Abstract
Bile duct epithelial cells (i.e., cholangiocytes), which line the intrahepatic biliary epithelium, are the target cells in a number of human cholestatic liver diseases (termed cholangiopathies). Cholangiocyte proliferation and death is present in virtually all human cholangiopathies. A number of recent studies have provided insights into the key mechanisms that regulate the proliferation and function of cholangiocytes during the pathogenesis of cholestatic liver diseases. In our review, we have summarised the most important of these recent studies over the past 3 years with a focus on those performed in the animal model of extrahepatic bile duct ligation. In the first part of the review, we provide relevant background on the biliary ductal system. We then proceed with a general discussion of the factors regulating biliary proliferation performed in the cholestatic animal model of bile duct ligation. Further characterisation of the factors that regulate cholangiocyte proliferation and function will help in elucidating the mechanisms regulating the pathogenesis of biliary tract diseases in humans and in devising new treatment approaches for these devastating diseases.
Keywords: Bile duct ligation, Cholangiocyte, Cholestatic liver diseases, Extrahepatic cholestasis, Proliferation
1. Introduction
The liver, the largest internal organ of the body, is composed of two types of epithelial cells: (i) hepatocytes; and (ii) cholangiocytes [1]. Cholangiocytes line the intrahepatic and extrahepatic bile duct system of the liver [1]. The bile ductules and ducts comprise a branched system of interconnected tubes [1–3], which collect bile secreted at the canalicular membranes of hepatocytes [4], and deliver it to the gallbladder or the duodenum [1,5]. Although cholangiocytes represent a small proportion (3 to 5%) of the cells of the liver [1,5,6], these cells play an important pathophysiological role in the modification of the composition of bile during the transit in the bile ducts, which involves the secretion and absorption of water, electrolytes and other organic solutes from hepatocellular bile [1,5–10]. The modification of bile by cholangiocytes is regulated by a number of gastrointestinal hormones, which has been recently reviewed [11,12]. The regulation of cholangiocyte bicarbonate secretion is regulated by the gastrointestinal hormone secretin [5,12]. Cholangiocytes are the only cell types in the liver that express the secretin receptor (SR) [13], which is of importance to the function of the biliary epithelium in normal and pathological conditions [5,8,14–18]. In large (but not small) cholangiocytes secretin stimulates increases in intracellular cyclic adenosine 3′,5′-monophosphate (cAMP) levels [14,16,19,20] and induces the opening of the Cl− channel (cystic fibrosis transmembrane conductance regulator, CFTR) [15], which leads to the activation of the Cl−/HCO3− anion exchanger 2 (AE2) [21] and secretion of bicarbonate in bile [5].
Cholangiocytes are the target cells of a number of diseases termed cholangiopathies. This disease class is made up of inherited disorders [Alagille syndrome and cystic fibrosis (CF)], autoimmune disorders [primary sclerosing cholangitis (PSC), primary biliary cirrhosis (PBC), autoimmune cholangitis (AIC), allograft rejection, graft-versus-host disease (GVHD)], infections (cholangitis due to bacteria, fungi, parasites or viruses), drug-induced injury, ischaemic injury and diseases of unknown aetiology (biliary atresia and idiopathic vanishing bile duct syndromes) [22]. Cholangiopathies are predominantly characterised by a bile duct-directed inflammatory response that leads to bile duct injury associated with biliary proliferation in the early stage of the disease course [22]. If the biliary injury is chronic there will be increased bile duct loss, biliary fibrosis and the increased incidence of bile duct cancer (i.e., cholangiocarcinoma) [22].
2. Anatomical and morphological features of the biliary tree
The intrahepatic biliary epithelium is divided into extrahepatic and intrahepatic bile ducts [2,3,23,24]. The intrahepatic bile ductal system consists of the portion of (i) bile canaliculi, small spaces localised between two adjacent hepatocytes (0.5–2 mm) forming a three-dimensional network that continues in (ii) bile ductules (canals of Hering), localised at the periphery of the hepatic lobule and characterised by 3–4 cholangiocytes, that form the junction between hepatocytes and cholangiocytes (ductular–canalicular junction) allowing the confluence of the bile in (iii) bile ducts (interlobular bile ducts) localised in the portal space. Interlobular bile ducts progressively continue in larger ducts until the right and left hepatic ducts, that, at the level of the hylus, determine the origin of extrahepatic biliary tree [25–27]. According to Ludwig, the human intrahepatic biliary epithelium is divided into small bile ductules (<15 μm), interlobular ducts (15–10 μm), septal ducts (100–300 μm), segmental ducts (400–800 μm) and hepatic ducts (>800 μm) [24]. The rodent intrahepatic bile duct system has been recently classified into small ducts (<15 μm in external diameter) lined by small cholangiocytes (approximately 8 μm in diameter characterised by high nucleus/cytoplasm ratio) and large bile ducts (>15 μm in diameter characterised by low nucleus/cytoplasm ratio) lined by large cholangiocytes (approximately 15 μm in diameter) [2,16,19,25,28]. These studies have also shown that a significant relationship exists between cholangiocyte area and external bile duct diameter, with small bile ducts lined by small cholangiocytes and large ducts lined by large cholangiocytes [2,16,19]. The latter finding is particularly relevant since it allows for the direct mapping of studies obtained in isolated small and large cholangiocytes to different portions (i.e., small and large) of the intrahepatic biliary epithelium ex situ [2,14–19]. In support of the morphological heterogeneity of the biliary epithelium, Masyuk et al. have reconstructed the intrahepatic biliary system that resembles a tree, with the common and hepatic ducts corresponding to the trunk, the intrahepatic bile ducts corresponding to the large branches and the small ductules corresponding to the smallest tree limbs of the tree [29].
3. Cholangiocyte proliferation in response to bile duct ligation
A number of studies have defined three types of cholangiocyte proliferation: “typical”, “atypical” and oval cell proliferation [30]. “Typical” cholangiocyte proliferation is a hyperplastic reaction, which induces an increase in the number of intrahepatic bile ducts (with a well-defined lumen) confined to portal areas [5,31]. “Atypical” cholangiocyte proliferation is commonly seen in patients with prolonged cholestatic liver diseases such as PBC or PSC and is characterised by irregular proliferation of intrahepatic bile ducts sprouting into periportal and parenchymal regions and occasionally forming anastomosing cords with adjacent hepatocytes [32,33]. Oval cell proliferation takes place in the early stages of chemically induced hepatocarcinogenesis and is characterised by a disorganised proliferation of biliary structures with a poorly defined lumen [34]. Oval cell proliferation is not discussed in this review.
