Abstract
Cerebellar ataxias are a group of disabling neurological disorders. Patients exhibit a cerebellar syndrome and can also present with extra-cerebellar deficits, namely pigmentary retinopathy, extrapyramidal movement disorders, pyramidal signs, cortical symptoms (seizures, cognitive impairment/behavioural symptoms), and peripheral neuropathy. Recently, deficits in cognitive operations have been unraveled. Cerebellar ataxias are heterogeneous both at the phenotypic and genotypic point of view. Therapeutical trials performed during these last 4 decades have failed in most cases, in particular because drugs were not targeting a deleterious pathway, but were given to counteract putative defects in neurotransmission. The identification of the causative mutations of many hereditary ataxias, the development of relevant animal models and the recent identifications of the molecular mechanisms underlying ataxias are impacting on the development of new drugs. We provide an overview of the pharmacological treatments currently used in the clinical practice and we discuss the drugs under development.
Keywords: Cerebellum, ataxias, dominant, recessive, X-linked, therapy.
I. INTRODUCTION
With the advent of sensitive techniques such as magnetic resonance imaging (MRI), cerebellar ataxias (CAs) are being growingly recognized [11, 36, 57, 145, 165, 224]. There is a medical need to develop effective therapies in this group of disabling disorders for which no cure is currently available. For the first time, novel therapeutics aiming to target deleterious pathways are under development [100, 135, 214, 219]. The deciphering of the molecular mechanisms underlying CAs is a preliminary and unavoidable step to reach the goal of the cure [135]. Major advances in our current understanding of the pathogenesis of cerebellar ataxias have originated in particular from the development of relevant animal models which mimic the phenotype observed in human [90, 135, 166, 167, 173, 185]. Advances in brain neuroimaging have also improved drastically the early detection and follow-up of the course of cerebellar disorders [51, 77, 113]. This paper reviews the most common causes of CAs, the therapies used in the past and the treatments under assessment both at the experimental and clinical level. The main cerebellar disorders will be briefly presented for a matter of clarity.
II. CEREBELLAR ATAXIAS: DESCRIPTION
CAs can affect the medial zone (vermal zone), the intermediate zone (paravermal zone) and/or the lateral zone of the cerebellum [133]. The main symptoms are listed in Table 1. Cerebellar patients are typically clumsy during voluntary movements involving proximal or distal joints [64, 84, 209]. Cerebellum is also involved in several forms of motor learning [121, 125, 207]. CAs are a heterogeneous group of disabling disorders characterized by a lack of coordination and imbalance [114]. Patients exhibit various combinations of oculomotor deficits, dysarthria, dysmetria and kinetic tremor [138, 220]. Recently, the association of cerebellar lesions and neuropsychiatric symptoms has been underlined (Table 2). It has been suggested that the cerebellum is involved in the pathogenesis of depression, schizophrenia and autism [58]. For instance, autism is associated with decreased densities of Purkinje neurons [124, 175, 228]. Some ataxic diseases present with marked cognitive dysfunction [181]. A typical example is SCA17, a highly heterogeneous disease with cognitive impairment in 80 to 100 % of cases [17, 65, 132, 239]. CAs can be divided in sporadic and inherited disorders [135]. Table 3 lists the principal disorders involving the cerebellum in young adults and for whom pharmacological treatments have been or are being evaluated [135].
Table 1.
Main Clinical Deficits in Cerebellar Patients
| Vermal Zone | Paravermal Zone | Lateral Zone |
|---|---|---|
| Oculomotor deficits | Dysarthria | Oculomotor deficits |
| Dysarthria | Dysarthria | |
| Head tilt | Dysmetria | |
| Ataxia of stance/gait | Kinetic tremor | |
| Hypotonia | ||
| Dysdiadochokinesia | ||
| Decomposition of movements | ||
| Ataxia of stance/gait | ||
Table 2.
Neuropsychiatric Symptoms in Cerebellar Disorders
| Domain | Symptoms |
|---|---|
| Attention | Distractibility |
| Hyperactivity | |
| Compulsive behaviour | |
| Perseveration | |
| Difficulties for shifting attention | |
| Obsessional behavior | |
| Emotion | Impulsiveness, disinhibition |
| Anxiety, agitation | |
| Pathological laughing and crying | |
| Anhedonia | |
| Depression | |
| Dysphoria | |
| Social skill set | Aggression |
| Irritability | |
| Passivity | |
| Difficulties with social interactions | |
| Psychosis | Illogical thinking |
| Hallucinations | |
| Lack of empathy | |
| Autism spectrum | Stereotypies |
| Avoidant behavior | |
| Sensory overload | |
Adapted from Schmahmann and Pandya (2008) [182].
Table 3.
Differential Diagnosis of Cerebellar Ataxias in Young Adults
| Spinocerebellar ataxia (SCA) |
| Episodic ataxia (EA) |
| Friedreich ataxia (FRDA) |
| Wilson disease |
| Primary tumor |
| Paraneoplastic ataxia |
| Infectious/para-infectious |
| Immune ataxia |
| Toxics (alcohol) |
| Endocrine diseases |
| Leukodystrophies |
| Mitochondrial disorders |
II.1. Cerebellar Circuitry: Composition, Neurotransmitters and Receptors
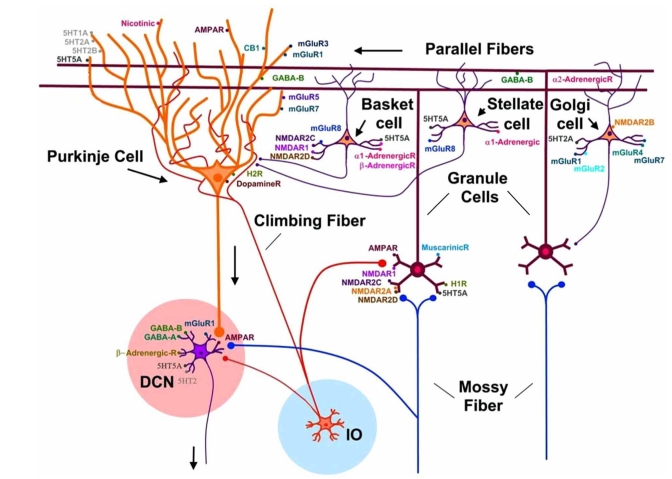
Cerebellum is the region of the brain containing the highest number of neurons [132]. Cerebellar circuitry is highly complex. The cerebellum is composed of a mantle of grey zone (cortex) surrounding white matter, in which cerebellar nuclei are disposed [49]. Despite an apparent homogeneous structure, cerebellum is divided into several functional zones [208]. Three rostro-caudal longitudinal zones have been identified in the cerebellar cortex: a vermal zone projecting to the fastigial nucleus medially, an intermediate zone projecting to the interpositus nucleus and a lateral zone projecting to the dentate nucleus [73]. Two categories of inputs reach cerebellar cortex: mossy fibers issued from brainstem nuclei and climbing fibers originating from the inferior olivary complex [86]. Cerebellar cortex is composed of Purkinje cells, granule cells and inhibitory interneurons (Fig. 1). Purkinje neurons exert an inhibitory effect upon cerebellar nuclei, which represent the sole output of cerebellar circuitry. There is increasing evidence of a functional asymmetry of the cerebellum, not only for motor but also for higher cognitive functions and sensory discrimination regarding processes like pain [18, 26, 85, 196, 232]. Another major feature of the cerebellar circuitry is the rostrocaudal and mediolateral subdivision of the cerebellar cortex into complex arrays of transverse zones and parasagittal stripes [3, 35, 82]. The most extensively studied marker for cerebellar compartmentation is the antigen zebrin II, an epitope on the respiratory isoenzyme aldolase C [156]. Zebrin II is expressed by a subset of Purkinje neurons forming parasagittal stripes which are highly reproducible between subjects and across species [156]. The molecular mechanisms which govern the distribution and organization of cerebellar zones are being unraveled and will probably lead to novel therapies [192].
Fig. (1).
Representation of the connectivity of cerebellar neurons and expression of receptors. Two categories of inputs reach the cerebellar cortex: (1) the mossy fibers targeting granule cells and cerebellar nuclei (DCN), and (2) the climbing fibers originating from the inferior olivary complex (IO) and projecting to cerebellar nuclei and Purkinje neurons. Granule cells give rise to parallel fibers which make numerous synapses with dendritic spines of Purkinje cells. Inhibitory interneurons of the cerebellar cortex include basket cells, stellate cells and Golgi cells. Abbreviations: AMPA: aminohydroxymethylisoxazoleproprionate, NMDA: N-methyl-D-aspartate, mGluR. GABAA: GABA-A receptor, GABAB: GABA-B receptor, 5-HT: serotonin, CB1: cannabinoid 1 receptor.
Table 4 lists the neurotransmitters and neuromodulators of cerebellar circuitry. Distribution of the main receptors is illustrated in Fig. (1). Glutamate is a transmitter for both the mossy fiber and the climbing fiber system [191]. The postsynaptic element of the synapse mossy fiber-granule cell presents N-methyl-D-aspartate (NMDA) and aminohydroxymethylisoxazoleproprionate (AMPA) receptors [199]. Some mossy fibers contain choline acetyl transferase and use acetylcholine (Ach) as transmitter [110]. Climbing fibers are enriched in glutamate and can retrogradely transport aspartate to the inferior olive [94]. Glutamate is also the transmitter of parallel fibers which make numerous synapses with dendritic spines. Purkinje cell spines contain high densities of AMPA receptors [230]. Purkinje cells are enriched in glutamic acid decarboxylase (GAD), a GABA synthesizing enzyme [16]. Both ionotropic GABA receptors (GABA-A) and metabotropic GABA receptors (GABA-B) are highly expressed in the cerebellum. GABA-B receptors are particularly enriched in the cerebellar cortex [118, 137, 218]. At the cellular level, the GABA-B1 and GABA-B2 subunits are distributed in most neurons of the adult cerebellar cortex, but in particular at high levels in Purkinje neurons [105, 130].
Table 4.
Main Neurotransmitters and Neuromodulators of Cerebellar Circuitry
| Glutamate |
| Aspartate |
| GABA |
| Glycine |
| Taurine |
| Amines (Serotonin, Noradrenaline, Acetylcholine, Dopamine, Histamine) |
| Nitric oxide |
| Peptides |
| Endocannabinoids |
Taurine is also enriched in Purkinje cells and is considered to play a role in osmoregulation [88]. Recent studies have demonstrated that retrograde messengers, the endocannabinoids, are released by Purkinje cells [179]. Type 1 cannabinoid receptors (CB1Rs) are expressed presynaptically at all synaptic inputs to the Purkinje neurons [206]. A high proportion of CB1Rs are also located at inhibitory interneurons throughout the molecular layer. Labelling studies are consistent with their presence in basket cell and stellate cell inhibitory interneurons [48].
GABA is the predominant transmitter of cerebellar interneurons (basket cells, stellate cells, Golgi cells, Lugaro cells). Glycine is also supposed to be involved in the inhibitory processes controlled by cerebellar interneurons [19]. The unipolar brush cells are an exception in the population of interneurons, since they are glutamatergic.
Aminergic fibers are found in the 3 layers of the cerebellar cortex (Table 5). Serotoninergic fibers are distributed in all parts of the cerebellum, except lobule X [227]. Serotonin inhibits glutamate release from mossy fibers, tunes cellular responses to GABA and regulates the activity of glial GABA transporters [189]. Local application of serotonin modulates the firing rate of Purkinje cells both in vivo and in vitro. Lugaro cells are also responsive to serotonin [226]. The noradrenergic input modulates the responses of cerebellar neurons to GABA and glutamate. Interestingly, a genuine dopaminergic innervation is also found in the cerebellum [189]. Dopamine and dopamine transporters are found in all the layers of the cerebellar cortex, with the highest densities in the molecular layer [44, 162]. Dopamine immunoreactive axons are found in the cerebellar vermis of primates, primarily innervating the granule cell layer and the adjacent Purkinje neurons [89, 146]. Biochemical investigations have shown active dopamine uptake into cerebellar synaptosomes and release of endogeneous dopamine by the cerebellum [55, 70]. Radioligand binding studies have demonstrated that dopamine receptors 1-5, which belong to the D1-like and D2-like superfamilies, are expressed in the cerebellum [28, 45]. D1 and D5 receptors are localized in Purkinje neurons and the molecular layer, D2 receptors are found in all layers, D3 receptors are principally found in Purkinje neurons and molecular layer of lobules IX and X, and D4 receptors are concentrated in the molecular layer [70]. Levels of dopamine transporters (DAT) binding are a good indicator of the extracellular dopamine content. DAT bindings change in parallel to the concentrations of dopamine in the extra-cellular space [161]. DAT knockout mice (DAT -/-) are hyperactive [237]. Extra-cellular dopamine levels are increased in the striatum, causing a depression in mRNA levels of both D1 and D2 receptors and decreased stores of dopamine [71, 96]. Interestingly, several lines of evidence suggest that cerebellar dopaminergic system is a potential target of drugs of abuse [70]. Systemic administration of d-amphetamine and cocaine causes a dose-response increase in c-fos expression in the rat cerebellum, an effect which is reduced by pretreatment with SCH23390, a D1 receptor antagonist [59]. Moreover, a chronic treatment with cocaine sensitizes c-fos induction in the cerebellum via D1 and D2 receptors, and d-amphetamine increases the density of D2-like receptors [27, 39, 111]. Studies with cerebellar membrane preparations have shown that the [3H]GBR12935 specific binding is sensitive to mazindol, a specific dopamine transporter antagonist, and dopamine. Mazindol inhibits 15-20 % of the total specific binding with high affinity and the remaining 80-85 % with low affinity [44]. A complementary inhibitory pattern is observed with cis-flupentixol. Saturation experiments in presence of cis-flupentixol have revealed a specific binding site with a Kd value similar to the value in striatal preparations. Nevertheless, the affinity of dopamine for the [3H]GBR12935 specific binding is lower in the cerebellum, suggesting different three-dimensional conformations and ligand binding properties.
Table 5.
Sites of Projections of Aminergic Pathways in the Cerebellum
| Amine | Site of Projection in the Cerebellum |
|---|---|
| Serotonin | Cerebellar cortex: dense plexus in granular and Purkinje cell layer |
| Cerebellar nuclei: dense plexus | |
| Noradrenaline | Cerebellar cortex: around glomeruli and around dendrites of Purkinje cells |
| Cerebellar nuclei | |
| Acetylcholine | Cerebellar cortex |
| Cerebellar nuclei | |
| Dopamine | Cerebellar cortex |
| Histamine | Cerebellar cortex |
The hypothalamus projects to the cerebellum using histamine as transmitter [50]. Histaminergic fibers are found in all cortical layers of the cerebellum. H1 receptors are preferentially expressed on Purkinje cell dendrites [213].
Activation of NMDA receptors in the cerebellum stimulates the production of nitric oxide (NO) [60]. Granule cells are a main source of NO [131]. Granule cells, parallel fibers and basket cells are equipped with the neuronal isoform of NO synthase (nNOS). Release of NO from parallel fibers is involved in long-term depression (LTD) [157]. Production of cyclic guanosine monophosphate (cGMP) results indirectly from NO production [76]. cGMP immunoreactivity is found mainly in Bergmann glia and astrocytes [198].
II.2. Inherited CAs
The inherited ataxias are related to a genetic deficit (Table 6). They can be divided into four groups: autosomal dominant ataxias, autosomal recessive ataxias, mitochondrial ataxias and X-linked ataxias [14, 112, 115, 135, 159].
Table 6.
