Abstract
Ventilator-associated pneumonia (VAP) is a complication of ventilator care that produces excess, avoidable resource use and treatment costs. Control of VAP is an important aspect of quality of care improvement for long-term care hospitals (LTCHs) since they provide post-acute ventilator care for many Medicare beneficiaries. Data for Medicare patients discharged from LTCHs during CY 2004 who received continuous mechanical ventilation are examined (N=13,759). Nearly 25% of Medicare LTCH ventilator patients acquired VAP. Despite having lower mortality and less co-morbidity than non-VAP patients, length of stay (LOS) and total charges were both higher for VAP patients. Some of this excess is avoidable.
Introduction
Ventilator-associated pneumonia (VAP) refers to nosocomial pneumonia occurring in patients receiving mechanical ventilation 48 hours or more after airway intubation. It is a common complication of care that affects approximately one-fourth of patients receiving mechanical ventilation and often produces excess (and likely avoidable) LOS, mortality and treatment costs (Kollef, 2005; Chastre and Fagon, 2002). VAP is the leading cause of nosocomial mortality for patients with respiratory failure (Kollef, 2005). Early onset VAP cases generally occur within 4 days of hospitalization and usually carry a better prognosis than late onset cases occurring later than 4 days from admission (Chastre and Fagon, 2002). Previous studies in acute care settings indicate that males, trauma patients and severely ill patients are at increased risk for VAP (Chastre and Fagon, 2002; Kollef, 2005). Kollef (2005) reviews the pathogenesis of VAP (an avoidable, hospital-acquired infection) and states that many VAP cases are preventable if appropriate interventions are in place.
Several studies have examined the effects of VAP in inpatient facilities. Rello et al. (2002) and Bregeon et al. (2001) found that there was no significant difference in inpatient mortality among ventilator patients with and without VAP. Several studies have found that the presence of VAP substantially increased duration of mechanical ventilation compared to patients without VAP. This, in turn, increased patient ICU days, inpatient LOS and billed charges for patients with VAP (Chastre and Fagon, 2002; Rello et al., 2002; Kollef, 2005; Safdar et al., 2005; Hugonnet et al., 2007). These studies suggest that control of VAP would save hospital resources and costs and improve outcomes. The incidence and outcomes of VAP in post acute settings have not been extensively examined. The largest study of mechanical ventilation in LTCHs (Ventilator Outcomes [Barlow] Study) found that 31% of the 1,419 study patients in 23 LTCHs were treated for pneumonia or tracheobronchitis in 2003 but did not discuss VAP control issues (Scheinhorn et al., 2007).
A recent study at a large LTCH examined 23 cases of VAP involving 19 patients that were associated with 157 LTCH admissions. This study found that the VAP rate in the study LTCH was lower than VAP rates found in acute care hospitals and that systematic implementation of several coordinated interventions to prevent the likelihood of hospital-acquired infections (VAP care bundles) were effective in reducing VAP rates in an LTCH setting (Walkey et al., 2009). In ICU settings, Resar et al. (2005) found that units that that consistently collected data on the level of adherence to administration of ventilator care bundle elements and incidence of VAP cases experienced an average reduction in VAP rates of 44.5%. The purpose of this article is to attempt to determine if similar excess days of care and costs are observed among Medicare ventilator patients contracting VAP in LTCHs.
Ventilator Care in LTCHs
Medicare LTCHs are distinguished by having a Medicare LOS of 25 days or more. LTCHs provide extended medical treatment for clinically complex patients who often have multiple acute or chronic conditions. Thus, the patients treated in LTCHs are very different from patients treated in acute care hospitals. LTCHs occupy an unusual position among Medicare providers since they must participate in Medicare as a hospital but they are among the set of providers that receive a high percentage of their patients from acute care hospitals (paid under the IPPS) for additional care.
