Abstract
Background
In 1994, an International Task Force proposed criteria for the clinical diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D) that facilitated recognition and interpretation of the frequently nonspecific clinical features of ARVC/D. This enabled confirmatory clinical diagnosis in index cases through exclusion of phenocopies and provided a standard on which clinical research and genetic studies could be based. Structural, histological, electrocardiographic, arrhythmic, and familial features of the disease were incorporated into the criteria, subdivided into major and minor categories according to the specificity of their association with ARVC/D. At that time, clinical experience with ARVC/D was dominated by symptomatic index cases and sudden cardiac death victims–the overt or severe end of the disease spectrum. Consequently, the 1994 criteria were highly specific but lacked sensitivity for early and familial disease.
Methods and Results
Revision of the diagnostic criteria provides guidance on the role of emerging diagnostic modalities and advances in the genetics of ARVC/D. The criteria have been modified to incorporate new knowledge and technology to improve diagnostic sensitivity, but with the important requisite of maintaining diagnostic specificity. The approach of classifying structural, histological, electrocardiographic, arrhythmic, and genetic features of the disease as major and minor criteria has been maintained. In this modification of the Task Force criteria, quantitative criteria are proposed and abnormalities are defined on the basis of comparison with normal subject data.
Conclusions
The present modifications of the Task Force Criteria represent a working framework to improve the diagnosis and management of this condition.
Clinical Trial Registration
clinicaltrials.gov Identifier: NCT00024505.
Keywords: Arrhythmias, cardiac; Arrhythmogenic right ventricular cardiomyopathy/dysplasia; Death, sudden, cardiac; Diagnosis; Echocardiography; Electrocardiography; Magnetic resonance imaging
Arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D) is predominantly a genetically determined heart muscle disorder that is characterized pathologically by fibrofatty replacement of the right ventricular (RV) myocardium.1 In the early stage of the disease, structural changes may be absent or subtle and confined to a localized region of the RV, typically the inflow tract, outflow tract, or apex of the RV, the ‘triangle of dysplasia’.2 Progression to more diffuse RV disease and left ventricular (LV) involvement, typically affecting the posterior lateral wall, is common.3 Predominant LV disease is also recognized.4 Postmortem diagnosis may require extensive sampling and transillumination.5 Disease expression is variable. In the early ‘concealed phase’, individuals are often asymptomatic but may nonetheless be at risk of sudden cardiac death, notably during exertion.6 In the overt ‘electrical phase’, individuals present with symptomatic arrhythmias, and RV morphological abnormalities are readily discernible by conventional imaging. Later, diffuse disease may result in biventricular heart failure, whereas ventricular arrhythmias may or may not be present. The ultimate phenotype may resemble dilated cardiomyopathy. Clinical manifestations vary with age and stage of disease.7
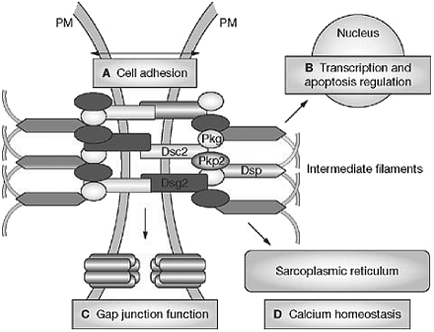
ARVC/D is considered to be familial with autosomal dominant inheritance, although there are recessive forms (eg, Naxos disease, Carvajal syndrome) that are associated with a cutaneous phenotype.8,9 Genetic variations have been found in the desmosomes that are responsible for cell-to-cell binding10,11 (Figure 1). Seven genes have been identified that are associated with ARVC/D: plakoglobin (JUP),12 desmoplakin (DSP),13 plakophilin-2 (PKP2),14 desmoglein-2 (DSG2),15,16 desmocollin-2 (DSC2),17,18 transforming growth factor beta-3 (TGFß3),19 and TMEM43.20 Mutations in RYR2 coding the ryanodine receptor have been reported in ARVC/D in patients with an arrhythmic presentation (stress-induced bidirectional ventricular tachycardia) in the absence of significant electrocardiographic or structural abnormalities. At present, catecholaminergic polymorphic ventricular tachycardia is considered a disorder distinct from ARVC/D.11 Preliminary observations suggest that the mechanical defect of the desmosomes alters function of the gap junction. Electrocardiographic (ECG) changes and arrhythmias may develop before histological evidence of myocyte loss or clinical evidence of RV dysfunction.21,22 It has been proposed that similar clinical phenotypes occur that are based on disruption of a ‘final common pathway’ by mutations in genes encoding proteins in the defined desmosomal pathway.23 Recognition of the genetic basis of ARVC/D facilitates examination of the pathogenesis in relation to arrhythmogenesis and disease progression.24
Figure 1.
The cardiac desmosome and proposed roles of the desmosome in (A) supporting structural stability through cell–cell adhesion, (B) regulating transcription of genes involved in adipogenesis and apoptosis, and maintaining proper electrical conductivity through regulation of (C) gap junctions and (D) calcium homeostasis. Dsc2 indicates desmocollin-2; Dsg2, desmoglein-2; Dsp, desmoplakin; Pkg, plakoglobin; Pkp2, plakophilin-2; and PM, plasma membrane. Reprinted by permission from Macmillan Publishers Ltd: Nat Clin Pract Cardiovasc Med11, © 2008.
It has been suggested that patients with ARVC/D may be predisposed or susceptible to viral myocarditis, which could lead to a decrease in cardiac function and accelerate progression of the disease.25–27 The link between ARVC/D and myocarditis is still undefined.
Background
The original 1994 International Task Force criteria for the clinical diagnosis of ARVC/D were based on structural, histological, ECG, arrhythmic, and familial features of the disease28 (Table 1). Abnormalities were subdivided into major and minor categories according to the specificity of their association with ARVC/D. ECG abnormalities such as complete and incomplete right bundle-branch block were excluded because of their lack of specificity. Right precordial T-wave inversion, though well recognized in ARVC/D, was considered a minor criterion because of its presence in other conditions, including anterior ischemia and RV hypertrophy. Arrhythmias of RV origin, another cardinal feature of ARVC/D, was designated a minor criterion because of its occurrence in other diseases, particularly idiopathic RV outflow tract tachycardia. Furthermore, the 1994 criteria focused on RV disease manifestations and stipulated the absence of or only mild LV involvement because of the need to exclude common disorders such as ischemic heart disease and dilated cardiomyopathy.
