Abstract
Context
A consistent body of evidence supports a role of reduced neurotrophic signaling in the pathophysiology of major depressive disorder (MDD) and suicidal behavior. Especially in suicide victims, lower postmortem brain messenger RNA and protein levels of neurotrophins and their receptors have been reported.
Objective
To determine whether the brain-derived neurotrophic factor (BDNF) gene or its high-affinity receptor gene, receptor tyrosine kinase 2 (NTRK2), confer risk for suicide attempt (SA) and MDD by investigating common genetic variants in these loci.
Design
Eighty-three tagging single-nucleotide polymorphisms (SNPs) covering the genetic variability of these loci in European populations were assessed in a casecontrol association design.
Setting
Inpatients and screened control subjects.
Participants
The discovery sample consisted of 394 depressed patients, of whom 113 had SA, and 366 matched healthy control subjects. The replication studies comprised 744 German patients with MDD and 921 African American nonpsychiatric clinic patients, of whom 152 and 119 were positive for SA, respectively.
Interventions
Blood or saliva samples were collected from each participant for DNA extraction and genotyping.
Main Outcome Measures
Associations of SNPs in BDNF and NTRK2 with SA and MDD.
Results
Independent SNPs within NTRK2 were associated with SA among depressed patients of the discovery sample that could be confirmed in both the German and African American replication samples. Multilocus interaction analysis revealed that single SNP associations within this locus contribute to the risk of SA in a multiplicative and interactive fashion (P = 4.7× 10−7 for a 3-SNP model in the combined German sample). The effect size was 4.5 (95% confidence interval, 2.1–9.8) when patients carrying risk genotypes in all 3 markers were compared with those without any of the 3 risk genotypes.
Conclusions
Our results suggest that a combination of several independent risk alleles within the NTRK2 locus is associated with SA in depressed patients, further supporting a role of neurotrophins in the pathophysiology of suicide.
Suicide represents a major public health problem. Each year, an estimated 10 to 20 million suicides are attempted and 1 million suicides are completed worldwide.1 The overall lifetime prevalence of suicide attempts (SAs) ranges between 3% and 5%, with similar numbers across different populations.2,3 Patients with psychiatric disorders are at higher risk for SA, with patients with mood disorder showing the highest relative risk for lifetime SA (odds ratio [OR]=7.8–29.9), followed by patients with other psychiatric diagnoses (OR=2.1–6.5).3 This increased risk is also reflected by reported estimates for lifetime prevalence of completed suicide being higher in patients with mood disorder than in the general population (2%–4% vs 0.5%, respectively).4 Twin and family studies suggest that suicide and SA are heritable traits5,6 and likely part of the same phenotype, with completed suicide and SA clustering in the same families.7–11 The genetic risk factors for suicide appear to be independent from the underlying psychiatric disorder.7,9,12–14
Regarding the neurobiological foundation of suicidal behavior, a compelling body of evidence points to alterations in the monoamine, neurotrophin, and stress response systems.15–19 Monoaminergic and stress hormone system dysregulations have already received support from human genetic association studies.20 On the other hand, the genetic effect of the neurotrophic system has not yet been extensively investigated, even though a series of postmortem studies now convincingly shows a downregulation of neurotrophic signaling in suicide victims.21–24 The neurotrophin family is composed of nerve growth factor, brain-derived neurotrophic factor (BDNF), neurotrophin 3, neurotrophin 4/5, their high-affinity receptors (receptor tyrosine kinase A [NTRK1], receptor tyrosine kinase B [NTRK2], and receptor tyrosine kinase C [NTRK3]), and the low-affinity nerve growth factor receptor (p75NTR).25 Postmortem brain studies uniformly report reduced BDNF and NTRK2 messenger RNA and protein expression in the prefrontal cortex and hippocampus of suicide victims with depression or other psychiatric disorders relative to nonpsychiatric and nonsuicidal control subjects. Moreover, suicidal subjects showed reduced expression of nerve growth factor, neurotrophin 3, neurotrophin 4/5, NTRK1, and NTRK3 and reduced phosphorylation of all of these receptor tyrosine kinases in the hippocampus.21–24,26 This suggests insufficient neurotrophic signaling and thus synaptic plasticity in suicidal subjects, which is consistent with results of other studies showing altered volumes of the hippocampus and prefrontal cortex27–30 and reduced plasma31 and serum BDNF levels in suicidal subjects.32
Genetic studies investigating the genes encoding the neurotrophic system in suicidal behavior and major depressive disorder (MDD) have mostly focused on a functional BDNF Val66Met (rs6265) polymorphism with inconsistent results33–36 or polymorphisms within the low-affinity receptor gene NGFR37,38 (for review, see the “Comment” section). To our knowledge, there are no published case-control studies in SA or MDD exploring the BDNF gene and the gene encoding its high-affinity receptor, NTRK2, with comprehensive genetic coverage. Here we report the results of a study investigating the association of 83 tagging single-nucleotide polymorphisms (SNPs) for these 2 genes with SA and MDD in a German sample with replication in a larger independent German case-control sample and an African American cohort. To avoid confounding by the underlying psychiatric disease, analyses testing association with SA were performed within the patient group.
METHODS
GERMAN DISCOVERY SAMPLE
A total of 405 inpatients with mood disorder (178 men, 227 women) were recruited for the Munich Antidepressant Response Signature study (http://www.mars-depression.de) of the Max Planck Institute of Psychiatry, Munich, Germany. The study has been described previously in detail.39–41 Briefly, diagnosis was ascertained by trained psychiatrists according to DSM-IV criteria. Patients classified as having an MDD by 2 independent psychiatrists and fulfilling the criteria for at least a moderate depressive episode (score ≥14 on the 21-item Hamilton Scale for Depression) were included. Table 1 and Table 2 show demographic and illness-related data. A lifetime history of SA was ascertained using a semistructured clinical interview established for the Munich Antidepressant Response Signature study39 and scoring points in the Hamilton Scale for Depression rating scale (score on suicide item=4). Information on lifetime history of SA was available in 394 patients (97.3%). As controls, 366 healthy subjects were randomly selected from a Munich-based community sample and matched to patients for age, sex, and ethnicity (Table 1). The healthy control subjects were screened for the absence of any DSM-IV Axis I psychiatric disorder using the face-to-face computer-assisted interview based on the Munich version of the Composite International Diagnostic Interview.42
Table 1.
Demographic Data of 2721 Depressed Patients and Control Subjects of Both German Studiesa
| Discovery Sample (n=771) |
Replication Sample (n=1950) |
Between Samples |
|||||
|---|---|---|---|---|---|---|---|
| Characteristic | Controls (n=366) |
Patients (n=405) |
P Valueb | Controls (n=1029) |
Patients (n=921) |
P Valueb | P Valuec |
| Women, No. (%) | 205 (56.0) | 227 (56.0) | >.99 | 693 (67.3) | 619 (67.2) | .96 | <1.0× 10−4 |
| Age, mean (SD),y | 48.6 (13.4) | 49.0 (14.4) | .67 | 50.7 (13.9) | 51.0 (13.8) | .68 | <1.0× 10−3 |
| Of European descent, % | 100 | 100 | >.99 | 100 | 100 | >.99 | >.99 |
| German origin, No. (%) | 299 (81.7) | 337 (83.2) | .64 | 845 (82.1) | 779 (84.6) | .16 | .45 |
| MDD, No. (%) | 353 (87.2) | 921 (100) | <1.0× 10−4 | ||||
| Recurrent MDD, No. (%) | 225 (55.6) | 921 (100) | <1.0× 10−4 | ||||
| Bipolar disorder, No. (%) | 47 (11.6) | 0 | <1.0× 10−4 | ||||
| Dysthymia, No. (%) | 5 (1.2) | 0 | |||||
| Lifetime history of SA, No. (%) | 113 (28.7) | 152 (20.4) | .002 | ||||
| Illness-related variables for patients with MDD | |||||||
| Age at onset of depression, mean (SD), y | 37.2 (15.7) | 36.0 (13.9) | .145 | ||||
| Previous episodes, mean (SD), No. | 2.8 (5.0) | 5.0 (4.2) | <1.0× 10−4 | ||||
| First-degree family history of MDD, No. (%) | 148 (37.1) | 121 (12.8) | 396 (47.8) | <.001 | <1.0× 10−3 | ||
Abbreviations: MDD, major depressive disorder; SA, suicide attempt.
Healthy control subjects were matched to patients for age, sex, and ethnicity per independent study. Subjects having both parents and grandparents with German mother tongue and nationality were referred to as being of German origin. For patients, depressive diagnosis and illness-related variables are given and compared between the 2 independent samples.
From χ2 test for dichotomous variables and from analysis of variance for quantitative variables with 1 df.
From χ2 test for dichotomous variables and from analysis of variance for quantitative variables with 3 df.
Table 2.
Demographic Characteristics, Depressive Diagnosis, and Illness-Related Variables for 1138 German Patients With Depression and With or Without a Lifetime History of Suicide Attempta
| Discovery Patients With SA Information (n=394) |
Replication Patients With SA Information (n=744) |
Between Samples |
|||||
|---|---|---|---|---|---|---|---|
| Characteristics |
Without SA (n=281) |
With SA (n=113) |
P Valueb | Without SA (n=592) |
With SA (n=152) |
P Valueb | P Value c |
| Women, No. (%) | 143 (50.9) | 77 (68.1) | 2.4 ×10−3 | 692 (66.2) | 106 (69.7) | .44 | <1.0×10−4 |
| Age, mean (SD),y | 49.1 (14.3) | 48.6 (14.5) | .74 | 51.5 (13.5) | 48.2 (13.7) | 7.3 ×10−3 | .008 |
| Of European descent, % | 100 | 100 | >.99 | 100 | 100 | >.99 | >.99 |
| German origin, No. (%) | 235 (83.6) | 92 (81.4) | .66 | 514 (86.8) | 125 (82.2) | .76 | .007 |
| MDD, No. (%) | 247 (87.2) | 78 (85.8) | .74 | 592 (100) | 152 (100) | >.99 | <1.0×10−4 |
| Recurrent MDD, No. (%) | 155 (63.2) | 66 (68.0) | .41 | 592 (100) | 152 (100) | >.99 | <1.0×10−4 |
| Bipolar disorder, No. (%) | 33 (11.7) | 13 (11.7) | .95 | 0 | 0 | >.99 | <1.0×10−4 |
| Age at onset of depression, mean (SD), y | 39.1 (15.5) | 32.3 (14.5) | 7.9 ×10−5 | 37.3 (14.2) | 32.4 (12.7) | 1.1 ×10−4 | <1.0×10−4 |
| Previous episodes, mean (SD), No. | 2.7 (5.3) | 3.3 (4.1) | .35 | 4.8 (3.9) | 5.8 (5.1) | .028 | <1.0×10−4 |
| First-degree family history of MDD, No. (%) | 105 (37.9) | 41 (36.9) | .86 | 251 (46.8) | 62 (48.4) | .74 | .027 |
| 21-Item HAM-D score, mean (SD)d | |||||||
| At admission | 26.4 (6.7) | 26.7 (6.3) | .71 | ||||
| At discharge | 8.9 (5.9) | 9.8 (5.9) | .20 | ||||
| Response, mean (SD), wk | |||||||
| Partiale | 2.9 (2.3) | 3.0 (3.4) | .56 | ||||
| Fullf | 4.7 (3.0) | 4.9 (3.4) | .55 | ||||
| Remissiong | 5.1 (3.1) | 6.0 (3.6) | .06 | ||||
| Different antidepressants in history, mean (SD), No. | 2.4 (1.2) | 2.9 (1.4) | .20 | ||||
| Lifetime history of benzodiazepine abuse, No. (%) | 35 (12.8) | 17 (15.3) | .51 | ||||
| Lifetime history of alcohol abuse, No. (%)h | 36 (13.1) | 26 (23.0) | .02 | 56 (8.7) | 24 (14.5) | .03 | <1.0×10−4 |
| Cigarettes, mean (SD), No./d | 6.8 (10.5) | 8.8 (13.1) | .21 | 8.3 (11.9) | 11.7 (13.0) | .003 | <1.0×10−4 |
Abbreviations: HAM-D, Hamilton Scale for Depression; MDD, major depressive disorder; SA, suicide attempt.