Many LTCHs specialize in respiratory care but almost all LTCHs treat some respiratory patients. LTCHs provide post-acute ventilator care for many Medicare beneficiaries with complex conditions requiring long stays (Liu et al., 2001). As a result, the LTCH patient population has a high level of comorbidities and infacility mortality. The number of LTCHs in operation has increased substantially since 2000. Because of the long average LOS in these facilities, LTCHs were exempted from the Medicare Acute Care Hospital Prospective Payment System from the beginning of its operation in 1984. A prospective payment system for LTCHs began operation in 2002. LTCHs are dependent on Medicare for patients and for revenue since over 70% of discharges from LTCHs are Medicare patients (Liu et al., 2001).
The Medicare Program has become increasingly concerned with quality of care for all service providers, especially those providing nursing home or home health care. One area of concern is linking payments for services to performance on quality of care measures to provide incentives for the provision of high quality care. Unfortunately, CMS' efforts toward measurement of quality of care for LTCHs lags behind established quality of care programs and data banks for other post acute care providers. Because of the importance of provision of mechanical ventilation for the LTCH industry and for facilities specializing in treating respiratory conditions, control of VAP is an important aspect of quality of care improvement in LTCHs. To date, quality of care in LTCHs and incidence and control of VAP in LTCH settings have not been extensively examined. As a result, there has been little information about the incidence of VAP in LTCHs and the effects of VAP on length of patient stays and costs of care in this setting. This is especially important since ventilator care provided in LTCHs has different treatment objectives from ventilator care received in ICUs to patients at risk of death.
Data
MEDPAR discharge data for LTCHs are examined for Medicare fee-for-service beneficiaries who were discharged during CY 2004 with a procedure code of 96.72 (continuous mechanical ventilation for 96 consecutive hours or more) to avoid early onset infections that may have begun prior to the LTCH admission (N=13,759). The following comorbidities were also examined: VAP, renal failure, diabetes, hypertension, stroke, chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF). Their coding is described in Table 1.
Table 1. Coding of Comorbidities.
| Ventilator-associated Pneumonia (VAP) | ICD-9-CM codes 481.xx – 486.xx. |
| Renal Failure | ICD-9-CM codes 584.xx – 586.xx. |
| Diabetes | ICD-9-CM codes 250.xx. |
| Hypertension | ICD-9-CM codes 401.xx – 405.xx. |
| Stroke | ICD-9-CM codes 430.xx – 438.xx. |
| Chronic Obstructive Pulmonary Disease (COPD) | ICD-9-CM codes 490.xx – 496.xx. |
| Congestive Heart Failure (CHF) | ICD-9-CM code 428. |
SOURCE: Centers for Disease Control and Prevention: International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), 2009.
Descriptive data on the percentage of continuous mechanical ventilation patients acquiring VAP are examined by age, race, sex, presence of comorbidities (renal failure, diabetes, hypertension, stroke, COPD, CHF, number of comorbidities), admission source, discharge destination, total Medicare charges, in-hospital mortality and post-discharge survival. Total Medicare charges are used to assess the overall expense of treatment (from the perspective of the provider rather than Medicare) and are used as a proxy for cost data.
The following multivariate models are presented.
A logistic model for the effects of demographics and comorbidities on acquiring VAP.
A proportional hazards model examining mortality rates at 2 years postdischarge.
Linear models predicting the impact of VAP on LOS and on total Medicare charges.
Results
As shown in Table 2, nearly 25% of Medicare LTCH ventilator patients acquired VAP. The average age of patients with and without VAP was the same (72 years). There were only minor differences in the distribution of VAP incidence across age groups. Men were more likely than women to have acquired VAP while in an LTCH. Blacks and Hispanics appeared to be were less likely to have acquired VAP during continuous mechanical ventilation in LTCHs than either whites or other races.
