Abstract
The development of iliac screws has provided a markedly easier way for spino-pelvic instrumentation than the classical Galveston technique. However, high rates of iliac screw loosening and breakage are usually reported, especially in cases where bilateral single iliac screws are used. Therefore, there is a need for exploring more stable iliac fixation techniques. Thus, the objective of this study was to compare the biomechanical effects of bilateral single and dual iliac screws on the stability of L3-iliac fixation construct under total sacrectomy condition. In this study, L2-pelvic specimens were harvested from seven fresh human cadavers. After biomechanically testing the intact state simulated by L3-L5 pedicle screw fixation, destabilization was introduced by total sacrectomy. Upon destabilization, L3-iliac screw-rod reconstructions were performed by four different techniques as follows: (1) bilateral single short iliac screws (Single-Short); (2) bilateral single long iliac screws (Single-Long); (3) bilateral dual short iliac screws, placed in the upper and lower iliac columns (Dual-UL); and (4) bilateral dual short iliac screws, all placed in the lower iliac column (Dual-Lower). These four iliac screw fixation techniques were sequentially preformed in the same specimen, and the lengths of the short and long iliac screws were 70 and 130 mm, respectively. Biomechanical testing was performed on a material testing machine under 800 N compression and 7 Nm torsion loading modes to evaluate the construct stiffness. In compression, the stiffness of the L3-iliac fixation constructs of Single-Short, Single-Long, Dual-UL, and Dual-Lower techniques were 73, 76, 98, and 108% of the intact state, respectively. No significant differences were detected between Single-Short and Single-Long (P = 0.589) techniques. However, the compressive stiffness of these two techniques was significantly lower than the intact state, and the Dual-UL and Dual-Lower techniques (P < 0.05). There was no statistical difference between the intact condition and the Dual-Lower technique (P = 0.109). Interestingly, Dual-Lower exhibited notably higher compressive stiffness than Dual-UL (+10.3%, P = 0.049). In torsion, the stiffness of Single-Short, Single-Long, Dual-UL, and Dual-Lower techniques were 72, 79, 105, and 109% of the intact condition, respectively. No significant differences were detected between Single-Short and Single-Long techniques (P = 0.338), and also among Dual-UL, Dual-lower techniques, and the intact state (P > 0.05). However, Single-Short and Single-Long techniques provided markedly lower construct torsional stiffness than the other three groups (P < 0.05). For lumbo-illiac reconstruction after total sacrectomy, even the use of bilateral single, long iliac screws do not help in restoring the local stability to the intact condition. However, dual iliac screws provide much higher construct stability than single iliac screw techniques. Therefore, dual iliac screw technique should be preferred for treating the unstable situation caused by total sacrectomy.
Keywords: Sacral tumor, Sacrectomy, Lumbo-iliac fixation, Iliac screw, Biomechanics
Introduction
Iliac screw technique is a common technique adopted in treating certain typical conditions requiring long segment fixation such as in the correction of neuromuscular and adult scoliosis, reduction of high-grade spondylolisthesis, sacral fractures, and surgical treatment of sacral tumors requiring sacrectomy [1–8]. Although iliac screw fixation provides a solid foundation to restore spinal balance and to stabilize the lumbosacral junction, high rate of implant failure including screw loosening and breakage has also been reported, especially in patients with bilateral single iliac screw fixation [2, 3, 5, 8]. Moreover, complications of the distal instrumentation are often considered to be relative to lumbosacral nonunion and low back pain [3]. Therefore, increasing the iliac fixation strength remains an important clinical issue.
Anatomic and radiographic studies have confirmed that there are two columns in the upper and lower areas of the ilium where the cancellous bone is found in abundance [6, 9–12]. The upper iliac column stands from the posterior superior iliac spine (PSIS) to the highest portion of the iliac crest; the lower column is located in the area from PSIS to the anterior inferior iliac spine (AIIS). These two columns contain a linear bony area which can provide sufficient anchoring for the placement of iliac screws [6, 9–12]. Importantly, at the level of great sciatic notch (GSN) of the lower iliac column, there is a narrow, cortex-rich point which can provide a rigid purchase for the iliac screws [9, 12]. Miller et al. [11] have reported a high rate of penetration (25%) of the iliac screws into the ilium and acetabulum during insertion from PSIS to AIIS, especially when the screw insertion depth exceeds 100 mm. Therefore, the use of iliac screws of length ranging from 70 mm (exceeding the level of GSN) to 90 mm has become a clinical consensus [1, 11].