In the discovery sample, there was no difference between patients with and without SA in relation to age; ethnicity; German origin; main psychiatric diagnosis number of previous depressive episodes; first-degree family history of depression; depression severity at admission and discharge; partial response, full response, and remission while receiving antidepressant therapy; number of different antidepressants in lifetime history; lifetime history of benzodiazepine abuse and nicotine consumption. However, SAwas more frequent in women (P=2.4×10−3), and patients with SA had an earlier age at onset of depression (P=7.9×10−5) and more alcohol abuse (P=.02). In the German replication sample, there was no difference between patients with and without SA in relation to sex; ethnicity; German origin; depressive diagnosis; and first-degree family history of depression. Patients with SA were younger than those without SA (P=7.3×10−3) and had an earlier age at onset of depression (P=1.1 × 10−4), a higher number of previous depressive episodes (P=.03), more alcohol abuse (P=.03), and more nicotine consumption (P=.003).
From χ2 test for dichotomous variables and from analysis of variance for quantitative variables with 1 df.
From χ2 test for dichotomous variables and from analysis of variance for quantitative variables with 3 df.
Total score of the index episode.
Stable reduction of 25% in the HAM-D scores over at least 2 weeks of the index episode
Stable reduction of 50% in the HAM-D scores over at least 2 weeks of the index episode
Stable HAM-D score lower than 10 over at least 2 weeks of the index episode.
In the replication sample, the patient was asked whether they had abused alcohol in the 30 days prior to admission to the clinic rather than whether they had a lifetime history of alcohol abuse.
GERMAN REPLICATION SAMPLE
A total of 921 patients (302 men, 619 women) with recurrent major depression were recruited at the Max Planck Institute of Psychiatry and psychiatric hospitals in Augsburg and Ingolstadt (both in Bavaria, Germany). For details on this sample, see the article by Lucae et al.43 Patients were diagnosed by World Health Organization–certified raters according to DSM-IV criteria using the World Health Organization Schedules for Clinical Assessment in Neuropsychiatry, version 2.1. Patients of European descent with at least 2 moderately severe depressive episodes were included. A lifetime history of SA was ascertained using the same semistructured clinical interview established for the Munich Antidepressant Response Signature study.39 Information on lifetime history of SA was available for 744 patients (80.8%). A total of 1029 healthy control subjects matched to the patient sample for age, sex, and ethnicity were randomly selected from a Munich-based community sample. They were free of lifetime anxiety and mood disorders according to the Munich version of the Composite International Diagnostic Interview.42
Both studies have been approved by the ethics committee of Ludwig-Maximilians University of Munich, and written informed consent was obtained from all subjects.
AFRICAN AMERICAN REPLICATION SAMPLE
From a cross-sectional study of nonpsychiatric clinic patients with significant levels of trauma, 921 African American patients (390 men, 531 women) with information on lifetime history of SA were selected (119 with SA and 802 without SA). Study design, ascertainment, and rating protocols have been described elsewhere in more detail.44 The patients’ mean (SD) age was 40.8 (14.1) years (men, 44.3 [12.7] years; women, 38.3 [14.5] years). Participants were seeking general medical or obstetric/gynecological care at an urban public hospital in Atlanta, Georgia. The Structured Clinical Interview for DSM-IV Axis I Disorders (nonpatient edition)45 was performed for 335 of these probands, of whom 80 fulfilled criteria for a lifetime history of MDD (32 with SA and 48 without SA; 32 men and 48 women; mean [SD] age for all 80 subjects, 45.5 [10.5] years; mean [SD] age for men, 49.3 [8.0] years; mean [SD] age for women, 42.9 [11.3] years). All procedures in this study were approved by the institutional review boards of Emory University School of Medicine and Grady Memorial Hospital.
DNA PREPARATION
On enrollment in the study, up to 40 mL of blood was drawn from each patient into anticoagulant EDTA tubes. The DNA was extracted from fresh blood using standard DNA extraction procedures with the Puregene whole-blood DNA extraction kit (Gentra Systems Inc, Minneapolis, Minnesota).
SNP SELECTION AND GENOTYPING
An SNP marker panel was used to tag the full-length NTRK2 (RefSeq NM_006180,355.04 kilobases [kb]) and the longest BDNF isoform (RefSeq NM_170731,66.86 kb) comprising 20 kb of flanking sequences according to Human HapMap Project phase I and II data for the central European population.46 The tagger software integrated in the HapMap project home page47 was used for tagging SNP selection. Pairwise r2 was set to ≥0.8 with a minor allele frequency (MAF) cutoff of ≥0.1 for NTRK2 and ≥0.01 for BDNF. The suggested number of tagging SNPs was 69 for NTRK2 and 18 for BDNF (total of 87 tagging SNPs). The SNPs were genotyped on a matrix-assisted laser desorption/ionization-time of flight mass spectrometer (MassARRAY system; Sequenom, Inc, San Diego, California) using the Assay Designer software (Sequenom, Inc) for primer selection, multiplexing, and assay design and using the homogeneous mass extension process for producing primer extension products. Matrix-assisted laser desorption/ ionization-time of flight SNP genotyping was performed at the facilities of the Helmholtz Zentrum Munich.
POWER CALCULATION
For power calculations, the Genetic Power Calculator was used48 (http://pngu.mgh.harvard.edu/~purcell/gpc). Given a unipolar depression prevalence of 16%,49 a common marker in perfect linkage disequilibrium (LD) (r2= 1) with the causative variation under an allelic, dominant, or recessive model, and 80% statistical power, we were able to detect an effect size of 1.7 or higher in our discovery sample (α = .05 divided by 83 SNPs equals 6.02 × 10−4). The prevalence of a lifetime history of SA among depressed patients was estimated to be 23% from our combined German samples, which is consistent with the reported prevalence.3 Under the earlier-mentioned settings, we had 80% statistical power to detect effect sizes of 2.1 or higher on SA among patients with depression in our discovery sample.
ASSOCIATION TESTING
Case-control association screening in the discovery sample was conducted using WG-Permer software (http://www.mpipsykl.mpg.de/wg-permer/). The SNPs were tested for association with MDD in a case-control design using 2-tailed χ2 test statistics under allelic, recessive, and dominant modes of inheritance. Genetic associations with lifetime history of SA among depressed patients were tested by 2-tailed analysis of variance with residual variables that were generated by logistic regression analysis correcting for age and sex. For this analysis, patients with and without history of SA were compared to avoid confounding by the underlying psychiatric disease. Obtained association P values were verified by calculating permutation-based empirical P values under 105 permutations (WG-Permer software) and by logistic regression analysis including sex and age as covariates using SPSS statistical software version 16 for Windows (SPSS Inc, Chicago, Illinois). Empirical P values and P values from logistic regression analysis with covariates did not differ from those of the residual analysis of variance test statistics of the screening analysis. The level of significancewassetto .05 for P values corrected for multiple comparisons by the permutation-based minimum P method50,51 under 105 permutations over all performed tests (3 genetic models, 83 SNPs) per phenotype (MDD, SA). In addition, the permutation-based Fisher product method (FPM)52 was performed, which allows association testing over all tested markers of a candidate gene with the phenotype of interest. The FPM was exerted under 105 permutations over all tested SNPs and genetic models for both phenotypes (MDD, SA) and genes (BDNF, NTRK2). The 4 resulting FPM P values were Bonferroni corrected for multiple comparisons (α = .05 divided by 4 equals .0125). The same statistical procedures were applied for association testing in the German replication sample but under the SNP-wise best genetic model and with the same risk allele/ genotype as observed in the discovery sample, which allowed 1-sided testing. In a second replication sample (African American probands), an allelic model with the same risk allele as determined in the German samples was tested (1-sided). Multilocus interaction testing on SA among depressed patients of the combined German sample was performed using stepwise logistic regression analysis conducted in R statistical software version 2.5.0 (http://cran.r-project.org). We included the 3 most significant SNPs (under their best genetic models), their pairwise interaction term, age, and sex in the model. Meta-analyses were computed by applying Comprehensive Meta-analysis statistical software version 2 (Biostat, Englewood, New Jersey).
LINKAGE DISEQUILIBRIUM
The LD pattern and haplotype block delineation were determined using Haploview software version 4.0 (http://www.broad.mit.edu/mpg/haploview) in control subjects of the discovery sample.53 Blocks were defined using the method described by Gabriel et al.54
RESULTS
QUALITY CONTROL AND SNP MARKER COVERAGE
In the discovery sample, a total of 87 tagging SNPs covering NTRK2 and BDNF were genotyped. Data of 4 single r2-bin SNPs of NTRK2 were excluded from association testing because of insufficient call rates. The remaining 83 SNPs were included in association analysis. Their mean (SD) call rate was 99.7% (0.82%), and no SNP displayed deviation from Hardy-Weinberg equilibrium after Bonferroni correction for multiple testing (eTable 1 and eTable 2; http://www.archgenpsychiatry.com). Overall, we obtained a 100% SNP marker coverage of BDNF with 20 kb of flanking sequences according to HapMap phase I and II data (central European population, r2≥0.8, MAF≥0.01). For NTRK2, SNP marker coverage was 94.2% (central European population, r2≥ 0.8, MAF ≥ 0.1).