Gene Mutations in Inherited Ataxias
| Autosomal Dominant Spinocerebellar Ataxias | ||
|---|---|---|
| Type | Gene Mutation | Protein |
| SCA1 | CAG (35-83) | Ataxin-1 |
| SCA2 | CAG (34-750) | Ataxin-2 |
| SCA3 | CAG (56-86) | Ataxin-3(MJD1) |
| SCA4 | - | - |
| SCA5 | Missense mutations | Spectrin |
| SCA6 | CAG (19-33) | Calcium channel, voltage-dependent, P/Q, α-A subinit |
| SCA7 | CAG (41-306) | Ataxin-7 |
| SCA8 | CTG (80-300) | Ataxin-8 |
| SCA10 | ATTCT (800-4500) | Ataxin-10 |
| SCA11 | TTBK2 (1329insA, 1284_1285delAG) | Tau Tubulin kinase-2 |
| SCA12 | CAG (66-93) | Protein phosphatase 2, regulatory subunit B, β-isoform |
| SCA13 | KCNC3 (R420H, F448L) | Voltage-gated potassium channels, shaw-related subfamily, member 3 |
| SCA14 | Missense mutations | Protein kinase C, g-polypeptide |
| SCA15 | ITPR1 (DEL EX1-48, P1059L) | Type 1 inositol 1, 4, 5-triphosphate receptor |
| SCA16 | - | - |
| SCA17 | CAG/CAA (43-63) | TATA box-binding protein |
| SCA18 | - | - |
| SCA19 | - | - |
| SCA20 | - | - |
| SCA21 | - | - |
| SCA22 | - | - |
| SCA24 | - | - |
| SCA25 | - | - |
| DRPLA | CAG (48-93) | Atrophin-1 |
| SCA27 | FGF 14 | Fibroblast growth factors |
| SCA31 | PLEKHG4 (16C-T) | Puratrophin-1 |
| FRDA | 9q13 | Frataxin |
| Familial coenzyme Q10(CoQ10) deficiency | CoQ10 | CoQ10 |
| Autosomal-recessive spastic ataxia of Charlevoix-Saguenay (ARSACS) | 13q12 | Sacsin |
| Mitochondrial recessive ataxic syndrome (MIRAS) | Polymerase-γ | |
| Marinesco-Sjögren syndrome | 5q32 | SILI |
| Ataxia with isolated vitamin E deficiency (AVED) | 8q13 | Alpha-tocopherol transfer protein (α-TTP) |
| Abetalipoptoteinemia(Bassen-Kornzweig syndrome) | 4q22-q24 | Microsomal triglyceride transfer protein |
| Hereditary motor and sensory neuropathy type IV (HMSM IV), Refsum disease | 10pter-p11.2 | Phytanoyl-CoA hydroxylase |
| Cerebrotendinous xanthomatosis | 2q33-qter | Cytocrome P-450, subfamily VVVIIA, polypeptide 1 (sterol 27-hydroxylase) |
| Metachromatic leucodystrophy | 22q13 | Arylsulfatase 1 |
| Niemann-Pick type C | 18q11-121 | NPC1 protein |
| GM2-gangliosidosis (Tay-Sachs disease) | 15q23-24 | Hexosaminidase 1 |
| Chorea-acanthocytosis | 9q21 | Chorein |
| Wilsons disease | 13q14-21 | ATPase Cu transporting beta-polypeptide |
| Aceruloplasminaemia | 3q23-q24 | Ceruloplasmin |
| Ataxia telangiectasia | 11q22.3 | ATM |
| Ataxia-telangiectasia-like disorder (ATLD) | 11q21 | MREIIA |
| Ataxia with oculomotor apraxia 1 (AOA1/EAOH) | 9p13 | Aprataxin |
| Ataxia with oculomotor apraxia 2 (AOA2) | 9q34 | Senataxin |
II.2.1. Autosomal Dominant Ataxias (ADCAs)
Onset varies from infancy to the elderly. In most cases, symptoms start between the ages of 20 and 60 [135].
Spinocerebellar Ataxias (SCAs)
SCAs are a set of genetic and clinically heterogeneous diseases which share the feature of progressive ataxia [135, 184]. They have an incidence of 1 to 4 affected every 100.000 [215]. SCAs are classified genetically according to a specific mutation or mapped locus, and also according to clinical findings [207]. Dentatorubropallidoluysian atrophy (DRPLA) and ataxia associated with fibroblast growth factor 14 (FGF14) mutation are also considered in this group [136].
The majority of known mutations involve a sequence of CAG trinucleotide repeats within the coding tract in the respective gene. This is the case for SCA1, SCA2, SCA3, SCA6, SCA7, SCA17, and DRPLA, while a CTG repeats is present in SCA8 [207]. Trinucleotide repeats are associated with an abnormal polyglutamine accumulation and formation of nuclear aggregates [155]. A pentanucleotide repeat expansion ATTCT is associated with SCA10 [142]. SCA5, SCA13, SCA14, and 16q22-linked autosomal dominant cerebellar ataxia (ADCA) are characterized by point mutations [108, 147, 158, 229]. Patients exhibit various combinations of cerebellar and extra-cerebellar deficits (Table 7).
Table 7.
Clinical Presentations of Spinocerebellar Ataxias
| Purecerebellar syndrome | SCA5, SCA6, SCA11, SCA26 |
| Cerebellar ataxia plus: | |
| Cognitive impairment/ behavioural symptoms | SCA1, SCA2, SCA3, SCA10, SCA12, SCA13, SCA14, SCA17, SCA19, SCA21, SCA-FGF14, DRPLA |
| Seizures | SCA10, SCA17, DRPLA |
| Eyes/oculomotor deficits | |
| Slow saccades | SCA1, SCA2, SCA3, SCA7, SCA28 |
| Down-beat nystagmus | SCA6 |
| Ophthalmoparesia | SCA1, SCA2, SCA3, SCA28, SCA30 |
| Ocular dyskinesia | SCA10 |
| Pigmentary retinopathy | SCA7 |
| Movement disorders | |
| Parkinsonism | SCA1, SCA2, SCA3, SCA12, SCA17, SCA21 |
| Dystonia | SCA3, SCA14, SCA17 |
| Tremor | SCA8, SCA12, SCA16, SCA19, SCA20 |
| Dyskinesias | SCA-FGF14 |
| Myoclonus | SCA2, SCA14, SCA19, DRPLA |
| Chorea | SCA1, SCA17, DRPLA |
| Myokymia | SCA5 |
| Pyramidal signs | SCA1, SCA2, SCA3, SCA4, SCA7, SCA8, SCA10, SCA11, SCA12, SCA13, SCA14, SCA15, SCA28, SCA30 |
| Peripheral neuropathy | SCA1, SCA2, SCA3, SCA4, SCA6, SCA8, SCA-FGF14, SCA12, SCA18, SCA22, SCA25 |
II.2.2. Episodic Ataxias (EAs)
EAs are a group of diseases underlying a monogenic mutation (EA 1-7; Table 8) [102]. The onset of symptoms is generally in the childhood [100]. Anxiety and fatigue increase the susceptibility to an attack [30]. EA-2 is the most common episodic ataxia [34]. Patients may exhibit myokymia, nystagmus, vertigo, and ataxia [101, 169]. EA-1 is characterized by short attacks of incoordination and dysarthria (slurred speech).
Table 8.
Genetics of Episodic Ataxias (EAs)
| Type of Ataxia | Gene Mutation and Function |
|---|---|
| Type 1(EA-1) | KCNA1-deficiency in voltage-gated potassium channel function Autosomal dominant |
| Type 2 (EA2) | CACNA1A-subunit of P/Q type calcium channel; different mutations in same gene lead to SCA6 and familial hemiplegic migraine CACNB4-dihydropyridine-sensitive L-type calcium channel Autosomal dominant |
| Type 3(EA-3) | Linked to 1q42 |
| Type 4 (EA-4) | Unknown |
| Type 6 (EA-6) | Unknown |
| Type 7 (EA-7) | 19q13 |
Adapted from Brust (2006) [31].
II.2.3. Autosomal Recessive Ataxias (ARCAs)
ARCAs are disorders characterized by variable combinations of central and peripheral nervous system involvement [57]. Dysfunctions of other organs are found in some ARCAs [220]. The most common ARCA is Friedreich’s ataxia (FRDA). Other recessive ataxias include ataxia-telangiectasia, ataxia with ocular motor apraxia (AOA), ataxia with vitamin E deficiency (AVED), ataxia with CoQ10 deficiency, abetalipoproteinemia, early-onset cerebellar ataxia with retained tendon reflexes, infantile onset spinocerebellar ataxia, Marinesco-Sjogren syndrome and spastic ataxia of Charlevoix-Saguenay [30, 135]. There are numerous additional types of recessive ataxias worldwide, identified in a few families only. The most common ARCAs are briefly described below.
Friedreich’s ataxia (FRDA) is due to a pathological GAA triplet expansion within the first intron of the FXN gene, codifying for the mitochondrial protein frataxin [32, 140]. It is a severe neurodegenerative disorder, with an incidence of 1/40.000 [43]. The clinical picture is characterized by gait and limb ataxia, dysarthria, areflexia, proprioceptive loss and Babinski sign [62]. Patients can also develop cardiomyopathy and diabetes mellitus [62]. There is a consensus that FRDA is a disorder of iron homeostasis at the mitochondrial level [66, 115].
Cerebellar ataxia with muscle Coenzyme Q10 deficiency is a heterogeneous disorder. The cerebellar form presents with ataxia and cerebellar atrophy [148, 150, 122]. Coenzyme Q10 (CoQ10; ubiquinone), is an electron carrier critical for electron transfer within the mitochondrial respiratory chain (see section IV.2).
Ataxia with Vitamin E deficiency (AVED), presents as a FRDA-like syndrome [6, 20]. The 744deletionA is the most common mutation. Abetalipoproteinaemia (ABL) is characterized by a deficit in the low density apolipoprotein-B (VLDLs). Symptoms are similar to AVED.
Ataxia-telangiectasia is the most frequent ARCA in children [67, 68]. First symptoms usually begin between 2-8 years. A mutation within the ATM gene results in a deficit in the DNA repair [193].
Ataxia with oculomotor apraxia (AOA) type 1 is due to a mutation of the aprataxin gene and is associated with hypoalbuminemia [41, 42]. AOA type 2 is due to a mutation in the senataxin gene [10]. AoA2 is associated with increased alpha-fetoprotein levels in blood [123].
Late-onset Tay-Sachs disease (LOTSD) is characterized by a deficiency in beta-hexosaminidase due to a mutation in the HEXA gene [149]. Patients presents a FRDA-like phenotype.
Cerebrotendinous xanthomatosis (CTX) patients carry a mutation within the mitochondrial enzyme sterol 27-hydroxylase (CYP27). Serum analysis shows increased levels of cholestanol and bile alcohols [202]. Patients exhibit combinations of dementia, psychiatric disturbances, pyramidal deficits, extra-pyramidal deficits (dystonia), cerebellar signs, seizures, and peripheral neuropathy [192]. Neuropsychiatric symptoms such as hallucinations, agitation, depression, and suicide attempts may be prominent. Infantile-onset diarrhea, cataract and tendon xanthomas are suggestive [223].
Refsum’s disease is caused by mutation of the gene for the peroxisomal enzyme phytanoyl-CoA hydroxylase, PHYH [99]. The age of onset varies from early childhood to 50 years of age. Most patients have symptoms before age of 20 years. The main clinical features are retinitis pigmentosa, chronic polyneuropathy, and cerebellar ataxia [109]. Anosmia, sensorineural deafness, cardiac arrhythmias, renal failure, bony and skin abnormalities have been reported [126].
SCA with axonal neuropathy (SCAN1) is due to a mutation within the TDP1 gene, encoding for the tyrosyl-DNA phosphodiesterase 1 [56]. SCAN1 is characterized by peripheral sensori-motor axonal neuropathy, distal muscular atrophy, and pes cavus. Patients exhibit steppage during gait. The phenotype can mimick Charcot-Marie-Tooth disease. Patients have a history of seizures.
The recessive spinocerebellar ataxia type 1 (SCAR8; ARCA1) maps to locus 6q25. The disease is caused by mutations in the SYNE1 gene [54]. SCAR8 was initially identified in French Canadian families originating mainly from the Beauce and Bas-St-Laurent regions of the province of Quebec (Canada). Patients present a late-onset cerebellar ataxia with slow progression [74]. They exhibit dysarthria, dysmetria, occasional brisk lower-extremity tendon reflexes, and minor oculomotor abnormalities. Brain MRI shows a diffuse pure cerebellar atrophy.
Autosomal recessive spastic ataxia of Charlevoix-Saguenay (ARSACS) is due to a deficit in the chaperone protein sacsin (SACS) [222]. The age of onset ranges from 1 to 14 years [29]. ARSACS is characterized by early-onset spastic ataxia, axonal and demyelinating neuropathy, and hypermyelination of retinal nerve fibers [205]. Pes cavus is common. Gait unsteadiness is the first symptom in most cases. A minority of patients develop seizures. Intelligence is usually normal.
In the infantile-onset spinocerebellar ataxia (IOSCA) the gene C10orf2 encoding for the protein twinkle, a mitochondrial helicase involved in DNA replication, is mutated [154]. The disease has been described in Finland and is characterized by a very early onset ataxia (between 1 and 2 years), athetosis and tendon hyporeflexia. Ophthalmoplegia, hearing loss, and sensory neuropathy appear later in the disease course. Refractory status epilepticus, migraine-like headaches and severe psychiatric symptoms are also suggestive [128].
Marinesco-Sjögren syndrome (MSS) is due to a mutation in the chaperone protein HSPA5 transcribed by the gene SIL1 [5]. Symptoms of MSS start in the infancy [221]. Manifestations include cerebellar ataxia, congenital cataracts, retarded somatic and mental development, muscle weakness, hypotonia and tendon areflexia.
Wilson disease, a treatable disorder resulting from copper accumulation and subsequent hepatic dysfunction, has variable presentations. Cerebellar symptoms may be present and tremor appears in up to 50% of patients. The Kayser-Fleischer ring (a deep copper-colored ring at the periphery of the cornea, the color ranging from greenish gold to brown) is observed in up to 90% of individuals and is almost invariably present in patients with neurologic manifestations. Low ceruloplasmin levels are found in blood. Levels of total copper are decreased. Hemolytic anemia (Coombs-negative) occurs in 10-15 % of cases.
II.2.4. Mitochondrial Disorders
This group gathers diseases due to mutations in mitochondrial genes. Most genes are involved in the energy production, essentially in oxidative phosphorylation [238]. Some mitochondrial disorders have ataxia as a main symptom, such as Kearns-Sayre Syndrome, May-White Syndrome, MNGIE (ophthalmoparesia, peripheral neuropathy, and gastrointestinal symptoms), Leigh syndrome, NARP (neuropathy, ataxia, and retinitis pigmentosa), MELAS (mitochondrial encephalomyopathy, lactic acidosis with stroke-like episodes), and MEERF (myoclonus epilepsy with ragged red fibers) [63]. Mutations within the mitochondrial DNA polymerase (POLG) catalytic subunit γ are associated with a progressive external ophthalmoplegia and hepatocerebral disturbances [33].
II.2.5. X-linked Inherited Ataxias
The commonest X-linked ataxias are listed in Table 9. Fragile-X tremor ataxia syndrome (FXTAS) is rare disease in which a CGG mutation is carried on the X chromosome [97, 98]. The disorder usually starts after 50 years. Typical symptoms are gait ataxia, kinetic tremor, parkinsonism, polyneuropathy, and cognitive dysfunctions [2, 21].
Table 9.
Main X-Linked Ataxias
| Fragile X tremor ataxia syndrome (FXTAS) |
| Arts Syndrome |
| X-linked adrenoleukodystrophy (X-ALD) |
| Congenital ataxias |
| Rett syndrome |
| Ataxia-Dementia (SCAX4) |
III. SPORADIC ATAXIAS
This class of ataxias can be divided in (1) degenerative and (2) acquired ataxias. Degenerative ataxias include multiple system atrophy (MSA) and idiopathic late-onset cerebellar ataxia (ILOCA) [69]. MSA is a progressive adult-onset disease. A cerebellar form (c-MSA) and a parkinsonian form (p-MSA) are observed. Patients exhibit dysautonomia.
Acquired ataxias are listed in Table 10. The drugs which can trigger a cerebellar syndrome are given in Table 11. The most common cerebellotoxic agent is alcohol. Chronic consumption leads to cerebellar atrophy which is most pronounced in the anterior vermis [95]. The principal neuropathological findings are a loss of Purkinje neurons and a drop in the dendritic network in the molecular layer [163]. By contrast, granule cells are relatively resistant to chronic ethanol exposure [203]. Excitotoxicity contributes to ethanol/withdrawal-induced lesions in the cerebellum [129]. Excitatory signaling outweighs inhibitory transmission. There is an excessive glutamate binding to NMDA receptors, followed by calcium influx into neuronal cytoplasm. Although acute doses of ethanol inhibit the NMDA-mediated toxicity of granule cells in culture, chronic administration enhances the NMDA receptor activity [91, 92]. Local administration of ethanol in cerebellar nuclei in vivo decreases extracellular levels of GABA and increases the NMDA-induced production of NO [134]. Chronic exposure of Purkinje neurons to ethanol increases the AMPA-elicited calcium influx [153]. Acute doses of ethanol act also directly on gabaergic pathways. In particular, acute doses potentiate the function of GABA-A receptors, explaining partly the sedative and anti-anxiety effects [119]. Chronic ethanol exposure depresses the expression of GABA-A receptors alpha1-subunit and increases alpha6-subunit expression, mediating the development of tolerance to the motor-impairing effects of ethanol [119]. Another mechanism of cerebellar toxicity of ethanol is linked to the effects on thiamine, an essential cofactor of alpha-ketoglutarate dehydrogenase, pyruvate dehydrogenase and transketolase, 3 key-enzymes of energy metabolism and lipid synthesis in the brain [95]. The effects of thiamine deficiency on diencephalic lesions in Wernicke encephalopathy are well demonstrated [112]. Cerebellum is the site of the brain with the highest turn-over rate of thiamine, which could explain the particular vulnerability of the cerebellum to thiamine deficit. Several studies have also underlined the relationship between ethanol and oxidative stress. Ethanol-induced oxidative stress contributes to the observed apoptotic neuron loss, with accumulation of 4-hydroxynonenal (HNE; see section IV), a toxic product of lipid peroxidation which accumulates in ethanol-exposed brain mitochondria and triggers a release of apoptosis-inducing factor from mitochondria in a dose-dependent manner [168].
Table 10.
Acquired Ataxias
| Stroke (infarction, haemorrhage) |
| Toxic-induced (ethanol, heavy metals, solvents, drugs) |
| Immune-mediated |
| Infectious/parainfectious diseases (abscess, cerebellitis) |
| Traumatic |
| Context of neoplastic disorder (Primary cancer, metastases, chemotherapy, stroke, paraneoplastic) |
| Endocrine (hypothyroidism) |
| Structural disease (Chiari malformations, agenesis, hypoplasias, dysplasias). |
Table 11.