In animal models, “typical” cholangiocyte proliferation is achieved by a number of experimental manoeuvres, including BDL (Fig. 1) [5], partial hepatectomy [35], acute carbon tetrachloride (CCl4) treatment [17,18] and chronic feeding of α-naphthylisothiocyanate (ANIT) [36], or bile salts [37]. In these hyperplastic models, cholangiocyte proliferation is closely associated with increased SR gene expression and secretin-stimulated cAMP levels [5,13,17,18,35–38]. cAMP, which is generated by adenylyl cyclases (AC), plays an important role in the modulation of cholangiocyte function [35,39–42]. A recent study by Strazzabosco et al. demonstrates that differential expression of AC isoforms mediate the secretory functions of small and large cholangiocytes [41]. This study demonstrated that large cholangiocyte responsiveness to secretin was mediated by the expression of AC8 [41]. A number of animal models that mimic cholestatic liver diseases and liver injury have been utilised to expand our knowledge related to the mechanisms of cholangiocyte proliferation [1,12,43]. Of these models of bile duct injury, the BDL model has been the most commonly used. A number of coordinate factors (stimulatory or inhibitory) have been shown to regulate cholangiocyte growth in the cholestatic BDL model. It has been shown that increased biliary pressure is a trigger for the stimulation or inhibition of these putative growth factors [44,45]. A recent study has shown [45] that increased biliary and portal hypertension (induced by the first), represent key proliferative triggers for the growth of bile ducts and hepatocytes. Similar to findings in human cholangiopathies (e.g., PBC and PSC), recent studies in rats have demonstrated that “typical” cholangiocyte proliferation occurs within a limited range of duct sizes [16,18,46]. In rats with BDL, enhanced cholangiocyte proliferative capacity is restricted to large bile ducts [18,46]. In an experimental animal model of bile duct damage, CCl4 induces loss of large ducts and loss of large duct secretion [17,18,47]. To compensate for the loss of duct function due to this toxin [17,18], small cholangiocytes proliferate and develop de novo secretory activity due to de novo expression of SR [17,18]. A hallmark of large cholangiocyte proliferation induced by BDL in rats is the increased SR expression and subsequent secretory activity [18,46]. A recent study in mice with BDL demonstrated that similar to rats, the mouse intrahepatic biliary epithelium is morphologically and functionally heterogeneous [16]. These findings are of importance due to increased availability and usage of transgenic mouse models for studying cholestatic liver disease pathogenesis [16]. The study indicates that the mouse is a suitable model for defining the heterogeneous responses of cholangiocytes during cholestasis and biliary damage [16]. Since SR is only expressed by cholangiocytes in the liver [13], changes in the functional expression of this receptor have been suggested as a pathophysiological tool for evaluating changes in the degree of cholangiocyte growth/loss [5,16–18,35–40,46]. Proliferating cholangiocytes acquire a neuroendocrine phenotype and secrete and respond to a number of hormones, neuropeptides and neurotransmitters [43,48–50]. The formation of a neuroendocrine compartment predominated by cholangiocytes represents a unique opportunity for cholangiocytes to regulate their own proliferation via autocrine pathways and for cholangiocytes to influence other nearby cell types, such as vascular endothelial cells, portal fibroblasts and hepatic stellate cells [43,49]. A number of recent studies have highlighted and expanded our knowledge of the concept that proliferating cholangiocytes display neuroendocrine features [43,49].
Fig. 1.
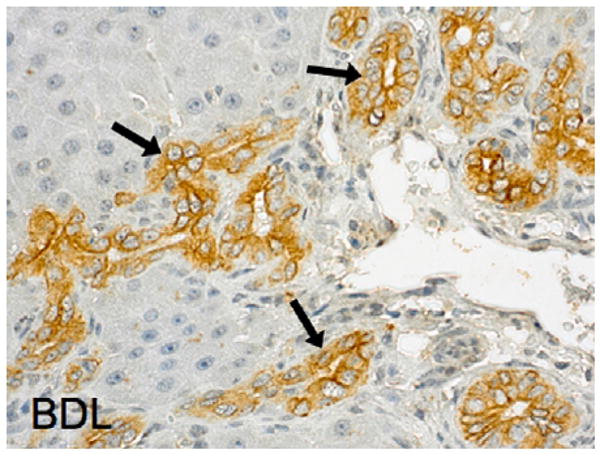
Immunolocalisation of cytokeratin-19 (CK-19) in proliferating cholangiocytes in the bile duct ligation (BDL) animal model. Original magnification 40×.
4. Update on neuroendocrine regulation of biliary proliferation during BDL
Over the past several years, a number of studies have explored the neuroendocrine regulation of cholangiocyte proliferation during extrahepatic cholestasis. The neuroendocrine factors contributing to cholangiocyte proliferation have been previously reviewed [43,48–50]. We discuss here the most recent advances which are highlighted in Tables 1 and 2.
Table 1.
Neuroendocrine regulation of cholangiocyte growth.
| Regulatory factors | Effect on cholangiocyte growth | Second messenger/transduction pathways | References |
|---|---|---|---|
| Calcitonin gene-related peptide | Sensory innervation and α- and β-CGRP stimulate biliary growth | Activation PKA and CREB | [53] |
| RAMH (HRH3 agonist) | Activation of HR3R decrease biliary hyperplasia | Downregulation of cAMP-dependent PKA–ERK1/2-Elk-1 signalling | [57] |
| GLP-1 receptor agonist exendin-4 | Activation of GLP-1 receptors stimulates biliary growth in normal and BDL rats | Activation of PI3K, cAMP/PKA and Ca2+-CaMKII α signalling mechanisms | [60] |
| GLP-1 receptor agonist exendin-4 | In vivo, exendin-4 prevents CCl4-induced biliary apoptosis | Exendin-4 prevents apoptosis-induced Bax mitochondrial translocation, cytochrome c release and increased caspase 3 activity | [61] |
| Progesterone |
|
|
[48] |
| Follicle-stimulating hormone | FSH increases biliary proliferation, whereas blockage of cholangiocyte FSH secretion decreases cholangiocyte proliferation |
|
[31] |
| Taurocholic acid |
|
Increased cholangiocyte VEGF expression | [47,63,67–70] |
BDL: bile duct ligation; CGRP: calcitonin gene-related peptide; CREB: cAMP response element binding; CaMKII α: calmodulin-dependent protein kinase α; ERK1/2: extracellular signal-regulated kinase 1/2; FSH: follicle-stimulating hormone; GLP-1: glucagon-like peptide-1; HR: histamine receptor; 3β-HSD: 3β-hydroxysteroid dehydrogenase; PKA: protein kinase A; p450scc: cytochrome P450 side-chain cleavage; PI3K: phosphoinositide 3-kinase; RAMH: (R)-(α)-(−)-methylhistamine dihydrobromide; STAR: steroidogenic acute regulatory protein; and VEGF: vascular endothelial growth factor.
Table 2.
Other factors regulating cholangiocyte proliferation during cholestasis.
| Regulatory factors | Effect on cholangiocyte growth | Second messenger/transduction pathways | References |
|---|---|---|---|
| Endocannabinoid system | Chronic treatment of rats with BDL with anandamide decreased cholangiocyte proliferation | Accumulation of reactive oxygen species; upregulation of the expression of TRX1, Ref1, c-Fos, and c-Jun expression; increase in the nuclear localisation of TRX1; increase in AP-1 transcriptional activity | [72] |
| CD44 and hyaluronic acid | Cholangiocyte proliferation is stimulated by hyaluronan treatment, and blocked by siRNA for CD44 or anti-CD44 antibody | Autocrine loop. Cholangiocytes are an important source of hepatic CD44 | [77] |
| Insulin-like growth factor-1 | Modulates response of cholangiocytes to damage. Promote cholangiocyte growth | Autocrine loop. In liver cells the ‘locally acting’ IGF1 isoform is important in modulating response of cholangiocytes to damage | [78–80] |
| Ezrin–radixin–moesin-binding phosphoprotein | Contribute to the proliferative responses of cholangiocytes. Organises and regulates bile secretory proteins in cholangiocytes | The expression and distribution of EBP50 (regulated by oestrogens) contribute to the proliferative responses of cholangiocytes | [82] |
| Death receptor 5 | BDL upregulates DR5 expression on cholangiocytes sensitising them to the effects of DR5 stimulation | [83] | |
| Foxl1 (winged helix transcription factor) |
|
Decreased expression of Wnt3a and Wnt7b expression along with reduced expression of the β-catenin target gene Cyclin D1 | [84,85] |
| Integrin αvβ6 |
|
Adhesion to fibronectin, auto/paracrine TGF-β1 activation | [86,87] |
HA: hyaluronic acid; BDL: bile duct ligation; DR5: death receptor 5; EBP50: ezrin–radixin–moesin-binding phosphoprotein 50; IGF-1: insulin-like growth factor; and TGF-β1: transforming growth factor-β1.