CASE-CONTROL ASSOCIATION WITH MDD IN THE DISCOVERY SAMPLE
We did not detect any case-control association with MDD in NTRK2 or in BDNF, which withstood correction for multiple comparison. The smallest P value (nominal P = 9.3×10−3, corrected P =.38) was obtained for rs9969765, an SNP located in the NTRK2 gene. There were 7 SNPs in NTRK2 and 4 SNPs in BDNF, which showed nominal P values less than .05 (eTable 1 and eTable 2). For instance, the often reported functional BDNF polymorphism (rs6265) showed nominal significant association with MDD (P = .035). Neither NTRK2 or BDNF were associated with MDD by applying the FPM overall-tested variants within a gene.
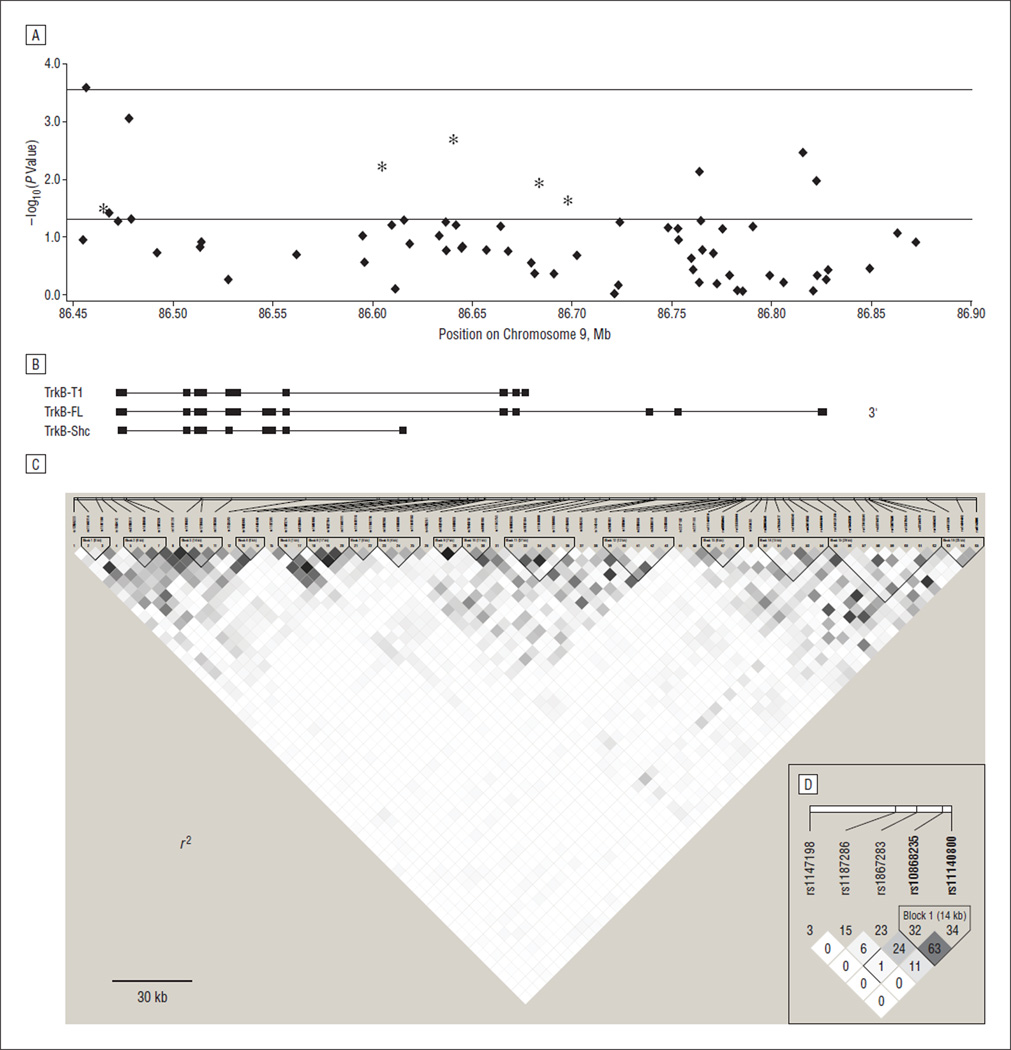
ASSOCIATIONS WITH SA AMONG DEPRESSED PATIENTS IN THE DISCOVERY SAMPLE
There was 1 SNP in the promoter region of NTRK2 that was associated with SA among depressed patients after correction for multiple comparison over all tested SNPs and genetic models (rs11140714: nominal P = 2.6 × 10−4, corrected P = .043). A total of 12 SNPs located in NTRK2 were associated with SA on a nominal significance level of .05 (Figure 1 and eTable 2), whereas in BDNF there were none (eTable 1). The FPM suggested association of NTRK2 with SA among depressed patients over all tested SNPs and models with P = 4.1 × 10−3. After correction for all 4 FPM tests performed in this study (2 phenotypes × 2 genes), NTRK2 was still significantly associated with SA among depressed patients (Bonferronicorrected P =.016). In contrast to NTRK2, BDNF was not significantly associated with SA by the FPM.
Figure 1.
Association results of NTRK2 with suicide attempt among depressed patients. A, The negative common logarithm of the best genetic model P value of the 65 tagging single-nucleotide polymorphisms (SNPs) obtained in the discovery sample was plotted against the SNP’s chromosome position throughout the NTRK2 locus on chromosome 9q22. The lower horizontal line indicates the nominal significance level of .05; the upper horizontal line, the significance level after correction for multiple comparisons over all tested SNPs and genetic models; asterisks, the 5 SNPs for which association with suicide attempt could be replicated in a larger independent German sample; and Mb, megabases. B, The 5’ to 3’ structures of the most prominent isoforms of NTRK2are depicted and aligned with part A. The boxes and lines show the exon-intron structure of NTRK2. TrkB indicates receptor tyrosine kinase B. C, The r2-based linkage disequilibrium structure overall genotyped tagging SNPs in control subjects of the discovery sample is shown. The genetic information content of NTRK2 spanning across 355 kilobases (kb) can be clustered into 16 D’-based haplotype blocks. D, The linkage disequilibrium (r2) between the 5 SNPs associated with suicide attempt among depressed patients in both German samples is displayed.
REPLICATION OF ASSOCIATIONS WITH SA IN AN INDEPENDENT GERMAN PATIENT SAMPLE
To follow-up the association between NTRK2 and SA among depressed patients in the discovery sample, we selected the 12 nominally significant NTRK2 SNPs to be genotyped in the independent German replication sample (eTable 3). We performed the FPM on SA with the best genetic model and the same risk allele/genotype per SNP as have been observed in the discovery sample. The FPM P value was significant in the replication sample (P=3.3 × 10−3), indicating real association of SNPs with SA among depressed patients. Five single SNP associations (rs10868235, rs1147198, rs1867283, rs1187286, and rs11140800) among the 12 tested SNPs showed nominal significance with the same risk allele/genotype and genetic model as in the discovery sample (Table 3). This number of nominally replicated single SNP associations is about 16.7 times higher than would be expected by chance.
Table 3.
