Abstract
The Cardiac Arrhythmia Suppression Trial demonstrated that antiarrhythmic drugs not only fail to prevent sudden cardiac death, but actually increase overall mortality. These findings have been confirmed in additional trials. The “proarrhythmic” effects of most currently available antiarrhythmic drugs makes it essential that we investigate novel strategies for the prevention of sudden cardiac death. Targeted ablation of cardiac sympathetic neurons may become a therapeutic option by reducing sympathetic activity. Thus cholera toxin B subunit (CTB) conjugated to saporin (a ribosomal inactivating protein that binds to and inactivates ribosomes; CTB-SAP) was injected into both stellate ganglia to test the hypothesis that targeted ablation of cardiac sympathetic neurons reduces the susceptibility to ischemia-induced, sustained ventricular tachycardia in conscious rats. Rats were randomly divided into three groups: 1) control (no injection); 2) bilateral stellate ganglia injection of CTB; and 3) bilateral stellate ganglia injection of CTB-SAP. CTB-SAP rats had a reduced susceptibility to ischemia-induced, sustained ventricular tachycardia. Associated with the reduced susceptibility to ventricular arrhythmias were a reduced number of stained neurons in the stellate ganglia and spinal cord (segments T1-T4), as well as a reduced left ventricular norepinephrine content and sympathetic innervation density. Thus CTB-SAP retrogradely transported from the stellate ganglia is effective at ablating cardiac sympathetic neurons and reducing the susceptibility to ventricular arrhythmias.
Keywords: cholera toxin B subunit, stellate ganglion, neurotoxin, saporin, sympathectomy
ischemia-induced sudden cardiac death, resulting from ventricular tachyarrhythmias, remains the leading cause of death in industrially developed countries (7). Myocardial ischemia increases cardiac sympathetic activity that contributes to the formation of malignant ventricular arrhythmias. For example, Schwartz (25, 44) and colleagues demonstrated that myocardial ischemia provokes a powerful increase in cardiac sympathetic efferent activity that directly promotes ventricular tachycardia. Furthermore, sympathetic nerve activity increases before the onset of ventricular tachyarrhythmias in conscious dogs (62).
Importantly, interventions that reduce cardiac sympathetic activity protect against ventricular tachyarrhythmias. Accordingly, efforts to reduce sympathetic activity are the first-line therapy for ventricular arrhythmias. For example, β-adrenergic-receptor blockade reduces mortality due to sudden death by 30–50% (14, 29, 39, 53, 56). However, despite these favorable outcomes, the mortality following myocardial infarction, even when placed on optimal β-adrenergic-receptor antagonist therapy (2), remains high among patients with ventricular dysfunction. Specifically, the 1-yr mortality is 10% or higher, with sudden death accounting for approximately one-third of the deaths in these high-risk patients (2). Furthermore, adverse complications (due to generalized sympathoinhibition; e.g., fatigue, impotence) limit compliance to these agents.
Surgical ablation of cardiac sympathetic nerves provides a more complete protection from arrhythmias (41, 42). For example, surgical excision of the left stellate ganglion (LSG) increases the ventricular fibrillation (VF) threshold and reduces arrhythmias induced by myocardial ischemia in animal models (43, 46, 49). Similarly left cardiac sympathetic denervation (stellate ganglion, together with second and third thoracic ganglia ablation) reduces arrhythmias in high-risk patients following myocardial infarction (52), patients with long QT syndrome (10, 45), and patients with catecholaminergic polymorphic ventricular tachycardia (10, 60). However, the potential complications associated with this procedure include Horner's syndrome [ptosis (drooping of the upper eyelid), upside-down ptosis (slight elevation of the lower lid), miosis (constricted pupil), dilation lag (slow response of the pupil to light), enophthalmos (the impression that the eye is sunk in), and anhydrosis (decreased sweating)], paraesthesia, compensatory hyperhidrosis, and residual flushing, as well as death in the individuals undergoing the procedure for intractable angina (37). These complications severely limit patient satisfaction with the procedure. However, targeted ablation of cardiac sympathetic neurons may reduce the incidence of these complications, as well as maintain afferent function (21).
Saporin (SAP) is a ribosomal inactivating protein that binds to and inactivates ribosomes, disabling the cell's protein synthetic machinery and causing the cell to die over a period of hours to days (1, 28, 34). SAP can be linked to molecules that allow targeting of the toxin to a precisely defined population of cells (19). For example, SAP can be linked to retrogradely transported molecules, like cholera toxin B (CTB) subunit that binds to specific membrane components that are differentially expressed on nerve cells. This provides a means for targeting SAP to a subset of neurons that could not previously be selectively ablated. Specifically, SAP conjugated to CTB (CTB-SAP), which binds to GM1 gangliosides located in the plasma membranes of sympathetic preganglionic neurons (SPNs), could be used to ablate SPNs by injecting the compound into the stellate ganglia. In fact, our laboratory recently demonstrated that CTB-SAP retrogradely transported from the stellate ganglia is effective at ablating cardiac sympathetic neurons and reducing resting, exercise, and reflex sympathetic activity (21).
Therefore, we tested the hypothesis that bilateral stellate ganglia injection of SAP conjugated to CTB reduces the susceptibility to ischemia-induced sustained ventricular tachycardia. We hypothesized that SAP would reduce the number of sympathetic postganglionic neurons in the stellate ganglia and virtually eliminate SPNs of spinal cord segments T1-T4 without altering afferent neurons. We also hypothesized that SAP would reduce left ventricular sympathetic innervation density and norepinephrine content. We determined the size and number of sympathetic postganglionic neurons in the stellate ganglia, as well as SPNs in spinal cord segments T1-T4. We also determined left ventricular sympathetic innervation density and norepinephrine content. To document that afferent neurons were not altered by SAP, we examined the dorsal root ganglia of spinal segments T1-T4. Finally, we hypothesized that the loss of cardiac projecting sympathetic neurons would reduce the susceptibility to ischemia-induced sustained ventricular tachycardia. We studied conscious, chronically instrumented rats to negate the confounding effects of anesthetic agents and surgical trauma.
MATERIALS AND METHODS
Surgical Procedures
Experimental procedures and protocols were reviewed and approved by the Animal Care and Use Committee of Wayne State University and adhered to the American Physiological Society's Guiding Principles in the Care and Use of Animals. Twenty-one adult Sprague-Dawley male rats were randomly divided into three groups: 1) control (no injection; n = 7); 2) bilateral stellate ganglia injection of unconjugated CTB (n = 5); and 3) bilateral stellate ganglia injection of CTB conjugated to SAP (CTB-SAP; n = 9). In addition, hearts from a separate group of rats (4 control noninjected, 5 CTB injected, and 5 CTB-SAP injected) were analyzed for left ventricular sympathetic innervation density (tyrosine hydroxylase immunoreactivity) and norepinephrine content. All surgical procedures were performed using aseptic surgical techniques. Rats were anesthetized with pentobarbital sodium (50 mg/kg ip), atropinized (0.05 mg/kg ip), intubated, and prepared for aseptic surgery. Supplemental doses of pentobarbital sodium (10–20 mg/kg ip) were administered, if the rat regained the blink reflex or responded during the surgical procedures.
Radiotelemetry implantation.
