Abstract
Purpose of review
Recent findings assessing the utility of neuroimaging and biofluid biomarkers are reviewed that help identify patients with frontotemporal lobar degeneration (FTLD) spectrum abnormality.
Recent findings
Neuroimaging studies using T1 structural MRI and diffusion tensor imaging (DTI) distinguish between patients with FTLD and Alzheimer’s disease, although the reliability of these group-level findings in individual patients has been assessed only rarely. However, innovative analyses such as support vector machine approaches are able to integrate T1 and DTI imaging results and to identify specific MRI profiles that distinguish between individual patients with FTLD and Alzheimer’s disease. Novel radioligand positron emission tomography assessments also can recognize Alzheimer’s disease patients with a clinical phenotype resembling that seen in FTLD. Biofluid studies identify about 15% of patients with FTLD due to a genetic mutation that is associated with the specific histopathologic features of TDP-43 or a tauopathy. Other genetically-based risk factors and targeted proteomic searches of plasma and cerebrospinal fluid have suggested additional markers in sporadic cases of FTLD that will lead to the identification of patients with TDP-43 or tau histopathology.
Summary
Great progress has been made in developing biomarkers for FTLD, but additional work is needed to extend these advances so that the histopathologic abnormality causing FTLD can be specified in an individual patient.
Keywords: biomarker, cerebrospinal fluid, frontotemporal lobar degeneration, neuroimaging
Introduction
Treatment trials for frontotemporal lobar degeneration (FTLD) are beginning to emerge. These trials are targeted at the histopathologic abnormality causing FTLD. The goal of these trials is to change the natural history of this disorder. Detailed descriptions have been developed that characterize the spectrum of FTLD abnormality [1•]. The most common abnormality is FTLD-TDP. This is due to the accumulation of ubiquitinated and hyperphosphorylated transactive DNA-binding protein of approximately 43kD(TDP-43) [2]. A family of conditions associated with the accumulation of the microtubule-associated protein tau constitutes another common cause of FTLD; although somewhat diverse biochemically, these abnormalities are collectively known as FTLD-tau [3]. Conditions contributing to the family of tauopathies include dementia with Pick bodies, corticobasal degeneration and progressive supranuclear palsy. A less common histopathologic finding is FTLD-FUS, related to fused-in-sarcoma immuno-reactive inclusions [4].
Clinical assessment is essential to identify patients with a phenotype corresponding to this FTLD spectrum of abnormality. In fact, there is some concordance between a particular clinical FTLD phenotype and an underlying pathological abnormality. For example, patients with the semantic variant of primary progressive aphasia (svPPA), also known as semantic dementia (SD), frequently have TDP-43 abnormality [5]. The nonfluent/agrammatic form of PPA (naPPA), also known as progressive non-fluent aphasia (PNFA), is said to be associated with a tauopathy [6]. Yet another group of PPA patients have an aphasic form of Alzheimer’s disease, also known as the logopenic variant of PPA (lvPPA) or logopenic progressive aphasia (LPA), and this is frequently confused with other forms of PPA that are due to FTLD spectrum abnormality [7]. A recent survey of unselected clinical–pathological series of PPA patients confirmed this general picture, but emphasized that the association of a clinical phenotype with histopathology at autopsy is less reliable in individual patients [8••]. Likewise, there are rare studies evaluating the clinical characteristics of a social disorder related to FTLD-tau or FTLD-TDP [9], but it is even difficult to distinguish these patients from cases with a frontal variant of autopsy-proven Alzheimer’s disease (fvAD) [10].
Several studies have assessed specific aspects of language and cognition quantitatively in autopsy-proven cases of FTLD. Patients with a TDP-43 proteinopathy were significantly more impaired than patients with a tauopathy or Alzheimer’s disease on measures of confrontation naming and category naming fluency guided by the letters F, A, and S [11–13]. By comparison, patients with tau-positive abnormality were significantly more impaired than patients with a TDP-43 proteinopathy and patients with Alzheimer’s disease on nonlinguistic measures of executive functioning involving visual constructions and reverse digit span [12,13]. Episodic memory was relatively impaired in lvPPA patients with Alzheimer’s disease compared to PPA patients with FTLD-tau or FTLD-TDP abnormality, although memory in the Alzheimer’s disease-PPA patients was significantly superior to that found in typical Alzheimer’s disease patients [3,14]. Whereas highly suggestive at a group level, follow-up observations have shown that quantitative neuropsychological measures are unreliable at identifying histopathology in individual patients [15•].
