Abstract
Purpose
To provide recommendations and standard operating procedures for intensive care unit (ICU) and hospital preparations for an influenza pandemic or mass disaster with a specific focus on critical care triage.
Methods
Based on a literature review and expert opinion, a Delphi process was used to define the essential topics including critical care triage.
Results
Key recommendations include: (1) establish an Incident Management System with Emergency Executive Control Groups at facility, local, regional/state or national levels to exercise authority and direction over resources; (2) developing fair and equitable policies may require restricting ICU services to patients most likely to benefit; (3) usual treatments and standards of practice may be impossible to deliver; (4) ICU care and treatments may have to be withheld from patients likely to die even with ICU care and withdrawn after a trial in patients who do not improve or deteriorate; (5) triage criteria should be objective, ethical, transparent, applied equitably and be publically disclosed; (6) trigger triage protocols for pandemic influenza only when critical care resources across a broad geographic area are or will be overwhelmed despite all reasonable efforts to extend resources or obtain additional resources; (7) triage of patients for ICU should be based on those who are likely to benefit most or a ‘first come, first served’ basis; (8) a triage officer should apply inclusion and exclusion criteria to determine patient qualification for ICU admission.
Conclusions
Judicious planning and adoption of protocols for critical care triage are necessary to optimize outcomes during a pandemic.
Keywords: Critical care triage, Triage, Staff protection, Recommendations, Standard operating procedures, Intensive care unit, Hospital, H1N1, Influenza epidemic, Pandemic, Infection control, Disaster
Introduction
Purpose
Mass casualty events (MCE) such as outbreaks of influenza or other infectious diseases, natural disasters and man-made disasters generate many critically ill or injured patients, which can overwhelm health care resources [1]. In military operations, international and humanitarian laws dictate that triage should be used to address health care resource shortfalls [2, 3]. These principles have become widely used in civilian settings to guide the allocation and prioritization of limited resources following disasters [4–10]. In severe circumstances insufficient ICU bed availability may result in the occurrence of potentially avoidable deaths, which may be influenced by compulsory triaging decisions. Recently work has described the process for developing triage protocols for critical care [11], and draft protocols have been proposed [12–15] based on the probability that needs during a disaster will be greater than availability. Ideally triage plans should be developed at a national or regional level.
The purpose of this standard operating procedure (SOP) is to describe the rationale, components, implementation and infrastructure to support a critical care (tertiary) triage protocol to guide the allocation and prioritization of scarce critical care resources during a MCE.
Scope
This SOP applies to any hospital or health care setting with the ability to provide critical care services that are involved in the response to an influenza pandemic or MCE. Facilities should implement this SOP within the broader framework of their local, regional/state and national authorities.
Goals and objectives
Minimize the loss of life due to critical injuries or illness during a MCE.
Prioritize patient care and allocate resources in accordance with generally accepted ethical principles.
Provide a process and structure to mitigate chaos and improve the effectiveness of actions taken during the response to a MCE.
Institute appropriate checks and balances to ensure that critical care triage will not be applied inappropriately and accountability will be incorporated into the process.
Triage protocols and decision making should be transparent, open and publicly debated [14].
Definitions
Central Triage Committee (CTC)
a body of experts that has broad regional situational awareness (knowledge of the supply resources and demands on them), capacity to conduct research in order to develop then modify triage protocols and monitor triage outcomes. This group would be a group within the operations arm of the incident management system (IMS) and would provide advice to the incident manager at either the regional/state or national level.
Command and control
the exercise of authority and direction over resources utilizing an appropriate management system such as an incident management system (IMS) or an equivalent system.
Inclusion criteria
identify patients who may benefit from admission to critical care and primarily focus on respiratory failure, since the provision of ventilatory support is what fundamentally differentiates the ICU from other acute care areas (e.g., step-down units) [12] (Table 1).
Table 1. Inclusion criteria for admission to critical care during a MCE.
The patient must have one of the following from either category A or B
|
Exclusion criteria
identify patients who are not candidates for ICU admission including patients: (1) with a poor prognosis despite care in an ICU, (2) requiring resources that cannot be provided, (3) whose underlying illness has a poor prognosis with a high likelihood of death and (4) who are “too well” [12] (Table 2).
Table 2. Exclusion criteria from admission to critical care during a MCE.
