Abstract
Background
Painful limbs/moving extremities is a relatively rare condition characterized by aching pain in one limb and involuntary movement in the affected fingers or toes. Its pathomechanism is unknown. We report two patients with painful limbs/moving extremities. In one patient with a painful arm and moving fingers, the symptoms were resolved after surgery.
Case Descriptions
Patient 1 was a 36-year-old man with a painful arm and moving fingers. Treatment with administration of analgesics was not effective. Postmyelographic CT showed stenosis of the right C5/C6 foramen attributable to cervical spondylosis and a defect of the contrast material at the foramen. He was treated with cervical foraminotomy. Patient 2 was a 26-year-old woman with a painful leg and moving toes. The pain and involuntary movement appeared 2 weeks after discectomy at L5/S1. Lumbar MRI and myelography showed no indications of nerve root compression. She was treated with a lumbar nerve root block. The pain and involuntary movement completely disappeared in both patients after treatment.
Literature Review
Numerous studies report treatments for painful limbs/moving extremities, but few report successful treatment. Recently, botulinum toxin A injection and epidural spinal cord stimulation have been used and are thought to benefit this condition. Successful surgical treatment previously was reported for only one patient.
Purposes and Clinical Relevance
If imaging indicates compression of nerve tissue, we believe surgical decompression should be considered for patients with painful limbs/moving extremities who do not respond to nonoperative treatment.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-010-1437-y) contains supplementary material, which is available to authorized users.
Introduction
Painful arm and moving fingers (PAMF), which is characterized by aching pain in the upper extremity and spontaneous involuntary movements of the fingers, was first reported by Verhagen et al. [39] in 1985. A similar and more common syndrome in the lower extremity is called painful legs and moving toes (PLMT), first coined by Spillane et al. [32] in 1971. Papapetropoulos and Argyriou [20] described these disorders as painful limbs/moving extremities (PLME). These were divided into several subtypes according to localization of movement and pain and laterality of symptoms. PLME is a relatively rare disorder and its pathomechanism is unknown.
We treated two patients with PLME. The first was a patient with PAMF in whom cervical nerve root compression potentially led to the symptoms, as indicated by improvement after cervical foraminotomy. The second was a patient with PLMT after surgery for lumbar disc herniation. We found only one previous report of patients with PAMF whose symptoms were resolved after surgery [34]. We herein report these two patients and review the literature.
Case Reports
Patient 1
A 36-year-old man was referred to our hospital after a 1-month history of pain in his neck and right scapular region, followed by aching or burning pain in his right thumb, index finger, and upper arm and involuntary movements of the right thumb. Treatment with administration of analgesics was not effective. He and his family had no remarkable contributory history including psychogenic disease.
On examination, there was aching pain at rest in his right thumb and index finger and involuntary flexion-extension movement of the thumb at the carpometacarpal joint (Video 1, Supplemental Website Material; supplemental materials are available with the online version of CORR).
Movement of the thumb increased in proportion to the degree of pain and could not be stopped by conscious effort. Moreover, the patient could not voluntarily reproduce the movement on the unaffected side when asked to do so. It disappeared during sleep but otherwise, basically, was a continuous movement. Neurologic examinations showed Grade 4 of 5 in manual muscle testing of the right biceps muscle and wrist extensor muscles, sensory disturbance in the right C6 distribution, weakness in the right brachioradialis tendon reflex, and radiating pain to the thumb and index finger reproduced by neck extension and side flexion (positive test using the criteria of Spurling and Scoville [33]) on the right side, indicating right C6 radiculopathy. MRI showed no compression of the spinal cord but minimal stenosis at the right C5/C6 foramen. Also, postmyelographic CT showed stenosis of the right C5/C6 foramen attributable to cervical spondylosis and a defect of the contrast material at the foramen (Fig. 1). A right C6 nerve root block was performed and resulted in temporary disappearance of the pain. The pain recurred the next morning and the involuntary movement did not stop while the nerve block was in effect.
Fig. 1.

A postmyelographic CT scan shows stenosis of the right C5/C6 foramen (arrow) attributable to cervical spondylosis and a defect of the contrast material at the foramen.
