Abstract
Injury mechanisms from frontal airbags, first identified in anecdotal reports, are now well documented for pediatric, small female, and out-of-position occupants. In contrast, torso side airbags have not yet been consistently associated with specific injury risks in field assessments. To determine possible torso side airbag-related injuries, the present study identified crashes involving side airbags from reports within the CIREN, NASS, and SCI databases. Injury patterns were compared to patterns from lateral crashes in absence of side airbag. Splenic trauma (AIS 3+) was found present in five cases of torso side airbag deployment at lower impact severity (as measured by velocity change and compartment intrusion) than cases of splenic trauma without side airbag. Five additional cases were found to contain similar injury patterns but occurred with greater crash severity. To supplement case analyses, full scale sled tests were conducted with a THOR-NT dummy and cadaveric specimen. Four THOR tests with door- and seat-mounted torso side airbags confirmed that out-of-position (early inflation stage) airbag contact elevated thoracic injury metrics compared to optimal (fully inflated) contact. Out-of-position seat-mounted airbag deployment also produced AIS 3 splenic trauma in the cadaveric specimen. Due to potentially sudden or delayed onset of intraperitoneal hemorrhage and hypovolemic shock following splenic trauma, further biomechanical investigation of this anecdotal evidence is essential to identify injury mechanisms, prevention techniques, and methods for early diagnosis.
INTRODUCTION
Injuries from frontal airbag systems have been well-documented in the literature since the implementation of these devices. Although deemed safe by early testing [Melvin et al., 1993], a collection of anecdotal reports accumulated throughout the 1990’s documenting traumatic injury risk to pediatric, small female, and out-of-position (OOP) occupants [e.g. Kleinberger & Summers, 1997]. These reported both risk of traumatic brain injury in restrained infants and risk of cervical spine injury in unrestrained children and small females. In response to such anecdotal reports, the National Highway Traffic Safety Administration (NHTSA) revised U.S. regulations to allow for “depowered” frontal airbags, shown to be safer to these at-risk occupants [NHTSA, 1997]. Retrospective analyses have confirmed improvements offered by these depowered airbags [Arbogast et al., 2005; Olson et al., 2006; Braver et al., 2008]. As a result of this action and public education efforts, over 75% of the 291 frontal airbag deaths confirmed by NHTSA occurred prior to 2001; none have been confirmed since 2006 [NHTSA, 2008]. From these experiences, scientists, design engineers, and regulators developed protocols by which the performance of new airbag technologies has been assessed throughout the current decade.
Side airbags (SABs) were implemented in the wake of these biomechanical test protocols. Their injury risk to vulnerable OOP occupants is currently evaluated by industry-accepted recommended procedures [IIHS, 2003]; manufacturer compliance is voluntary. This collection of protocols, which evolved from frontal airbag testing methods, duplicates studies of injury risk to pediatric [Pintar et al., 1999; Tylko & Dalmotas, 2000; Prasad et al., 2001] and small female [Khadilker & Pauls, 1998; Duma et al., 2003; Duma, Boggess et al., 2003] occupants subjected to SAB deployment in stationary test conditions. Yet due to the small number of documented SAB deployments, scientists and medical professionals have not identified any conditions in which SABs may produce predictable injury patterns in real-world crashes [Yoganandan et al., 2007]. Consequently, injury modalities evaluated in test procedures remain assumed.
The rapid incorporation of SABs into the U.S. automobile fleet has led to their availability in as many as 89% of 2009 model year vehicles [Highway Loss Data Institute, 2008]. This rate of implementation has led to a rapidly expanding collection of documented crashes involving SAB deployment [Yoganandan et al., 2007]. Because current test protocols may not reveal the propensity of SABs to induce injury in real-world scenarios, the present study revisited crash databases for documented SAB deployments. Thoracoabdominal injury patterns from lateral impacts with and without torso-interacting SAB were comparatively evaluated to identify potential adverse effects. Collectively, cases suggested splenic trauma can result from SAB; a plausible injury mechanism was reproduced in a sled environment with occupant surrogates.
METHODS
The present study analyzed crash injury databases for low severity impacts involving torso SAB deployment. Individual cases were examined for recurrent patterns of thoracoabdominal injury uncommon to impact severity as measured by velocity change (ΔV) and occupant compartment lateral intrusion. Supplement to the case examination, five laboratory full-scale sled tests were conducted. Injury modalities suggested by the databases were replicated using seat- and door-mounted torso SABs in conjunction with two occupant surrogates: a THOR-NT anthropomorphic test device (THOR) and an unembalmed post-mortem human subject (PMHS).
Crash Databases
Individual motor vehicle crash reports were examined in the Crash Injury Research and Engineering Network (CIREN), Special Crash Investigations (SCI), and National Automotive Sampling System (NASS) databases. These databases, administered by the U.S. Department of Transportation, are sanitized of personally identifiable data. The CIREN database, formed in 1996, is a collaboration of clinicians and engineers at up to twelve Level 1 Trauma Centers in the U.S. Enrolled cases generally involve AIS 3+ (or multiple AIS 2) injuries occurring in late model vehicle crashes. The SCI program began in 1972 and collects data nationally from crashes involving special circumstances or emerging safety technologies. The NASS database is composed of cases selected from a sample of police crash reports. Sampling design ensures cases are a representative and random sample of the hundreds of thousands of minor, serious and fatal crashes occurring annually in the U.S. The NASS now samples approximately 5,000 cases annually within regions selected from over 1,000 population-based sampling units. In this study, individual (unweighted) NASS cases involving SABs were considered.
Databases were queried for all cases with ΔV ≤ 27 km/h and documented SAB deployment. Low ΔV ensured that SAB deployment energy was a proportionally greater component of the total energy encompassing the crash event. Reported ΔV and WinSmash inputs were evaluated with vehicle photographs to eliminate erroneous cases. Vehicle photos were also examined to determine SAB type and deployment status; vehicles were included if equipped with SAB offering protection to the torso (torso SAB) or protection to the combined head and torso (combination SAB). These varieties were available in seat- or door-mounted arrangement. Vehicles containing curtains and head protection devices were included only if also equipped with torso SAB; head injury was not evaluated. Case occupants consisted of drivers injured in nearside impacts. From case reports vehicle damage, crash reconstruction, injury documentation, and injury analysis were evaluated individually.