After anesthesia was induced, a telemetry device (Data Sciences International PhysioTel C50-PXT; pressure, temperature, and electrocardiogram) was implanted in all rats, as previously described (9, 38), and a catheter was placed in the intraperitoneal (IP) space for the infusion of fluids and drugs. Specifically, the transmitter body, which contains the thermistor, and the IP catheter were placed in the IP space through a ventral abdominal approach. The IP catheter was exteriorized on the dorsal aspect of the neck. The pressure sensor of the telemetry device, located within the tip of a catheter, was inserted into the descending aorta for continuous, nontethered, recording of pulsatile arterial blood pressure. The electrical leads from the telemetry device were placed in a modified lead II configuration by placing the negative electrode slightly to the right of the manubrium and the positive electrode at the anterior axillary line along the fifth intercostal space. A minimum of 1 wk was allowed for recovery and for the animals to regain their presurgical weight. During the recovery period, the rats were handled, weighed, and acclimatized to the laboratory and investigators.
Thoracotomy procedures.
After the recovery period, the animals were anesthetized as described above, and the hearts were approached via a left thoracotomy through the fourth intercostal space. A coronary artery occluder was made from an atraumatic needle holding 5.0-gauge prolene suture (8720H, Ethicon). The needle and suture were passed around the left main coronary artery 2–3 mm from the origin by inserting the needle into the left ventricular wall under the overhanging left atrial appendage and bringing it out high on the pulmonary conus. The needle was cut from the suture, and the two ends of the suture were passed through a PE-50 polyethylene guide tubing. The guide tubing with the two ends of the suture were then exteriorized and secured at the back of the neck. The tubing was filled with a mixture of Vaseline and mineral oil to prevent a pneumothorax. At least 1 wk was allowed for recovery. During the recovery period, the rats were handled, weighed, and acclimatized to the laboratory and investigators.
Stellate ganglia injections.
After the recovery period, the animals were anesthetized as described above, and the stellate ganglia were approached (one at a time) via a ventral thoracotomy through the first intercostal space. Specifically, a 2-cm midline incision was made, and the left and subsequently the right pectoral and intercostal muscles were partially dissected (∼5 mm) between the first and second rib to obtain access to the left and subsequently the right stellate ganglion (RSG), which are localized dorsal of the subclavian artery and vein. Four microliters of CTB subunit (1 mg CTB dissolved in 200 μl of distilled water) or 4 μl of CTB conjugated with SAP (2.5 mg/ml; Advanced Targeting Systems, San Diego, CA, catalog no. IT-14) were mixed with 1 μl of 3% Evans blue dye. The purpose of the Evans blue dye was to visualize the injectate (CTB and SAP are colorless), ensuring localization within the ganglia. All injections were confined within the stellate ganglia. The CTB/Evans blue dye or CTB-SAP/Evan blue dye solutions (∼5-μl total volume) were mineral oil pressure injected into the RSG and LSG using a glass micropipette (10–15 micron tip). A minimum of 1 wk was allowed for recovery and for the animals to regain their presurgical weight. Three separate surgeries (telemetry, thoracotomy, and stellate injections) were performed, because the animals recover significantly better than if three major surgeries are conducted during one session.
Experimental Procedures
Ventricular arrhythmia threshold.
Conscious, unrestrained rats were studied in their home cages for all experiments. Rats were allowed to adapt to the laboratory environment for ∼1 h to ensure stable hemodynamic conditions. After the stabilization period, beat by beat, steady-state preocclusion hemodynamic variables were recorded over 10–15 s. Subsequently, the left main coronary artery was temporarily occluded by use of the prolene suture. Specifically, acute coronary artery occlusion was performed by pulling up on the suture that was around the left main coronary artery (Fig. 1) (20). Rapid changes in the ECG (peaked T wave followed by S-T segment elevation) and arterial pressure occur within seconds of pulling on the suture, documenting coronary artery occlusion. The coronary artery occlusion was maintained until the onset of sustained ventricular tachycardia, but no longer than 10 min to prevent permanent myocardial damage (31). The ventricular arrhythmia threshold (VAT) was defined as the time from coronary artery occlusion to sustained ventricular tachycardia, resulting in a reduction in arterial pressure. If the time to sustained ventricular tachycardia exceeded 10 min, the occlusion was stopped, and 10 min was used as the VAT. Ventricular tachycardia was defined as sustained ventricular rate (absence of p wave, wide bizarre QRS complex) >1,000 beats/min, with a reduction in arterial pressure to ∼40 mmHg. Normal sinus rhythm appeared on termination of the occlusion by gently compressing the thorax. Without compressing the thorax, the sustained ventricular tachycardia progresses to VF. VF was defined as a ventricular rhythm without recognizable QRS complex, in which signal morphology changed from cycle to cycle, and for which it was impossible to estimate heart rate (HR). In the event that the animal did not resume normal sinus rhythm, cardioversion was achieved (after the rat lost consciousness) with the use of one shock (10 J) of DC current.
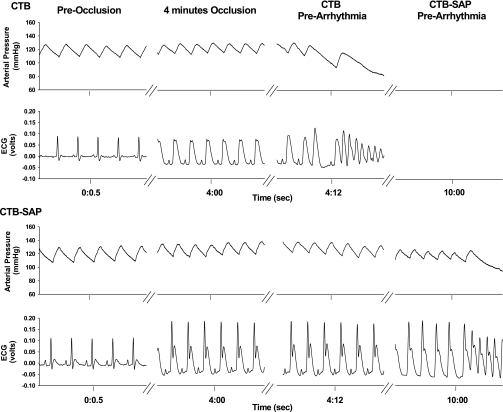
Fig. 1.
One-second analog recordings of arterial pressure and the electrocardiogram (ECG) before coronary artery occlusion (preoccclusion), at 4 min of occlusion, and at the onset of sustained ventricular tachycardia and reduction in arterial pressure (prearrhythmia) from two rats. Each rat received bilateral stellate injections of cholera toxin B (CTB; top) or CTB-saporin (SAP; bottom). The time from coronary artery occlusion to the onset of sustained ventricular tachycardia and reduction in arterial pressure was defined as the ventricular arrhythmia threshold. Coronary artery occlusion was documented by ST segment elevation. Note the higher ST segment elevation in the CTB rat compared with the CTB-SAP rat at 4 min of occlusion. CTB-SAP rats had a significantly longer ventricular arrhythmia threshold compared with control and CTB rats. In this example, the sustained ventricular tachycardia and reduction in arterial pressure occurred at 4 min and 12 s in the CTB rat compared with 10 min in the CTB-SAP rat.
Perfusion, tissue processing, and immunohistochemistry.
After completion of the studies (∼2 wk), the rats were deeply anesthetized with pentobarbital sodium (100 mg/kg), injected with heparin (1,000 IU), and flushed transcardially with 500-ml oxygenated tissue culture medium (catalogue no. D-8900; Sigma, St. Louis, MO), followed by 1 liter of 4% formaldehyde in 0.1 M phosphate buffer, pH 7.4. Spinal cords, stellate, and dorsal root ganglia from all rats were removed and postfixed intact in formaldehyde for 3 days at room temperature on a shaker. The heart and a short segment of the ascending aorta were excised with the occluder intact for subsequent determination of the ischemic zone (see below). After postfixation, the thoracic spinal cords segments (T1-T4) were removed. The rostral edge of each dorsal root entry zone was taken as the rostral boundary for each segment. Blocks of thoracic segments T1-T4 were obtained because SPNs projecting to the stellate ganglia are concentrated in these segments (55). Spinal cords and ganglia were cryoprotected in increasing concentrations of sucrose (10, 20, and 30%), embedded in OCT, and stored at −80°C until analysis.
