Abstract
Background
Recently developed crowding measures, such as the Emergency Department (ED) Work Index (EDWIN) score, provide a quantifiable measurement of overcrowding in the ED.
Aims
We sought to determine the association between overcrowding, measured with the EDWIN score, and the time required to initiate percutaneous coronary intervention (PCI) for patients presenting to the ED with acute myocardial infarction (AMI).
Methods
We retrospectively reviewed the performance improvement (PI) data on all patients presenting to the ED over a 2-month period with chest pain and whose subsequent ECG showed AMI requiring PCI. We recorded the time from patient presentation to the (1) time to first ECG, (2) time to patient arrival in the catheterization laboratory, and (3) time to catheter balloon inflation. We calculated EDWIN scores using data archived from our electronic tracking board and compared the proportion of patients who achieved our established ED goal times between patients presenting during low crowding (EDWIN < 1.5) and high crowding (EDWIN ≥ 1.5) conditions.
Results
Seventeen patients underwent emergent PCI in the study period. Patients presenting to the ED during periods of low crowding had shorter times to balloon inflation (median of 84 min, IQR 80 to 93 min) than patients presenting to the ED during periods of high crowding (median of 107 min, IQR 94 to 122 min), P = 0.008. Times to first ECG and to arrival in the catheterization laboratory were not significantly different between patients presenting during low and high crowding conditions.
Conclusion
Overcrowding appears to be associated with a decreased likelihood of timely treatment for acute AMI in our ED.
Keywords: Overcrowding, Myocardial infarction, Edwin score, Treatment delays
Introduction
The Institute of Medicine issued a report in 2006 describing the precarious state of the emergency medical system as a whole, and little has improved since that time [1]. A primary cause of overcrowding in the emergency department (ED) is a lack of inpatient beds, leading to a back-up of patients awaiting them [2–10]. A recent meta-analysis found that ED overcrowding contributes to increased patient mortality, transport delays, treatment delays, ambulance diversion, and to patients leaving without being seen, among other problems [11].
Several recently developed crowding measures now provide a quantifiable measurement of overcrowding in the ED [12–22]. One of these metrics, the ED Work Index (EDWIN) score, correlates with an active but manageable ED when the EDWIN score is less than 1.5, a busy ED when the EDWIN score is between 1.5 and 2, and a crowded ED when the EDWIN score is greater than 2 [16].
Previous studies of the effects of overcrowding on times to treat acute myocardial infarction (AMI) have produced differing results. One study of percutaneous coronary intervention (PCI) found no significant associations when summary data from a large number of academic hospitals were analyzed [23]. A study of delays in thrombolysis showed that ED crowding is associated with increased door-to-needle times [24]. To investigate the effects of crowding in our single community teaching hospital, we sought to measure associations between crowding and time to treat STEMI with PCI in our ED, hypothesizing that increasing EDWIN scores would correlate positively with increased times to achieve PCI.
Methods
Study design, setting, and population
We performed a retrospective review of the performance improvement (PI) data on all patients presenting to the ED during the first 2 months of 2007 with chest pain and whose subsequent ECG showed STEMI requiring PCI. The study was performed at our large tertiary-care suburban community teaching hospital, which has an annual ED census of approximately 85,000 patients. We included in this study all patients presenting to the ED with an ECG showing STEMI or new left bundle-branch block requiring emergent activation of the catheterization team for performance of PCI. The hospital’s institutional review board approved the study with a waiver of informed consent.
Study protocol
Our ED has a protocol in place, referred to as a “Code 60,” for activation of the catheterization laboratory by the ED when urgent PCI is required for STEMI; the use of the number 60 refers to our goal in minutes for the time from patient presentation in the ED to arrival of the patient in the catheterization laboratory. Additional goals include 10 min from the time of patient presentation to the time of ECG acquisition and 90 min from the time of patient presentation to PCI balloon inflation.
At all activations of our Code 60 protocol, the unit secretary begins entries on a data collection sheet that is used by the PI committee to improve efforts to reach goals. The data collection sheet is used to record the time of patient presentation to the ED, along with times to first ECG, contact with the on-call cardiologist, arrival of the patient to the catheterization laboratory, and inflation of the PCI balloon. Data collection sheets are maintained by the PI committee chairman.
At the time of this study we did not have access to a real-time EDWIN score, so we calculated scores based on available data archived from our electronic tracking board.
Measurements
We reviewed the Code 60 data collection sheets and recorded the time from patient presentation to (1) the time to first ECG, (2) the time to patient arrival in the catheterization laboratory, and (3) the time to PCI catheter balloon inflation. The study authors served as abstractors and agreed on the values of all available data points, but the authors were not blinded to study purpose.