To evaluate severity of trauma in SAB impacts, injury patterns were compared to left side impacts without SABs. The CIREN database was queried for side impacts with ΔV ≤ 27 km/h, PDOF = 8 – 11 o’clock, and without airbag deployment. Frequency of injury types and aggregate thoracic and abdominal AIS values were compared to cases with SAB to assess reasonable likelihood of injury patterns with SAB deployment. Additionally, the NASS database (1997–2006) was queried for splenic trauma in left side impact without SAB (PDOF = 8 – 11 o’clock).
Experiments
The injurious SAB deployments suggested by case reports were triggered by lateral ΔV. Therefore, previously established static SAB test protocols were insufficient to evaluate occupant-SAB interaction. For this study, dynamic sled tests were performed to reproduce injury mechanisms found in real crashes. The experimental protocols were similar for both occupant surrogates employed in this study, THOR and PMHS. The results from the database investigations were used to design the conditions of the sled tests to induce maximum SAB loading. The Heidelberg-type sled setup simulated left side impact loading, and the geometric details have been presented elsewhere [Pintar et al., 1997].
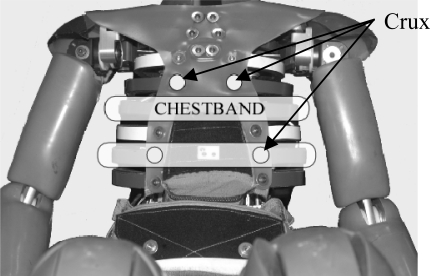
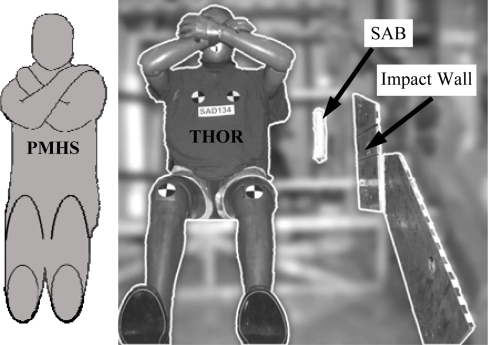
The THOR was instrumented with two 59 channel chestbands at the middle and lower thoracic levels. These corresponded to the levels just below the upper and over the lower oblique thoracic deflection cruxes (Fig. 1). The PMHS was instrumented with three chestbands at the fourth, eighth, and tenth rib levels laterally [Pintar et al., 1996]. Chestbands were wrapped with metallic shielding and sealed with conductive adhesive tape to prevent signal interference from electrostatic discharge during SAB deployment. This shielding was overlaid with a cotton garment to maintain realistic interaction between the occupant surrogate and the deploying SAB. Surrogates were seated upright on the sled with the Frankfort plane horizontal, legs stretched parallel to the midsagittal plane, and normal spinal curvature and alignment. To maximize thoracic exposure to SAB deployment characteristics, both arms were oriented forward and away from the lateral thorax (Fig. 2). This maintained an unprotected thorax throughout the progression of impact. All data were gathered and processed according to the SAE J211 specifications. Following PMHS testing, an autopsy was performed by a board-certified pathologist.
Figure 1.
Chestband location on THOR dummy thorax in relation to deflection cruxes, viewed from anterior.
Figure 2.
Occupant surrogate positioning in sled buck. Impact wall and seat-mounted SAB are indicated. Door-mounted SAB was positioned at thorax level within impact wall.
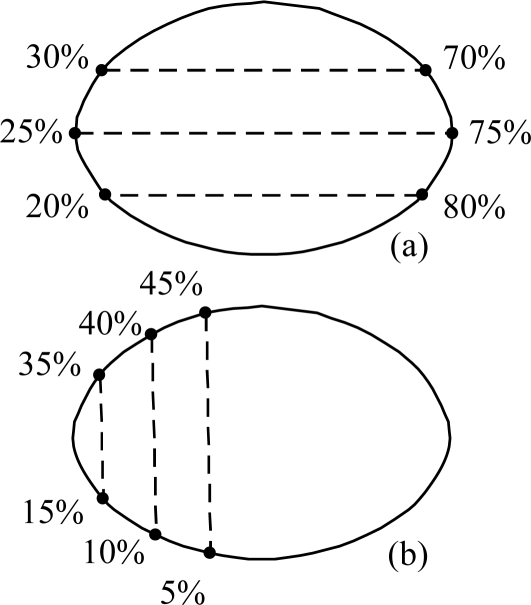
Contours at the upper, middle, and lower thoracic levels for the PMHS test and at the middle and lower thoracic level for dummy tests were obtained from chestband signals. Deflection profiles and biomechanical injury metrics of chest compression (C) [Kuppa et al., 2003] and viscous metric (VC) [Viano & Lau, 1988] were compared for the dummy and PMHS tests as follows. Contours were calculated at 12.5 kHz from chestband curvature signals using RBandPC software (v. 3.0, Conrad Technologies Inc., Washington, D.C.) and pretest measurements of the specimen [Pintar et al., 1996]. Proceeding clockwise, contours were sectioned according to normalized circumference distance. Contour origin (0%) was designated by the spinous process of the adjacent vertebral body. On each contour, full lateral chest C and VC were computed between 20% and 80%, 25% and 75%, and 30% and 70% circumference distances (Fig. 3a). Maximum value attained from these three computations was considered peak lateral metric [Kuppa et al., 2003]. To characterize posterolateral chest deflection resulting from seat-mounted SAB deployment, deflection and velocity time traces were computed between 5% and 45%, 10% and 40%, and 15% and 35% (Fig. 3b). PMHS data were normalized to 50th percentile male total body mass based on equal stress-equal velocity approach [Eppinger et al., 1984]. Peak deformation metrics from THOR tests were compared with the corresponding PMHS results.
Figure 3.
Chestband contour analysis methods for (a) lateral and (b) posterolateral deformations.
RESULTS
Case histories selected for review totaled 338. Cases involving side impact with deployed torso-interacting SAB totaled 272 and were distributed as follows: 161 from the SCI, 45 from the CIREN, and 66 from the NASS databases. In addition, 66 CIREN cases involving side impact without SAB were selected to provide the thoracoabdominal injury baseline. Injuries demonstrated in radiology were compared with cases involving SAB deployment. Cases without SAB were limited to ΔV ≤ 27 km/h.
Occupants involved in left-side impacts without SAB sustained injuries distributed as follows: trauma to head/neck (n = 18, rate = 35%), thorax (36, 69%), abdomen (8, 15%) and extremities (8, 15%). Of thorax cases, 32 (62%) included rib fracture and 16 (31%) included lung trauma. Eight (15%) case occupants sustained splenic trauma AIS 2+. All splenic trauma was associated with at least 1 rib fracture. Average door intrusion for all left side cases was 17 cm. Door intrusion in splenic trauma sub-group averaged 21 cm with a minimum of 17 cm. Analysis of splenic trauma in NASS revealed a weighted total of 3,551 occupants with splenic trauma in left side impact. Within the dataset, no cases below ΔV = 13 km/h were associated with splenic trauma. Additionally, 85% of weighted cases occurred at ΔV > 27 km/h.