Results for the Single-Nucleotide Polymorphisms Showing the Strongest Association With Lifetime History of Suicide Attempt Among Depressed German Patients and Healthy Control Subjectsa
| German Discovery Patients |
German Replication Patients |
Combined German Sample |
||||
|---|---|---|---|---|---|---|
| SNP | Without SA | With SA | Without SA | With SA | Without SA vs With SA |
Healthy Controls vs Patients With SAb |
| rs10868235 | ||||||
| All genotypes, No. | 281 | 113 | 589 | 150 | 1133 | 1648 |
| CC, No. (%) | 51 (18.1) | 33 (29.2) | 125 (21.2) | 45 (30.0) | 254 (22.4) | 386 (23.4) |
| CT, No. (%) | 143 (50.9) | 52 (46.0) | 311 (52.8) | 74 (49.3) | 580 (51.2) | 826 (50.1) |
| TT, No. (%) | 87 (31.0) | 28 (24.8) | 153 (26.0) | 31 (20.7) | 299 (26.4) | 436 (26.5) |
| HWE P value | .56 | .41 | .17 | .95 | .25 | .89 |
| Allelic P value | .020 | .011 | 1.3 × 10−3 | 4.4 × 10−3 | ||
| Allelic OR (lower 95% confidence limit) | 1.41 (1.04) | 1.33 (1.07) | 1.34 (1.10) | 1.28 (1.12) | ||
| T-carrier P valuec | .012 | 8.6 ×10−3 | ×10−4 | 4.3 ×10−3 | ||
| T-carrier OR (lower 95% confidence limit) | 1.86 (1.12) | 1.59 (1.14) | 1.66 (1.22) | 1.47 (1.20) | ||
| rs1867283 | ||||||
| All genotypes, No. | 281 | 113 | 583 | 149 | 1126 | 1638 |
| GG, No. (%) | 63 (22.4) | 38 (33.6) | 132 (22.6) | 45 (30.2) | 278 (24.7) | 435 (26.6) |
| AG, No. (%) | 141 (50.2) | 59 (52.2) | 304 (52.1) | 71 (47.7) | 575 (51.1) | 834 (50.9) |
| AA, No. (%) | 77 (27.4) | 16 (14.2) | 147 (25.2) | 33 (22.1) | 273 (24.2) | 369 (22.5) |
| HWE P value | .92 | .34 | .29 | .62 | .51 | .42 |
| Allelic P value | .002 | .041 | 1.2×10−3 | .014 | ||
| Allelic OR (lower 95% confidence limit) | 1.64 (1.20) | 1.24 (1.00) | 1.39 (1.14) | 1.24 (1.06) | ||
| A-carrier P valued | .034 | .013 | 3.5 ×10−3 | .023 | ||
| A-carrier OR (lower 95% confidence limit) | 1.75 (1.08) | 1.48 (1.06) | 1.59 (1.17) | 1.35 (1.03) | ||
| rs1147198 | ||||||
| All genotypes, No. | 281 | 113 | 581 | 149 | 1124 | 1639 |
| CC, No. (%) | 10 (3.6) | 10 (8.8) | 26 (4.5) | 14 (9.4) | 60 (5.3) | 104 (6.3) |
| AC, No. (%) | 101 (35.9) | 34 (30.1) | 208 (35.8) | 44 (29.5) | 387 (34.4) | 546 (33.3) |
| AA, No. (%) | 170 (60.5) | 69 (61.1) | 347 (59.7) | 91 (61.1) | 677 (60.2) | 989 (60.3) |
| HWE P value | .29 | .08 | .47 | .02 | .62 | .02 |
| Allelic P value | .500 | .284 | .392 | .287 | ||
| Allelic OR (lower 95% confidence limit) | 1.14 (0.79) | 1.11 (0.86) | 1.12 (0.89) | 1.07 (0.93) | ||
| A-carrier P valued | .032 | .016 | 2.1 ×10−3 | .025 | ||
| A-carrier OR (lower 95% confidence limit) | 2.63 (1.06) | 2.21 (1.25) | 2.31 (1.35) | 1.63 (1.05) | ||
| rs11140800 | ||||||
| All genotypes, No. | 280 | 113 | 581 | 149 | 1123 | 1638 |
| CC, No. (%) | 39 (13.9) | 22 (19.5) | 79 (13.6) | 34 (22.8) | 174 (15.5) | 290 (17.7) |
| AC, No. (%) | 140 (50.0) | 63 (55.8) | 304 (52.3) | 65 (43.6) | 572 (50.9) | 772 (47.1) |
| AA, No. (%) | 101 (36.1) | 28 (24.8) | 198 (34.1) | 50 (33.6) | 377 (33.6) | 576 (35.2) |
| HWE P value | .39 | .21 | .03 | .15 | .52 | .89 |
| Allelic P value | .023 | .039 | 5.9 ×10−3 | .015 | ||
| Allelic OR (lower 95% confidence limit) | 1.41 (1.03) | 1.22 (1.00) | 1.30 (1.06) | 1.25 (1.06) | ||
| A-carrier P valued | .168 | 1.6 ×10−3 | 1.5×10−3 | .045 | ||
| A-carrier OR (lower 95% confidence limit) | 1.49 (0.84) | 1.88 (1.29) | 1.71 (1.20) | 1.33 (1.01) | ||
| rs1187286 | ||||||
| All genotypes, No. | 281 | 113 | 589 | 151 | 1134 | 1652 |
| CC, No. (%) | 12 (4.3) | 13 (11.5) | 27 (4.6) | 10 (6.6) | 62 (5.5) | 102 (6.2) |
| AC, No. (%) | 98 (34.9) | 38 (33.6) | 191 (32.4) | 58 (38.4) | 385 (34.0) | 607 (36.7) |
| AA, No. (%) | 171 (60.9) | 62 (54.9) | 371 (63.0) | 83 (55.0) | 687 (60.6) | 943 (57.1) |
| HWE P value | .66 | .07 | .70 | .98 | .87 | .87 |
| Allelic P value | .039 | .035 | 6.5 ×10−3 | .085 | ||
| Allelic OR (lower 95% confidence limit) | 1.42 (1.00) | 1.33 (1.04) | 1.38 (1.10) | 1.16 (0.97) | ||
| A-carrier P valued | 5.9 ×10−3 | .167 | .012 | .033 | ||
| A-carrier OR (lower 95% confidence limit) | 2.91 (1.29) | 1.48 (0.79) | 2.03 (1.19) | 1.58 (1.05) | ||
Abbreviations: HWE, Hardy-Weinberg equilibrium; OR, odds ratio; SA, suicide attempt; SNP, single-nucleotide polymorphism.
All 5 SNPs are located in the NTRK2gene (Figure 1). Genotype distributions, HWE, and association P values of the best genetic and allelic model and ORs are given, tested separately in both independent German patient samples and the combined patient sample.
The P values are shown from post hoc testing between depressed patients with SA vs healthy control subjects in the combined German sample
T-carrier indicates BB vs TT + TB.
A-carrier indicates BB vs AA + AB
When depressed patients with SA from both studies were tested vs healthy control subjects for the 5 associated SNPs mentioned earlier, significant associations were again observed but with effect sizes smaller than when compared with depressed patients with no SA (Table 3). These 5 SNPs did not show case-control association with MDD in the combined sample, indicating a specific genetic effect on SA. Of the replicated SNPs, only rs2277193 became nominally significantly associated with MDD in the combined sample (n = 1250/1375, allelic P =.033), but this association did not withstand correction for multiple testing.
CORRECTING FOR POTENTIALLY CONFOUNDING CLINICAL VARIABLES FOR GENETIC ASSOCIATIONS WITH SA
Age at onset of depressive disorder was 5.6 years lower in those with SA compared with those without SA in the combined German sample (P = 5.1 × 10−8) (Table 2). This result is consistent with a previous study.55 In addition, a higher number of previous depressive episodes in patients with a lifetime history of SA compared with patients without SA has been reported.55 In our samples, we observed the same direction of this effect, approaching significance in the combined sample (P = .061) (Table 2). We thus controlled for the age at onset of depressive disorder and the number of previous depressive episodes for the described genetic associations with SA among depressed patients, in addition to age and sex, in post hoc logistic regression analysis. In these models, all 5 SNPs remained significant predictors for SA, with sex and age at onset as significant covariates. We repeated these analyses with other potentially confounding variables showing at least trend significance between SA-positive and SA-negative patients in at least 1 sample (alcohol and nicotine consumption, remission) (Table 2). Only alcohol consumption became another significant covariate, but neither alcohol consumption nor nicotine consumption affected the reported genetic associations with SA.
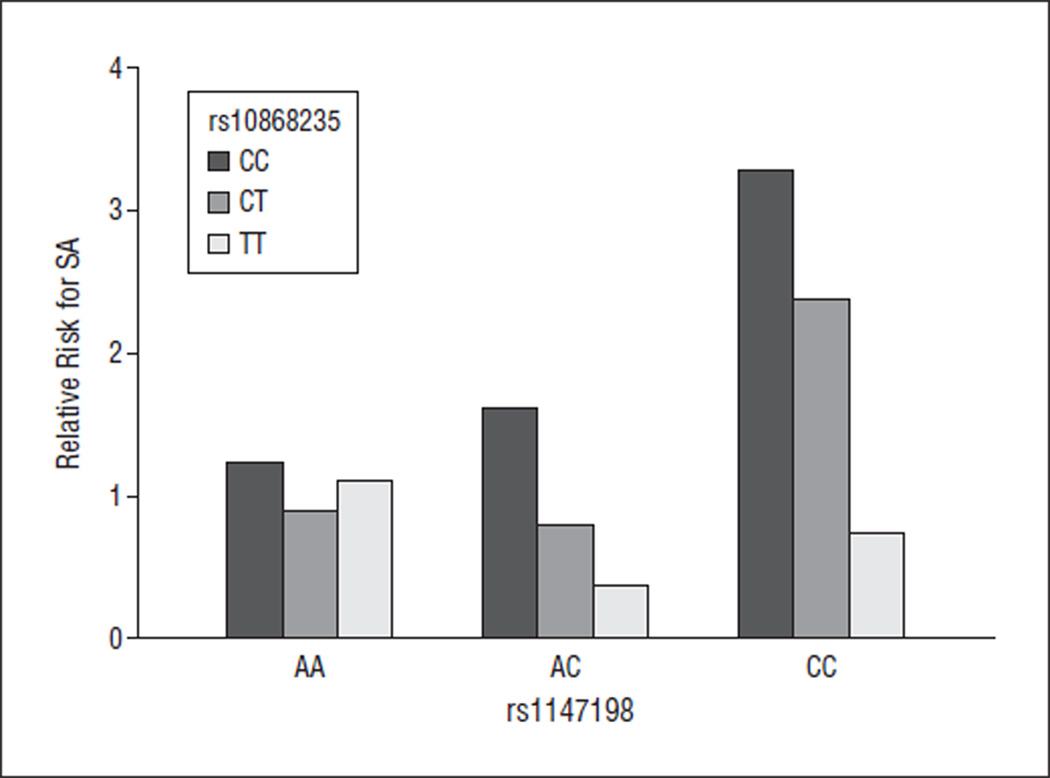
MULTILOCUS MODEL AND GENE-GENE INTERACTION ANALYSIS IN THE COMBINED GERMAN SAMPLE
The LD structure of tested NTRK2 SNPs is shown in Figure 1C and D. By definition, tagging SNPs are not in high LD with each other. Among the 5 SNPs associated with SA, rs10868235 and rs11140800 correlated most (r2 = 0.63; D′ = 0.94), while rs1147198 was not correlated with any of the other 4 associated SNPs. Its pairwise r2 value with each other SNP was below 0.01 (D′max= 0.14 with rs1867283). rs1147198 maps 8 kb 5′ of the transcription start site into the putative promoter region of NTRK2. The other 4 SNPs are located in introns 14 and 16 of full-length NTRK2 (Figure 1A and B). Because 4 of the 5 associated SNPs show low or no LD among each other, they might reflect more than 1 causal variant of the NTRK2 gene conferring risk for SA. Therefore, we performed multilocus regression analysis allowing 2-way and 3-way interactions between the 3 associated SNPs (rs10868235, rs1147198, and rs1867283) with the lowest P values in the combined sample. The model showed a multiplicative effect of the combined SNPs on SA and became highly significant (P = 4.7 × 10−7). Main effects for each single SNP, age, sex, and the interaction between rs10868235 and rs1147198 were significant predictors (P <.05). Figure 2 illustrates the interaction between genotypes of rs10868235I and rs1147198II. The OR of the association with SA was 3.3 (95% confidence interval [CI], 1.7–6.1; P = 1.5 × 10−4) when patients carrying risk genotypes in both interacting loci (CCI or CTI+ CCII) were com- pared with patients without risk genotypes (TTI + AAII or ACII). In analogy, the effect size became even larger when risk genotype carriers in all 3 markers (rs10868235I, rs1147198II, and rs1867283III: CCI or CTI+CCII + AGIII or GGIII) were compared with those without any risk genotype in any marker (TTI+ CCII or ACII + AAIII) (OR = 4.5; 95% CI, 2.1–9.8; P = 5.1 ×10−5).
Figure 2.
Multilocus regression analysis revealed a single-nucleotide polymorphism (SNP)–SNP interaction in suicide attempt (SA). Only the 3 SNPs most strongly associated with SA among depressed patients in the combined sample were included in multilocus modeling to conserve power. In addition to the SNPs’ main effects on risk for SA (Table 3), the ndependent SNPs (Figure 1D) rs10868235 and rs1147198 also showed an nteraction effect on SA. The relative risk for SA is plotted against all genotype combinations of the 2 markers.