A separate group of rats (4 control noninjected, 5 CTB injected, and 5 CTB-SAP injected) were deeply anesthetized with pentobarbital sodium (100 mg/kg) and flushed transcardially with 500-ml oxygenated tissue culture medium. A small section of the left ventricular free wall was carefully dissected from the heart, flash frozen in liquid nitrogen, and stored at −80°C until analysis for norepinephrine content (see below). Subsequently, the rats were perfused transcardially with 4% formaldehyde. The remaining left ventricular free wall was cryoprotected in increasing concentrations of sucrose (10, 20, and 30%), embedded in OCT, and stored at −80°C until analysis.
The stellate and dorsal root ganglia (T1-T4) were sectioned at 10-μm intervals, mounted on Superfrost Plus slides (Fisher), and stained with cresyl violet. The cardiac sympathetic postganglionic cell bodies, on every 10th section, were counted and measured with the aid of a ×20 objective and MicroBrightField Neurolucida software interfaced with BH-2 Olympus microscope. Only neurons with distinct, prominent nucleoli were counted. Based on a study by Jones (15), no correction for split nucleoli is necessary in 10-μm sections.
The spinal cord (T1-T4) were sectioned horizontally at 10-μm intervals, mounted on Superfrost Plus slides, and stored at −20°C until analysis. On the day of the analysis, the slides were brought to room temperature, air dried, rinsed (3 × 10 min each) in Tris phosphate-buffered saline, pH 7.4 (TPBS) containing 0.03% Triton X-100 (TPBS-Triton), then incubated in 10% heat-inactivated normal horse serum (NHS; Invitrogen) in TPBS-Triton for at least 1 h. Spinal cord slides were incubated in goat anti-CTB antiserum (1:10,000, List Biologicals) in TPBS-Triton containing 10% NHS for 48 h at room temperature. After rinsing (TPBS, 3 × 10 min each), slides were incubated with biotinylated donkey anti-goat immunoglobulin (1:500, Jackson Laboratories) in TPBS-Triton with 1% NHS overnight at room temperature. Slides were rinsed again (TPBS, 3 × 10 min each) and incubated 4–6 h in 1:1,500 ExtrAvidinperoxidase in TPBS-Triton (catalog no. E-2886; Sigma). Immunoreactive axons were revealed with the nickel-intensified diaminobenzidine reaction (18). Consistent with recent findings (21), bilateral injection of CTB into the stellate ganglia revealed many immunopositive neurons, whereas bilateral injection of CTB-SAP revealed no neurons (see Fig. 5).
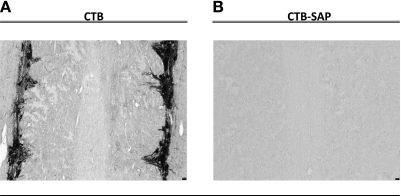
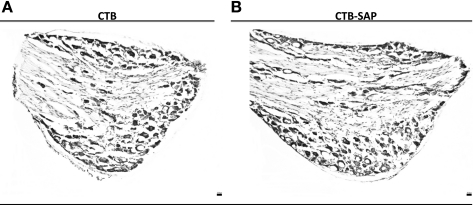
Fig. 5.
Horizontal sections of spinal cord segments T1-T4 from two rats that had CTB (A) or CTB-SAP (B) injected into both stellate ganglia. Many CTB-immunoreactive sympathetic preganglionic neurons are identified in the CTB rat; however, none is observed in the CTB-SAP rat. CTB-immunoreactive sympathetic preganglionic neurons are seen in the intermediolateral cell column, lateral funiculus, intercalated nucleus, and central automomic nucleus. Scale bar (bottom right) = 25 μm.
Heart tissue was processed in a similar manner to the spinal cord tissue, with the exception of the primary and secondary antibodies. Briefly, heart blocks were cut in transverse cross sections, at 10-μm intervals, mounted on Superfrost Plus slides, and stored at −20°C until analysis. On the day of analysis, the slides were air dried, incubated in rabbit anti-tyrosine hydroxylase (Millipore, 1:300) for 5 days at 4°C, then in 1:500 biotinylated donkey anti-rabbit immunoglobin (Jackson Laboratories) overnight at room temperature, and finally in 1:1,500 ExtrAvidinperoxidase. Tyrosine hydroxylase immunoreactivity was revealed with nickel-intensified diaminobenzidine reaction. Heart tissue obtained from control and CTB-injected animals revealed many tyrosine hydroxylase immunopositive sympathetic terminals, whereas heart tissue from CTB-SAP-injected animals revealed fewer terminals (see Fig. 7).
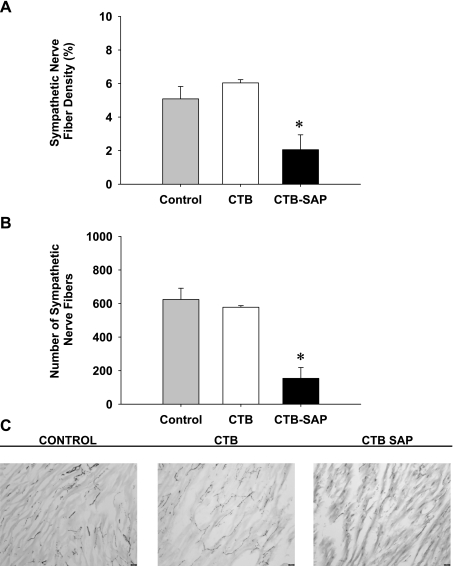
Fig. 7.
Tyrosine hydroxylase-immunoreactive fiber density (A), fiber number (B), and stained sympathetic fibers (C) from rats that had no injection (control), CTB, or CTB-SAP injected into both stellate ganglia. The CTB-SAP group showed a significant reduction in sympathetic nerve fiber density and number compared with the control and CTB groups. These results are consistent with C, showing many sympathetic fibers in the control and CTB groups and few sympathetic fibers in the CTB-SAP group. Values are means ± SE. *P < 0.05, CTB-SAP vs. control or CTB.
For cardiac innervation density analysis, photos were obtained using consistent camera settings from sections that had been processed together. Identical areas of the heart were analyzed for each rat: two regions of the left ventricle were quantified from each section by threshold discrimination with the aid of a ×20 objective using the MicroBrightField Neurolucida software interfaced with BH-2 Olympus microscope. Photos for analysis were obtained from four sections per heart, with each section separated from the others by at least 250 μm. Sections were quantified from three rats of each group.
Determination of ischemic zone and infarction.
To determine the size of the ischemic zone, the heart was perfused via the aorta with 30 ml of 0.9% saline to wash out the blood. Subsequently, the left main coronary artery was occluded by tying the suture. Evans Blue dye (100 μl, 0.5%) was perfused via the aorta, allowing the dye to infuse into the nonischemic area of the heart, leaving the ischemic regions unstained.
The heart was then sliced from base to apex into six to eight sections (∼2 mm thickness). Each section was compressed between two microscope slides, separated by a distance of 2 mm, to achieve uniform thickness. Images of each section were taken with a 3-megapixel digital camera mounted on a microscope. The total section area and the ischemic area of each slice were quantified using the SPOT Imaging software (version 4.7, SPOT Imaging Solutions, Sterling Heights, MI). The ischemic zone was devoid of Evans blue dye. The percentage of the ischemic zone was calculated for each slice by dividing the ischemic zone by the total slice area. The ischemic zones for all slices were averaged to obtain the percentage of the heart that was ischemic. There were no differences in the ischemic zone between the CTB and CTB-SAP groups (64 ± 6 vs. 69 ± 5%).