The patient is excluded from admission to critical care if any of the following are present
|
| Inhalation injury |
|
| Requirement for home oxygen |
| 3. Liver |
| Child-Pugh score ≥7 |
| Total serum bilirubin |
| Bilirubin <2 mg/dl: 1 point |
| Bilirubin 2–3 mg/dl: 2 points |
| Bilirubin >3 mg/dl: 3 points |
| Serum albumin |
| Albumin >3.5 g/dl: 1 point |
| Albumin 2.8–3.5 g/dl: 2 points |
| Albumin <2.8 g/dl: 3 points |
| INR |
| INR <1.70: 1 point |
| INR 1.71–2.20: 2 points |
| INR >2.20: 3 points |
| Ascites |
| No ascites: 1 point |
| Ascites controlled medically: 2 points |
| Ascites poorly controlled: 3 points |
| Encephalopathy |
| No encephalopathy: 1 point |
| Encephalopathy controlled medically: 2 points |
| Encephalopathy poorly controlled: 3 points |
|
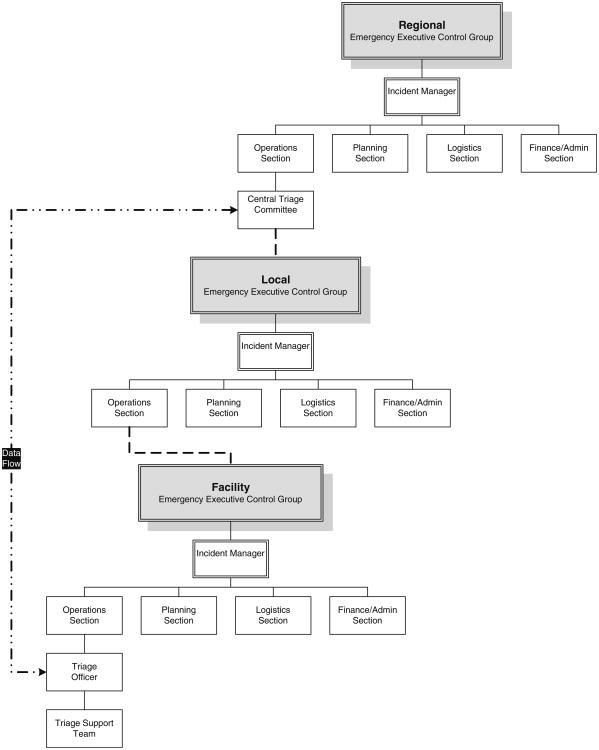
Incident management system (IMS)
employs standardized processes, protocols and procedures that all responders use to coordinate and conduct response actions. It includes a standard organizational structure with five functional areas: command, operations, planning, logistics and finance/administration [16]. The IMS structure contains Emergency Executive Control Groups at the facility, local, regional/state or national levels (Fig. 1).
Fig. 1.
The incident management system (IMS) structure. Dashed lines indicate the continuity of the lines of authority for triage from the CTC down through the IMS levels. Two-way communication should flow through this chain. This is not meant to indicate lines of command and control. The dash-dotted line indicates the direct data inputs that will flow between (bidirectional) the local triage officer and the CTC
Incident manager
implements the IMS at the facility, local, regional/state or national levels.
Mass casualty event (MCE)
an event generating a large number of victims but not exceeding the facility or community resources.
Minimum qualifications for survival (MQS)
represent a ceiling on the amount of resources that will be expended on any one patient [12].
Overtriage
allocating critical care resources to patients who do not medically require such specialized care.
Patient care team
the multidisciplinary team, usually organized under the leadership of a physician, responsible for direct care of the patient.
Primary triage
occurs in the pre-hospital field, is usually performed by paramedics and is based on very simple criteria that can be rapidly assessed [14].
Secondary triage
is typically performed by emergency physicians or surgeons immediately upon a patient's arrival at the hospital and prioritizes patients to treatment areas for initial interventions [14].
Sequential (formerly ‘Sepsis’) organ failure assessment (SOFA)
a critical care scoring system to determine the extent of a patient's organ dysfunction. The score is based on six different scores, one each for the respiratory, cardiovascular, hepatic, coagulation, renal and neurological systems [17, 18] (Table 3).