SECOND REPLICATION ATTEMPT IN AN AFRICAN AMERICAN SAMPLE
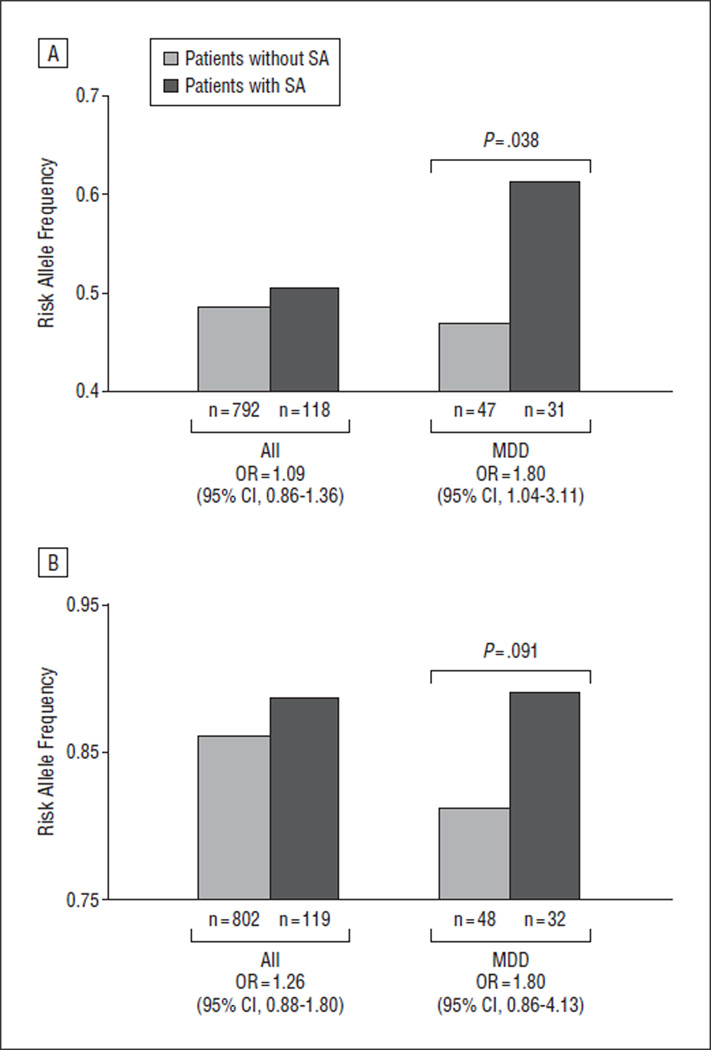
The 3 SNPs (rs10868235, rs1147198, and rs1867283) showing the most robust associations with SA in both German samples were genotyped in African American, nonpsychiatric clinic patients from a cross-sectional study. rs10868235 was excluded from association analysis owing to an insufficient genotyping call rate. Both other SNPs did not show allelic association with a lifetime history of SA in the complete sample (802 subjects without SA vs 119 with SA; P >.05) (Figure 3). However, in the subgroup of probands with a lifetime diagnosis of MDD as ascertained by the Structured Clinical Interview for DSM-IV, the rs1147198 risk allele (C) for SA was significantly more common in the SA-positive MDD group than in the SA-negative MDD group (n = 78; P = .038; OR=1.80; 95% CI, 1.04–3.11) (Figure 3). Thus, the association is in the same direction as for the German samples. The rs1867283 risk allele (G) for SA was also more frequent in the SA-positive African American MDD group compared with the SA-negative African American MDD group, with trend significance (n = 80; P=.091; OR=1.88; 95% CI, 0.86–4.13) (Figure 3).
Figure 3.
Replication of suicide attempt (SA) association in an African American cross-sectional study of nonpsychiatric clinic patients. The 2 tested single-nucleotide polymorphisms, rs1147198 (A) and rs1867283 (B), showed no association with SA in the complete sample (all) but did show association with SA among the subgroup of subjects with an ascertained lifetime diagnosis of major depressive disorder (MDD) for rs1147198 (A) and with trend significance also for rs1867283 (B). The risk alleles were the same as in the German samples (eTable 3). OR indicates odds ratio; CI, confidence interval.
Meta-analyses of these associations with SA among depressed patients in the German and African American samples gave best-model P = 4 × 10−3 for rs1147198 (CC vs AC + AA) and P =5 × 10−4 for rs1867283 (G vs A).
COMMENT
In this study, we show association of 5 tagging SNPs (Table 3) located within the NTRK2 locus with a lifetime history of SA within depressed patients in 2 independent German samples. This association appears to be carried by several independent risk loci within this gene, and carriers of the risk genotypes of the 3 most significant markers had a 4.5-fold higher risk for SA than depressed patients carrying the nonrisk genotypes. Moreover, we report supportive evidence for these associations in African American patients with MDD. In contrast, no polymorphisms within BDNF were found to be associated with SA. Case-control associations with MDD did not withstand correction for multiple testing in either of the genes. Our results thus support the large body of evidence implicating the neurotrophic system in the pathophysiology of suicide.
The facts that the genetic associations with SA were stronger when comparing depressed patients with SA vs depressed patients without SA than with healthy control subjects and that these SNPs were not associated with MDD suggest that these associations are specific to SA. Moreover, the discovery sample consisted of patients with dif- ferent mood disorders, whereas the German replication patient sample comprised only patients with recurrent unipolar depression (Table 2). The associations with SA showed very similar effect sizes in these 2 diagnostically different samples and were unaffected by introducing type of mood disorder as a covariate, which further points toward a specificity of these genetic associations to SA.
We could replicate previous studies showing an earlier age at onset of depression and a higher number of previous depressive episodes in those with SA who have mood disorders.55 However, covarying for these variables did not change the strength of the genetic association, suggesting that they did not confound our analysis. Our results are thus in concordance with the hypothesis that psychiatric disease, social risk factors, and other environmental risk factors are additive or interactive factors with genetic susceptibility specific to suicidal behavior (for review, see the articles by Zubenko et al56 and Mann57). While we have sufficient statistical power (74%–99%) to detect each of the 5 described associations with SA among depressed patients in our combined German sample, independent positive replications are needed to further validate these results and answer the question of whether these associations are specific to SA within patients with mood disorder or are also seen in other psychiatric disorders.
Besides testing for association with SA, we also tested association with MDD with our complete marker panel in the discovery sample. We analyzed 353 patients with unipolar depression and 366 nonpsychiatric control subjects. Neither BDNF nor NTRK2 were associated over all tested markers, and no single SNP association withstood correction for multiple testing. While large effects of polymorphisms in these genes are not likely, our study lacked power to detect effects of smaller magnitude (OR < 1.6) as are often reported for complex disease.33,58,59
In contrast to our study, most reported studies have only typed the functional Val66Met polymorphism (rs6265) within the BDNF locus. Interestingly, this polymorphism showed nominal significant association with MDD but not with SA (eTable 1 and eTable 2) in our discovery sample. No association with this variant was seen in our larger German replication sample. Conflicting association results with this SNP and MDD have been reported by several groups. One study35 in Mexican American patients reported a positive association and 4 other studies34,60–62 failed to show significant single-marker case-control association with this or any other BDNF polymorphism. Nevertheless, Schumacher et al33 showed significant association of a 3-marker haplotype (rs988748-(GT)n-rs6265) that withstood correction for multiple testing in the original German sample and replication in our independent German sample, and Kaufman et al59 reported a significant 3-way interaction between the BDNF Val66Met and serotonin transporter length (5-HTTLPR) polymorphisms and maltreatment history in children with MDD. However, our overall negative results for markers in BDNF and NTRK2 associated with MDD are concordant with results from a large genome-wide case-control association study on MDD (Genetic Association Information Network study),63 where no SNP within BDNF and NTRK2 reached a nominal association P value below .01. Our negative association results with polymorphisms in BDNF and NTRK2 and MDD are thus congruent with most published studies, including recent genome-wide association studies.
Population stratification is a concern in genetic association studies.64 We recorded ethnicity of parents and all 4 grandparents of each proband. Affiliation with an ethnicity other than one of European descent in 1 or more relatives led to the exclusion of a proband from statistical analysis in this study. The proportion of depressed patients with SA having all 4 grandparents of German origin over both studies was 89.6%, which was not different from the proportion in depressed patients without SA (90.2%) (Table 2). We repeated our analysis for the 5 associated SNPs after exclusion of all probands with 1 or more grandparent with a nationality other than German. We could not detect any significant change in the strength of association with SA among depressed patients in this restricted analysis. Furthermore, previously reported data indicate little if any detectable population stratification within individuals of German ethnicity.64 Both German samples explored in this study were recruited in Bavaria, thus exclusively in southern Germany, and therefore it is not likely that our results are substantially biased by population stratification. The fact that similar associations are also seen in an African American sample may point to the fact that these variants are close to functional polymorphisms relevant for several different populations.
In our study, we achieved an almost complete tagging SNP coverage according to HapMap phase I and II data over both genes under investigation. This allowed us to identify several independent common markers associated with SA among depressed patients in NTRK2. Multilocus interaction analysis in the combined German patient sample revealed that the 3 most significant SNPs (Table 3) contribute to the risk for SA in a multiplicative fashion. The model showed P = 4.7 × 10−7 with a significant interaction between 2 of these SNPs (Figure 2). When patients carrying risk genotypes in all 3 markers were compared with those without any risk genotype in any marker, the effect size was 4.5 (95% CI, 2.1–9.8). Four of the 5 SNPs found to be associated with SA were in low LD (Figure 1D). Our results thus suggest that a combination of several independent risk alleles within the NTRK2 locus is associated with SA in depressed patients. While the BDNF locus was tagged down to an MAF of 1%, our study was not powered to detect associations with variants below an MAF of 10%; therefore, we cannot exclude associations with the tested rare variants in this gene.