To determine whether the coronary artery occlusion produced a myocardial infarction, the sections were incubated in a 1% TTC solution (2,3,5-triphenyltetrazolium chloride; Sigma) at 37°C for 20 min. The heart sections were placed between two glass slides and immersed in 10% formalin overnight to enhance the contrast of the stain. TTC staining differentiates viable tissue by reacting with myocardial dehydrogenase enzymes to form a red brick stain. Necrotic tissue, which has lost its dehydrogenase enzymes, does not form a red stain and shows up as pale yellow. This stain has been shown to be a reliable indicator of myocardial infarction (13). Based on the TTC staining, no animal sustained an infarct. It is important to note that the duration of the coronary artery occlusion used in this study was very short relative to the time required to induce permanent damage. Specifically, it is well documented that a period of transition from reversible to irreversible injury occurs at ∼20 min of normothermic global ischemia in the rat heart (31). In addition, the TTC method is well documented to be valid and reliable weeks after myocardial infarction (40).
ELISA analysis of norepinephrine.
The left ventricular free wall was pulverized into fine powder using a liquid nitrogen cooled mortar and pestle. Approximately 10 mg tissue were suspended in 200 μl of buffer (0.01 N HCl in the presence of 1 mM EDTA and 4 mM sodium metabisulfite) and incubated for 30 min at room temperature. Following the incubation, samples were homogenized with an ultrasonic dismembrator (Fisher Scientific) for 20 s (20 × 1 s) and immediately centrifuged at 10,000 rpm for 10 min. The supernatant protein concentration was determined with the Thermo Scientific Pierce BCA protein assay reagent kit (Pierce 23225). Norepinephrine was determined from a sample of 20 μg of protein in 10 μl using a commercially available ELISA kit (Noradrenaline ELISA, IBL-America, Minneapolis, MN).
Data analysis.
All recordings were sampled at 2 kHz, and the data were expressed as means ± SE. All data were the average of every beat during the last 10–15 s of the period. A one-factor ANOVA with post hoc Dunn's method was used to compare the VAT between the control, CTB, and CTB-SAP groups (Fig. 2). A repeated-measures two-factor ANOVA with post hoc Holm-Sidak method was used to compare mean arterial blood pressure and HR immediately before the occlusion (preocclusion), at 4 min of occlusion, and immediately before the onset of ventricular tachycardia (prearrhythmia). Four minutes was chosen as the standardized point to compare identical time points between conditions. This was necessary because the VAT was different between conditions. Importantly, no animal experienced sustained ventricular tachycardia before 4 min of occlusion in the three groups. In addition, a one-way ANOVA was used to compare ST segment elevation at 4 min of occlusion between the three groups, as well as neuronal number and soma area (see Fig. 4), sympathetic innervation density (see Fig. 7), and left ventricular norepinephrine content (see Fig. 8) between the control, CTB, and CTB-SAP groups. The ECGs were analyzed offline to measure the ST segment elevation (voltage difference between the baseline and J point) using the ECG analysis software for Chart [ADInstruments (54)].
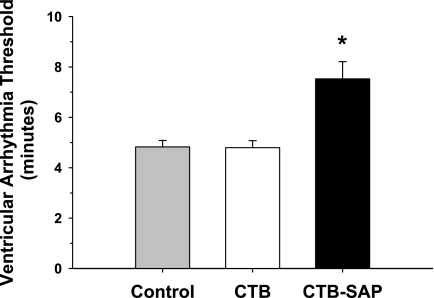
Fig. 2.
Ventricular arrhythmia threshold (VAT) in the control, CTB, and CTB-SAP groups. There was no difference in the VAT between the control and CTB group. However, the VAT was significantly longer in the CTB-SAP group. Values are means ± SE. *P < 0.05, CTB-SAP vs. control or CTB.
Fig. 4.
Neuronal number (A), soma area (B), and cresyl violet-stained neurons (C) of the stellate ganglia from three rats that had no injection (control), CTB, or CTB-SAP injected into both stellate ganglia. A: counts of stellate neurons in the CTB-SAP group showed a significant reduction in the number of neurons compared with the control or CTB groups. These results are consistent with C, showing many stellate neurons in the control and CTB groups and few neurons in the CTB-SAP group. B: however, mean soma area was not different between the three groups. The counts reported in this figure are similar to counts reported in two publications (6, 21). Values are means ± SE. *P < 0.05, CTB-SAP vs. control or CTB. Scale bar (C, bottom right) = 25 μm.
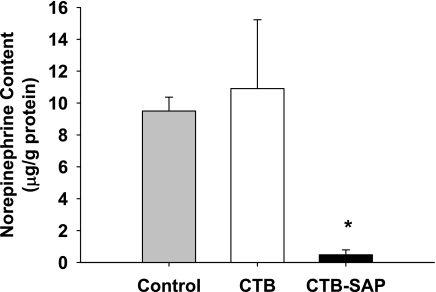
Fig. 8.
Left ventricular norepinephrine content from rats that had no injection (control), CTB, or CTB-SAP injected into both stellate ganglia. The CTB-SAP group showed a significant reduction in norepinephrine content compared with control and CTB groups. Values are means ± SE. *P < 0.05, CTB-SAP vs. control or CTB.
RESULTS
Mean arterial pressure and HR immediately before the occlusion (preocclusion), at 4 min of occlusion, and immediately before the onset of sustained ventricular tachycardia (prearrhythmia) in the three groups of rats (control, CTB, and CTB-SAP) are presented in Table 1. Resting (preocclusion) mean arterial pressure was not different between the control, CTB, and CTB-SAP groups. Similarly, resting HR was not different between the control and CTB groups. However, resting HR was significantly lower in the CTB-SAP group compared with the control and CTB groups (significant group effect).
Table 1.
Resting mean arterial pressure and heart rate immediately before the occlusion, at 4 min of occlusion, and immediately before the onset of sustained ventricular tachycardia in noninjected rats and rats that had CTB or CTB-SAP injected into both stellate ganglia
| Preocclusion | 4 Min | Prearrhythmia | |
|---|---|---|---|
| Mean arterial pressure, mmHg | |||
| Control | 107 ± 3 | 114 ± 5 | 113 ± 5 |
| CTB | 112 ± 3 | 118 ± 3 | 119 ± 4 |
| CTB-SAP | 118 ± 3 | 120 ± 4 | 117 ± 5 |
| Heart rate, beats/min | |||
| Control | 327 ± 6 | 394 ± 20† | 392 ± 19† |
| CTB | 332 ± 8 | 381 ± 17† | 384 ± 17† |
| CTB-SAP | 303 ± 12* | 346 ± 11*† | 353 ± 9*† |
Values are means ± SE. Preocclusion, before occlusion; 4 min, at 4 min of occlusion; prearrhythmia, immediately before the onset of sustained ventricular tachycardia; CTB, cholera toxin B; SAP, saporin.
P ≤ 0.05, CTB-SAP vs. control and CTB, group effect.
P ≤ 0.05, preocclusion vs. 4 min and prearrhythmia, condition effect.
Mean arterial pressure was not different between the control, CTB, and CTB-SAP groups at 4 min of occlusion or immediately before sustained ventricular tachycardia (prearrhythmia). Similarly, HR was not different between the control and CTB groups at 4 min of occlusion or immediately before sustained ventricular tachycardia (prearrhythmia). However, HR was significantly lower in the CTB-SAP group compared with the control and CTB groups at 4 min of occlusion, as well as immediately before sustained ventricular tachycardia (significant condition effect).
