Abstract
Using Union Army veterans’ lifetime socioeconomic and health records, this essay finds a consistent and persistent hierarchy in survival rates and hazard ratios by urban size at and across three stages of life: birth, late adolescence, and death. This urban mortality penalty remains after controlling for variables associated with each individual veteran. The results of our geographical mobility analyses suggest that, with respect to these veterans, the search for an explanation should focus on late adolescence and adulthood as much as on early life. A complete explanation of the penalty requires a project of greater scope.
Keywords: urban mortality penalty, cohort analysis, survival rate, hazard ratio, mobility
Although it is widely known that, during the 19th century, life expectancy was substantially lower in cities than in rural areas, the differences in survival rates and proportional hazard ratios across urban sizes and rural environments are less well understood.1 Further, the longitudinal impact of lifetime mobility on life expectancy during this period rarely has been studied.
This essay examines these less explored subjects using historical data from Union Army veterans’ lifetime socioeconomic and health records collected by the Center for Population Economics (CPE). In particular, using veterans who survived the Civil War, survival rates and hazard ratios are estimated for different urban size and rural environmental categories at three stages of life: birth, late adolescence, and death. We also exploit the association with the local malaria ecology to differentiate rural areas.
Our analyses show a persistent urban mortality penalty for all three stages of life even after controlling for health-related events incurred during the Civil War and those incurred by contracting a chronic health condition by 1875. This supports the idea that individuals are exposed to “insults” that eventually reduce their life expectancy.2 The results of our geographical mobility analyses suggest that, with respect to these veterans, the search for an explanation should focus on late adolescence and adulthood as much as on early life. The data permit us to document the magnitude of this urban mortality penalty. It persists after the inclusion of all our explanatory variables. While we cannot yet explain why it occurred, we are able to narrow the search for an explanation.
There is a well-developed literature on urban versus rural mortality rates. Vinovskis, correcting the earlier work of Jaffe and Lourie, found that, in Massachusetts towns with an 1830 population of 10,000 or more, life expectancy at ages 10 to 14 was 46.7 years. In towns with less than 1,000 inhabitants, it was 52.5 years.3
In 1900, the U.S. Bureau of the Census created an official Death Registration Area (DRA) which included ten states and the District of Columbia. Using the DRA, it was estimated that white males born in rural areas had a life expectancy at birth in 1901 that was ten years higher than that for white males born in cities. For white females, life expectancy at birth was seven years higher in rural areas than in cities.4 For blacks, male and female, in the District of Columbia, life expectancy at birth was about four years less than it was for the DRA as a whole.5 As late as 1939, actuaries for the Metropolitan Life Insurance Company reported life expectancy at birth for white males was 64.07 years in rural areas as compared to 61.45 years in urban areas. For white females, the figures were 67.46 and 66.20 years, respectively. Although a small urban penalty remained, differences by urban size had largely disappeared for whites, but they persisted for blacks.6
With the aid of the Union Army database, we can look at the urban mortality penalty in several ways.7 Survival rates and proportional hazard ratios will be used in this analysis, as will age-specific mortality rates to a lesser extent. Given the data, we are able to define survival rates for a large number of veterans. These rates compare the number of veterans alive in 1900 to those alive in 1866. The data reveal a hierarchical pattern of rates with the largest cities having the lowest rate. This hierarchy is also visible in the age-specific mortality rates. Then, Cox proportional hazard ratios are estimated for a smaller number of individuals for whom we have a death date. The largest cities have the highest ratios, but, even after including a relatively large number of control variables from each individual’s record (e.g., insults to their health during and shortly after the Civil War), the urban mortality penalty is still present in the data.
As a first step, we identified 25,044 men who did not desert and survived the Civil War. We have death records for 17,950 of this group. Of the remaining 7,094 individuals, we can locate 1,173 in the post-1900 Union Army pension records where information from the veterans’ regular medical examinations can be found. Finally, of the 5,921 that remain, we looked to see if they could be linked to the 1900 Census. This gives us the ability to construct an 1866-1900 survival rate by dividing the number of veterans in any class we can ascertain were alive in 1900 by those we know survived the Civil War.8 It is important to keep in mind that this is not the survival rate of the male cohort born circa 1840. This is the survival rate of a group of men healthy enough to be inducted into the Union Army and lucky enough to survive the insults of battle and disease during the War.9
We begin by defining six mutually exclusive areas. The urban places are classified into four groups on the basis of population size in the 1860 census.10 Together they include 94 of the 100 largest cities in 1860.11 Rural areas are classified into two groups on the basis of the estimated probability of contracting malarial fever (remittent or intermittent fever as broadly called by 19th-century physicians).12
The malaria risk was estimated by looking at county level environmental factors.13 A high-malaria area was one with an estimated risk of 0.25 or greater, while a low-malaria area had a risk below 0.25.14 The South had a more malarial environment than the North, which means there are comparatively few Union Army veterans from high-malaria areas. Nevertheless, malaria was much more widespread geographically in the nineteenth century than it is today, extending as far north as Madison, WI.
Table 1 presents the survival rates of Union Army veterans according to where they were born and where they resided in 1860. About half the veterans in 1860 resided in the place where they were born. The survival rate is the percentage of non-deserting veterans in each group who survived the war and lived to at least 1900. Since the average veteran was born in 1839, this is essentially the proportion of veterans who survived into their early 60s. These rates clearly reveal an urban mortality penalty.
Table 1.
Survival Rate of Union Army Veterans by Birthplace and 1860 Residence
| Type of Place | Classification | Sample Size | Average birth year | Survival Rate * 100 (1866-1900) |
|---|---|---|---|---|
| Birthplace | U.S. Urban | 1,613 | 1839.6 | 49.10 |
| Urban 1 | 852 | 1839.4 | 44.01 | |
| Urban 2 | 146 | 1840.1 | 47.26 | |
| Urban 3 | 216 | 1840.2 | 54.63 | |
| Urban 4 | 399 | 1839.7 | 57.64 | |
| U.S. Rural | 12,604 | 1839.1 | 63.91 | |
| High-Malaria | 2,187 | 1839.4 | 62.19 | |
| Low-Malaria | 10,417 | 1839.0 | 64.27 | |
| Foreign | 5,951 | 1835.2 | 35.14 | |
| Unknown | 4,876 | 1837.4 | 39.46 | |
| Residence in 1860 | U.S. Urban | 530 | 1835.2 | 37.55 |
| Urban 1 | 235 | 1833.4 | 30.64 | |
| Urban 2 | 34 | 1835.9 | 47.06 | |
| Urban 3 | 75 | 1837.9 | 42.67 | |
| Urban 4 | 186 | 1836.2 | 42.47 | |
| U.S. Rural | 7,674 | 1837.7 | 60.53 | |
| High-Malaria | 1,203 | 1838.2 | 58.94 | |
| Low-Malaria | 6,471 | 1837.7 | 60.83 | |
| Unknown | 285 | 1836.9 | 62.46 | |
Notes: The survival rate is the percentage of veterans in each group who survived the war and then lived to at least 1900. See the text for the classification of urban and rural places.
In terms of birthplace, on average, 49.1 % of the veterans born in urban places who survived the war lived to 1900. The percent surviving for those born in rural places is 14.8 percentage points greater. Foreign-born veterans had the lowest survival rate when sorted by place of birth (35.1%), but they are four to five years older than non-foreign born veterans. As will be shown in the next section, when the birth year is taken into consideration, the experience of the foreign-born appears less dire. Immigration into large cities has been proffered as a partial explanation for the urban mortality penalty, but, when we exclude foreign-born veterans, the penalty is still present.15
Veterans belonging to the Urban 1 group (cities with 1860 populations greater than 100,000) had the lowest survival rate, followed by those living in Urban 2 (populations between 50,000 and 100,000). Urban 3 and 4 (populations between 25,000 and 50,000 and between 9,552 and 25,000) had approximately equal rates, higher than larger urban areas, but lower than any rural place. By a relatively slim margin, those with a low-malaria rural birthplace had a slightly higher survival rate than those from a high-malaria one. Those with unknown birthplaces had low survival rates, with only foreign birthplaces lower.