Right C6 cervical spondylotic radiculopathy was diagnosed on the basis of this patient’s pain. We consulted a neurologist and planned to observe the patient closely and obtain additional studies including electromyography (EMG) and brain MRI. However, because the pain was severe and resistant to oral medication or nerve root block, we proceeded with surgery for the right C6 cervical spondylotic radiculopathy. Two months later a C5 laminoplasty and right C5/C6 foraminotomy were performed. After the surgery, the pain and involuntary movements had completely disappeared. At 2 years followup, the patient had no recurrence of pain or involuntary movements.
Patient 2
A 26-year-old woman was referred to our hospital after a 6-month history of left sciatica unsuccessfully treated by nonsurgical therapies. Lumbar disc herniation at L5/S1 was diagnosed and she underwent discectomy. Two weeks later, she felt pain in her left leg and involuntary movement of her left toes appeared. The movement was a combination of flexion-extension and adduction-abduction, and each toe motion was independent (Video 2, Supplemental Website Materials; supplemental materials are available with the online version of CORR). Moreover, the movement could not be stopped by conscious effort and the patient could not voluntarily reproduce the movement on the unaffected side when asked to do so. However, the movement did disappear during sleep. Lumbar MRI and myelography showed no indications of nerve root compression. The neurologist to whom we referred the patient ruled out any psychogenic disorder and other neurologic movement disorders by MRI of the brain. The pain was not relieved and the involuntary movement was not resolved by a caudal block and administration of clonazepam, diazepam, haloperidol, and adenosine triphosphate disodium. A left S1 nerve root block had a temporary effect, resulting in disappearance of the pain in her leg and the involuntary movement of the toes for a few days. Therefore, we performed the same nerve root block seven times, and 4 months after administration of the first nerve root block, the pain and involuntary movement had completely disappeared. Three months after disappearance of the pain and involuntary movement, the patient was lost to followup because she changed her residence.
Discussion
PLME is defined as the association of aching or burning pain in at least one limb and involuntary movement of at least one finger or toe. The involuntary movement is spontaneous and continuous and characterized by flexion-extension and/or abduction-adduction movement of affected fingers or toes. Typically, the movement increases in proportion to the degree of pain and cannot be reproduced on the unaffected side. Some of the patients can stop the movement for a short time by conscious effort and the movement disappears during sleep. There are some reports of patients with PLME without pain, called painless limbs/moving extremities [2–5, 21, 31, 41].
We identified 12 patients with PLME of the upper extremity (PAMF), and of these patients, only one was successfully treated surgically [34] (Table 1). There are more reported cases of PLME in the lower extremity (PLMT) than in the upper extremities (PAMF). However, there have been no reports of PLMT being successfully resolved surgically, and only two reports of PLMT being partially or temporary improved surgically [14, 42] (Table 2).
Table 1.
Review of the literature (painful arms and moving fingers)
| Study | Age (years), gender | Pathology | Treatment | Clinical outcome | |
|---|---|---|---|---|---|
| Pain | Involuntary movement | ||||
| Verhagen et al. [39] | 54 F | Brachial plexus | |||
| Funakawa et al. [8] | 52 M | Peripheral nerve (trauma) | Oral medication | No change | No change |
| Ebersbach et al. [6] | 64 M | Oral medication | No change | No change | |
| Jabbari et al. [13] | 35 F | Peripheral nerve (trauma) | Oral medication | No change | No change |
| Botulinum toxin A injection | No change | Transient relief | |||
| Supiot et al. [35] | 68 M | Brachial plexus | Transportion of the ulnar nerve | No change | No change |
| Oral medication (calcitonin) | Transient relief | Decreased | |||
| 25 F | Nerve root (CSR) | Oral medication (calcitonin) | Transient relief | Transient relief | |
| 49 M | Peripheral nerve (trauma) | Oral medication (amantadine) | Decreased | Decreased | |
| 66 F | CNS (stroke) | Oral medication | No change | No change | |
| Sudo et al. [34] | 56 F | Spinal cord (CSM) | Cervical laminoplasty | Disappeared | Disappeared |
| Singer and Papapetropoulos [31] | 20 F | Painless | Botulinum toxin A injection | None | Disappeared |
| Schwingenschuh and Bhatia [29] | 62 F | Hypothyroidism | Oral medication | No change | No change |
| Current study | 36 M | CSR | Cervical foraminotomy | Disappeared | Disappeared |
F = female; M = male; CNS = central nervous system; CSR = cervical spondylotic radiculopathy; CSM = cervical spondylotic myelopathy.
Table 2.