Table 3. Sequential (formerly ‘Sepsis’) organ failure assessment (SOFA) score.
| Variable | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| PaO2/FiO2, mmHg | >400 | 400 | 300 | 200 | 100 |
| Platelets, ×103/μl (×106/l) | >150 (>150) | 150 (150) | 100 (100) | 50 (50) | 20 (20) |
| Bilirubin, mg/dl (μmol/l) | <1.2 (<20) | 1.2–1.9 (20–32) | 2.0–5.9 (33–100) | 6.0–11.9 (101–203) | >12 (>203) |
| Hypotension | None | MABP <70 mmHg | Dop = 5 | Dop >5, Epi = 0.1, Norepi = 0.1 | Dop >15, Epi >0.1 Norepi > 0.1 |
| Glasgow Coma Score | 15 | 13–14 | 10–12 | 6–9 | <6 |
| Creatinine, mg/dl (μmol/l) | <1.2 (<106) | 1.2–1.9 (106–168) | 2.0–3.4 (169–300) | 3.5–4.9 (301–433) | >5 (>434) |
Doses in μg/kg/min, SI units in brackets
Adapted from [17]
Dop Dopamine, Epi epinephrine, Norepi norepinephrine
For the renal SOFA score, 4 points may be given for renal replacement therapy, which was not included in the original paper
Situational awareness
involves being aware of what is happening in the environment, understanding how information, events and one's own actions will impact on goals and objectives in both the present and the near future. With regard to triage, this deals specifically with being aware of both the supply of and demand on resources.
Critical care (tertiary) triage
is conducted by intensivists or surgeons in an influenza pandemic or mass casualty situation to prioritize patients for definitive care in either the intensive care unit (ICU) or operating room [14].
Triage officer
an intensivist or other physician/surgeon with appropriate critical care experience who applies the triage protocol to decide the disposition of critically ill and injured patients during a MCE.
Triage protocol
inclusion criteria, exclusion criteria and MQS combined with a prioritization tool (Table 4) used to assist the triage officer in allocating critical care resources during a MCE (Tables 1, 2, 4).
Table 4. Triage prioritization tool.
| Colour Code | Initial Assessment | 48 hour Assessment | 120 hour Assessment | Priority/Action |
|---|---|---|---|---|
| Blue | Exclusion Criteria or SOFA >11 | Exclusion Criteria Or SOFA > 11 Or SOFA 8 – 11 no Δ | Exclusion Criteria or SOFA > 11 or SOFA < 8 no Δ | Medical Mgmt +/- Palliate & d/c from critical care |
| Red | SOFA ≤ 7 or Single Organ Failure | SOFA score < 11 and decreasing | SOFA score < 11 and decreasing progressively | Highest |
| Yellow | SOFA 8 –11 | SOFA < 8 no Δ | SOFA < 8 with < 3 point decrease in past 72h | Intermediate |
| Green | No significant organ failure | No longer ventilator dependant | No longer ventilator dependant | Defer or d/c, reassess as needed |
Triage support team
a team of varying composition that may include allied health professionals and administrative staff who act to support the triage officer in the execution of his/her duties.
Undertriage
failure to allocate critical care resources to a patient who meets the inclusion and exclusion criteria as a result of failure to recognize the true severity of the patient's injuries or illness.
Basic assumptions
An incident management system is in place at the facility.
Response activities are being coordinated with neighboring/regional facilities.
The hospital has prepared for mass casualty events including stockpiling equipment, medications and basic supplies.
Restrictions in treatment should be proportional to the realized or expected shortfall in resources.
Developing fair and equitable policies for “the greatest good for the greatest number” of patients may require restricting ICU services to patients believed most likely to benefit.
Usual treatments and standards of practice normally given may be impossible to deliver. ICU care and treatments may have to be withheld from patients likely to die even with ICU care and withdrawn after a trial in patients who do not improve or who deteriorate [19].
Triage criteria should be objective, ethical, transparent, applied equitably and be publically disclosed.
The triage protocol should be based upon evidence and best practices, where possible.
Triage should only be initiated when critical care resources are or will be overwhelmed and all efforts to extend available resources or obtain additional resources have been instituted (Table 5) [14].
In an influenza pandemic, hospitals should expect the greatest surge of ICU patients approximately 4 to 6 weeks after the first confirmed winter ICU admission and substantial extra workload and resource use lasting several weeks [19–22].