Compared with the Galveston technique, iliac screw fixation technique can provide easier manipulation along with higher fixation strength [1, 13]. Biomechanical studies have further confirmed that increasing the length or diameter of the iliac screws can significantly enhance the iliac fixation strength [12, 14]. However, Zheng et al. [12], when investigating the effect of iliac screw insertion depth on the stability of lumbo-iliac fixation constructs in a total sacrectomy model, found that regardless of whether long or short, the use of single iliac screws restored about 60% of the stability of the local initial condition. Moreover, such an extent of the construct stability is comparable only with the destabilization condition of under-1/2 S1 partial sacrectomy combined with one side sacroiliac joint resection in Yu et al.’s biomechanical study [15]. Therefore, biomechanical limitations still exist when using bilateral single iliac screws to restore the local stability in the scenario of total sacrectomy.
To improve the lumbo-iliac fixation strength, some clinical studies have proposed the use of bilateral dual iliac screw techniques for total sacrectomy in removal of sacral tumors [3, 4, 6, 7]. Fujibayashi et al. [7] proposed a dual iliac screw technique in which the double screws were all placed in the lower iliac column; whereas, Acharya et al. [6] preferred insertion of dual iliac screws both in the upper and lower columns. However, the difference in biomechanical function between the use of dual and single iliac screws in lumbo-iliac fixation construct still remains unclear. Therefore, this study aimed at comparing the biomechanical effects of the bilateral single and dual iliac screws on the stability of lumbo-iliac fixation constructs, and determining which iliac screw fixation technique should be applied in the unstable scenario of total sacrectomy.
Materials and methods
Specimen preparation
Seven, fresh, adult cadavers (four males and three females) in an age range of 31–69 years (average age = 53.6 years) were used in this study. The medical history of each cadaver was inspected and their radiographies were used to exclude cadavers that showed metastatic or primary neoplastic bone lesions or evidence of any other gross abnormalities. For each cadaver, the bone mineral density (BMD) was evaluated at L1-L4 by CT scan (DEXA®; Densiscan 1000, Scanco Medical, Switzerland) with a slice thickness of 2 mm [15]. L2-pelves were harvested from the cadavers and stored in double-layered plastic bags at −20°C. Before the experiment, the specimens were thawed for 24 h at room temperature, followed by careful removal of the residual musculature leaving the spinal ligaments, osseous, and articular structures intact.
Biomechanical testing
Several screws were inserted at the cranial (L2 and partial L3 vertebrae) and caudal (both sides of ischiadic tuberosity) sites of the specimens and the sides were potted in steel cubic containers filled with polyester resin for embedding. During embedding, the specimen was positioned in such a way that the L3-L4 interbody space was horizontal to the testing table. Upon setting of the resin, the upper and lower polyester resin cubes were firmly fixed to the grips of an MTS machine (MTS 858 Bionix; MTS System Inc, Minneapolis, MN) using 4-point compression screws (Fig. 1). This setting made the axis of rotation centered at the middle-column of the S1 [12, 15]. Pedicle screw fixation (6.5 mm diameter and 45 mm length) was performed at the L3-L5 level using a posterior spino-pelvic fixation system made of titanium (Medtronic-WeiGao Inc., Wei-Hai, China), leaving the L5-S1 segments and the sacroiliac joints move freely. This instrumented condition was defined as the lumbo-iliac intact state in this experimental study. Nondestructive biomechanical testing was first performed on the intact condition to evaluate the initial stability of the lumbo-ilium which included compression (0 to −800 N) and bilateral axial rotation (−7 to +7 Nm with 100 N compressive preload). These maximum loading levels were decided for this study based on previous in vitro studies [12, 15]. Each testing mode was repeated for five cycles at a rate of 0.5 Hz, the data from the fourth cycle of the compression and torsion tests were used for biomechanical analysis. The linear and angular range of motion (ROM) of the fixation constructs were measured by transducers in the MTS machine. The same biomechanical testing protocol was repeated on the specimens after each reconstruction. While conducting the experiments, a saline humidifier was used to keep the specimens moist. The testing of each specimen was completed within 4 h after thawing.
Fig. 1.