Review of the literature (painful legs and moving toes)
| Study | Age (years), gender | Pathology | Treatment | Clinical outcome | |
|---|---|---|---|---|---|
| Pain | Involuntary movement | ||||
| Spillane et al. [32] | 48 M | SNS | Block of SNS | Transient relief | Transient relief |
| Sympathectomy | No change | No change | |||
| 54 M | SNS | Block of SNS | Disappeared | Disappeared | |
| 67 F, 54 M | SNS | Block of SNS | Transient relief | Transient relief | |
| 68 F, 53 M | Oral medication | No change | No change | ||
| Okamoto et al. [18] | 62 F | Oral medication | No change | ||
| Block of SNS | Disappeared | ||||
| Nathan [17] | 46 F | Nerve root (herpes zoster) | |||
| 30 F | Nerve root (trauma) | ||||
| 57 M | Nerve root (cyst) | Nerve root decompression | No change | No change | |
| 62 F | Peripheral nerve (trauma) | ||||
| Schott [28] | 69 F | Trauma | Block of SNS | Transient relief | Transient relief |
| 56 F, 77 F | Trauma | Block of SNS | No change | No change | |
| 66 M, 57 F | Oral medication | No change | No change | ||
| Wulff [42] | 56 M, 64 M | Oral medication | NC | NC | |
| 41 F | Herniotomy | Herniotomy | Disappeared | Transient relief | |
| Montagna et al. [15] | 60 M | Peripheral nerve (neuropathy) | Oral medication | Transient relief | No change |
| 74 F, 76 F | Peripheral nerve (neuropathy) | Oral medication | No change | No change | |
| Schoenen et al. [27] | 71 F, 80 F, 49 M, 69 F, 68 F, 74 M | Oral medication | No change | No change | |
| Sahashi et al. [24] | 62 F, 75 M | Block of SNS | No change | No change | |
| Oral medication | No change | No change | |||
| Sandyk [26] | 51 F | Neuroleptic | Oral medication (baclofen) | Decreased | Decreased |
| Oral medication (clonazepam) | Decreased | No change | |||
| Mitsumoto et al. [14] | 40 F | Peripheral nerve (lymphoma) | Resection | Decreased | Disappeared |
| Guieu et al. [10] | 29 M | CNS, peripheral nerve (trauma) | Clonazepam injection | Transient relief | Transient relief |
| TENS | Disappeared | ||||
| Uchihara et al. [38] | 56 M | Hypophysectomy | Epidural block | Transient relief | Transient relief |
| Block of SNS | Disappeared | Disappeared | |||
| 46 M | Parkinson’s disease | Epidural block | Transient relief | Transient relief | |
| Block of SNS | Disappeared | Disappeared | |||
| Walters et al. [41] | 25 M | Peripheral nerve Painless |
None | ||
| Guieu et al. [9] | 30 M | Peripheral nerve (trauma) | ATP injection | Disappeared | |
| 72 F | ATP injection | Disappeared | |||
| Dressler et al. [4] | 36 M | Spinal cord (trauma) | Block of SNS | No change | No change |
| 76 F | Nerve root (herpes zoster) | Block of SNS | Transient relief | Transient relief | |
| 49 F | Nerve root | Block of SNS | No change | No change | |
| 69 F | Nerve root | ||||
| 28 M | Nerve root (hemangioma) | ||||
| 66 F, 73 M | Nerve root | ||||
| 28 F | Peripheral nerve (trauma) | Block of SNS | Decreased | Decreased | |
| 68 F | Peripheral nerve (trauma) | ||||
| 67 F | Peripheral nerve (trauma) | Block of SNS | Transient relief | Transient relief | |
| 66 F, 74 F | Peripheral nerve (trauma) | Block of SNS | No change | No change | |
| 61 F, 72 F | Peripheral nerve (neuropathy) | ||||
| 69 F, 54 M | Peripheral nerve (neuropathy) | ||||
| 67 F, 72 F | |||||
| 65 F | Block of SNS | No change | No change | ||
| 64 F | |||||
| 28 M, 36 M | Painless | None | |||
| 45 M | Painless | None | |||
| Mosek et al. [16] | 57 F | Nerve root | Laminectomy | No change | No change |
| Dorsal root block | Transient relief | Transient relief | |||
| Pla et al. [23] | 35 M | Peripheral nerve (neuropathy) | Block of plantar nerve | Transient relief | Transient relief |
| Foot orthosis | Decreased | Decreased | |||