Main Drugs which May Trigger Cerebellar Ataxia
| Lithium salts |
| Phenytoin |
| Valproate |
| Amiodarone |
| Metronidazole |
| Procainamide |
| Calcineurin inhibitors |
| Mefloquine |
| Isoniazid |
Immune-mediated ataxias include: multiple sclerosis, cerebellar ataxia with anti-glutamic acid decarboxylase (GAD) antibodies, gluten ataxia, Miller-Fisher syndrome, systemic lupus erythematosus, Sjögren syndrome, Cogan syndrome, thyroiditis [7, 15, 75, 180, 190]. In children, tumors causing ataxic syndromes include medulloblastomas, astrocytomas, and ependymomas [143]. In adults metastatic tumors and hemangioblastomas are the most common cerebellar neoplasms. Paraneoplastic ataxias often present as a subacute cerebellar syndrome, sometimes mimicking a cerebellitis [104]. Patients may present with neurologic symptoms before identification of the underlying tumor. Paraneoplastic cerebellar degeneration is often mediated by antibodies usually generated against various tumor antigens (in particular anti-Yo/anti-Hu/anti-Ri/ Anti-mGluR1/Anti-Zic4/anti-CV2 antibodies). The most commonly associated cancers involve the ovary, uterus, breast, lungs, or ataxia may be associated with Hodgkin lymphoma.
IV. TREATMENTS OF CAS
IV.1. Current Symptomatic Therapy
Several treatments, mainly targeting neurotransmitters, have been assessed these last decades. It should be pointed out that 4 barriers have hampered meaningful clinical trials [219]: the rarity of each cerebellar disorder considered alone, the heteregeneous presentation of CAs, the fact that a substantial degree of neuronal loss has already occurred when symptoms appear, and the absence of biomarkers. However, some CAs do respond to specific therapies and should not be overlooked, such as AVED which responds to vitamin E supplements [160]. We briefly summarize below the current general management of cerebellar disorders.
General Recommandations
Speech rehabilitation and regular physiotherapy/occupational therapy are recommended in CAs. Most patients have some improvements with the use of orthosis, sticks, or strollers. Unfortunately, many patients will become wheelchair bound during the course of their illness. Gastrostomy is usually recommended when swallowing difficulties worsen.
Pharmacotherapy
The principal drugs which have been suggested for treatment of nystagmus are gabapentin (a GABA analogue), clonazepam, 3, 4-diaminopyridine, baclofen and memantine (an uncompetitive NMDA antagonist). Action tremor may respond to primidone, beta-adrenergic blocking agents, such as propanolol, and to benzodiazepines [135]. Appropriate medications may be given for associated symptoms such as spasticity, parkinsonism, dystonia, bladder dysfunction, and orthostatic hypotension. In particular, parkinsonian symptoms may improve with levodopa or dopamine agonists. Spasticity is treated with baclofen/tinazidine. Alternatives include benzodiazepines and tizanidine. Dystonia may respond to diphenhydramide, benzotropine mesylate, or biperiden. Seizures are treated with conventional antiepileptic medications. Myoclonus may be attenuated with benzodiazepines, high doses of piracetam or sodium valproate. For urinary urgencies, the use of spasmolytics or adrenergic a-receptor blockers is effective. Hypotension may respond to increasing salt in the diet or may subside with the use of fludrocortisone or midodrine.
Surgical Therapy
High-frequency electrical stimulation (DBS) of the ventral intermediate nucleus (Vim), or surgical lesions (thalamotomy), can reduce cerebellar tremor. However, there is usually no effect on dysmetria.
Treatment of Paraneoplastic Cerebellar Ataxia
The treatment of the primary cancer should be performed as soon as possible in paraneoplastic cerebellar ataxia, hence the importance of early detection. Various combinations of surgery, chemotherapy and radiotherapy are considered according to the neoplasm. Intravenous immunoglobulins and plasmaphereses have been used in some cases with variable results. The role of intravenous steroids is not established.
Autosomal Dominant Cerebellar Ataxias (ADCAs)
In case of neurodegeneration as observed in SCAs, none of the symptomatic therapies mentioned above has stopped the progression of the disease, although symptomatic improvements have been reported (Table 11). Slight benefits have been observed using 5-hydroxytryptophan, buspirone or tandospirone, sulfamethoxazole/trimethoprim or lamotrigine. Acetazolamide may decrease the ataxic symptoms in SCA6. Muscle cramps may be disabling, especially in SCA3, and may respond to magnesium, quinine, or mexiletine [52, 160, 233].
Episodic Ataxias
The main treatment for episodic ataxia (EA1) is acetazolamide [81]. 4-aminopyridine, phenytoin and cabamazepine are alternatives. Phenytoin and carbamazepine may exacerbate symptoms in EA2.
Recessive Ataxias
In FRDA patients, a monitoring for cardiomyopathy and diabetes yearly is important [188]. Idebenone (2, 3-dimethoxy-5-methyl-6-(10-hydroxydecyl)-1, 4-benzoquinone) has been shown to reduce cardiac hypertrophy in most patients, but does not stop progression of ataxia [46, 139, 164, 177, 211]. Iron chelators, such as desferoxiamine and deferiprone could have beneficial effects [72, 127, 195]. Recombinant human erythropoietin (EPO) and peroxisome proliferator activated receptor gamma agonists (PPARgamma) are under investigation (see section IV.2) [1, 25, 79, 141, 201]. Beta-blockers at high doses could provide benefits in patients with heart involvement.
In AVED, oral supplementation of vitamin E is the treatment of choice to improve the clinical status [186]. ABL is also treated with vitamin E. CoQ10 supplementation improves ataxia in case of deficiency of CoQ10. Treatment of CTX includes oral administration of chenodeoxycholic acid and statins such as pravastatin to inhibit hydroxylmethylglutaryl (HMG)-CoA reductase. Refsum’s disease is treated with dietary restriction of phytanic acid.
Sporadic Ataxias
Specific intoxications and endocrine ataxias should be treated with specific therapies. Vitamin B1 supplementation is recommended in cerebellar degeneration due to alcoholic intoxication [95]. Abstinence is mandatory to avoid the progression of the degeneration.
In gluten ataxia, the benefits of a gluten-free diet in the treatment of patients with celiac disease are well established [75]. The most reliable marker of adherence to a gluten-free diet is serological evidence of elimination of circulating anti-gliadin antibodies [75]. Patients with gluten ataxia in absence of enteropathy may improve with intravenous immunoglobulins. Treatment with immunosuppressants should be considered if strict gluten-free diet has not resulted in improvement of ataxia after a year or if the ataxia is rapidly progressive [75].
Medications used to slow the progression of multiple sclerosis include immune modulators such as interferons, monoclonal antibodies, glatiramer acetate, mitoxantrone, methotrexate, azathioprine, cyclophosphamide, and natalizumab. Steroids may be used to decrease the severity of attacks. It is still unclear whether i.v. (intravenous) immunoglobulin and plasmapheresis improve patients’ outcomes in Miller-Fisher syndrome [151]. Steroids are also useful for the management of raised intra-cranial pressure associated with cerebellar disorders and for post-infectious cerebellitis [236].
Mitochondrial Disorders
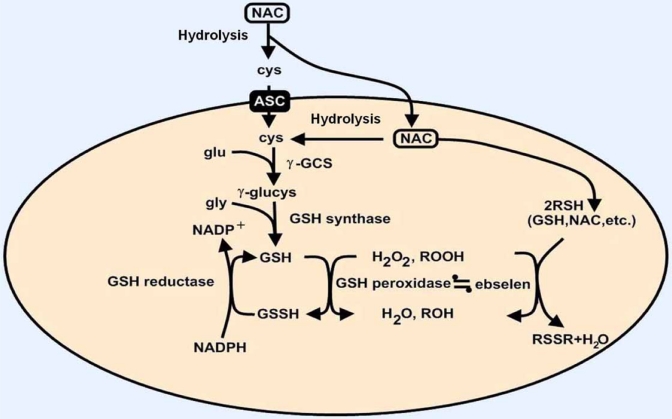
High doses of CoQ10 and N-acetylcysteine (NAC), which was considered as one of the most promising drug, are used in maternally inherited mitochondrial diseases, but their efficacy is not established. Oxidative stress decreases cellular bioenergetic capacity, which will generate reactive oxygen species (ROS) [9]. Antioxidants such as NAC are involved in glutathione regeneration (Fig. 2). Cysteine is transported by the alanine-serine-cysteine (ASC) system, but NAC does not require any active transport to deliver cysteine to the cell [12]. NAC is rapidly hydrolyzed and under the consecutive effects of gamma-glutamylcysteine synthetase and GSH synthetase, GSH is generated. This synthesis is highly limited by the availability of the substrates. Gamma-glutamylcysteine synthetase is inhibited by feedback from GSH (Ki around 1, 5 mM). Therefore, this enzyme is not operating at its maximal rate under physiological conditions. Intracellular GSH is maintained in the thiol form by the gluthatione reductase, which requires NADPH. GSH can react with non enzymatically with ROS, and GSH peroxidase catalyzes the destruction of hydrogen peroxide and hydroperoxides. From a pharmacokinetic point of view, infused NAC rapidly generates disulfides in plasma, which prolongs the existence of the drug from a few minutes to up to 6 hours. Nevertheless, free thiol is undetectable following oral ingestion of a dose of 200 mg of NAC. The bioavailability of the oral formulation is less than 5 %. This factor contributes to the failure of NAC given orally to prevent the raise in ROS in neurodegenerative disorders like CAs.
Fig. (2).
Mechanism of action of N-acetylcysteine (NAC). ASC, alanine-serine-cysteine (ASC) transport system; c-GCS, c-glutamylcysteine synthetase; cys, cysteine; glu, glutamine; gly, glycine; GSH, glutathione. Adapted from Arakawa and Ito (2007), [9].
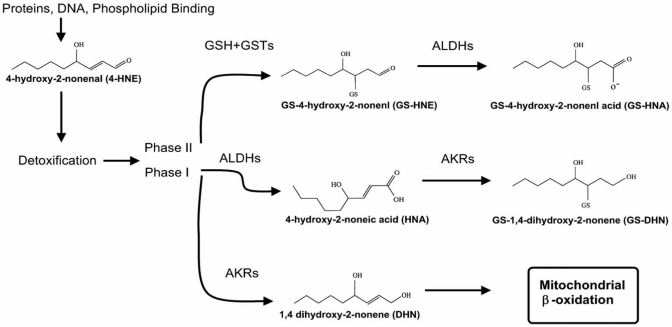
Membrane lipid peroxidation results from accumulation of ROS. One of the products of lipid peroxidation is HNE (Fig. 3), which is associated with inhibition of the activity of several types of cellular function and signaling, and exhibits cytotoxicity through alkylation [22, 106]. High levels of HNE have been found in the brain of patients with Alzheimer’s disease (AD). Increased HNE levels have also been found in the cerebellum of patients with spinocerebellar degeneration [235]. HNE-induced neurotoxicity is suppressed by Ac-DEVD-CHO, a caspase-3 inhibitor, in rat cerebellar granule neurons, suggesting that HNE-induced neuronal death is attributable to activation of the caspase-3-dependent pathway [93]. HNE affects in particular mitochondrial function, signal transduction, transport function, cytokine production and the cytoskeleton [117]. Interestingly, a pre-treatment with high concentrations of NAC completely suppresses the formation of HNE-modified protein, mitochondrial injury and neuronal death [8]. This protective effect is due to an increase of GSH-HNE conjugation by increased GSH levels after treatment with NAC. This highlights the potential of NAC for neurodegenerative disorders.
Fig. (3).
Potential routes of mitochondrial HNE metabolism. HNE is able to alkylate diverse classes of biological molecules. Balancing this toxicity is the metabolism of HNE by multiple phase I and phase II pathways. GS-HNE and GS-HNE acid can dehydrate to form a cyclic hemiacetal and lactone, respectively. Adapted from Arakawa and Ito 2007, [9].
IV.2. Current Pharmaceutical Trials
Several human trials have been launched these last years, especially in FRDA (Table 12). The most promising drugs are discussed.
Table 12.
Results of Clinical Trials in Spinocerebellar Ataxias (SCAs) Caused by CAG Repeats
| Disease Ref | Treatment | Design of the Trial | Results |
|---|---|---|---|
| SCA3 [38] | Sulfamethoxazole Trimethoprim | Double-blind, placebo controlled crossover | Improved gait and coordination |
| SCA3 [187] | Sulfamethoxazole Trimethoprim | Double-blind, placebo controlled crossover | No effect |
| SCA3 [178] | Tetrahydrobiopterin | Double-blind crossover | Improvement on timed tests |
| SCA6 [233] | Acetazolamide | Open label | Improvement on Ataxia Rating Scale |
| SCA3 [204] | Tandospirone | Open label | Improvement on Ataxia Rating Scale |
From Underwood and Rubinsztein (2008) [219].
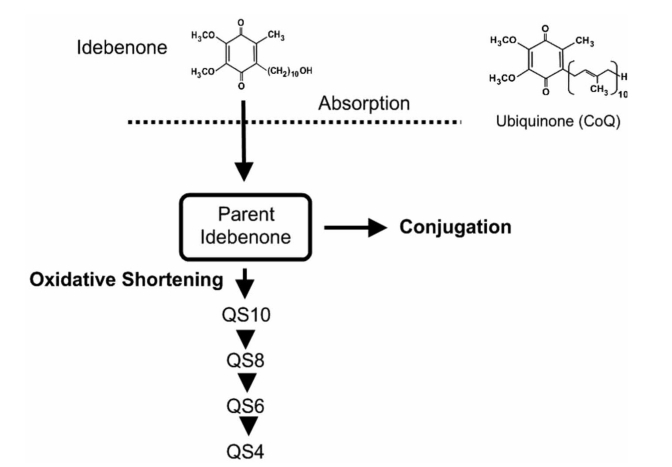
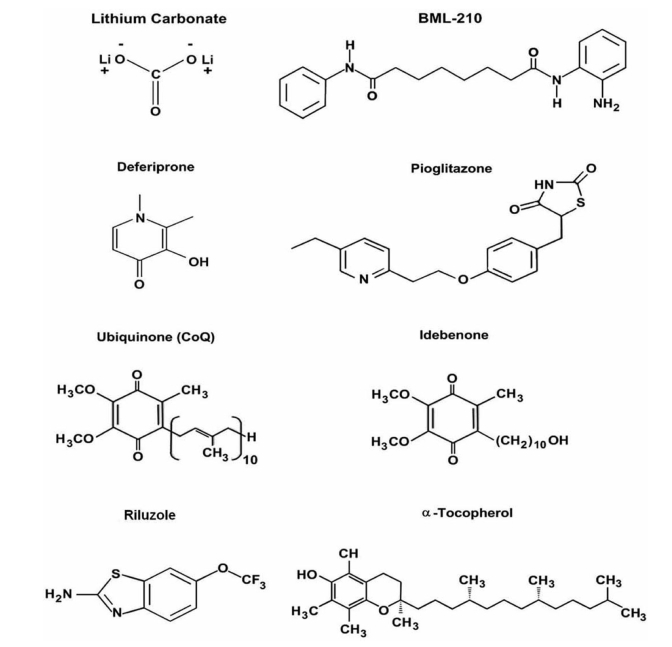
Idebenone
Idebenone is an organic compound of the quinone family and promoted commercially as a synthetic analog of CoQ10. Idebenone is claimed to have properties similar to CoQ10 in terms of antioxidant effects [144]. Idebenone improves deficiencies in electron flow and reduces oxidative stress [120]. Parent idebenone is rapidly metabolized by oxidation and side chain shortening to the inactive metabolites QS10, QS8, QS6 and QS4 (Fig. 4). Both parent idebenone and the metabolites may be conjugated to sulfates and glucuronides. Phase 1 studies (doses ranging from 150 mg to 1050 mg, either as single oral dose or repeated doses) have shown very low concentrations of the parent drug, with high inter-subject variability [40]. Cmax varies from 1.64 to 23.6 ng/ml according to studies, and tmax ranges from 0.87 to 3.37 hours. Total QS4 is the main metabolic fraction of idebenone in plasma. The pharmacokinetics remain linear for doses ranging from 150 mg to 750 mg daily. The bioavailability is slightly increased when the drug is given after a fat-rich meal. Idebenone is used in Europe in the treatment of vascular and degenerative diseases of the central nervous system [144, 107]. The drug has been used recently in the treatment of FRDA [188]. In a one-year trial on a small number of patients, idebenone reduced the rate of deterioration of cardiac function, without blocking the progression of ataxia [144]. Results of a 3- to 5-years trial suggest that idebenone (1) prevents the progression of cardiomyopathy in both pediatric and adult patients, and (2) stabilizes the neurological dysfunction in pediatric subjects. EPI-A0001 (Edison Pharmaceuticals, San Jose, CA, USA), a bioisostere of CoQ10, is entering in clinical trials [194]. Penwest Pharmaceuticals has just initiated a phase I clinical trial (that will be conducted in healthy volunteers) to evaluate its safety and tolerability at various doses and to collect pharmacokinetic data.
Fig. (4).
Schematic rappresentation of the metabolism of Idebenone. Idebenone is absorbed and can be converted via the oxidative shortening or directly being conjugated. The structure of ubiquinone is shown on the upper right corner.
