Abstract
Leiomyosarcoma of the inferior vena cava is a rare tumour arising from the smooth muscle fibres of the media with a mean size at diagnosis generally around 12 cm (range 2–38 cm). This study compares a 4-cm leiomyosarcoma of the inferior vena cava discovered incidentally with a symptomatic late stage leiomyosarcoma.
Keywords: Inferior vena cava, mesenchymal tumour, leiomyosarcoma of the inferior vena cava, multidetector computed tomography, magnetic resonance
Introduction
Leiomyosarcoma (LMS) of the inferior vena cava (IVC) is a very rare tumour (less than 1% of all malignant tumours)[1] but is the most common primary IVC neoplasm. It is a mesenchymal tumour arising from the smooth muscle fibres of the media, more frequently in the sixth decade of life in women[2]. The clinical and radiological features depend on its original site and on its pattern of growth (extra or intraluminal). En bloc resection with negative margins is the gold standard treatment, but it is not always possible to carry out because the diagnosis is often delayed; most of these tumours in fact have a slow growth pattern and are located in the retroperitoneal space, so that symptoms are non-specific and occur later on[3]. The imaging findings of 2 different cases are compared: a small (4 cm) LMS discovered incidentally in a breast cancer follow-up, studied by abdominal magnetic resonance (MRI) and a symptomatic advanced stage IVC mass detected by multidetector-row computed tomography (MDCT).
Case report 1
A 67-year-old woman was admitted to our hospital with an abdominal ultrasound scan performed for a breast cancer follow-up, showing an hypoechogenic 44-mm rounded mass at the porta hepatis. No clinical symptoms and blood test abnormalities were present. Serum levels of the breast tumour markers (cancer antigen 125 and cancer antigen 15.3) were in the normal range. To better characterize the lesion an abdominal contrast-enhanced MRI was then performed on a 1.5 T scanner using a phased array body coil. Unenhanced MR axial scans including gradient-echo (GRE) fast low-angle shot (FLASH) axial breath hold sequences, T1-weighted (w) (repetition time (TR): 143 ms, echo time (TE) 6 ms, slice thickness 5 mm, acquisition time 21 s), T1w fat saturation (fs) (TR 333 ms, TE 4.32 ms, slice thickness 5 mm, acquisition time 24 s) and a turbo spin-echo (TSE) multi-breath hold T2w (TR 3120 ms, TE 120 ms, slice thickness 5 mm, acquisition time 109 s) were performed. The axial GRE FLASH T1w sequences 30 s and 70 s post intravenous administration of 16 ml of contrast medium (paramagnetic Gd-diethylenetriamine pentaacetic acid (DTPA), Dotarem, Guerbet) were obtained.
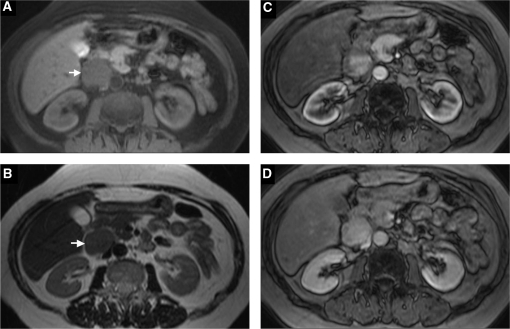
MRI showed a rounded, solid retroperitoneal mass (4 cm) with regular edges, which involved the space between the pancreas head, the duodenum and the IVC, homogeneously hypointense on T1w and T1w fs (Fig. 1A), with an intermediate signal intensity on T2w (Fig. 1B). No internal necrotic areas were seen. Scans post Gd showed an early high non-homogeneous enhancement with greater filling in venous phase (Fig. 1C,D). The IVC appeared compressed by the lesion without internal filling defects. The pancreatic head and the right adrenal gland were not involved; no sure plane of cleavage with the duodenal intestinal wall was clearly depicted. No other pathological findings were seen.
Figure 1.
MR axial images: GRE FLASH T1w fs (A) and TSE T2w (B). GRE VIBE T1w post-Gd in arterial (C) and venous phase (D). The lesion appears homogenous and hypointense (arrow) on T1w fs scan (A) and shows an intermediate signal intensity (arrow) on the T2w sequence (B). An intense, non-homogeneous enhancement in arterial phase (C), with greater filling in venous phase (D) is detected. The IVC appears compressed but well opacified. No plane of cleavage with the duodenal wall is visible.