Of the 272 cases with a deployed torso-interacting SAB, injury patterns were partially similar to non-SAB deployment cases. These injuries included incidences of head and cervical spine trauma, thorax trauma, pelvic fracture, and trauma to extremities. However, five cases suggested SAB-induced splenic trauma: Case occupants presented with splenic laceration or contusion following seat-mounted SAB deployment. In these cases, door intrusion was not present, and mean lateral ΔV was 8 km/h (max = 14 km/h). In addition to these five cases, five cases of splenic trauma were identified as possibly resulting from seat-mounted SAB. Higher ΔV (mean = 20 km/h) and intrusion (mean = 13 cm) precluded more conclusive determination.
SAB Trauma Cases
The following reports detail the circumstances surrounding suspected SAB-induced splenic trauma. They are summarized in Table 1.
Table 1.
Torso airbag injury pattern from case occupants
| Case | Age, Gender | Height, Weight | ΔV | Int. (cm) | Rib Injury | Lung Injury | Spleen Injury |
|---|---|---|---|---|---|---|---|
| 1 | 44, F | 170 cm, 52 kg | N/A | 0 | 2 fx (posterior) | contusion | Laceration (AIS 4) |
| 2 | 34, M | 175 cm, 76 kg | 5 km/h | 0 | * | * | Laceration (AIS 4) |
| 3 | 56, M | 163 cm, 88 kg | 14 km/h | 10 | 6 fx (posterior) | contusion | Laceration (AIS 3) |
| 4 | 48, F | 163 cm, 66 kg | 10 km/h | 0 | contusion | * | Fracture (NFS) |
| 5 | 61, M | 185 cm, 79 kg | 11 km/h | 0 | 2–3 fx | * | Laceration & Contusion (AIS 3) |
| The following cases suggest SAB related trauma: | |||||||
| 6 | 42, M | 175 cm, 88 kg | N/A | 0 | 4 fx (posterior) | L Basilar pneumothorax | Laceration (AIS 2) |
| 7 | 51, M | 157 cm, 65 kg | N/A | 20 | * | * | Contusion (AIS 2) |
| 8 | 22, F | 165 cm, 77 kg | 26 km/h | 12 | * | * | Laceration (AIS 4) |
| 9 | 23, F | 163 cm 50 kg | 27 km/h | 17 | 4 fx (posterior) | Contusion | Laceration (AIS 2) |
| 10 | 43, F | 158 cm, 48 kg | N/A | 13 | 2+ fx, displaced | * | Laceration (AIS 2) |
Case 1
The case vehicle, a 2000 minivan, was involved in a sideswipe collision. The left side of a 1992 compact pickup in the opposing lane contacted the left side of the case vehicle. The case vehicle came to a controlled stop. The impact was classified as minor, no intrusion into the occupant compartment was documented, and ΔV could not be calculated (Fig. 4).
Figure 4.
Case 1 vehicle damage and SAB.
The case occupant, the 44 year-old, 170 cm (5′ 7″), 52 kg (114 lb), female driver of the minivan, was reportedly using a three-point belt and the seat-mounted combination SAB deployed. She sustained a left pulmonary contusion, posterior fractures to left ribs 9 and 11, a left posterior chest wall contusion, and a severe (AIS 4) splenic laceration. Other occupants of the case vehicle (three, ages 9 to 11) were using the available three-point belts, were not subject to airbag deployments, and were not injured.
Case 2
The case vehicle, a 2001 four door sport-utility vehicle, lost control over ice on a one way limited access highway. The left front followed by the left rear struck a concrete barrier on the left shoulder of the roadway. The vehicle continued a counter-clockwise rotation before coming to rest facing oncoming traffic. The lateral ΔV was calculated to be 5 km/h and no occupant compartment intrusion occurred (Fig. 5).
Figure 5.
Case 2 vehicle damage and SAB.
The case occupant, the 34 year-old, 175 cm (5’9”), 76 kg (168 lb), male driver, was reportedly wearing a three-point belt and the seat-mounted combination SAB deployed (Fig. 5). The occupant, who drove the case vehicle to his residence following the incident, was reportedly jogging the subsequent morning when he began to experience abdominal pain. Upon hospital arrival, he was diagnosed with a severe (AIS 4) splenic laceration.
Case 3
The case vehicle, a 2004 compact SUV, was struck laterally by a 2003 mid-sized four door sedan in a four-leg intersection. Following a counterclockwise rotation, the case vehicle came to rest within the roadway facing the opposing direction. The lateral ΔV was calculated to be 14 km/h and maximum intrusion (below occupant hip level) was 10 cm (Fig. 6).
Figure 6.
Case 3 vehicle damage and SAB.
The case occupant, the 56 year-old, 163 cm (5’4”), 88 kg (191 lb) male driver, was restrained by a three-point belt and the seat-mounted combination SAB deployed through an overlaid sweatshirt (Fig. 6). He suffered contusions to left back and scapula, non-displaced fractures to left ribs 6 through 11, minimally-displaced fracture to rib 10, left unilateral lower lobe pulmonary contusion, and spleen laceration (AIS 3).
Case 4
The case vehicle, a 2003 compact SUV, was struck by a 1985 sub-compact coupe in a four leg intersection. The front right of the striking vehicle made contact with the front left of the case vehicle; both vehicles initiated opposing rotations causing a side-slap contact. The lateral ΔV was calculated to be 10 km/h and no intrusion occurred (Fig. 7).
Figure 7.
Case 4 vehicle damage and SAB.
The case occupant, the 48 year-old, 163 cm (5’4”), 66 kg (146 lb), female driver, was restrained by a three-point belt and the seat-mounted combination SAB deployed (Fig. 7). She was initially diagnosed with rib contusion (AIS 1) and abdominal skin contusion (AIS 1). While under care she developed abdominal pain with rapid onset of hypovolemic shock. She was diagnosed with a fractured spleen (NFS), and treated surgically.