Whereas the clinical phenotype provides useful screening information suggesting FTLD spectrum abnormality, additional information is needed to improve our ability to define the cause of an individual patient with PPA or bvFTD. Biomarkers thus must be developed to supplement the clinical examination. A biomarker is a validated measure that reliably reflects the underlying pathology of a disease associated with several different abnormalities like FTLD. Some biomarkers are categorical and thus provide diagnostic information. This class of biomarkers should be sensitive to the distinction between healthy controls and patients, and also should be specific enough to distinguish patients with FTLD from patients with other age-associated neurodegenerative conditions like Alzheimer’s disease. Other biomarkers reflect disease severity and the course of the condition, and this class of biomarkers may be useful in trials to determine whether the disease is responding to the treatment. Importantly, these two classes of biomarkers need not involve the same measures. Several biomarker modalities are potentially available to help determine the basis for FTLD. These include neuroimaging, blood and serum studies, and studies of analytes in the cerebrospinal fluid (CSF).
Imaging biomarkers
Combinations of representational and processing nodes within a large-scale, interconnected neural network work together to support crucial aspects of language and social cognition. Progressive interruption of this network results in PPA or bvFTD. Structural and functional imaging studies associate the distinct features of a clinical FTLD syndrome with partially selective interruptions of these large-scale networks, and these anatomic distributions of disease also may reflect a particular histopathologic abnormality.
An example of the anatomic distribution of cortical thinning in the three major PPA syndromes is illustrated in Fig. 1 [8••]. PNFA appears to be related largely to anterior peri-Sylvian atrophy involving inferior, opercular, and insular portions of the left frontal lobe [16,17]. Whereas longitudinal imaging studies are rare, personal observations suggest that atrophy associated with PNFA often extends superiorly into dorsolateral prefrontal cortex, inferiorly into the anterior superior temporal lobe, medially into orbital frontal and anterior cingulate regions, and posteriorly along the Sylvian fissure into the parietal lobe. SD has a different anatomic distribution. Imaging studies associate this syndrome with left anterior temporal atrophy, affecting lateral and ventral surfaces of the temporal lobe as well as the anterior hippocampus and the amygdala [18,19]. Longitudinal studies show atrophy extending in a posterior and superior direction in the ipsilateral temporal lobe, and often involve the adjacent frontal lobe and homologous anterior temporal regions of the right hemisphere [20–22]. LPA tends to be associated with atrophy in a left posterior-peri-Sylvian distribution affecting the temporal–parietal junction [16]. Longitudinal observations have not been published, but personal observation suggests progressive disease involving more inferior regions of the temporal lobe, superior extension into the parietal lobe, and anterior extension along the Sylvian fissure into the frontal lobe.
Figure 1. Cortical atrophy corresponding to primary progressive aphasia syndromes1.
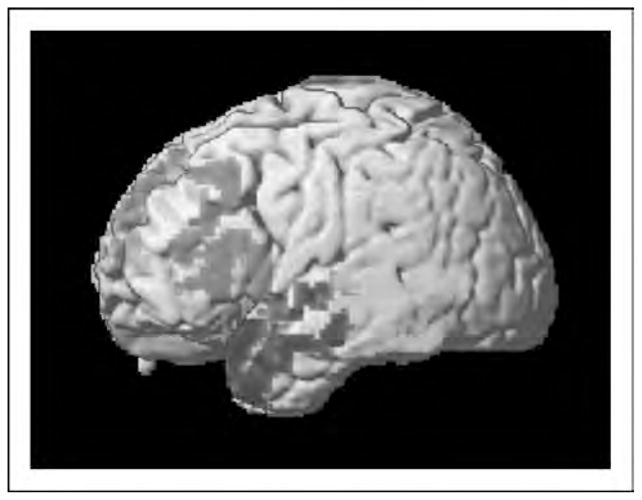
1Frontal = nonfluent/agrammatic variant PPA; anterior temporal = mantic variant; posterior temporal-parietal = logopenic variant. Printed with permission from: Grossman M. Primary progressive aphasia: Clinical-pathological correlations. Nature Reviews Neurology 2010; 88–97.