Table 1.
Comparison of original and revised task force criteria
| Original task force criteria | Revised task force criteria |
|---|---|
| I. Global or regional dysfunction and structural alterations* Major | |
|
By 2D echo:
|
By MRI:
|
|
|
By RV angiography: • Regional RV akinesia, dyskinesia, or aneurysm |
|
| Minor | |
|
By 2D echo:
|
By MRI:
|
|
| II. Tissue characterization of wall | |
| Major | |
| • Fibrofatty replacement of myocardium on endomyocardial biopsy | • Residual myocytes <60% by morphometric analysis (or <50% if estimated), with fibrous replacement of the RV free wall myocardium in ≥1 sample, with or without fatty replacement of tissue on endomyocardial biopsy |
| Minor | • Residual myocytes 60% to 75% by morphometric analysis (or 50% to 65% if estimated), with fibrous replacement of the RV free wall myocardium in ≥1 sample, with or without fatty replacement of tissue on endomyocardial biopsy |
| III. Repolarization abnormalities | |
| Major | • Inverted T waves in right precordial leads (V1, V2, and V3) or beyond in individuals >14 years of age (in the absence of complete right bundle-branch block QRS ≥120 ms) |
| Minor | |
| • Inverted T waves in right precordial leads (V2 and V3) (people age >12 years, in absence of right bundle-branch block) | • Inverted T waves in leads V1 and V2 in individuals >14 years of age (in the absence of complete right bundle-branch block) or in V4, V5, or V6 |
| • Inverted T waves in leads V1, V2, V3, and V4 in individuals >14 years of age in the presence of complete right bundle-branch block | |
| IV. Depolarization/conduction abnormalities Major | |
| • Epsilon waves or localized prolongation (>110 ms) of the QRS complex in right precordial leads (V1 to V3) | • Epsilon wave (reproducible low-amplitude signals between end of QRS complex to onset of the T wave) in the right precordial leads (V1 to V3) |
| Minor | |
| • Late potentials (SAECG) | • Late potentials by SAECG in ≥1 of 3 parameters in the absence of a QRS duration of ≥110 ms on the standard ECG |
| • Filtered QRS duration (fQRS) ≥114 ms | |
| • Duration of terminal QRS <40 µV (low-amplitude signal duration) ≥38 ms | |
| • Root-mean-square voltage of terminal 40 ms ≤20 µV | |
| • Terminal activation duration of QRS ≥55 ms measured from the nadir of the S wave to the end of the QRS, including R′, in V1, V2, or V3, in the absence of complete right bundle-branch block | |
| V. Arrhythmias | |
| Major | |
| • Nonsustained or sustained ventricular tachycardia of left bundle-branch morphology with superior axis (negative or indeterminate QRS in leads II, III, and aVF and positive in lead aVL) | |
| Minor | |
|
|
| VI. Family history | |
| Major | |
| • Familial disease confirmed at necropsy or surgery | • ARVC/D confirmed in a first-degree relative who meets current Task Force criteria |
| • ARVC/D confirmed pathologically at autopsy or surgery in a first-degree relative | |
| • Identification of a pathogenic mutation† categorized as associated or probably associated with ARVC/D in the patient under evaluation | |
| Minor | |
|
|
PLAX indicates parasternal long-axis view; RVOT, RV outflow tract; BSA, body surface area; PSAX, parasternal short-axis view; aVF, augmented voltage unipolar left foot lead; and aVL, augmented voltage unipolar left arm lead.
Diagnostic terminology for original criteria: This diagnosis is fulfilled by the presence of 2 major, or 1 major plus 2 minor criteria or 4 minor criteria from different groups. Diagnostic terminology for revised criteria: definite diagnosis: 2 major or 1 major and 2 minor criteria or 4 minor from different categories; borderline: 1 major and 1 minor or 3 minor criteria from different categories; possible: 1 major or 2 minor criteria from different categories.
*Hypokinesis is not included in this or subsequent definitions of RV regional wall motion abnormalities for the proposed modified criteria.
†A pathogenic mutation is a DNA alteration associated with ARVC/D that alters or is expected to alter the encoded protein, is unobserved or rare in a large non-ARVC/D control population, and either alters or is predicted to alter the structure or function of the protein or has demonstrated linkage to the disease phenotype in a conclusive pedigree.
At the time of the publication of the original Task Force guidelines, clinical experience with ARVC/D was dominated by symptomatic index cases and sudden cardiac death victims–the overt or severe end of the disease spectrum. Consequently, the 1994 criteria were highly specific, but they lacked sensitivity for early and familial disease.29–31
Over the past 15 years, additional ECG markers have been proposed.32–34 In addition, the genetic basis of the disease has been recognized, with the potential for mutation analysis. Experience with quantification of imaging criteria of ARVC/D has increased, and newer imaging techniques have been introduced, such as contrast-enhanced echocardiography, 3-dimensional echocardiography, cardiovascular magnetic resonance with late enhancement, and electroanatomic voltage mapping.35–40
Since publication of the 1994 Task Force guidelines, cardiovascular evaluation of the relatives of ARVC/D index cases and, more recently, genotype–phenotype association studies have also highlighted the shortcomings of the criteria. It is now recognized that LV involvement may occur early in the course of the disease with some frequency.4,41 The criteria also lack sensitivity for the diagnosis of familial disease. Modifications of the original criteria have been proposed to facilitate clinical diagnosis in first-degree relatives who often have incomplete expression of the disease.42 According to these recommendations, in the context of proven ARVC/D in a first-degree relative, the diagnosis of familial ARVC/D is based on the documentation of one of the following in a family member:
T-wave inversion in right precordial leads V1, V2, and V3 in individuals over the age of 14 years.
Late potentials by signal-averaged ECG (SAECG).
Ventricular tachycardia of left bundle-branch block morphology on ECG, Holter monitor, or during exercise testing or >200 premature ventricular contractions in 24 hours.
Either mild global dilatation or reduction in RV ejection fraction with normal LV or mild segmental dilatation of the RV or regional RV hypokinesis.