Erythropoietin (EPO)
Clinical trials have started, with encouraging results [25]. In one pilot clinical trial, a reduction in oxidative stress markers such as urinary 8-hydroxydeoxyguanosine and serum peroxides has been observed after 5, 000 IU rhu-EPO administration for 8 weeks, three times a week. The frataxin increase observed in this trial is 27%, with high variability between patients (ranging from 15% to 63%). Some non-responders have been identified. However, considering the commercial availability of EPO as drug with assessed safety, these results are promising. Further longer trials are required.
Deferiprone (DFP)
For systemic iron overload diseases, like hemochromatosis, the use of iron chelators (desferal or deferiprone DFP, Fig. 5) has an undeniable relevance [24, 170]. However, the possible role of iron chelators for the treatment of FRDA and other neurodegenerative conditions is still largely controversial [127, 195]. The main point of discussion is the vagueness of the molecular targets of the actual iron chelating drugs. DFP acts as a siderophore to chelate both cytosolic and mitochondrial labile iron. DFP redistributes iron between cellular compartments and to different cell populations, including erythroid precursors, to be used for other metabolic purposes, such as the heme biosynthesis. DFP, as any other clinically relevant chelator, should be used with moderation to avoid overchelation that could affect normal cellular iron metabolism and thereby induce iron deficiency anemia. The importance of exercising moderation in applying chelation relates not only to drug dosage but also to drug exposure time, as dictated by drug pharmacokinetics.
Fig. (5).
Molecular structures of current drugs assessed for therapy of cerebellar disorders.
Lithium Salts
Lithium carbonate, a compound commonly used to treat manic depression, might also provide symptomatic relief for a group of inherited movement disorders such as SCA1. Treatment with lithium salts reduce motor control difficulties in the mouse model of SCA1. The drug might slow down degenerative changes in the brain. Starting from this important finding, the National Institutes of Health Clinical Center (CC) has started a phase I clinical trial (first patient recruited in March 2009). It should be pointed out that this drug is potentially cerebellotoxic and that a close monitoring is required. Irreversible cerebellar syndromes have been reported.
Riluzole
Riluzole preferentially blocks tetrodotoxin (TTX)-sensitive sodium channels which are associated with damaged neurons [197]. This results in a reduction of calcium influx and prevents indirectly the stimulation of glutamate receptors. Together with a direct glutamate receptor blockade, the deleterious effect of glutamate on motor neurons is greatly reduced. However, the action of riluzole on glutamate receptors has been controversial, as no binding of the molecule has been shown on any known receptor [13, 53, 231]. A phase II trial for multiple sclerosis and inherited ataxias is ongoing to assess efficacy of riluzole (S.Andrea Hospital Rome, Italy).
Valproic Acid
Valproic acid (VPA) is primarily used for the treatment of epilepsy, bipolar disorder, and major depression. It is also prescribed to treat headaches and schizophrenia. Valproate may affect neurotransmitter GABA function (as a GABA transaminase inhibitor) in the human brain, making it an alternative to lithium salts in treatment of bipolar disorder. In addition, Valproate may also reverse the transamination process to form more GABA. Hence, VPA acts indirectly as a GABA agonist. However, several other mechanisms of action have been proposed [176]. In particular, it might act as a histone deacetylase 1(HDAC1) inhibitor. A phase I trial has begun in China for SCA3 patients.
PPAR-γ Agonists
PPAR-γ agonists, such as rosiglitazone and pioglitazone, are commonly used for the treatment of diabetes mellitus [171, 172] and represent also a promising therapeutic strategy for other diseases including neurodegenerative disorders with an inflammatory component such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and amyotrophic lateral sclerosis (ALS) [78, 79]. Interestingly, this class of molecule has been proposed for mitochondrial diseases, because of their ability to increase the response to oxidative stress, and to act upon mitochondrial biogenesis [1, 37]. A phase II/III trial has started at the Hôpital Robert Debré (France) for FRDA.
V. THERAPIES UNDER DEVELOPMENT
New drugs are currently tested in transgenic models of CAs. These new strategies are summarized in Table 13. In particular, therapeutic strategies which have been successful for Huntington’s disease are being considered for SCAs. This is the case for RNAi therapies which aim to inhibit polyglutamine-induced neurodegeneration. Prevention of protein misfolding and aggregation by overexpressing chaperones, such as heat-shock protein HSP70 or DNAJ1 are being evaluated [87]. HDAC inhibitors can revert silent heterochromatin to an active chromatin conformation, and thus restore the normal function of genes which are silenced in these diseases [47, 80, 174]. Today, the precise site of action of these inhibitors is still unknown. Moreover, it is of great relevance to assess the safety/toxicity of these compounds. Nevertheless, this innovative approach remains one of the most interesting options for the treatment of diseases such as FRDA or FXTAS in which heterochromatin mediating gene silencing occurs. Drugs modulating the cannabinoid receptors and nitric oxide pathways are at a very early stage, and require additional efforts to bring them to the pre-clinical route. Another approach under development is the use of neurotrophic factors promoting survival of Purkinje cells. Two factors play a key-role in this function: glial derived neurotrophic factor (GDNF) and insulin-like growth factor-1 (IGF-1), synthetized by Bergmann glia and Purkinje cells/inferior olive, respectively [152]. GDNF promotes both survival and differentiation of Purkinje neurons, and has shown a protective effect in several models of excitoxicity [4, 210]. Intra-ventricular administration of GDNF protects the shaker mutant rats from loss of Purkinje cells [210]. IGF-1 exerts also neuroprotective effects. In particular, IGF-1 promotes reinnervation and functional recovery after inferior olive lesion [61]. Another potential approach is based on the modulation of microglial activation which follows focal brain damage [225]. Activated microglial cells participate in the process of remote cell death by producing proinflammatory cytokines, nitric oxide, glutamate and free radicals [23]. Minocycline is a tetracycline derivative which reduces microglial activation in axotomized precerebellar nuclei by modulating the inflammatory response consecutive to a cerebellar injury. There is some hope that acting on this mechanism may provide benefits for CAs in the future.
Table 13.
Therapeutical Trials in Cerebellar Ataxias
| FRIEDREICH’S ATAXIA |
| Coenzyme Q10 (CoQ10) with E-pilot study |
| Idebenone - Phase III |
| Mitoquinone (MitoQ) - Phase II |
| Erythropoetin (EPO) - pilot, PhaseI/II |
| Chelation therapy (Deferiprone) - Phase I/II |
| EPI-A0001 (RAID program)-pre-drug |
| HDAC inhibitors - pre-drug |
| PPARgamma agonists - Phase II/III |
| Varenicline - Phase II |
| SPORADIC ATAXIAS |
| Gluten-free dietpilot study |
| Immunomodulation (IV immunoglobulins, plasmapheresis) -pilot study |
Cerebellum is a target of numerous hormones [116, 217]. It is established that hormonal defects induce cerebellar lesions and that hormones interact with dendritic growth, spinogenesis and synaptogenesis [216]. Surprisingly, very few experimental studies have attempted to take advantages of these effects. The use of hormones for therapy of ataxias probably deserves more attention.
Transplantation of stem cells is another approach under development, but will not be discussed here for a matter of clarity. Regarding gene therapy and the use of viral vectors, recent advances have contributed to selective and efficient gene transfer to Purkinje cells in vivo [83]. A promising application of viral vectors is the rescue of a deficient gene, followed by functional recovery [103]. This strategy might become an appealing approach for therapeutic targeting of disorders affecting Purkinje neurons in the coming decades.
VI. OVERVIEW OF THE SITES OF ACTION OF THERAPIES OF CEREBELLAR ATAXIAS
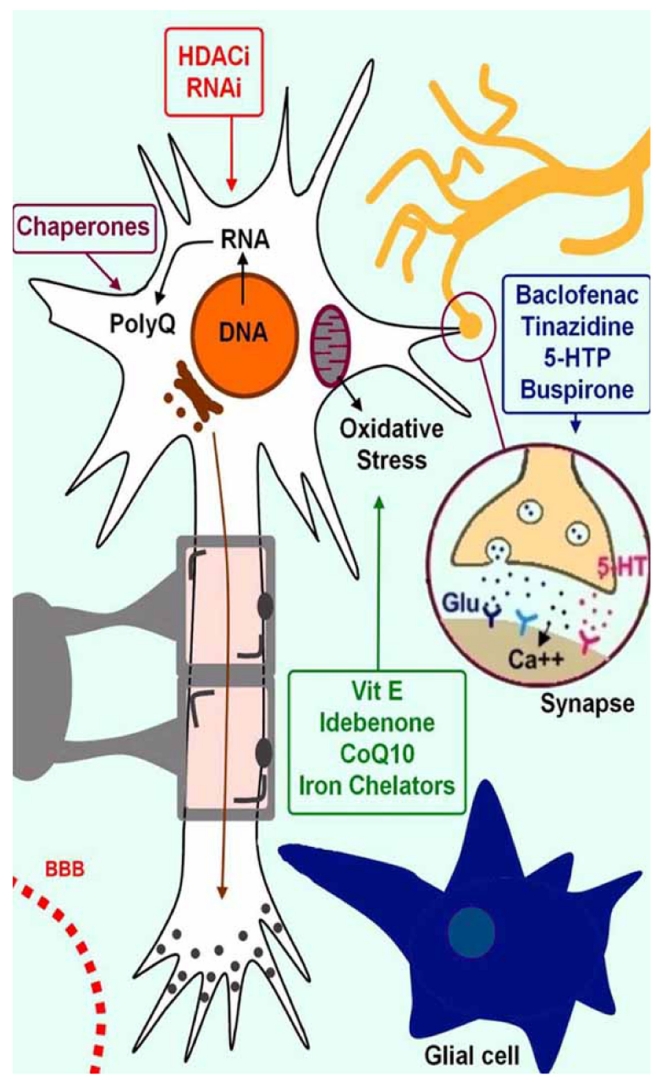
The topic of therapeutics of CAs has been considered as a “black box” these last 3 decades. Sets of therapies are being evaluated and it is now possible to draw the lines of therapies in this category of so-called “untreatable neurological disorders” (Fig. 6):
Fig. (6).
Illustration of the sites of action of anti-ataxic drugs. Drugs can be gathered in 4 groups according to the mechanism of action: modulation of synaptic activity, action against oxidative stress, acting on the DNA/RNA level, and targeting the clearance of specific proteins.
drugs acting at synaptic level
drugs targeting the oxidative stress
drugs acting on the DNA or RNA
drugs aiming to decrease the synthesis of abnormal proteins or to increase their clearance.
VII. CONCLUSION
Our understanding of the pathogenesis of CAs has increased dramatically these last 15 years. Unraveling of genetic defects and developments of animal models are reshaping the neuropharmacology of CAs. For the first time, drugs under development and ongoing clinical trials aim to restore cerebellar function by acting on a deleterious pathway. Several avenues of research are still to be explored. One illustrative example is the therapeutics of neuropsychiatric symptoms recently characterized in cerebellar patients. As a result of the functional heterogeneity of the cerebellar circuitry, it is plausible that drugs under development may selectively improve some cerebellar deficits, whereas other therapies would improve the full clinical deficits.
There is an obvious medical need to develop anti-ataxic drugs with proved efficacy. The identification of the molecular cascades leading to neuronal death in cerebellar circuitry will greatly help in this endeavor. Such knowledge is required to develop potential therapeutic agents in order to prevent neuronal dysfunction and neurodegeneration.
Table 14.
Drugs Targetting A Deleterious Pathway
| Acting against oxidative Stress and Free Radicals (Mitochondria) |
| Vitamin E |
| Coenzyme Q10 (CoQ10) |
| Creatine |
| Alpha lipoic acid |
| Tauroursodeoxycholic acid (TUDCA) |
| Ethyl-EPA (LAX-101) |
| Apoptosis/Excitotoxicity |
| Anti-glutamate (remacemide, riluzole, memantine) |
| Anti-caspase-1 (minocycline, ethyl-EPA) |
| “Declumping”-reducing fragment load |
| Anti-caspase 3 (minocycline and others) |
| Anti-caspase 6 |
| Anti-transglutaminase (cystamine) |
| “Declumping”-reducing aggregation |
| Inhibition of GSK-3beta (lithium chloride, trehalose) |
| Transcriptional re-regulation-upregulating expression of genes inhibited by mHtg. |
| Valproic acid |
| SAHA/suberoylanilide hydroxamic acid, |
| Phenylbutyrate |
| Transcriptional hijacking-small inhibitory RNAs to block the production of mHtg. |
ACKNOWLEDGEMENTS
D.M. is supported by the Fonds Erasme-Belgium. M.M. is supported by the FNRS-Belgium.