We calculated EDWIN scores using data archived from our electronic tracking board; these data were available for our analysis for the months of January and February of 2007, and were stored on a remote server used for administrative purposes. The EDWIN score is defined as Σniti/Na(BT-BA), where ni = number of patients in the ED in triage category i, ti = triage category, Na = number of attending physicians on duty, BT = number of treatment bays, and BA = number of admitted patients in the ED. Triage category is defined by the Emergency Severity Index (ESI)[25], which is in widespread use in North America; in order to assign higher numerical values to higher severity patients, the ESI is reversed from the standard ordinal ranking of triage categories so that ESI level-1 patients, who have the highest acuity, are assigned a value of 5, ESI level-2 patients are given a value of 4, continuing down to ESI level-5 patients (lowest acuity) being assigned a value of 1. The archived data were obtained from our electronic tracking board sampled at 20-min intervals and included the total number of patients in the ED, their location in the ED, and the number of admitted patients in the ED. Because the ESI score assigned to each patient was not archived, we assigned ESI scores to patients by geographic location based on average values typically encountered in each location of our ED and took the reverse of the score to obtain the required value for calculation of the EDWIN score. Thus, patients were assigned average acuity scores as follows: patients in the critical care section of the ED, 4.5; patients in the chest pain unit, 3.5; patients in the general care section, 3; fast track patients, 2; and pediatric section patients, 2.5. The total number of licensed beds in our ED is 50, and the number of attendings working in the ED was obtained from our departmental schedule. The total number of attendings working in the ED at any given time varies from a low of 2 to a high of 8.
Data analysis
Descriptive data are reported with means and 95% confidence intervals (CIs) as well as medians and interquartile ranges (IQRs) to provide greater descriptive analysis of data with small sample sizes. To facilitate comparisons, we divided the EDWIN scores into two groups, low crowding (less than 1.5) and high crowding (greater than or equal to 1.5), and compared the times to arrival in the catheterization laboratory and times to balloon inflation between patients presenting to the ED during periods of low crowding and patients presenting during periods of high crowding. The Mann-Whitney U test was used to provide more robust and less biased analysis of data with smaller sample sizes. We entered all of our data into an Excel spreadsheet (Microsoft) in order to perform the necessary calculations and performed further analysis with SPSS version 15.0 (SPSS Inc., Chicago, IL).
Results
Site characteristics
Seventeen patients underwent emergent PCI in the 2-month study period. The mean EDWIN score at the time of each procedure was 1.3 (95% CI for the mean: 0.9 to 1.7) with a median of 1.0 (IQR 0.8 to 1.9). The mean time from patient presentation to arrival in the catheterization laboratory was 71 min (95% CI for the mean: 54 to 88 min) with a median of 64 min (IQR 58 to 82 min). The mean time from patient presentation to balloon inflation was 93 min (95% CI for the mean: 83 to 102 min) with a median of 88 min (IQR 82 to 101 min). Seven patients arrived in the catheterization laboratory within 60 min, and 8 patients had catheter balloon inflation within 90 min. Three patients did not undergo balloon inflation, either because of diffuse disease requiring bypass grafting or because no lesion requiring angioplasty was identified.
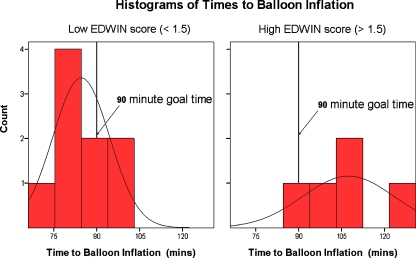
Crowding comparison: balloon inflation time
Patients presenting to the ED during periods of low crowding (EDWIN < 1.5) had shorter times to balloon inflation, with a mean of 85 min (95% CI for the mean: 77 to 92 min) and median of 84 min (IQR 80 to 93 min) when compared to patients presenting to the ED during periods of high crowding (EDWIN ≥ 1.5), with a mean of 107 min (95% CI for the mean: 88 to 127 min) and median of 107 min (IQR 94 to 122 min), shown in Fig. 1. This difference was statistically significant, with P = 0.008 (Mann-Whitney U test). Table 1 summarizes these and the following results.
Fig. 1.
Comparison of time to catheter balloon inflation during periods of low and high crowding conditions
Table 1.