Revision of the diagnostic criteria is important to provide guidance on the role of emerging diagnostic modalities and to recognize advances in the genetics of ARVC/D. The criteria have been modified to incorporate new knowledge and technology to improve diagnostic sensitivity, but with the important requisite of maintaining diagnostic specificity, and they include quantitative parameters for Task Force criteria, particularly for the imaging studies (Table 1). The approach of classifying structural, histological, ECG, arrhythmic, and genetic features of the disease as major and minor criteria has been maintained.
Methods
A limitation of the previous Task Force criteria was the reliance on subjective criteria for assessing ventricular structure and function and for evaluation of myocardial histology. In this modification of the Task Force criteria, quantitative criteria are proposed and abnormalities are defined on the basis of comparison with normal subject data (Table 1). The data from 108 probands with newly diagnosed ARVC/D, age ≥12 years, who were enrolled in the National Institutes of Health-supported Multidisciplinary Study of Right Ventricular Dysplasia,43 were compared with those of normal subjects (online-only Data Supplement). The criteria were selected on the basis of analysis of sensitivity and specificity from receiver operating characteristic curves. For analysis of each test [e.g. echocardiogram, magnetic resonance imaging (MRI)], proband data were excluded if that test was crucial for the diagnosis of the individual patient. This was done to eliminate bias in estimating the sensitivity and specificity of that particular test. In general, when determining the sensitivity and specificity of a new screening test, it is recommended that none of the screening test elements be used in making the primary diagnosis; this principle also holds when establishing diagnostic criteria.
Results
There were 44 proband MRIs compared with 462 MRIs of normal subjects, 69 proband echocardiograms compared with 450 echocardiograms of normal subjects, 69 proband SAECGs compared with 103 SAECGs of normal subjects, and 68 proband Holters compared with 398 Holters of normal subjects. The minor criteria for echocardiography were selected where specificity and sensitivity are equal (sensitivity equals specificity) (Table 2). The major criteria were selected as the value that yielded 95% specificity. Sensitivity and specificity for the MRI criteria were made independently for each sex and with consideration of both the RV end-diastolic volume indexed to body surface area (size) and RV ejection fraction (function) simultaneously by using the OR logistical function. If either RV size or function was positive in conjunction with RV wall motion abnormality, then the subject would be classified as having a major criterion for the MRI. The sensitivity of RV size alone or function alone ranged from 41% to 50% for major criteria and 31% to 41% for minor criteria, with specificity of 96% to 100%. Using the OR logistical function improved the sensitivity of the MRI to 79% to 89% for major criteria and 68% to 78% for minor criteria.
Table 2.
Sensitivity and specificity of proposed RV imaging criteria*
| Value | Sensitivity, % | Specificity, % | |
|---|---|---|---|
| Echocardiogram | |||
| Major | |||
| PLAX RVOT (diastole) | ≥32 mm | 75 | 95 |
| Corrected for body size (PLAX/BSA) | ≥19 mm/m2 | ||
| PSAX RVOT (diastole) | ≥36 mm | 62 | 95 |
| Corrected for body size (PSAX/BSA) | ≥21 mm/m2 | ||
| Fractional area change | ≤33% | 55 | 95 |
| Minor | |||
| PLAX RVOT (diastole) | ≥29 mm | 87 | 87 |
| Corrected for body size (PLAX/BSA) | ≥16 to ≤18 mm/m2i | ||
| PSAX RVOT (diastole) | ≥32 mm | 80 | 80 |
| Corrected for body size (PSAX/BSA) | ≥18 to ≤20 mm/m2 | ||
| Fractional area change | ≤40% | 76 | 76 |
| MRI† | |||
| Major | |||
| Ratio of RV end-diastolic volume to BSA | |||
| Males | ≥110 mL/m2 | ||
| Females | ≥100 mL/m2 | 76 | 90 ♂ |
| or | 68 | 98 ♀ | |
| RV ejection fraction | ≤40% | ||
| Minor | |||
| Ratio of RV end-diastolic volume to BSA | |||
| Males | ≥100 mL/m2 | ||
| Females | ≥90 mL/m2 | 79 | 85 ♂ |
| or | 89 | 97 ♀ | |
| RV ejection fraction | ≤45% | ||
Abbreviations as in Table 1.
*All the major and minor criteria listed in this table are in addition to the requirement that regional wall motion abnormalities must also be present.
†The sensitivity and specificity for males and females are the same as listed if, in addition to the stated wall motion criteria, there is either abnormal RV size or function or both.
The original Task Force criteria list late potentials as a minor criterion. It has become common practice, though not based on evidence, to state that the SAECG is positive if 2 of the following 3 parameters are abnormal: filtered QRS duration (fQRS), root-mean square voltage of the terminal 40 ms of the QRS, or duration of the terminal QRS signal <40 µV. Analysis of each of the single parameters of the SAECG with late potentials by using a 40- to 250-Hz filter had a sensitivity ranging from 58% to 60%, with a specificity of 94% to 96%. Two of three parameters had a sensitivity of 66% and specificity of 95%, adding little advantage with regard to sensitivity and specificity. Using any one of the 3 SAECG parameters had a sensitivity of 74% and specificity of 92%.
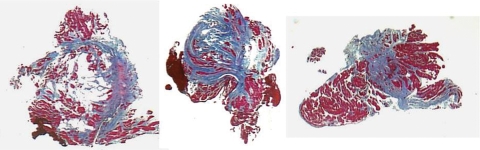
A definitive diagnosis of ARVC/D is based on histological demonstration of transmural fibrofatty replacement of RV myocardium at biopsy (Figure 2), necropsy, or surgery.5,44 In most patients, however, assessment of transmural myocardium is not possible. In addition, diagnosis based on RV endomyocardial biopsy specimens is limited because the segmental nature of the disease causes false negatives. Use of electroanatomic voltage mapping to identify pathological areas for biopsy sampling may improve the yield.45 RV free wall biopsy has a slight risk of perforation, but the more accessible interventricular septum rarely exhibits histological changes. Nevertheless, endomyocardial biopsy may identify other conditions (e.g. myocarditis, sarcoidosis, endomyocardial fibrosis), and the recognition of myocyte loss with fibrous or fibrofatty replacement can be a valuable diagnostic feature.46
Figure 2.
Endomyocardial biopsy findings in a proband affected by a diffuse form of ARVC/D. All 3 biopsy samples are from different regions of the RV free wall. There is extensive fibrofatty tissue replacement with myocardial atrophy, which is a major criterion (i.e. residual myocytes <60% by morphometric analysis or <50% if estimated). Contributed by C. Basso, Padua, Italy.