The sample sizes for the lower panel are much smaller due to the necessity of linking the Union Army database to the 1860 Census; the urban mortality penalty is larger. The inclusion of information concerning residence in 1860 reduces the sample size by roughly two-thirds, from 25,044 to approximately 8,489.
With respect to the lower panel, Table 1 again reveals considerable variability within the urban strata. Veterans belonging to the Urban 1 group had the lowest survival rate. Those living in Urban 2 had a relatively high survival rate, but, given the small size of the Urban 2 sample, this rate may be less accurately measured than the others. Urban 3 and 4 had approximately equal rates. All four urban survival rates are lower than rural places.
Of veterans who resided in Urban 1 in 1860 and who survived the war, only about 31% survived to 1900. This is consistent with a population belonging to a life table with ℮o (life expectancy at birth) = 27.2. By contrast, 61% of veterans who lived in all rural areas combined in 1860 and survived the war lived to 1900. This is consistent with a population belonging to a life table with ℮o = 46.7.16
As a second step, we examined the urban mortality penalty at the city level based on a veteran’s birthplace. This is the only analysis we’ve undertaken at the city level; all the others are at the level of the individual veteran.17 We calculated a survival rate for each city where we could find at least six non-deserting veterans born in that city who survived the war. As in Table 1, the city survival rate is calculated as the number of survivors in 1900 divided by the total number of surviving veterans who never deserted. Figure 1 presents two graphs of these survival rates versus population and population density, respectively, for those cities among the 100 largest in 1860. As is immediately apparent in the left-hand panel, the larger cities, those with the open circles, tend to be among the lowest in terms of survival rates. The right-hand panel reveals there is also a downward-sloping relationship between survival rates and population density. In both figures, the difference between best and worst is approximately 20 percentage points; this is consistent with what was found in Table 1.
Figure 1. Aggregate Urban Mortality Penalty by City Population Size and Population Density.
Notes: Out of 100 population cities in 1860, we selected the cities where more than 6 veterans were born and survived the Civil War. Population size in the panel on the left is log-scaled. City population density in the panel on the right is measured as population per square mile.
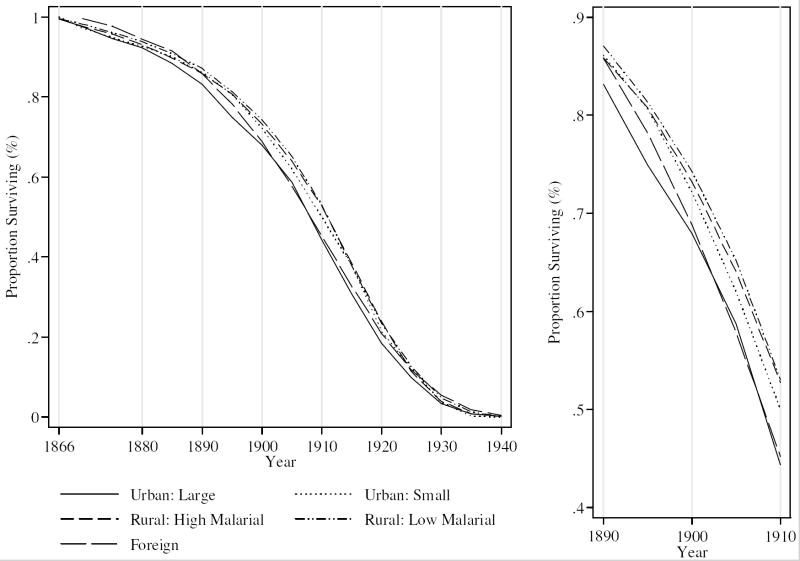
Finally, we limited the data to those veterans we could find in the death records to minimize sample selection problems. Then we looked at survival rates across the years according to five possible birthplaces, three less than in Table 1. We have collapsed Urban 1 and Urban 2 into Urban: Large, and the second two urban areas into Urban: Small. Rural areas remain split into two groups, with a malaria risk of 0.25 still being the dividing point. The main reason for reducing the number of study areas is that the Union Army sample is biased toward rural areas, and given the need to link veterans to the 1860 Census in the larger analysis, we are concerned about sample size. In Figure 2, the survival rates to particular years have been graphed, with an adjustment of four years for the foreign born reflecting their earlier birth dates. The panel on the right provides an enlarged view of the period around 1900. Again, the urban mortality penalty is readily apparent. The difference in survival rates between Urban: Large and Rural: Low Malarial is 6.3 percentage points (= 74.3 – 68.0).
Figure 2. Observed Survival Curves by Type of Birthplace.
Notes: The survival curves were made for the veterans who survived the Civil War and whose death years are currently known. The panel on the right provides an enlarged view of the period around 1900.
Before 1890 when the law creating a service pension was passed, disability pensions were awarded to those who were severely injured and impaired during the Civil War. Many veterans were not eligible for a pension initially, and may not have been able to apply under the service pension law, especially if they died before 1890. Most of the information about death places is found in the pension records. Since many veterans did not enter the pension system until after 1890, the sample found in the death records is more representative of those veterans who survived to at least 1890 and could apply for a service pension than it is of all veterans. In consequence, the survival rates observed in Figure 2 are higher than those in Table 1 – especially for urban strata. The survival rate gap between urban and rural environments is lower than that found in Table 1. The results in Figure 2 and the following sections should be considered in the light of this selection issue.
To investigate the urban mortality penalty in greater depth, we use a Cox proportional hazard model that specifies the hazard for veteran i as λi(t) = λ0(t)×exp(Xiβ), where λ0(t) is the hazard in a group at time t. The group is non-deserting veterans who survived the Civil War and reside in the specified type of area; time is measured as years since 1865. Xi is an n × p matrix that includes p components associated with each of n veterans. The β’s are the estimated log hazard ratios, the multiplier by which the hazard is increased or decreased with a unit change in the associated component of X as compared to the reference group.18 The estimated hazard ratio is based on a year-by-year evaluation of the data; the survival rate, on a comparison of two years, 1866 and 1900. Consequently, we believe the Cox specification provides more reliable results.
As a first step, we estimated hazard ratios reflecting a veteran’s birthplace, residence in 1860, and death place for all four urban areas, with simply “Rural” as the reference group, the omitted category. We also included the veteran’s birth year in this regression to control for age; the results are reported in Table 2. Standard errors are reported below each coefficient; conventional tests of whether a coefficient is statistically significantly different from one are reported by asterisks. As a rough rule of thumb, a 0.01 difference in a hazard ratio is equal to approximately 45 days of life; a 0.1 difference is equal to approximately 1.2 years. The first column is similar to Table 1 and Figure 2, but the inclusion of birth year shows a reduced hazard (higher survival) for the foreign born.
Table 2.