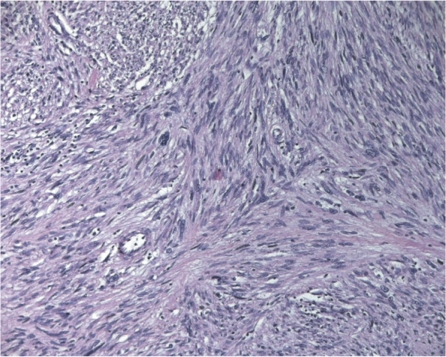
At surgery the lesion was located on the anterior wall of the inter-renal IVC segment (segment II), with tumour development predominantly extracaval. The lesion was resected with a macroscopic free margin of the anterior wall of the vein. Primary closure of the defect was performed. No patch repair was necessary. Postoperative recovery was uneventful and the patient was discharged on postoperative day 4. No oedema or venous stasis of the lower limbs occurred. Pathologic exam showed a 4.5×3.5×3 cm moderately circumscribed, encapsulate fibrous tumour adherent to the IVC wall with an extension of 1.5 cm. The tumour parenchyma was white with areas of myxoid change and necrosis. The neoplasia presented a pattern of intersecting sharply marginated groups of spindle cells, with palisaded arrangement (Fig. 2). It was characterized by immunoreactivity for smooth muscle actin (SMA), desmin and CD34, by the absence of staining for CD117 and by a moderate proliferative index valued with Ki-67 (20%). The final diagnosis was a leiomyosarcoma of the IVC (pT1b N0 Mx, G2 Stage I sec AJCC 2002). There was no recurrence at 15 months follow-up.
Figure 2.
Leiomyosarcoma with typical intersecting clusters of spindle cells (haematoxylin and eosin stain, magnification×20).
Case report 2
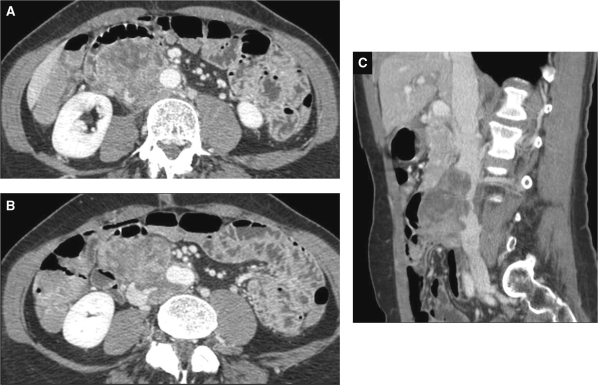
A 54-year-old woman was admitted to our hospital for moderately severe progressive back pain in the right lower abdominal quadrant, occurring several weeks prior to admission. Physical examination revealed the presence of a relatively immobile and non-tender egg-shaped mass in the lower right quadrant. An abdominal MDCT (16 row, slice thickness 1.25 mm, rotation time 0.5 s, collimation 16×1.25 mm, pitch 1.75:1, interval 1.25 mm) before and after administration of intravenous iodinated contrast medium with enhanced scans acquired at 30 and 70 s (140 ml contrast medium bolus, flow rate of 3 ml/s) was performed. Computed tomography (CT) showed a large, lobulated, retroperitoneal mass (7.5×5×4.3 cm), heterogeneously enhanced in venous phase, with internal necrotic areas; the lesion involved the infra-renal IVC segment, which appeared narrowed and irregular up to the confluence of the iliac vessels. The mass surrounded the abdominal aorta, involving more than 50% of the aortic wall and displacing the intestinal loops anteriorly (Fig. 3A–C). Multiple pelvic (gluteus and perineal) venous collateral vessels were seen. A lower IVC tumour with a bidirectionally, predominantly extraluminal spread was diagnosed.
Figure 3.
Contrast-enhanced CT axial images in venous phase A large heterogeneously enhanced retroperitoneal mass, arising from the lower IVC, involving more than 50% of the aortic wall and displacing the intestinal loops anteriorly (A) is depicted. The tumour extends to the confluence of the iliac vessels (B). A sagittal multi-planar reconstruction shows a narrowed and irregular IVC for throughout the longitudinal spread of the mass (C).