Case 5
The case vehicle, a 2000 minivan, lost control while negotiating a left curve on a wet six-lane divided highway. The vehicle departed the roadway to the right in a clockwise yaw, struck a large wooden two-post roadway sign laterally, and came to rest entangled in a chain link fence. The vehicle contacted the signposts forward of the A-pillar and aft of the B-pillar. The lateral ΔV was calculated as 11 km/h, and no intrusion occurred in the vicinity of the case occupant (Fig. 8).
Figure 8.
Case 5 vehicle damage and SAB.
The case occupant, the 61 year-old, 185 cm (6’1”), 79 kg (174 lb), male driver, was restrained by a three-point belt and the seat mounted torso SAB deployed (Fig. 8). He sustained a splenic contusion and laceration (AIS 3), fractures of 2–3 ribs (AIS 2), and abrasions and contusions to the chest and abdomen (AIS 1). He was hospitalized for five days.
Possible Trauma
Five additional cases involving deployed SAB were noted in which with injury patterns were consistent with the preceding pattern. However, the severity of the crash did not allow the SAB to be conclusively designated as the source of energy. These cases, shown in Table 1, included four seat-mounted torso SABs and one seat-mounted combination SAB. Because the severity of impact, i.e., ΔV and/or intrusion, was similar to cases of splenic trauma in absence of SAB, conclusive determination of the injury source could not be made.
Summary
In addition to splenic trauma, Cases 1, 3, 4, and 5 demonstrated posterolateral injury to ribs, which varied from chest wall contusion (Case 4) to six total rib fractures including minimal rib displacement (Case 3). Cases 1 and 3 also included lung contusion to the posterior aspect of the lower left lobe. These injuries resulted from low severity impacts with little or no intrusion. Intrusion was reported only in Case 3 (10 cm) but was below both occupant abdomen and hip. Although one case did not include a calculation of crash velocity, all other cases were calculated between ΔV = 5 km/h and 14 km/h (3 mph and 9 mph).
Experiments
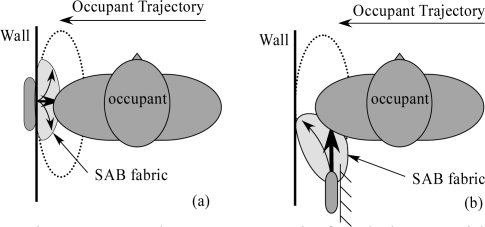
The aggregate thoracoabdominal injuries reported in these cases suggested that torso-interacting SABs may induce splenic trauma. Due to the anatomical location of the trauma, it was hypothesized that close-proximity deployment with coexistent lateral ΔV may represent a heretofore neglected injurious OOP scenario. Using seat- and door-mounted torso SABs, this scenario was reproduced in sled experiments by deploying the SAB with insufficient time to expand prior to thorax contact at ΔV = 24 km/hr (Fig. 9). A test matrix is shown in Table 2. The door-mounted SAB was activated when the occupant surrogate was 7 cm from the module, preventing occupant interaction with SAB cover flaps. The seat-mounted SAB was activated when the surrogate posterolateral thorax was directly forward of the module. Optimal deployment, in which thorax contact occurred following full airbag inflation, was also conducted with the THOR for purposes of comparison. Using lateral chestband analysis (Fig. 3a), thoracic injury metrics C and VC were obtained in the time domain for all five tests. THOR metrics in time domain are shown in Figure 10 for seat-mounted
Figure 9.
Deployment scenario for sled tests with (a) door-mounted and (b) seat-mounted SAB.
Table 2.
Scenarios of Biomechanical Investigation
| Test | Surrogate | Airbag | Scenario |
|---|---|---|---|
| 1 | THOR | Door | Optimal |
| 2 | THOR | Door | OOP |
| 3 | THOR | Seat | Optimal |
| 4 | THOR | Seat | OOP |
| 5 | PMHS | Seat | OOP |
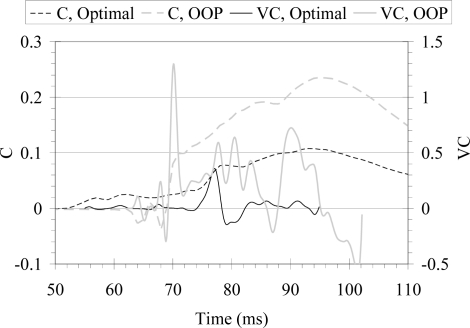
Figure 10.
Lateral biomechanical metrics of compression and viscous criterion in time domain for THOR seat-mounted SAB in optimal and OOP scenario.
SAB in optimal and OOP scenarios. Metrics are time-shifted such that without SAB, wall interaction would have occurred at t = 75 ms in both scenarios. The compression metric responded earlier in optimal deployment than in OOP scenario (t = 55 vs. 68 ms) due to contact with deeper fully-inflated SAB; both airbag scenarios induced peak compression at similar times (t = 95 ms). With optimal SAB inflation, the viscous metric peaked simultaneous to wall interaction (t ≈ 77 ms). In OOP, peak viscous metric was induced following initial airbag interaction (t ≈ 70 ms). Similar patterns were noted with the THOR during door-mounted side airbag tests: peak compression followed maximum wall interaction, peak viscous metric followed airbag interaction in OOP.
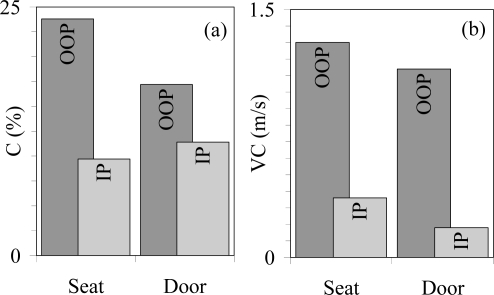
Peak biomechanical metrics resulting from THOR with seat- and door-mounted SAB are shown in Figure 11. While the optimally inflated seat-mounted SAB yielded lower lateral compression metrics than the optimum door-mounted SAB, the seat-mounted SAB also yielded greater compression than the door-mounted SAB in OOP scenario. Considering the viscous metric, the door SAB induced lower metrics than the seat SAB when optimally deployed, and the seat SAB induced greater metrics than the door SAB in OOP. Lateral compression in OOP was C = 24% with seat- and C = 17% with door-mounted SAB; viscous metric was VC = 1.3 m/s with seat- and VC = 1.1 m/s with door-mounted SAB. PMHS lateral metrics in OOP with seat-mounted airbag attained C = 35% and VC = 1.6 m/s.
Figure 11.
Peak lateral biomechanical metrics of (a) compression and (b) viscous criterion calculated in THOR deformation for seat- and door-mounted SABs. Out-of-position (OOP) and in-position (IP) scenarios are indicated.