Table 2. Demographic Statistics for CY 2004 LTCH Continuous Mechanical Ventilation Patients.
| VAP | Percent | Non-VAP | Percent | Total | Percent | |
|---|---|---|---|---|---|---|
|
| ||||||
| Total | 3,371 | 100.0% | 10,388 | 100.0% | 13,759 | 100.0% |
| Age Group NS | ||||||
| 90 and Older | 91 | 2.7 | 351 | 3.4 | 442 | 3.2 |
| 85 - 89 | 251 | 7.4 | 823 | 7.9 | 1,074 | 7.8 |
| 80 - 84 | 522 | 15.5 | 1,574 | 15.2 | 2,096 | 15.2 |
| 75 - 79 | 719 | 21.3 | 2,118 | 20.4 | 2,837 | 20.6 |
| 70 - 74 | 623 | 18.5 | 1,959 | 18.9 | 2,582 | 18.8 |
| 65 - 69 | 573 | 17.0 | 1,685 | 16.2 | 2,258 | 16.4 |
| 60 - 64 | 196 | 5.8 | 621 | 6.0 | 817 | 5.9 |
| 55 - 59 | 148 | 4.4 | 435 | 4.2 | 583 | 4.2 |
| 50 - 54 | 99 | 2.9 | 344 | 3.3 | 443 | 3.2 |
| 0 - 49 | 149 | 4.4 | 478 | 4.6 | 627 | 4.6 |
| Mean Age | 72.3 | 72.2 | 72.2 | T=0.29 | ||
| Sex ** | ||||||
| Male | 1,822 | 54.0 | 4,908 | 47.2 | 6,730 | 48.9 |
| Female | 1,549 | 46.0 | 5,480 | 52.8 | 7,029 | 51.1 |
| Race ** | ||||||
| White | 2,635 | 78.2 | 7,619 | 73.3 | 10,254 | 74.5 |
| Black | 570 | 16.9 | 2,190 | 21.1 | 2,760 | 20.1 |
| Hispanic | 60 | 1.8 | 247 | 2.4 | 307 | 2.2 |
| Other | 106 | 3.1 | 332 | 3.2 | 438 | 3.2 |
NOTES:
= Chi Square not significant at .05 level.
= Chi Square significant at .05 level.
= Chi Square significant at .01 level or greater.
SOURCE: CY 2004 Medicare Discharge Data for LTCHs.
The most common comorbidity observed was COPD (Table 3) but the difference between patients with and without VAP was not significant. Other comorbidities of importance were CHF, hypertension, renal failure, diabetes and stroke. Each of these comorbidities was more prevalent in non-VAP patients, although the difference associated with renal failure was not statistically significant. Patients with VAP tended to have less total comorbidity than ventilator patients without VAP (Table 3). Patients with VAP were more likely to have no comorbidities or one comorbidity. In contrast, ventilator patients without VAP were more likely to have either two, or three or more comorbidities. While both patient groups are very ill and comorbid as one would expect in an LTCH ventilator population, non-VAP patients may well be more comorbid than patients with VAP. The logistic model for the effects of demographics and comorbidities on acquiring VAP (Table 4) concurs with the descriptive results in Tables 2 and 3. Females, Blacks and Hispanics were significantly less likely to have VAP. Again, presence of comorbidities tended to negatively associated with having VAP.
Table 3. Comorbidities for LTCH Continuous Mechanical Ventilation Patients.
| VAP | Percent | Non-VAP | Percent | Total | Percent | |
|---|---|---|---|---|---|---|
| Total | 3,371 | 24.5% | 10,388 | 75.5% | 13,759 | 100.0% |
| Renal Failure NS | 638 | 18.9 | 1,998 | 19.2 | 2,636 | 19.2 |
| Diabetes ** | 386 | 11.5 | 1,804 | 17.4 | 2,190 | 15.9 |
| Hypertension ** | 668 | 19.8 | 1,574 | 28.2 | 3,595 | 26.1 |
| Stroke** | 127 | 3.8 | 583 | 5.6 | 710 | 5.2 |
| Chronic Obstructive NS Pulmonary Disease | 1,675 | 49.7 | 5,032 | 48.4 | 6,707 | 48.8 |
| Congestive Heart ** Failure | 1,247 | 37.0 | 4,164 | 40.1 | 5,411 | 39.3 |
| Number of Comorbidities ** | ||||||
| No Comorbidities | 598 | 17.7 | 1,443 | 13.9 | 2,041 | 14.8 |
| 1 Comorbidity | 1,305 | 38.7 | 3,568 | 34.4 | 4,873 | 35.4 |
| 2 Comorbidities | 1,034 | 30.7 | 3,551 | 34.2 | 4,585 | 33.3 |
| 3 or More Comorbidities | 434 | 12.9 | 1,826 | 17.5 | 2,260 | 16.5 |
| Average Number of Comorbidities | 1.4 | 1.6 | 1.5 | T=3.52 | ||
NOTES:
= Chi Square not significant at .05 level.