Photograph of the experimental setup. The cranial and caudal sites of the specimen were mounted in polyester resin, by which the specimen was firmly clamped between the upper and lower grips of the MTS machine; insertion of the screws for reconstruction and the biomechanical testing were performed under the displacement control mode of the MTS machine
Four iliac screw techniques in the L3-iliac fixation construct
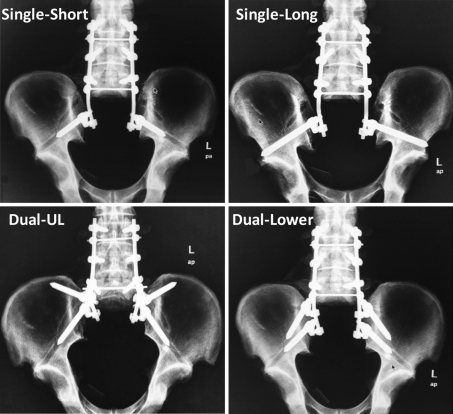
After the intact analysis, the lumbo-iliac destabilization by total sacrectomy combined with the L3-iliac fixation was conducted using four different iliac screw techniques on the same specimen as follows: (1) bilateral single short iliac screws (Single-Short); (2) bilateral single long iliac screws (Single-Long); (3) bilateral dual short iliac screws, each placed in the upper and lower iliac columns (Dual-UL); and (4) bilateral dual short iliac screws, all placed in the lower iliac column (Dual-Lower) (Fig. 2).
Fig. 2.
X-ray images showing the four iliac screw techniques used for lumbo-iliac fixation after total sacrectomy in this study. Single-Short bilateral single short iliac screws, Single-Long bilateral single long iliac screws, Dual-UL bilateral dual short iliac screws (each placed in the upper and lower iliac columns), Dual-Lower bilateral dual short iliac screws (all placed in the lower iliac column)
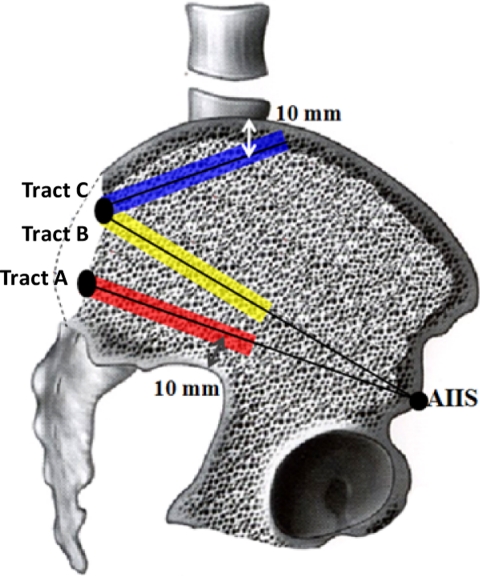
A trapezoid-shaped tricortical iliac bone block of size 30 × 20 mm was cut around the center of PSIS [6]. This osteotomy made the bottom of the residual cancellous bone area reach the surface of sacral ala. The two centers in the superior and inferior portions following the osteotomy were identified as the screw entry points [6, 7]. From the two entry points, three types of iliac screw tracts were made as follows. (1) Tract A: passage from inferior entry point of PSIS to AIIS; (2) Tract B: starting from the superior entry point of PSIS towards AIIS; and (3) Tract C: passage from the superior entry point directing to the point 10 mm below the highest portion of iliac crest (Fig. 3). A straight surgical probe was inserted between the inner and outer cortical walls of the ilium along the tract direction and a ball-tip feeler was used to identify the hole without breaking the inner and outer iliac cortices. Then the hole was tapped using a 7.0 mm tap. Iliac screws of 7.5 mm diameter were used in the present study; the lengths of the short and long iliac screws were 70 and 130 mm, respectively [12]. The tracts and screw lengths applied in the four different iliac screw fixation techniques are as follows: the iliac screw of Single-Short or Single-Long was placed into Tract A; in the Dual-UL technique, iliac screws were inserted into the Tract A and C each; and in the Dual-Lower technique, iliac screws were placed into the Tract A and B each. Visual inspection and radiographic evaluation were employed to confirm the correct placement of the screws. Two 6.35-mm diameter pre-bent rods were used in combination with the pedicle and iliac screws. In all the testing groups, cross-links were set at the L3-L4 and L5-S1 levels to connect the two longitudinal rods [4, 6, 7]. Total sacrectomy was performed following the first establishment of the lumbo-iliac fixation with iliac screw. In this procedure, the inter-osseous ligaments, dorsal ligaments of sacroiliac joints, and the anterior ligaments were removed. Thereafter, a surgical T-saw was used to cut the L5-S1 disc and the two sacroiliac joints leaving the bilateral iliolumbar ligaments intact [12].