Figure 2 presents the VAT in the control, CTB, and CTB-SAP groups. The VAT was not different between the control and CTB groups. However, the VAT was significantly longer in the CTB-SAP group compared with the control and CTB groups. Importantly, in the CTB-SAP group, the VAT exceeded the 10-min occlusion limit in two animals; thus 10 min was used as the VAT. Both animals experienced sustained ventricular tachycardia upon reperfusion. No animals in the control or CTB groups exceeded the 10-min occlusion limit.
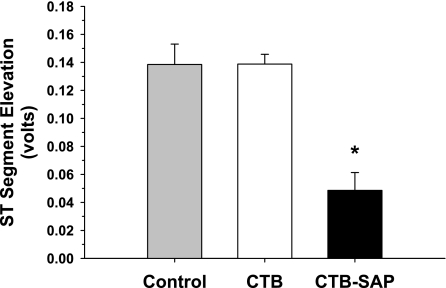
Figure 3 presents the ST-segment elevation at 4.0 min of occlusion for the control, CTB, and CTB-SAP groups. The ST-segment elevation was not different between the control and CTB groups. However, the ST segment elevation was significantly lower in the CTB-SAP group compared with the control and CTB groups.
Fig. 3.
ST-segment elevation at 4 min of occlusion in the control, CTB, and CTB-SAP groups. There were no differences in the ST-segment elevation between the control and CTB groups. However, the ST-segment elevation was significantly lower in the CTB-SAP group. Values are means ± SE. *P < 0.05, CTB-SAP vs. control or CTB.
Figure 4 presents neuronal number (A), soma area (B), and cresyl violet stained stellate neurons (C) from rats that had no injection (control), CTB, or CTB-SAP injected into both stellate ganglia. Counts of stellate neurons in the CTB-SAP group showed a significant reduction in the number of neurons compared with the control and CTB groups (1,566 ± 359 vs. 8,437 ± 834 and 8,081 ± 802, respectively). These results are consistent with Fig. 4C showing many stellate neurons in the control and CTB groups and few neurons in the CTB-SAP group. However, of the 6,648 neurons analyzed (control, n = 3,128; CTB, n = 2,945; and CTB-SAP, n = 575), the soma area (Fig. 4B) was not different between the three groups (control, 322 ± 9; CTB, 337 ± 25 vs. CTB-SAP, 293 ± 4 μm2).
Figure 5 presents CTB-immunoreactive neurons of the T1-T4 spinal cord from rats that had CTB or CTB-SAP injected into both stellate ganglia. A similar number of CTB-immunoreactive SPNs were found on both sides of the intermediolateral cell column of the T1-T4 spinal cord in CTB rats (Fig. 5A). However, virtually all of the CTB-immunoreactive SPNs were eliminated in the CTB-SAP group (Fig. 5B). Control slides (without primary antibody) did not have labeled cells.
Figure 6 presents cresyl violet-stained neurons of the dorsal root ganglia from rats that had CTB or CTB-SAP injected into both stellate ganglia. It is clear that CTB-SAP did not alter neurons within the dorsal root ganglia.
Fig. 6.
Cresyl violet-stained neurons of the dorsal root ganglia from rats that had CTB (A) or CTB-SAP (B) injected into both stellate ganglia. It is clear that CTB-SAP did not alter neurons within the dorsal root ganglia. Scale bar (bottom right) = 25 μm.
Figure 7 presents tyrosine hydroxylase-immunoreactive fiber density (A), number (B), and stained sympathetic fibers (C) from rats that had no injection (control), CTB, or CTB-SAP injected into both stellate ganglia. Counts of sympathetic fibers in the CTB-SAP group showed a significant reduction in the number and density compared with the control and CTB groups. These results are consistent with Fig. 7C showing many sympathetic fibers in the control and CTB groups and few sympathetic terminals in the CTB-SAP group. Consistent with the reduction of tyrosine hydroxylase-immunoreactive fibers in the CTB-SAP group was a reduction in norepinephrine content (Fig. 8).
DISCUSSION
In this study, we tested the hypothesis that targeted ablation of cardiac sympathetic neurons with bilateral stellate ganglia injection of SAP reduces the susceptibility to ischemia-induced sustained ventricular tachycardia in conscious rats. The major findings of this study include the following. 1) CTB-SAP rats had a reduced HR at rest and during coronary artery occlusion compared with control and CTB rats (Table 1), as well as a reduced ST-segment elevation at 4 min of coronary artery occlusion (Fig. 3). 2) Associated with the reduced resting and coronary artery occlusion-induced sympathetic activation was a reduction in the number of stellate postganglionic neurons and cardiac SPNs (Figs. 4 and 5), as well as left ventricular sympathetic innervation density (Fig. 7) and norepinephrine content (Fig. 8). 3) Together, these changes were associated with a reduced susceptibility to ischemia-induced sustained ventricular tachycardia (Fig. 2). These results are consistent with and extend our recent report that CTB-SAP retrogradely transported from the stellate ganglia is effective at ablating cardiac sympathetic neurons and reducing resting, exercise, and reflex sympathetic activity (21).
It is well documented that the majority of cardiac sympathetic axons and nerve terminals originate in the cell bodies of the bilateral stellate ganglia. Specifically, bilateral stellate ganglionectomy in the rat reduces cardiac norepinephrine content by 89–100% (32, 61), suggesting that >90% of cardiac sympathetic innervation arises from the stellates. However, to document cardiac specificity and that cardiac sympathetics are ablated with this procedure, we determined left ventricular norepinephrine content (ELISA), as well as cardiac sympathetic innervation density (tyrosine hydroxylase positive terminals). The results from these protocols document reductions in both left ventricular sympathetic terminals (Fig. 7) and norepinephrine content (Fig. 8). Furthermore, this procedure reduced the maximal HR response to exercise and sodium nitroprusside by 30% (21). This is important because the gold standard for the extent of sympathetic blockade is the reduction in exercise HR (11, 57). Thus this procedure is cardiac specific, mainly (>90%) targeting cardiac axons and nerve terminals.
In this study as well as our laboratory's recent report (21), we performed bilateral stellate ganglia injections. It is well documented that the sympathetic control of HR is primarily exerted by the RSG (36, 47). Accordingly, resting and coronary artery occlusion-induced HRs were lower in CTB-SAP rats. It is also well documented that the LSG is primarily responsible for ventricular arrhythmic events (47, 49, 50). However, both ganglia contribute to the deadly arrhythmias. Specifically, the cardiac and sympathetic responses to ischemia are mediated, in part, by the cardio-cardiac sympathetic reflex, with the efferent limb mainly through the RSG and the afferent limb mainly through left afferent fibers (23–25). Specifically, cardiac sympathetic afferents are excited by ischemia and elicit a cardio-cardiac sympathetic reflex (3, 24), which plays a major role in the genesis of ventricular arrhythmias (44). The cardio-cardiac sympathetic reflex, in addition to mediating cardiac sympathoexcitation, inhibits cardiac vagal efferent activity (low vagal activity is associated with ventricular arrhythmic events) (22, 30). Left sympathectomy reduces the influence of the cardio-cardiac sympathetic reflex and protects the heart during ischemia. However, very high HRs may overcome the protective effects of removal of the LSG (49). For these reasons, we studied the effect of bilateral ablation of cardiac sympathetic neurons (21).