= Chi Square significant at .05 level.
= Chi Square significant at .01 level or greater.
SOURCE: CY 2004 Medicare Discharge Data for LTCHs.
Table 4. Effects of Demographics and Comorbidities on Ventilator Patients Acquiring VAP.
| Predictors | Coefficient | Standard Error | T | Odds Ratio |
|---|---|---|---|---|
| Age | 0.0016 | 0.0018 | 0.87 | 1.002 |
| Female | -0.2463 | 0.0403 | - 6.10 | 0.782 |
| Black | -0.1879 | 0.0531 | - 3.57 | 0.827 |
| Hispanic | -0.2947 | 0.1468 | - 2.01 | 0.745 |
| Renal Failure | -0.0429 | 0.0515 | - 0.83 | 0.958 |
| Diabetes | -0.3971 | 0.0609 | - 6.52 | 0.672 |
| Hypertension | -0.3909 | 0.0492 | - 7.94 | 0.677 |
| Stroke | - 0.3889 | 0.1015 | - 3.83 | 0.688 |
| Chronic Obstructive Pulmonary Disease | -0.0082 | 0.0406 | - 0.20 | 0.992 |
| Congestive Heart Failure | -0.1332 | 0.0419 | - 3.18 | 0.876 |
| Intercept | -0.5972 |
NOTES: N = 13,759. Likelihood Ratio X2 = 232.21 with 10 Degrees of Freedom.
SOURCE: CY 2004 Medicare Discharge Data for LTCHs.
The overwhelming majority of ventilator patients in LTCHs were admitted from an inpatient hospital (Table 5). The most frequently occurring discharge status was in-hospital death. Patients discharged alive were most often discharged from LTCHs to skilled nursing facilities (Table 5). Other frequently occurring discharge destinations were to inpatient hospitals and home health. The differences observed between VAP and non-VAP patients do not appear to indicate a substantive difference in discharge patterns between groups.
Table 5. Admission Source, Discharge Destination, Length of Stay and Total Medicare Charges for LTCH Continuous Mechanical Ventilation Patients.
| Admission Source ** | ||||||
|---|---|---|---|---|---|---|
| Hospital | 2,954 | 87.6 | 8,732 | 84.1 | 11,686 | 85.0 |
| SNF | 5 | 0.2 | 38 | 0.4 | 43 | 0.3 |
| Physician Referral | 332 | 9.9 | 1,202 | 11.6 | 1,534 | 11.2 |
| Other | 80 | 2.3 | 416 | 3.9 | 496 | 3.5 |
| Discharge Destination ** | ||||||
| Died | 1,079 | 32.0 | 3,640 | 35.0 | 4,719 | 34.3 |
| SNF | 1,085 | 32.2 | 2,826 | 27.2 | 3,911 | 28.4 |
| Hospital | 425 | 12.6 | 1,559 | 15.0 | 1,984 | 14.4 |
| Home Health | 358 | 10.6 | 1,020 | 9.8 | 1,378 | 10.0 |
| IRF | 185 | 5.5 | 549 | 5.3 | 734 | 5.3 |
| Home | 73 | 2.2 | 307 | 3.0 | 380 | 2.8 |
| ICF/Medicaid | 62 | 1.8 | 185 | 1.8 | 247 | 1.8 |
| Hospice | 65 | 1.9 | 160 | 1.5 | 225 | 1.6 |
| Other Facility | 16 | 0.5 | 76 | 0.7 | 92 | 0.7 |
| LTCH | 19 | 0.6 | 56 | 0.5 | 75 | 0.5 |
| Other | 4 | 0.1 | 10 | 0.1 | 14 | 0.1 |
| Length of Stay (Days) | 46.5 | 43.8 | 44.4 | T=9.24 | ||
| Total Charges | $194,957 | $179,481 | $183,273 | T=4.39 | ||
NOTES:
= Chi Square not significant at .05 level.