REFERENCES
- 1.Acquaviva F, Castaldo I, Filla A, Giacchetti M, Marmolino D, Monticelli A, Pinelli M, Saccà F, Cocozza S. Recombinant human erythropoietin increases frataxin protein expression without increasing mRNA expression. Cerebellum. 2008;7:360–365. doi: 10.1007/s12311-008-0036-x. [DOI] [PubMed] [Google Scholar]
- 2.Adams JS, Adams PE, Nguyen D, Brunberg JA, Tassone F, Zhang W, Koldewyn K, Rivera SM, Grigsby J, Zhang L, DeCarli C, Hagerman PJ, Hagerman RJ. Volumetric brain changes in females with fragile X-associated tremor/ataxia syndrome (FXTAS) Neurology. 2007;69:851–859. doi: 10.1212/01.wnl.0000269781.10417.7b. [DOI] [PubMed] [Google Scholar]
- 3.Ahn AH, Dziennis S, Hawkes R, Herrup K. The cloning of zebrin II reveals its identity with aldolase C. Development. 1994;120:2081–90. doi: 10.1242/dev.120.8.2081. [DOI] [PubMed] [Google Scholar]
- 4.Alberch J, Pérez-Navarro E, Canals JM. Neuroprotection by neurotrophins and GDNF family members in the excitotoxic model of Huntington's disease. Brain Res. Bull. 2002;57:817–22. doi: 10.1016/s0361-9230(01)00775-4. [DOI] [PubMed] [Google Scholar]
- 5.Anttonen AK, Siintola E, Tranebjaerg L, Iwata NK, Bijlsma EK, Meguro H, Ichikawa Y, Goto J, Kopra O, Lehesjoki AE. Novel SIL1 mutations and exclusion of functional candidate genes in Marinesco-Sjogren syndrome. Eur. J. Hum. Genet. 2008;16:961–969. doi: 10.1038/ejhg.2008.22. [DOI] [PubMed] [Google Scholar]
- 6.Aoki K, Washimi Y, Fujimori N, Maruyama K, Yanagisawa N. Familial idiopathic vitamin E deficiency associated with cerebellar atrophy. Rinsho Shinkeigaku. 1990;30:966–971. [PubMed] [Google Scholar]
- 7.Appenzeller S, Cendes F, Costallat L. Cerebellar ataxia in systemic lupus erythematosus. Lupus. 2008;17:1122–6. doi: 10.1177/0961203308093071. [DOI] [PubMed] [Google Scholar]
- 8.Arakawa M, Ishimura A, Arai Y, Kawabe K, Suzuki S, Ishige K, Ito Y. Characterization of 4-hydroxynonenalinduced neuronal death in cerebellar granule neurons. Neurosci Res. doi: 10.1016/j.neures.2006.10.011. in press. [DOI] [PubMed] [Google Scholar]
- 9.Arakawa M, Ito Y. N-acetylcysteine and neurodegenerative diseases: Basic and clinical pharmacology. Cerebellum. 2007;19:1–7. doi: 10.1080/14734220601142878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arning L, Schols L, Cin H, Souquet M, Epplen J T, Timmann D. Identification and characterisation of a large senataxin (SETX) gene duplication in ataxia with ocular apraxia type 2 (AOA2) Neurogenetics. 2008;9:295–299. doi: 10.1007/s10048-008-0139-z. [DOI] [PubMed] [Google Scholar]
- 11.Arpa J, Campos Y, Cruz Martínez A, Gutiérrez Molina M, Arenas J, Alonso M, Plaza I, Morales C, Palomo F, Barreiro P, et al. Clinical and investigative approaches in mitochondrial diseases. A review of 15 cases. Neurologia. 1994;9:324–36. [PubMed] [Google Scholar]
- 12.Awasthi YC, Sharma R, Cheng JZ, Yang Y, Sharma A, Singhal SS, Awasthi S. Role of 4-hydroxynonenal in stressmediated apoptosis signaling. Mol. Aspects Med. 2003;24:219–30. doi: 10.1016/s0098-2997(03)00017-7. [DOI] [PubMed] [Google Scholar]
- 13.Azbill RD, Mu X, Springer JE. "Riluzole increases high-affinity glutamate uptake in rat spinal cord synaptosomes". Brain Res. 2000;871:175–80. doi: 10.1016/s0006-8993(00)02430-6. [DOI] [PubMed] [Google Scholar]
- 14.Banfi S, Zoghbi HY. Baillieres. Molecular genetics of hereditary ataxias. Clin. Neurol. 1994;3 :281–95. [PubMed] [Google Scholar]
- 15.Bataller L, Valero C, Díaz R, Froufe A, Garcia-Zarza A, Ribalta T, Vilchez JJ, Saiz A. Cerebellar ataxia associated with neuroendocrine thymic carcinoma and GAD antibodies. J. Neurol. Neurosurg. Psychiatry. 2009;80:696–7. doi: 10.1136/jnnp.2008.161042. [DOI] [PubMed] [Google Scholar]
- 16.Baude A, Molnár E, Latawiec D, McIlhinney RA, Somogyi P. Synaptic and nonsynaptic localization of the GluR1 subunit of the AMPA-type excitatory amino acid receptor in the rat cerebellum. J. Neurosci. 1994;14:2830–43. doi: 10.1523/JNEUROSCI.14-05-02830.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bauer P, Laccone F, Rolfs A, Wüllner U, Bösch S, Peters H, Liebscher S, Scheible M, Epplen JT, Weber BH, Ho-linski-Feder E, Weirich-Schwaiger H, Morris-Rosendahl DJ, Andrich J, Riess O. Trinucleotide repeat expansion in SCA17/TBP in white patients with Huntington's disease-like phenotype. J. Med. Genet. 2004;41:230–2. doi: 10.1136/jmg.2003.015602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Becerra L, Morris S, Bazes S, Gostic R, Sherman S, Gostic J, Pendse G, Moulton E, Scrivani S, Keith D, Chizh B, Borsook D. Trigeminal neuropathic pain alters responses in CNS circuits to mechanical (brush) and thermal (cold and heat) stimuli. J. Neurosci. 2006;26:10646–57. doi: 10.1523/JNEUROSCI.2305-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beierlein M, Regehr WG. Local interneurons regulate synaptic strength by retrograde release of endocannabinoids. J. Neurosci. 2006;26:9935–43. doi: 10.1523/JNEUROSCI.0958-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ben Hamida M, Belal S, Sirugo G, Ben Hamida C, Panayides K, Ionannou P, Beckmann J, Mandel J L, Hentati F, Koenig M, Middleton L. Friedreich's ataxia phenotype not linked to chromosome 9 and associated with selective autosomal recessive vitamin E deficiency in two inbred Tunisian families. Neurology. 1993;43:2179–2183. doi: 10.1212/wnl.43.11.2179. [DOI] [PubMed] [Google Scholar]
- 21.Berry-Kravis E, Abrams L, Coffey SM, Hall DA, Greco C, Gane LW, Grigsby J, Bourgeois JA, Finucane B, Jacquemont S, Brunberg JA, Zhang L, Lin J, Tassone F, Hagerman PJ, Hagerman RJ, Leehey MA. Fragile X-associated tremor/ataxia syndrome: clinical features, genetics, and testing guidelines. Mov. Disord. 2007;22:2018–2030. doi: 10.1002/mds.21493. [DOI] [PubMed] [Google Scholar]
- 22.Blanc EM, Kelly JF, Mark RJ, Waeg , Mattson MP. 4-Hydroxynonenal, an aldehydic product of lipid peroxidation, impairs signal transduction associated with muscarinic acetylcholine and metabotropic glutamate receptors: possible action on Gaq/11. J. Neurochem. 1997;69:570–80. doi: 10.1046/j.1471-4159.1997.69020570.x. [DOI] [PubMed] [Google Scholar]
- 23.Block ML, Zecca L, Hong JS. Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat. Rev. Neurosci. 2007;8 :57–69. doi: 10.1038/nrn2038. [DOI] [PubMed] [Google Scholar]
- 24.Boddaert N, Le Quan Sang K, Rötig A, Leroy-Willig A, Gallet S, Brunelle F, Sidi D, Thalabard JC, Munnich A, Cabantchik ZI. Selective iron chelation in Friedreich ataxia: biologic and clinical implications. Blood. 2007;110:401–408. doi: 10.1182/blood-2006-12-065433. [DOI] [PubMed] [Google Scholar]
- 25.Boesch S, Sturm B, Hering S, Goldenberg H, Poewe W, Scheiber-Mojdehkar B. Friedreich’s ataxia: clinical pilot trial with recombinant human erythropoietin. Ann. Neurol. 2007;62:521–524. doi: 10.1002/ana.21177. [DOI] [PubMed] [Google Scholar]
- 26.Borsook D, Moulton EA, Tully S, Schmahmann JD, Becerra L. Human cerebellar responses to brush and heat stimuli in healthy and neuropathic pain subjects. Cerebellum. 2008;7:252–72. doi: 10.1007/s12311-008-0011-6. [DOI] [PubMed] [Google Scholar]
- 27.Bortolozzi A, Duffard R, Antonelli M, Evangelista de Duffard AM. Increased sensitivity in dopamine D(2)-like brain receptors from 2,4-dichlorophenoxyacetic acid (2,4-D)-exposed and amphetamine-challenged rats. Ann. N.Y. Acad. Sci. 2002;965:314–23. doi: 10.1111/j.1749-6632.2002.tb04173.x. [DOI] [PubMed] [Google Scholar]
- 28.Boyson SJ, McGonigle P, Molinoff PB. Quantitative autoradiographic localization of the D1 and D2 subtypes of dopamine receptors in rat brain. J. Neurosci. 1986;6:3177–88. doi: 10.1523/JNEUROSCI.06-11-03177.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Breckpot J, Takiyama Y, Thienpont B, Van Vooren S, Vermeesch JR, Ortibus E, Devriendt K. A novel genomic disorder: a deletion of the SACS gene leading to spastic ataxia of Charlevoix-Saguenay. Eur. J. Hum. Genet. 2008;16:1050–1054. doi: 10.1038/ejhg.2008.58. [DOI] [PubMed] [Google Scholar]
- 30.Brusse E, Maat-Kievit JA, Van Swieten JC. Diagnosis and management of early-and late-onset cerebellar ataxia. Clin. Genet. 2007;71:12–24. doi: 10.1111/j.1399-0004.2006.00722.x. [DOI] [PubMed] [Google Scholar]
- 31.Brust JCM. Current diagnosis & treatment in neurology. 1. McGraw-Hill Medical: 2006. [Google Scholar]
- 32.Campuzano V, Montermini L, Lutz Y, Cova L, Hindelang C, Jiralerspong S, Trottier Y, Kish SJ, Faucheux B, Trouillas P, Authier FJ, Dürr A, Mandel JL, Vescovi A, Pandolfo M, Koenig M. Frataxin is reduced in Friedreich ataxia patients and is associated with mitochondrial membranes. Hum. Mol. Genet. 1997;6:1771–1780. doi: 10.1093/hmg/6.11.1771. [DOI] [PubMed] [Google Scholar]
- 33.Chan SS, Copeland WC. Functional analysis of mutant mitochondrial DNA polymerase proteins involved in human disease. Methods Mol. Biol. 2009;554:59–72. doi: 10.1007/978-1-59745-521-3_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen H, Von Hehn C, Kaczmarek LK, Ment LR, Pober BR, Hisama FM. Functional analysis of a novel potassium channel (KCNA1) mutation in hereditary myokymia. Neurogenetics. 2007;8:131–135. doi: 10.1007/s10048-006-0071-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chung SH, Kim CT, Hawkes R. Compartmentation of GABA B receptor2 expression in the mouse cerebellar cortex. Cerebellum. 2008;7:295–303. doi: 10.1007/s12311-008-0030-3. [DOI] [PubMed] [Google Scholar]
- 36.Clausi S, Bozzali M, Leggio MG, Di Paola M, Hagberg GE, Caltagirone C, Molinari M. Quantification of gray matter changes in the cerebral cortex after isolated cerebellar damage: A voxel-based morphometry study. Neuroscience. 2009;7 doi: 10.1016/j.neuroscience.2009.02.001. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 37.Coppola G, Marmolino D, Lu D, Wang Q, Cnop M, Rai M, Acquaviva F, Cocozza S, Pandolfo M, Geschwind DH. Functional genomic analysis of frataxin deficiency reveals tissue-specific alterations and identifies the PPARgamma pathway as a therapeutic target in Friedreich's ataxia. Hum. Mol. Genet. 2009;18:2452–61. doi: 10.1093/hmg/ddp183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Correia M, Coutinho P, Silva MC, Guimaraes J, Amado J, Matos E. Evaluation of the effect of sulphametoxazole and trimethoprim in patients with Machado-Joseph disease. Rev. Neurol. 1995;23:632–4. [PubMed] [Google Scholar]
- 39.Couceyro P, Pollock KM, Drews K, Douglass J. Cocaine differentially regulates activator protein-1 mRNA levels and DNA-binding complexes in the rat striatum and cerebellum. Mol. Pharmacol. 1994;46:667–76. [PubMed] [Google Scholar]
- 40.Damulin IV, Korsakova SS. The use of idebenone (noben) in neurological practice. Zh. Nevrol. Psikhiatr. Im. 2006;106:66–71. [PubMed] [Google Scholar]
- 41.Date H, Onodera O, Tanaka H, Iwabuchi K, Uekawa K, Igarashi S, Koike R, Hiroi T, Yuasa T, Awaya Y, Sakai T, Takahashi T, Nagatomo H, Sekijima Y, Kawachi I, Takiyama Y, Nishizawa M, Fukuhara N, Saito K, Sugano S, Tsuji S. Early-onset ataxia with ocular motor apraxia and hypoalbuminemia is caused by mutations in a new HIT superfamily gene. Nat. Genet. 2001;29:184–188. doi: 10.1038/ng1001-184. [DOI] [PubMed] [Google Scholar]
- 42.Dawson DM. Recessive ataxia with ocular motor apraxia. Arch. Neurol. 2001;58:173–174. doi: 10.1001/archneur.58.2.173. [DOI] [PubMed] [Google Scholar]
- 43.Delatycki M, Williamson R, Forrest S. Friedreich ataxia: an overview. J. Med. Genet. 2000;37:1–8. doi: 10.1136/jmg.37.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Delis F, Mitsacos A, Giompres P. Pharmacological characterization and anatomical distribution of the dopamine transporter in the mouse cerebellum. Cerebellum. 2008;7:242–51. doi: 10.1007/s12311-008-0005-4. [DOI] [PubMed] [Google Scholar]
- 45.Dethy S, Manto M, Bastianelli E, Gangji V, Laute MA, Goldman S, Hildebrand J. Cerebellar spongiform degeneration induced by acute lithium intoxication in the rat. Neurosci. Lett. 1997;224:25–8. doi: 10.1016/s0304-3940(97)13461-9. [DOI] [PubMed] [Google Scholar]
- 46.Di Prospero N, Baker A, Jeffries N, Fischbeck K. Neurological effects of high-dose idebenone in patients with Friedreich’s ataxia: a randomised, placebo-controlled trial. Lancet Neurol. 2007;6:878–886. doi: 10.1016/S1474-4422(07)70220-X. [DOI] [PubMed] [Google Scholar]
- 47.Di Prospero N, Fischbeck K. Therapeutics development for triplet repeat expansion diseases. Nat. Rev. Genet. 2005;6:756–765. doi: 10.1038/nrg1690. [DOI] [PubMed] [Google Scholar]
- 48.Diana G, Pieri M, Valentini G. Eur Effects of Win 55,212-2 on hippocampal CA1 long-term potentiation in experiments controlled for basal glutamatergic synaptic transmission. J. Pharmacol. 2002;453:251–4. doi: 10.1016/s0014-2999(02)02448-2. [DOI] [PubMed] [Google Scholar]
- 49.Dietrichs E. Clinical manifestation of focal cerebellar disease as related to the organization of neural pathways. Acta Neurol. Scand. Suppl. 2008;188:6–11. doi: 10.1111/j.1600-0404.2008.01025.x. [DOI] [PubMed] [Google Scholar]
- 50.Dietrichs E, Haines DE, Røste GK, Røste LS. Hypothalamocerebellar and cerebellohypothalamic projections--circuits for regulating nonsomatic cerebellar activity? Histol. Histopathol. 1994;9:603–14. [PubMed] [Google Scholar]
- 51.Döhlinger S, Hauser TK, Borkert J, Luft AR, Schulz JB. Magnetic resonance imaging in spinocerebellar ataxias. Cerebellum. 2008;7:204–14. doi: 10.1007/s12311-008-0025-0. [DOI] [PubMed] [Google Scholar]
- 52.Dressler D, Benecke R. Diagnosis and management of acute movement disorders. J. Neurol. 2005;252:1299–306. doi: 10.1007/s00415-005-0006-x. [DOI] [PubMed] [Google Scholar]
- 53.Dunlop J, Beal McIlvain H, She Y, Howland DS. "Impaired spinal cord glutamate transport capacity and reduced sensitivity to riluzole in a transgenic superoxide dismutase mutant rat model of amyotrophic lateral sclerosis". J. Neurosci. 2003;23:1688–96. doi: 10.1523/JNEUROSCI.23-05-01688.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dupre N, Gros-Louis F, Chrestian N, Verreault S, Brunet D, de Verteuil D, Brais B, Bouchard J.-P, Rouleau G.A. Clinical and genetic study of autosomal recessive cerebellar ataxia type 1. Ann. Neurol. 2007;62:93–98. doi: 10.1002/ana.21143. [DOI] [PubMed] [Google Scholar]
- 55.Efthimiopoulos S, Giompres P, Valcana T. Kinetics of dopamine and noradrenaline transport in synaptosomes from cerebellum, striatum and frontal cortex of normal and realer mice. J. Neurosci. Res. 1991;29:510–9. doi: 10.1002/jnr.490290411. [DOI] [PubMed] [Google Scholar]
- 56.El-Khamisy SF, Saifi GM, Weinfeld M, Johansson F, Helle-day T, Lupski JR, Caldecott KW. Defective DNA single-strand break repair in spinocerebellar ataxia with axonal neuropathy-1. Nature. 2005;434 :108–13. doi: 10.1038/nature03314. [DOI] [PubMed] [Google Scholar]