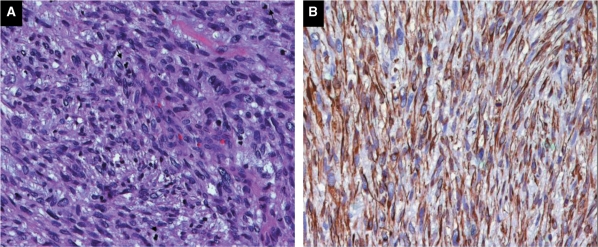
Exploration of the abdomen disclosed an oval tumour originating from the wall of the IVC, below the origin of the renal veins. No metastases were observed. The mass caused a wide infiltration of the aorta and the adjacent structures. In order to achieve a histological diagnosis and to plan adjuvant chemotherapy a wide portion of the tumour was resected. The postoperative course was uneventful. Microscopically the features of the mass suggested a highly cellular spindle cell tumour, arising from the wall of the IVC. The tumour showed prominent mitotic activity (up to 40 mitotic figures/10 high power fields) and multiple foci of necrosis (Fig. 4A). Immunoperoxidase staining showed SMA and desmin (S-l00, CD34 and CD117 negative) (Fig. 4B). The overall conclusion was suggestive of a high-grade leiomyosarcoma.
Figure 4.
Leiomyosarcoma composed of elongated cells some with larger and hyperchromatic nuclei (haematoxylin and eosin stain, ×20) (A). Neoplastic cells showed cytoplasmic staining with desmin (immunohistochemistry, ×20) (B).
The patient underwent 3 cycles of chemotherapy with epirubicin (90 mg/m2 per day) and ifosfamide (2500 mg/m2 for 1–3 days). Unfortunately, CT follow-up showed no improvement after treatment. Therefore, the patient underwent a new surgical procedure at another institution and part of the IVC involved was resected. This procedure was possible because collateral circulation was already established. The adjacent aorta, also infiltrated, was resected and replaced with a Dacron prosthetic graft. The postoperative course was uneventful.
Discussion
LMS of the IVC is a mesenchymal retroperitoneal tumour arising from the media of the vessel wall. The majority of cases occur in women (74%), with a mean age of 52 years[1]. It is a rare tumour described for the first time by Pearl in 1871; in 1992 the International Registry of the IVC sarcomas recorded 218 cases[4] and 418 cases have been reported in the literature[3]. The clinical, radiological and prognostic features depend on the site of origin (IVC upper, middle or lower tract) and on the pattern of growth[5]. The tumour arises from the middle segment of the IVC (from the renal to the hepatic veins) in 33%, from the lower level (below the renal veins) in 8% and from the upper level (from the right atrium to the origin of the hepatic veins) in 3%. In other cases the tumour involves more than one level or the level of origin is not specified[1].
Patients with tumours that arise from the middle segment had better prognosis (5- and 10-year survival rates of 56.7% and 4.3%) than those of the lower segment (37.8% and 14.2%)[6]. The tumour initially grows in an intramural fashion, often associated with thromboses[7]; the extraluminal spreading is predominant (76%) and in this case lesions have to be differentiated from tumours of the surrounding organs, such as kidney, adrenal glands, pancreas, duodenum[8] and from other retroperitoneally developing masses (lymphoma, soft tissue sarcomas, germ cell tumours, lymph-node metastasis). α-Fetoprotein (AFP) and β-subunit of human chorionic gonadotropin (β-hCG) are invaluable tumour markers in the diagnosis of non-seminomatous germ cell tumours, showing elevated serum levels, and could be useful to differentiate these tumours from the other retroperitoneal masses[9].
Symptoms are non-specific (abdominal pain, nausea, vomiting, weight loss) and they present late in the disease course. Other possible presenting symptoms according to the segment of the IVC involved and LMS spread are the Budd–Chiari syndrome in 17% and deep vein thrombosis (4%)[1]. Biopsy can be useful to obtain histological findings to plan the best treatment; percutaneous access is usually preferred or, if this is not suggested for technical reasons, surgical access may be required.