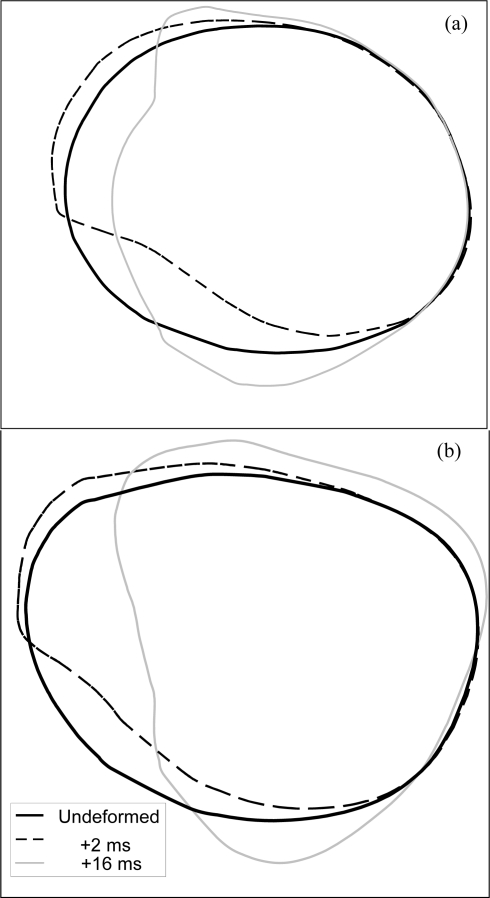
Posterolateral loading was unique to the seat-mounted SAB. Shown in Figure 12 are chestband contours for the THOR and PMHS obtained from seat-mounted airbag deployment in OOP. Following SAB activation, forward inflation subjected the posterolateral thorax to high velocity low magnitude deformation. Quantified as shown in Figure 3b, THOR peak posterolateral deflection and deflection rate were 36 mm and 30 m/s; PMHS values, scaled to subject mass, were 23 mm and 20 m/s. Peak values were measured between the 10% and 40% circumference locations in both surrogates; this was the approximate site of initial airbag interaction. Peak deformation was attained two milliseconds following airbag contact. With impact progression, the seat-mounted airbag inflated into the narrowing space between occupant and impact wall. Posterolateral deformation was then dominated by lateral deformation response. The autopsy post-test revealed injuries to the thorax in the form of unilateral left flail chest, left labrum tear, and AIS 3 splenic laceration.
Figure 12.
Chestband contours at level demonstrating posterolateral deformation of (a) THOR and (b) PMHS occupant surrogates with OOP seat-mounted SAB deployment.
DISCUSSION
The present study examined individual case reports of lateral impacts involving torso-interacting SABs. Five cases were identified in which case occupants presented with splenic trauma. These injuries were suspect because they occurred (i) at ΔV less than all cases of side impact splenic trauma found within the CIREN and NASS databases and (ii) in absence of substantial occupant compartment intrusion. An additional five cases were identified in which occupants presented with similar injury patterns but sustained either (i) ΔV greater than minimum NASS and CIREN values or (ii) compartment intrusion in the vicinity of the occupant seat location. Laboratory experiments reproducing close-proximity SAB deployment with coexistent lateral ΔV revealed elevated lateral thoracic injury metrics when compared to optimal deployment metrics. Posterolateral thoracic deformation also occurred in THOR and PMHS occupant surrogates with seat-mounted SAB deployment; in this scenario splenic laceration (AIS 3) was reproduced in PMHS.
Other sources of injury in these five real-world cases were considered unlikely. These sources included other occupants, belt pretensioners, vehicle yawing and excessive ΔV. Of five cases presented in this study, two case vehicles contained more than one occupant. All occupants were restrained by three-point belts, reducing likelihood of occupant torso interaction. Although belt pretensioners were present in three vehicles, none appeared to be activated. Vehicle yawing, shown to affect occupant kinematics [Marine & Werner, 1998], may have contributed to crash severity. However, yaw rate demonstrated in these five cases was not consistent in presence or direction. Accuracy of reported ΔV was also considered. Previous comparison of ΔV, reconstructed by computer algorithms using vehicle crush profiles, and onboard Event Data Recorders (EDR) demonstrated ΔV to underestimate actual impact severity in frontal scenarios [Niehoff & Gabler, 2006]. Conversely, examination of reconstructed ΔV and lateral crash tests has revealed algorithmic overestimations averaging 10 km/h [Johnson et al., 2009]. Despite possible error in reported ΔV, cases demonstrated minimal vehicle crush and lack of compartment intrusion. By these measures, impacts could still be classified as minor validly.
Although not uncommon in motor vehicle crashes, splenic trauma has not been associated heretofore with low ΔV near-side impacts involving SAB deployment. Risk did not appear associated with factors such as age, gender, height, weight, or body mass index. Epidemiological analyses of splenic trauma have identified door interior contact as the most probable injury mechanism in lateral impact [Siegel et al., 1993; Reiff et al., 2001]. Reported by Reiff et al., splenic injury risk increased five-fold when intrusion was > 30 cm as compared to intrusion of 1 – 30 cm magnitude. Biomechanical assessments have also identified intrusion as the primary mechanism of injury in lateral impact [Cesari et al., 1978]. The lack of intrusion reported during these SAB cases, in combination with low ΔV, may indicate the presence of a contrasting injury mechanism.
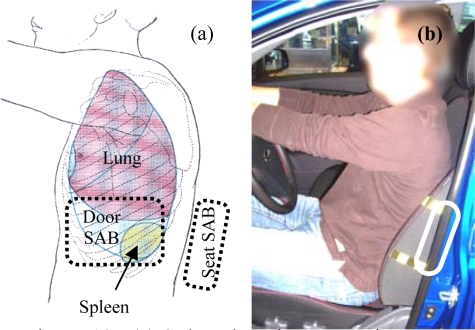
Shown in Figure 13(a) are representative seat- and door-mounted SAB locations in relationship to spleen location in situ [Gray, 1985]. It is apparent that the thoracoabdominal region containing the spleen is nearest the site of SAB deployment. Therefore, this region may be more susceptible to injury if occupant posture deviates toward the SAB. Postural deviation is not abnormal; unaware subject position variations have been reported in excess of 22 cm under normal driving conditions [Dinas & Fildes, 2002]. A fiftieth percentile male exemplar occupant is shown in Figure 13(b). The SAB location in this vehicle seat was palpated and marked, demonstrating the preferred installation region within the seat-back of vehicles sold in the U.S. If the occupant deviated laterally in this exemplar vehicle, the posterolateral thorax and abdomen likely would be exposed to SAB deployment forces. The response of the lateral thorax reported in this study indicated that deformations were greater in these OOP scenarios. Lateral injury metrics recorded on THOR tests were elevated by both seat- and door-mounted SAB when lateral position deviation was considered.