Cox Hazard Ratio of Union Army Veterans by Type of Places at Birth, in 1860, and at Death
| Dependent Variable: Years to Death after the Civil War (1865) | |||
|---|---|---|---|
| Variables | Type of Place |
||
| Birthplace | Residence in 1860 | Death Place | |
| Urban 1 | 1.2244*** (0.0242) | 1.4568*** (0.1315) | 1.5518*** (0.0670) |
| Urban 2 | 1.3502*** (0.1357) | 1.5573** (0.3123) | 1.4777*** (0.1056) |
| Urban 3 | 1.1416* (0.0907) | 1.1663 (0.1553) | 1.0867 (0.0653) |
| Urban 4 | 1.1401** (0.0669) | 1.3821*** (0.1203) | 1.1429*** (0.0476) |
| Foreign | 1.1719*** (0.0242) | ||
| U.S. Rural | Omitted | Omitted | Omitted |
| Birth Year | 0.9234*** (0.0011) | 0.9238*** (0.0016) | 0.9200*** (0.0013) |
| LR χ2 (p-value) | 3969.5 (0.000) | 1890.3 (0.000) | 3290.0 (0.000) |
| n | 14,492 | 6,569 | 11,922 |
Notes: The Cox regressions are conducted only for the veterans whose death years and the place of birth, 1860 residence or death place are known. The survival time in the regression is defined as the duration to death from the end of the Civil War. Standard errors are reported in parentheses. Single asterisk denotes statistical significance at the 90% level of confidence, double 95%, triple 99%.
As can be seen, the hazard ratios for the two larger urban classes and the two smaller urban classes are similar. The former two are larger than the smaller two, and the foreign born fall between them. All are larger than rural places, the reference group in each case. The hazard ratios increase over the three periods for Urban 1, but for the other three, they first increase, then decrease. The lowest ratio is that of Urban 3 for death places, and that is still more than eight points higher than a rural death place. Again, it should also be noted that the sample size for 1860 residence is lower than the other two because of the need to link the Union Army sample to the 1860 Census.19
Our larger analysis involves as much information as we have on a veteran’s life cycle in the CPE database. The first panel of Table 3 repeats the exercise in Table 2, but, following Figure 2, Urban 1 and Urban 2 are combined into Urban: Large (large cities) and Urban 3 and Urban 4 are combined in Urban: Small (small cities). Other possible birthplaces are high malaria rural areas (Rural: High Malaria), low malaria rural areas (Rural: Low Malaria), and foreign. There are four possible residences in 1860, and four possible places of death.
Table 3.
Hazard Ratio by Lifetime Locations
| Dependent Variable: Years to Death after the Civil War (1865) | |||||||
|---|---|---|---|---|---|---|---|
| Control variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) |
| Birthplace | |||||||
| Urban: Large | 1.1982* (0.1117) | 1.0844 (0.1053) | 1.1200 (0.1057) | 1.0552 (0.1026) | |||
| Urban: Small | 1.3403*** (0.1201) | 1.2231** (0.1198) | 1.2769*** (0.1159) | 1.1916* (0.1170) | |||
| Rural: High Malaria | 0.9775 (0.0460) | 1.0067 (0.0556) | 0.9842 (0.0476) | 1.0089 (0.0561) | |||
| Rural: Low Malaria | Omitted | Omitted | Omitted | Omitted | |||
| Foreign | 1.2410*** (0.0619) | 1.1922*** (0.0608) | 1.2050*** (0.0606) | 1.1749*** (0.0602) | |||
| Residence in 1860 | |||||||
| Urban: Large | 1.7515*** (0.1854) | 1.6137*** (0.1803) | 1.4825*** (0.1667) | 1.3968*** (0.1632) | |||
| Urban: Small | 1.4216*** (0.1304) | 1.2957** (0.1301) | 1.3497*** (0.1290) | 1.2525** (0.1293) | |||
| Rural: High Malaria | 0.9472 (0.0443) | 0.9540 (0.0524) | 0.9511 (0.0463) | 0.9542 (0.0534) | |||
| Rural: Low Malaria | Omitted | Omitted | Omitted | Omitted | |||
| Death place | |||||||
| Urban: Large | 1.5449*** (0.1167) | 1.4828*** (0.1138) | 1.4296*** (0.1143) | 1.4021*** (0.1127) | |||
| Urban: Small | 1.2184*** (0.0782) | 1.1748** (0.0764) | 1.1454** (0.0765) | 1.1297* (0.0757) | |||
| Rural: High Malaria | 0.9742 (0.0387) | 0.9887 (0.0404) | 0.9945 (0.0411) | 0.9988 (0.0416) | |||
| Rural: Low Malaria | Omitted | Omitted | Omitted | Omitted | |||
| Birth Year | 0.9159*** (0.0023) | 0.9150*** (0.0023) | 0.9141*** (0.0023) | 0.9159*** (0.0023) | 0.9152*** (0.0023) | 0.9145*** (0.0023) | 0.9154*** (0.0023) |
| LR χ2 (p-value) | 1143.9 (0.000) | 1152.4 (0.000) | 1152.7 (0.000) | 1167.1 (0.000) | 1173.0 (0.000) | 1174.0 (0.000) | 1203.8 (0.000) |
Notes: We conducted Cox proportional-hazards survival regressions for types of birthplace, 1860 residence and birthplace, and birth year without additional explanatory variables. The sample size of each regression is 3,732. Standard errors are reported in parentheses. Single asterisk denotes statistical significance at the 90% level of confidence, double 95%, triple 99%.
In Table 3, the results of Cox regressions on the various locations are reported for the three time periods separately and in combination with other time periods. The only control variable included in this set of regressions is the veteran’s birth year, and it is always about 0.915 (younger veterans faced a lower hazard) and highly statistically significant. The coefficients for those in a particular life stage and place are also highly stable with one notable exception. The hazard ratios (and their statistical significance) of being born in U.S. cities and foreign countries diminishes when residence in 1860 is included in the regression. They also diminish, albeit by less, when death place is included in the regression. 20 To the extent that, in the regression with all three dates included, the hazard ratio of having been born in a large city is much lower than having resided in one in 1860 or having died in one, our result suggests that the early years of life are relatively less important in explaining the later life experience of these surviving veterans.21
Table 4 presents the results of regressions that include all three stages. Recall that column 7 of Table 3 reports the results when birth year is the only control variable. Table 4 introduces various control variables in three steps. The first step involves socio-economic variables, the individual’s wealth in 1860 and his occupation at enlistment.22 Clearly there is a relationship between a rural residence and being a farmer, but the correlation is not as high as one might expect.23 The second step adds variables that reflect the veteran’s wartime experience. In addition to the year of enlistment, there are data on initial rank and the insults experienced during the war -- whether he experienced infections or illness, whether he had wounds or other injuries, and whether he was a POW. The final step adds variables that reflect morbidity later in life as reported in the Surgeon’s Certificates for pension purposes; these are measured by a dummy variable indicating if a veteran was diagnosed with a specific chronic disease by 1875, ten years after the war.
Table 4.
Hazard Ratio by Lifetime Locations and by Different Model Specifications
| Dependent Variable: Years to Death after the Civil War (1865) | |||
|---|---|---|---|
| Control variables | (1) | (2) | (3) |
| Birthplace | |||
| Urban: Large | 1.0367 (0.1010) | 1.0392 (0.1016) | 1.0319 (0.1010) |
| Urban: Small | 1.1720 (0.1153) | 1.1638 (0.1150) | 1.1421 (0.1136) |
| Rural: High Malaria | 1.0339 (0.0580) | 1.0348 (0.0580) | 1.0289 (0.0578) |
| Rural: Low Malaria | Omitted | Omitted | Omitted |
| Foreign | 1.1714*** (0.0604) | 1.1973*** (0.0629) | 1.1961*** (0.0631) |
| Residence in 1860 | |||
| Urban: Large | 1.3182** (0.1546) | 1.2752** (0.1508) | 1.2721** (0.1506) |
| Urban: Small | 1.2130* (0.1256) | 1.2100* (0.1260) | 1.2012* (0.1263) |
| Rural: High Malaria | 0.9686 (0.0546) | 0.9698 (0.0547) | 0.9700 (0.0549) |
| Rural: Low Malaria | Omitted | Omitted | Omitted |
| Death Place | |||
| Urban: Large | 1.3659*** (0.1101) | 1.3609*** (0.1102) | 1.3708*** (0.1110) |
| Urban: Small | 1.1059 (0.0742) | 1.1075 (0.0744) | 1.1101 (0.0750) |
| Rural: High Malaria | 1.0212 (0.0428) | 1.0139 (0.0428) | 1.0152 (0.0429) |
| Rural: Low Malaria | Omitted | Omitted | Omitted |
| Birth Year | 0.9172*** (0.0027) | 0.9186*** (0.0027) | 0.9184*** (0.0027) |
| Other Specifications | |||
| SES Conditions around 1860 | YES | YES | YES |
| Wartime Experiences | NO | YES | YES |
| Later Health Conditions | NO | NO | YES |
| LR χ2 (p-value) | 1214.9 (0.000) | 1225.5 (0.000) | 1253.6 (0.000) |
Notes: Additional control variables in each category of other specifications are listed in Table 5. The regression coefficients for other control variables in model (3) are also presented in Table 5. The sample size of each regression is 3,732. Standard errors are reported in parentheses. Single asterisk denotes statistical significance at the 90% level of confidence, double 95%, triple 99%.