4.1. Neuropeptides and neurotransmitters
CGRP (calcitonin gene-related peptide) is a potent vasodilator peptide that participates in the regulation of vascular tone and regional organ blood flow [51,52]. We have recently demonstrated that hepatic sensory innervation and cholangiocyte expression of α-CGRP (Fig. 2) play a key role in the regulation of cholangiocyte proliferation during cholestasis induced by BDL [53]. Knockout of αα CGRP decreases intrahepatic bile duct mass and inhibits cholangiocyte proliferation in BDL mice [53]. Both α- and β-CGRP stimulated proliferation of isolated BDL cholangiocytes by activation of protein kinase A (PKA) and cAMP response element binding (CREB) [53]. These studies indicate that sensory innervation plays a role in the regulation of biliary proliferation and other sensory neuropeptides may play a role in chronic inflammation during cholangiopathies
Fig. 2.
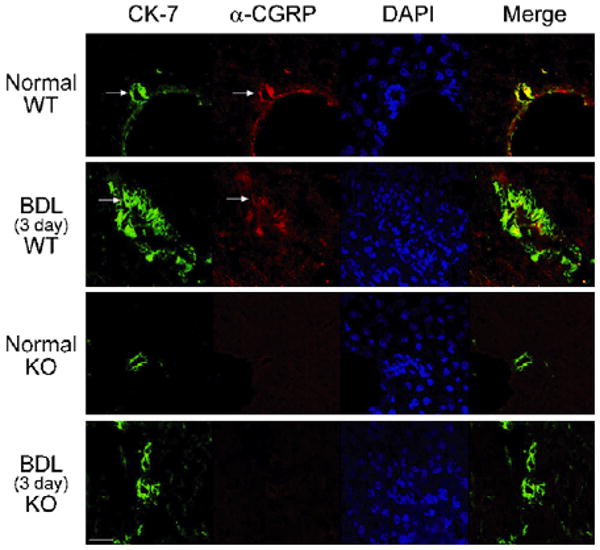
Localisation of α-CGRP (red) by immunofluorescence in normal and 3-day BDL WT mice liver sections. Bile ducts were stained with CK-7 (green). α-CGRP-positive staining and CK-7 colocalise in the bile ducts of 3-day BDL WT mice. The scale bar represents 20 μM. Arrows indicate bile ducts.
Reproduced with permission from Ref. [53].
The aminergic peptide and neurotransmitter histamine regulates many functions in the body, such as neurogenic functions, inflammatory responses, allergic responses, and gastric secretion [54–56]. Normal and BDL rat cholangiocytes express all of the G-protein coupled histamine receptor subtypes (HRH1, HRH2, HRH3 and HRH4) [57]. Following BDL, the expression of HR3R is significantly increased in proliferating cholangiocytes. Activation of HR3R by the chronic administration of the agonist (R)-(α)-(−)-methylhistamine dihydrobromide (RAMH) to rats for 7 days after BDL resulted in a decrease in the growth of the biliary tree with no difference in the rate of apoptosis [57]. In addition, administration of histamine to this animal model of cholestasis also resulted in a decrease in cholangiocyte proliferation, and blocking histamine actions by using the selective HR3R antagonist thioperamide maleate resulted in a partial reversal of these effects [57]. Both in vivo and in vitro, RAMH inhibition of cholangiocyte growth was associated with downregulation of cAMP-dependent PKA–ERK1/2-Elk-1 signalling pathway [57].
4.2. Glucagon-like peptide-1 (GLP-1)
GLP-1 is secreted by a number of neuroendocrine cell types and plays a role in sustaining beta-cell survival in experimental models of diabetes and induces the transdifferentiation of pancreatic ductal cells [58,59]. GLP-1 and the GLP-1 receptor specific agonist exendin-4 had similar effects on cholangiocytes by stimulating proliferation in vivo in normal rats and in isolated cholangiocytes from normal and BDL rats [60]. GLP-1 receptor was significantly upregulated during BDL compared to sham operated animals [60]. Cholangiocytes from BDL but not normal rats express the message for the precursor for GLP-1, preproglucagon, which is a finding that suggests that GLP-1 is an important player in biliary growth during cholestasis [60]. In fact, administration of the GLP-1R antagonist, exendin-9–39 significantly decreased ductal mass and biliary functional activity in BDL rats [60]. The pro-proliferative effect of GLP-1 was mediated through phosphoinositide 3-kinase (PI3K), cAMP/PKA and Ca2+-CaMKII α (calmodulin-dependent protein kinase α) signalling mechanisms [60]. The mechanisms by which GLP-1 regulates cholangiocyte growth are depicted in Fig. 3. More recently, exendin-4 has been shown to protect cholangiocytes from apoptosis in in vivo and in vitro models of cholangiocyte apoptosis [61]. In vitro, exendin-4 prevented glycochenodeoxycholic acid-induced Bax mitochondrial translocation, cytochrome c release and caspase 3 activities, which was blocked by inhibition of PI3K [61]. In vivo, exendin-4 administration prevented the increase in TUNEL, positive cholangiocytes and the loss of bile ducts that is observed in BDL rats treated with CCl4 [61]. These findings suggest that exendin-4 can correct the dysregulated balance between cholangiocyte proliferation and death during cholestasis [61]. Further studies are required to determine if exendin-4 will be effective for preventing the progression of cholangiopathies towards ductopenia.
Fig. 3.
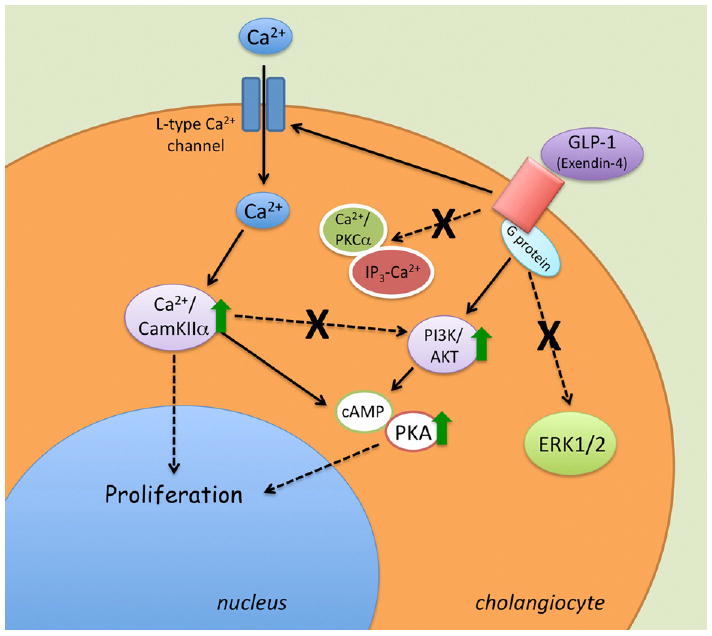
Proposed sequence of intracellular events associated to GLP-1R activation in cholangiocytes. GLP-1R activation sustains cell growth enhancing the activation state of the PI3K and cAMP/PKA cascades. Cell proliferation is also elicited by the extracellular Ca2+-dependent activation of CaMKIIα that can modulate cholangiocyte proliferation both directly and by cross-talking with the cAMP/PKA cascade. In contrast, GLP-1R activation does not result in any change of ERK1/2 activation state and does not increase the IP3-PKCα signalling.
Reproduced with permission from Ref. [60].