Fig. 3.
Sketch showing the three tracts used for iliac screw insertion in this study. Tract A (red color): the passage from the inferior insertion point of PSIS to AIIS; Tract B (yellow color): the passage from the superior entry site of PSIS towards AIIS; Tract C (blue color): the passage from the superior entry point directing to the point of 10 mm below the highest portion of the iliac crest
In this study, the reconstruction and destabilization were carried out by a senior spine surgeon under displacement control mode of the MTS testing machine. A random generator was applied to decide the implanting orders of the four iliac screw techniques in each specimen. All the screw-rod junctions were tightened using a torque wrench with 60 inch-pounds of torque.
Data analysis
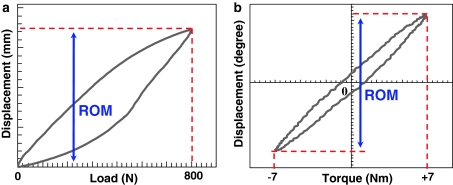
Two typical load–displacement curves were drawn using the data of the fourth loading cycle of each specimen. The maximal compressive and rotational angular displacements between the peak and trough points of the curves were obtained (Fig. 4). The compressive and torsional stiffness of fixation construct were calculated by the following formulas:
 |
1 |
 |
2 |
Fig. 4.
Two representative load–displacement curves plotted using the data from the 4th loading cycle. The range of motion (ROM) was defined as the linear (a) or angular (b) displacement under the maximum load
In this study, the construct stiffness was normalized to the intact condition of the same specimen to eliminate inter-specimen variations [12, 15]. Statistical analyses were performed with SPSS software (version 11.5, Chicago, IL, USA). One-way ANOVA and post hoc LSD test were used for statistical analysis of the data at a significance level of P < 0.05.
Results
The average BMD value of the 7 specimens was 1.07 g/cm2 ranging from 0.83 to 1.26 g/cm2. All the specimens had normal bones without osteoporosis [16]. No radiolucent ‘halo’ around the screws was observed in radiographs, and huge torque was still required for removing the iliac screws after each testing. The mean values and standard deviations of all the biomechanical parameters are summarized in Table 1.
Table 1.
Mean values and standard deviations of construct stiffness
| Groups | Compressive stiffness (%) | Torsional stiffness (%) |
|---|---|---|
| Intact | 100 ± 0 | 100 ± 0 |
| Single-Short | 73.1 ± 8.4 | 72.2 ± 11.4 |
| Single-Long | 75.7 ± 9.5 | 79.2 ± 13.2 |
| Dual-UL | 97.6 ± 6.9 | 104.9 ± 16 |
| Dual-Lower | 112.4 ± 10.2 | 109.1 ± 18.2 |
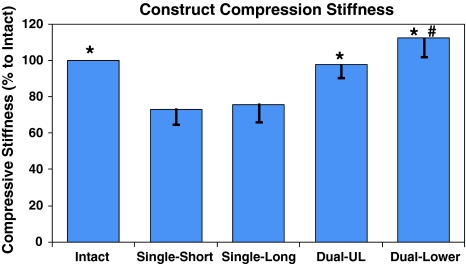
Compressive stiffness of L3-iliac fixation construct
Statistical differences were detected among the five groups under compressive loading condition (F = 21.88; P = 0.001) (Fig. 5). The mean compressive stiffness of the intact condition of the specimens was 392.25 ± 119.5 N/mm. The compressive stiffness of the reconstructed specimens by Single-Short, Single-Long, Dual-UL, and Dual-Lower techniques were 73, 76, 98, and 108% of the intact condition, respectively. No significant differences were demonstrated between Single-Short and Single-Long specimens (P = 0.589). However, these two reconstructions exhibited significantly lower compressive stiffness than the intact condition, and Dual-UL and Dual-Lower specimens (P < 0.05). No significant difference was observed in the compressive stiffness between the intact state and Dual-UL (P = 0.109). Interestingly, the Dual-Lower technique provided significantly higher compressive stiffness than the Dual-UL technique (+10.3%, P = 0.049).
Fig. 5.