Given the inclusion of all three stages, the hazard ratio for a large urban birthplace is, in fact, less than that of a small urban birthplace. Large cities have the highest hazard ratio for residences in 1860 regardless of specification. For urban death places, large cities have higher hazard ratios than small cities, higher than rural places, but there is little difference between the two rural places, with the low malaria areas having a slightly higher ratio than the high malaria areas. Most important, there is little difference by specification in Table 4. The spread of the hazard ratios by life stage is still quite large. These results also suggest that the urban mortality penalty as it affected these veterans may be more a function of what happened in late adolescence and adulthood than what happened during one’s formative years. But this does not imply that life conditions at birth are unimportant. As will be discussed at the end of this section, the finding is highly related to sample selection; while the early-life and wartime insults experienced by these veterans varied, all were survivors of the war.
Table 5 presents the coefficients for the control variables that were generated from the regression involving all the control variables reported in Table 4, column 3. It should be noted that the coefficients presented in this table are almost identical in magnitude and statistical significance to those from the other regressions in which they appear. It also is worth noting that, in the face of all these variables, the urban mortality penalty persists.
Table 5.
Estimated Hazard Ratios for Other Control Variables
| Other Control Variables | Hazard Ratio | Standard Error | |
|---|---|---|---|
| Panel A: Socio-Economic Conditions around 1860 | |||
| 1860 individual wealth | 0.9894 | * | 0.0059 |
| Dummy of occupation at enlistment | |||
| Professional worker | 1.1284 | 0.1530 | |
| Farmer | 0.8217 | *** | 0.0365 |
| White collar worker | 0.9417 | 0.1009 | |
| Blue collar worker | 0.9468 | 0.0472 | |
| Unemployed or unknown | Omitted | ||
| Panel B: Wartime Experiences | |||
| Enlistment year dummy | |||
| 1861 | 1.1587 | ** | 0.0799 |
| 1862 | 1.1263 | * | 0.0728 |
| 1863 | 1.0424 | 0.0907 | |
| 1864 | 1.0336 | 0.0665 | |
| 1865 | Omitted | ||
| Initial Rank: Private | 1.0288 | 0.0557 | |
| Dummy of wartime experience | |||
| Infections and illness | 1.0021 | 0.0383 | |
| Wounds and injuries | 0.9433 | 0.0365 | |
| POW | 1.0055 | 0.0642 | |
| Panel C: Later Health Conditions | |||
| Dummy of later health conditions | |||
| Cardiovascular diseases | 1.0524 | 0.3862 | |
| Rheumatism/musculo-skeletal | 1.0700 | 0.4947 | |
| Respiratory | 4.9981 | *** | 1.6406 |
| Diarrhea | 0.8303 | 0.2281 | |
| Nervous System | 1.0563 | 0.5301 | |
| Genito-Urinary | 0.7346 | 0.3355 | |
| Infections | 0.6683 | 0.3714 | |
| Eye | 0.6337 | 0.2580 | |
| Gastrointestinal | 0.8178 | 0.8226 | |
| Poor Appearance | 2.6073 | * | 1.4267 |
| Hernia | 1.7358 | ** | 0.4839 |
| Injuries | 1.1281 | 0.1018 | |
| Liver/Spleen/Gallbladder | 1.1286 | 0.8021 | |
| Rectum/Hemorrhoids | 0.5504 | 0.3185 | |
| Varicose Veins | 0.9295 | 0.3656 | |
| Fevers | 0.8942 | 0.2697 | |
| LR χ2 (p-value) | 1253.6 (0.000) | ||
Notes: 1860 individual wealth is obtained from the 1860 census records, summing real estate and personal property values. Later health conditions are found in the surgeons’ certificates of the pension records. The other variables are found in the Union Army military records. Single asterisk denotes statistical significance at the 90% level of confidence, double 95%, triple 99%.
Veterans who were wealthier in 1860 had a statistically significantly lower hazard ratio. The Census reported wealth as either property wealth (greater than $100) or real estate wealth. We used the sum of these two in our regressions.24 Few veterans had accumulated substantial property wealth by 1860 when they would have been approximately age 20, an age at which few veterans had title to real estate. The only occupational category that is statistically significant is farmer, and, as noted, it is closely related to a rural residence. Clearly, much of the reported wealth could be the ownership of farmland.
Those who enlisted earlier were at greater risk; the hazard ratios decline uniformly as time passed. Having an initial rank of private increased one’s risk. While wartime infections and being a POW did not seem to have much effect, wartime wounds reduced the hazard of early death after the war. For the veterans from rural areas, surviving wartime infections meant they were on average healthier than their compatriots, but the exposure to those infections worked in the opposite direction. One would expect that some of the wounded veterans were discharged from service before the end of the war, returned home, and were less at risk for things that might affect them later in life. In short, spending less time at war increased one’s longevity. None of the wartime experience variables are statistically significant.
The variables associated with illness within 10 years following the Civil War have several that proved statistically significant, including respiratory diseases, poor appearance, and hernia; all were associated with a higher hazard ratio. Poor health conditions identified by age 35 generally shortened a veteran’s life expectancy.25
The effect of the foreign-born veterans was addressed by re-running the above regressions including only the native-born veterans or only the foreign-born veterans. The results are in Table 6. Compared with column 3 of Table 4, excluding the foreign-born reduces the hazard ratio in smaller cities in 1860, but that is the only major difference. Similarly, including only the foreign-born veterans produces an extremely high hazard ratio of living in small cities in 1860, although this involves a very small sample size. Although the effects are small, it is worth noting that the hazard ratios for all estimated birthplaces increase when the foreign-born are omitted, but they generally decrease for residence in 1860 and death place. It is possible that, the greater the proportion of foreign born in a city, the lower that city’s survival rate for the native born. Regardless, the urban mortality penalty is apparent in each regression, and that penalty is more pronounced for the later stages of life. As before, the foreign born do not explain the urban mortality penalty.
Table 6.