4.3. Progesterone
We have recently demonstrated that the steroid hormone progesterone stimulates the proliferation of both male and female cholangiocytes [48]. Cholangiocytes express the PR-B nuclear receptor and several membrane receptors for progesterone (PRGMC1, PRGMC2, and mPRalpha) [48]. Chronic administration of progesterone increased the number of bile ducts of normal rats [48]. Administration of an anti-progesterone antibody inhibited cholangiocyte growth stimulated by BDL [48]. Interestingly, normal and BDL cholangiocytes expressed the biosynthetic pathway (i.e., steroidogenic acute regulatory protein or STAR, 3β-hydroxysteroid dehydrogenase or 3β-HSD, and cytochrome P450 side-chain cleavage or p450scc) for and secrete progesterone [48] (Fig. 4). In vitro, supernatants collected from normal and BDL cholangiocytes increased cholangiocyte proliferation, which was partially inhibited by preincubation with anti-progesterone and inhibition of progesterone steroidogenesis with aminoglutethimide prevented cholangiocyte proliferation [48]. These findings provide further support for the concept that neuroendocrine autocrine/paracrine mechanisms play a key role in the modulation of cholangiocyte proliferative responses to cholestasis
Fig. 4.
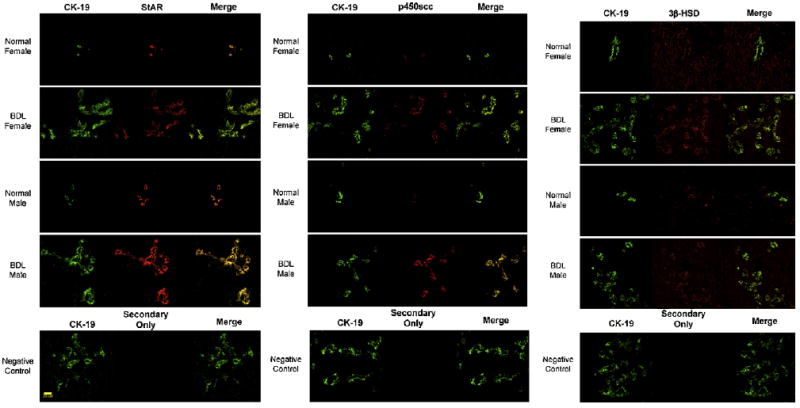
Immunofluorescence for key proteins in the progesterone steroidogenesis pathway [steroidogenic acute regulatory protein (StAR), P450 side-chain cleavage (p450scc), and 3β-hydroxysteroid dehydrogenase (3β-HSD)] in liver sections from normal and BDL female and male rats demonstrates that bile ducts express these steroidogenesis pathway proteins (red staining). Colocalisation with CK-19 (green staining, a cholangiocyte-specific marker) of the bile ducts expressing StAR, p450scc, and 3β-HSD is also visible.
Reproduced with permission from Ref. [48].
4.4. Follicle-stimulating hormone (FSH)
FSH, also called gonadotropin because it stimulates the gonads, is produced in the anterior pituitary gland of the brain [62]. We found that cholangiocytes expressed the FSH receptor (FSHR) and secreted FSH [31]. Chronic administration of FSH to normal rats increased, whereas administration of antide (a gonadotropin-releasing hormone antagonist that blocks FSH secretion) and anti-FSH to normal rats decreased cholangiocyte proliferation and secretory responses [31]. In vitro, FSH increased cholangiocyte proliferation, cAMP levels, and ERK1/2 and Elk-1 phosphorylation, which were prevented by preincubation with anti-FSH [31]. Silencing of FSH expression also decreases basal cholangiocyte proliferation suggesting that FSH is a key autocrine factor regulating biliary mass [31]. These findings have important pathological implications since modulation of the expression and secretion of FSH may be used to modulate cholangiocyte proliferation during cholestatic liver diseases
4.5. Angiogenic factors
Vascular endothelial growth factor (VEGF) is a mitogen for vascular endothelial cells for vascular cells and regulates vascular pathophysiology [63,64]. We have previously shown that VEGF-A and VEGF-C are secreted by cholangiocytes and play an important role in the regulation of cholangiocyte proliferation and apoptosis during cholestasis and biliary injury induced by hepatic artery ligation [65,66]. We have also shown that the bile acid TC prevents cholangiocyte death by apoptosis, and the loss of proliferative and functional responses of cholangiocytes in response to CCl4 and cholinergic or adrenergic denervation [47,67,68]. Also, taurocholic acid feeding prevents tumour necrosis factor (TNF)-alpha-induced damage of cholangiocytes by a PI3K-mediated pathway [69].
A recent study has provided additional evidence that VEGF plays a role in both the protection of cholangiocytes from damage in an experimental model of cholestasis [70]. In an animal model of cholestasis and biliary damage induced by caffeic acid, the feeding of the protective bile acid, taurocholate prevented bile duct damage, which was associated with increased cholangiocyte VEGF-A, VEGF-C, VEGFR-2 and VEGFR-3 expression [70].
4.6. Other factors regulating cholangiocyte proliferation during cholestasis
4.6.1. Endocannabinoid system
The endocannabinoid system has been implicated in the pathogenesis of liver fibrosis and portal hypertension [71]. Recent evidence also indicates that the endocannabinoid system plays a role in regulating cholangiocyte proliferation during cholestasis induced by BDL [72]. Chronic treatment of rats with BDL with anandamide decreased cholangiocyte proliferation and induced the accumulation of reactive oxygen species, upregulated the expression of TRX1, Ref1, c-Fos and c-Jun expression, increased the nuclear localisation of TRX1 and increased AP-1 transcriptional activity [72]. These effects occurred via the activation of the cannabinoid receptor, Cb2 [72]. This work demonstrated that modulation of the endocannabinoid system and/or the ROS/TRX1/Ref1/AP-1 pathway may have therapeutic implications for the treatment of early stage cholestatic liver diseases characterised by cholangiocyte proliferation [72].
4.6.2. CD44 and hyaluronic acid
CD44 is a multifunctional cell adhesion molecule, which takes part in cell–cell and cell–matrix interactions [73,74]. Hyaluronic acid (HA), the main component of extracellular matrices, is the primary ligand of CD44 [75]. High levels of hepatic CD44 expression have been observed in patients with PSC [76]. He et al. provide evidence that suggests that the proliferative cholangiocytes lining the intrahepatic ducts are an important source of hepatic CD44 [77]. CD44-positive cholangiocytes were closely associated with extracellular hyaluronan accumulated in the portal tracts of BDL livers [77]. They demonstrated in vitro that cholangiocyte proliferation was stimulated by hyaluronan treatment, and blocked by siRNA for CD44 or anti-CD44 antibody [77]. CD44–hyaluronan interactions may play a pathogenic role in the development of cholestatic liver diseases by enhancing biliary proliferation [77].