Rare comparative studies have evaluated whether these characterizations validly reflect specific forms of pathological disease. Some reports have focused on the distinction between FTLD and Alzheimer’s disease. One study compared patients with a fluent form of PPA, including five cases with Alzheimer’s disease and five with FTLD-U abnormality presumably due to TDP-43 [11]. Patients with Alzheimer’s disease had T1 cortical atrophy in a temporal–parietal distribution with sparing of the hippocampus, but FTLD-U cases had sparing of parietal cortex. Reduced parietal cortex functioning was reported in FDG-glucose-PET or SPECT scans of patients with pathologically confirmed PNFA due to Alzheimer’s disease compared to PNFA patients with non-Alzheimer’s disease [23].
Other work has focused on the distinction between FTLD-tau and FTLD-TDP. For example, T1 MRI cortical thinning has been assessed in small groups of PNFA patients with tau-positive disease and SD patients with FTLD-U abnormality, presumably due to TDP-43 [24]. The PNFA patients showed superior temporal and inferior frontal thinning that was more prominent in the left hemisphere than the right hemisphere, and the SD patients showed prominent left anterior temporal thinning.
We are aware of only one study assessing the validity of T1 structural imaging to identify abnormality in individual patients. This study examined 34 nonfluent PPA patients with autopsy or CSF-based evidence consistent with underlying FTLD or Alzheimer’s disease [15•]. Subtle but statistically significant differences in the anatomic distribution of cortical atrophy in the FTLD and Alzheimer’s disease subgroups were described. However, a receiver operating characteristic (ROC) curve analysis of MRI cortical atrophy alone revealed an area under the curve of only 0.64, with 72.7% sensitivity and 66.7% specificity.
Recent work also has demonstrated the utility of diffusion tensor imaging (DTI) to distinguish clinical syndromes on the basis of white matter abnormalities. Patients with so-called frontal-variant FTD showed changes most prominently in the superior longitudinal fasciculus, whereas temporal-variant FTD patients showed significant changes in the inferior longitudinal fasciculus [25]. DTI studies in patients with autopsy-confirmed disease have been rare. One preliminary study evaluated clinically diagnosed FTLD patients who had autopsy or CSF-based biomarkers consistent with FTLD or Alzheimer’s disease [26]. Significantly reduced fractional anisotropy was seen in FTLD compared to Alzheimer’s disease in the anterior corpus callosum and the inferior longitudinal fasciculus in the area of the uncinate.
One recent study combined T1 cortical atrophy and DTI to classify 50 individual cases of clinically diagnosed FTLD who had autopsy or CSF-based findings consistent with FTLD or Alzheimer’s disease [27••]. These investigators used a support vector machine technique that selects the optimal voxels from T1 and DTI imaging, and applies the resulting algorithm to categorize individual participants. In FTLD, changes were most prominent in frontal and anterior temporal regions, whereas changes in temporal–parietal brain areas were more evident in Alzheimer’s disease. The algorithm combining T1 and DTI accurately categorized 49 (98%) of the 50 participants.
Recent advances in PET metabolic imaging are poised to provide important advances in determining the specific cause of a FTLD syndrome. This is because of the tracer Pittsburgh Compound B (PiB) that radiolabels beta-amyloid (Aβ), one of the proteins that accumulates in Alzheimer’s disease [28]. By comparison, Aβ does not contribute to FTLD spectrum abnormality. One study described reduced PiB uptake in 8 of 12 clinically diagnosed FTLD patients [29]. A follow-up study of PPA reported PiB uptake in all four of the lvPPA patients who were evaluated, and signal was strongest in a left temporal–parietal distribution [30]. By comparison, PiB uptake was less common in other PPA syndromes: left frontal uptake was seen in only one of six naPPA patients, and left temporal uptake was seen in only one of five svPPA patients. Although only small numbers of non-autopsied patients were studied, these findings are consistent with clinical-pathological studies showing that lvPPA is associated with Alzheimer’s disease pathology more commonly than naPPA and svPPA. Caution should be exercised in interpreting these findings because quantitative analyses of histopathologic burden in PPA patients with Alzheimer’s disease do not always correspond to the expected anatomic distribution of disease for the PPA syndrome [3,7,31].