Besides the herein reported association of polymorphisms with NTRK2 and SA among depressed patients, most recent large meta-analyses support the association of monoaminergic genes with suicidal behavior, including polymorphisms in the tryptophan hydroxylase (TPH), serotonin transporter (SLC6A4),65–67 and catechol O-methyltransferase (COMT) genes.68 Several single studies report association of corticotrophin-releasing hormone system–related genes (CRH, CRHR1, CRHR2, and CRHBP) and the angiotensin-converting enzyme (ACE) gene, all genes related to the stress hormone system, with suicidal behavior among psychiatric patients or compared with control subjects.69–72 Animal models suggest that the monoaminergic genes and stress hormone system closely interact with the neurotrophic system. In fact, neurotrophic signaling is decreased following chronic stress, which can be prevented by selective serotonin reuptakeinhibiting antidepressants.73–75 Individuals with a genetic liability for dysfunctional NTRK2 signaling might more easily pass the threshold for insufficient neurotrophic signaling in the additional presence of a current mood disorder. This could lead to an enhanced impairment of neuronal survival and synaptic plasticity and might be related to the development of suicidal behavior in patients with MDD. In addition, neurobiological factors related to impulsive and aggressive behavior have been shown to be of importance in the development of suicidal behavior.20,76–78 The combined presence of risk polymorphisms in these pathways and environmental factors might be necessary to trigger an SA. Unfortunately, the sample size of our study does not allow for such analysis.
In summary, this study shows association of several independent common variants of NTRK2 with SA among depressed patients in independent samples. This supports the large body of evidence that dysfunctional neurotrophic signaling might be involved in the pathophysiology of suicidal behavior.
Acknowledgments
Financial Disclosure: Within the last 3 years, Dr Ressler has received research funding support from the National Institute of Mental Health, the National Institute on Drug Abuse, Lundbeck, the Burroughs Wellcome Foundation, and the National Alliance for Research on Schizophrenia and Depression, and he has an unrelated consulting agreement with Tikvah Therapeutics for N-methyl-D-aspartate–based therapeutics. Dr Holsboer has received grant support from Bristol-Myers Squibb, is a founder and shareholder of Affectis Pharmaceuticals, and is a shareholder of Corcept Therapeutics and Neurocrine Biosciences. Dr Binder currently receives grant support from the National Institute of Mental Health and the Doris Duke Charitable Foundation and in the past 2 years has received grant support from Pfizer Pharmaceuticals. Drs Menke, Holsboer, and Binder are inventors of “Means and Methods for Diagnosing Predisposition for Treatment Emergent Suicidal Ideation (TESI),” European patent application 08016477.5; Drs Holsboer and Binder are inventors of “FKBP5: A Novel Target for Antidepressant Therapy,” international patent publication WO 2005/054500; and Drs Holsboer and Binder are inventors of “Polymorphisms in ABCB1 Associated With a Lack of Clinical Response to Medicaments,” international patent application PCT/EP2005/005194.
Funding/Support: The study is supported by a grant from the Exzellenz-Stiftung of the Max Planck Society and by grant FKZ 01GS0481 from the National Genome Research Network, Federal Ministry of Education and Research.
Footnotes
Previous Presentation: This work was presented in part as a poster at the XXIV CINP Congress; July 14, 2008; Munich, Germany.
Online-Only Material: The eTables are available at http://www.archgenpsychiatry.com.
Additional Contributions: Sabine Damast, Maik Koedel, Susann Sauer, and Alina Tontsch provided technical assistance and Benno Pütz, PhD, Hildegard Pfister, MS, and Macus Ising, PhD, provided database management.
REFERENCES
- 1.World Health Organization. [Accessed November 18];Suicide prevention (SUPRE) http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/index.html.
- 2.Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Joyce PR, Karam EG, Lee CK, Lellouch J, Lepine JP, Newman SC, Rubio-Stipec M, Wells JE, Wickramaratne PJ, Wittchen HU, Yeh EK. Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med. 1999;29(1):9–17. doi: 10.1017/s0033291798007867. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 4.Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. Am J Psychiatry. 2000;157(12):1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- 5.Statham DJ, Heath AC, Madden PAF, Bucholz KK, Bierut L, Dinwiddie SH, Slutske WS, Dunne MP, Martin NG. Suicidal behaviour: an epidemiological and genetic study. Psychol Med. 1998;28(4):839–855. doi: 10.1017/s0033291798006916. [DOI] [PubMed] [Google Scholar]
- 6.Wender PH, Kety SS, Rosenthal D, Schulsinger F, Ortmann J, Lunde I. Psychiatric disorders in the biological and adoptive families of adopted individuals with affective disorders. Arch Gen Psychiatry. 1986;43(10):923–929. doi: 10.1001/archpsyc.1986.01800100013003. [DOI] [PubMed] [Google Scholar]
- 7.Brent DA, Bridge J, Johnson BA, Connolly J. Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry. 1996;53(12):1145–1152. doi: 10.1001/archpsyc.1996.01830120085015. [DOI] [PubMed] [Google Scholar]
- 8.Brent DA, Mann JJ. Family genetic studies, suicide, and suicidal behavior. Am J Med Genet C Semin Med Genet. 2005;133C(1):13–24. doi: 10.1002/ajmg.c.30042. [DOI] [PubMed] [Google Scholar]
- 9.Cheng AT, Chen TH, Chen CC, Jenkins R. Psychosocial and psychiatric risk factors for suicide: case-control psychological autopsy study. Br J Psychiatry. 2000;177:360–365. doi: 10.1192/bjp.177.4.360. [DOI] [PubMed] [Google Scholar]
- 10.Roy A. Genetic and biologic risk factors for suicide in depressive disorders. Psychiatr Q. 1993;64(4):345–358. doi: 10.1007/BF01064927. [DOI] [PubMed] [Google Scholar]
- 11.Roy A. Relation of family history of suicide to suicide attempts in alcoholics. Am J Psychiatry. 2000;157(12):2050–2051. doi: 10.1176/appi.ajp.157.12.2050. [DOI] [PubMed] [Google Scholar]
- 12.Fu Q, Heath AC, Bucholz KK, Nelson EC, Glowinski AL, Goldberg J, Lyons MJ, Tsuang MT, Jacob T, True MR, Eisen SA. A twin study of genetic and environmental influences on suicidality in men. Psychol Med. 2002;32(1):11–24. doi: 10.1017/s0033291701004846. [DOI] [PubMed] [Google Scholar]
- 13.Glowinski AL, Bucholz KK, Nelson EC, Fu Q, Madden PAF, Reich W, Heath AC. Suicide attempts in an adolescent female twin sample. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1300–1307. doi: 10.1097/00004583-200111000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powell J, Geddes J, Deeks J, Goldacre M, Hawton K. Suicide in psychiatric hospital in-patients: risk factors and their predictive power. Br J Psychiatry. 2000;176:266–272. doi: 10.1192/bjp.176.3.266. [DOI] [PubMed] [Google Scholar]
- 15.Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003;4(10):819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 16.Ströhle A, Holsboer F. Stress responsive neurohormones in depression and anxiety. Pharmacopsychiatry. 2003;36(suppl 3):S207–S214. doi: 10.1055/s-2003-45132. [DOI] [PubMed] [Google Scholar]
- 17.Westrin A. Stress system alterations and mood disorders in suicidal patients: a review. Biomed Pharmacother. 2000;54(3):142–145. doi: 10.1016/S0753-3322(00)89047-2. [DOI] [PubMed] [Google Scholar]
- 18.Pfennig A, Kunzel HE, Kern N, Ising M, Majer M, Fuchs B, Ernst G, Holsboer F, Binder EB. Hypothalamus-pituitary-adrenal system regulation and suicidal behavior in depression. Biol Psychiatry. 2005;57(4):336–342. doi: 10.1016/j.biopsych.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 19.Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59(12):1116–1127. doi: 10.1016/j.biopsych.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 20.Wasserman D, Geijer T, Sokolowski M, Rozanov V, Wasserman J. Nature and nurture in suicidal behavior, the role of genetics: some novel findings concerning personality traits and neural conduction. Physiol Behav. 2007;92(1–2):245–249. doi: 10.1016/j.physbeh.2007.05.061. [DOI] [PubMed] [Google Scholar]
- 21.Dwivedi Y, Mondal AC, Rizavi HS, Conley RR. Suicide brain is associated with decreased expression of neurotrophins. Biol Psychiatry. 2005;58(4):315–324. doi: 10.1016/j.biopsych.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 22.Dwivedi Y, Rizavi HS, Conley RR, Roberts RC, Tamminga CA, Pandey GN. Altered gene expression of brain-derived neurotrophic factor and receptor tyrosine kinase B in postmortem brain of suicide subjects. Arch Gen Psychiatry. 2003;60(8):804–815. doi: 10.1001/archpsyc.60.8.804. [DOI] [PubMed] [Google Scholar]
- 23.Dwivedi Y, Rizavi HS, Zhang H, Mondal AC, Roberts RC, Conley RR, Pandey GN. Neurotrophin receptor activation and expression in human postmortem brain: effect of suicide. Biol Psychiatry. 2009;65(4):319–328. doi: 10.1016/j.biopsych.2008.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karege F, Vaudan G, Schwald M, Perroud N, La Harpe R. Neurotrophin levels in postmortem brains of suicide victims and the effects of antemortem diagnosis and psychotropic drugs. Brain Res Mol Brain Res. 2005;136(1–2):29–37. doi: 10.1016/j.molbrainres.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 25.Alderson RF, Curtis R, Alterman AL, Lindsay RM, DiStefano PS. Truncated TrkB mediates the endocytosis and release of BDNF and neurotrophin-4/5 by rat astrocytes and Schwann cells in vitro. Brain Res. 2000;871(2):210–222. doi: 10.1016/s0006-8993(00)02428-8. [DOI] [PubMed] [Google Scholar]
