Summary
A case of dural sinus thrombosis complicated with heparin induced thrombocytopenia and thrombosis (HITT) is presented. Interventional neuroradiologic procedures have potential risks of this devastating complication that is related with heparin. Clinical features and pathophysiologic mechanisms of HITT are discussed.
Key words: dural sinus trombosis, thrombocytopenia, thrombosis
Introduction
Heparin has been empirically used during many endovascular procedures to prevent thromboembolic and ischemic complications. It has also been used during diagnostic angiography in cases of high-risk patients such as hypercoagulable state or patients with intracranial vasculitis. Despite its clinical benefit, the usage of heparin also has some important complications such as hemorrhage, heparin induced thrombocytopenia and thrombosis (HITT), heparin associated osteoporosis, eosinophillia, skin reactions, and alopecia1. The incidence of HITT is reported to be 0.3 ~ 3%2-4. However, in spite of HITT's relatively high frequency, there have been few reports5,6 regarding this complication related to angiography or endovascular therapy. We present a case of dural sinus thrombosis complicated with HITT after attempted dural sinus thrombolysis.
Case Report
A 50 year-old lady presented with increasing frequency of headache and difficulty in expressing herself. Her past medical history revealed migraine and borderline hypertension. She was non-smoker, didn't drink alcohol and had no history of a prior neurologic problem. Neurologic examinations showed right side motor weakness and paresthesia. Brain CT showed a left transverse sinus thrombosis (figure 1) Carotid ultrasonograhy showed less than 40% narrowing of left internal carotid artery due to atherosclerotic plaque. Complete blood cell count showed mild polycythemia (Hgb = 159g/L, Hct = 0.498, WBC count = 8200/mm3, Platelet count = 304,000/mm3). Treatment of dural sinus thrombosis was intravenous heparin therapy, started with 3000 unit of bolus injection followed by continuous infusion (200 units/hour). On 13th hospital day, she developed right hemiparesis, aphasia, and her consciousness level was deteriorated to stuporous condition. She was transferred to our hospital for possible endovascular dural sinus thrombolysis.
Figure 1.
Brain CT shows curvilinear high attenuated lesion on proximal left transverse sinus and torcular (arrow) suggesting dural sinus thrombosis.
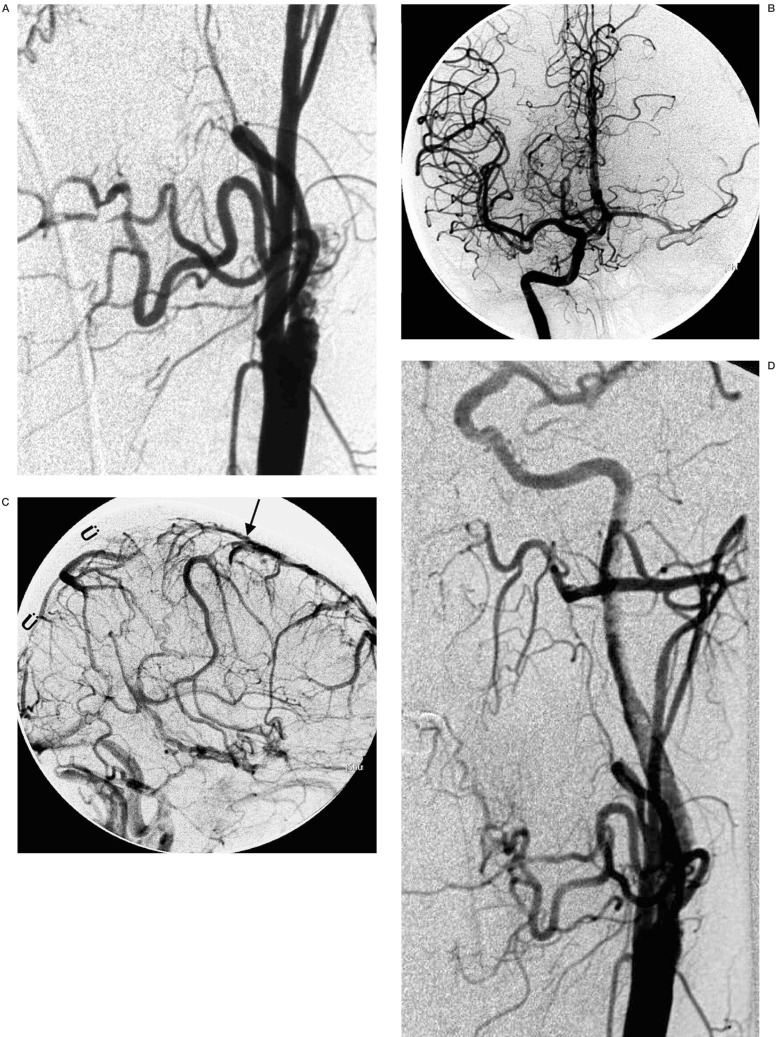
After placement of femoral arterial and venous sheaths, we gave her 6000 units of heparin [about 100 units/body weight (Kg)] as a bolus. At angiography the left internal carotid artery was totally occluded with thrombus (figure 2A) and left hemisphere was supplied by right internal carotid artery through anterior communicating artery (figure 2B).