Hazard Ratios of Native-Born Veterans by Lifetime Locations
| Dependent Variable: Years to Death after the Civil War (1865) | ||
|---|---|---|
| Control variables | (1) Native-Born | (2) Foreign-Born |
| Birthplace | ||
| Urban: Large | 1.0614 (0.1085) | |
| Urban: Small | 1.1879* (0.1202) | |
| Rural: High Malaria | 1.0335 (0.0591) | |
| Rural: Low Malaria | Omitted | |
| Foreign | Not Included | |
| Residence in 1860 | ||
| Urban: Large | 1.2227 (0.2129) | 1.0619 (0.2049) |
| Urban: Small | 1.0770 (0.1317) | 1.6859** (0.3475) |
| Rural: High Malaria | 0.9428 (0.0567) | 1.0716 (0.1849) |
| Rural: Low Malaria | Omitted | Omitted |
| Death place | ||
| Urban: Large | 1.3115*** (0.1241) | 1.4862** (0.2561) |
| Urban: Small | 1.1602** (0.0861) | 0.9337 (0.1585) |
| Rural: High Malaria | 1.0358 (0.0462) | 0.8357 (0.1206) |
| Rural: Low Malaria | Omitted | Omitted |
| Birth Year | 0.9187*** (0.0030) | 0.9203*** (0.0069) |
| Other Specifications | ||
| SES Conditions around 1860 | YES | YES |
| Wartime Experiences | YES | YES |
| Later Health Conditions | YES | YES |
| LR χ2 (p-value) | 947.18 (0.000) | 217.7 (0.000) |
| n | 3,227 | 505 |
Notes: Additional control variables in each category of other specifications are listed in Table 5. Standard errors are reported in parentheses. Single asterisk denotes statistical significance at the 90% level of confidence, double 95%, triple 99%.
To get a better handle on the three life stages, we examined age-specific death rates based on the veteran’s location at each stage. The rate is for those 60 years of age and older who died in each five-year interval. We selected 60 as the appropriate age for the calculation given that the pool of pensioners increased with the reforms of the 1890s, when the average veteran was in his 50s, and given that the survival rates reported at the beginning of this paper are based on 1900. The age-specific death rates for each interval appear in Figure 3. The upper panels are for the entire sample; the lower panels, for native-born veterans.
Figure 3. Five-Year-Period Age-Specific Mortality Rate of Union Army Veterans (aged 60 or more at the beginning year of each period).
Notes: We limited the sample to veterans who were at 60 or older at the beginning year of each period. The mortality rate is calculated as total deaths during the period out of total veterans alive at the beginning of the period.
What is immediately apparent is that, although all three upper panels are quite similar, the urban mortality penalty is most pronounced for panel b, for the residence in 1860. This is consistent with what was found in the regression analysis above. Panel c, for death place, indicates that large cities were generally the worst, but the small cities are often indistinguishable from rural areas. Panel a, for birthplace, shows that those born in large cities and outside the U.S. had the highest rates in general, and specifically from 1906-1915. The slight U-shape in panels b and c is the result of some relatively small sample sizes and the inclusion of the foreign born. When the foreign born are excluded from panels b and c, the U-shape is slightly reduced in the figure for the residence in 1860 where the sample sizes are smallest (panel d) and essentially eliminated in the figure for death place (panel e). It should be recalled that the foreign-born were four to five years older on average, so they turned 60 one period sooner than the native-born.
In sum, the Cox hazard regressions indicate that the urban mortality penalty is likely to be important at all three life stages, but it may well be the case that, for these veterans, the birthplace played a less important role than residence in 1860 or death place. This might appear to be surprising given that two well-established population theories relate the effects of early life health conditions to later health outcomes. The “insult theory” argues that insults from disease or injury accumulate, weaken individuals, and make them more susceptible to future health problems.26 The Barker hypothesis argues that early life conditions, especially at birth and in utero, are significant determinants of adult health.27 Our finding of an urban mortality penalty at all three life stages supports the insult theory; prior exposure to health insults in an urban environment reduced the probability of living longer. However, our finding that later environments are perhaps more important than one’s birthplace seems to contradict the Barker hypothesis. Can we reconcile that hypothesis with our findings?
The Barker hypothesis says that early life and in utero health insults lead to adverse health outcomes in adult health through reduced fetal growth and malnutrition. This implies that urban-born veterans faced more disadvantages in later life because they suffered more health insults earlier in life than the rural-born veterans did. However, some types of prior insults may result in later health outcomes different than what the insult theory and the Barker hypothesis suggest. For example, Lee (2003) found that recruits who came from unsanitary urban places were more resistant to immunity-conferring diseases during the war (e.g., typhoid and measles) because they were more likely to have been exposed and to have developed immunity to those infections early in life in comparison to their rural compatriots. Thus, it is reasonable to think that, for urban veterans, the physiological stress they faced during the war contributed to their mortality experience after the war. For the rural-born veterans, although they typically were healthier in early life than their urban counterparts, they experienced a larger number of the insults during the war including the infectious diseases that the urban-born had experienced before they enlisted and then brought to the camps.
Closely related is the fact our sample is composed of veterans who survived not only early life infections but also the war and the camps. These all have to be viewed as insults veterans faced during their lives. Thus, there is a sample selection issue. Enlistees were selected into the Union Army after physical examinations. Recruits who were less healthy, perhaps following the Barker Hypothesis due to insults at birth or before adolescence, were not selected. In addition, even if their potential health problems were not detected at the physical examinations, they had a higher probability of dying from infections and diseases during the war. In other words, the urban-born recruits who were selected for service in the Union Army and survived the war were healthier than other urban-dwellers before the war, perhaps as healthy as rural-born veterans. This also would weaken our estimated urban mortality penalty with respect to one’s birthplace.
In short, at war’s end, the health status of the survivors from urban and rural places may have been similar. Thus, while the urban mortality penalty for these veterans may be more a reflection of later life insults, it is not necessarily inconsistent with the Barker Hypothesis. One cannot use this evidence to reject the hypothesis. In fact, the importance of birthplace is still found when we investigate the effect of lifetime mobility as below.
As a final step, we constructed a dummy variable that reflects each of the three life stages we have been considering: a veteran’s birthplace, his residence in 1860, and his death place. We have assigned a three-digit number to each of the 80 possibilities that result from the fact there are 5 possible birthplaces, 4 possible residences in 1860, and 4 possible death places. In each position, the number 1 reflects the larger city category (Urban: Large); 2, the smaller city category (Urban: Small); 3, the high malaria rural area (Rural: High Malaria); and 4, the low malaria rural area (Rural: Low Malaria). A “5” in the first position indicates a foreign born veteran. Thus, a number such as “432” indicates a veteran born in a low malaria rural area, who resided in a high malaria rural area in 1860, and died in a small city. Because there are no veterans in some of these cells and very few in others, we have limited our analysis to those cells in which there are at least five veterans. This regression includes a full set of control variables. While they are not reported, the estimated coefficients for the control variables (and their statistical significance) are essentially identical to those reported in Table 5.
Table 7 presents the coefficients for the mobility variables according to a veteran’s birthplace. The reference group is those veterans who were born and lived in low malaria rural areas throughout their lives (444).
Table 7.
Coefficients of Mobility Sorted by Type of Birthplace
| Birthplace | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Large City | Small City | High Malaria Rural | Low Malaria Rural | Foreign | ||||||||||
| 111 | 1.7964 | ** | 211 | — | 311 | 411 | 511 | 1.9026 | *** | |||||
| 112 | 212 | — | 312 | — | 412 | 512 | 1.0193 | |||||||
| 113 | — | 213 | — | 313 | — | 413 | 513 | |||||||
| 114 | 1.0364 | 214 | — | 314 | — | 414 | 1.0106 | 514 | 2.9922 | *** | ||||
| 121 | — | 221 | 321 | — | 421 | 521 | ||||||||
| 122 | 1.6488 | 222 | 1.4335 | * | 322 | — | 422 | 1.7306 | ** | 522 | 2.6564 | *** | ||
| 123 | 223 | 323 | — | 423 | — | 523 | — | |||||||
| 124 | — | 224 | 0.7380 | 324 | 424 | 1.1024 | 524 | 1.4083 | ||||||
| 131 | 231 | — | 331 | 0.9883 | 431 | 531 | 2.2441 | ** | ||||||
| 132 | — | 232 | — | 332 | 0.7060 | 432 | 0.7648 | 532 | 1.2373 | |||||
| 133 | 233 | 333 | 1.2293 | *** | 433 | 0.7060 | *** | 533 | 1.6062 | ** | ||||
| 134 | 234 | 334 | 0.9927 | 434 | 0.9408 | 534 | 0.9572 | |||||||
| 141 | 1.4953 | 241 | 1.5468 | 341 | 0.9879 | 441 | 1.2786 | * | 541 | 2.1323 | *** | |||
| 142 | 242 | 1.6339 | ** | 342 | 442 | 1.1338 | 542 | 0.9193 | ||||||
| 143 | 0.7492 | 243 | 1.5950 | 343 | 0.8678 | 443 | 1.0234 | 543 | 0.9402 | |||||
| 144 | 1.0603 | 244 | 1.4263 | ** | 344 | 0.8934 | 444 | Omitted | 544 | 1.1876 | *** | |||
Notes: Out of 3,732 samples employed in the previous analyses, we used 3,684 veterans here by limiting our analysis to the mobility groups with 5 samples or more. The groups with blank above were dropped because of their sample sizes are less than 5. On the other hand, we denoted the groups without observation by hyphens (—). ‘Omitted’ group is the reference group. Values of the hazard ratios over 1.5000 have been bolded. Besides mobility dummies, we controlled for birth year and other explanatory variables listed in Table 5. Single asterisk denotes statistical significance at the 90% level of confidence, double 95%, triple 99%.
