar]
- Eifert GH. Cardiophobia: An anxiety disorder in its own right? Behaviour Change. 1991;8:100–116. [Google Scholar]
- Eifert GH. Cardiophobia: A paradigmatic behavioural model of heart-focused anxiety and non-anginal chest pain. Behaviour Research and Therapy. 1992;30:329–345. doi: 10.1016/0005-7967(92)90045-i. [DOI] [PubMed] [Google Scholar]
- Eifert GH, Hodson SE, Tracey DR, Seville JL, Gunsawardane K. Heart-focused anxiety, illness beliefs, and behavioral impairment: Comparing healthy heart-anxious patients with cardiac and surgical inpatients. Journal of Behavioral Medicine. 1996;19:385–399. doi: 10.1007/BF01904764. [DOI] [PubMed] [Google Scholar]
- Eifert GH, Thompson RN, Zvolensky MJ, Edwards K, Frazer NL, Haddad JW, et al. The Cardiac Anxiety Questionnaire: Development and preliminary validity. Behaviour Research and Therapy. 2000;38:1039–1053. doi: 10.1016/s0005-7967(99)00132-1. [DOI] [PubMed] [Google Scholar]
- Eifert GH, Zvolensky MJ, Lejuez CW. Heart-focused anxiety and chest pain: A conceptual and clinical review. Clinical Psychology: Science and Practice. 2000;7:403–417. [Google Scholar]
- Eslick GD, Talley NJ. Natural history and predictors of outcome for non-cardiac chest pain: A prospective 4-year cohort study. Neurogastroenterology and Motility. 2008;20:989–997. doi: 10.1111/j.1365-2982.2008.01133.x. [DOI] [PubMed] [Google Scholar]
- Gibbons RJ, Balady GJ, Beasley JW, Bricker JT, Duvernoy WF, Froelicher VF, et al. ACC/AHA guidelines for exercise testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee of Exercise Testing) Journal of the American College of Cardiology. 1997;30:260–311. doi: 10.1016/s0735-1097(97)00150-2. [DOI] [PubMed] [Google Scholar]
- Goldschlager N, Selzer A, Cohn K. Treadmill stress tests as indicators of presence and severity of coronary artery disease. Annals of Internal Medicine. 1976;85:277–286. doi: 10.7326/0003-4819-85-3-277. [DOI] [PubMed] [Google Scholar]
- Grice JW. Computing and evaluating factor scores. Psychological Methods. 2001;6:430–450. [PubMed] [Google Scholar]
- Henningsen P, Zimmermann T, Sattel H. Medically unexplained physical symptoms, anxiety, and depression: A meta-analytic review. Psychosomatic Medicine. 2003;65:528–533. doi: 10.1097/01.psy.0000075977.90337.e7. [DOI] [PubMed] [Google Scholar]
- Katon W, Lin EHB, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. General Hospital Psychiatry. 2007;29:147–155. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- Kellner R. Somatization and hypochondriasis. New York, NY: Praeger; 1986. [Google Scholar]
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Lichtlen PR, Bargheer K, Wenzlaff P. Long-term prognosis of patients with angina-like chest pain and normal coronary angiographic findings. Journal of the American College of Cardiology. 1995;25:1013–1018. doi: 10.1016/0735-1097(94)00519-v. [DOI] [PubMed] [Google Scholar]
- Liebhart EH. On attributing fictitious cardiac responses. Perceptual and Motor Skills. 1976;43:202. doi: 10.2466/pms.1976.43.1.202. [DOI] [PubMed] [Google Scholar]
- Little RJA, Schenker N. Missing data. In: Arminger GH, Clogg CC, Sobel ME, editors. Handbook of statistical modeling for the social and behavioral sciences. New York: Plenum; 1995. pp. 39–75. [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Mayou RA. Chest pain, palpitations and panic. Journal of Psychosomatic Research. 1998;44:53–70. doi: 10.1016/s0022-3999(97)00209-2. [DOI] [PubMed] [Google Scholar]
- McCallum RC, Wegener DT, Uchino BN, Fabriger LR. The problem of equivalent models in applications of covariance structure analysis. Psychological Bulletin. 1993;114:185–199. doi: 10.1037/0033-2909.114.1.185. [DOI] [PubMed] [Google Scholar]
- McCarberg B, Wolf J. Chronic pain management in a health maintenance organization. Journal of Pain. 1999;15:5057. doi: 10.1097/00002508-199903000-00008. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus Statistical Analysis with Latent Variables, Version 4.21. Los Angeles, CA: Muthén & Muthén; 1998-2007. [Google Scholar]
- Ockene IS, Shay MJ, Alpert JS, Weiner BH, Dalen JE. Unexplained chest pain in patients with normal coronary arteriograms: A follow-up study of functional status. New England Journal of Medicine. 1980;303:1249–1252. doi: 10.1056/NEJM198011273032201. [DOI] [PubMed] [Google Scholar]