Table 5. Conditions required to initiate a triage process to allocate scarce resources [14].
| Declared state of emergency or incident of national significance |
| Initiation of national disaster medical system and national mutual aid and resource management |
| Surge capacity fully employed within health care facility |
| Attempts at conservation, reutilization, adaptation and substitution are performed maximally |
| Identification of critically limited resources (ventilators, antibiotics) |
| Identification of limited infrastructure (isolation, staff, power) |
| Request for resources and infrastructure made to local and regional health officials |
| Current attempt at regional, state, and federal level for resource or infrastructure allocation |
Lines of authority
Adequate situational awareness is essential to undertaking ethical and successful triage [12, 14]. No individual institution can ever have a sufficient situational awareness to make decisions regarding the implementation of triage as the level of awareness required is across a broad geographic region. However, it is rare that any authority above the individual institution can have an accurate awareness of resources within the institution without some form of reporting from the institution (active or passive). Thus, cooperation and communication between various levels, which is supported by the required infrastructure, are essential for success [12].
A Central Triage Committee (CTC), integrated into the incident management structure, should exist prior to the MCE. The level of authority at which the CTC should exist depends upon geographic characteristics and political structures. The CTC should be situated within the authority responsible for a large geographic/population base in which mutual aid is feasible between health care facilities. In North America and Australia this would most commonly be the provincial or state level, whereas in Europe it would be the national or even international level.
Authority for conducting triage should flow from the CTC through the regional IMS structure, down to the local IMS structure, onto the facility IMS structure and ultimately to the triage officers functioning within the Operations section of an IMS. A bidirectional flow of information should move through this command chain. A schematic of the lines of authority is provided in Fig. 1.
Concepts of operations
Normal operations
under normal circumstances critical care triage protocols should not be utilized. Training and exercise of the triage protocol should occur.
Irregular operations
during irregular operations critical care triage protocols should not be utilized. The CTC should be notified and a situational analysis should be conducted to assess potential for deterioration. Depending upon the circumstances, triage officers should be put on alert. The CTC should monitor resource supply and demand status.
Emergency operations
during emergency operations, such as a MCE, the CTC should convene and a conduct a situational assessment. Triage officers should be put on stand-by and the triage system made ready. Triage protocols should only be triggered when it is evident that resource shortfalls are or will occur across a broad geographic area based upon current or predicted demands, despite all reasonable efforts to extend resources or obtain additional resources.
Once the decision to institute triage has been made, primary triage of patients should occur in the pre-hospital settings (field, physician's offices, community assessment centers, etc.) and secondary triage in emergency departments, both based upon protocols appropriate for their settings.
All critically ill patients requiring consideration for definitive ICU care should be assessed by a triage officer. The triage of patients for ICU remains controversial. Experts have recommended accepting patients likely to benefit most from ICU [23, 24] or a ‘first come, first served’ basis [25]. Each institution should determine its own triage criteria using senior clinicians in a transparent fashion. The triage officer should apply the inclusion and exclusion criteria together possibly with a prioritization tool (Tables 1, 2, 4 are one example) to determine qualification for ICU admission. The Table 4 prioritization tool utilizes the Sequential Organ Failure Assessment (SOFA) score [17, 18], which has limitations and has not yet been validated. Although SOFA day-1 scores have been shown in recent H1N1 patients to be significantly associated with 28-day and overall mortality [21, 26], little improvement in SOFA scores of influenza patients between admission and day 3 raises the question as to what specific interval for re-assessment is most appropriate for patients with influenza [27]. However, it is important to note that the triage protocol must apply to all critically ill patients with a variety of illnesses or injuries, and re-assessment at 48 h did show an ability to predict outcomes [17]. The SOFA score was not designed for use in disaster triage and has several limitations, including the need for laboratory investigations, inclusion of variables that can be influenced by clinician treatment decisions (i.e., use of vasopressors) rather then purely physiologic variables and variability in applying/interpreting the score (i.e., assessment of Glasgow Coma Scores). Findings of a recent pilot study suggest that the application of a SOFA-based critical care triage protocol could direct scarce resources to patients who are most likely to benefit from them and increase resource availability [28]. However, another study did not share this finding [29].