- 26.Pandey GN, Ren X, Rizavi SR, Conley RR, Roberts RC, Dwivedi Y. Brain-derived neurotrophic factor and tyrosine kinase B receptor signalling in post-mortem brain of teenage suicide victims. Int J Neuropsychopharmacol. 2008;11(8):1047–1061. doi: 10.1017/S1461145708009000. [DOI] [PubMed] [Google Scholar]
- 27.Drevets WC, Price JL, Simpson JR, Jr, Todd RD, Reich T, Vannier M, Raichle ME. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386(6627):824–827. doi: 10.1038/386824a0. [DOI] [PubMed] [Google Scholar]
- 28.Soares JC, Mann JJ. The anatomy of mood disorders: review of structural neuroimaging studies. Biol Psychiatry. 1997;41(1):86–106. doi: 10.1016/s0006-3223(96)00006-6. [DOI] [PubMed] [Google Scholar]
- 29.Bremner JD, Narayan M, Anderson ER, Staib LH, Miller HL, Charney DS. Hippocampal volume reduction in major depression. Am J Psychiatry. 2000;157(1):115–118. doi: 10.1176/ajp.157.1.115. [DOI] [PubMed] [Google Scholar]
- 30.Frodl T, Schüle C, Schmitt G, Born C, Baghai T, Zill P, Bottlender R, Rupprecht R, Bondy B, Reiser M, Möller HJ, Meisenzahl EM. Association of the brainderived neurotrophic factor Val66Met polymorphism with reduced hippocampal volumes in major depression. Arch Gen Psychiatry. 2007;64(4):410–416. doi: 10.1001/archpsyc.64.4.410. [DOI] [PubMed] [Google Scholar]
- 31.Kim YK, Lee HP, Won SD, Park EY, Lee HY, Lee BH, Lee SW, Yoon D, Han CS, Kim DJ, Choi SH. Low plasma BDNF is associated with suicidal behavior in major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(1):78–85. doi: 10.1016/j.pnpbp.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 32.Deveci A, Aydemir O, Taskin O, Taneli F, Esen-Danaci A. Serum BDNF levels in suicide attempters related to psychosocial stressors: a comparative study with depression. Neuropsychobiology. 2007;56(2–3):93–97. doi: 10.1159/000111539. [DOI] [PubMed] [Google Scholar]
- 33.Schumacher J, Jamra RA, Becker T, Ohlraun S, Klopp N, Binder EB, Schulze TG, Deschner M, Schmäl C, Höfels S, Zobel A, Illig T, Propping P, Holsboer F, Rietschel M, Nöthen MM, Cichon S. Evidence for a relationship between genetic variants at the brain-derived neurotrophic factor (BDNF) locus and major depression. Biol Psychiatry. 2005;58(4):307–314. doi: 10.1016/j.biopsych.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Oswald P, Del-Favero J, Massat I, Souery D, Claes S, Van Broeckhoven C, Mendlewicz J. No implication of brain-derived neurotrophic factor (BDNF) gene in unipolar affective disorder: evidence from Belgian first and replication patientcontrol studies. Eur Neuropsychopharmacol. 2005;15(5):491–495. doi: 10.1016/j.euroneuro.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 35.Ribeiro L, Busnello JV, Cantor RM, Whelan F, Whittaker P, Deloukas P, Wong ML, Licinio J. The brain-derived neurotrophic factor rs6265 (Val66Met) polymorphism and depression in Mexican-Americans. Neuroreport. 2007;18(12):1291–1293. doi: 10.1097/WNR.0b013e328273bcb0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarchiapone M, Carli V, Roy A, Iacoviello L, Cuomo C, Latella MC, di Giannantonio M, Janiri L, de Gaetano M, Janal MN. Association of polymorphism (Val66Met) of brain-derived neurotrophic factor with suicide attempts in depressed patients. Neuropsychobiology. 2008;57(3):139–145. doi: 10.1159/000142361. [DOI] [PubMed] [Google Scholar]
- 37.Kunugi H, Hashimoto R, Yoshida M, Tatsumi M, Kamijima K. A missense polymorphism (S205L) of the low-affinity neurotrophin receptor p75(NTR) gene is associated with depressive disorder and attempted suicide. Am J Med Genet B Neuropsychiatr Genet. 2004;129B(1):44–46. doi: 10.1002/ajmg.b.30062. [DOI] [PubMed] [Google Scholar]
- 38.McGregor S, Strauss J, Bulgin N, De Luca V, George CJ, Kovacs M, Kennedy JL. p75(NTR) gene and suicide attempts in young adults with a history of childhoodonset mood disorder. Am J Med Genet B Neuropsychiatr Genet. 2007;144B(5):696–700. doi: 10.1002/ajmg.b.30418. [DOI] [PubMed] [Google Scholar]
- 39.Hennings JM, Owashi T, Binder EB, Horstmann S, Menke A, Kloiber S, Dose T, Wollweber B, Spieler D, Messer T, Lutz R, Künzel H, Bierner T, Pollmächer T, Pfister H, Nickel T, Sonntag A, Uhr M, Ising M, Holsboer F, Lucae S. Clinical characteristics and treatment outcome in a representative sample of depressed in-patients: findings from the Munich Antidepressant Response Signature (MARS) project. J Psychiatr Res. 2009;43(3):215–229. doi: 10.1016/j.jpsychires.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 40.Binder EB, Salyakina D, Lichtner P, Wochnik GM, Ising M, Pütz B, Papiol S, Seaman S, Lucae S, Kohli MA, Nickel T, Künzel HE, Fuchs B, Majer M, Pfennig A, Kern N, Brunner J, Modell S, Baghai T, Deiml T, Zill P, Bondy B, Rupprecht R, Messer T, Köhnlein O, Dabitz H, Brückl T, Müller N, Pfister H, Lieb R, Mueller JC, Lo˜hmussaar E, Strom TM, Bettecken T, Meitinger T, Uhr M, Rein T, Holsboer F, Muller-Myhsok B. Polymorphisms in FKBP5 are associated with increased recurrence of depressive episodes and rapid response to antidepressant treatment. Nat Genet. 2004;36(12):1319–1325. doi: 10.1038/ng1479. [DOI] [PubMed] [Google Scholar]
- 41.Heck A, Lieb R, Ellgas A, Pfister H, Lucae S, Erhardt A, Himmerich H, Horstmann S, Kloiber S, Ripke S, Müller-Myhsok B, Bettecken T, Uhr M, Holsboer F, Ising M. Polymorphisms in the angiotensin-converting enzyme gene region predict coping styles in healthy adults and depressed patients. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(1):104–114. doi: 10.1002/ajmg.b.30784. [DOI] [PubMed] [Google Scholar]
- 42.Wittchen HU, Höfler M, Gander F, Pfister H, Storz S, Üstün B, Müller N, Kessler RC. Screening for mental disorders: performance of the Composite International Diagnostic-Screener (CID-S) Int J Methods Psychiatr Res. 1999;8(2):59–70. [Google Scholar]
- 43.Lucae S, Salyakina D, Barden N, Harvey M, Gagne B, Labbe M, Binder EB, Uhr M, Paez-Pereda M, Sillaber I, Ising M, Bruckl T, Lieb R, Holsboer F, MullerMyhsok B. P2RX7, a gene coding for a purinergic ligand-gated ion channel, is associated with major depressive disorder. Hum Mol Genet. 2006;15(16):2438–2445. doi: 10.1093/hmg/ddl166. [DOI] [PubMed] [Google Scholar]
- 44.Binder EB, Bradley RG, Liu W, Epstein MP, Deveau TC, Mercer KB, Tang Y, Gillespie CF, Heim CM, Nemeroff CB, Schwartz AC, Cubells JF, Ressler KJ. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. JAMA. 2008;299(11):1291–1305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.First MB, Spitzer RL, Gibbon M, Gibbon W, Janet BW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 46.Frazer KA, Ballinger DG, Cox DR, Hinds DA, Stuve LL, Gibbs RA, Belmont JW, Boudreau A, Hardenbol P, Leal SM, Pasternak S, Wheeler DA, Willis TD, Yu F, Yang H, Zeng C, Gao Y, Hu H, Hu W, Li C, Lin W, Liu S, Pan H, Tang X, Wang J, Wang W, Yu J, Zhang B, Zhang Q, Zhao H, Zhao H, Zhou J, Gabriel SB, Barry R, Blumenstiel B, Camargo A, Defelice M, Faggart M, Goyette M, Gupta S, Moore J, Nguyen H, Onofrio RC, Parkin M, Roy J, Stahl E, Winchester E, Ziaugra L, Altshuler D, Shen Y, Yao Z, Huang W, Chu X, He Y, Jin L, Liu Y, Shen Y, Sun W, Wang H, Wang Y, Wang Y, Xiong X, Xu L, Waye MM, Tsui SK, Xue H, Wong JT, Galver LM, Fan JB, Gunderson K, Murray SS, Oliphant AR, Chee MS, Montpetit A, Chagnon F, Ferretti V, Leboeuf M, Olivier JF, Phillips MS, Roumy S, Sallée C, Verner A, Hudson TJ, Kwok PY, Cai D, Koboldt DC, Miller RD, Pawlikowska L, Taillon-Miller P, Xiao M, Tsui LC, Mak W, Song YQ, Tam PK, Nakamura Y, Kawaguchi T, Kitamoto T, Morizono T, Nagashima A, Ohnishi Y, Sekine A, Tanaka T, Tsunoda T, Deloukas P, Bird CP, Delgado M, Dermitzakis ET, Gwilliam R, Hunt S, Morrison J, Powell D, Stranger BE, Whittaker P, Bentley DR, Daly MJ, de Bakker PI, Barrett J, Chretien YR, Maller J, McCarroll S, Patterson N, Pe’er I, Price A, Purcell S, Richter DJ, Sabeti P, Saxena R, Schaffner SF, Sham PC, Varilly P, Altshuler D, Stein LD, Krishnan L, Smith AV, Tello-Ruiz MK, Thorisson GA, Chakravarti A, Chen PE, Cutler DJ, Kashuk CS, Lin S, Abecasis GR, Guan W, Li Y, Munro HM, Qin ZS, Thomas DJ, McVean G, Auton A, Bottolo L, Cardin N, Eyheramendy S, Freeman C, Marchini J, Myers S, Spencer C, Stephens M, Donnelly P, Cardon LR, Clarke G, Evans DM, Morris AP, Weir BS, Tsunoda T, Mullikin JC, Sherry ST, Feolo M, Skol A, Zhang H, Zeng C, Zhao H, Matsuda I, Fukushima Y, Macer DR, Suda E, Rotimi CN, Adebamowo CA, Ajayi I, Aniagwu T, Marshall PA, Nkwodimmah C, Royal CD, Leppert MF, Dixon M, Peiffer A, Qiu R, Kent A, Kato K, Niikawa N, Adewole IF, Knoppers BM, Foster MW, Clayton EW, Watkin J, Gibbs RA, Belmont JW, Muzny D, Nazareth L, Sodergren E, Weinstock GM, Wheeler DA, Yakub I, Gabriel SB, Onofrio RC, Richter DJ, Ziaugra L, Birren BW, Daly MJ, Altshuler D, Wilson RK, Fulton LL, Rogers J, Burton J, Carter NP, Clee CM, Griffiths M, Jones MC, McLay K, Plumb RW, Ross MT, Sims SK, Willey DL, Chen Z, Han H, Kang L, Godbout M, Wallenburg JC, L’Archevêque P, Bellemare G, Saeki K, Wang H, An D, Fu H, Li Q, Wang Z, Wang R, Holden AL, Brooks LD, McEwen JE, Guyer MS, Wang VO, Peterson JL, Shi M, Spiegel J, Sung LM, Zacharia LF, Collins FS, Kennedy K, Jamieson R, Stewart J. International Hap-Map Consortium A second generation human haplotype map of over 3.1 million SNPs. Nature. 2007;449(7164):851–861. doi: 10.1038/nature06258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.de Bakker PIW, Yelensky R, Pe’er I, Gabriel SB, Daly MJ, Altshuler D. Efficiency and power in genetic association studies. Nat Genet. 2005;37(11):1217–1223. doi: 10.1038/ng1669. [DOI] [PubMed] [Google Scholar]