Whereas PET imaging with PiB is available only at a few specialized centers, functional neuroimaging with arterial spin labeling (ASL) perfusion MRI is widely available. Using ASL, a signature abnormality of hypoperfusion in frontal regions and hyperperfusion in parietal regions has been identified in patients with autopsy and CSF-defined FTLD [32]. Moreover, in contrast to patients with autopsy and CSF-defined Alzheimer’s disease, perfusion in FTLD was significantly lower in frontal regions and significantly elevated in temporal–parietal regions.
Genetically related biomarkers in blood
One important source of information about the pathology causing a FTLD syndrome is DNA. This can indicate an inherited mutation in a chromosome coding for a protein associated with a specific histopathologic abnormality leading to FTLD. This is particularly useful because familial disorders are frequent in FTLD. Up to 45% of index cases can have a strongly positive family history [33,34], and about 15% of FTLD patients have an identifiable mutation. In several carefully studied families, for example, naPPA and possibly bvFTD have been associated with a mutation of the GRN gene coding progranulin (PGRN) on chromosome 17 [35,36]. GRN mutations are reliably associated with FTLD-TDP pathology [37–40]. Less common mutations associated with FTLD-TDP pathology include VCP on chromosome 9, CHMP2B on chromosome 3, and TARDBP on chromosome 1. Other familial patients with an FTLD syndrome have a mutation of the microtubule-associated protein tau (MAPT) gene coding tau on chromosome 17. This is associated with tau histopathology [41–43].
It is important to note that the clinical FTLD syndrome can be highly variable, even in patients with the identical GRN mutation [44] or members of a family with the same mutation of GRN [45,46]. Likewise, the phenotype associated with a specific MAPT mutation may be highly variable [47]. The presence of a mutation thus may reliably reflect underlying pathology, but it is difficult to identify the index patients who should be assessed genetically on the basis of a clinical evaluation alone.
Biomarkers also may play a role in defining the risk associated with a particular pathologic basis for an FTLD syndrome in sporadic cases. Tau haplo-types are derived from the region of chromosome 17 that spans the portion in which the MAPT gene is represented. The H1 haplotype is over-represented in conditions associated with tau pathology such as corticobasal degeneration, progressive supranuclear palsy, and sporadic FTLD [48–50]. However, the association of a tau haplotype directly with tau pathology has been verified only rarely [51].
A recent study proposed a risk biomarker associated with TDP-43 pathology. In this genome-wide association study of more than 500 autopsy-proven cases with FTLD-TDP pathology, the investigators reported that TMEM106B, coded on chromosome 7p21, is associated with an increased risk for the presence of TDP-43 pathology. Indeed, it is possible to measure TDP-43 levels directly in plasma. The proportions of FTLD patients (46%) and Alzheimer’s disease patients (22%) with elevated plasma levels of TDP-43 corresponded roughly to the percentages of these populations with TDP-43 detected in the brains at autopsy [52]. A follow-up study correlated plasma levels of phosphorylated TDP-43 with the density of FTLD-TDP brain pathology, although plasma levels of TDP-43 did not distinguish between patients with FTLD and Alzheimer’s disease [53].
Cerebrospinal fluid biomarkers
Another potential source of biomarker information comes from cerebrospinal fluid (CSF). About 20% of individual patients with FTLD had significantly low levels of CSF tau relative to healthy controls, although this was never seen in patients with Alzheimer’s disease, and the ratio of tau to Aβ1–42 was significantly lower in FTLD than Alzheimer’s disease [54]. In patients with known abnormality, the tau : Aβ1–42 ratio was significantly lower in FTLD than Alzheimer’s disease, and a ROC curve analysis showed that a ratio of 1.06 had excellent sensitivity and specificity for distinguishing FTLD from Alzheimer’s disease [55].
TDP-43 levels have been assayed in the CSF of patients with a clinical diagnosis of FTLD, and in ALS in which the vast majority of patients have TDP-43 pathology [56,57]. Significantly elevated CSF levels of TDP-43 were reported. However, the participants in these studies did not have autopsy-proven disease, TDP-43 levels of patients overlapped with those of controls, and this work has not been able to dissociate tau-positive disease from a TDP-43 proteinopathy in individual cases.