4.6.3. Insulin-like growth factor-1
Previous studies [78,79] have shown that IGF1 plays a key role in mediating cholangiocyte proliferation after BDL and in protecting cholangiocytes from the cytotoxic effect of hydrophobic bile salts. More recently, we evaluated the expression of IGF1 isoforms in rat cholangiocytes, and evaluated their involvement in cell proliferation or damage induced by BDL or hydrophobic bile salts [80]. In both hepatocytes and cholangiocytes, the ‘locally acting’ IGF1 isoform (XO6108) and ‘circulating’ IGF1 isoform (NM 178866) [81] represent respectively 44% and 52% of the total IGF1 [80]. Basal mRNAs for both ‘locally acting’ and ‘circulating’ IGF1 isoforms are significantly higher in hepatocytes compared to cholangiocytes [80]. After BDL for 3 h, the ‘locally acting’ IGF1 isoform decreases threefold in hepatocytes but remains stable in cholangiocytes with respect to sham-controls [80]. After 1 week of BDL, hepatocytes displays a further fivefold decrease of ‘locally acting’ IGF1 mRNA. In contrast, cholangiocytes show an eightfold increase of the ‘locally acting’ IGF1 mRNA. The effect of BDL for 3 h on IGF1 isoforms was reproduced in vitro by incubation with glycochenodeoxycholate (GCDC) [80]. The cytotoxic effects (inhibition of proliferation and induction of apoptosis) of GCDC on isolated cholangiocytes were more pronounced after silencing (siRNA) of ‘locally acting’ than ‘circulating’ IGF1 isoform [80]. Therefore, these findings demonstrate that rat cholangiocytes express the ‘locally acting’ IGF1 isoform, which decreases during cell damage and increases during cell mitosis [80]. The ‘locally acting’ IGF1 is more active than the ‘circulating’ isoform in protecting cholangiocytes from GCDC-induced cytotoxicity [80]. These findings indicate that, besides muscle and neural tissues, also in liver cells the ‘locally acting’ IGF1 isoform is important in modulating response of cholangiocytes to damage.
4.6.4. Ezrin–radixin–moesin-binding phosphoprotein
Ezrin–radixin–moesin-binding phosphoprotein 50 (EBP50) is inducible by oestrogen and alters cell proliferation. This study demonstrated the expression and role of EBP50 in ductular reaction in normal human liver, human cholangiopathies (i.e., CF, PBC and PSC) and BDL rats [82]. The study demonstrated that in normal human liver, EBP50 is expressed in the canalicular membranes of hepatocytes and, together with ezrin and CFTR, in the apical domains of cholangiocytes [82]. In human cholangiopathies and BDL rats, EBP50 was redistributed to the cytoplasmic and nuclear compartments [82]. There was transient increase of EBP50 in rat cholangiocytes after BDL, whereas such expression was downregulated in ovariectomised rats [82]. These studies demonstrated that the expression and distribution of EBP50 (regulated by oestrogens) contribute to the proliferative responses of cholangiocytes [82].
4.6.5. Death receptor 5
Takeda et al. have demonstrated that the death signalling pathway mediated by TNF-related apoptosis-inducing ligand (TRAIL) receptor 2/death receptor 5 (DR5) contributes to the pathogenesis of biliary cirrhosis [83]. Administration of an agonistic anti-DR5 monoclonal antibody triggered cholangiocyte apoptosis, cholangitis and cholestatic liver injury reminiscent of PSC [83]. BDL upregulates DR5 expression on cholangiocytes, sensitising them to the effects of DR5 stimulation [83]. DR5 and TRAIL expression were also found to be elevated in cholangiocytes of human PSC and PBC patient samples suggesting that modulation of DR5 death signalling might be a therapeutic option for chronic cholestatic liver diseases [83]
4.6.6. Foxl1 (winged helix transcription factor)
Foxl1 has been previously shown to be dramatically induced in cholangiocytes by both BDL and in response to 3,5-diethoxycarbonyl-1,4-dihydrocollidine diet [84]. In Foxl1 knockout mice with BDL, they observed an increase in parenchymal necrosis and significantly impaired cholangiocyte and hepatocyte proliferation [85]. In addition, there was decreased expression of Wnt3a and Wnt7b expression along with reduced expression of the β-catenin target gene Cyclin D1 [85]. This work suggests that Foxl1 is an upstream mediator of β-catenin-induced cholangiocyte proliferation during cholestasis [85].
4.6.7. Integrin αvβ6
The expression of αvβ6 is markedly increased on cholangiocytes in response to extrahepatic obstruction by BDL and drives fibrogenesis [86,87]. Inhibition of αvβ6 by EMD527040 reduced cholangiocyte proliferation and inhibits the progression of primary and secondary biliary fibrosis [87]. The regulation of cholangiocyte proliferation may provide a means to prevent biliary fibrosis during chronic cholestatic liver diseases.
5. Summary and future directions
We have reviewed recent studies that address factors that regulate cholangiocyte proliferation during extrahepatic cholestasis induced by BDL. Cholangiocyte proliferation is closely associated with transdifferentiation to a neuroendocrine phenotype. Future studies will be necessary to determine the role that proliferating cholangiocytes play in the pathogenesis of biliary fibrosis during cholestasis and how cholangiocytes interact with other cell types of the liver such as hepatic stellate cells during cholestatic liver diseases. Our developing knowledge of the fundamental factors that control cholangiocyte proliferation during cholestasis will aid in the development of therapies for the treatment of chronic cholestatic liver diseases.
Acknowledgments
Portions of the studies discussed here were supported partly by a grant award from Scott & White and NIH RO1 DK081442 to Shannon Glaser, by the Dr. Nicholas C., Hightower Centennial Chair of Gastroenterology from Scott & White, the VA Research Career Scientist Award, a VA Merit Award and the NIH grants DK76898, DK58411 and DK62975 to Gianfranco Alpini, by University and Federate Athenaeum funds from University of Rome “La Sapienza” to Eugenio Gaudio and MIUR grants: PRIN #2007, prot. 2007HPT7BA 003 to Domenico Alvaro.
List of abbreviations
- AIC
autoimmune cholangitis
- BDL
Bile duct ligation
- CaMKII α
calmodulin-dependent protein kinase α
- cAMP
cyclic adenosine 3′,5′-monophosphate
- CCl4
carbon tetrachloride
- CF
cystic fibrosis
- CFTR
cystic fibrosis transmembrane conductance regulator
- CGRP
calcitonin gene-related peptide
- CREB
cAMP response element binding
- ERK1/2
extracellular signal-regulated kinase
- FSH
follicle-stimulating hormone
- GCDC
glycochenodeoxycholate
- GLP-1
glucagon-like peptide-1
- GVHD
graft-versus-host disease
- 3β-HSD
3β-hydroxysteroid dehydrogenase
- IGF-1
insulin-like growth factor-1
- PBC
primary biliary cirrhosis
- PI3K
phosphoinositide 3-kinase
- PKA
protein kinase A
- PSC
primary sclerosing cholangitis
- p450scc
cytochrome P450 side-chain cleavage
- SR
secretin receptor
- STAR
steroidogenic acute regulatory protein
- TNF
tumor necrosis factor
- VEGF
vascular endothelial growth factor
Footnotes
Conflict of interest statement: None declared.
Contributor Information
S.S. Glaser, Email: sglaser@tamu.edu.