Figure 13.
(a) Spleen location in situ in relationship to common seat- and door-mounted SAB locations. Modified from Gray (1985) (b) Exemplar vehicle occupant with seat-mounted SAB marked by palpation and indicated.
The occurrence of splenic trauma in PMHS in this study is quite significant. At this lower impact ΔV, splenic trauma has not been induced in this laboratory with rigid or padded wall boundary conditions in cadaveric test subjects [Pintar et al., 1997; Kuppa et al., 2003; Yoganandan et al., 2008]. Including a literature review of left lateral impact cadaveric testing, only one instance of splenic trauma was reported among seventy-five cadaveric specimens tested below 26 km/h [Melvin et al., 1976; Morgan et al., 1980; Kallieris et al., 1981; Eppinger et al., 1984; Viano, 1989; Cavanaugh et al., 1996]. These experiments utilized both sleds and pendulum impactors with padded and rigid boundary conditions. Although the mechanism by which splenic trauma was induced with SAB remains obscure, this study suggests that it may be unique to side airbag loading in OOP at this ΔV.
Biomechanical tests also revealed posterolateral loading and deformation patterns not yet addressed in the literature. Trauma resulting from thoracic deformation has previously been evaluated from frontal [Rouhana et al., 1985; Lebarbe et al., 2005], lateral [Viano et al., 1989; Cavanaugh et al., 1996; Pintar et al., 1997; Chung et al., 1999; Kuppa et al., 2003], and most recently anterolateral [Yoganandan et al., 1997; Shaw et al., 2006; Yoganandan et al., 2008] loading. Although posterolateral loading has not been considered previously, these studies of thoracic injury have noted injury mechanisms resulting both from magnitude of deformation (compression) and from rate of deformation (velocity). Therefore, it is likely that posterolateral loading may induce injuries by similar mechanisms. In OOP, seat-mounted side airbag was found to induce small posterolateral deformations but high deformation rates. Because visceral injury response is dominated by velocity when rates approach 30 m/s [Lau & Viano, 1986], the high velocity of posterolateral deformation found in this study may be most relevant to the splenic injury sustained.
The apparent possibility of splenic trauma from SAB is problematic for both clinicians and biomechanical researchers. The vascular nature of the spleen and its location in situ, deep to the posterolateral curvature of left ribs 9–11, exposes it to compression and viscous injury from blunt trauma [Yoganandan et al., 2000; Yoganandan et al., 2001]. Acute splenic trauma can be life-threatening, and hemorrhaging requires immediate medical intervention [Harbrecht et al., 2007]. Although treatment course is increasingly non-operative, as many as one-third of cases still necessitate splenectomy [Harbrecht et al., 2007]. This procedure has been associated with a lifelong risk of overwhelming sepsis [El-Alfy & El-Sayed, 2004]. Furthermore, risk of splenic trauma may be increased by splenomegaly, a secondary indication to many common conditions [Vasef & Platz, 2002]. Therefore any association between splenic trauma risk and torso SABs should be thoroughly explored.
One case presented in this study demonstrated the potential latency of splenic hemorrhage induced by SAB deployment. As many as one-third of patients presenting with acute splenic trauma suffer from “delayed rupture” [Leppaniemi et al., 1988]. This condition is characterized by splenic trauma from which hemorrhaging does not manifest for at least 48 hours [Parithivel et al., 2002]. During this latency, even contrast-enhanced abdominal imaging scans may appear normal [Leppaniemi et al., 1988]. Reported delays are commonly two to ten days [Leppaniemi et al., 1988; Parithivel et al., 2002]. Although many mechanisms may contribute to this condition [Parithivel et al., 2002], delayed rupture poses unique complications to treatment. The onset of splenic hemorrhaging can present with “explosive suddenness” and can rapidly develop into hypovolemic shock [Wooldridge, 1969; Ruffolo, 2002]. The patient, two days or more removed from the traumatic event, may be unprepared to seek emergency medical attention. Although the latency period reported in this study was insufficient to be characterized as a delayed rupture (twelve hours), the case occupant was participating in strenuous exercise prior to seeking medical treatment, subjecting himself to further risk of complication. Given the latencies previously reported [Leppaniemi et al., 1988], acute SAB-induced splenic injuries may exist in the current population which were simply not correctly associated with airbag deployment.
Many of the patients presented in this study would not be evaluated for serious trauma due to the low apparent crash energy. Recognition of the association of side airbag deployment with splenic injury should heighten clinicians’ suspicion for splenic injury in patients with low ΔV and/or minimal intrusion with SAB deployment. Even minor abdominal signs or symptoms in these patients should be evaluated with either CT scan or inhospital observation.
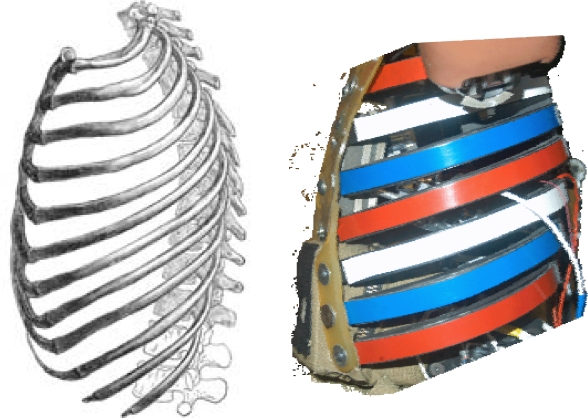
Further PMHS testing may delineate other injury risks associated with this posterolateral loading modality, provide corridors for biofidelity assessments, and establish injury criteria specific to OOP occupants with SAB deployment in side impacts. Future biofidelity assessments may be especially important to regulatory crashworthiness evaluations utilizing anthropomorphic test devices. The THOR thorax utilized in this study, although not instrumented for lateral impact, was composed of ribs oriented physiologically (Fig. 14). This permitted the measurement of thoracic deformation in multiple directions of loading. Side airbag loading modalities in current U.S. automobiles may necessitate similar designs for regulatory evaluations of side impact performance.
Figure 14.