Histogram showing the mean values and standard deviations of compressive stiffness for the five types of lumbo-iliac constructs: Intact, Single-Short, Single-Long, Dual-UL, and Dual-Lower. *P < 0.05 in comparison with Single-Short and Single-Long; #P < 0.05 in comparison with Dual-UL
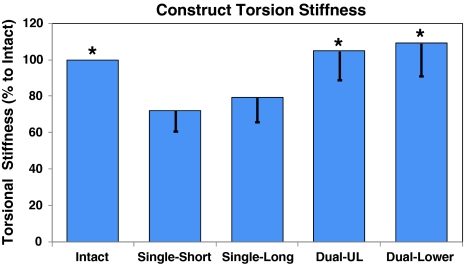
Torsional stiffness of L3-iliac fixation construct
Significant differences in torsional stiffness were demonstrated among the five groups (F = 10.53; P = 0.001) (Fig. 6). The mean torsional stiffness of the intact state was 2.8 ± 1.1 N/deg. The torsional stiffness of the Single-Short, Single-Long, Dual-UL, and Dual-Lower specimens were 72, 79, 105, and 109% of their intact states, respectively. No significant differences were detected between Single-Short and Single-Long (P = 0.338), as well as among Dual-UL and Dual-Lower specimens, and the intact condition (P > 0.05). However, the reconstructions of Single-Short and Single-Long techniques offered markedly lower torsional stiffness than the other three groups (P < 0.05).
Fig. 6.
Histogram showing the mean values and standard deviations of torsional stiffness for the five types of lumbo-iliac constructs: Intact, Single-Short, Single-Long, Dual-UL, and Dual-Lower. *P < 0.05 in comparison with Single-Short and Single-Long
Discussion
In this study, the superior and inferior iliac regions rich in cancellous bone were named as the upper and lower iliac columns, respectively, and were regarded as the important anchoring areas for iliac screw fixation [6, 9, 10]. Previous imaging and anatomical research have confirmed that the height and width of the lower column is sufficient for inserting two 8 mm diameter screws till the level of GSN [9, 12]. Moreover, in our pilot study, we evaluated the dimensions of the upper iliac column and identified that the zone from PSIS through the point of 10 mm below the highest portion of iliac crest is abundant in bone that can offer sufficient anchoring for the placement of iliac screws. Based on these data, in this study the screws of 7.5 mm diameter and 70 mm length were inserted successfully into Tract A, B, and C of all the 14 ilia without any malpositioning.
In this study, to evaluate the effectiveness of the four iliac screw techniques in restoring the stability of lumbo-iliac fixation construct, destabilization by total sacrectomy and L3-iliac fixation were performed similar to the clinical situation of surgical treatment for sacral tumor. Although total sacrectomy is usually followed by L4-iliac reconstruction in several clinical and in vitro biomechanical studies [4, 12], most clinical studies have advocated longer reconstruction similar to this study to enhance the immediate local stability and simplify the post-operative brace for total sacrectomy patients [4, 6–8].
This study was designed very carefully to accurately document the biomechanical differences between the four iliac screw techniques. Although human cadavers are ideal for performing in vitro biomechanical testing, cadaveric tissues possess variation in BMD, size, and age from specimen to specimen. Therefore, to minimize the inter-specimen variation in the current study, the biomechanical testing of the four different iliac screw techniques was conducted on the same specimen and the construct stiffness of each reconstruction was normalized to its intact condition for statistical analysis [12, 15]. In clinical scenario, there is a common consideration that replacement of a screw with another screw of same diameter will inevitably lead to an unstable condition. In order to minimize the errors generated due to the sequence of the testing protocol, the sequence of the four different iliac screw techniques were assigned in a random order for each specimen. Therefore, it can be assured that the difference in biomechanical stability between the testing groups is not biased due to the loosening of the screws. Furthermore, in this study, nondestructive testing was performed under only five cycles of 0 to −800 N compression and −7 to 7 Nm torsion loading modes which are at the low level of physiological loads [12, 15]. The bone mineral density of each specimen was also normal. Therefore, there is hardly any chance for loosening to have occurred even in the single short iliac screw technique. Moreover, radiolucent ‘halo’ around the screws was not observed in radiographs and huge torque was still required for removing the iliac screws after each testing.