All ICU patients at the time of the MCE should also be assessed for eligibility based on the same criteria. Patients not meeting inclusion criteria for ICU admission remain on the ward. Patients can be re-evaluated by the triage officer/support team if their condition deteriorates for those not sick enough or improves for those excluded. Patients who are triaged as ‘red’ are given priority for the ICU followed by those triaged as ‘yellow.’ Patients categorized as ‘blue/black’ should remain on the ward and receive palliative care with or without active medical therapy at the discretion of the primary care team taking into consideration the patient and/or family preferences.
All patients receiving critical care at the time critical care triage is instituted should be assessed by the triage officer/support team utilizing the inclusion and exclusion criteria together possibly with the prioritization tool and will be categorized using the ‘initial assessment.’ Patients who do not meet the inclusion criteria for critical care should be transferred to the appropriate ward for management by the primary care team. Patients categorized as ‘red’ or ‘yellow’ should remain in critical care and be reassessed as described below. Patients categorized as ‘blue/black’ should be transitioned to palliative care and transferred to the appropriate ward under a primary care team.
Patients admitted to critical care should be reassessed by the triage officer/support team at 48 and 120 h (day 2 and 5) and re-categorized. An ICU trial with reappraisal at day 5 has proved useful in mechanically ventilated cancer patients [30].
Decisions regarding management of patients beyond day 5 of critical care will be dependent upon resource availability. Within the first 5 days of the emergency, the CTC should provide direction regarding treatment beyond day 5. Potential options include: daily reassessment and categorization according to the 120-h criteria for an unlimited period; daily reassessment and categorization according to the 120-h criteria for a limited time period; institution of alternative criteria; or transition to palliative care and transfer to the ward.
During the surge of critically ill patients, the possibility of transferring stable patients to other facilities may have to be considered [13].
As soon as resource availability permits, critical care triage should cease, and management should be provided initially according to altered standards of care and eventually normal standards of care. Cessation of triage may occur in a graduated fashion by altering the exclusion thresholds and prioritization criteria at the discretion of the CTC.
Functional roles and responsibilities of the internal personnel and interface agencies or sectors
Government/Emergency Management Authority (State/Regional and National Levels)
Establish a legislative/policy framework for emergency response (including critical care triage) and provide infrastructure to support triage. Appoint the CTC.
Central Triage Committee (CTC)
the body of experts at the regional level with local, regional and/or national situational awareness should have a mandate to develop triage protocols, train triage officers, help determine if critical care triage should be instituted during an MCE, monitor triage outcomes, monitor the MCE and advise on regional distribution or re-distribution of ICU resources, refine triage protocols and determine when to cease critical care triage.
Local Emergency Executive Control Group (local level)
Liaise with and facilitate flow of information between the Regional and Health Facilities IMS structures. Coordinate response among Health Facilities within their locality.
Health Facility Emergency Executive Control Group (hospital/facility level)
Through their incident manager, ensure that a triage officer or officers are appointed and provided with the support and resources necessary to conduct triage in accordance with protocols developed by the CTC. During normal operation ensure that appropriate training of triage officers and exercises occur.
Triage officer (hospital level)
Assess all patients referred for consideration of critical care and those admitted to the ICU to assign a level of priority for each patient according to the triage protocol. The triage officer should review necessary patient data by chart review and discussion with the clinical team if needed. The triage officer is not expected to examine patients, except under circumstances where this information may be crucial in reaching a triage decision. The triage officer has the ultimate responsibility and authority for making decisions as to which patients should receive the highest priority for receiving critical care and is empowered to make decisions regarding reallocation of critical care resources. He/she is expected to make decisions that benefit the greatest number of patients given potentially limited resources. The triage officer should share decisions with the attending clinician and document all assessments and decisions in the medical record (Table 6). The triage officer should provide information pertaining to all patients assessed and details of the triage decisions as requested by the CTC [14].