| Ebersbach et al. [6] | 64 M | Oral medication | No change | No change | |
| Touge et al. [37] | 37 M | Peripheral nerve (neuropathy) | Oral medication | No change | No change |
| Block of SNS | Decreased | Disappeared | |||
| Okuda et al. [19] | 36 F | Epidural block | Disappeared | Disappeared | |
| 56 M | Epidural block | Transient relief | Transient relief | ||
| Block of SNS | No change | No change | |||
| 50 F | Oral medication | No change | No change | ||
| Epidural block | Transient relief | Transient relief | |||
| Shime and Sugimoto [30] | 63 F | Block of SNS | Transient relief | Transient relief | |
| Pitagoras de Mattos et al. [22] | 38 M, 51 M | Peripheral nerve (neuropathy), HIV | Oral medication | No change | No change |
| Sanders et al. [25] | 76 F | Oral medication | No change | No change | |
| Takahashi et al. [36] | 51 M | Epidural block, TENS | No change | No change | |
| Block of SNS | Transient relief | Transient relief | |||
| ESCS | Decreased | Decreased | |||
| Dziewas et al. [5] | 38 F, 70 F | Painless | None | ||
| Ikeda et al. [12] | 75 F | Spinal cord (herpes zoster) | Block of SNS | No change | No change |
| Epidural block, ESCS | No change | No change | |||
| Villarejo et al. [40] | 66 M | Oral medication (gabapentin) | Disappeared | Disappeared | |
| Papapetropoulos and Singer [21] | 20 F | Wilson’s disease Painless |
Oral medication (zinc acetate) | None | Disappeared |
| Aizawa [1] | 73 F | Oral medication (gabapentin) | Decreased | No change | |
| Guimaraes et al. [11] | 60 M | Hashimoto disease | Prednisolone | No change | No change |
| Bermejo and Zabala [2] | 82 F | Spinal cord Painless |
Laminectomy | None | Disappeared |
| DiFabio et al. [3] | 74 F | Peripheral nerve Painless |
Oral medication (quetiapene) | None | Transient relief |
| Eisa et al. [7] | 62 M, 76 F | Oral medication | No change | No change | |
| BTA injection | Decreased | Decreased | |||
| Schwingenschuh and Bhatia [29] | 62 F | Hypothyroidism | Oral medication | No change | No change |
| Current study | 26 F | Nerve root (after herniotomy) | Nerve root block | Disappeared | Disappeared |
M = male; F = female; SNS = sympathetic nervous system; CNS = central nervous system; TENS = transcutaneous electrical nerve stimulation; ATP = adenosine triphosphate; ESCS = epidural spinal cord stimulation; BTA = botulinum toxin A.
PLME is a relatively rare disorder; therefore, the pathophysiology is not fully understood. Based on the effectiveness of the lumbar sympathetic ganglion block, Spillane et al. [32] speculated that abnormal impulses from afferent fibers in the sympathetic nervous system activated ventral horn cells in the spinal cord, resulting in the involuntary movement. Nathan [17] proposed that abnormal stimulation to the nerve root or peripheral nerve caused pain in the limbs and evoked involuntary movement by stimulating ventral horn cells via the spinal interneuron. Meanwhile, as involuntary movement does not appear during sleep, Schott suggested it was associated with the reticular activating system [28], which is controlled by consciousness.
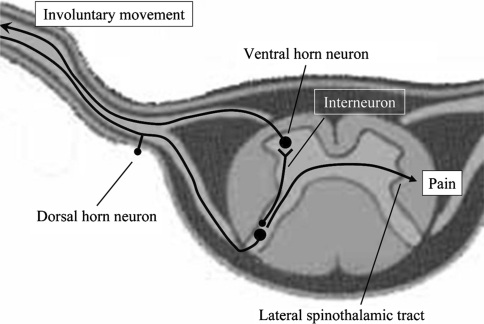
In our patients, the pain and involuntary movement disappeared after decompression or block of the spinal nerve root, supporting Nathan’s theory regarding the pathomechanism of PLME (Fig. 2). He theorized that ectopic impulses of the nerve root caused by irritation are conducted to the spinal dorsal horn neurons through the afferent pathway, leading to pain perception. At the same time, the impulses from the nerve root would excite the local spinal interneuron and lead to stimulation of spinal ventral horn neurons, resulting in involuntary movement of the extremity.
Fig. 2.