Mean times to ECG, catheter laboratory, and balloon inflation during low and high EDWIN scores
| Mean time (minutes) | EDWIN <1.5 | EDWIN ≥ 1.5 | P value |
|---|---|---|---|
| To first ECG | 4 | 12 | 0.06 |
| To catheter lab | 63 | 85 | 0.44 |
| To balloon inflation | 85 | 107 | 0.008 |
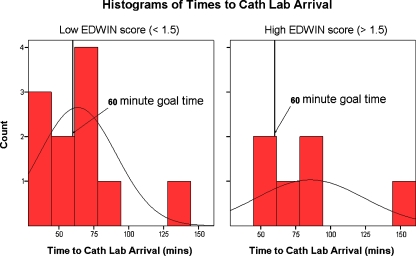
Crowding comparison: catheterization laboratory arrival time
Time from presentation to arrival in the catheterization laboratory for patients presenting to the ED during periods of low crowding was 63 min (95% CI for the mean: 45 to 82 min) with a median of 62 min (IQR 44 to 69 min), compared to patients presenting to the ED during periods of high crowding, who had a mean of 85 min (95% CI for the mean: 45 to 126 min) and median of 76 min (IQR 58 to 103 min); however, this difference (Fig. 2) did not reach statistical significance, with P = 0.44 (Mann-Whitney U test).
Fig. 2.
Comparison of time to catheterization laboratory arrival during periods of low and high crowding conditions
Crowding comparison: time to first ECG
Likewise, we did not see a statistically significant difference between times from patient presentation to acquisition of first ECG during high and low crowding; the mean time to first ECG during low crowding was 12 min (95% CI for the mean: 3 to 20 min) with a median of 9 min (IQR 3 to 13 min), while the mean time to first ECG during high crowding was 4 min (95% CI for the mean: 1 to 6 min) with a median of 4 min (IQR 1 to 5 min), P = 0.06 (Mann-Whitney U test).
Discussion
Our analysis suggests that overcrowding may indeed be associated with increased times to achieve the important end-point of catheter balloon inflation during PCI for the treatment of acute STEMI. This is perhaps not unexpected, given the increasing number of adverse effects related to overcrowding being discovered [4, 9, 11, 23, 24, 26–38].
An earlier study of the effect of overcrowding on the treatment of AMI with thrombolysis showed that ED crowding is associated with increased door-to-needle times, with a delay of almost 6 min in high crowding conditions [24]. In contrast, a multi-site study at academic medical centers found that PCI timing for patients with acute myocardial infarction was not associated with crowding; however, the main crowding metrics in this study were patient length of stay and turnaround time for chest X-rays, which may limit sensitivity [23].
We did not see statistically significant associations between crowding and time to the first ECG or time to patient arrival in the catheterization laboratory, although crowding was associated with a non-statistically significant increase in the point-estimates of mean times to arrival in the catheterization laboratory. It is perhaps likely that overcrowding affects multiple steps of a complex process, such as activation of emergent treatment of acute STEMI with PCI, and that a minor delay in many of the steps may have a cumulative effect in the overall time to complete the process. A cumulative effect would result in potentially non-statistically significant differences in the early steps of the process, with statistical significance reached at later steps of the process. Although the final step of our protocol, catheter balloon inflation, occurs outside the ED, the increasing realization that ED overcrowding is in fact caused by hospital-wide factors lends support to the hypothesis that factors contributing to hospital crowding continue to affect patient care even outside the ED. For example, increased workloads and patient volumes may in turn affect the availability of personnel as well as equipment when patients with sudden emergent conditions require treatment. Even prior to hospital arrival, overcrowding has been shown to be associated with delays in patient transport [32].
Limitations
Our study relied on retrospective data analysis, a methodology that has well-known limitations. Our department takes great care to obtain accurate recordings of times on our Code 60 data sheets, but the possibility remains that inaccurate data may affect our results.
Our study was also limited by the amount of archived data available to calculate EDWIN scores; we were not able to obtain data for an additional month to increase our sample size. The retrospective calculation of EDWIN scores introduces potential error, although we believe that the uniform calculation method we applied is unlikely to introduce significant bias.
Although we found an association between crowding and the time required to complete emergent PCI in our ED, the observational nature of our study precludes our attributing the cause of these treatment delays to overcrowding.
Conclusion
Overcrowding appears to be associated with a decreased likelihood of timely treatment for acute STEMI in our ED. Although the ability to attribute the cause of increased treatment times to overcrowding is limited by the observational nature of our study, these results raise further concerns over hospital overcrowding being associated with potentially harmful delays in patient care.