- 57.Espinós-Armero C, González-Cabo P, Palau-Martínez F. Autosomal recessive cerebellar ataxias. Their classification, genetic features and pathophysiology. Neurology. 2005;41:409–22. [PubMed] [Google Scholar]
- 58.Fatemi SH, Reutiman TJ, Folsom TD, Sidwell RW. The role of cerebellar genes in pathology of autism and schizophrenia. Cerebellum. 2008;7:279–94. doi: 10.1007/s12311-008-0017-0. [DOI] [PubMed] [Google Scholar]
- 59.Fauchey V, Jaber M, Bloch B, Le Moine C. Dopamine control of striatal gene expression during development: relevance to knockout mice for the dopamine transporter. Eur. J. Neurosci. 2000;12:3415–25. doi: 10.1046/j.1460-9568.2000.00220.x. [DOI] [PubMed] [Google Scholar]
- 60.Fedele E, Raiteri M. In vivo studies of the cerebral glutamate receptor/NO/cGMP pathway. Prog. Neurobiol. 1999;58:89–120. doi: 10.1016/s0301-0082(98)00077-x. [DOI] [PubMed] [Google Scholar]
- 61.Fernandez AM, Gonzalez de la Vega AG, Planas B, Torres-Aleman I. Neuroprotective actions of peripherally administered insulin-like growth factor I in the injured olivo-cerebellar pathway. Eur. J. Neurosci. 1999;11:2019–30. doi: 10.1046/j.1460-9568.1999.00623.x. [DOI] [PubMed] [Google Scholar]
- 62.Filla A, De Michele G, Coppola G, Federico A, Vita G, Toscano A, Uncini A, Pisanelli P, Barone P, Scarano V, Perretti A, Santoro L, Monticelli A, Cavalcanti F, Caruso G, Cocozza S. Accuracy of clinical diagnostic criteria for Friedreich’s ataxia. Mov. Disord. 2000;15:1255–1258. doi: 10.1002/1531-8257(200011)15:6<1255::aid-mds1031>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 63.Finsterer J. Mitochondrial disorders, cognitive impairment and dementia. J. Neurol. Sci. 2009 doi: 10.1016/j.jns.2009.02.347. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 64.Flament D, Hore J. Movement and electromyographic disorders associated with cerebellar dysmetria. J. Neurophysiol. 1986;55:1221–33. doi: 10.1152/jn.1986.55.6.1221. [DOI] [PubMed] [Google Scholar]
- 65.Fujigasaki H, Martin JJ, De Deyn PP, Camuzat A, Deffond D, Stevanin G, Dermaut B, Van Broeckhoven C, Dürr A, Brice A. CAG repeat expansion in the TATA box-binding protein gene causes autosomal dominant cerebellar ataxia. Brain. 2001;124:1939–47. doi: 10.1093/brain/124.10.1939. [DOI] [PubMed] [Google Scholar]
- 66.Gakh O, Park S, Liu G, Macomber L, Imlay J, Ferreira G, Isaya G. Mitochondrial iron detoxification is a primary function of frataxin that limits oxidative damage and preserves cell longevity. Hum. Mol. Genet. 2006;15:467–479. doi: 10.1093/hmg/ddi461. [DOI] [PubMed] [Google Scholar]
- 67.Gatti RA, Boder E, Vinters HV, Sparkes RS, Norman A, Lange K. Ataxia-telangiectasia: an interdisciplinary approach to pathogenesis. Medicine. 1991;70:99–117. [PubMed] [Google Scholar]
- 68.Gilad S, Chessa L, Khosravi R, Russell P, Galanty Y, Piane M, Gatti RA, Jorgensen T J, Shiloh Y, Bar-Shira A. Genotype-phenotype relationships in ataxia-telangiectasia and variants. Am. J. Hum. Genet. 1998;62:551–561. doi: 10.1086/301755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, Wood NW, Colosimo C, Dürr A, Fowler CJ, Kaufmann H, Klockgether T, Lees A, Poewe W, Quinn N, Revesz T, Robertson D, Sandroni P, Seppi K, Vidailhet M. Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 2008;71:670–676. doi: 10.1212/01.wnl.0000324625.00404.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Giompres P, Delis F. Dopamine transporters in the cerebellum of mutant mice. Cerebellum. 2005;4:105–11. doi: 10.1080/14734220510007851. [DOI] [PubMed] [Google Scholar]
- 71.Giros B, Jaber M, Jones SR, Wightman RM, Caron MG. Hyperlocomotion and indifference to cocaine and amphetamine in mice lacking the dopamine transporter. Nature. 1996;379:606–12. doi: 10.1038/379606a0. [DOI] [PubMed] [Google Scholar]
- 72.Goncalves S, Paupe V, Dassa E, Rustin P. Deferiprone targets aconitase: implication for Friedreich’s ataxia treatment. BMC Neurol. 2008;8:20. doi: 10.1186/1471-2377-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Goodkin HP, Thach WT. Cerebellar control of constrained and unconstrained movements. I. Nuclear inactivation. J. Neurophysiol. 2003;89:884–95. doi: 10.1152/jn.00114.2002. [DOI] [PubMed] [Google Scholar]
- 74.Gros-Louis F, Dupre N, Dion P, Fox M. A, Laurent S, Verreault S, Sanes J.R, Bouchard J.-P, Rouleau G. A. Mutations in SYNE1 lead to a newly discovered form of autosomal recessive cerebellar ataxia. Nat. Genet. 2007;39:80–85. doi: 10.1038/ng1927. [DOI] [PubMed] [Google Scholar]
- 75.Hadjivassiliou M, Sanders DS, Woodroofe N, Williamson C, Grünewald RA. Gluten ataxia. Cerebellum. 2008;7:494–498. doi: 10.1007/s12311-008-0052-x. [DOI] [PubMed] [Google Scholar]
- 76.Hall CN, Attwell D. Assessing the physiological concentration and targets of nitric oxide in brain tissue. J. Physiol. 2008;586:3597–615. doi: 10.1113/jphysiol.2008.154724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hauser TK, Luft A, Skalej M, Nägele T, Kircher TT, Leube DT, Schulz JB. Visualization and quantification of disease progression in multiple system atrophy. Mov. Disord. 2006;21:1674–81. doi: 10.1002/mds.21032. [DOI] [PubMed] [Google Scholar]
- 78.Heneka M, Landreth G. PPARs in the brain. Biochim. Biophys. Acta. 2007;1771:1031–1045. doi: 10.1016/j.bbalip.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 79.Heneka M, Landreth G, Hüll M. Drug insight: effects mediated by peroxisome proliferator-activated receptorgamma in CNS disorders. Nat. Clin. Pract. Neurol. 2007;3:496–504. doi: 10.1038/ncpneuro0586. [DOI] [PubMed] [Google Scholar]
- 80.Herman D, Jenssen K, Burnett R, Soragni E, Perlman S, Gottesfeld J. Histone deacetylase inhibitors reverse gene silencing in Friedreich’s ataxia. Nat. Chem. Biol. 2006;2:551–558. doi: 10.1038/nchembio815. [DOI] [PubMed] [Google Scholar]
- 81.Herrmann A, Braathen GJ, Russell MB. Episodic ataxias. Tidsskr. Nor. Laegeforen. 2005;125:2005–7. [PubMed] [Google Scholar]
- 82. Herrup K, Kuemerle B. The compartmentalization of the cerebellum. Annu. Rev. Neurosci. 1997;20:61–90. doi: 10.1146/annurev.neuro.20.1.61. [DOI] [PubMed] [Google Scholar]
- 83.Hirai H. Progress in transduction of cerebellar Purkinje cells in vivo using viral vectors. Cerebellum. 2008;7:273–8. doi: 10.1007/s12311-008-0012-5. [DOI] [PubMed] [Google Scholar]
- 84.Hore J, Wild B, Diener HC. Cerebellar dysmetria at the elbow, wrist, and fingers. J. Neurophysiology. 1991;65:563–71. doi: 10.1152/jn.1991.65.3.563. [DOI] [PubMed] [Google Scholar]
- 85. Hu D, Shen H, Zhou Z. Functional asymmetry in the cerebellum: a brief review. Cerebellum. 2008;7:304–13. doi: 10.1007/s12311-008-0031-2. [DOI] [PubMed] [Google Scholar]
- 86.Huang C. Implications on cerebellar function from information coding. Cerebellum. 2008;7:314–31. doi: 10.1007/s12311-008-0032-1. [DOI] [PubMed] [Google Scholar]
- 87.Huen NY, Wong SL, Chan HY. Transcriptional malfunctioning of heat shock protein gene expression in spinocerebellar ataxias. Cerebellum. 2007;6:111–7. doi: 10.1080/14734220600996480. [DOI] [PubMed] [Google Scholar]
- 88.Ige AO, Bolam JP, Billinton A, White JH, Marshall FH, Emson PC. Cellular and sub-cellular localisation of GABA(B1) and GABA(B2) receptor proteins in the rat cerebellum. Mol. Brain Res. 2000;83:72–80. doi: 10.1016/s0169-328x(00)00199-6. [DOI] [PubMed] [Google Scholar]
- 89.Ikai Y, Takada M, Shinonaga Y, Mizuno N. Dopaminergic and non-dopaminergic neurons in the ventral tegmental area of the rat project, respectively, to the cerebellar cortex and deep cerebellar nuclei. Neuroscience. 1992;51:719–28. doi: 10.1016/0306-4522(92)90310-x. [DOI] [PubMed] [Google Scholar]
- 90.Ikeda H, Yamaguchi M, Sugai S, Aze , Narumiya S, Kaki-zuka A. Expanded polyglutamine in the Machado-Joseph disease protein induces cell death in vitro and in vivo. Nat. Genet. 1996;13:196–202. doi: 10.1038/ng0696-196. [DOI] [PubMed] [Google Scholar]
- 91.Iorio KR, Reinlib L, Tabakoff B, Hoffman PL. Chronic exposure of cerebellar granule cells to ethanol results in increased N-methyl-D-aspartate receptor function. Mol. Pharmacol. 1992;41:1142–8. [PubMed] [Google Scholar]
- 92.Iorio KR, Tabakoff B, Hoffman PL. Glutamate-induced neurotoxicity is increased in cerebellar granule cells exposed chronically to ethanol. Eur. J. Pharmacol. 1993;248:209–12. doi: 10.1016/0926-6917(93)90045-r. [DOI] [PubMed] [Google Scholar]
- 93.Ito Y, Arakawa M, Ishige K, Fukuda H. Comparative study of survival signal withdrawal- and 4-hydroxynonenal-induced cell death in cerebellar granule cells. Neurosci. Res. 1999;35:321–7. doi: 10.1016/s0168-0102(99)00097-8. [DOI] [PubMed] [Google Scholar]
- 94.Jaarsma D, Ruigrok TJ, Caffé R, Cozzari C, Levey AI, Mugnaini E, Voogd J. Cholinergic innervation and receptors in the cerebellum. Prog. Brain Res. 1997;114:67–96. doi: 10.1016/s0079-6123(08)63359-2. [DOI] [PubMed] [Google Scholar]
- 95.Jaatinen P, Rintala J. Mechanisms of ethanol-induced degeneration in the developing, mature, and aging cerebellum. Cerebellum. 2008;7:332–47. doi: 10.1007/s12311-008-0034-z. [DOI] [PubMed] [Google Scholar]
- 96.Jaber M, Dumartin B, Sagné C, Haycock JW, Roubert C, Giros B, Bloch B, Caron MG. Differential regulation of tyrosine hydroxylase in the basal ganglia of mice lacking the dopamine transporter. Eur. J. Neurosci. 1999;11:3499–511. doi: 10.1046/j.1460-9568.1999.00764.x. [DOI] [PubMed] [Google Scholar]
- 97.Jacquemont S, Hagerman R J, Hagerman P J, Leehey M A. Fragile-X syndrome and fragile X-associated tremor/ataxia syndrome: two faces of FMR1. Lancet. 2007;6:45–55. doi: 10.1016/S1474-4422(06)70676-7. [DOI] [PubMed] [Google Scholar]
- 98.Jacquemont S, Hagerman R J, Leehey M, Grigsby J, Zhang L, Brunberg J A, Greco C, Des Portes V, Jardini T, Levine R, Berry-Kravis E, Brown W T, Schaeffer S, Kissel J, Tas-sone F, Hagerman P J. Fragile X premutation tremor/ataxia syndrome: molecular, clinical, and neuroimaging correlates. Am. J. Hum. Genet. 2003;72:869–878. doi: 10.1086/374321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jansen GA, Waterham HR, Wanders RJ. Molecular basis of Refsum disease: sequence variations in phytanoyl-CoA hydroxylase (PHYH) and the PTS2 receptor (PEX7) Hum. Mutat. 2004;23:209–18. doi: 10.1002/humu.10315. [DOI] [PubMed] [Google Scholar]
- 100. Jen JC. Hereditary episodic ataxias. Ann. N. Y. Acad. Sci. 2008;1142:250–3. doi: 10.1196/annals.1444.016. [DOI] [PubMed] [Google Scholar]
- 101.Jen J, Kim GW, Baloh RW. Clinical spectrum of episodic ataxia type 2. Neurology. 2004;62:7–22. doi: 10.1212/01.wnl.0000101675.61074.50. [DOI] [PubMed] [Google Scholar]
- 102.Jen JC, Baloh RW. Genetics of episodic ataxia. Adv. Neurol. 2002;89:459–61. [PubMed] [Google Scholar]
- 103.Jin D, Liu HX, Hirai H, Torashima T, Nagai T, Lopatina O, Shnayder NA, Yamada K, Noda M, Seike T, Fujita K, Takasawa S, Yokoyama S, Koizumi K, Shiraishi Y, Tanaka S, Hashii M, Yoshihara T, Higashida K, Islam MS, Yamada N, Hayashi K, Noguchi N, Kato I, Okamoto H, Matsushima A, Salmina A, Munesue T, Shimizu N, Mochida S, Asano M, Higashida H. CD38 is critical for social behaviour by regulating oxytocin secretion. Nature. 2007;446:41–5. doi: 10.1038/nature05526. [DOI] [PubMed] [Google Scholar]
- 104.Karmon Y, Inbar E, Cordoba M, Gadoth N. Paraneoplastic Cerebellar Degeneration Mimicking Acute Post-Infectious Cerebellitis. Cerebellum. 2009 doi: 10.1007/s12311-009-0128-2. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 105.Kaupmann K, Malitschek B, Schuler V, Heid J, Froestl W, Beck P, Mosbacher J, Bischoff S, Kulik A, Shigemoto , Karschin A, Bettler B. GABA(B)-receptor subtypes assemble into functional heteromeric complexes. Nature. 1998;396:683–7. doi: 10.1038/25360. [DOI] [PubMed] [Google Scholar]
- 106.Keller JN, Mattson MP. Roles of lipid peroxidation in modulation of cellular signaling pathways, cell dysfunction, and death in the nervous system. Rev. Neurosci. 1998;9:105–16. doi: 10.1515/revneuro.1998.9.2.105. [DOI] [PubMed] [Google Scholar]
- 107.Kelso G, Porteous C, Coulter C, Hughes G, Porteous W, Ledgerwood E, Smith RA, Murphy MP. Selective targeting of a redox-active ubiquinone to mitochondria within cells: antioxidant and antiapoptotic properties. J. Biol. Chem. 2001;276:4588–4596. doi: 10.1074/jbc.M009093200. [DOI] [PubMed] [Google Scholar]
- 108.Klebe S, Durr A, Rentschler A, Hahn-Barma V, Abele M, Bouslam N, Schöls L, Jedynak P, Forlani S, Denis E, Dussert C, Agid Y, Bauer P, Globas C, Wüllner U, Brice A, Riess O, Stevanin G. New mutations in protein kinase Cgamma associated with spinocerebellar ataxia type 14. Ann. Neurol. 2005;58:720–9. doi: 10.1002/ana.20628. [DOI] [PubMed] [Google Scholar]
- 109.Klenk E, Kahlke W. Ueber das Vorkommen der Hoppe, Seylers, Z. 3.7.11.15-tetramethyl-hexadecansaeure (Phytansaeure) in den Cholesterinestern und anderen Lipoidfraktionen der Organe bei einem Krankheitsfall unbekannter Genese (Verdacht auf heredopathia atactica polyneuritiformis Refsum-syndrom) Physiol. Chem. 1963;333:133–142. doi: 10.1515/bchm2.1963.333.1.133. [DOI] [PubMed] [Google Scholar]
- 110.Klimaviciusa L, Safiulina D, Kaasik A, Klusa V, Zharkovsky A. The effects of glutamate receptor antagonists on cerebellar granule cell survival and development. Neurotoxicology. 2008;29:101–8. doi: 10.1016/j.neuro.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 111.Klitenick MA, Tham CS, Fibiger HC. Cocaine and d-amphetamine increase c-fos expression in the rat cerebellum. Synapse. 1995;19:29–36. doi: 10.1002/syn.890190105. [DOI] [PubMed] [Google Scholar]
- 112.Klockgether T, Bürk K, Auburger G, Dichgans J. Classification and diagnosis of degenerative ataxias. Nervenarzt. 1995;66:571–81. [PubMed] [Google Scholar]
- 113.Klockgether T, Skalej M, Wedekind D, Luft AR, Welte D, Schulz JB, Abele M, Bürk K, Laccone F, Brice A, Dichgans J. Autosomal dominant cerebellar ataxia type I. MRI-based volumetry of posterior fossa structures and basal ganglia in spinocerebellar ataxia types 1, 2 and 3. Brain. 1998;121:1687–93. doi: 10.1093/brain/121.9.1687. [DOI] [PubMed] [Google Scholar]
- 114.Klockgether T. The clinical diagnosis of autosomal dominant spinocerebellar ataxias. Cerebellum. 2008;7:101–105. doi: 10.1007/s12311-008-0023-2. [DOI] [PubMed] [Google Scholar]
- 115.Koenig M, Sirugo G, Duclos F. Molecular genetics and familial ataxia. Rev. Neurol. 1993;149:698–702. [PubMed] [Google Scholar]
- 116.Koibuchi N. Hormonal regulation of cerebellar development and plasticity. Cerebellum. 2008;7:1–3. doi: 10.1007/s12311-008-0048-6. [DOI] [PubMed] [Google Scholar]
- 117.Kosuge Y, Koen Y, Ishige K, Minami K, Urasawa H, Saito H, Ito Y. S-allyl-L-cysteine selectively protects cultured rat hippocampal neurons from amyloid b-protein- and tunicamycin-induced neuronal death. Neuroscience. 2003;122:885–95. doi: 10.1016/j.neuroscience.2003.08.026. [DOI] [PubMed] [Google Scholar]