THOR thorax composition and anatomical rib arrangement, viewed from lateral. Modified from Gray (1985)
CONCLUSION
This anecdotal and biomechanical study may suggest a new adverse effect of torso-protecting SABs. Splenic trauma was found to result from low severity crashes (as measured by ΔV and occupant compartment intrusion) involving vehicles equipped with seat-mounted SAB. Sled tests with mechanical and biological occupant surrogates revealed elevated lateral thoracic injury metrics when SAB was deployed in close proximity to the occupant with coexistent lateral ΔV. When occupant thorax obstructed seat-mounted SAB deployment, high velocity low magnitude posterolateral thoracoabdominal deformation was observed, and AIS 3 splenic trauma was induced in a cadaveric specimen. Because of the severity of splenic trauma and the possibility of delayed hemorrhage, any potential injury risk associated with SAB deployment should be thoroughly investigated.
Acknowledgments
This research was supported in part by: US DOT NHTSA DTNH22-05-H-41001, NSF Graduate Research Fellowship Program, AAAM Student Research Grant, and VA Medical Research. The authors are grateful for the assistance of Mr. Dale Halloway of the Wisconsin CIREN Center and Mr. Mark Meyer of the Neuroscience-Biomechanics Laboratories. The views and opinions expressed in this manuscript do not represent the consensus or policy of the sponsoring organizations and are solely from the authors.
REFERENCES
- Arbogast KB, Durbin DR, Kallan MJ, et al. Injury risk to restrained children exposed to deployed first- and second-generation air bags in frontal crashes. Arch.Pediatr.Adolesc.Med. 2005;159(4):342–346. doi: 10.1001/archpedi.159.4.342. [DOI] [PubMed] [Google Scholar]
- Braver ER, Scerbo M, Kufera JA, et al. Deaths among drivers and right-front passengers in frontal collisions: Redesigned air bags relative to first-generation air bags. Traffic Inj.Prev. 2008;9(1):48–58. doi: 10.1080/15389580701722787. [DOI] [PubMed] [Google Scholar]
- Cavanaugh JM, Wililko T, Chung J, et al. Abdominal injury and response in side impact. 40th Stapp Car Crash Conference; Albuquerque, New Mexico, USA. 1996. [Google Scholar]
- Cesari D, Ramet M, Herry-Martin D. Injury mechanisms in side impact. 22nd Stapp Car Crash Conference; Ann Arbor, Michigan, USA. 1978. [Google Scholar]
- Chung J, Cavanaugh JM, King AI, et al. Thoracic injury mechanisms and biomechanical responses in lateral velocity pulse impacts. 43rd Stapp Car Crash Conference; San Diego, California, USA. 1999. [Google Scholar]
- Dinas A, Fildes BN. Observations of seating position of front seat occupants relative to the side of the vehicle. Annu.Proc.Assoc.Adv. Automot Med. 2002;46:27–43. [PubMed] [Google Scholar]
- Duma SM, Crandall JR, Rudd RW, et al. Small female head and neck interaction with a deploying side airbag. Accid.Anal.Prev. 2003;35(5):811–816. doi: 10.1016/s0001-4575(02)00085-4. [DOI] [PubMed] [Google Scholar]
- Duma SM, Boggess BM, Crandall JR, et al. Upper extremity interaction with a deploying side airbag: A characterization of elbow joint loading. Accid.Anal.Prev. 2003;35(3):417–425. doi: 10.1016/s0001-4575(02)00020-9. [DOI] [PubMed] [Google Scholar]
- El-Alfy MS, El-Sayed MH. Overwhelming postsplenectomy infection: Is quality of patient knowledge enough for prevention? Hematol.J. 2004;5(1):77–80. doi: 10.1038/sj.thj.6200328. [DOI] [PubMed] [Google Scholar]
- Eppinger RH, Marcus JH, Morgan RM. Development of dummy and injury index for NHTSA’s thoracic side impact protection research program. SAE 840885. 1984 [Google Scholar]
- Gray H. Gray’s anatomy. 30th ed. Baltimore: Williams & Wilkins; 1985. [Google Scholar]
- Harbrecht BG, Zenati MS, Ochoa JB, et al. Evaluation of a 15-year experience with splenic injuries in a state trauma system. Surgery. 2007;141(2):229–238. doi: 10.1016/j.surg.2006.06.032. [DOI] [PubMed] [Google Scholar]
- Highway Loss Data Institute Vehicles equipped with side airbags. 2008.
- Insurance Institute for Highway Safety Recommended procedures for evaluating occupant injury risk from deploying side airbags. Side Airbag Out-of-Position Injury Technical Working Group. 2003 [Google Scholar]
- Johnson N, Hampton C, Gabler HC. Evaluation of the accuracy of side impact crash test reconstructions. Biomed.Sci.Instrum. 2009;45:250–255. [PubMed] [Google Scholar]
- Kallieris D, Mattern R, Schmidt G, et al. Quantification of side impact responses and injuries. 25th Stapp Car Crash Conference.; San Francisco, California, USA. 1981. [Google Scholar]
- Khadilker AV, Pauls LS. Assessment of injury protection performance of side impact airbags for out-of-position and other than 50th percentile adult male occupants. 16th International ESV Conference; Windsor, Ontario, Canada. 1998. [Google Scholar]
- Kleinberger M, Summers L. Mechanisms of injuries for adults and children resulting from airbag interaction. Annu.Proc.Assoc.Adv. Automot Med. 1997;41:405–420. [Google Scholar]
- Kuppa S, Eppinger RH, McKoy F, et al. Development of side impact thoracic injury criteria and their application to the modified ES-2 dummy with rib extensions (ES-2re) Stapp Car Crash J. 2003;47:189–210. doi: 10.4271/2003-22-0010. [DOI] [PubMed] [Google Scholar]
- Lau IV, Viano DC. The viscous criterion - bases and applications of an injury severity index for soft tissues. 30th Stapp Car Crash Conference; San Diego, California, USA. 1986. [Google Scholar]
- Lebarbe M, Potier P, Baudrit P, et al. Thoracic injury investigation using PMHS in frontal airbag out-of-position situations. Stapp Car Crash J. 2005;49:323–342. doi: 10.4271/2005-22-0015. [DOI] [PubMed] [Google Scholar]