Table 6. Medical record documentation [14].
| In the event of an emergency mass critical care (EMCC) scenario, patient records should include specific notations highlighting the following |
| A state of declared emergency exists, and the emergency response system of the facility has been activated |
| All existing resources and surge capacity of the institution and the region have been overwhelmed and/or exhausted |
| No obvious resource capability is imminent, and a mass triage strategy has been instituted per hospital instruction that will result in rationing of care |
| A triage officer/team has made the assessment to withhold a resource and is acting in a nondiscretionary manner and with the approval of the regional incident commander and in concert with state emergency declarations and enacted legal protections |
| All existing medical modalities for supportive care and for alleviation of suffering will be instituted or continued |
| Internal records (by the triage committee) should include |
| All patients receiving critical care services for whom reallocation of critical care resources are seriously considered, whether those resources are reallocated or not. There should be an explanation and rationale for why patients who had their critical care resources reallocated were selected, compared with those who were not |
| All patients seeking critical care services who are not already receiving them, the priority ranking of these patients, and which patients ultimately are admitted to critical care |
Triage support team (hospital level)
Provide assistance and information to the triage officer to help facilitate and support execution of her/his duties.
Logistics support and requirements necessary for the effective implementation of the SOPs
Legislative or policy framework for triage
Central triage committee
Data collection system (linking front lines and CTC for situational awareness and to monitor triage outcomes)
Incident management system
Communication network (facilitate rapid communication between CTC and triage officers)
Triage protocols
Triage officers (with appropriate training)
Triage support team
Palliative care team/protocols
Commitment of the senior hospital administration
Maintenance of standard operating procedure
This SOP should be reviewed semi-annually, following exercises and post-MCEs to incorporate the latest evidence and lessons learned.
Recommended training and exercises activities
Every health facility that provides critical care will require triage officers. The number will depend upon the size of the hospital and number of critical care beds (Table 7). Training for triage officers and alternates should be standardized across a region and provided by the CTC. Training programmes should include the components outlined in Table 8. Training modules for members of the Triage Support Team should be developed by the CTC to provide ‘just in time’ training in the event of an MCE (see Chap. 9, Educational process).
Table 7. Number of triage officers and alternates.
| Number of critical care beds | Number of triage officers | Number of alternates |
|---|---|---|
| <20 | 2 | 2 |
| 20–40 | 4 | 3 |
| >40 | 6 | 4 |
Table 8. Components of triage officer training.
| Incident management system |
| Fundamentals of disaster management |
| History and evolution of triage |
| Principles of triage |
| Overtriage and undertriage implications |
| Triage ethics |
| Regional legislative and policy framework for triage |
| Regional triage protocols |
| Regional triage infrastructure |
| Central triage committee |
| Data collection system |
| Triage communication network |
| Documentation of triage decisions |
| Communication skills |
| Stress management |
| Psychological impact of conducting triage |
Awareness training regarding triage during MCEs should be included in the standard emergency training provided to all hospital clinical staff in critical and acute care areas as well as senior administrative staff.
Triage officers should participate in one full-scale exercise annually and one tabletop exercise (either manual or computer based) annually. The CTC should participate in at least one full-scale exercise in conjunction with at least two health facilities annually and two tabletop exercises annually. In addition, the CTC should use research and computer modeling to test and refine triage protocols during periods of normal operations.
Footnotes
Conflict of interest statement None.
The views expressed in the paper are those of the authors and do not reflect policies of the US Department of Health and Human Services or the National Institutes of Health or the Department of National Defence/Canadian Forces.
Contributor Information
Michael D. Christian, Division of Infectious Diseases and Critical Care, Department of National Defence, Canadian Forces and Department of Medicine, Mount Sinai Hospital, University of Toronto, Toronto, Canada
Gavin M. Joynt, Department of Anesthesia and Intensive Care, Prince of Wales Hospital, The Chinese University of Hong Kong, Sha Tin, Hong Kong, People's Republic of China
John L. Hick, Department of Emergency Medicine, Hennepin County Medical Center, Minneapolis, MN, USA
John Colvin, Department of Anaesthesiology, Ninewells Hospital, Dundee, Scotland, UK.
Marion Danis, Department of Bioethics, Clinical Center of the National Institutes of Health, Bethesda, MD, USA.
Charles L. Sprung, Email: charles.sprung@ekmd.huji.ac.il, Department of Anesthesiology and Critical Care Medicine, Hadassah Hebrew University Medical Center, Jerusalem, Israel.