E. Gaudio, Email: eugenio.gaudio@uniroma1.it.
References
- 1.Alpini G, Prall RT, LaRussoF NF. The pathobiology of biliary epithelia. In: Arias IM, Boyer JL, Chisari FV, Fausto N, Jakoby W, Schachter D, Shafritz DA, editors. The liver; biology & pathobiology. 4th. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. pp. 421–35. [Google Scholar]
- 2.Kanno N, LeSage G, Glaser S, et al. Functional heterogeneity of the intrahepatic biliary epithelium. Hepatology. 2000;31:555–61. doi: 10.1002/hep.510310302. [DOI] [PubMed] [Google Scholar]
- 3.Sasaki H, Schaffner F, Popper H. Bile ductules in cholestasis: morphologic evidence for secretion and absorption in man. Lab Invest. 1967;16:84–95. [PubMed] [Google Scholar]
- 4.Nathanson MH, Boyer JL. Mechanisms and regulation of bile secretion. Hepatology. 1991;14:551–66. [PubMed] [Google Scholar]
- 5.Alpini G, Lenzi R, Sarkozi L, et al. Biliary physiology in rats with bile ductular cell hyperplasia. Evidence for a secretory function of proliferated bile ductules. J Clin Invest. 1988;81:569–78. doi: 10.1172/JCI113355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Racanelli V, Rehermann B. The liver as an immunological organ. Hepatology. 2006;43:S54–62. doi: 10.1002/hep.21060. [DOI] [PubMed] [Google Scholar]
- 7.Glaser S, Rodgers RE, Phinizy JL, et al. Gastrin inhibits secretin-induced ductal secretion by interaction with specific receptors on rat cholangiocytes. Am J Physiol Gastrointest Liver Physiol. 1997;273:G1061–70. doi: 10.1152/ajpgi.1997.273.5.G1061. [DOI] [PubMed] [Google Scholar]
- 8.Glaser S, Francis H, DeMorrow S, et al. Heterogeneity of the intrahepatic biliary epithelium. World J Gastroenterol. 2006;12:3523–36. doi: 10.3748/wjg.v12.i22.3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvaro D, Cho WK, Mennone A, et al. Effect of secretion on intracellular pH regulation in isolated rat bile duct epithelial cells. J Clin Invest. 1993;92:1314–25. doi: 10.1172/JCI116705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvaro D, Alpini G, Jezequel AM, et al. Role and mechanisms of action of acetylcholine in the regulation of rat cholangiocyte secretory functions. J Clin Invest. 1997;100:1349–62. doi: 10.1172/JCI119655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Esteller A. Physiology of bile secretion. World J Gastroenterol. 2008;14:5641–9. doi: 10.3748/wjg.14.5641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanno N, LeSage G, Glaser S, et al. Regulation of cholangiocyte bicarbonate secretion. Am J Physiol Gastrointest Liver Physiol. 2001;281:G612–25. doi: 10.1152/ajpgi.2001.281.3.G612. [DOI] [PubMed] [Google Scholar]
- 13.Alpini G, Ulrich CD, 2nd, Phillips JO, et al. Upregulation of secretin receptor gene expression in rat cholangiocytes after bile duct ligation. Am J Physiol. 1994;266:G922–8. doi: 10.1152/ajpgi.1994.266.5.G922. [DOI] [PubMed] [Google Scholar]
- 14.Alpini G, Roberts S, Kuntz SM, et al. Morphological, molecular, and functional heterogeneity of cholangiocytes from normal rat liver. Gastroenterology. 1996;110:1636–43. doi: 10.1053/gast.1996.v110.pm8613073. [DOI] [PubMed] [Google Scholar]
- 15.Alpini G, Ulrich C, Roberts S, et al. Molecular and functional heterogeneity of cholangiocytes from rat liver after bile duct ligation. Am J Physiol Gastrointest Liver Dis. 1997;272:G289–97. doi: 10.1152/ajpgi.1997.272.2.G289. [DOI] [PubMed] [Google Scholar]
- 16.Glaser S, Gaudio E, Rao A, et al. Morphological and functional heterogeneity of the mouse intrahepatic biliary epithelium. Lab Invest. 2009;89:456–69. doi: 10.1038/labinvest.2009.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LeSage G, Benedetti A, Glaser S, et al. Acute carbon tetrachloride feeding selectively damages large, but not small, cholangiocytes from normal rat liver. Hepatology. 1999;29:307–19. doi: 10.1002/hep.510290242. [DOI] [PubMed] [Google Scholar]
- 18.LeSage G, Glaser S, Marucci L, et al. Acute carbon tetrachloride feeding induces damage of large but not small cholangiocytes from BDL rat liver. Am J Physiol Gastrointest Liver Physiol. 1999;276:G1289–301. doi: 10.1152/ajpgi.1999.276.5.G1289. [DOI] [PubMed] [Google Scholar]
- 19.Alpini G, Glaser S, Robertson W, et al. Large but not small intrahepatic bile ducts are involved in secretin-regulated ductal bile secretion. Am J Physiol Gastrointest Liver Physiol. 1997;272:G1064–74. doi: 10.1152/ajpgi.1997.272.5.G1064. [DOI] [PubMed] [Google Scholar]
- 20.Ueno Y, Alpini G, Yahagi K, et al. Evaluation of differential gene expression by microarray analysis in small and large cholangiocytes isolated from normal mice. Liver Int. 2003;23:449–59. doi: 10.1111/j.1478-3231.2003.00876.x. [DOI] [PubMed] [Google Scholar]
- 21.Banales JM, Arenas F, Rodriguez-Ortigosa CM, et al. Bicarbonate-rich choleresis induced by secretin in normal rat is taurocholate-dependent and involves AE2 anion exchanger. Hepatology. 2006;43:266–75. doi: 10.1002/hep.21042. [DOI] [PubMed] [Google Scholar]
- 22.Xia X, DeMorrow S, Francis H, et al. Cholangiocyte injury and ductopenic syndromes. Semin Liver Dis. 2007;27:401–12. doi: 10.1055/s-2007-991516. [DOI] [PubMed] [Google Scholar]
- 23.Schaffner F, Popper H. Electron microscopic studies of normal and proliferated bile ductules. Am J Pathol. 1961;38:393–410. [PMC free article] [PubMed] [Google Scholar]
- 24.Ludwig J. New concepts in biliary cirrhosis. Semin Liver Dis. 1987;7:293–301. doi: 10.1055/s-2008-1040584. [DOI] [PubMed] [Google Scholar]
- 25.Gaudio E, Carpino G, Cardinale V, et al. New insights into liver stem cells. Dig Liver Dis. 2009;41:455–62. doi: 10.1016/j.dld.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Gaudio E, Marinozzi G, Carpino F, et al. Scanning electron microscopic stereo views of rat liver following bile duct ligation. Ultramicroscopy. 1980;5:420. [Google Scholar]
- 27.Carpino F, Gaudio E, Marinozzi G, et al. A scanning and transmission electron microscopic study of experimental extrahepatic cholestasis in the rat. J Submicrosc Cytol. 1981;13:581–98. [PubMed] [Google Scholar]
- 28.Benedetti A, Bassotti C, Rapino K, et al. A morphometric study of the epithelium lining the rat intrahepatic biliary tree. J Hepatol. 1996;24:335–42. doi: 10.1016/s0168-8278(96)80014-6. [DOI] [PubMed] [Google Scholar]
- 29.Masyuk TV, Ritman EL, LaRusso NF. Quantitative assessment of the rat intrahepatic biliary system by three-dimensional reconstruction. Am J Pathol. 2001;158:2079–88. doi: 10.1016/S0002-9440(10)64679-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roskams T, Van den Oord JJ, De Vos R, et al. Neuroendocrine features of reactive bile ductules in cholestatic liver disease. Am J Pathol. 1990;137:1019–25. [PMC free article] [PubMed] [Google Scholar]