According to the interneuron theory of Nathan [17], pain is perceived through the lateral spinothalamic tract. The impulse excites the spinal interneuron and leads to stimulation of spinal ventral horn cells, resulting in involuntary movement of the extremity.
Nonsurgical treatments, including administration of benzodiazepine or γ-aminobutyric acid and sympathetic ganglion block, are commonly performed [6–8, 13, 15, 18, 19, 22, 24–29, 32, 35–37, 40, 42] for patients with PLME because the central nervous system or sympathetic nervous system also is considered to be the cause of PLME, as mentioned above. However, symptoms of PAMF (Table 1) and PLMT (Table 2) usually are resistant to such treatments.
Dressler et al. [4] reported that sympathetic ganglion block was effective in approximately 50% of patients with PLME but the effects were transient. Guieu et al. [9] treated two patients with PLMT by injection of adenosine triphosphate. The pain disappeared but the effect on movement was not mentioned. Okuda et al. [19] suggested several advantages of epidural block over sympathetic ganglion block, and Takahashi et al. [36] reported the benefit of epidural spinal cord stimulation for PLMT. Recently, treatment with botulinum toxin A (BTA) injection was reported by Singer and Papapetropoulos [31] and Eisa et al. [7]. The injection resulted in substantial pain relief and reduction of involuntary movement owing to reduction of the muscle spindle leading to decreased activity of the gamma loop and central sensitization.
Sudo et al. [34] reported the only case of a patient with PAMF in whom pain and involuntary movement were resolved by surgery. In their patient, cervical radiculopathy or segmental myelopathy was thought to be the cause of the symptoms, and bilateral open-door laminoplasty was performed. Similarly, the symptoms in our first patient were resolved by decompression of the nerve root. Therefore, we believe surgical treatment should be considered for patients in whom compression of nerve tissue is recognized by MRI and/or CT but in whom no response is obtained by nonsurgical treatment.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aizawa H. Gabapentin for painful legs and moving toes syndrome. Intern Med. 2007;46:1937. doi: 10.2169/internalmedicine.46.0416. [DOI] [PubMed] [Google Scholar]
- 2.Bermejo PE, Zabala JA. “Painless legs and moving toes” syndrome due to spinal cord compression. Eur Spine J. 2008;17(suppl 2):S294–S295. doi: 10.1007/s00586-008-0590-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Fabio R, Casali C, Pierelli F. Quetiapine: an alternative treatment in painless legs and moving toes. Mov Disord. 2008;23:1326–1328. doi: 10.1002/mds.22047. [DOI] [PubMed] [Google Scholar]
- 4.Dressler D, Thompson PD, Gledhill RF, Marsden CD. The syndrome of painful legs and moving toes. Mov Disord. 1994;9:13–21. doi: 10.1002/mds.870090104. [DOI] [PubMed] [Google Scholar]
- 5.Dziewas R, Kuhlenbäumer G, Okegwo A, Lüdemann P. Painless legs and moving toes in a mother and her daughter. Mov Disord. 2003;18:718–722. doi: 10.1002/mds.10435. [DOI] [PubMed] [Google Scholar]
- 6.Ebersbach G, Schelosky L, Schenkel A, Scholz U, Poewe W. Unilateral painful legs and moving toes syndrome with moving fingers: evidence for distinct oscillators. Mov Disord. 1998;13:965–968. doi: 10.1002/mds.870130617. [DOI] [PubMed] [Google Scholar]
- 7.Eisa M, Singer C, Sengun C, Russel A, Jabbari B, Papapetropoulos S. Treatment of painful limbs/moving extremities with botulinum toxin type A injections. Eur Neurol. 2008;60:104–106. doi: 10.1159/000138962. [DOI] [PubMed] [Google Scholar]
- 8.Funakawa I, Mano Y, Takayanagi T. Painful hand and moving fingers: a case report. J Neurol. 1987;234:342–343. doi: 10.1007/BF00314292. [DOI] [PubMed] [Google Scholar]