The identification of disease-causing genes has led to the recognition of a broader spectrum of disease expression within families, including individuals who have predominantly LV disease, manifest clinically by inferolateral T-wave changes, ventricular ectopy, or ventricular tachycardia with right bundle-branch block morphology and epicardial or midmyocardial late enhancement by MRI.4,7,38,39,41 The importance of familial disease highlights a role for mutation analysis of probands with cascade screening of relatives that offers an alternative strategy to serial noninvasive cardiovascular evaluation of families. A positive diagnosis in a family member changes the probability of disease in an individual suspected of the disease to 1:2 from 1:1000 to 1:5000. Thus, confirmed disease in a first degree relative is a major criterion for diagnosis.42
Discussion
The diagnosis of ARVC/D relies on the demonstration of structural, functional, and electrophysiological abnormalities that are caused by or reflect the underlying histological changes. Technical advances in MRI and 2-dimensional echocardiography have improved the capability to image the RV with reproducible measurements of volume and systolic function, which permits classification of severity and differentiation from normality47 (Table 2). Previous diagnostic reliance on subjective assessment of RV wall thinning, wall motion abnormalities, and fatty infiltration of the myocardium by MRI has proven problematic.48,49 Recognition of significant fatty involvement without concomitant fibrosis of the RV in normal individuals renders this unique MRI capability of limited value. Late enhancement on MRI permits myocardial tissue characterization in the LV. It can be difficult to be certain of late enhancement for characterization of RV myocardium because of the thin wall of the RV and possible confusion with fat.50
There also have been recent developments to quantify the extent of RV wall motion abnormalities by angiography with computer-based analysis, as well as to determine RV volumes.51,52 In addition, commercial software is available to determine RV volumes and ejection fraction.53 The RV angiogram obtained in multiple views is considered to be a reliable imaging test to assess wall motion abnormalities but requires considerable experience. Standardized protocols for performance of these diagnostic studies (ECG, SAECG, echocardiogram, RV angiogram, and MRI) are available on www.arvd.org.
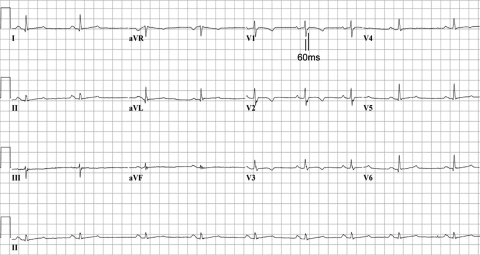
Repolarization abnormalities are early and sensitive markers of disease expression in ARVC/D. T-wave inversion in V1, V2, and V3 and beyond in individuals >14 years of age who are otherwise healthy is observed in only 4% of healthy women and 1% of men. Therefore, it is reasonably specific in this population and considered a major diagnostic abnormality in ARVC/D.54 Depolarization delay in right precordial leads is also common in ARVC/D.33,34 Evaluation of the duration of terminal QRS activation (Figure 3) incorporates slurring of the S wave, as well as R′, into a single measure of terminal activation duration.34 Depolarization abnormalities cannot be evaluated in the presence of typical complete right bundle-branch block with terminal delay in leads I and V6. However, T-wave inversion in V1, V2, V3, and V4 is uncommon in patients with right bundle-branch block who do not have ARVC/D and is seen frequently in those who do have the disease. Conventional definitions are used for ventricular arrhythmias. An abnormal SAECG is based on time domain criteria with cutoffs generated from receiver operating characteristic curves.55,56 The sensitivity and specificity of any one of the time domain criteria is similar to that of any 2 or 3 of these criteria; therefore, any one of the criteria is proposed as a criterion for this modality. The presence of left bundle-branch block ventricular tachycardia with an inferior axis (R wave positive in leads II and III and negative in lead aVL) is typical of focal RV outflow tract tachycardia.57 Similar features may be seen in patients with ARVC/D but usually coexist with anterior T-wave inversion and ventricular arrhythmias of varying morphologies. The presence of ventricular ectopy increases with age, but >200 ventricular premature beats in 24 hours in an adult <50 years of age suggests underlying myocardial disease.58
Figure 3.
ECG from proband with T-wave inversion in V1 through V4 and prolongation of the terminal activation duration ≥55 ms measured from the nadir of the S wave to the end of the QRS complex in V1. Contributed by M.G.P.J. Cox, Utrecht, The Netherlands.
The revised criteria were applied post hoc to 108 newly diagnosed probands enrolled in the Multidisciplinary Study of Right Ventricular Dysplasia, a study supported by the National Institutes of Health. They had been carefully evaluated, including assessment of diagnostic tests by expert core laboratories.43 Of the 73 probands with final classification as ‘affected’, 71 remain affected and 2 were reclassified as borderline. The change from affected to borderline in the 2 was due to the echocardiogram's fulfilling only minor criteria in one and only mild hypokinesis in the angiogram of the other. Of the 28 probands classified as borderline (met some but not all of the original Task Force criteria–i.e. 1 major and 1 minor or 3 minor), 5 remain borderline and 16 were reclassified by the new criteria as affected. Seven became unaffected (did not meet the proposed modified Task Force criteria). Of 7 probands previously classified as unaffected, 4 remained unaffected, 1 became affected, and 2 became borderline. Therefore, the effect of the revised criteria is to increase the sensitivity of the classification, primarily in probands previously classified as borderline.
Nine of 28 probands classified as borderline by original criteria had gene variants consistent with ARVC/D. The sensitivity of the revised criteria is not perfect, as exemplified by the observation that if the genetic criteria are ignored, the proposed criteria classified 2 as unaffected and 3 remained borderline, and 4 became affected. Including the proposed genetic criteria resulted in all 9 being classified as affected.