References
- 1.Christian MD, Devereaux AV, Dichter JR, Geiling JA, Rubinson L. Definitive care for the critically ill during a disaster: current capabilities and limitations: from a Task Force for Mass Critical Care summit meeting, January 26–27, 2007, Chicago, IL. Chest. 2008;133:8S–17S. doi: 10.1378/chest.07-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fauci AS. Pandemic influenza threat and preparedness. Emerg Infect Dis. 2006;12:73–77. doi: 10.3201/eid1201.050983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vollmar LC. Military medicine in war: the Geneva Conventions today. In: Beam TE, Sparacino LR, editors. Military medical ethics. Office of The Surgeon General Department of the Army, USA; 2003. [Google Scholar]
- 4.Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE–a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med. 1996;11:117–124. doi: 10.1017/s1049023x0004276x. [DOI] [PubMed] [Google Scholar]
- 5.Garner A, Lee A, Harrison K, Schultz CH. Comparative analysis of multiple-casualty incident triage algorithms. Ann Emerg Med. 2001;38:541–548. doi: 10.1067/mem.2001.119053. [DOI] [PubMed] [Google Scholar]
- 6.Romig LE. Pediatric triage. A system to JumpSTART your triage of young patients at MCIs. JEMS. 2002;27:52–53. [PubMed] [Google Scholar]
- 7.Robertson-Steel I. Evolution of triage systems. Emerg Med J. 2006;23:154–155. doi: 10.1136/emj.2005.030270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iserson KV, Moskop JC. Triage in medicine, part I: concept, history, and types. Ann Emerg Med. 2007;49:275–281. doi: 10.1016/j.annemergmed.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 9.Moskop JC, Iserson KV. Triage in medicine, part II: underlying values and principles. Ann Emerg Med. 2007;49:282–287. doi: 10.1016/j.annemergmed.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy K, Aghababian RV, Gans L, Lewis CP. Triage: techniques and applications in decision making. Ann Emerg Med. 1996;28:136–144. doi: 10.1016/s0196-0644(96)70053-7. [DOI] [PubMed] [Google Scholar]
- 11.Hick JL, O'Laughlin DT. Concept of operations for triage of mechanical ventilation in an epidemic. Acad Emerg Med. 2006;13:223–229. doi: 10.1197/j.aem.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 12.Christian MD, Hawryluck L, Wax RS, Cook T, Lazar NM, Herridge MS, Muller MP, Gowans DR, Fortier W, Burkle FM. Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175:1377–1381. doi: 10.1503/cmaj.060911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devereaux A, Christian MD, Dichter JR, Geiling JA, Rubinson L. Summary of suggestions from the Task Force for Mass Critical Care summit, January 26–27, 2007. Chest. 2008;133:1S–7S. doi: 10.1378/chest.08-0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Devereaux AV, Dichter JR, Christian MD, Dubler NN, Sandrock CE, Hick JL, Powell T, Geiling JA, Amundson DE, Baudendistel TE, Braner DA, Klein MA, Berkowitz KA, Curtis JR, Rubinson L. Definitive care for the critically ill during a disaster: a framework for allocation of scarce resources in mass critical care: from a Task Force for Mass Critical Care summit meeting, January 26–27, 2007, Chicago, IL. Chest. 2008;133:51S–66S. doi: 10.1378/chest.07-2693. [DOI] [PubMed] [Google Scholar]
- 15.Powell T, Christ KC, Birkhead GS. Allocation of ventilators in a public health disaster. Disaster Med Public Health Prep. 2008;2:20–26. doi: 10.1097/DMP.0b013e3181620794. [DOI] [PubMed] [Google Scholar]
- 16.Christian MD, Kollek D, Schwartz B. Emergency preparedness: what every healthcare worker needs to know. Can J Emerg Med. 2005;7:330–337. doi: 10.1017/s1481803500014548. [DOI] [PubMed] [Google Scholar]