Cardiovascular diseases (e.g., hypertension, stroke, heart failure, coronary heart disease) are the leading causes of death for both men and women in the United States. Excessive sympathetic activity is responsible for, and/or contributes to, the morbidity and mortality associated with these life-threatening disorders. Similarly, the mechanisms mediating several forms of life-threatening ventricular arrhythmias involve excess sympathetic activity. Sympathetic activity increases myocardial oxygen consumption and cardiac conduction and reduces refractory period. Sympathetic activity also increases intracellular calcium concentration. Increased intracellular calcium concentration may generate depolarizing membrane currents, which lead to delayed afterdepolarizations and ventricular arrhythmias (16, 59). Accordingly, efforts to reduce sympathetic activity are the first-line therapy for most, if not all, cardiovascular diseases. For example, β-adrenergic-receptor antagonists are the first-line therapy for symptomatic ventricular tachycardia (17, 33). However, despite their favorable effects, adverse complications limit compliance to these medications. For example the Medical Research Council trial (26) on hypertensive patients documented that, for every myocardial infarction or stroke prevented by β-adrenergic-receptor antagonists, three patients withdrew from the study secondary to impotence, and another seven withdrew because of fatigue (27). Furthermore, compliance for these agents is low due to the expense, forgetfulness, and the asymptomatic nature of the conditions.
Thoracic sympathectomy (stellate ganglion together with second and third thoracic ganglia ablation) partially overcomes these limitations and is an established, minimally invasive procedure for sympathetic blockade in patients with hyperhidrosis, facial flushing, intractable angina, and ventricular tachyarrhythmias. For example, reductions in cardiac sympathetic activity via left stellate ganglionectomy increase the threshold for VF (46) and increase ventricular refractoriness (51). In addition, left stellate ganglionectomy reduces arrhythmic events in high-risk patients with myocardial infarction (52), young adults with catecholaminergic polymorphic ventricular tachycardia (60), and individuals with long-QT syndrome who were not protected by full-dose β-adrenergic-receptor antagonist therapy (45). However, thoracic sympathectomy may produce Horner's syndrome, paraesthesia, compensatory hyperhidrosis, and residual flushing, as well as death in the individuals undergoing the procedure for intractable angina (37). Thus these complications severely limit patient satisfaction with the procedure.
Targeted, bilateral stellate ganglia injection of SAP provides an additional option for individuals susceptible to ventricular arrhythmias, because this procedure reduces resting, reflex, and exercise-induced (21), as well as coronary artery occlusion-induced, sympathetic activity. As recently noted (21), bilateral stellate ganglia injection of SAP may selectively reduce the major source of norepinephrine release to the heart, since stellate ganglionectomy markedly reduces myocardial norepinephrine content (61). Importantly, bilateral stellate ganglia injection of SAP is a preganglionic denervation, which suggests that there would be no reinnervation (60). Furthermore, bilateral stellate ganglia injection of SAP does not completely eliminate catecholamines to the heart, which suggests that postdenervation supersensitivity would be reduced (48). This procedure may also avoid limitations of medical therapy, such as the potential for anhydrosis, Horner's syndrome, and compensatory hyperhidrosis.
As recently noted (21), thoracic sympathectomy is markedly different from targeted ablation of cardiac sympathetic pre- and postganglionic fibers. Stellectomy ablates fibers passing through the ganglia, disrupting afferent signals, as well as efferent fibers ascending and descending within the sympathetic chain. For example, fibers traveling to the superior cervical ganglia may be disrupted, resulting in Horner' syndrome, and afferent fibers are disrupted, resulting in paraesthesia and the absence of cardiac pain. In this context, rats with bilateral stellate ganglia injections of SAP did not have Horner's syndrome, and neurons within the dorsal root ganglia were not affected (Fig. 6), suggesting that afferent pathways remained functional.
Finally, as recently noted (21), stellectomy largely prevents norepinephrine release in the heart (32, 42, 46, 61); thus there is no way to grade the level of sympathetic denervation. In sharp contrast, with stellate injections of SAP, it may be possible to adjust the dosage to partially denervate the heart to desirable levels.
Clinical Perspective
Sudden cardiac death (SCD) is an enormous problem and is most commonly caused by ventricular tachyarrhythmias that culminate in VF. It is thought that effective prevention of VF will require long-term prophylaxis by drugs (8). However, the pharmacological approach to antiarrhythmic therapy has serious problems. Most antiarrhythmic drugs are less effective and far more dangerous than once believed. For example, the Cardiac Arrhythmia Suppression Trial demonstrated that antiarrhythmic drugs not only fail to prevent SCD, but actually increase overall mortality (4, 5). These findings have been confirmed in additional trials (5, 12, 35, 58). The “proarrhythmic” effects of most currently available antiarrhythmic drugs, combined with the enormity of the problem, makes it essential that we investigate novel strategies for the prevention of SCD. Targeted ablation of cardiac sympathetic neurons may become a therapeutic option. Specifically, results of a recent study in rats showed that CTB-SAP retrogradely transported from the stellate ganglia is effective at ablating neurons innervating the heart and reducing resting, exercise, and reflex sympathetic activity (21). In addition, the present study documented that this procedure is effective in increasing the VAT. However, additional studies are required to further characterize the physiological responses to this procedure and determine whether this new approach is safe and efficacious for the treatment of conditions associated with excess sympathetic activity. In this context, it is important to compare the effects of cardiac sympathetic neuronal ablation with the effects of β-blockade, since the ablation procedure should at least mimic the beneficial actions of β-adrenergic receptor blockade on arrhythmogenesis. In addition, the comparison would clarify whether all responses to neuronal ablation are due to preventing sympathetic input to the heart, and whether circulating catecholamines might participate in arrhythmogenesis.
Conclusion
The results of this study show that CTB-SAP retrogradely transported from the stellate ganglia is effective at ablating cardiac sympathetic neurons and reducing the susceptibility to ventricular arrhythmias. Additional studies are required to further characterize the physiological responses to this procedure, as well as determine whether this new approach is safe and efficacious for the treatment of conditions associated with excess sympathetic activity.
GRANTS
This study was supported by National Heart, Lung, and Blood Institute Grant HL-88615.
DISCLOSURES
No conflicts of interest are declared by the author(s).