The modified Task Force criteria have been applied to 2 different sets of phenotyped-genotyped cohorts (N. Protonotarios et al. and M.D.G.J. Cox et al., unpublished data). In both studies, sensitivity increased without loss of specificity. Additionally, the ECG criteria have been applied to known ARVC/D cohorts and have shown an increase in diagnostic value.59
The proposed modifications of the original Task Force criteria represent a working framework to improve the diagnosis and management of ARVC/D. Awareness is growing that ARVC/D as such is the most well recognized form of a broad disease spectrum that includes left-dominant and biventricular subtypes. Lack of specific diagnostic guidelines contributes to under-recognition of non-classic disease. Future revisions of the Task Force criteria may fill this gap by incorporating features such as ventricular tachycardia of right bundle branch block morphology, subepicardial or midmyocardial late gadolinium enhancement of the LV myocardium, and global or regional LV dysfunction in patients presenting with arrhythmia rather than heart failure. With the identification of disease-causing genes, the potential exists for diagnostic mutation analysis and improved pedigree evaluation, with better understanding of natural history and pathogenesis and development of targeted therapies. Individuals who carry newly discovered disease-causing genes but who have incomplete or no disease expression will be recognized; their natural history and appropriate management remains to be determined.
Limitations
The reference values for the normal subjects have been determined from select populations from centers with expertise in the diagnostic test (online-only Data Supplement) because data on a large cohort of normal subjects studied by all the modalities were not available from any one center. Therefore, the reference values may not apply to all ethnic populations or those <12 years of age.
Supplementary material
Supplementary material is available at European Heart Journal online.
Funding
This project was supported by National Institutes of Health research grant R13 HL086825, funded by the National Heart, Lung & Blood Institute and the Office of Rare Disorders, and was supported in part by research grants U01-HL65594, U01-HL65652, U01-HL65691, and K23-HL093350 from the National Heart, Lung and Blood Institute of the National Institutes of Health, Bethesda, MD, and by research grant QLG1-CT-2000-01091 5th Framework Programme from the European Commission, Brussels, Belgium. Additional funding was obtained from the International Society for Holter and Noninvasive Electrocardiography and donations from the Peter French Memorial Foundation, United Desert Charities, the Podolsky Family Foundation, and private donors Mr and Mrs L. Becker, Mr and Mrs H. Danz, Mr K. Dorn, Mr T. Livolsi, Mr and Mrs L. Long, and Mr and Mrs H. Wilmerding.
Conflict of interest: none declared.
Supplementary Material
References
- 1.Basso C, Corrado D, Marcus FI, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373:1289–1300. doi: 10.1016/S0140-6736(09)60256-7. [DOI] [PubMed] [Google Scholar]
- 2.Marcus FI, Fontaine GH, Guiraudon G, Frank R, Laurenceau JL, Malergue C, Grosgogeat Y. Right ventricular dysplasia: a report of 24 adult cases. Circulation. 1982;65:384–398. doi: 10.1161/01.cir.65.2.384. [DOI] [PubMed] [Google Scholar]
- 3.Corrado D, Basso C, Thiene G, McKenna WJ, Davies MJ, Fontaliran F, Nava A, Silvestri F, Blomstrom-Lunquist C, Wlodarska EK, Fontaine G, Camerini F. Spectrum of clinicopathologic manifestation of arrhythmogenic right ventricular cardiomyopathy/dysplasia: a multicenter study. J Am Coll Cardiol. 1997;6:1512–1520. doi: 10.1016/s0735-1097(97)00332-x. [DOI] [PubMed] [Google Scholar]
- 4.Norman M, Simpson N, Mogensen J, Shaw A, Hughes S, Syrris P, Sen-Chowdhry S, Rowland E, Crosby A, McKenna WJ. Novel mutation in desmoplakin causes arrhythmogenic left ventricular cardiomyopathy. Circulation. 2005;112:636–642. doi: 10.1161/CIRCULATIONAHA.104.532234. [DOI] [PubMed] [Google Scholar]
- 5.Basso C, Thiene G. Autopsy and endomyocardial biopsy findings. In: Marcus FI, Nava A, Thiene G, editors. Milan, Italy: Springer Verlag; 2007. pp. 29–44. Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia. [Google Scholar]
- 6.Thiene G, Nava A, Corrado D, Rossi L, Pennelli N. Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med. 1988;318:129–133. doi: 10.1056/NEJM198801213180301. [DOI] [PubMed] [Google Scholar]
- 7.Sen-Chowdhry S, Syrris P, Ward D, Asimaki A, Sevdalis E, McKenna WJ. Clinical and genetic characterization of families with arrhythmogenic right ventricular dysplasia/cardiomyopathy provides novel insights into patterns of disease expression. Circulation. 2007;115:1710–1720. doi: 10.1161/CIRCULATIONAHA.106.660241. [DOI] [PubMed] [Google Scholar]
- 8.Protonotarios N, Tsatsopoulou A, Anastasakis A, Sevdalis E, McKoy G, Stratos K, Gatzoulis K, Tentolouris K, Spiliopoulou C, Panagiotakos D, McKenna W, Toutouzas P. Genotype–phenotype assessment in autosomal recessive arrhythmogenic right ventricular cardiomyopathy (Naxos disease) caused by a deletion in plakoglobin. J Am Coll Cardiol. 2001;38:1477–1484. doi: 10.1016/s0735-1097(01)01568-6. [DOI] [PubMed] [Google Scholar]
- 9.Carvajal-Huerta L. Epidermolytic-palmoplantar keratoderma with woolly hair and dilated cardiomyopathy. J Am Acad Dermatol. 1998;39:418–421. doi: 10.1016/s0190-9622(98)70317-2. [DOI] [PubMed] [Google Scholar]