= Chi Square significant at .05 level.
= Chi Square significant at .01 level or greater.
SOURCE: CY 2004 Medicare Discharge Data for LTCHs.
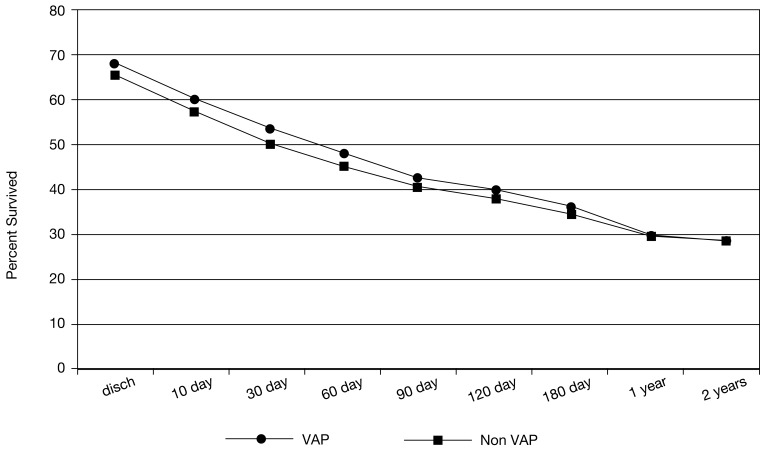
Ventilator patients with VAP had approximately similar rates of unadjusted postdischarge survival to ventilator patients without VAP over a 2-year period (Figure 1). Any differences between these two groups narrowed as time from discharge increased. The 2-year period was chosen to allow for more than 1 year post-discharge. It is striking that the “half-life” of LTCH ventilator patients occurs between 30 and 60 days post-discharge. A proportional hazards model for survival at 2 years post discharge showed that VAP was not significantly associated with increased mortality after demographic factors and presence of comorbidities are controlled for (Table 6). In this model, the effects of increasing age, race (Black), and presence of renal failure, or congestive heart failure (CHF) had a greater effect on increased mortality rates than presence of VAP. Females, and patients with diabetes or stroke comorbidities also had a below average risk of mortality.
Figure 1. Post-Discharge Survival for LTCH Continuous Mechanical Ventilation Patients.
Table 6. Proportional Hazards Two Year Post-Discharge Mortality Model.
| Predictors | Coefficient | Standard Error | T | Odds Ratio |
|---|---|---|---|---|
| Age | 0.0251 | 0.0010 | 25.25 | 1.025 |
| Female | -0.0962 | 0.0205 | -4.69 | 0.908 |
| Black | 0.1955 | 0.0250 | 7.81 | 1.216 |
| Hispanic | 0.1461 | 0.0664 | 2.20 | 1.157 |
| VAP | -0.0280 | 0.0237 | -1.18 | 0.972 |
| Renal Failure | 0.3172 | 0.0247 | 12.84 | 1.373 |
| Diabetes | -0.0746 | 0.0287 | -2.60 | 0.928 |
| Hypertension | 0.0332 | 0.0233 | 1.42 | 1.034 |
| Stroke | -0.1396 | 0.0476 | -2.93 | 0.870 |
| Chronic Obstructive Pulmonary Disease | 0.0481 | 0.0205 | 2.35 | 1.049 |
| Congestive Heart Failure | 0.1284 | 0.0208 | 6.18 | 1.137 |
NOTES: N = 13,759. Likelihood Ratio X2 = 1,082.25 with 11 Degrees of Freedom.
SOURCE: CY 2004 Medicare Discharge Data for LTCHs.