Figure 2.
A) Left common carotid angiography (AP view) shows total occlusion of left internal carotid artery. B) Right internal carotid angiography (AP view) demonstrates that left hemisphere is supplied by the right side through anterior communicating artery. C) Right internal carotid artery angiography (lateral view) shows the patent anterior 1/3 of superior sagittal sinus (SSS) (arrow) with well-developed venous collaterals and occlusion of the distal SSS (arrow heads). D) Left common carotid angiography (AP view) shows that the left internal carotid artery is open with reconstitution of ante-grade flow. Note, the filling defects in the proximal internal carotid artery.
The venous phase of right carotid angiogram demonstrated partially thrombosed superior sagittal sinus with well-developed venous collaterals (figure 2C). Dural sinus thrombolysis was nor done, because her dural sinus was partially thrombosed and venous collateral pathways were well developed. Arterial thrombolysis was not performed either, because it was more than 24 hours since her recent deterioration. We repeated left common carotid angiogram to evaluate extracranial to intracranial collaterals about 30 minutes later. Surprisingly, we found her left internal carotid artery was opened (figure 2D). She woke up from general anesthesia uneventfully and her right hemiparesis was improved.
Her neurologic condition deteriorated on the next day (Day 14th) with the development of a complete right hemiplegia and decreased level of consciousness. The platelet count was decreased to 61,000 /mm3. Because the platelet count had decreased rapidly and the brain infarction had progressed despite anti-coagulation therapy, HITT was suspected. The heparin was discontinued immediately and the anti-coagulation agent was changed to Liperidin.
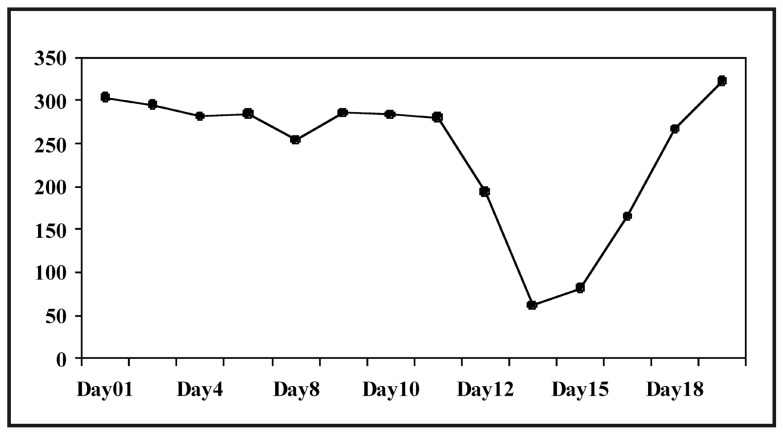
Her platelet count recovered to 165,000/mm3 on Day 16th and to 322,000/mm3 on Day 19th. The temporal change of her platelet count is shown on figure 3. The ELISA test for heparin induced antibody for platelet factor IV was positive confirming the diagnosis of HITT. Her mild polycythemia was investigated by bone marrow biopsy and a diagnosis of a myeloproliferative disease was made.
Figure 3.
Temporal changes of the platelet counts are plotted. The platelet counts start to decrease on the 11th day after heparinization. The black arrow indicates the 13th day when the patient's clinical condition deteriorated. The platelet counts increase as soon as the heparinization is discontinued.
Discussion
Heparin induced thrombocytopenia and associated paradoxical thrombotic events typically appear five or more days after the initiation of therapeutic or prophylactic unfractionated heparin therapy 2. The mechanism of HITT is that the antibodies specific for heparin and platelet factor IV (PF4) complex, either IgG or IgM, activate normal platelets and cause them to aggregate and develop a consumptive thrombocytopenia. These antibodies also react with glycosaminoglycans-PF4 complexes on endothelial cells and present with paradoxic intravascular thrombosis7. This untoward effect can also happen after very brief and low-dose heparin exposure such as intra-operative arterial catheter flushing8. Therefore, most all of interventional neuroradiology (INR) patients have some risks of developing HITT. Pre-existing vascular endothelial damages such as previous catheterization or surgical trauma might further potentiate HITT9.
INR patients who have multi-staged embolizations or multiple follow-up angiographies may have a higher risk of developing HITT. However, to date, there have been no HITT reports that related to INR procedures. In our experience of more than 1000 consecutive INR procedures, this is the first case of HITT that was confirmed clinically and serologically. Therefore, there may be differences in the incidence of HITT between the INR patients and the patients who receive therapeutic or prophylactic dose of heparin.