- 10.Sen-Chowdhry S, Syrris P, McKenna WJ. Genetics of right ventricular cardiomyopathy. J Cardiovasc Electrophysiol. 2005;16:927–935. doi: 10.1111/j.1540-8167.2005.40842.x. [DOI] [PubMed] [Google Scholar]
- 11.Awad MM, Calkins H, Judge DP. Mechanisms of disease: molecular genetics of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Nat Clin Pract Cardiovasc Med. 2008;5:258–267. doi: 10.1038/ncpcardio1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKoy G, Protonotarius P, Crosby A, Tsatsopoulou A, Anastasakis A, Coonar A, Norman M, Baboonian C, Jeffrey S, McKenna WJ. Identification of a detection in plakoglobin in arrhythmogenic right ventricular cardiomyopathy with palmoplantar kertoderma and woolly hair (Naxos disease) Lancet. 2000;355:2119–2124. doi: 10.1016/S0140-6736(00)02379-5. [DOI] [PubMed] [Google Scholar]
- 13.Norgett EE, Hatsell SJ, Carvahal-Huerta L, Cabezas JR, Common J, Purkis PE, Whittock N, Leigh IM, Stevens HP, Kelsell DP. Recessive mutation in desmoplakin disrupts desmoplakin-intermediate filament interactions and causes dilated cardiomyopathy, woolly hair and keratoderma. Hum Mol Genet. 2000;9:2761–2766. doi: 10.1093/hmg/9.18.2761. [DOI] [PubMed] [Google Scholar]
- 14.Gerull B, Heuser A, Wichter T, Paul M, Basson CT, McDermott DA, Lerman BB, Markowitz SM, Ellinor PT, MacRae CA, Peters S, Grossmann KS, Michely B, Sasse-Klaassen S, Birchmeier W, Dietz R, Breithardt G, Schulze-Bahr G, Thierfelder L. Mutations in the desmosomal protein plakophilin-2 are common in arrhythmogenic right ventricular cardiomyopathy. Nat Genet. 2004;36:1162–1164. doi: 10.1038/ng1461. [DOI] [PubMed] [Google Scholar]
- 15.Awad MM, Dalal D, Cho E, Amat-Alarcon N, James C, Tichnell C, Tucker A, Russel SD, Bluemke DA, Dietz HC, Calkins H, Judge DP. DSG2 mutations contribute to arrhythmogenic right ventricular dysplasia/cardiomyopathy. Am J Hum Genet. 2006;79:136–142. doi: 10.1086/504393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pilichou K, Nava A, Basso C, Beffagna GB, Lorenzon A, Frigo G, Vettori A, Valente M, Towbin J, Thiene G, Danieli G, Rampazzo A. Mutations in desmoglein-2 gene are associated with arrhythmogenic right ventricular cardiomyopathy. Circulation. 2006;113:1171–1179. doi: 10.1161/CIRCULATIONAHA.105.583674. [DOI] [PubMed] [Google Scholar]
- 17.Syrris P, Ward D, Evans A, Asimaki A, Gandjbakhch E, Sen-Chowdhry S, McKenna WJ. Arrhythmogenic right ventricular dysplasia/cardiomyopathy associated with mutations in the desmosomal gene desmocollin-2. Am J Hum Genet. 2006;79:978–984. doi: 10.1086/509122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heuser A, Plovie ER, Ellinor PT, Grossmann KS, Shin JT, Wichter T, Basson CT, Lerman BB, Sasse-Klaassen S, Thierfelder L, MacRae CA, Gerull B. Mutant desmocollin-2 causes arrhythmogenic right ventricular cardiomyopathy. Am J Hum Genet. 2006;79:1081–1088. doi: 10.1086/509044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beffagna G, Occhi G, Nava A, Vitiello L, Ditadi A, Basso C, Bauce B, Carraro G, Thiene G, Towbin JA, Danieli GA, Rampazzo A. Regulatory mutations in transforming growth factor-ß3 gene cause arrhythmogenic right ventricular cardiomyopathy type 1. Cardiovasc Res. 2005;65:366–373. doi: 10.1016/j.cardiores.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Merner ND, Hodgkinson KA, Haywood AFM, Connors S, French VM, Drenckhahn JD, Kupprion C, Ramadanova K, Thierfelder L, McKenna W, Gallagher B, Morris-Larkin L, Bassett AS, Parfrey PS, Young TL. Arrhythmogenic right ventricular cardiomyopathy is a fully penetrant, lethal arrhythmic disorder caused by a missense mutation in the TMEM43 gene. Am J Hum Genet. 2008;82:1–13. doi: 10.1016/j.ajhg.2008.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saffitz JE. Cell adhesion pathology. In: Marcus FI, Nava A, Thiene G, editors. Milan, Italy: Springer Verlag; 2007. pp. 45–52. Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy. [Google Scholar]
- 22.Kaplan SR, Gard JJ, Protonotarios N, Tsatsopoulou A, Spiliopoulou C, Anastasakis A, Squarcioni CP, McKenna WJ, Thiene G, Basso C, Brousse N, Fontaine G, Saffitz JE. Remodeling of myocyte gap junctions in arrhythmogenic right ventricular cardiomyopathy due to a deletion in plakoglobin (Naxos disease) Heart Rhythm. 2004;1:3–11. doi: 10.1016/j.hrthm.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Vatta M, Marcus F, Towbin JA. Arrhythmogenic right ventricular cardiomyopathy: a ‘final common pathway’ that defines clinical phenotype. Eur Heart J. 2007;28:529–530. doi: 10.1093/eurheartj/ehl530. [DOI] [PubMed] [Google Scholar]
- 24.Tsatsopoulou A, Protonotarios N, McKenna WJ. Arrhythmogenic right ventricular dysplasia, a cell-adhesion cardiomyopathy: insights into disease pathogenesis from preliminary genotype–phenotype assessment. Heart. 2006;92:1720–1723. doi: 10.1136/hrt.2005.081679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Calabrese F, Angelini A, Thiene G, Basso C, Nava A, Valente M. No detection of enteroviral genome in the myocardium of patients with arrhythmogenic right ventricular cardiomyopathy. J Clin Pathol. 2000;53:382–387. doi: 10.1136/jcp.53.5.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fontaliran F, Fontaine G, Brestescher C, Labrousee J, Vilde F. Signification del infiltrats lymphoplasmocytaires dans la dyplasia ventriculare droite arhythmogene. Arch Mal Cœur. 1995;88:1021–1028. [PubMed] [Google Scholar]