As indicated in Table 5, LOS and total Medicare charges were both higher for VAP patients than for other ventilator patients. The linear models predicting LOS and total Medicare charges (Tables 7 and 8) each indicate that presence of VAP is a major significant factor associated with longer stay lengths and higher total Medicare charges. Table 7 indicates that the most important predictor of LOS was in-hospital death (introduced as a control for differences in group death rates). Age, sex, and race/ethnicity were not significant predictors. Renal failure and congestive heart failure increased LOS while hypertension, stroke and COPD decreased LOS.
Table 7. Effects of VAP and other Comorbidities on Length of Stay.
| Predictors | Coefficient | Standard Error | T |
|---|---|---|---|
| Age | -0.0097 | 0.0297 | -0.32 |
| Female | 0.2310 | 0.6610 | 0.35 |
| Black | 1.2648 | 0.8333 | 1.52 |
| Hispanic | 2.4658 | 2.2230 | 1.11 |
| VAP | 2.1767 | 0.7663 | 2.84 |
| Renal Failure | 2.9992 | 0.8473 | 3.54 |
| Diabetes | -2.1748 | 0.9079 | -2.40 |
| Hypertension | -2.8904 | 0.7587 | -3.81 |
| Stroke | -2.8451 | 1.4931 | -1.91 |
| Chronic Obstructive Pulmonary | -0.4263 | 0.6647 | -0.64 |
| Disease | |||
| Congestive Heart Failure | 1.4953 | 0.6819 | 2.19 |
| Died in Hospital | -7.5987 | 0.7088 | -10.72 |
| Intercept | 46.8599 |
NOTES: N = 13,759, R2 = 0.012, F= 14.06 with (12, 13,746) Degrees of Freedom.
SOURCE: CY 2004 Medicare Discharge Data for LTCHs.
Table 8. Effects of VAP and other Comorbidities on Total Medicare Charges.
| Predictors | Coefficient | Standard Error | T |
|---|---|---|---|
| Age | -94.28 | 137.3 | -0.69 |
| Female | 720.14 | 3,052.2 | 0.24 |
| Black | 11,263.00 | 3,847.9 | 2.93 |
| Hispanic | 36,659.00 | 10,265.0 | 3.57 |
| VAP | 15,004.00 | 3,538.4 | 4.24 |
| Renal Failure | 27,276.00 | 3,912.7 | 6.97 |
| Diabetes | -20,393.00 | 4,192.6 | -4.86 |
| Hypertension | -818.46 | 3,503.3 | -0.23 |
| Stroke | -30,340.00 | 6.894.9 | -4.40 |
| Chronic Obstructive Pulmonary | -2,403.22 | 3,069.7 | -0.78 |
| Disease | |||
| Congestive Heart Failure | 12,344.00 | 3,148.6 | 3.92 |
| Died in Hospital | 4,041.20 | 3,273.0 | 1.23 |
| Intercept | 176,976.0 |
NOTES: N = 13,759, R2 = 0.012, F= 13.94 with (12, 13,746) Degrees of Freedom.
SOURCE: CY 2004 Medicare Discharge Data for LTCHs.
Table 8 indicates that age, sex and in-hospital death had no effect on total Medicare charges. Blacks and Hispanics have higher total Medicare charges independent of presence of VAP. Here as well, presence of comorbidities had mixed effects on total Medicare charges. Renal failure and congestive heart failure increased total charges while hypertension, stroke and COPD decreased total charges. After demographics, in-hospital death and comorbidities are controlled for VAP contributed a significant increase in total charges indicating the economic impact of this avoidable hospital-acquired complication of care.
Discussion
Ventilator patients in LTCHs with VAP have longer LOS and total Medicare charges than ventilator patients without VAP. This finding is consistent with the excess resource consumption and billed charges found in previous studies among short stay inpatients with VAP (Rello et al., 2002) and among LTCH patients (Walkey et al., 2009) and suggests that some amount of VAP is preventable with appropriate intervention. However, LTCH patients with VAP do not appear to be clearly a “sicker” group of patients in terms of greater mortality and comorbidity. The increased cost and LOS for VAP patients is, thus, not linked to these factors. The results observed may possibly reflect patient intake patterns at LTCHs but the more likely explanation is acquiring VAP is a distinct process not directly linked to determinants of mortality or to patient complexity. The results suggest that there is room to improve practices to control VAP and other hospital acquired infections in LTCHs.