However, the differences in the lumbosacral alignments of the seven specimens produced differences in setting and loading axis on the MTS testing machine. Moreover, although the biomechanical effects of the various iliac screw techniques on lumbo-iliac fixation constructs were evaluated, the stabilizing effects of the extrinsic stabilizers such as the neuromuscular system were not considered in this study. Furthermore, this in vitro study has only measured the early stabilities of the instrumented constructs, but their long-term biomechanical effects have not been evaluated. Therefore, considering these limitations, care has to be taken when using the data from this study as a guide for clinical practice.
In regard to the differences between the use of long and short iliac screws, Zheng et al. [12] have demonstrated that the use of long iliac screws (through PSIS-AIIS) can provide twofold higher fixation strength than short iliac screws (inserted till the level of GSN). However, in lumbo-iliac reconstruction after total sacrectomy, they observed no significant biomechanical advantages in the use of long screws over short iliac screws in terms of offering stability. In agreement, the current study also confirms that no significant difference of construct stiffness exist between these two single iliac screw techniques. Furthermore, the Single-Short and Single-Long could only regain 73 and 76% stiffness in compression and 72 and 79% stiffness in torsion of the intact condition, respectively. These findings revealed that enhancing the fixation strength of the single iliac screws cannot effectively increase the stability of lumbo-iliac fixation construct as a whole. Therefore, single iliac screw technique may not provide sufficient stability to the construct in unstable situations as caused by total sacrectomy.
This study has also discovered that both the dual iliac screw techniques offered significantly higher construct stiffness in terms of compression and torsion than the single iliac screw techniques. Moreover, the construct stability provided by Dual-UL and Dual-Lower was comparable with the stability of the intact conditions. Previous clinical studies on lumbo-iliac reconstruction performed on patients who underwent total sacrectomy for the treatment of sacral tumors have also reported such biomechanical advantages of using dual over single iliac screws [6–8]. Acharya et al. [6] applied dual iliac screw fixation (similar to Dual-UL) in four patients, and observed that no implant failure including iliac screw loosening or breakage occurred after 53 months of follow-up. Fujibayashi et al. [7] used dual iliac screws (all placed in lower iliac column, similar to Dual-Lower) in five patients and reported that after an average 28.4 months of follow-up, only one case with osteoporosis encountered iliac screw loosening. On the other hand, Mindea et al. [8] performed single iliac screw fixation in six patients and their follow-up results showed that two patients had complications due to iliac screw loosening and breakage within 1 year of follow up. Therefore, the use of dual iliac screw technique should be considered in treating severe unstable condition of the lumbosacral junction as caused by total sacrectomy.
Regarding torsion stiffness of the construct, no significant differences were observed between Dual-UL and Dual-Lower techniques, whereas in compressive loading condition the Dual-Lower technique regained significantly higher construct stiffness than Dual-UL. It is understandable that the lower iliac column serves as a “bridge” transmitting various stresses between the spine and the hip joint [9, 12], whereas the upper iliac column mainly offers the attachments for ligaments. These anatomic and biomechanical characteristics explain why the dual iliac screws placed in the lower iliac column alone (Dual-Lower) could acquire more anchorage strength. In terms of clinical practice, when compared with Dual-UL, Dual-Lower technique may decrease the exposure of the outer cortex and the difficulty in screw-rod connection. Therefore, Dual-Lower technique should be given priority when using dual iliac screw fixations.
Thus, the results of this study suggest that increasing the iliac screw anchoring points may be the key to improve the overall stability of the lumbo-iliac fixation construct. However, dual iliac screw technique increases the difficulty of screw-rod connection and medical cost in the clinical scenario. Moreover, single iliac screw technique is still commonly used in the lumbo-iliac reconstruction surgery [1, 2]. Therefore, further clinical and biomechanical studies are needed to determine which types of lumbosacral instabilities require single- and which ones require dual iliac screw fixation technique.
Conclusions
To sum up, as the use of the single long iliac screws is insufficient to restore the initial local stability and that the dual iliac screw techniques provide much higher construct stability than the single iliac screw techniques, the use of dual iliac screw techniques should be given preference in treating severe unstable situations as caused by total sacrectomy, and the key to improve the stability of the lumbo-iliac fixation construct is to increase the iliac screw anchoring points.
Acknowledgment
The authors would like to thank Medtronic-WeiGao Inc. for providing the posterior spinal fixation system. This study was supported by Guangdong Provincial Medical Research Foundation of China (A2008161 and 2008B050100012).