- 17.Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 18.Vincent JL, Moreno R, Takala J, Willatts S, De MA, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 19.Rubinson L, Nuzzo JB, Talmor DS, O'Toole T, Kramer BR, Inglesby TV. Augmentation of hospital critical care capacity after bioterrorist attacks or epidemics: recommendations of the Working Group on Emergency Mass Critical Care. Crit Care Med. 2005;33:2393–2403. doi: 10.1097/01.ccm.0000173411.06574.d5. [DOI] [PubMed] [Google Scholar]
- 20.The ANZIC Influenza Investigators. Critical Care Services and 2009 H1N1 Influenza in Australia and New Zealand. N Engl J Med. 2009;361(20):1925–1934. doi: 10.1056/NEJMoa0908481. [DOI] [PubMed] [Google Scholar]
- 21.Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, Stelfox T, Bagshaw S, Choong K, Lamontagne F, Turgeon AF, Lapinsky S, Ahern SP, Smith O, Siddiqui F, Jouvet P, Khwaja K, McIntyre L, Menon K, Hutchison J, Hornstein D, Joffe A, Lauzier F, Singh J, Karachi T, Wiebe K, Olafson K, Ramsey C, Sharma S, Dodek P, Meade M, Hall R, Fowler R. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA. 2009;302(17):1872–1879. doi: 10.1001/jama.2009.1496. [DOI] [PubMed] [Google Scholar]
- 22.Webb SA, Seppelt IM. Pandemic (H1N1) 2009 influenza (“swine flu”) in Australian and New Zealand intensive care. Crit Care Resusc. 2009;11:170–172. [PubMed] [Google Scholar]
- 23.Society of Critical Care Medicine Ethics Committee. Sprung CL, Danis M, Baily MA, Chalfin D, Dagi TF, Davila F, De Vita M, Engelhardt HT, Grenvik A, Hofmann PB, Hoyt JW, Kofke WA, Lynn J, Marshall MF, McCartney JJ, Nelson RM, Ninos N, Raphaely RC, Reardon F, Rie MA, Rosenbaum SH, Silverman H, Sottile FD, Spanier A, Steinberg A, Tendier MD, Teres D, Truog RD, Wallace TE, Wlody G, Yeh TS. Consensus statement on the triage of critically ill patients. Society of Critical Care Medicine Ethics Committee. JAMA. 1994;271:1200–1203. [PubMed] [Google Scholar]
- 24.Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Egol A, Fromm R, Guntupalli KK, Fitzpatrick M, Kaufman D, Nasraway S, Ryon D, Zimmerman J. Guidelines for intensive care unit admission, discharge, and triage. Crit Care Med. 1999;27:633–638. [PubMed] [Google Scholar]
- 25.American Thoracic Society Bioethics Task Force. Fair allocation of intensive care unit resources. American Thoracic Society. Am J Respir Crit Care Med. 1997;156:1282–1301. doi: 10.1164/ajrccm.156.4.ats7-97. [DOI] [PubMed] [Google Scholar]
- 26.Dominguez-Cherit G, Lapinsky SE, Macias AE, Pinto R, Espinosa-Perez L, de la TA, Poblano-Morales M, Baltazar-Torres JA, Bautista E, Martinez A, Martinez MA, Rivero E, Valdez R, Ruiz-Palacios G, Hernandez M, Stewart TE, Fowler RA. Critically ill patients with 2009 influenza A(H1N1) in Mexico. JAMA. 2009;302(17):1880–1887. doi: 10.1001/jama.2009.1536. [DOI] [PubMed] [Google Scholar]
- 27.Khan Z, Hulme J, Sherwood N. An assessment of the validity of SOFA score based triage in H1N1 critically ill patients during an influenza pandemic. Anaesthesia. 2009;64:1282–1288. doi: 10.1111/j.1365-2044.2009.06135.x. [DOI] [PubMed] [Google Scholar]
- 28.Christian M, Hamielec C, Lazar N, Wax R, Griffith L, Herridge M, Lee D, Cook D. A retrospective cohort pilot study to evaluate a triage tool for use in a pandemic. Crit Care. 2009;13:R170. doi: 10.1186/cc8146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guest T, Tantam G, Donlin N, Tantam K, McMillan H, Tillyard A. An observational cohort study of triage for critical care provision during pandemic influenza: ‘clipboard physicians’ or ‘evidenced based medicine’? Anaesthesia. 2009;64:1199–1206. doi: 10.1111/j.1365-2044.2009.06084.x. [DOI] [PubMed] [Google Scholar]
- 30.Lecuyer L, Chevret S, Thiery G, Darmon M, Schlemmer B, Azoulay E. The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med. 2007;35:808–814. doi: 10.1097/01.CCM.0000256846.27192.7A. [DOI] [PubMed] [Google Scholar]