REFERENCES
- 1.Bolognesi A, Tazzari PL, Olivieri F, Polito L, Falini B, Stirpe F. Induction of apoptosis by ribosome-inactivating proteins and related immunotoxins. Int J Cancer 68: 349–355, 1996 [DOI] [PubMed] [Google Scholar]
- 2.Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med 341: 1882–1890, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Casati R, Lombardi F, Malliani A. Afferent sympathetic unmyelinated fibres with left ventricular endings in cats. J Physiol 292: 135–148, 1979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CAST II Investigators Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. The Cardiac Arrhythmia Suppression Trial II Investigators. N Engl J Med 327: 227–233, 1992 [DOI] [PubMed] [Google Scholar]
- 5.CAST Investigators Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. The Cardiac Arrhythmia Suppression Trial (CAST) Investigators. N Engl J Med 321: 406–412, 1989 [DOI] [PubMed] [Google Scholar]
- 6.Cavalcanti RA, da Pureza DY, de Melo MP, de Souza RR, Bergamaschi CT, do Amaral SL, Tang H, Loesch A, Ribeiro AA. Low-intensity treadmill exercise-related changes in the rat stellate ganglion neurons. J Neurosci Res 87: 1334–1342, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Chugh SS, Reinier K, Teodorescu C, Evanado A, Kehr E, Al Samara M, Mariani R, Gunson K, Jui J. Epidemiology of sudden cardiac death: clinical and research implications. Prog Cardiovasc Dis 51: 213–228, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clements-Jewery H, Andrag E, Curtis MJ. Druggable targets for sudden cardiac death prevention: lessons from the past and strategies for the future. Curr Opin Pharmacol 9: 146–153, 2009 [DOI] [PubMed] [Google Scholar]
- 9.Collins HL, DiCarlo SE. TENS attenuates response to colon distension in paraplegic and quadriplegic rats. Am J Physiol Heart Circ Physiol 283: H1734–H1739, 2002 [DOI] [PubMed] [Google Scholar]
- 10.Collura CA, Johnson JN, Moir C, Ackerman MJ. Left cardiac sympathetic denervation for the treatment of long QT syndrome and catecholaminergic polymorphic ventricular tachycardia using video-assisted thoracic surgery. Heart Rhythm 6: 752–759, 2009 [DOI] [PubMed] [Google Scholar]
- 11.De Mey C, Breithaupt-Grogler K, Schloos J, Palm D, Belz GG. Reproducibility and consistency of the responses to supine bicycle ergometry; evaluation in conjunction with beta 1-adrenoceptor occupancies. Br J Clin Pharmacol 38: 480–483, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, Barker AH, Arensberg D, Baker A, Friedman L, Greene HL, et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The Cardiac Arrhythmia Suppression Trial. N Engl J Med 324: 781–788, 1991 [DOI] [PubMed] [Google Scholar]
- 13.Fishbein MC, Meerbaum S, Rit J, Lando U, Kanmatsuse K, Mercier JC, Corday E, Ganz W. Early phase acute myocardial infarct size quantification: validation of the triphenyl tetrazolium chloride tissue enzyme staining technique. Am Heart J 101: 595–600, 1981 [DOI] [PubMed] [Google Scholar]
- 14.Hjalmarson A, Elmfeldt D, Herlitz J, Holmberg S, Malek I, Nyberg G, Ryden L, Swedberg K, Vedin A, Waagstein F, Waldenstrom A, Waldenstrom J, Wedel H, Wilhelmsen L, Wilhelmsson C. Effect on mortality of metoprolol in acute myocardial infarction. A double-blind randomised trial. Lancet 2: 823–827, 1981 [DOI] [PubMed] [Google Scholar]
- 15.Jones R. Split nucleoli as a source of error in nerve cell counts. Stain Technology 19: 91–95, 1937 [Google Scholar]
- 16.Kontula K, Laitinen PJ, Lehtonen A, Toivonen L, Viitasalo M, Swan H. Catecholaminergic polymorphic ventricular tachycardia: recent mechanistic insights. Cardiovasc Res 67: 379–387, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Leenhardt A, Lucet V, Denjoy I, Grau F, Ngoc DD, Coumel P. Catecholaminergic polymorphic ventricular tachycardia in children. A 7-year follow-up of 21 patients. Circulation 91: 1512–1519, 1995 [DOI] [PubMed] [Google Scholar]
- 18.Llewellyn-Smith IJ, DiCarlo SE, Collins HL, Keast JR. Enkephalin-immunoreactive interneurons extensively innervate sympathetic preganglionic neurons regulating the pelvic viscera. J Comp Neurol 488: 278–289, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Llewellyn-Smith IJ, Martin CL, Arnolda LF, Minson JB. Retrogradely transported CTB-saporin kills sympathetic preganglionic neurons. Neuroreport 10: 307–312, 1999 [DOI] [PubMed] [Google Scholar]
- 20.Lujan HL, Chen Y, DiCarlo SE. Paraplegia increased cardiac NGF content, sympathetic tonus and the susceptibility to ischemia-induced ventricular tachycardia in conscious rats. Am J Physiol Heart Circ Physiol 296: H1364–H1372, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lujan HL, Palani G, Chen Y, Peduzzi-Nelson J, DiCarlo SE. Targeted ablation of cardiac sympathetic neurons reduces resting, reflex and exercise-induced sympathetic activation in conscious rats. Am J Physiol Heart Circ Physiol 296: H1305–H1311, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malliani A, Pagani M, Recordati G, Schwartz PJ. Spinal sympathetic reflexes elicited by increases in arterial blood pressure. Am J Physiol 220: 128–134, 1971 [DOI] [PubMed] [Google Scholar]
- 23.Malliani A, Parks M, Tuckett RP, Brown AM. Reflex increases in heart rate elicited by stimulation of afferent cardiac sympathetic nerve fibers in the cat. Circ Res 32: 9–14, 1973 [PubMed] [Google Scholar]
- 24.Malliani A, Recordati G, Schwartz PJ. Nervous activity of afferent cardiac sympathetic fibres with atrial and ventricular endings. J Physiol 229: 457–469, 1973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malliani A, Schwartz PJ, Zanchetti A. A sympathetic reflex elicited by experimental coronary occlusion. Am J Physiol 217: 703–709, 1969 [DOI] [PubMed] [Google Scholar]
- 26.Medical Research Council Medical Research Council trial of treatment of hypertension in older adults: principal results. MRC Working Party. BMJ 304: 405–412, 1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Messerli FH, Grossman E. Beta-blocker therapy and depression. JAMA 288: 1845–1846, 2002 [PubMed] [Google Scholar]
- 28.Nayate A, Moore SA, Weiss RM, Taktakishvili O, Lin LH, Talman WT. Cardiac damage after lesions of the nucleus tractus solitarii. Am J Physiol Regul Integr Comp Physiol 296: R272–R279, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norris RM, Barnaby PF, Brown MA, Geary GG, Clarke ED, Logan RL, Sharpe DN. Prevention of ventricular fibrillation during acute myocardial infarction by intravenous propranolol. Lancet 2: 883–886, 1984 [DOI] [PubMed] [Google Scholar]
- 30.Pagani M, Schwartz PJ, Banks R, Lombardi F, Malliani A. Reflex responses of sympathetic preganglionic neurones initiated by different cardiovascular receptors in spinal animals. Brain Res 68: 215–225, 1974 [DOI] [PubMed] [Google Scholar]
- 31.Palmer BS, Hadziahmetovic M, Veci T, Angelos MG. Global ischemic duration and reperfusion function in the isolated perfused rat heart. Resuscitation 62: 97–106, 2004 [DOI] [PubMed] [Google Scholar]
- 32.Pardini BJ, Lund DD, Schmid PG. Organization of the sympathetic postganglionic innervation of the rat heart. J Auton Nerv Syst 28: 193–201, 1989 [DOI] [PubMed] [Google Scholar]