Since levels of these CSF biomarkers overlap with those of healthy controls, it is important to extend the hunt to identify other, potentially informative biomarkers. A targeted proteomic search thus attempted to identify novel CSF biomarkers that distinguish between 66 autopsy-confirmed cases of Alzheimer’s disease and a group of 25 patients in whom 92% had FTLD spectrum abnormality [58]. Three converging statistical strategies identified phosphorylated-tau181, Aβ1–42, and agouti-related peptide (AgRP) as useful classifying analytes. AgRP levels were significantly elevated in a high proportion of FTLD-TDP cases, but were elevated only rarely in FTLD-tau cases. A follow-up study pursued this finding in the CSF of 14 patients with FTLD-TDP and 9 patients with FTLD-tau [59•]. In addition to AgRP, four analytes were identified as distinguishing biomarkers, including adrenocorticotropic hormone (ACTH), eotaxin-3, Fas, and interleukin 17 (IL-17).
Conclusion
Significant advances have occurred recently that suggest the potential usefulness of imaging and biofluid biomarkers in the identification of the specific histopathologic abnormality causing a FTLD clinical syndrome. Following a careful clinical screening, a two-stage diagnostic approach appears to be emerging to identify histopathology in FTLD. First, imaging studies appear to be useful at distinguishing FTLD from patients with Alzheimer’s disease. Biomarkers in blood then can identify patients with a genetic mutation that is associated with FTLD-tau or FTLD-TDP histopathology, although this represents only about 15% of patients with a FTLD clinical syndrome. Studies of CSF and plasma are beginning to identify the specific histopathologic abnormality in patients with a sporadic FTLD syndrome. These findings, whereas not yet definitive enough to identify the causative disease in individual patients, point the way for future work that will support the accurate identification of patients who are eligible for trials targeted at the specific histopathologic abnormalities causing FTLD.
Acknowledgments
The study was supported in part by funding from NIH (AG15116, AG17586, NS44266, NS53488, AG32953).
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Additional references related to this topic can also be found in the Current World Literature section in this issue (pp. 708–709).
- 1•.Mackenzie IR, Neumann M, Bigio E, et al. Nomenclature for neuropathologic subtypes of frontotemporal lobar degeneration: consensus recommendations. Acta Neuropathologica. 2009;117:15–18. doi: 10.1007/s00401-008-0460-5. Important nosologic characterization of FTLD spectrum abnormality. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neumann M, Sampathu DM, Kwong LK, et al. Ubiquinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclereosis. Science. 2006;314:130–133. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 3.Forman MS, Farmer J, Johnson JK, et al. Frontotemporal dementia: clinico-pathological correlations. Ann Neurol. 2006;59:952–962. doi: 10.1002/ana.20873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neumann M, Rademakers R, Roeber S, et al. Frontotemporal lobar degeneration with FUS pathology. Brain. 2009:awp214. doi: 10.1093/brain/awp214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snowden J, Neary D, Mann D. Frontotemporal lobar degeneration: clinical and pathological relationships. Acta Neuropathologica. 2007;114:31–38. doi: 10.1007/s00401-007-0236-3. [DOI] [PubMed] [Google Scholar]
- 6.Josephs KA, Duffy JR, Strand EA, et al. Clinicopathological and imaging correlates of progressive aphasia and apraxia of speech. Brain. 2006;129:1385–1398. doi: 10.1093/brain/awl078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mesulam M, Wicklund A, Johnson N, et al. Alzheimer and frontotemporal pathology in subsets of primary progressive aphasia. Ann Neurol. 2008;63:709–719. doi: 10.1002/ana.21388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8••.Grossman M. Primary progressive aphasia: clinical-pathological correlations. Nature Rev Neurol. 2010;6:88–97. doi: 10.1038/nrneurol.2009.216. Comprehensive summary of clinical–pathological correlations and biomarker approaches to the primary progressive aphasias. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hu WT, Mandrekar JN, Parisi JE, et al. Clinical features of pathologic subtypes of behavioral-variant frontotemporal dementia. Arch Neurol. 2007;64:1611–1616. doi: 10.1001/archneur.64.11.1611. [DOI] [PubMed] [Google Scholar]