- 9.Guieu R, Sampiéri F, Pouget J, Guy B, Rochat H. Adenosine in painful legs and moving toes syndrome. Clin Neuropharmacol. 1994;17:460–469. doi: 10.1097/00002826-199410000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Guieu R, Tardy-Gervet MF, Blin O, Pouget J. Pain relief achieved by transcutaneous electrical nerve stimulation and/or vibratory stimulation in a case of painful legs and moving toes. Pain. 1990;42:43–48. doi: 10.1016/0304-3959(90)91090-6. [DOI] [PubMed] [Google Scholar]
- 11.Guimarães J, Santos L, Bugalho P. Painful legs and moving toes syndrome associated with Hashimoto’s disease. Eur J Neurol. 2007;14:343–345. doi: 10.1111/j.1468-1331.2006.01513.x. [DOI] [PubMed] [Google Scholar]
- 12.Ikeda K, Deguchi K, Touge T, Sasaki I, Tsukaguchi M, Shimamura M, Komatsu E, Takeuchi H, Kuriyama S. Painful legs and moving toes syndrome associated with herpes zoster myelitis. J Neurol Sci. 2004;219:147–150. doi: 10.1016/j.jns.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Jabbari B, Molloy FM, Erickson M, Floeter MK. Bilateral painful hand-moving fingers: electrophysiological assessment of the central nervous system oscillator. Mov Disord. 2000;15:1259–1263. doi: 10.1002/1531-8257(200011)15:6<1259::AID-MDS1032>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 14.Mitsumoto H, Levin KH, Wilbourn AJ, Chou SM. Hypertrophic mononeuritis clinically presenting with painful legs and moving toes. Muscle Nerve. 1990;13:215–221. doi: 10.1002/mus.880130308. [DOI] [PubMed] [Google Scholar]
- 15.Montagna P, Cirignotta F, Sacquegna T, Martinelli P, Ambrosetto G, Lugaresi E. “Painful legs and moving toes” associated with polyneuropathy. J Neurol Neurosurg Psychiatry. 1983;46:399–403. doi: 10.1136/jnnp.46.5.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mosek A, Rabey JM, Kushnir M, Korczyn AD. Painful calf, moving foot. Mov Disord. 1996;11:339–340. doi: 10.1002/mds.870110325. [DOI] [PubMed] [Google Scholar]
- 17.Nathan PW. Painful legs and moving toes: evidence on the site of the lesion. J Neurol Neurosurg Psychiatry. 1978;41:934–939. doi: 10.1136/jnnp.41.10.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okamoto S, Takegami T, Mano T. [Peculiar involuntary movement of the toes associated with discomfort of the foot, a case of so-called “painful legs and moving toes”] [in Japanese] Rinsho Shinkeigaku. 1974;14:829–834. [PubMed] [Google Scholar]
- 19.Okuda Y, Suzuki K, Kitajima T, Masuda R, Asai T. Lumbar epidural block for ‘painful legs and moving toes’ syndrome: a report of three cases. Pain. 1998;78:145–147. doi: 10.1016/S0304-3959(98)00129-8. [DOI] [PubMed] [Google Scholar]
- 20.Papapetropoulos S, Argyriou AA. Painful limbs/moving extremities. Acta Neurol Scand. 2008;117:224–230. doi: 10.1111/j.1600-0404.2007.00936.x. [DOI] [PubMed] [Google Scholar]
- 21.Papapetropoulos S, Singer C. Painless legs moving toes in a patient with Wilson’s disease. Mov Disord. 2006;21:579–580. doi: 10.1002/mds.20805. [DOI] [PubMed] [Google Scholar]
- 22.Pitagoras de Mattos J, Oliveira M, André C. Painful legs and moving toes associated with neuropathy in HIV-infected patients. Mov Disord. 1999;14:1053–1054. doi: 10.1002/1531-8257(199911)14:6<1053::AID-MDS1031>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 23.Pla ME, Dillingham TR, Spellman NT, Colon E, Jabbari B. Painful legs and moving toes associates with tarsal tunnel syndrome and accessory soleus muscle. Mov Disord. 1996;11:82–86. doi: 10.1002/mds.870110115. [DOI] [PubMed] [Google Scholar]
- 24.Sahashi K, Tsuchiya I, Iwase S, Ibi T, Mano T. [Clinical analyses on moving toes in “painful legs and moving toes”] [in Japanese] Rinsho Shinkeigaku. 1989;29:849–853. [PubMed] [Google Scholar]