- 27.Basso C, Thiene G, Corrado D, Angelini A, Nava A, Valente M. Arrhythmogenic right ventricular cardiomyopathy: dysplasia, dystrophy or myocarditis? Circulation. 1996;94:983–991. doi: 10.1161/01.cir.94.5.983. [DOI] [PubMed] [Google Scholar]
- 28.McKenna WJ, Thiene G, Nava A, Fontaliron F, Blomstrom-Lundquist G, Fontaine G, Camerini F on behalf of the Task Force of the working group myocardial and pericardial disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Diagnosis of arrhythmogenic right ventricular dysplasia cardiomyopathy. Br Heart J. 1994;71:215–218. doi: 10.1136/hrt.71.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Antoniades L, Tsatsopoulou A, Anastasakis A, Syrris P, Asimaki A, Panagiotakos D, Zambartas C, Stefanadis C, McKenna WJ, Protonotarios N. Arrhythmogenic right ventricular cardiomyopathy caused by deletions in plakophilin-2 and plakoglobin (Naxos Disease) in families from Greece and Cyprus: genotype–phenotype relations, diagnostic features and prognosis. Eur Heart J. 2006;27:2008–2016. doi: 10.1093/eurheartj/ehl184. [DOI] [PubMed] [Google Scholar]
- 30.Ward D, Syrris P, Sen-Chowdhry S, McKenna WJ. Diagnosis: task force criteria including modifications for family members. In: Marcus FI, Nava A, Thiene G, editors. Milan, Italy: Springer Verlag; 2007. pp. 87–96. Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia. [Google Scholar]
- 31.Marcus FI, Sherrill D. Strengths and weaknesses of the task force criteria: proposed modifications in arrhythmogenic right ventricular cardiomyopathy/dysplasia. In: Marcus FI, Nava A, Thiene G, editors. Milan, Italy: Springer Verlag; 2007. pp. 97–104. Arrhythmogenic Right Ventricular Cardiomyopathy Dysplasia. [Google Scholar]
- 32.Peters S, Trummel M. Diagnosis of arrhythmogenic right ventricular dysplasia-cardiomyopathy: value of standard ECG revisited. Ann Noninvasive Electrocardiol. 2003;8:238–245. doi: 10.1046/j.1542-474X.2003.08312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nasir K, Bomma C, Tandri H, Roguin A, Dalal D, Prakasa K, Tichnell C, James C, Spevak PJ, Marcus F, Calkins H. Electrocardiographic features of arrhythmogenic right ventricular dysplasia/cardiomyopathy according to disease severity: a need to broaden diagnostic criteria. Circulation. 2004;110:1527–1534. doi: 10.1161/01.CIR.0000142293.60725.18. [DOI] [PubMed] [Google Scholar]
- 34.Cox MGPJ, Nelen MR, Wilde AAM, Wiesfeld AC, van der Smagt J, Loh P, Cramer MJ, Doevendans PA, van Tintelen JP, de Bakker JMT, Hauer RNW. Activation delay and VT parameters in arrhythmogenic right ventricular dysplasia/cardiomyopathy: toward improvement of diagnostic ECG criteria. J Cardiovasc Electrophysiol. 2008;19:775–781. doi: 10.1111/j.1540-8167.2008.01140.x. [DOI] [PubMed] [Google Scholar]
- 35.Yoerger DM, Marcus F, Sherrill D, Calkins H, Towbin JA, Zareba W, Picard M. Echocardiographic findings in patients meeting task force criteria for arrhythmogenic right ventricular dysplasia. J Am Coll Cardiol. 2005;45:860–865. doi: 10.1016/j.jacc.2004.10.070. [DOI] [PubMed] [Google Scholar]
- 36.Prakasa KR, Dalal D, Wang J, Bomma C, Tandri H, Dong J, James C, Tichnell C, Russell SD, Spevak P, Corretti M, Bluemke DA, Calkins H, Abraham TP. Feasibility and variability of three dimensional echocardiography in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Am J Cardiol. 2006;97:703–709. doi: 10.1016/j.amjcard.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 37.Tandri H, Friedrich MG, Calkins H, Bluemke DA. MRI of arrhythmogenic right ventricular cardiomyopathy/dysplasia. J Cardiovasc Magn Reson. 2004;6:557–563. doi: 10.1081/jcmr-120030583. [DOI] [PubMed] [Google Scholar]
- 38.Sen-Chowdhry S, Prasad SK, Syrris P, Wage R, Ward D, Merrifield R, Smith GC, Firmin DN, Pennell DJ, McKenna WJ. Cardiovascular magnetic resonance in arrhythmogenic right ventricular cardiomyopathy revisited: comparison with task force criteria and genotype. J Am Coll Cardiol. 2006;48:2132–2140. doi: 10.1016/j.jacc.2006.07.045. [DOI] [PubMed] [Google Scholar]
- 39.Sen-Chowdhry S, Prasad SK, McKenna WJ. Complementary role of echocardiography and cardiac magnetic resonance in the non-invasive evaluation of suspected arrhythmogenic right ventricular cardiomyopathy. J Interv Card Electrophysiol. 2004;11:15–17. doi: 10.1023/B:JICE.0000035923.16175.78. [DOI] [PubMed] [Google Scholar]
- 40.Corrado D, Basso C, Leoni L, Tokajuk B, Bauce B, Frigo G, Tarantini G, Napodano M, Turrini P, Ramondo A, Daliento L, Nava A, Buja G, Iliceto S, Thiene G. Three-dimensional electroanatomic voltage mapping increases accuracy of diagnosing arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2005;111:3042–3050. doi: 10.1161/CIRCULATIONAHA.104.486977. [DOI] [PubMed] [Google Scholar]
- 41.Sen-Chowdhry S, Syrris P, Prasad SK, Hughes SE, Merrifield R, Ward D, Pennell DJ, McKenna WJ. Left-dominant arrhythmogenic cardiomyopathy: an under-recognized clinical entity. J Am Coll Cardiol. 2008;52:2175–2187. doi: 10.1016/j.jacc.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 42.Hamid MS, Norman M, Quraishi A, Firoozi S, Thaman R, Gimeno JR, Sachdev B, Rowland E, Elliott PM, McKenna WJ. Prospective evaluation of relatives for familial arrhythmogenic right ventricular cardiomyopathy/dysplasia reveals a need to broaden diagnostic criteria. J Am Coll Cardiol. 2002;40:1445–1450. doi: 10.1016/s0735-1097(02)02307-0. [DOI] [PubMed] [Google Scholar]