- Papanicolaou MN, Califf RM, Hlatky MA, McKinnis RA, Harrel FEJ, Mark DB, et al. Prognostic implications of angiographically normal and insignificantly narrowed coronary arteries. American Journal of Cardiology. 1986;58:1181–1187. doi: 10.1016/0002-9149(86)90378-4. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW, Gonder-Frederick L, Cox DJ, Hoover CW. The perception of general versus specific visceral activity in the activity and the regulation of health-related behavior. Advances in Behavioral Medicine. 1985;1:165–198. [Google Scholar]
- Piotrowski C. Assessment of pain: A survey of practicing clinicians. Perceptual and Motor Skills. 1998;86:181–182. doi: 10.2466/pms.1998.86.1.181. [DOI] [PubMed] [Google Scholar]
- Pope JH, Ruthazer R, Beshansky JR, Griffith JL, Selker HP. Clinical features of emergency department patients presenting with symptoms suggestive of acute cardiac ischemia: A multicenter study. Journal of Thrombosis and Thrombolysis. 1998;6:63–74. doi: 10.1023/A:1008876322599. [DOI] [PubMed] [Google Scholar]
- Potts SG, Bass CM. Psychosocial outcome and use of medical resources in patients with chest pain and normal or near normal coronary arteries: A long-term follow-up study. Quarterly Journal of Medicine. 1993;86:583–593. [PubMed] [Google Scholar]
- Rapee RM, Craske MG, Barlow DH. Assessment instrument for panic disorder that includes fear of sensation producing activities: The Albany Panic and Phobia Questionnaire. Anxiety. 1994/1995;1:114–122. doi: 10.1002/anxi.3070010303. [DOI] [PubMed] [Google Scholar]
- Reiss S. Expectancy model of fear, anxiety and panic. Clinical Psychology Review. 1991;11:141–154. [Google Scholar]
- Schmidt NB, Lerew DR, Trakowski JH. Body vigilance in panic disorder: Evaluating attention to bodily perturbations. Journal of Consulting and Clinical Psychology. 1997;65:214–220. doi: 10.1037//0022-006x.65.2.214. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Woolaway-Bickel K. Cognitive-vulnerability to panic disorder. In: Alloy LB, Riskind JH, editors. Cognitive vulnerability to emotional disorders. Hillsdale, NJ: Erlbaum; 2006. [Google Scholar]
- Stein DS, White KS, Berman S, Covino NA, Gervino EV. Psychological and sociodemographic factors in the non-cardiac chest pain patient impacting performance on the cardiac stress test. Manuscript in preparation for publication. 2009 [Google Scholar]
- Thompson M. Investigation into the reliability and validity of a multidimensional pain inventory in an oncology population. Oncology Nursing Forum. 1990;17:160. [Google Scholar]
- Turk DC, Rudy TE. The robustness of an empirically derived taxonomy of chronic pain patients. Pain. 1990;43:27–35. doi: 10.1016/0304-3959(90)90047-H. [DOI] [PubMed] [Google Scholar]
- Warwick HM, Salkovskis PM. Hypochondriasis. Behaviour Research and Therapy. 1990;28:105–117. doi: 10.1016/0005-7967(90)90023-c. [DOI] [PubMed] [Google Scholar]
- White KS. Cardiovascular disease and anxiety disorders. In: Zvolensky MJ, Smits JAS, editors. Health behaviors and physical illness in anxiety and its disorders: Contemporary theory and research. New York, NY: Springer; 2007. pp. 279–315. [Google Scholar]
- White KS, Raffa SD. Anxiety and other emotional factors in noncardiac chest pain. Mental Fitness. 2004;3:60–67. [Google Scholar]
- White KS, Raffa SD, Jakle KR, Stoddard JA, Barlow DH, Brown TA, et al. Morbidity of DSM-IV Axis I disorders in non-cardiac chest pain: Psychiatric morbidity linked with increased pain and health care utilization. Journal of Consulting and Clinical Psychology. 2008;76:422–430. doi: 10.1037/0022-006X.76.3.422. [DOI] [PubMed] [Google Scholar]
- White KS, Ruhr LR, Gervino EV. Fearful and non-fearful panic attacks associated with elevated CAD-risk profiles in patients with non-cardiac chest pain. Manuscript in preparation for publication. 2009 [Google Scholar]
- Wielgosz AT, Fletcher RH, McCants CB, McKinnis RA, Haney TL, Williams RB. Unimproved chest pain in patients with minimal or no coronary disease: A behavioral phenomenon. American Heart Journal. 1984;108:67–72. doi: 10.1016/0002-8703(84)90546-5. [DOI] [PubMed] [Google Scholar]