The data indicate that LTCHs have an incidence rate of VAP that is similar to that found in general inpatient hospitals and home care settings (Chenoweth et al., 2007). Overall, the results are consistent with the findings of Kollef et al. (1995), Bregeon et al. (2001) and Rello et al. (2002) among general acute care hospital patients.
The data in Table 2 indicate that VAP incidence is not associated with age. There were no indication that incidence patterns differed between aged (65 and over) and disabled (less than 65) beneficiaries. The comorbidity indicators examined in Table 3 suggest that ventilator patients acquiring VAP in LTCHs are no more comorbid than ventilator patients that do not have VAP. Thus, ventilator patients with VAP in LTCHs do not appear to be significantly more frail or infirm than ventilator patients without VAP. Indeed both patient groups are very sick. One is concerned that possibly less comorbid patients do not receive the same level of attention as more comorbid patients thus leaving the former group more vulnerable to VAP and other hospital acquired infections.
Patients with VAP have approximately similar in-LTCH mortality rates and postdischarge mortality rates to patients without VAP. The low rate of survival shown in Figure 1 is similar to the survival/mortality patterns found in prior studies of survival rates in inpatient and special care ventilator units (Stoller et al., 2003). The results found in this analysis do not contradict observations about the frequency and clinical importance of VAP as a cause of death. Among ventilator patients in LTCHs the non-VAP reference group is sicker and has higher mortality than reference groups in the general acute care population or other settings.
One should be concerned about the high rate of VAP among Medicare LTCH ventilator patients and that a substantial portion of their excess LOS and Medicare charges may be avoidable through improved management of ventilator patients and improved quality of care. Kollef (1999) presents several strategies to prevent VAP and other hospital acquired infections in clinical settings. Care bundles for mechanical ventilation patients employ several of the intervention strategies for control of nosocomial infections. Examples of these are development of a formal infection control program, tube removal as soon as clinically feasible, adequate nutritional support and avoidance of reintubation (Kollef, 1999). Since effective control of hospital acquired infection requires multifaceted intervention to be effective, care bundles employ these interventions in a coordinated manner, are used to facilitate the consistent delivery of selected interventions for ventilator patients, and have been implemented in several ICU settings. Several recent studies indicate that the use of ventilator care bundles shows promise for lowering rates of VAP in ICUs (Resar et al., 2005; Wip and Napolitano, 2009; Walkey et al., 2009). Relatedly, protocol-driven weaning approaches appear to reduce VAP rates in ICU settings (Dries et al., 2005).
Although the Medicare, Medicaid, and SCHIP Extension Act (MMSEA) of 2007 required LTCHs to have an ongoing patient review process to assess a patients continuing need for care in an LTCH, CMS currently does not require LTCHs to report information about the care of patients they treat and quality of care to the extent that such information is required of skilled nursing facilities, inpatient rehabilitation providers and home health providers. Capturing more specific information on ventilator patients and use of procedures included in ventilator care bundles appears to be a possible first step toward improving VAP control in LTCHs.
Footnotes
The author is with the Centers for Medicare & Medicaid Services (CMS). The statements expressed in this article are those of the author and do not necessarily reflect the views or policies of CMS.