- 33.Postma AV, Denjoy I, Kamblock J, Alders M, Lupoglazoff JM, Vaksmann G, Dubosq-Bidot L, Sebillon P, Mannens MM, Guicheney P, Wilde AA. Catecholaminergic polymorphic ventricular tachycardia: RYR2 mutations, bradycardia, and follow up of the patients. J Med Genet 42: 863–870, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Potts JT, Fong AY, Anguelov PI, Lee S, McGovern D, Grias I. Targeted deletion of neurokinin-1 receptor expressing nucleus tractus solitarii neurons precludes somatosensory depression of arterial baroreceptor-heart rate reflex. Neuroscience 145: 1168–1181, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pratt CM, Moye LA. The Cardiac Arrhythmia Suppression Trial: background, interim results and implications. Am J Cardiol 65: 20B–29B, 1990 [DOI] [PubMed] [Google Scholar]
- 36.Randall WC, Rohse WG. The augmentor action of the sympathetic cardiac nerves. Circ Res 4: 470–475, 1956 [DOI] [PubMed] [Google Scholar]
- 37.Rathinam S, Nanjaiah P, Sivalingam S, Rajesh PB. Excision of sympathetic ganglia and the rami communicantes with histological confirmation offers better early and late outcomes in video assisted thoracoscopic sympathectomy. J Card Surg 3: 50, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rodenbaugh DW, Collins HL, Nowacek DG, DiCarlo SE. Increased susceptibility to ventricular arrhythmias is associated with changes in Ca2+ regulatory proteins in paraplegic rats. Am J Physiol Heart Circ Physiol 285: H2605–H2613, 2003 [DOI] [PubMed] [Google Scholar]
- 39.Salathia KS, Barber JM, McIlmoyle EL, Nicholas J, Evans AE, Elwood JH, Cran G, Shanks RG, Boyle DM. Very early intervention with metoprolol in suspected acute myocardial infarction. Eur Heart J 6: 190–198, 1985 [DOI] [PubMed] [Google Scholar]
- 40.Santos L, Mello AF, Antonio EL, Tucci PJ. Determination of myocardial infarction size in rats by echocardiography and tetrazolium staining: correlation, agreements, and simplifications. Braz J Med Biol Res 41: 199–201, 2008 [DOI] [PubMed] [Google Scholar]
- 41.Schwartz PJ. Cutting nerves and saving lives. Heart Rhythm 6: 760–763, 2009 [DOI] [PubMed] [Google Scholar]
- 42.Schwartz PJ. The rationale and the role of left stellectomy for the prevention of malignant arrhythmias. Ann N Y Acad Sci 427: 199–221, 1984 [DOI] [PubMed] [Google Scholar]
- 43.Schwartz PJ, Billman GE, Stone HL. Autonomic mechanisms in ventricular fibrillation induced by myocardial ischemia during exercise in dogs with healed myocardial infarction. An experimental preparation for sudden cardiac death. Circulation 69: 790–800, 1984 [DOI] [PubMed] [Google Scholar]
- 44.Schwartz PJ, Foreman RD, Stone HL, Brown AM. Effect of dorsal root section on the arrhythmias associated with coronary occlusion. Am J Physiol 231: 923–928, 1976 [DOI] [PubMed] [Google Scholar]
- 45.Schwartz PJ, Priori SG, Cerrone M, Spazzolini C, Odero A, Napolitano C, Bloise R, De Ferrari GM, Klersy C, Moss AJ, Zareba W, Robinson JL, Hall WJ, Brink PA, Toivonen L, Epstein AE, Li C, Hu D. Left cardiac sympathetic denervation in the management of high-risk patients affected by the long-QT syndrome. Circulation 109: 1826–1833, 2004 [DOI] [PubMed] [Google Scholar]
- 46.Schwartz PJ, Snebold NG, Brown AM. Effects of unilateral cardiac sympathetic denervation on the ventricular fibrillation threshold. Am J Cardiol 37: 1034–1040, 1976 [DOI] [PubMed] [Google Scholar]
- 47.Schwartz PJ, Stone HL. Effects of unilateral stellectomy upon cardiac performance during exercise in dogs. Circ Res 44: 637–645, 1979 [DOI] [PubMed] [Google Scholar]
- 48.Schwartz PJ, Stone HL. Left stellectomy and denervation supersensitivity in conscious dogs. Am J Cardiol 49: 1185–1190, 1982 [DOI] [PubMed] [Google Scholar]
- 49.Schwartz PJ, Stone HL. Left stellectomy in the prevention of ventricular fibrillation caused by acute myocardial ischemia in conscious dogs with anterior myocardial infarction. Circulation 62: 1256–1265, 1980 [DOI] [PubMed] [Google Scholar]
- 50.Schwartz PJ, Stone HL, Brown AM. Effects of unilateral stellate ganglion blockade on the arrhythmias associated with coronary occlusion. Am Heart J 92: 589–599, 1976 [DOI] [PubMed] [Google Scholar]
- 51.Schwartz PJ, Verrier RL, Lown B. Effect of stellectomy and vagotomy on ventricular refractoriness in dogs. Circ Res 40: 536–540, 1977 [DOI] [PubMed] [Google Scholar]
- 52.Schwartz P, Motolese M, Pollavini G, Lotto A, Ruberti U, Trazzi R, Bartorelli C, Zanchetti A. Prevention of sudden cardiac death after a first myocardial infarction by pharmacologic or surgical antiadrenergic interventions. J Cardiovasc Electrophysiol 3: 2–16, 1992 [Google Scholar]
- 53.Shivkumar K, Schultz L, Goldstein S, Gheorghiade M. Effects of propanolol in patients entered in the Beta-Blocker Heart Attack Trial with their first myocardial infarction and persistent electrocardiographic ST-segment depression. Am Heart J 135: 261–267, 1998 [DOI] [PubMed] [Google Scholar]
- 54.Smith SW. ST segment elevation differs depending on the method of measurement. Acad Emerg Med 13: 406–412, 2006 [DOI] [PubMed] [Google Scholar]
- 55.Strack AM, Sawyer WB, Marubio LM, Loewy AD. Spinal origin of sympathetic preganglionic neurons in the rat. Brain Res 455: 187–191, 1988 [DOI] [PubMed] [Google Scholar]
- 56.The MIAMI Trial Research Group Metoprolol in acute myocardial infarction (MIAMI): a randomized placebo controlled international trial. Eur Heart J 6: 199–226, 1985 [PubMed] [Google Scholar]
- 57.Vittorio TJ, Zolty R, Kasper ME, Khandwalla RM, Hirsh DS, Tseng CH, Jorde UP, Ahuja K. Differential effects of carvedilol and metoprolol succinate on plasma norepinephrine release and peak exercise heart rate in subjects with chronic heart failure. J Cardiovasc Pharmacol Ther 13: 51–57, 2008 [DOI] [PubMed] [Google Scholar]
- 58.Waldo AL, Camm AJ, deRuyter H, Friedman PL, MacNeil DJ, Pauls JF, Pitt B, Pratt CM, Schwartz PJ, Veltri EP. Effect of d-sotalol on mortality in patients with left ventricular dysfunction after recent and remote myocardial infarction. The SWORD Investigators Survival With Oral d-Sotalol. Lancet 348: 7–12, 1996 [DOI] [PubMed] [Google Scholar]
- 59.Wehrens XH, Lehnart SE, Reiken S, Vest JA, Wronska A, Marks AR. Ryanodine receptor/calcium release channel PKA phosphorylation: a critical mediator of heart failure progression. Proc Natl Acad Sci U S A 103: 511–518, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wilde AA, Bhuiyan ZA, Crotti L, Facchini M, De Ferrari GM, Paul T, Ferrandi C, Koolbergen DR, Odero A, Schwartz PJ. Left cardiac sympathetic denervation for catecholaminergic polymorphic ventricular tachycardia. N Engl J Med 358: 2024–2029, 2008 [DOI] [PubMed] [Google Scholar]
- 61.Yoshimoto M, Wehrwein EA, Novotny M, Swain GM, Kreulen DL, Osborn JW. Effect of stellate ganglionectomy on basal cardiovascular function and responses to β1-adrenoceptor blockade in the rat. Am J Physiol Heart Circ Physiol 295: H2447–H2454, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhou S, Jung BC, Tan AY, Trang VQ, Gholmieh G, Han SW, Lin SF, Fishbein MC, Chen PS, Chen LS. Spontaneous stellate ganglion nerve activity and ventricular arrhythmia in a canine model of sudden death. Heart Rhythm 5: 131–139, 2008. [DOI] [PubMed] [Google Scholar]