Thrombocytopenia in HITT has been defined1,2,10 as a platelet count of less than 150,000 /mm3 or a platelet decrease of more than 50% of the initial count after beginning of heparin therapy. However, because the prognosis of HITT is so poor, prompt clinical suspicion of HITT is important for the patients who develop unexplained platelet count drop about 20 to 30%1. Our case developed arterial thrombosis. In general, venous thrombosis such as pulmonary embolism, venous sinus thrombosis or deep venous thrombosis is more frequently associated with HITT than arterial thrombosis 11. However, among the patients with HITT presenting with neurologic complications (about 9% of HITT), arterial thrombosis is more frequent than venous thrombosis 10.
One of the interesting findings of our case is the re-opening of the previously occluded left internal carotid artery after heparin bolus injection only. Delayed extensive multi-focal posterior fossa infarctions developed suggesting aggravation of the arterial occlusions. The reopening of the internal carotid artery can be explained by characteristics of an antigen-antibody reaction. Initial occlusion of the carotid artery can be explained by the so called “white clot syndrome” of HITT 12. Because HITT process is an immune mediated antigen-antibody reaction, it can be inhibited when we infuse large amount of antigen (heparin). And there is no evidence that the HITT process affects the intrinsic fibrinolytic system. Therefore, our explanation for the re-opening of left carotid artery can be summarized: the bolus injection of heparin initially created an antigen excess state; the antigen excess state inhibited the formation of additional “white clot”; and the activated intrinsic fibrinolytic system thrombolysed the “white clot” opening the carotid artery. However, corresponding antibody production due to the antigen excess state resulted more extensive arterial occlusion and deterioration of her clinical status.
Although the incidence of HITT during and after usual INR procedures is low, it is important to understand the mechanism of HITT for early diagnosis and proper management of this devastating complication.
References
- 1.Walenga JM, Bick RL. Heparin-induced thrombocytopenia, paradoxical thromboembolism, and other side effects of heparin therapy. Med Clin North Am. 1998;82:635–658. doi: 10.1016/s0025-7125(05)70015-8. [DOI] [PubMed] [Google Scholar]
- 2.Warkentin TE, Levine MN, et al. Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractionated heparin. N Engl J Med. 1995;332:1330–1335. doi: 10.1056/NEJM199505183322003. [DOI] [PubMed] [Google Scholar]
- 3.Jackson MR, Gillespie DL, et al. The incidence of heparin-induced antibodies in patients undergoing vascular surgery: a prospective study. J Vasc Surg. 1998;28:439–444. doi: 10.1016/s0741-5214(98)70129-6. [DOI] [PubMed] [Google Scholar]
- 4.Kappers-Klunne MC, Boon DM, et al. Heparin-induced thrombocytopenia and thrombosis: a prospective analysis of the incidence in patients with heart and cerebrovascular diseases. Br J Haematol. 1997;96:442–446. doi: 10.1046/j.1365-2141.1997.d01-2056.x. [DOI] [PubMed] [Google Scholar]
- 5.van Sambeek MR, Segeren CM, et al. Endovascular repair of an extracranial internal carotid artery aneurysm complicated by heparin-induced thrombocytopenia and thrombosis. J Endovasc Ther. 2000;7:353–358. doi: 10.1177/152660280000700502. [DOI] [PubMed] [Google Scholar]
- 6.Seidensticker D, Wilcox J, Gagne P. Treatment of May-Thurner syndrome with catheter-directed thrombolysis and stent placement, complicated by heparin-induced thrombocytopenia. Cardiovasc Surg. 1998;6:607–613. doi: 10.1016/s0967-2109(98)00086-6. [DOI] [PubMed] [Google Scholar]
- 7.Visentin GP, Ford SE, et al. Antibodies from patients with heparin-induced thrombocytopenia/thrombosis are specific for platelet factor 4 complexed with heparin or bound to endothelial cells. J Clin Invest. 1994;93:81–88. doi: 10.1172/JCI116987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slaughter TF, Greenberg CS. Heparin-associated thrombocytopenia and thrombosis: implications for perioperative management. Anesthesiology. 1997;87:667–675. doi: 10.1097/00000542-199709000-00029. [DOI] [PubMed] [Google Scholar]
- 9.Makhoul RG, Greenberg CS, McCann RL. Heparin-associated thrombocytopenia and thrombosis: a serious clinical problem and potential solution. J Vasc Surg. 1986;4:522–528. doi: 10.1067/mva.1986.avs0040522. [DOI] [PubMed] [Google Scholar]
- 10.Pohl C, Harbrecht U, et al. Neurologic complications in immune-mediated heparin-induced thrombocytopenia. Neurology. 2000;54:1240–1245. doi: 10.1212/wnl.54.6.1240. [DOI] [PubMed] [Google Scholar]
- 11.Warkentin TE, Kelton JG. A 14-year study of heparininduced thrombocytopenia. Am J Med. 1996;101:502–507. doi: 10.1016/s0002-9343(96)00258-6. [DOI] [PubMed] [Google Scholar]
- 12.Melanson SW, Silver B, Heller MB. Deep vein thrombosis, pulmonary embolism, and the white clot syndrome. Am J Emerg Med. 1996;14:558–560. doi: 10.1016/S0735-6757(96)90098-4. [DOI] [PubMed] [Google Scholar]