Biographies
Erik Kulstad is the Research Director for the Department of Emergency Medicine at Advocate Christ Medical Center in Oak Lawn, Illinois, with appointment as Clinical Assistant Professor through the Department of Emergency Medicine at the University of Illinois, Chicago.
Ken Kelley is a third-year resident in the Department of Emergency Medicine at Advocate Christ Medical Center in Oak Lawn, Illinois.
Footnotes
No financial support was provided for this study.
The views expressed in this paper are those of the author(s) and not those of the editors, editorial board or publisher.
References
- 1.Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: Institute of Medicine (US) Committee on the Future of Emergency Care in the United States Health System; 2006 [DOI] [PubMed]
- 2.Steele R, Kiss A. EMDOC (Emergency Department overcrowding) Internet-based safety net research. J Emerg Med. 2008;35(1):101–107. doi: 10.1016/j.jemermed.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 3.Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68. doi: 10.1016/S0196-0644(00)70105-3. [DOI] [PubMed] [Google Scholar]
- 4.Gilligan P, Winder S, Singh I, et al. The Boarders in the Emergency Department (BED) study. Emerg Med J. 2008;25(5):265–269. doi: 10.1136/emj.2007.048173. [DOI] [PubMed] [Google Scholar]
- 5.Gordon JA, Billings J, Asplin BR, et al. Safety net research in emergency medicine: proceedings of the Academic Emergency Medicine Consensus Conference on “The Unraveling Safety Net”. Acad Emerg Med. 2001;8(11):1024–1029. doi: 10.1111/j.1553-2712.2001.tb01110.x. [DOI] [PubMed] [Google Scholar]
- 6.Hwang U, Concato J. Care in the emergency department: how crowded is overcrowded? Acad Emerg Med. 2004;11(10):1097–1101. doi: 10.1111/j.1553-2712.2004.tb00686.x. [DOI] [PubMed] [Google Scholar]
- 7.Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006;355(13):1300–1303. doi: 10.1056/NEJMp068194. [DOI] [PubMed] [Google Scholar]
- 8.Kunz Howard P. Overcrowding: not just an emergency department issue. J Emerg Nurs. 2005;31(3):227–228. doi: 10.1016/j.jen.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Olshaker JS, Rathlev NK. Emergency Department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the Emergency Department. J Emerg Med. 2006;30(3):351–356. doi: 10.1016/j.jemermed.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 10.Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20(5):402–405. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–136. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asplin BR, Flottemesch TJ, Gordon BD. Developing models for patient flow and daily surge capacity research. Acad Emerg Med. 2006;13(11):1109–1113. doi: 10.1111/j.1553-2712.2006.tb01632.x. [DOI] [PubMed] [Google Scholar]
- 13.Asplin BR. Measuring crowding: time for a paradigm shift. Acad Emerg Med. 2006;13(4):459–461. doi: 10.1111/j.1553-2712.2006.tb00326.x. [DOI] [PubMed] [Google Scholar]
- 14.Asplin BR, Magid DJ, Rhodes KV, et al. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42(2):173–180. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 15.Asplin BR, Rhodes KV, Flottemesch TJ, et al. Is this emergency department crowded? A multicenter derivation and evaluation of an emergency department crowding scale (EDCS) Acad Emerg Med. 2004;11(5):484. doi: 10.1197/j.aem.2004.02.378. [DOI] [Google Scholar]
- 16.Bernstein SL, Verghese V, Leung W, et al. Development and validation of a new index to measure emergency department crowding. Acad Emerg Med. 2003;10(9):938–942. doi: 10.1111/j.1553-2712.2003.tb00647.x. [DOI] [PubMed] [Google Scholar]
- 17.Hoot NR, Zhou C, Jones I, et al. Measuring and forecasting emergency department crowding in real time. Ann Emerg Med. 2007;49(6):747–755. doi: 10.1016/j.annemergmed.2007.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones SS, Allen TL, Flottemesch TJ, et al. An independent evaluation of four quantitative emergency department crowding scales. Acad Emerg Med. 2006;13(11):1204–1211. doi: 10.1111/j.1553-2712.2006.tb01649.x. [DOI] [PubMed] [Google Scholar]