Perhaps the first thing to observe is that there are no estimated coefficients reported for veterans born in a large city (1) or in a small city (2) who resided in high malarial rural area (3) in 1860. There are no coefficients for veterans born in a high malarial rural area (3) who resided in a small or large city in 1860. The absence of estimates is the result of a lack of data. Even though this regression is based on 3,684 observations, the relative lack of urban observations creates a void that begs to be filled.
Of the 12 bolded coefficients that exceed 1.5000, 2 are in the column reflecting a large city birthplace and 6 in the column reflecting a foreign birthplace. Of those 8, 6 involve living in a large city at another stage. For small cities, the hazard ratio is generally high regardless of where veterans moved after the war. These results suggest that environments in early years are significant in determining later health and longevity. For those born in low malaria rural areas, the hazard ratios are extremely high if they resided in a small city until death. There are no bolded coefficients in the column for those born in high malaria rural areas.
If one looks just at those who remained in an area like their birthplace, the urban mortality effect is quite apparent. The hazard ratio for large cities (111) is 1.7964; that for small cities (222) is 1.4335, and that for high malaria rural areas (333) is 1.2293. Recall that the omitted category in this regression is that for low malaria rural areas (444), which presumes that value is 1.000. Sample size may be an issue for large cities, as there are only 14 veterans in large cities (111). The numbers in the other three categories are 25, 212, and 1,633, respectively.
From Table 7, we can also observe the complexity of the mobility effect. If we look at the effect of residence in 1860 among those who were born and died in low malaria rural areas (i.e., 414, 424, 434, and 444), we do not find a systematic urban mortality penalty regarding the residence in 1860. But, if we look at the effect among foreign-born veterans who died in low malaria rural areas (i.e., 514, 524, 534, and 544), the effect of residing in a large or small city around 1860 is considerable. This result suggests that the urban morality penalty at adolescence largely depends on the earlier life conditions. A similar implication is also found in the comparison between the hazard ratios in the row of 141 and those in the row of 144. Although the coefficients in both rows show a systematic urban morality penalty at birth, the penalty is more substantial when the veterans lived in large cities in adulthood.
Were Table 7 to be sorted to reflect a veteran’s residence in 1860, 3 of the bolded coefficients would be in the column for large cities, 3 in the column for small cities, 2 in the column for the high malaria rural areas, and 4 in the column for low malaria rural areas. Both of the latter coefficients are for veterans who were born in foreign countries or small cities and lived in a large city at the end of their lives. Were the sorting to reflect a veteran’s place of death, 5 of the 12 bolded coefficients would be in the column reflecting death in a large city, 4 in the column for small cities. The remaining 3 all involve death in a rural place, but involve residence in a large city in 1860 or an urban or foreign birthplace. Of the 9 bolded coefficients involving death in an urban place, all suggest that a veteran either was foreign born or lived in cities at previous stage of their life.
In summary, the general impression we take from this table is that those born in large cities and the foreign born who moved to large cities faced high hazard ratios. This table also gives the impression that the urban mortality penalty was present over all the life stages, that the initial years were an important component of that penalty, but perhaps not the most important. In other words, the urban mortality penalty at birth is aggravated by living in urban environments in later life, and the same can be applied to explain the effect of urban environments in later life.
After controlling for life events and health insults at the individual level, the urban mortality penalty persists. It may well be that additional information on the specific insults that each veteran survived during the war could help explain the situation. This will be the subject of future research.
Several explanations have been proffered why mortality was higher in cities. Rapid population growth taxed the limited ability of late nineteenth century cities to provide even rudimentary sanitation. Water and sewer systems were inadequate, especially when faced with industrial pollution. The influx of native-born migrants from rural areas arrived with few natural defenses to diseases with which they had no previous exposure, while foreign immigrants introduced new diseases. Immigrants tended to crowd into tenements, which facilitated the spread of disease. Contaminated milk and food supplies were common.28
The present results are a small first step at shedding light on these hypotheses. To the extent that population growth increased urban density, this clearly contributed to a worsening of the survival rate, but the information currently available for each veteran does not allow an imputation for the density of the neighborhood in which he lived. Sanitation systems are likely to be important factors, but we only have good information for some, not all, of the urban areas in our sample, less for rural areas, and relatively little of that is available before 1890.29 Future research will focus on urban areas to try to assess the importance of these explanations through the use of GIS analysis and urban data at the level of the individual ward.
Although the disparity between urban and rural mortality has been studied extensively, there has been relatively little work done on the urban mortality penalty itself. The relatively conventional (and some unconventional) measures that are readily available and used here do not offer a complete explanation for why the hazard ratio for large cities is, on average, 30-40 percent higher than that of a low malarial rural area. We feel it is reasonable to conclude from this initial statistical analysis that both socioeconomic and environmental variables contributed to that penalty. It appears that for these veterans much emphasis should be placed on where they lived later, particularly where they spent their adolescence, as much as on where they were. The fact all these veterans survived the many health insults to which they were exposed during the Civil War means their later health experience may well be different from the other members of their birth cohort – those who did not go to war or those who did not survive it. Regardless of the specification, the urban mortality penalty persists throughout our analyses.
It is clear that a great deal more work needs to be done. These results seem filled with puzzles that can’t be resolved without expanding the sample of urban veterans. This is especially true for veterans from small cities where we expect some of the anomalies we observe are attributable to small sample sizes. It is also important to look within cities as well as across them. We have used a figure for the average individual wealth in a city, but wealth varied widely within cities, between neighborhoods with tenements and those with single family homes. The same is true of urban density. Finally, the variables themselves, particularly the environmental variables, need to be refined. This essay has revealed how persistent the urban mortality penalty was, but a complete explanation of the penalty requires a project of much greater scope.
Acknowledgments
While the authors thank all their colleagues, Hoyt Bleakley, Joe Ferrie, Mark Guglielmo, and Chulhee Lee deserve special thanks. We would like to thank the anonymous referees and the Journal editor for their valuable comments and suggestions. We also have benefited from comments and suggestions by the participants in the workshops at the University of Chicago, Northwestern University, University of Wisconsin - La Crosse, the 2007 Economic History Association Meetings, the 2007 Social Science History Association Meetings, the 2007 Illinois Economics Association Meetings, the 2008 Canadian Network for Economic History Meetings, and NBER Cohort Study Meetings. Research reported in this article was supported by NIH grant number P01 AG10120.