- 31.Mancinelli R, Onori P, Gaudio E, et al. Follicle-stimulating hormone increases cholangiocyte proliferation by an autocrine mechanism via camp-dependent phosphorylation of ERK1/2 and Elk-1. Am J Physiol Gastrointest Liver Physiol. 2009;297:G11–26. doi: 10.1152/ajpgi.00025.2009. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Desmet V, Roskams T, Van Eyken P. Ductular reaction in the liver. Pathol Res Pract. 1995;191:513–24. doi: 10.1016/s0344-0338(11)80870-8. [DOI] [PubMed] [Google Scholar]
- 33.Sirica AE, Gainey TW, Mumaw VR. Ductular hepatocytes. Evidence for a bile ductular cell origin in furan-treated rats. Am J Pathol. 1994;145:375–83. [PMC free article] [PubMed] [Google Scholar]
- 34.Sirica AE. Biology of biliary epithelial cells. Prog Liver Dis. 1992;10:63–87. [PubMed] [Google Scholar]
- 35.LeSage G, Glaser S, Gubba S, et al. Regrowth of the rat biliary tree after 70% partial hepatectomy is coupled to increased secretin-induced ductal secretion. Gastroenterology. 1996;111:1633–44. doi: 10.1016/s0016-5085(96)70027-6. [DOI] [PubMed] [Google Scholar]
- 36.LeSage G, Glaser S, Ueno Y, et al. Regression of cholangiocyte proliferation after cessation of ANIT feeding is coupled with increased apoptosis. Am J Physiol Gastrointest Liver Physiol. 2001;281:G182–90. doi: 10.1152/ajpgi.2001.281.1.G182. [DOI] [PubMed] [Google Scholar]
- 37.Alpini G, Glaser S, Ueno Y, et al. Bile acid feeding induces cholangiocyte proliferation and secretion: evidence for bile acid-regulated ductal secretion. Gastroenterology. 1999;116:179–86. doi: 10.1016/s0016-5085(99)70242-8. [DOI] [PubMed] [Google Scholar]
- 38.LeSage G, Glaser S, Alpini G. Regulation of cholangiocyte proliferation. Liver. 2001;21:73–80. doi: 10.1034/j.1600-0676.2001.021002073.x. [DOI] [PubMed] [Google Scholar]
- 39.Francis H, Glaser S, Ueno Y, et al. cAMP stimulates the secretory and proliferative capacity of the rat intrahepatic biliary epithelium through changes in the PKA/Src/MEK/ERK1/2 pathway. J Hepatol. 2004;41:528–37. doi: 10.1016/j.jhep.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 40.Glaser S, Benedetti A, Marucci L, et al. Gastrin inhibits cholangiocyte growth in bile duct-ligated rats by interaction with cholecystokinin-b/gastrin receptors via d-myo-inositol 1,4,5-triphosphate-, Ca(2+)-, and protein kinase C alpha-dependent mechanisms. Hepatology. 2000;32:17–25. doi: 10.1053/jhep.2000.8265. [DOI] [PubMed] [Google Scholar]
- 41.Strazzabosco M, Fiorotto R, Melero S, et al. Differentially expressed adenylyl cyclase isoforms mediate secretory functions in cholangiocyte subpopulation. Hepatology. 2009;50:244–52. doi: 10.1002/hep.22926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minagawa N, Nagata J, Shibao K, et al. Cyclic AMP regulates bicarbonate secretion in cholangiocytes through release of ATP into bile. Gastroenterology. 2007;133:1592–602. doi: 10.1053/j.gastro.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alvaro D, Mancino MG, Glaser S, et al. Proliferating cholangiocytes: a neuroendocrine compartment in the diseased liver. Gastroenterology. 2007;132:415–31. doi: 10.1053/j.gastro.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 44.Slott PA, Liu MH, Tavoloni N. Origin, pattern, and mechanism of bile duct proliferation following biliary obstruction in the rat. Gastroenterology. 1990;99:466–77. doi: 10.1016/0016-5085(90)91030-a. [DOI] [PubMed] [Google Scholar]
- 45.Azmaiparashvili E, Kordzaia D, Dzidziguri D. Biliary hypertension as the cell proliferation trigger in bile duct ligated rats. Georgian Med News. 2009:111–6. [PubMed] [Google Scholar]
- 46.Alpini G, Glaser S, Ueno Y, et al. Heterogeneity of the proliferative capacity of rat cholangiocytes after bile duct ligation. Am J Physiol Gastrointest Liver Physiol. 1998;274:G767–75. doi: 10.1152/ajpgi.1998.274.4.G767. [DOI] [PubMed] [Google Scholar]
- 47.Marucci L, Alpini G, Glaser S, et al. Taurocholate feeding prevents CCl4-induced damage of large cholangiocytes through PI3-kinase-dependent mechanism. Am J Physiol Gastrointest Liver Physiol. 2003;284:G290–301. doi: 10.1152/ajpgi.00245.2002. [DOI] [PubMed] [Google Scholar]
- 48.Glaser S, DeMorrow S, Francis H, et al. Progesterone stimulates the proliferation of female and male cholangiocytes via autocrine/paracrine mechanisms. Am J Physiol Gastrointest Liver Physiol. 2008;295:G124–36. doi: 10.1152/ajpgi.00536.2007. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 49.Glaser S, Gaudio E, Miller T, et al. Cholangiocyte proliferation and liver fibrosis. Expert Rev Mol Med. 2009;11:e7. doi: 10.1017/S1462399409000994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marzioni M, Fava G, Benedetti A. Nervous and neuroendocrine regulation of the pathophysiology of cholestasis and of biliary carcinogenesis. World J Gastroenterol. 2006;12:3471–80. doi: 10.3748/wjg.v12.i22.3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tippins JR. CGRP: a novel neuropeptide from the calcitonin gene is the most potent vasodilator known. J Hypertens Suppl. 1986;4:S102–5. [PubMed] [Google Scholar]
- 52.Wimalawansa SJ. Calcitonin gene-related peptide and its receptors: molecular genetics, physiology, pathophysiology, and therapeutic potentials. Endocr Rev. 1996;17:533–85. doi: 10.1210/edrv-17-5-533. [DOI] [PubMed] [Google Scholar]
- 53.Glaser S, Ueno Y, DeMorrow S, et al. Knockout of alpha-calcitonin gene-related peptide reduces cholangiocyte proliferation in bile duct ligated mice. Lab Invest. 2007;87:914–26. doi: 10.1038/labinvest.3700602. [DOI] [PubMed] [Google Scholar]
- 54.Hou YF, Zhou YC, Zheng XX, et al. Modulation of expression and function of toll-like receptor 3 in A549 and H292 cells by histamine. Mol Immunol. 2006;43:1982–92. doi: 10.1016/j.molimm.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 55.Jancso G, Santha P, Horvath V, et al. Inhibitory neurogenic modulation of histamine-induced cutaneous plasma extravasation in the pigeon. Regul Pept. 2000;95:75–80. doi: 10.1016/s0167-0115(00)00140-3. [DOI] [PubMed] [Google Scholar]
- 56.Parsons ME, Ganellin CR. Histamine and its receptors. Br J Pharmacol. 2006;147(Suppl 1):S127–35. doi: 10.1038/sj.bjp.0706440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Francis H, Franchitto A, Ueno Y, et al. H3 histamine receptor agonist inhibits biliary growth of BDL rats by downregulation of the cAMP-dependent PKA/ERK1/2/Elk-1 pathway. Lab Invest. 2007;87:473–87. doi: 10.1038/labinvest.3700533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Drucker DJ. Glucagon-like peptides: regulators of cell proliferation, differentiation, and apoptosis. Mol Endocrinol. 2003;17:161–71. doi: 10.1210/me.2002-0306. [DOI] [PubMed] [Google Scholar]
- 59.Bulotta A, Hui H, Anastasi E, Bertolotto, et al. Cultured pancreatic ductal cells undergo cell cycle re-distribution and beta-cell-like differentiation in response to glucagon-like peptide-1. J Mol Endocrinol. 2002;29:347–60. doi: 10.1677/jme.0.0290347. [DOI] [PubMed] [Google Scholar]