Reprint Requests: William Buczko, Ph.D., Centers for Medicare & Medicaid Services, ORDI, Mail Stop C3-19-07, 7500 Security Blvd, Baltimore, MD 21244-1850. E-mail WBuczko@cms.hhs.gov
References
- Bregeon F, Ciais V, Carret V, et al. Is Ventilator-associated Pneumonia an Independent Risk Factor for Death? Anesthesiology. 2001;94(4):551–553. doi: 10.1097/00000542-200104000-00005. [DOI] [PubMed] [Google Scholar]
- Chenoweth C, Washer L, Obeyesekera K, et al. Ventilator-associated Pneumonia in the Home Care Setting. Infection Control in Hospital Epidemiology. 2007;28(8):910–915. doi: 10.1086/519179. [DOI] [PubMed] [Google Scholar]
- Chastre J, Fagon JY. Ventilator-associated Pneumonia. American Journal of Respiratory and Critical Care Medicine. 2002;165:867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- Dries D, McGonigal M, Malian M, et al. Protocol-driven Ventilator Weaning Reduces Use of Mechanical Ventilation, Rate of Early Intubation and Ventilator-associated Pneumonia. Journal of Trauma. 2005;56(5):943–951. doi: 10.1097/01.ta.0000124462.61495.45. [DOI] [PubMed] [Google Scholar]
- Hugonnet S, Uckay I, Pittet D. Staffing Level: A Determinant of Late-onset Ventilator-associated Pneumonia. Critical Care. 2007;11:R80. doi: 10.1186/cc5974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollef M. The Prevention of Ventilator-associated Pneumonia. The New England Journal of Medicine. 1999;340(8):627–634. doi: 10.1056/NEJM199902253400807. [DOI] [PubMed] [Google Scholar]
- Kollef M. What Is Ventilator-associated Pneumonia and Why Is It Important. Respiratory Care. 2005;50(6):714–724. [PubMed] [Google Scholar]
- Kollef M, Silver P, Murphy D, et al. The Effect of Late-onset Ventilator-associated Pneumonia in Determining Patient Mortality. Chest. 1995;108(6):1655–1662. doi: 10.1378/chest.108.6.1655. [DOI] [PubMed] [Google Scholar]
- Liu K, Baseggio C, Wissoker D, et al. Long-term Care Hospitals Under Medicare: Facility Level Characteristics. Health Care Financing Review. 2001 Winter;23(2):1–18. [PMC free article] [PubMed] [Google Scholar]
- Rello J, Ollendorf D, Oster G, et al. Epidemiology and Outcomes of Ventilator-associated Pneumonia in a Large US Database. Chest. 2002;122(6):2115–2121. doi: 10.1378/chest.122.6.2115. [DOI] [PubMed] [Google Scholar]
- Resar R, Pronovost P, Haraden C, et al. Using a Bundle Approach to Improve Ventilator Care Processes and Reduce Ventilator-associated Pneumonia. Joint Commission Journal of Quality and Patient Safety. 2005;31(5):243–248. doi: 10.1016/s1553-7250(05)31031-2. [DOI] [PubMed] [Google Scholar]
- Safdar N, Dezfulian C, Collard H, et al. Clinical and Economic Consequences of Ventilator-associated Pneumonia: A Systematic Review. Critical Care Medicine. 2005;33(10):2184–2193. doi: 10.1097/01.ccm.0000181731.53912.d9. [DOI] [PubMed] [Google Scholar]
- Scheinhorn D, Hassenpflug M, Votto J, et al. Post-ICU Mechanical Ventilation at 23 Long-Term Care Hospitals: A Multicenter Outcome Study. Chest. 2007;2007(131):85–93. doi: 10.1378/chest.06-1081. [DOI] [PubMed] [Google Scholar]
- Stoller J, Xu M, Mascha E, et al. Long-term Outcomes for Patients Discharged From a Long-term Hospital-based Weaning Unit. Chest. 2003;124(5):1892–1899. doi: 10.1378/chest.124.5.1892. [DOI] [PubMed] [Google Scholar]
- Walkey A, Reardon C, Sulis C, et al. Epidemiology of Ventilator-associated Pneumonia in a Long-term Acute Care Hospital. Infection Control in Hospital Epidemiology. 2009;30(4):319–324. doi: 10.1086/596103. [DOI] [PubMed] [Google Scholar]
- Wip C, Napolitano L. Bundles to Prevent Ventilator-associated Pneumonia: How Valuable Are They? Current Opinion in Infectious Disease. 2009;22(2):159–166. doi: 10.1097/QCO.0b013e3283295e7b. [DOI] [PubMed] [Google Scholar]