Footnotes
For example, in 1899, Weber (1899) reported life expectancy at birth in the cities of Massachusetts was almost seven years less than that in the state as a whole. See also Condran and Crimmins (1980), Glover (1921), Haines (1977), United Nations (1953), Vinovskis (1981), and Woods et al. (1988).
See Riley (1989), for example.
Massachusetts had a good system of birth and death registrations in the early 19th century. Vinovskis (1972), Jaffe and Lourie (1942). Other scholars reporting similar disparities in the second half of the 19th century are Condran and Crimmins (1980), Haines (1977), Higgs (1973), and Yasuba (1961).
By 1910, these differences were about eight years for men and six years for women.
Glover (1921). The problems with the original DRA are well known. The coverage was limited, only 26.3 percent of the U.S. population. The included states were more urban, had a larger percentage of foreign residents, and a smaller percentage of black residents than the U.S. as a whole. Moreover, blacks in the DRA were four times more likely to live in urban areas than blacks in the U.S. as a whole. Consequently, scholars have concluded the Census Bureau overestimated mortality for whites and especially for blacks. See Haines (1998) and Preston and Haines (1991).
For whites, see Dublin, Lotka, and Spiegelman (1949); for blacks, Ewbank (1987), Haines (2001, 2002), and Preston and Haines (1991).
This article is based on historical data collected by the ‘Early Indicators of Later Work Levels, Disease, and Death’ project, which is sponsored by the National Bureau of Economic Research, the National Institutes of Health, the Center for Population Economics at the University of Chicago, and Brigham Young University. The data used in this essay are available online at www.cpe.uchicago.edu. The primary sample for the project consists of 35,570 white males mustered into the Union Army during the Civil War, who were chosen randomly from the company books stored at the National Archives in Washington, D.C. Commissioned officers were excluded. In addition, the project provides lifetime military, medical, and socioeconomic information on these individuals by linking the veterans to other historical documents: the military, pension and medical records, the surgeons’ certificates data, and the census records data. Given the data, it is not possible to say anything about the survival rates of women.
We can also calculate 1866-1910 survival rates by linking to the 1910 Census, but we are unable to calculate similar rates for any other time period using the full Union Army sample.
There are selection issues involved in using this sample. Enlistees were selected into the Union Army after physical examinations. Less healthy recruits were not selected. Thus, using this data may overestimate the survival rate of the total population. However, veterans experienced various stressful and harmful environments during the war, and survivors could be considered less healthy at war’s end than those who were not exposed to wartime insults. In fact, veterans who were discharged early because of injuries developed less health problems in later life than others because they were exposed to infections and other insults associated with war for a shorter time. Unfortunately, the data do not allow us to determine the direction of selection bias. The results in the essay should be considered in the light of this issue.
We also performed the analyses using 1840 and 1900 city populations to classify urban birth and urban death places, respectively. The results based on this alternative classification were similar to that from using the 1860 definition for all three time periods.
The remaining six were in the Confederacy.
Inasmuch as almost all the urban places are in northern states and would be classified as in low malarial areas, we chose not to apply that classification to urban places.
See Hong (2007) for the estimation and mapping of malaria risk in the U.S. The estimated risk index ranges between 0 and 0.56. The number can be interpreted as the annual probability of contracting remittent or intermittent fever in a county. The estimation results suggest that a malarial environment can be characterized by warmer, wetter, and flatter areas, but extremely hot temperatures can stop the development of the parasite. Using the estimated malaria risk, Hong found that Union Army recruits from the most malarial rural counties were about 1.1 inch shorter at enlistment and about 13% more susceptible to infectious diseases during the war than were those from the least malarial counties because of malnutrition in childhood and immune disorders resulting from malaria infections.
The selection of the breakpoint is based on actual malaria mortality. The U.S. Census Bureau (1885, Section 8) provides maps and tables suggesting that more than 30 deaths per 1,000 were caused by malarial fevers in the most malarial areas including the Mississippi and Missouri River valleys, Southern and South West Central Regions, and Gulf areas. From the 1880 malaria risk index (0.0009-0.5616) which was estimated by the method of Hong (2007), we chose a value of 0.25 to separate low- from high-malarial areas, which well corresponds to ‘30 deaths per 1,000’ in the census record. When we used different values of the index as the dividing line, the urban mortality penalty was present until the index reached very high values. When we used geographic areas (Northeast, Midwest, etc.) to differentiate rural areas, the urban mortality penalty was still present.
We have not attempted to ascertain whether it made a difference if a foreign-born veteran arrived in the U.S. closer to his birth or to 1860.
We used Coale and Demeny’s (1983) North Male Life Table to estimate life expectancy at birth: level 5 for urban 1 veterans and level 13 for rural veterans. Coale and Demeny provides demographic models and a tabulation of the varying chances of dying as a function of age by gender and region. Using the sample average of birth year and survival rate, a particular table is chosen. The estimation changes depending on which table is used, but they vary within a small margin. For example, if the West Female Life Table is used, the values of ℮o are 25.0 and 45.0, respectively.
For urban dwellers, we have information on such things as the sanitation services supplied in many, but not all, of the cities over time. We do not have that for the vast majority of the rural areas, which includes several smaller urban places (i.e., between 2.500 and 9,552 population). In general, sanitation services were expanding in both quality and quantity after 1890. We do expect to make use of information on sanitation in future work that will focus on survivorship within cities as opposed to this study which focuses on survivorship across cities and rural areas.
There are well-defined problems that emerge when this specification is used with a fixed population. Each group has a survivor rate of 1 at the start, and they each have a rate of 0 by some year. In between, the survival rates depicted in Figure 2 show the requisite proportionality. Nevertheless, we tried alternative specifications (OLS with age at death the dependent variable and Probit with dummy variables for death before a given year). The results are consistent with the Cox analysis, and it is the Cox results that are presented here.
Only 3,732 veterans have information on all three places: birth, 1860 residence and death. Using those veterans produces a similar pattern of hazard ratios by urban strata to that in Table 2.
It should be noted that, in many cases, Table 3 reports that the hazard ratio for high malaria rural areas was less than one. There are roughly one-fifth as many observations from high malaria rural areas than for small. As an alternative, we ran the regressions underlying Table 3 with rural areas divided into northeast, midwest, south and west. South and west was the omitted variable. In general, hazard ratios in the northeast were the highest, with the midwest second. Given that the high malaria rural areas tended to be in the south, the results are consistent with those reported here -- the impact of having an urban birthplace is reduced by adding residence in 1860 and death place.
A study of age-specific mortality for each of the three places (reported below) further emphasizes the importance of 1860 residence and death place in relation to birthplace.
A veteran’s height at enlistment, the population density of the county in which he is located in 1860, and the infant mortality rate in those counties for which it was reported are available. Height and infant mortality are only available for a subset of the sample. Both height and population density are highly correlated with other variables we report. When one or both are used in place of the variables we report, the explanatory power of the regression equation diminishes slightly. The results when we include infant mortality are essentially identical to those reported. Thus, we elected not to report these regressions; they are available from the authors. Suffice to note that mortality tends to increase with increasing density.
This was true whether we excluded “laborers, not elsewhere classified” or, in the spirit of Thomas Weiss’ revisions of the farm labor force series, included all so listed with a rural residence. The correlation coefficient when they are excluded is 0.20 and rises to 0.24 when they are included.
Breaking total wealth into its two components added nothing to the explanation.
We also ran these regressions using a set of dummies indicating whether a veteran was diagnosed with each of these chronic diseases before death. This produces lower hazard ratios because the longer a veteran lived, the more likely he was to be diagnosed with one or more of these conditions. It should be recalled that the pension roles expanded greatly with the liberalization of the rules in 1890 when the average surviving veteran was in his early 50s. Although prior to 1890, there were well-known fluctuations in eligibility (see Kang and Rockoff (2007)), we do not believe those fluctuations affect this analysis.