Complete surgical resection is the only chance for cure. Radical tumour resection was associated with better 5- and 10-year survival rates (49.4% and 29.5%)[6]. We report 2 cases with 2 different clinical and prognostic findings: the first case is a small, incidentally discovered, asymptomatic middle IVC tumour; its small size allowed complete lesion resection with primary closure of the IVC defect; no recurrence after 15 months follow-up was observed. The second case is a symptomatic, large, invasive lower IVC tumour, discovered at a late stage because of its slow growth, non-specific and delayed symptoms (mean size at LMS diagnosis reported in literature generally around 12 cm[1]); complete surgical tumour resection was unsuccessful because of the size and extension of the tumour. A large, highly heterogeneous enhanced mass with internal areas of necrosis, infiltrating the surrounding soft tissues and the aorta, was clearly depicted by CT. A lower IVC neoplasm with bidirectional and predominantly extraluminal spread was diagnosed. On MRI the first case was reported as a fairly homogeneous small mass, regular in shape, hypointense on T1w fs scan, with an intermediate signal intensity on T2w sequence; the lesion appeared hyper-vascular, with moderate non-homogeneous enhancement due to its small size and the absence of internal necrotic areas. No signs of infiltration of the surrounding structures and no IVC filling defects were detected. Accurate detection of the origin of the lesion and its characterization could not be determined exactly, because of the lack of a specific signal intensity on the MR findings. Surgical and pathological findings showed a 4-cm IVC middle segment LMS with extraluminal growth. Thus, in the first case, detection on imaging was early and favourable and complete surgical excision was possible. The second case clearly represents a natural evolution of LMS, generally discovered and treated at an advanced stage, with a less favourable prognosis. Imaging plays an important role in the characterization and preoperative staging of retroperitoneal masses, showing the extension of the lesion and the relationship with surrounding organs and structures[5]. The imaging accuracy in the diagnosis of an LMS site of origin depends on size, pattern of growth and the relationship between the lesion and the IVC lumen[10]. For these reasons the site of origin of the lesion in the first case represented a diagnostic dilemma; in the second case the site of origin was clearly detected.
Footnotes
This paper is available online at http://www.cancerimaging.org. In the event of a change in the URL address, please use the DOI provided to locate the paper.
References
- 1.Hilliard NJ, Heslin MJ, Castro CY. Leiomyosarcoma of the inferior vena cava. Three case reports and review of the literature. Ann Diagn Pathol. 2005;9:259–66. doi: 10.1016/j.anndiagpath.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Abisi S, Morris-Stiff GJ, Scott-Coombes D, et al. Leiomyosarcoma of the inferior vena cava: clinical experience with four cases. World J Surg Oncol. 2006;4:1. doi: 10.1186/1477-7819-4-1. doi:10.1186/1477-7819-4-1. PMid:16393338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jenkins S, Marshall B, Gray R. Leiomyosarcoma of the inferior vena cava. J Can Chir. 2005;48:252–3. [PMC free article] [PubMed] [Google Scholar]
- 4.Mingoli A, Cavallaro A, Sapienza P, et al. International registry of inferior vena cava leiomyosarcoma: analysis of a world series on 218 patients. Anticancer Res. 1996;16:3201–5. [PubMed] [Google Scholar]
- 5.Hemant D, Krantikumar R, Amita J, Chawla A, Ranjeet N. Primary leiomyosarcoma of inferior vena cava, a rare entity: imaging features. Aust Radiol. 2001;45:448–51. doi: 10.1046/j.1440-1673.2001.00955.x. doi:10.1046/j.1440-1673.2001.00955.x. PMid:11903177. [DOI] [PubMed] [Google Scholar]
- 6.Vinaykumar BT, Rajeev RS, Geeta MK, Apurva SC. Leiomyosarcoma of the inferior vena cava: a case report and review of literature. Int Surg. 2005;90:262–5. [PubMed] [Google Scholar]
- 7.Hollenbeck ST, Grobmyer SR, Kent KC, Brennan MF. Surgical treatment and outcomes of patients with primary inferior vena cava leiomyosarcoma. J Am Coll Surg. 2003;197:575–9. doi: 10.1016/S1072-7515(03)00433-2. doi:10.1016/S1072-7515(03)00433-2. [DOI] [PubMed] [Google Scholar]
- 8.Illuminati G, Caliò FG, D’Urso A, Giacobbi D, Papaspyropoulos V, Ceccanei G. Prosthetic replacement of the infrahepatic inferior vena cava for leiomyosarcoma. Arch Surg. 2006;141:919–24. doi: 10.1001/archsurg.141.9.919. doi:10.1001/archsurg.141.9.919. PMid:16983035. [DOI] [PubMed] [Google Scholar]
- 9.Abe H, Taui T, Noiothetal H, et al. Retroperitoneal germ cell humour treated by PVeBv chemotherapy: a case report. Jpn J Clin Oncol. 1999;29:261–3. doi: 10.1093/jjco/29.5.261. doi:10.1093/jjco/29.5.261. PMid:10379339. [DOI] [PubMed] [Google Scholar]
- 10.Kleffer E, Alaoui M, Piette JC, et al. Leiomyosarcoma of the inferior vena cava: experience in 22 cases. Ann Surg. 2006;244:289–95. doi: 10.1097/01.sla.0000229964.71743.db. doi:10.1097/01.sla.0000229964.71743.db. PMid:16858193. [DOI] [PMC free article] [PubMed] [Google Scholar]