- 60.Marzioni M, Alpini G, Saccomanno S, et al. Glucagon-like peptide-1 and its receptor agonist exendin-4 modulate cholangiocyte adaptive response to cholestasis. Gastroenterology. 2007;133:244–55. doi: 10.1053/j.gastro.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 61.Marzioni M, Alpini G, Saccomanno S, et al. Exendin-4, a glucagon-like peptide 1 receptor agonist, protects cholangiocytes from apoptosis. Gut. 2009;58:990–7. doi: 10.1136/gut.2008.150870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ulloa-Aguirre A, Uribe A, Zarinan T, et al. Role of the intracellular domains of the human FSH receptor in G(alphas) protein coupling and receptor expression. Mol Cell Endocrinol. 2007;260-262:153–62. doi: 10.1016/j.mce.2005.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Larrivee B, Karsan A. Signaling pathways induced by vascular endothelial growth factor. Int J Mol Med. 2000;5:447–56. doi: 10.3892/ijmm.5.5.447. review. [DOI] [PubMed] [Google Scholar]
- 64.Larrivee B, Lane DR, Pollet I, et al. Vascular endothelial growth factor receptor-2 induces survival of hematopoietic progenitor cells. J Biol Chem. 2003;278:22006–13. doi: 10.1074/jbc.M212158200. [DOI] [PubMed] [Google Scholar]
- 65.Gaudio E, Barbaro B, Alvaro D, et al. Vascular endothelial growth factor stimulates rat cholangiocyte proliferation via an autocrine mechanism. Gastroenterology. 2006;130:1270–82. doi: 10.1053/j.gastro.2005.12.034. [DOI] [PubMed] [Google Scholar]
- 66.Gaudio E, Barbaro B, Alvaro D, et al. Administration of r-VEGF-A prevents hepatic artery ligation-induced bile duct damage in bile duct ligated rats. Am J Physiol Gastrointest Liver Physiol. 2006;291:G307–17. doi: 10.1152/ajpgi.00507.2005. [DOI] [PubMed] [Google Scholar]
- 67.Marzioni M, Ueno Y, Glaser S, et al. Cytoprotective effects of taurocholic acid feeding on the biliary tree after adrenergic denervation of the liver. Liver Int. 2007;27:558–68. doi: 10.1111/j.1478-3231.2007.01443.x. [DOI] [PubMed] [Google Scholar]
- 68.Marzioni M, LeSage G, Glaser S, et al. Taurocholate prevents the loss of intrahepatic bile ducts due to vagotomy in bile duct-ligated rats. Am J Physiol Gastrointest Liver Physiol. 2003;284:G837–52. doi: 10.1152/ajpgi.00398.2002. [DOI] [PubMed] [Google Scholar]
- 69.Ueno Y, Francis H, Glaser S, et al. Taurocholic acid feeding prevents tumor necrosis factor-alpha-induced damage of cholangiocytes by a PI3k-mediated pathway. Exp Biol Med (Maywood) 2007;232:942–9. [PubMed] [Google Scholar]
- 70.Mancinelli R, Onori P, Gaudio E, et al. Taurocholate feeding to bile duct ligated rats prevents caffeic acid-induced bile duct damage by changes in cholangiocyte VEGF expression. Exp Biol Med (Maywood) 2009;234:462–74. doi: 10.3181/0808-RM-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jimenez W. Endocannabinoids and liver disease. Hepatology. 2005;41:983–5. doi: 10.1002/hep.20714. [DOI] [PubMed] [Google Scholar]
- 72.DeMorrow S, Francis H, Gaudio E, et al. Anandamide inhibits cholangiocyte hyperplastic proliferation via activation of thioredoxin 1/redox factor 1 and AP-1 activation. Am J Physiol Gastrointest Liver Physiol. 2008;294:G506–19. doi: 10.1152/ajpgi.00304.2007. [DOI] [PubMed] [Google Scholar]
- 73.Bartolazzi A, Nocks A, Aruffo A, et al. Glycosylation of CD44 is implicated in CD44-mediated cell adhesion to hyaluronan. J Cell Biol. 1996;132:1199–208. doi: 10.1083/jcb.132.6.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bajorath J. Molecular organization, structural features, and ligand binding characteristics of CD44, a highly variable cell surface glycoprotein with multiple functions. Proteins. 2000;39:103–11. [PubMed] [Google Scholar]
- 75.Mikami T, Saegusa M, Mitomi H, et al. Significant correlations of e-cadherin, catenin, and CD44 variant form expression with carcinoma cell differentiation and prognosis of extrahepatic bile duct carcinomas. Am J Clin Pathol. 2001;116:369–76. doi: 10.1309/VV6D-3GAH-VEJM-DUJT. [DOI] [PubMed] [Google Scholar]
- 76.Xu B, Broome U, Ericzon BG, et al. High frequency of autoantibodies in patients with primary sclerosing cholangitis that bind biliary epithelial cells and induce expression of CD44 and production of interleukin 6. Gut. 2002;51:120–7. doi: 10.1136/gut.51.1.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.He Y, Wu GD, Sadahiro T, et al. Interaction of CD44 and hyaluronic acid enhances biliary epithelial proliferation in cholestatic livers. Am J Physiol Gastrointest Liver Physiol. 2008;295:G305–12. doi: 10.1152/ajpgi.90229.2008. [DOI] [PubMed] [Google Scholar]
- 78.Alvaro D, Metalli VD, Alpini G, et al. The intrahepatic biliary epithelium is a target of the growth hormone/insulin-like growth factor 1 axis. J Hepatol. 2005;43:875–83. doi: 10.1016/j.jhep.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 79.Drudi Metalli V, Mancino MG, Mancino A, et al. Bile salts regulate proliferation and apoptosis of liver cells by modulating the IGF1 system. Dig Liver Dis. 2007;39:654–62. doi: 10.1016/j.dld.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 80.Gatto M, Drudi-Metalli V, Torrice A, et al. Insulin-like growth factor-1 isoforms in rat hepatocytes and cholangiocytes and their involvement in protection against cholestatic injury. Lab Invest. 2008;88:986–94. doi: 10.1038/labinvest.2008.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gil-Pena H, Garcia-Lopez E, Alvarez-Garcia O, et al. Alterations of growth plate and abnormal insulin-like growth factor I metabolism in growth-retarded hypokalemic rats: effect of growth hormone treatment. Am J Physiol Renal Physiol. 2009;297:F639–45. doi: 10.1152/ajprenal.00188.2009. [DOI] [PubMed] [Google Scholar]
- 82.Fouassier L, Rosenberg P, Mergey M, et al. Ezrin–radixin–moesin-binding phosphoprotein (ebp50), an estrogen-inducible scaffold protein, contributes to biliary epithelial cell proliferation. Am J Pathol. 2009;174:869–80. doi: 10.2353/ajpath.2009.080079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Takeda K, Kojima Y, Ikejima K, et al. Death receptor 5 mediated-apoptosis contributes to cholestatic liver disease. Proc Natl Acad Sci U S A. 2008;105:10895–900. doi: 10.1073/pnas.0802702105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sackett SD, Li Z, Hurtt R, et al. Foxl1 is a marker of bipotential hepatic progenitor cells in mice. Hepatology. 2009;49:920–9. doi: 10.1002/hep.22705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sackett SD, Gao Y, Shin S, et al. Foxl1 promotes liver repair following cholestatic injury in mice. Lab Invest. 2009;89:1387–96. doi: 10.1038/labinvest.2009.103. [DOI] [PubMed] [Google Scholar]
- 86.Wang B, Dolinski BM, Kikuchi N, et al. Role of alphavbeta6 integrin in acute biliary fibrosis. Hepatology. 2007;46:1404–12. doi: 10.1002/hep.21849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Patsenker E, Popov Y, Stickel F, et al. Inhibition of integrin alphavbeta6 on cholangiocytes blocks transforming growth factor-beta activation and retards biliary fibrosis progression. Gastroenterology. 2008;135:660–70. doi: 10.1053/j.gastro.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]