- 19.Raj K, Baker K, Brierley S, et al. National Emergency Department Overcrowding Study tool is not useful in an Australian emergency department. Emerg Med Australas. 2006;18(3):282–288. doi: 10.1111/j.1742-6723.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- 20.Weiss SJ, Ernst AA, Nick TG. Comparison of the National Emergency Department Overcrowding Scale and the Emergency Department Work Index for quantifying emergency department crowding. Acad Emerg Med. 2006;13(5):513–518. doi: 10.1111/j.1553-2712.2006.tb01001.x. [DOI] [PubMed] [Google Scholar]
- 21.Epstein SK, Tian L. Development of an emergency department work score to predict ambulance diversion. Acad Emerg Med. 2006;13(4):421–426. doi: 10.1111/j.1553-2712.2006.tb00320.x. [DOI] [PubMed] [Google Scholar]
- 22.Weiss SJ, Ernst AA, Sills MR, et al. Development of a novel measure of overcrowding in a pediatric emergency department. Pediatr Emerg Care. 2007;23(9):641–645. doi: 10.1097/PEC.0b013e31814a69e2. [DOI] [PubMed] [Google Scholar]
- 23.Pines JM, Hollander JE, Localio AR, et al. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006;13(8):873–878. doi: 10.1111/j.1553-2712.2006.tb01741.x. [DOI] [PubMed] [Google Scholar]
- 24.Schull MJ, Vermeulen M, Slaughter G, et al. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44(6):577–585. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Wuerz RC, Milne LW, Eitel DR, et al. Reliability and validity of a new five-level triage instrument. Acad Emerg Med. 2000;7(3):236–242. doi: 10.1111/j.1553-2712.2000.tb01066.x. [DOI] [PubMed] [Google Scholar]
- 26.Sun BC, Binstadt ES, Pelletier A, et al. Characteristics and temporal trends of “left before being seen” visits in US Emergency Departments, 1995–2002. J Emerg Med. 2007;32(2):211–215. doi: 10.1016/j.jemermed.2006.05.045. [DOI] [PubMed] [Google Scholar]
- 27.Asaro PV, Lewis LM, Boxerman SB. Emergency department overcrowding: analysis of the factors of renege rate. Acad Emerg Med. 2007;14(2):157–162. doi: 10.1111/j.1553-2712.2007.tb01760.x. [DOI] [PubMed] [Google Scholar]
- 28.Kelen GD, Scheulen JJ, Hill PM. Effect of an emergency department (ED) managed acute care unit on ED overcrowding and emergency medical services diversion. Acad Emerg Med. 2001;8(11):1095–1100. doi: 10.1111/j.1553-2712.2001.tb01122.x. [DOI] [PubMed] [Google Scholar]
- 29.Polevoi SK, Quinn JV, Kramer NR. Factors associated with patients who leave without being seen. Acad Emerg Med. 2005;12(3):232–236. doi: 10.1111/j.1553-2712.2005.tb00874.x. [DOI] [PubMed] [Google Scholar]
- 30.Weiss SJ, Ernst AA, Derlet R, et al. Relationship between the National ED Overcrowding Scale and the number of patients who leave without being seen in an academic ED. Am J Emerg Med. 2005;23(3):288–294. doi: 10.1016/j.ajem.2005.02.034. [DOI] [PubMed] [Google Scholar]
- 31.Fordyce J, Blank FS, Pekow P, et al. Errors in a busy emergency department. Ann Emerg Med. 2003;42(3):324–333. doi: 10.1016/S0196-0644(03)00398-6. [DOI] [PubMed] [Google Scholar]
- 32.Schull MJ, Morrison LJ, Vermeulen M, et al. Emergency department overcrowding and ambulance transport delays for patients with chest pain. Cmaj. 2003;168(3):277–283. [PMC free article] [PubMed] [Google Scholar]
- 33.Fatovich DM, Hirsch RL. Entry overload, emergency department overcrowding, and ambulance bypass. Emerg Med J. 2003;20(5):406–409. doi: 10.1136/emj.20.5.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clements A, Halton K, Graves N, et al. Overcrowding and understaffing in modern health-care systems: key determinants in meticillin-resistant Staphylococcus aureus transmission. The Lancet infectious diseases. 2008;8(7):427–434. doi: 10.1016/S1473-3099(08)70151-8. [DOI] [PubMed] [Google Scholar]
- 35.Cameron PA. Hospital overcrowding: a threat to patient safety? Managing access block involves reducing hospital demand and optimising bed capacity. Med J Aust. 2006;184(5):203–204. doi: 10.5694/j.1326-5377.2006.tb00200.x. [DOI] [PubMed] [Google Scholar]
- 36.Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184(5):213–216. doi: 10.5694/j.1326-5377.2006.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 37.Sprivulis PC, Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184(5):208–212. doi: 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 38.McMullan JT, Veser FH. Emergency department volume and acuity as factors in patients leaving without treatment. South Med J. 2004;97(8):729–733. doi: 10.1097/00007611-200408000-00006. [DOI] [PubMed] [Google Scholar]