- Leppaniemi A, Haapiainen R, Standertskjold-Nordenstam CG, et al. Delayed presentation of blunt splenic injury. Am.J.Surg. 1988;155(6):745–749. doi: 10.1016/s0002-9610(88)80035-7. [DOI] [PubMed] [Google Scholar]
- Marine MC, Werner SM. Delta-V analysis from crash test data for vehicles with post-impact yaw motion. SAE 980219. 1998 [Google Scholar]
- Melvin JW, Robbins DH, Stalnaker RL. Side impact response and injury. Sixth International ESV Conference; London, England. 1976. [Google Scholar]
- Melvin JW, Horsch JD, McCleary JD, et al. Assessment of airbag deployment loads with the small female hybrid III dummy. 37th Stapp Car Crash Conference; San Antonio, Texas, USA. 1993. [Google Scholar]
- Morgan RM, Waters HP. Comparison of two promising side impact dummies. Eighth International ESV Conference; Wolfsburg, Germany. 1980. [Google Scholar]
- National Highway Traffic Safety Administration. Actions to reduce the adverse effects of airbags: Depowering. Final Regulatory Evaluation. 1997
- National Highway Traffic Safety Administration Counts of airbag related fatalities and seriously injured persons. AB0708. 2008 [Google Scholar]
- Niehoff P, Gabler HC. The accuracy of WinSmash delta-V estimates: The influence of vehicle type, stiffness, and impact mode. Annu.Proc. Assoc.Adv.Automot Med. 2006;50:73–89. [PMC free article] [PubMed] [Google Scholar]
- Olson CM, Cummings P, Rivara FP. Association of first- and second-generation air bags with front occupant death in car crashes: A matched cohort study. Am.J.Epidemiol. 2006;164(2):161–169. doi: 10.1093/aje/kwj167. [DOI] [PubMed] [Google Scholar]
- Parithivel VS, Sajja SB, Basu A, et al. Delayed presentation of splenic injury: Still a common syndrome. Int.Surg. 2002;87(2):120–124. [PubMed] [Google Scholar]
- Pintar FA, Yoganandan N, Sances A, et al. Instrumentation of human surrogates for side impact. 40th Stapp Car Crash Conference; Albuquerque, New Mexico, USA. 1996. [Google Scholar]
- Pintar FA, Yoganandan N, Maltese MR, et al. Three-year-old child out-of-position side airbag studies. 43rd Stapp Car Crash Conference; San Diego, California, USA. 1999. [Google Scholar]
- Pintar FA, Yoganandan N, Hines MH, et al. Chestband analysis of human tolerance to side impact. 41st Stapp Car Crash Conference; Lake Buena Vista, Florida. 1997. [Google Scholar]
- Prasad AK, Samaha RR, Louden AE. Evaluation of injury risk from side impact air bags. 17th International ESV Conference; Amsterdam, The Netherlands. 2001. [Google Scholar]
- Reiff DA, McGwin G, Jr, Rue LW., 3rd Splenic injury in side impact motor vehicle collisions: Effect of occupant restraints. J.Trauma. 2001;51(2):340–345. doi: 10.1097/00005373-200108000-00020. [DOI] [PubMed] [Google Scholar]
- Rouhana SW, Lau IV, Ridella SA. Influence of velocity and forced compression on the severity of abdominal injury in blunt, nonpenetrating lateral impact. J.Trauma. 1985;25(6):490–500. doi: 10.1097/00005373-198506000-00004. [DOI] [PubMed] [Google Scholar]
- Ruffolo DC. Delayed splenic rupture: Understanding the threat. J.Trauma Nurs. 2002;9(2):34–40. doi: 10.1097/00043860-200209020-00002. [DOI] [PubMed] [Google Scholar]
- Shaw JM, Herriott RG, McFadden JD, et al. Oblique and lateral impact response of the PMHS thorax. Stapp Car Crash J. 2006;50:147–167. doi: 10.4271/2006-22-0007. [DOI] [PubMed] [Google Scholar]
- Siegel JH, Mason-Gonzalez S, Dischinger P, et al. Safety belt restraints and compartment intrusions in frontal and lateral motor vehicle crashes: Mechanisms of injuries, complications, and acute care costs J.Trauma. 345736–58.; discussion 758–9. 1993 [DOI] [PubMed] [Google Scholar]
- Tylko S, Dalmotas D. Assessment of injury risk to children from side airbags. 44th Stapp Car Crash Conference; Atlanta, Georgia, USA. 2000. [DOI] [PubMed] [Google Scholar]
- Vasef M, Platz CE. The pathology of the spleen. In: Bowdler AJ, editor. The complete spleen. 2nd ed. USA: Humana Press; 2002. pp. 72–106. [Google Scholar]
- Viano DC. Biomechanical responses and injuries in blunt lateral impact. 33rd Stapp Car Crash Conference; Washington, D.C., USA. 1989. [Google Scholar]
- Viano DC, Lau IV. A viscous tolerance criterion for soft tissue injury assessment. J.Biomech. 1988;21(5):387–399. doi: 10.1016/0021-9290(88)90145-5. [DOI] [PubMed] [Google Scholar]
- Viano DC, Lau IV, Andrzejak DV, et al. Biomechanics of injury in lateral impacts. Accid.Anal.Prev. 1989;21(6):535–551. doi: 10.1016/0001-4575(89)90069-9. [DOI] [PubMed] [Google Scholar]
- Wooldridge BF. Traumatic rupture of the spleen. A review. Mo.Med. 1969;66(10):804–806. [PubMed] [Google Scholar]
- Yoganandan N, Pintar FA, Maltese MR. Biomechanics of abdominal injuries. Crit. Rev.Biomed.Eng. 2001;29(2):173–246. doi: 10.1615/critrevbiomedeng.v29.i2.10. [DOI] [PubMed] [Google Scholar]
- Yoganandan N, Pintar FA, Gennarelli TA, et al. Patterns of abdominal injuries in frontal and side impacts. Annu.Proc.Assoc.Adv.Automot Med. 2000;44:17–36. [PMC free article] [PubMed] [Google Scholar]
- Yoganandan N, Pintar FA, Zhang J, et al. Lateral impact injuries with side airbag deployments-a descriptive study. Accid.Anal.Prev. 2007;39(1):22–27. doi: 10.1016/j.aap.2006.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoganandan N, Pintar FA, Kumaresan S, et al. Impact biomechanics of the human thoraxabdomen complex. Int. J. Crashworthiness. 1997;2(2):219. [Google Scholar]
- Yoganandan N, Pintar FA, Stemper BD, et al. Biomechanics of side impact: Injury criteria, aging occupants, and airbag technology. J.Biomech. 2007;40(2):227–243. doi: 10.1016/j.jbiomech.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoganandan N, Pintar FA, Gennarelli TA, et al. Chest deflections and injuries in oblique lateral impacts. Traffic Inj.Prev. 2008;9(2):162–167. doi: 10.1080/15389580701775942. [DOI] [PubMed] [Google Scholar]