- 118.Kulik A, Nakadate K, Nyíri G, Notomi T, Malitschek B, Bettler B, Shigemoto R. Distinct localization of GABA(B) receptors relative to synaptic sites in the rat cerebellum and ventrobasal thalamus. Eur. J. Neurosci. 2002;15:291–307. doi: 10.1046/j.0953-816x.2001.01855.x. [DOI] [PubMed] [Google Scholar]
- 119.Kumar S, Fleming RL, Morrow AL. Ethanol regulation of gamma-aminobutyric acid A receptors: genomic and nongenomic mechanisms. Pharmacol. Ther. 2004;101:211–26. doi: 10.1016/j.pharmthera.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 120.Kutz K, Drewe J, Vankan P. Pharmacokinetic properties and metabolism of idebenone. J. Neurol. 2009;1:31–5. doi: 10.1007/s00415-009-1006-z. [DOI] [PubMed] [Google Scholar]
- 121.Lalonde R. Cerebellar contributions to instrumental learning. Neurosci. Biobehav. Rev. 1994;18:161–70. doi: 10.1016/0149-7634(94)90022-1. [DOI] [PubMed] [Google Scholar]
- 122.Lamperti C, Naini A, Hirano M, De Vivo DC, Bertini E, Servidei S, Valeriani M, Lynch D, Banwell B, Berg M, Dubrovsky T, Chiriboga C, Angelini C, Pegoraro E, Di Mauro S. Cerebellar ataxia and coenzyme Q10 deficiency. Neurology. 2003;60:1206–8. doi: 10.1212/01.wnl.0000055089.39373.fc. [DOI] [PubMed] [Google Scholar]
- 123.Isabelle Le B, Naïma B, Rivaud-Péchoux S, Guimarães J, Benomar A, Chamayou C, Goizet C, Maria-Ceù M, Sandra K, Mohamed Y, Yves A, Michel K, Giovanni S, Alexis B, Alexandra D. Frequency and phenotypic spectrum of ataxia with oculomotor apraxia 2: a clinical and genetic study in 18 patients. Brain. 2004;127:759–767. doi: 10.1093/brain/awh080. [DOI] [PubMed] [Google Scholar]
- 124.Lee M, Martin-Ruiz C, Graham A, Court J, Jaros E, Perry R, Iversen P, Bauman M, Perry E, Iversen P, Bauman M, Perry E. Nicotinic receptor abnormalities in the cerebellar cortex in autism. Brain. 2002;125:1483–95. doi: 10.1093/brain/awf160. [DOI] [PubMed] [Google Scholar]
- 125.Leggio MG, Neri P, Graziano A, Mandolesi L, Molinari M, Petrosini L. Cerebellar contribution to spatial event processing: characterization of procedural learning. Exp. Brain Res. 1999;127:1–11. doi: 10.1007/s002210050768. [DOI] [PubMed] [Google Scholar]
- 126.Leys D, Petit H, Bonte-Adnet C, Millaire A, Fourrier F, Dubois F, Rousseaux M, Ducloux G. Refsum's disease revealed by cardiac disorders. Lancet. 1989;333:621. doi: 10.1016/s0140-6736(89)91654-1. [DOI] [PubMed] [Google Scholar]
- 127.Li K, Besse E, Ha D, Kovtunovych G, Rouault T. Iron dependent regulation of frataxin expression: implications for treatment of Friedreich ataxia. Hum. Mol. Genet. 2008;17:2265–2273. doi: 10.1093/hmg/ddn127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lönnqvist T, Paetau A, Valanne L, Pihko H. Recessive twinkle mutations cause severe epileptic encephalopathy. Brain. 2009;132:1553–62. doi: 10.1093/brain/awp045. [DOI] [PubMed] [Google Scholar]
- 129.Lovinger DM. Excitotoxicity and alcohol-related brain damage. Alcohol Clin. Exp. Res. 1993;17:19–27. doi: 10.1111/j.1530-0277.1993.tb00720.x. [DOI] [PubMed] [Google Scholar]
- 130.Luján R. Subcellular regulation of metabotropic GABA receptors in the developing cerebellum. Cerebellum. 2007;6:123–9. doi: 10.1080/14734220601039157. [DOI] [PubMed] [Google Scholar]
- 131.Maffei A, Prestori F, Shibuki K, Rossi P, Taglietti V, D'Angelo E. NO enhances presynaptic currents during cerebellar mossy fiber-granule cell LTP. J. Neurophysiol. 2003;90:2478–83. doi: 10.1152/jn.00399.2003. [DOI] [PubMed] [Google Scholar]
- 132.Manto M. The cerebellum, cerebellar disorders, and cerebellar research--two centuries of discoveries. Cerebellum. 2008;7:505–16. doi: 10.1007/s12311-008-0063-7. [DOI] [PubMed] [Google Scholar]
- 133.Manto M, Bastian AJ. Cerebellum and the deciphering of motor coding. Cerebellum. 2007;6:3–6. [Google Scholar]
- 134.Manto M, Laute MA, Pandolfo M. Depression of extra-cellular GABA and increase of NMDA-induced nitric oxide following acute intra-nuclear administration of alcohol in the cerebellar nuclei of the rat. Cerebellum. 2005;4:230–8. doi: 10.1080/14734220500243835. [DOI] [PubMed] [Google Scholar]
- 135.Manto M, Marmolino D. Cerebellar ataxias. Curr. Opin. Neurol. 2009;5 doi: 10.1097/WCO.0b013e32832b9897. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 136.Manto MU. The wide spectrum of spinocerebellar ataxias (SCAs) Cerebellum. 2005;4:2–6. doi: 10.1080/14734220510007914. [DOI] [PubMed] [Google Scholar]
- 137.Manto MU, Laute MA, Aguera M, Rogemond V, Pandolfo M, Honnorat J. Effects of anti-glutamic acid decarboxylase antibodies associated with neurological diseases. Ann. Neurol. 2007;61:544–51. doi: 10.1002/ana.21123. [DOI] [PubMed] [Google Scholar]
- 138.Mariotti C, Di Donato S. Cerebellar/spinocerebellar syndromes. Neurol. Sci. 2001;22 :S88–92. doi: 10.1007/s100720100042. [DOI] [PubMed] [Google Scholar]
- 139.Mariotti C, Solari A, Torta D, Marano L, Fiorentini C, Di Donato S. Idebenone treatment in Friedreich patients: one-year-long randomized placebo-controlled trial. Neurology. 2003;60:1676–9. doi: 10.1212/01.wnl.0000055872.50364.fc. [DOI] [PubMed] [Google Scholar]
- 140.Marmolino D, Acquaviva F. Friedreich's Ataxia: From the (GAA)(n) Repeat Mediated Silencing to New Promising Molecules for Therapy. Cerebellum. 2009 doi: 10.1007/s12311-008-0084-2. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 141.Marmolino D, Acquaviva F, Pinelli M, Monticelli A, Cas-taldo I, Filla A, Cocozza S. PPAR-gamma agonist azelaoyl PAF increases frataxin protein and mRNA expression. New implications for the Friedreich’s ataxia theraphy. Cerebellum. 2008;23 doi: 10.1007/s12311-008-0087-z. (PMID: 19104905) [DOI] [PubMed] [Google Scholar]
- 142.Matsuura T, Yamagata T, Burgess DL, Rasmussen A, Gre-wal RP, Watase K, Khajavi M, McCall AE, Davis CF, Zu L, Achari M, Pulst SM, Alonso E, Noebels JL, Nelson DL, Zoghbi HY, Ashizawa T. Large expansion of the ATTCT pentanucleotide repeat in spinocerebellar ataxia type 10. Nat. Genet. 2000;26:191–194. doi: 10.1038/79911. [DOI] [PubMed] [Google Scholar]
- 143.Mehta SH, Morgan JC, Sethi KD. Paraneoplastic movement disorders. Curr. Neurol. Neurosci. Rep. 2009;9:285–91. doi: 10.1007/s11910-009-0043-4. [DOI] [PubMed] [Google Scholar]
- 144.Meier T, Buyse G. Idebenone: an emerging therapy for Friedreich ataxia. J. Neurol. 2009;1:25–30. doi: 10.1007/s00415-009-1005-0. [DOI] [PubMed] [Google Scholar]
- 145.Melberg A, Dahl N, Hetta J, Valind S, Nennesmo I, Lundberg PO, Raininko R. Neuroimaging study in autosomal dominant cerebellar ataxia, deafness, and narcolepsy. Neurology. 1999;10:2190–2. doi: 10.1212/wnl.53.9.2190. [DOI] [PubMed] [Google Scholar]
- 146.Melchitzky DS, Lewis DA. Tyrosine hydroxylase- and dopamine transporter-immunoreactive axons in the primate cerebellum. Evidence for a lobular- and laminar-specific dopamine innervation. Neuropsychopharmacology. 200;22:466–72. doi: 10.1016/S0893-133X(99)00139-6. [DOI] [PubMed] [Google Scholar]
- 147.Miyoshi Y, Yamada T, Tanimura M, Taniwaki T, Arakawa K, Ohyagi Y, Furuya H, Yamamoto K, Sakai K, Sasazuki T, Kira J. A novel autosomal dominant spinocerebellar ataxia (SCA16) linked to chromosome 8q22.1-24.1. Neurology. 2001;57:96–100. doi: 10.1212/wnl.57.1.96. [DOI] [PubMed] [Google Scholar]
- 148.Mollet J, Giurgea I, Schlemmer D, Dallner G, Chretien D, Delahodde A, Bacq D, de Lonlay P, Munnich A, Rötig A. Prenyldiphosphate synthase, subunit 1 (PDSS1) and OH-benzoate polyprenyltransferase (COQ2) mutations in ubiquinone deficiency and oxidative phosphorylation disorders. J. Clin. Invest. 2007;117:765–772. doi: 10.1172/JCI29089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Montalvo A, Filocamo M, Vlahovicek K, Dardis A, Lualdi S, Corsolini F, Bembi B, Pittis MG. Molecular analysis of the HEXA gene in Italian patients with infantile and late onset Tay-Sachs disease: detection of fourteen novel alleles. Hum. Mutat. 2005;26:2–8. doi: 10.1002/humu.9363. [DOI] [PubMed] [Google Scholar]
- 150.Montero R, Pineda M, Aracil A, Vilaseca MA, Briones P, Sánchez-Alcázar JA, Navas P, Artuch R. Clinical, biochemical and molecular aspects of cerebellar ataxia and Coenzyme Q10 deficiency. Cerebellum. 2007;6:118–122. doi: 10.1080/14734220601021700. [DOI] [PubMed] [Google Scholar]
- 151.Mori M, Kuwabara S, Fukutake T, Hattori T. Intravenous immunoglobulin therapy for Miller-Fisher syndrome. Neurology. 2007;68:1144–1146. doi: 10.1212/01.wnl.0000258673.31824.61. [DOI] [PubMed] [Google Scholar]
- 152.Mount HT, Dean DO, Alberch J, Dreyfus CF, Black IB. Glial cell line-derived neurotrophic factor promotes the survival and morphologic differentiation of Purkinje cells. Proc. Natl. Acad. Sci. 1995;92:9092–6. doi: 10.1073/pnas.92.20.9092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Netzeband JG, Trotter C, Caguioa JN, Gruol DL. Chronic ethanol exposure enhances AMPA-elicited Ca2+ signals in the somatic and dendritic regions of cerebellar Purkinje neurons. Neurochem. Int. 1999;35:163–74. doi: 10.1016/s0197-0186(99)00058-3. [DOI] [PubMed] [Google Scholar]
- 154.Nikali K, Suomalainen A, Saharinen J, Kuokkanen M, Spelbrink JN, Lönnqvist T, Peltonen L. Infantile onset spinocerebellar ataxia is caused by recessive mutations in mitochondrial proteins Twinkle and Twinky. Hum. Mol. Genet. 2005;14:2981–90. doi: 10.1093/hmg/ddi328. [DOI] [PubMed] [Google Scholar]
- 155.Nukina N. Pathomechanism of polyglutamine diseases and strategic design for their therapies. Rinsho Shinkeigaku. 2008;48:913–4. doi: 10.5692/clinicalneurol.48.913. [DOI] [PubMed] [Google Scholar]
- 156.Oberdick J, Baader SL, Schilling K. From zebra stripes to postal zones: deciphering patterns of gene expression in the cerebellum. Trends Neurosci. 1998;21:383–90. doi: 10.1016/s0166-2236(98)01325-3. [DOI] [PubMed] [Google Scholar]
- 157.Ogasawara H, Doi T, Kawato M. Systems biology perspectives on cerebellar long-term depression. Neurosignals. 2008;16:300–17. doi: 10.1159/000123040. [DOI] [PubMed] [Google Scholar]
- 158.Ohata T, Yoshida K, Sakai H, Hamanoue H, Mizuguchi T, Shimizu Y, Okano T, Takada F, Ishikawa K, Mizusawa H, Yoshiura K, Fukushima Y, Ikeda S, Matsumoto N. A-16C>T substitution in the 5' UTR of the puratrophin-1 gene is prevalent in autosomal dominant cerebellar ataxia in Nagano. J. Hum. Genet. 2006;51:461–6. doi: 10.1007/s10038-006-0385-6. [DOI] [PubMed] [Google Scholar]
- 159.Orr H, Zoghbi H. Trinucleotide Rev. Neurosci. 2007;30:575–621. doi: 10.1146/annurev.neuro.29.051605.113042. [DOI] [PubMed] [Google Scholar]
- 160.Palau F, Espinós C. Autosomal recessive cerebellar ataxias. Orphanet. J. Rare Dis. 2006;1:47. doi: 10.1186/1750-1172-1-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Panagopoulos NT, Matsokis NA, Valcana T. Cerebellar and striatal dopamine receptors: effects of reeler and weaver murine mutations. J. Neurosci. Res. 1993;35 :499–506. doi: 10.1002/jnr.490350506. [DOI] [PubMed] [Google Scholar]
- 162.Panagopoulos NT, Papadopoulos GC, Matsokis NA. Dopaminergic innervation and binding in the rat cerebellum. Neurosci. Lett. 1991;130:208–12. doi: 10.1016/0304-3940(91)90398-d. [DOI] [PubMed] [Google Scholar]
- 163.Phillips SC, Harper CG, Kril J. A quantitative histological study of the cerebellar vermis in alcoholic patients. Brain. 1987;110:301–14. doi: 10.1093/brain/110.2.301. [DOI] [PubMed] [Google Scholar]
- 164.Pineda M, Arpa J, Montero R, Aracil A, Domínguez F, Galván M, Mas A, Martorell L, Sierra C, Brandi N, García-Arumí E, Rissech M, Velasco D, Costa JA, Artuch R. Idebenone treatment in paediatric and adult patients with Friedreich ataxia: long-term follow-up. Eur. J. Paediatr. Neurol. 2008;12:470–475. doi: 10.1016/j.ejpn.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 165.Poretti A, Wolf NI, Boltshauser E. Differential diagnosis of cerebellar atrophy in childhood. Eur. J. Paediatr. Neurol. 2008;12:155–67. doi: 10.1016/j.ejpn.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 166.Potts MB, Adwanikar H, Noble-Haeusslein LJ. Models of Traumatic Cerebellar Injury. Cerebellum. 2009;5 doi: 10.1007/s12311-009-0114-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Puccio H. Multicellular models of Friedreich ataxia. J. Neurol. 2009;1:18–24. doi: 10.1007/s00415-009-1004-1. [DOI] [PubMed] [Google Scholar]
- 168.Ramachandran V, Perez A, Chen J, Senthil D, Schenker S, Henderson GI. In utero ethanol exposure causes mitochondrial dysfunction, which can result in apoptotic cell death in fetal brain: a potential role for 4-hydroxynonenal. Alcohol. Clin. Exp. Res. 2001;25:862–71. [PubMed] [Google Scholar]
- 169.Riant F, Mourtada R, Saugier-Veber P, Tournier-Lasserve E. Large CACNA1A deletion in a family with episodic ataxia type 2. Arch. Neurol. 2008;65:817–820. doi: 10.1001/archneur.65.6.817. [DOI] [PubMed] [Google Scholar]
- 170.Richardson D. Friedreich’s ataxia: iron chelators that target the mitochondrion as a therapeutic strategy? Expert. Opin. Investig. Drugs. 2003;12:235–245. doi: 10.1517/13543784.12.2.235. [DOI] [PubMed] [Google Scholar]
- 171.Richter B, Bandeira-Echtler E, Bergerhoff K, Clar C, Ebra-him S. Pioglitazone for type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2006;4 doi: 10.1002/14651858.CD006060.pub2. CD006060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Richter B, Bandeira-Echtler E, Bergerhoff K, Clar C, Ebrahim S. Rosiglitazone for type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2007;3 doi: 10.1002/14651858.CD006063.pub2. CD006063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Riess O, Rüb U, Pastore A, Bauer P, Schöls L. SCA3: neurological features, pathogenesis and animal models. Cerebellum. 2008;7:125–37. doi: 10.1007/s12311-008-0013-4. [DOI] [PubMed] [Google Scholar]
- 174.Riessland M, Brichta L, Hahnen E, Wirth B. The benzamide M344, a novel histone deacetylase inhibitor, significantly increases SMN2 RNA/protein levels in spinal muscular atrophy cells. Hum. Genet. 2006;120:101–110. doi: 10.1007/s00439-006-0186-1. [DOI] [PubMed] [Google Scholar]
- 175.Ritvo ER, Freeman BJ, Scheibel AB, Duong T, Robinson H, Guthrie D, Ritvo A. Lower Purkinje cell counts in the cerebella of four autistic subjects: initial findings of the UCLA-NSAC Autopsy Research Report. Am. J. Psychiatry. 1986;143:862–6. doi: 10.1176/ajp.143.7.862. [DOI] [PubMed] [Google Scholar]
- 176.Rosenberg G. "The mechanisms of action of valproate in neuropsychiatric disorders: can we see the forest for the trees?”. Cell Mol. Life Sci. 2007;64:2090. doi: 10.1007/s00018-007-7079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rustin P, Von Kleist-Retzow J, Chantrel-Groussard K, Sidi D, Munnich A, Rötig A. Effect of idebenone on cardiomyopathy in Friedreich’s ataxia: a preliminary study. Lancet. 1999;354:477–479. doi: 10.1016/S0140-6736(99)01341-0. [DOI] [PubMed] [Google Scholar]
- 178.Sakai T, Yasunobu A, Matsuishi T, Iwashita H. Tetra-hydrobiopterin double-blind, crossover trial in Machado-Joseph disease. J. Neurol. Sci. 1996;136:71–2. doi: 10.1016/0022-510x(95)00296-e. [DOI] [PubMed] [Google Scholar]