- 48.Purcell S, Cherny SS, Sham PC. Genetic Power Calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics. 2003;19(1):149–150. doi: 10.1093/bioinformatics/19.1.149. [DOI] [PubMed] [Google Scholar]
- 49.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. National Comorbidity Survey Replication The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 50.Westfall PH, Young SS. Resampling-Based Multiple Testing. New York, NY: John Wiley & Sons; 1993. [Google Scholar]
- 51.Westfall PH, Zaykin DV, Young SS. Multiple tests for genetic effects in association studies. Methods Mol Biol. 2002;184:143–168. doi: 10.1385/1-59259-242-2:143. [DOI] [PubMed] [Google Scholar]
- 52.Fisher RA. Statistical Methods for Research Workers. 4th ed. London, England: Oliver & Boyd; 1932. [Google Scholar]
- 53.Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21(2):263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 54.Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, Higgins J, DeFelice M, Lochner A, Faggart M, Liu-Cordero SN, Rotimi C, Adeyemo A, Cooper R, Ward R, Lander ES, Daly MJ, Altshuler D. The structure of haplotype blocks in the human genome. Science. 2002;296(5576):2225–2229. doi: 10.1126/science.1069424. [DOI] [PubMed] [Google Scholar]
- 55.Claassen CA, Trivedi MH, Rush AJ, Husain MM, Zisook S, Young E, Leuchter A, Wisniewski SR, Balasubramani GK, Alpert J. Clinical differences among depressed patients with and without a history of suicide attempts: findings from the STAR*D trial. J Affect Disord. 2007;97(1–3):77–84. doi: 10.1016/j.jad.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 56.Zubenko GS, Maher BS, Hughes HB, III, Zubenko WN, Scott Stiffler J, Marazita ML. Genome-wide linkage survey for genetic loci that affect the risk of suicide attempts in families with recurrent, early-onset, major depression. Am J Med Genet B Neu-ropsychiatr Genet. 2004;129B(1):47–54. doi: 10.1002/ajmg.b.30092. [DOI] [PubMed] [Google Scholar]
- 57.Mann JJ. The neurobiology of suicide. Nat Med. 1998;4(1):25–30. doi: 10.1038/nm0198-025. [DOI] [PubMed] [Google Scholar]
- 58.Sklar P, Gabriel SB, McInnis MG, Bennett P, Lim YM, Tsan G, Schaffner S, Kirov G, Jones I, Owen M, Craddock N, DePaulo JR, Lander ES. Family-based association study of 76 candidate genes in bipolar disorder: BDNF is a potential risk locus. Mol Psychiatry. 2002;7(6):579–593. doi: 10.1038/sj.mp.4001058. [DOI] [PubMed] [Google Scholar]
- 59.Kaufman J, Yang BZ, Douglas-Palumberi H, Grasso D, Lipschitz D, Houshyar S, Krystal JH, Gelernter J. Brain-derived neurotrophic factor-5-HTTLPR gene interactions and environmental modifiers of depression in children. Biol Psychiatry. 2006;59(8):673–680. doi: 10.1016/j.biopsych.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 60.Hong CJ, Huo SJ, Yen FC, Tung CL, Pan GM, Tsai SJ. Association study of a brain-derived neurotrophic-factor genetic polymorphism and mood disorders, age of onset and suicidal behavior. Neuropsychobiology. 2003;48(4):186–189. doi: 10.1159/000074636. [DOI] [PubMed] [Google Scholar]
- 61.Tsai SJ, Cheng CY, Yu YW, Chen TJ, Hong CJ. Association study of a brain-derived neurotrophic-factor genetic polymorphism and major depressive disorders, symptomatology, and antidepressant response. Am J Med Genet B Neuropsychiatr Genet. 2003;123B(1):19–22. doi: 10.1002/ajmg.b.20026. [DOI] [PubMed] [Google Scholar]
- 62.Surtees PG, Wainwright NW, Willis-Owen SA, Sandhu MS, Luben R, Day NE, Flint J. No association between the BDNF Val66Met polymorphism and mood status in a non-clinical community sample of 7389 older adults. J Psychiatr Res. 2007;41(5):404–409. doi: 10.1016/j.jpsychires.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 63.Sullivan PF, de Geus EJ, Willemsen G, James MR, Smit JH, Zandbelt T, Arolt V, Baune BT, Blackwood D, Cichon S, Coventry WL, Domschke K, Farmer A, Fava M, Gordon SD, He Q, Heath AC, Heutink P, Holsboer F, Hoogendijk WJ, Hottenga JJ, Hu Y, Kohli M, Lin D, Lucae S, Macintyre DJ, Maier W, McGhee KA, McGuffin P, Montgomery GW, Muir WJ, Nolen WA, Nöthen MM, Perlis RH, Pirlo K, Posthuma D, Rietschel M, Rizzu P, Schosser A, Smit AB, Smoller JW, Tzeng JY, van Dyck R, Verhage M, Zitman FG, Martin NG, Wray NR, Boomsma DI, Penninx BW. Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Mol Psychiatry. 2009;14(4):359–375. doi: 10.1038/mp.2008.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Steffens M, Lamina C, Illig T, Bettecken T, Vogler R, Entz P, Suk EK, Toliat MR, Klopp N, Caliebe A, König IR, Köhler K, Ludemann J, Diaz Lacava A, Fimmers R, Lichtner P, Ziegler A, Wolf A, Krawczak M, Nürnberg P, Hampe J, Schreiber S, Meitinger T, Wichmann HE, Roeder K, Wienker TF, Baur MP. SNP-based analysis of genetic substructure in the German population. Hum Hered. 2006;62(1):20–29. doi: 10.1159/000095850. [DOI] [PubMed] [Google Scholar]
- 65.Li D, He L. Further clarification of the contribution of the tryptophan hydroxylase (TPH ) gene to suicidal behavior using systematic allelic and genotypic meta-analyses. Hum Genet. 2006;119(3):233–240. doi: 10.1007/s00439-005-0113-x. [DOI] [PubMed] [Google Scholar]
- 66.Li D, He L. Meta-analysis supports association between serotonin transporter (5-HTT ) and suicidal behavior. Mol Psychiatry. 2007;12(1):47–54. doi: 10.1038/sj.mp.4001890. [DOI] [PubMed] [Google Scholar]
- 67.Anguelova M, Benkelfat C, Turecki G. A systematic review of association studies investigating genes coding for serotonin receptors and the serotonin transporter, II: suicidal behavior. Mol Psychiatry. 2003;8(7):646–653. doi: 10.1038/sj.mp.4001336. [DOI] [PubMed] [Google Scholar]
- 68.Kia-Keating BM, Glatt SJ, Tsuang MT. Meta-analyses suggest association between COMT, but not HTR1B, alleles, and suicidal behavior. Am J Med Genet B Neuropsychiatr Genet. 2007;144B(8):1048–1053. doi: 10.1002/ajmg.b.30551. [DOI] [PubMed] [Google Scholar]
- 69.Wasserman D, Sokolowski M, Rozanov V, Wasserman J. The CRHR1 gene: a marker for suicidality in depressed males exposed to low stress. Genes Brain Behav. 2008;7(1):14–19. doi: 10.1111/j.1601-183X.2007.00310.x. [DOI] [PubMed] [Google Scholar]
- 70.De Luca V, Tharmalingam S, Kennedy JL. Association study between the corticotropin-releasing hormone receptor 2 gene and suicidality in bipolar disorder. Eur Psychiatry. 2007;22(5):282–287. doi: 10.1016/j.eurpsy.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 71.De Luca V, Tharmalingam S, Zai C, Potapova N, Strauss J, Vincent J, Kennedy J. Association of HPA axis genes with suicidal behaviour in schizophrenia [published online October 6, 2008] J Psychopharmacol. doi: 10.1177/0269881108097817. [DOI] [PubMed] [Google Scholar]
- 72.Sparks DL, Hunsaker JC, III, Amouyel P, Malafosse A, Bellivier F, Leboyer M, Courtet P, Helbecque N. Angiotensin I-converting enzyme I/D polymorphism and suicidal behaviors. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(2):290–294. doi: 10.1002/ajmg.b.30793. [DOI] [PubMed] [Google Scholar]
- 73.Smith MA, Makino S, Kvetnansky R, Post RM. Stress and glucocorticoids affect the expression of brain-derived neurotrophic factor and neurotrophin-3 mRNAs in the hippocampus. J Neurosci. 1995;15(3, pt 1):1768–1777. doi: 10.1523/JNEUROSCI.15-03-01768.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nibuya M, Morinobu S, Duman RS. Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci. 1995;15(11):7539–7547. doi: 10.1523/JNEUROSCI.15-11-07539.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Müller MB, Toschi N, Kresse AE, Post A, Keck ME. Long-term repetitive transcranial magnetic stimulation increases the expression of brain-derived neurotrophic factor and cholecystokinin mRNA, but not neuropeptide tyrosine mRNA in specific areas of rat brain. Neuropsychopharmacology. 2000;23(2):205–215. doi: 10.1016/S0893-133X(00)00099-3. [DOI] [PubMed] [Google Scholar]
- 76.Hishimoto A, Cui H, Mouri K, Nushida H, Ueno Y, Maeda K, Shirakawa O. A functional polymorphism of the micro-opioid receptor gene is associated with completed suicides. J Neural Transm. 2008;115(3):531–536. doi: 10.1007/s00702-007-0853-y. [DOI] [PubMed] [Google Scholar]
- 77.Cui H, Nishiguchi N, Ivleva E, Yanagi M, Fukutake M, Nushida H, Ueno Y, Kitamura N, Maeda K, Shirakawa O. Association of RGS2 gene polymorphisms with suicide and increased RGS2 immunoreactivity in the postmortem brain of suicide victims. Neuropsychopharmacology. 2008;33(7):1537–1544. doi: 10.1038/sj.npp.1301557. [DOI] [PubMed] [Google Scholar]
- 78.Baud P. Personality traits as intermediary phenotypes in suicidal behavior: genetic issues. Am J Med Genet C Semin Med Genet. 2005;133C(1):34–42. doi: 10.1002/ajmg.c.30044. [DOI] [PubMed] [Google Scholar]