- 43.Marcus FI, Zareba W, Calkins H, Towbin JA, Basso C, Bluemke DA, Estes NAM, Picard MH, Sanborn DY, Thiene G, Wichter T, Cannom D, Wilber DJ, Scheinman M, Duff H, Daubert J, Talajic M, Krahn A, Sweeney M, Garan H, Sakaguchi S, Lerman BB, Kerr C, Kron J, Steinberg JS, Sherrill D, Gear K, Brown M, Severski P, Polonsky S, McNitt S. Arrhythmogenic right ventricular cardiomyopathy/dysplasia, clinical presentation and diagnostic evaluation: results from the North American Multidisciplinary Study. Heart Rhythm. 2009;6:984–992. doi: 10.1016/j.hrthm.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Basso C, Burke M, Fornes P, Gallagher PJ, de Gouveia RH, Sheppard M, Thiene G, van der Wal A on behalf of the Association for European Cardiovascular Pathology. Guidelines for autopsy investigation of sudden cardiac death. Virchows Arch. 2008;452:11–18. doi: 10.1007/s00428-007-0505-5. [DOI] [PubMed] [Google Scholar]
- 45.Avella A, D'Amati G, Pappalardo A, Re F, Silenzi PF, Laurenzi F, De Girolamo P, Pelargonia G, Messina G, Xecchi P, Zachara E, Tondo C. Diagnostic value of endomyocardial biopsy guided by electroanatomic voltage mapping in arrhythmogenic right ventricular cardiomyopathy/dysplasia. J Cardiovasc Electrophysiol. 2008;19:1127–1134. doi: 10.1111/j.1540-8167.2008.01228.x. [DOI] [PubMed] [Google Scholar]
- 46.Basso C, Ronco F, Marcus F, Abudureheman A, Rizzo S, Frigo AC, Bauce B, Maddalena F, Nava A, Corrado D, Grigoletto F, Thiene G. Quantitative assessment of endomyocardial biopsy in arrhythmogenic right ventricular cardiomyopathy/dysplasia: an in vitro validation of diagnostic criteria. Eur Heart J. 2008;29:2760–2771. doi: 10.1093/eurheartj/ehn415. [DOI] [PubMed] [Google Scholar]
- 47.Tandri H, Daya SK, Nasir K, Bomma C, Lima JAC, Calkins H, Bluemke DA. Normal reference values for the adult right ventricle by magnetic resonance imaging. Am J Cardiol. 2006;98:1660–1664. doi: 10.1016/j.amjcard.2006.07.049. [DOI] [PubMed] [Google Scholar]
- 48.Bluemke DA, Krupinski EA, Ovitt T, Gear K, Unger E, Axel L, Boxt LM, Casolo G, Ferrari VA, Funaki B, Globits S, Higgins CB, Julsrud P, Lipton N, Mawson J, Nygren A, Pennell DJ, Stillman A, White RD, Wichter T, Marcus F. MRI Imaging of arrhythmogenic right ventricular cardiomyopathy: morphological findings and intraobserver reliability. Cardiology. 2003;99:153–162. doi: 10.1159/000070672. [DOI] [PubMed] [Google Scholar]
- 49.Bomma C, Rutberg J, Tandri H, Nasir K, Roguin A, Tichnell C, Rodriguez R, Kasper E, Spevak P, Bluemke DA, Calkins H. Misdiagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Cardiovasc Electrophysiol. 2004;15:300–306. doi: 10.1046/j.1540-8167.2004.03429.x. [DOI] [PubMed] [Google Scholar]
- 50.Tandri H, Saranathan M, Rodriguez R, Martinez C, Bomma C, Nasir K, Rosen B, Lima JA, Calkins H, Bluemke DA. Noninvasive detection of myocardial fibrosis in arrhythmogenic right ventricular cardiomyopathy using delayed-enhancement magnetic resonance imaging. J Am Coll Cardiol. 2005;45:98–103. doi: 10.1016/j.jacc.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 51.Indik JH, Dallas WJ, Ovitt T, Wichter T, Gear K, Marcus FI. Do patients with right ventricular outflow tract ventricular arrhythmias have a normal right ventricular wall motion? Cardiology. 2005;104:10–15. doi: 10.1159/000086047. [DOI] [PubMed] [Google Scholar]
- 52.Indik JH, Wichter T, Gear K, Dallas WJ, Marcus FI. Quantitative assessment of angiographic right ventricular wall motion in arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) J Cardiovasc Electrophysiol. 2008;19:39–45. doi: 10.1111/j.1540-8167.2007.00974.x. [DOI] [PubMed] [Google Scholar]
- 53.Wellnhofer E, Ewert P, Hug J, Hui W, Kretschmar O, Chavengsuk D, Kuhne T, Abdul-Khalig H, Nagel E, Lange PE, Fleck E. Evaluation of new software for angiographic determination of right ventricular volumes. Int J Cardiovasc Imaging. 2005;21:575–585. doi: 10.1007/s10554-005-1797-7. [DOI] [PubMed] [Google Scholar]
- 54.Marcus FI. Prevalence of T-wave inversion beyond V1 in young normal individuals and usefulness for the diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Am J Cardiol. 2005;95:1070–1071. doi: 10.1016/j.amjcard.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 55.Marcus FI, Zareba W, Sherrill D. Evaluation of the normal values for signal-averaged electrocardiogram. J Cardiovasc Electrophysiol. 2007;18:231–233. doi: 10.1111/j.1540-8167.2006.00685.x. [DOI] [PubMed] [Google Scholar]
- 56.Kamath GS, Zareba W, McKenna WJ, Gear K, Sherrill D, Marcus F, Steinberg JS. Value of signal averaged electrocardiogram for the diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Heart Rhythm. 2008;5(Suppl.):S38. doi: 10.1016/j.hrthm.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ainsworth CD, Skanes AC, Klein GJ, Gula LJ, Yee R, Krahn AD. Differentiating arrhythmogenic right ventricular cardiomyopathy from right ventricular outflow tract ventricular tachycardia using multilead QRS duration and axis. Heart Rhythm. 2006;3:416–423. doi: 10.1016/j.hrthm.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 58.DePaula SR, Antelmi I, Vincenzi MA, Andre CD, Artes R, Grupi CJ, Mansur AJ. Cardiac arrhythmias and atrioventricular block in a cohort of asymptomatic individuals without heart disease. Cardiology. 2007;108:111–116. doi: 10.1159/000095950. [DOI] [PubMed] [Google Scholar]
- 59.Cox MGPJ, van der Smagt JJ, Wilde AM, Wiesfeld ACP, Atsma DE, Nelen MR, Rodriguez LM, Loh P, Cramer MJ, Doevendans PA, van Tintelen JP, de Bakker JMT, Hauer RNW. New ECG criteria in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circ Arrhythm Electrophysiol. 2009;2:524–530. doi: 10.1161/CIRCEP.108.832519. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.