- 179.Sánchez-Olea R, Morales M M, Morán J, Pasantes-Morales H. Inhibition by dihydropyridines of regulatory volume decrease and osmolyte fluxes in cultured astrocytes is unrelated to extracellular calcium. Neurosci. Lett. 1995;193:165–8. doi: 10.1016/0304-3940(95)11691-o. [DOI] [PubMed] [Google Scholar]
- 180.Sander HW, Magda P, Chin RL, Wu A, Brannagan TH, 3rd, Green PH, Latov N. Cerebellar ataxia and coeliac disease. Lancet. 2003;362:1548. doi: 10.1016/S0140-6736(03)14743-5. [DOI] [PubMed] [Google Scholar]
- 181.Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J. Neuropsychiatry Clin. Neurosci. 2004;16:367–78. doi: 10.1176/jnp.16.3.367. [DOI] [PubMed] [Google Scholar]
- 182.Schmahmann JD, Pandya DN. Disconnection syndromes of basal ganglia, thalamus, and cerebrocerebellar systems. Cortex. 2008;44:1037–66. doi: 10.1016/j.cortex.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Schoenfeld R, Napoli E, Wong A, Zhan S, Reutenauer L, Morin D, Buckpitt AR, Taroni F, Lonnerdal B, Ristow M, Puccio H, Cortopassi GA. Frataxin deficiency alters heme pathway transcripts and decreases mitochondrial heme metabolites in mammalian cells. Hum. Mol. Genet. 2005;14:3787–3799. doi: 10.1093/hmg/ddi393. [DOI] [PubMed] [Google Scholar]
- 184.Schöls L, Bauer P, Schmidt T, Schulte T, Riess O. Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurol. 2004;3:291–304. doi: 10.1016/S1474-4422(04)00737-9. [DOI] [PubMed] [Google Scholar]
- 185.Schook LB, Kuzmuk K, Adam S, Rund L, Chen K, Ro-gatcheva M, Mazur M, Pollock C, Counter C. DNA-based animal models of human disease: from genotype to phenotype. Dev. Biol. 2008;132:15–25. doi: 10.1159/000317140. [DOI] [PubMed] [Google Scholar]
- 186.Schuelke M, Mayatepek E, Inter M, Becker M, Pfeiffer E, Speer A, Hubner C, Finckh B. Treatment of ataxia in isolated vitamin E deficiency caused by alpha-tocopherol transfer protein deficiency. J. Pediatr. 1999;134:240–244. doi: 10.1016/s0022-3476(99)70424-5. [DOI] [PubMed] [Google Scholar]
- 187.Schulte T, Mattern R, Berger K, Szymanski S, Klotz P, Kraus PH, Przuntek H, Schols L. Double-blind crossover trial of trmethoprim-sulfamethoxazole in spinocerebellar ataxia type 3. Arch. Neurol. 2002;59:1044–5. doi: 10.1001/archneur.58.9.1451. [DOI] [PubMed] [Google Scholar]
- 188.Schulz JB, Boesch S, Bürk K, Dürr A, Giunti P, Mariotti C, Pousset F, Schöls L, Vankan P, Pandolfo M. Diagnosis and treatment of Friedreich ataxia: a European perspective. Nat. Rev. Neurol. 2009;5:222–34. doi: 10.1038/nrneurol.2009.26. [DOI] [PubMed] [Google Scholar]
- 189.Schweighofer N, Doya K, Kuroda S. Cerebellar aminergic neuromodulation: towards a functional understanding. Brain Res. 2004;44:103–16. doi: 10.1016/j.brainresrev.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 190.Selim M, Drachman DA. Ataxia associated with Hashimoto's disease: progressive non-familial adult onset cerebellar degeneration with autoimmune thyroiditis. J. Neurol. Neurosurg. Psychiatry. 2001;71:81–7. doi: 10.1136/jnnp.71.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Shen Y, Mishra R, Mani S, Meiri KF. Both cell-autonomous and cell non-autonomous functions of GAP-43 are required for normal patterning of the cerebellum in vivo. Cerebellum. 2008;7:451–66. doi: 10.1007/s12311-008-0049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Sillitoe RV, Marzban H, Larouche M, Zahedi S, Affanni J, Hawkes R. Conservation of the architecture of the anterior lobe vermis of the cerebellum across mammalian species. Prog. Brain Res. 2005;148:283–97. doi: 10.1016/S0079-6123(04)48022-4. [DOI] [PubMed] [Google Scholar]
- 193.Smirnov DA, Cheung VG. ATM gene mutations result in both recessive and dominant expression phenotypes of genes and microRNAs. Am. J. Hum. Genet. 2008;83:243–53. doi: 10.1016/j.ajhg.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Smith R, Porteous C, Gane A, Murphy M. Delivery of bioactive molecules to mitochondria in vivo. Proc. Natl. Acad. Sci. 2003;100:5407–5412. doi: 10.1073/pnas.0931245100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Sohn Y, Breuer W, Munnich A, Cabantchik Z. Redistribution of accumulated cell iron: a modality of chelation with therapeutic implications. Blood. 2008;111:1690–16. doi: 10.1182/blood-2007-07-102335. [DOI] [PubMed] [Google Scholar]
- 196.Solodkin A, Hlustik P, Noll DC, Small SL. Lateralization of motor circuits and handedness during finger movements. Eur. J. Neurol. 2001;8:425–34. doi: 10.1046/j.1468-1331.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- 197.Song JH, Huang CS, Nagata K, Yeh JZ, Narahashi T. "Differential action of riluzole on tetrodotoxin-sensitive and tetrodotoxin-resistant sodium channels". J. Pharmacol. Exp. Ther. 1997;282:707–14. [PubMed] [Google Scholar]
- 198.Southam E, Morris R, Garthwaite J. Sources and targets of nitric oxide in rat cerebellum. Neurosci. Lett. 1992;137:241–4. doi: 10.1016/0304-3940(92)90413-2. [DOI] [PubMed] [Google Scholar]
- 199.Stell BM, Rostaing P, Triller A, Marty A. Activation of presynaptic GABA(A) receptors induces glutamate release from parallel fiber synapses. J. Neurosci. 2007;27:9022–31. doi: 10.1523/JNEUROSCI.1954-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Stevanin G, Brice A. Spinocerebellar ataxia 17 (SCA17) and Huntington's disease-like 4 (HDL4) Cerebellum. 2008;7:170–8. doi: 10.1007/s12311-008-0016-1. [DOI] [PubMed] [Google Scholar]
- 201.Sturm B, Stupphann D, Kaun C, Boesch S, Schranzhofer M, Wojta J, Goldenberg H, Scheiber-Mojdehkar B. Recombinant human erythropoietin: effects on frataxin expression in vitro. Eur. J. Clin. Invest. 2005;35:711–717. doi: 10.1111/j.1365-2362.2005.01568.x. [DOI] [PubMed] [Google Scholar]
- 202.Szlago M, Gallus G N, Schenone A, Patiño ME, Sfaelo Z, Rufa A, Pozzo P Da, Cardaioli E, Dotti M T, Federico A. The first cerebrotendinous xanthomatosis family from Argentina: a new mutation in CYP27A1 gene. Neurology. 2008;70:402–404. doi: 10.1212/01.wnl.0000280460.28039.3d. [DOI] [PubMed] [Google Scholar]
- 203.Tabbaa S, Dlugos C, Pentney R. The number of granule cells and spine density on Purkinje cells in aged, ethanol-fed rats. Alcohol. 1999;17:253–60. doi: 10.1016/s0741-8329(98)00059-7. [DOI] [PubMed] [Google Scholar]
- 204.Takei A, Fukazawa T, Hamada T, Sohma H, Yabe I, Sasaki H, Tashiro K. Effects of tandospirone on ‘5-HT1A receptor associated symptoms’ in patients with Machado-Joseph disease: An open label study. Clin. Neuropharmacol. 2004;27:9–13. doi: 10.1097/00002826-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 205.Takiyama Y. Sacsinopathies: sacsin-related ataxia. Cerebellum. 2007;1:7. doi: 10.1080/14734220701230466. [DOI] [PubMed] [Google Scholar]
- 206.Tanimura A, Kawata S, Hashimoto K, Kano M. Not glutamate but endocannabinoids mediate retrograde suppression of cerebellar parallel fiber to Purkinje cell synaptic transmission in young adult rodents. Neuropharmacology. 2009 doi: 10.1016/j.neuropharm.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 207.Thoma P, Bellebaum C, Koch B, Schwarz M, Daum I. The cerebellum is involved in reward-based reversal learning. Cerebellum. 2008;7:433–43. doi: 10.1007/s12311-008-0046-8. [DOI] [PubMed] [Google Scholar]
- 208.Timmann D, Brandauer B, Hermsdörfer J, Ilg W, Konczak J, Gerwig M, Gizewski ER, Schoch B. Lesion-symptom mapping of the human cerebellum. Cerebellum. 2008;7:602–6. doi: 10.1007/s12311-008-0066-4. [DOI] [PubMed] [Google Scholar]
- 209.Timmann D, Lee P, Watts S, Hore J. Kinematics of arm joint rotations in cerebellar and unskilled subjects associated with the inability to throw fast. Cerebellum. 2008;7:366–78. doi: 10.1007/s12311-008-0037-9. [DOI] [PubMed] [Google Scholar]
- 210.Tolbert DL, Clark BR. GDNF and IGF-I trophic factors delay hereditary Purkinje cell degeneration and the progression of gait ataxia. Exp. Neurol. 2003;183:205–19. doi: 10.1016/s0014-4886(03)00172-9. [DOI] [PubMed] [Google Scholar]
- 211.Tonon C, Lodi R. Idebenone in Friedreich’s ataxia. Expert Opin. Pharmacother. 2008;9:2327–2337. doi: 10.1517/14656566.9.13.2327. [DOI] [PubMed] [Google Scholar]
- 212.Torvik A. Two types of brain lesions in Wernicke's encephalopathy. Neuropathol. Appl. Neurobiol. 1985;11:179–90. doi: 10.1111/j.1365-2990.1985.tb00016.x. [DOI] [PubMed] [Google Scholar]
- 213.Traiffort E, Leurs R, Arrang JM, Tardivel-Lacombe J, Diaz J, Schwartz JC, Ruat M. Guinea pig histamine H1 receptor. I. Gene cloning, characterization, and tissue expression revealed by in situ hybridization. J. Neurochem. 1994;62:507–18. doi: 10.1046/j.1471-4159.1994.62020507.x. [DOI] [PubMed] [Google Scholar]
- 214.Trujillo-Martín MM, Serrano-Aguilar P, Monton-Alvarez F, Carrillo-Fumero R. Effectiveness and safety of treatments for degenerative ataxias: a systematic review. Mov. Disord. 2009;24:1111–24. doi: 10.1002/mds.22564. [DOI] [PubMed] [Google Scholar]
- 215.Tsuji S, Onodera O, Goto J, Nishizawa M. Sporadic ataxias in Japan--a population-based epidemiological study. Study Group on Ataxic Diseases. Cerebellum. 2008;7:189–97. doi: 10.1007/s12311-008-0028-x. [DOI] [PubMed] [Google Scholar]
- 216.Tsutsui K. Neurosteroids in the Purkinje cell: biosynthesis, mode of action and functional significance. Mol. Neurobiol. 2008;37:116–25. doi: 10.1007/s12035-008-8024-1. [DOI] [PubMed] [Google Scholar]
- 217.Tsutsui K. Progesterone biosynthesis and action in the developing neuron. Endocrinology. 2008;149:2757–61. doi: 10.1210/en.2007-1592. [DOI] [PubMed] [Google Scholar]
- 218.Turgeon SM, Albin RL. Pharmacology, distribution, cellular localization, and development of GABAB binding in rodent cerebellum. Neuroscience. 1993;55:311–23. doi: 10.1016/0306-4522(93)90501-6. [DOI] [PubMed] [Google Scholar]
- 219.Underwood BR, Rubinsztein DC. Spinocerebellar ataxias caused by polyglutamine expansions: a review of therapeutic strategies. Cerebellum. 2008;7:215–21. doi: 10.1007/s12311-008-0026-z. [DOI] [PubMed] [Google Scholar]
- 220.Van de Warrenburg BP, Sinke RJ, Kremer B. Recent advances in hereditary spinocerebellar ataxias. J. Neuropathol. Exp. Neurol. 2005;64:171–80. doi: 10.1093/jnen/64.3.171. [DOI] [PubMed] [Google Scholar]
- 221.Van Raamsdonk JM. Loss of function mutations in SIL1 cause Marinesco-Sjögren syndrome. Clin. Genet. 2006;69:399–400. doi: 10.1111/j.1399-0004.2006.00595a.x. [DOI] [PubMed] [Google Scholar]
- 222.Vermeer S, Meijer RP, Pijl BJ, Timmermans J, Cruysberg JR, Bos MM, Schelhaas HJ, Van de Warrenburg BP, Knoers NV, Scheffer H, Kremer B. ARSACS in the Dutch population: a frequent cause of early-onset cerebellar ataxia. Neurogenetics. 2008;9:207–14. doi: 10.1007/s10048-008-0131-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Verrips A, Hoefsloot LH, Steenbergen GCH, Theelen JP, Wevers R, Gabreëls FJM, van Engelen BGM, van den Heuve LPWJ. Clinical and molecular genetic characteristics of patients with cerebrotendinous xanthomatosis. Brain. 2000;123:908–919. doi: 10.1093/brain/123.5.908. [DOI] [PubMed] [Google Scholar]
- 224.Villanueva-Haba V, Garcés-Sánchez M, Bataller L, Palau F, Vílchez J. Neuroimaging study with morphometric analysis of hereditary and idiopathic ataxia. Neurologia. 2001;16:105–11. [PubMed] [Google Scholar]
- 225.Viscomi MT, Latini L, Florenzano F, Bernardi G, Molinari M. Minocycline attenuates microglial activation but fails to mitigate degeneration in inferior olive and pontine nuclei after focal cerebellar lesion. Cerebellum. 2008;7:401–5. doi: 10.1007/s12311-008-0042-z. [DOI] [PubMed] [Google Scholar]
- 226.Voutsinos B, Dutuit M, Reboul A, Fevre-Montange M, Bernard A, Trouillas P, Akaoka H, Belin MF, Didier-Bazès M. Serotoninergic control of the activity and expression of glial GABA transporters in the rat cerebellum. Glia. 1998;23:45–60. [PubMed] [Google Scholar]
- 227.Webb TI, Lynch JW. Molecular pharmacology of the glycine receptor chloride channel. Curr. Pharm. Des. 2007;13:2350–67. doi: 10.2174/138161207781368693. [DOI] [PubMed] [Google Scholar]
- 228.Whitney ER, Kemper TL, Bauman ML, Rosene DL, Blatt GJ. Cerebellar Purkinje cells are reduced in a subpopulation of autistic brains: a stereological experiment using calbindin-D28k. Cerebellum. 2008;7:406–16. doi: 10.1007/s12311-008-0043-y. [DOI] [PubMed] [Google Scholar]
- 229.Wieczorek S, Arning L, Alheite I, Epplen JT. Mutations of the puratrophin-1 (PLEKHG4) gene on chromosome 16q22.1 are not a common genetic cause of cerebellar ataxia in a European population. J. Hum. Genet. 2006;51:363–7. doi: 10.1007/s10038-006-0372-y. [DOI] [PubMed] [Google Scholar]
- 230.Wiklund L, Toggenburger G, Cuénod M. Selective retrograde labelling of the rat olivocerebellar climbing fiber system with D-[3H]aspartate. Neuroscience. 1984;13:441–68. doi: 10.1016/0306-4522(84)90242-2. [DOI] [PubMed] [Google Scholar]
- 231.Wokke J. Riluzole. Lancet. 1996;348:795–9. doi: 10.1016/S0140-6736(96)03181-9. [DOI] [PubMed] [Google Scholar]
- 232.Xiang H, Lin C, Ma X, Zhang Z, Bower JM, Weng X, Gao JH. Involvement of the cerebellum in semantic discrimination: an fMRI study. Hum. Brain Mapp. 2003;18:208–14. doi: 10.1002/hbm.10095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Yabe I, Sasaki H, Yamashita I, Takei A, Tashiro K. Clinical trial of acetazolamide in SCA6, with assessment using the Ataxia Rating Scale and body stabilometry. Acta Neurol. Scand. 2001;104(1):44–7. doi: 10.1034/j.1600-0404.2001.00299.x. [DOI] [PubMed] [Google Scholar]
- 234.Yabe I, Sasaki H, Yamashita I, Takei A, Fukazawa T, Hamada T, Tashiro K. A clinical trial of acetazolamide for SCA 6. Clin. Neurol. 2006;39:793–799. [PubMed] [Google Scholar]
- 235.Yamashita T, Ando Y, Obayashi K, Terazaki H, Sakashita N, Uchida K, Ohama E, Ando M, Uchino M. Oxidative injury is present in Purkinje cells in patients with olivopontocerebellar atrophy. J. Neurol. Sci. 2000;175:107–10. doi: 10.1016/s0022-510x(00)00296-3. [DOI] [PubMed] [Google Scholar]
- 236.Yis U, Kurul SH, Cakmakçi H, Dirik E. Acute cerebellitis with cerebellar swelling successfully treated with standard dexamethasone treatment. Cerebellum. 2008;7:430–2. doi: 10.1007/s12311-008-0045-9. [DOI] [PubMed] [Google Scholar]
- 237.Zahniser NR, Doolen S. Chronic and acute regulation of Na+/Cl- -dependent neurotransmitter transporters: drugs, sub-strates, presynaptic receptors, and signaling systems. Pharmacol. Ther. 2001;92:21–55. doi: 10.1016/s0163-7258(01)00158-9. [DOI] [PubMed] [Google Scholar]
- 238.Zeviani M. The expanding spectrum of nuclear gene mutations in mitochondrial disorders. Semin. Cell Dev. Biol. 2001;12:407–416. doi: 10.1006/scdb.2001.0278. [DOI] [PubMed] [Google Scholar]
- 239.Zühlke C, Bürk K. Spinocerebellar ataxia type 17 is caused by mutations in the TATA-box binding protein. Cerebellum. 2007;6:300–307. doi: 10.1080/14734220601136177. [DOI] [PubMed] [Google Scholar]