Contributor Information
Bin-Sheng Yu, Email: hpyubinsheng@hotmail.com.
William W. Lu, Email: wwlu@hku.hk
References
- 1.Moshirfar A, Rand FF, Sponseller PD. Pelvic fixation in spine surgery: historical overview, indications, biomechanical relevance, and current techniques. J Bone Joint Surg Am. 2005;87:S89–S106. doi: 10.2106/JBJS.E.00453. [DOI] [PubMed] [Google Scholar]
- 2.Emami A, Deviren V, Berven S, et al. Outcome and complications of long fusions in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine. 2002;27:776–786. doi: 10.1097/00007632-200204010-00017. [DOI] [PubMed] [Google Scholar]
- 3.Tsuchiya K, Bridwell KH, Kuklo TR, et al. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine. 2006;31:303–308. doi: 10.1097/01.brs.0000197193.81296.f1. [DOI] [PubMed] [Google Scholar]
- 4.Zhang HY, Thongtrangan I, Balabhadra RS, et al. Surgical techniques for total sacrectomy and spinopelvic reconstruction. Neurosurg Focus. 2003;15:E5. doi: 10.3171/foc.2003.15.2.5. [DOI] [PubMed] [Google Scholar]
- 5.Schildhauer TA, Bellabarba C, Nork SE, et al. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447–457. doi: 10.1097/00005131-200608000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Acharya NK, Bijukachhe B, Kumar RJ, et al. Ilio-lumbar fixation–the Amrita technique. J Spinal Disord Tech. 2008;21:493–499. doi: 10.1097/BSD.0b013e31815b5cc4. [DOI] [PubMed] [Google Scholar]
- 7.Fujibayashi S, Neo M, Nakamura T. Palliative dual iliac screw fixation for lumbosacral metastasis. technical note. J Neurosurg Spine. 2007;7:99–102. doi: 10.3171/SPI-07/07/099. [DOI] [PubMed] [Google Scholar]
- 8.Mindea SA, Salehi SA, Ganju A, et al. Lumbosacropelvic junction reconstruction resulting in early ambulation for patients with lumbosacral neoplasms or osteomyelitis. Neurosurg Focus. 2003;15:E6. doi: 10.3171/foc.2003.15.2.6. [DOI] [PubMed] [Google Scholar]
- 9.Berry LJ, Stahurski T, Asher MA. Morphometry of the supra sciatic notch intrailiac implant anchor passage. Spine. 2001;26:E143–E148. doi: 10.1097/00007632-200104010-00002. [DOI] [PubMed] [Google Scholar]
- 10.Schildhauer TA, McCulloch P, Chapman JR, et al. Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech. 2002;15:199–205. doi: 10.1097/00024720-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Miller F, Moseley C, Koreska J. Pelvic anatomy relative to lumbosacral instrumentation. J Spinal Disord. 1990;3:169–173. doi: 10.1097/00002517-199006000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Zheng ZM, Yu BS, Chen H, et al. Effect of iliac screw insertion depth on the stability and strength of lumbo-iliac fixation constructs: an anatomical and biomechanical study. Spine. 2009;34:E565–E572. doi: 10.1097/BRS.0b013e3181ac8fc4. [DOI] [PubMed] [Google Scholar]
- 13.Schwend RM, Sluyters R, Najdzionek J. The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine. 2003;28:542–547. doi: 10.1097/00007632-200303150-00006. [DOI] [PubMed] [Google Scholar]
- 14.Akesen B, Wu C, Mehbod AA, et al. Revision of loosened iliac screws: a biomechanical study of longer and bigger screws. Spine. 2008;33:1423–1428. doi: 10.1097/BRS.0b013e3181753c04. [DOI] [PubMed] [Google Scholar]
- 15.Yu BS, Zheng ZM, Zhuang XM, et al. Biomechanical effects of transverse partial sacrectomy on the sacroiliac joints: an in vitro human cadaveric investigation of the borderline of sacroiliac joint instability. Spine. 2009;34:1370–1375. doi: 10.1097/BRS.0b013e3181a3d440. [DOI] [PubMed] [Google Scholar]
- 16.Roig-Vilaseca D, Nolla JM, Roig-Escofet D. Suitability of the T-score for establishing bone mineral density categories. Osteoporos Int. 2000;11:408–410. doi: 10.1007/s001980070107. [DOI] [PubMed] [Google Scholar]