See Riley (1989).
See Barker (1997).
Brown (forthcoming), Davis (1973), Duffy (1990), Haines (2001), McKeown and Record (1962), Meeker (1972, 1974), Melosi (2000), Preston and Haines (1991), Voegele (1994), and Williamson (1982, 1990).
See also Cain and Rotella (2001), Cutler and Miller (2006), and Ferrie and Troesken (2008).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Louis Cain, Professor of Economics at Loyola University Chicago, Adjunct Professor of Economics at Northwestern University, and a Senior Investigator at the Center for Population Economics at the University of Chicago (Email: lcain@northwestern.edu).
Sok Chul Hong, Assistant Professor of Economics at Sogang University (Email: shong@sogang.ac.kr).
Bibliography
- Barker DJ. Maternal Nutrition, Fetal Nutrition, and Disease in Later Life. Nutrition. 1997;13(9):807–13. doi: 10.1016/s0899-9007(97)00193-7. [DOI] [PubMed] [Google Scholar]
- Brown JC. Forthcoming. Public health reform and the decline in urban mortality: The case of Germany, 1876-1912. In: Kearns G, Lee WR, Nelson MC, Rogers J, editors. Improving the Public Health: Essays in Medical History. Liverpool, UK: Liverpool University Press; [Google Scholar]
- Cain LP, Rotella EJ. Death and spending: Did urban mortality shocks lead to municipal expenditure increases? Annales de demographie historique. 2001;1:139–54. [Google Scholar]
- Coale A, Demeny P. Regional model life tables and stable populations. New York: Academic; 1983. [Google Scholar]
- Condran GA, Crimmins E. Mortality differentials between rural and urban areas of states in the northeastern United States, 1890-1900. Journal of Historical Geography. 1980;6(2):179–202. doi: 10.1016/0305-7488(80)90111-5. [DOI] [PubMed] [Google Scholar]
- Cutler D, Miller G. Water, Water, Everywhere: Municipal Finance and Water Supply in American Cities. In: Glaeser E, Goldin C, editors. Corruption and Reform: Lessons from America’s Economic History. Chicago: University of Chicago Press; 2006. [Google Scholar]
- Davis K. International Population Conference: Liege, 1973. Vol. 3. Liege: International Union for the Scientific Study of Population; 1973. Cities and mortality; pp. 259–282. [Google Scholar]
- Duffy J. The Sanitarians. Urbana, IL: University of Illinois Press; 1990. [Google Scholar]
- Dublin LI, Lotka AJ, Spiegelman M. Length of Life. New York: Ronald Press; 1949. [Google Scholar]
- Ewbank DC. History of black mortality and health before 1940. The Milbank Quarterly. 1987;65(Supp 1):100–128. [PubMed] [Google Scholar]
- Ferrie JP, Troesken W. Water and Chicago’s Mortality Transition, 1850-1925. Explorations in Economic History. 2008;45(1):1–16. [Google Scholar]
- Glover JW. United States Life Tables, 1890, 1901, 1910 and 1901-1910. Washington: US Government Printing Office; 1921. [Google Scholar]
- Haines MR. Mortality in nineteenth century America: Estimates from New York and Pennsylvania census data, 1865 and 1900. Demography. 1977;14(3):311–31. [PubMed] [Google Scholar]
- Haines MR. Estimated life tables for the United States, 1850-1910. Historical Methods. 1998;31(4):149–169. [Google Scholar]
- Haines MR. The urban mortality transition in the United States, 1800-1940. Annales de démographie historique. 2001;1:33–64. [Google Scholar]
- Haines MR. Ethnic differences in demographic behavior in the United States: Has there been convergence? 2002 NBER Working Paper No. 9042. [Google Scholar]
- Higgs R. Mortality in rural America, 1870-1920: Estimates and conjectures. Explorations in Economic History. 1973;10(2):177–195. doi: 10.1016/0014-4983(73)90008-9. [DOI] [PubMed] [Google Scholar]
- Hong SC. The burden of early exposure to malaria in the United States, 1850-1860: Malnutrition and Immune Disorders. The Journal of Economic History. 2007;67(4):1001–1035. doi: 10.1017/S0022050707000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe AJ, Lourie WI. An abridged life table for the white population of the United States in 1830. Human Biology. 1942;14(3):352–71. [Google Scholar]
- Kang SW, Rockoff H. After Johnny Came Marching Home: The Political Economy of Veterans’ Benefits in the Nineteenth Century. NBER Working Paper No. 13223. Issued in June 2007. [Google Scholar]
- Lee C. Prior exposure to disease, and later health and mortality: Evidence from Civil War medical records. In: Costa D, editor. Health and Labor Force Participation over the Life Cycle. Chicago: University of Chicago Press; 2003. [Google Scholar]
- McKeown T, Record R. Reasons for the decline of mortality in England and Wales during the nineteenth century. Population Studies. 1962;16:94–122. [PubMed] [Google Scholar]
- Meeker E. The improving health of the United States, 1850-1915. Explorations in Economic History. 1972;10:353–73. [PubMed] [Google Scholar]
- Meeker E. The social rate of return on investment in public health, 1880-1910. Journal of Economic History. 1974;34(2):392–421. doi: 10.1017/s0022050700080128. [DOI] [PubMed] [Google Scholar]
- Melosi MV. The sanitary city: Urban infrastructure in America from colonial times to the present. Baltimore: Johns Hopkins University Press; 2000. [PubMed] [Google Scholar]
- Preston SH, Haines MR. The fatal years: Child mortality in late nineteenth-century America. Princeton, NJ: Princeton University Press; 1991. [Google Scholar]
- Riley JC. Sickness, Recovery and Death: A History and Forecast of Ill Health. Iowa City: University of Iowa Press; 1989. [Google Scholar]
- Troesken W. Water, Race, and Disease. Cambridge, MA: MIT Press; 2004. [Google Scholar]
- Troesken W. The Great Lead Water Pipe Disaster. Cambridge, MA: MIT Press; 2006. [Google Scholar]
- United Nations. The determinants and consequences of population trends: A summary of the findings of studies on the relationships between population changes and economic and social conditions. New York: United Nations; 1953. [Google Scholar]
- Census Bureau US. Report on mortality and vital statistics. Washington D.C.: Government Printing Office; 1885. [Google Scholar]
- Vinokskis MA. Mortality rates and trends in Massachusetts before 1860. The Journal of Economic History. 1972;32(1):184–213. doi: 10.1017/s002205070007546x. [DOI] [PubMed] [Google Scholar]
- Vinovskis M. Fertility in Massachusetts from the Revolution to the Civil War. New York: Academic Press; 1981. [Google Scholar]
- Voegele JP. Urban infant mortality in imperial Germany. Social History of Medicine. 1994;7(3):401–25. doi: 10.1093/shm/7.3.401. [DOI] [PubMed] [Google Scholar]
- Weber AF. The growth of cities in the 19th century: A study in statistics. New York: The Macmillan Co; 1899. [Google Scholar]
- Williamson JG. Coping with city growth during the British industrial revolution. New York: Cambridge University Press; 1990. [Google Scholar]
- Williamson JG. Was the Industrial Revolution worth it? Disamenities and death in 19th century British towns. Explorations in Economic History. 1982;19:221–245. [Google Scholar]
- Woods RI, Watterson PA, Woodward JH. The causes of rapid infant mortality decline in England and Wales, 1861-1921, Part I. Population Studies. 1988;42(3):343–66. doi: 10.1080/0032472031000143516. [DOI] [PubMed] [Google Scholar]
- Yasuba Y. Birth rates of the white population in the United States, 1800-1860: An economic study. Baltimore, MD: Johns Hopkins University Press; 1962. [Google Scholar]