- 25.Sanders P, Waddy HM, Thompson PD. An “annoying” foot: unilateral painful legs and moving toes syndrome. Pain. 1999;82:103–104. doi: 10.1016/S0304-3959(99)00030-5. [DOI] [PubMed] [Google Scholar]
- 26.Sandyk R. Neuroleptic-induced “painful legs and moving toes” syndrome: successful treatment with clonazepam and baclofen. Ital J Neurol Sci. 1990;11:573–576. doi: 10.1007/BF02337440. [DOI] [PubMed] [Google Scholar]
- 27.Schoenen J, Gonce M, Delwaide PJ. Painful legs and moving toes: a syndrome with different physiopathologic mechanisms. Neurology. 1984;34:1108–1112. doi: 10.1212/wnl.34.8.1108. [DOI] [PubMed] [Google Scholar]
- 28.Schott GD. “Painful legs and moving toes”: the role of trauma. J Neurol Neurosurg Psychiatry. 1981;44:344–346. doi: 10.1136/jnnp.44.4.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schwingenschuh P, Bhatia KP. Painful moving tongue in a patient with the painful legs moving toes syndrome. Mov Disord. 2008;23:1324–1325. doi: 10.1002/mds.22160. [DOI] [PubMed] [Google Scholar]
- 30.Shime N, Sugimoto E. Lumbar sympathetic ganglion block in a patient with painful legs and moving toes syndrome. Anesth Analg. 1998;86:1056–1057. doi: 10.1097/00000539-199805000-00029. [DOI] [PubMed] [Google Scholar]
- 31.Singer C, Papapetropoulos S. A case of painless arms/moving fingers responsive to botulinum toxin a injections. Parkinsonism Relat Disord. 2007;13:55–56. doi: 10.1016/j.parkreldis.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Spillane JD, Nathan PW, Kelly RE, Marsden CD. Painful legs and moving toes. Brain. 1971;94:541–556. doi: 10.1093/brain/94.3.541. [DOI] [PubMed] [Google Scholar]
- 33.Spurling RG, Scoville WB. Lateral rupture of the cervical intervertebral discs: a common cause of shoulder and arm pain. Surg Gynecol Obstet. 1944;78:350–358. [Google Scholar]
- 34.Sudo H, Ito M, Minami A. A moving middle finger. Lancet. 2003;361:2202. doi: 10.1016/S0140-6736(03)13774-9. [DOI] [PubMed] [Google Scholar]
- 35.Supiot F, Gazagnes MD, Blecic SA, Zegers de Beyl D. Painful arm and moving fingers: clinical features of four new cases. Mov Disord. 2002;17:616–618. doi: 10.1002/mds.10116. [DOI] [PubMed] [Google Scholar]
- 36.Takahashi H, Saitoh C, Iwata O, Nanbu T, Takada S, Morita S. Epidural spinal cord stimulation for the treatment of painful legs and moving toes syndrome. Pain. 2002;96:343–345. doi: 10.1016/S0304-3959(01)00479-1. [DOI] [PubMed] [Google Scholar]
- 37.Touge T, Ishibashi T, Kamoda M, Tsukaguchi M, Takeuchi H. [“Painful legs and moving toes” and muscle cramps spreading to the bilateral legs in a patient with alcoholic polyneuropathy] [in Japanese] Rinsho Shinkeigaku. 1998;38:762–766. [PubMed] [Google Scholar]
- 38.Uchihara T, Ichikawa T, Furukawa T, Tsukagoshi H. Myoclonus with burning sensation in legs that remits with sympathetic blockade. J Neurol Sci. 1990;100:161–164. doi: 10.1016/0022-510X(90)90028-L. [DOI] [PubMed] [Google Scholar]
- 39.Verhagen WI, Horstink MW, Notermans SL. Painful arm and moving fingers. J Neurol Neurosurg Psychiatry. 1985;48:384–385. doi: 10.1136/jnnp.48.4.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Villarejo A, Porta-Etessam J, Camacho A, González De La Aleja J, Martínez-Salio A, Penas M. Gabapentin for painful legs and moving toes syndrome. Eur Neurol. 2004;51:180–181. doi: 10.1159/000077669. [DOI] [PubMed] [Google Scholar]
- 41.Walters AS, Hening WA, Shah SK, Chokroverty S. Painless legs and moving toes: a syndrome related to painful legs and moving toes? Mov Disord. 1993;8:377–379. doi: 10.1002/mds.870080325. [DOI] [PubMed] [Google Scholar]
- 42.Wulff CH. Painful legs and moving toes: a report of 3 cases with neurophysiological studies. Acta Neurol Scand. 1982;66:283–287. doi: 10.1111/j.1600-0404.1982.tb04526.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.