- 10.Johnson JK, Head E, Kim R, et al. Clinical and pathological evidence for a frontal variant of Alzheimer disease. Arch Neurol. 1999;56:1233–1239. doi: 10.1001/archneur.56.10.1233. [DOI] [PubMed] [Google Scholar]
- 11.Josephs KA, Whitwell JL, Duffy JR, et al. Progressive aphasia secondary to Alzheimer disease vs. FTLD pathology. Neurology. 2008;70:25–34. doi: 10.1212/01.wnl.0000287073.12737.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grossman M, Xie SX, Libon DJ, et al. Longitudinal decline in autopsy-defined frontotemporal lobar degeneration. Neurology. 2008;70:2036–2045. doi: 10.1212/01.wnl.0000303816.25065.bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grossman M, Libon DJ, Forman MS, et al. Distinct antemortem profiles in patients with pathologically defined frontotemporal dementia. Arch Neurol. 2007;64:1601–1609. doi: 10.1001/archneur.64.11.1601. [DOI] [PubMed] [Google Scholar]
- 14.Rascovsky K, Salmon DP, Ho GJ, et al. Cognitive profiles differ in autopsy-confirmed frontotemporal dementia and AD. Neurology. 2002;58:1801–1808. doi: 10.1212/wnl.58.12.1801. [DOI] [PubMed] [Google Scholar]
- 15•.Hu WT, McMillan C, Libon DJ, et al. Multimodal predictors for Alzheimer’s disease in nonfluent primary progressive aphasia. Neurology. 2010;75:595–602. doi: 10.1212/WNL.0b013e3181ed9c52. Integrated clinical, quantitative neuropsychological and imaging method to evaluate histopathologic basis for nonfluent forms of PPA in individual cases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorno-Tempini M, Dronkers NF, Rankin KP, et al. Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol. 2004;55:335–346. doi: 10.1002/ana.10825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peelle JE, Troiani V, Gee JC, et al. Sentence comprehension and voxel-based morphometry in progressive nonfluent aphasia, semantic dementia, and nonaphasic frontotemporal dementia. J Neuroling. 2008;21:418–432. doi: 10.1016/j.jneuroling.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mummery CJ, Patterson K, Price CJ, Hodges JR. A voxel-based morphometry study of semantic dementia: relationship between temporal lobe atrophy and semantic memory. Ann Neurol. 2000;47:36–45. [PubMed] [Google Scholar]
- 19.Bonner MF, Vesely L, Price C, et al. Reversal of the concreteness effect in semantic dementia. Cogn Neuropsychol. 2009;26:568–579. doi: 10.1080/02643290903512305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Avants B, Anderson C, Grossman M, Gee JC. Spatiotemporal normalization for longitudinal analysis of gray matter atrophy in frontotemporal dementia. Med Image Comput Computer-Assist Interven. 2007;10:309–310. doi: 10.1007/978-3-540-75759-7_37. [DOI] [PubMed] [Google Scholar]
- 21.Rohrer JD, McNaught E, Foster J, et al. Tracking progression in frontotemporal lobar degeneration: serial MRI in semantic dementia. Neurology. 2008;71:1445–1451. doi: 10.1212/01.wnl.0000327889.13734.cd. [DOI] [PubMed] [Google Scholar]
- 22.Brambati SM, Rankin KP, Narvid J, et al. Atrophy progression in semantic dementia with asymmetric temporal involvement: a tensor-based morphometry study. Neurobiol Aging. 2009;30:103–111. doi: 10.1016/j.neurobiolaging.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nestor PJ, Balan K, Cheow HK, et al. Nuclear imaging can predict pathologic diagnosis in progressive nonfluent aphasia. Neurology. 2007;68:238–239. doi: 10.1212/01.wnl.0000251309.54320.9f. [DOI] [PubMed] [Google Scholar]
- 24.Rohrer JD, Warren JD, Modat M, et al. Patterns of cortical thinning in the language variants of frontotemporal lobar degeneration. Neurology. 2009;72:1562–1569. doi: 10.1212/WNL.0b013e3181a4124e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borroni B, Brambati SM, Agosti C, et al. Evidence of white matter changes on diffusion tensor imaging in frontotemporal dementia. Arch Neurol. 2007;64:246–251. doi: 10.1001/archneur.64.2.246. [DOI] [PubMed] [Google Scholar]
- 26.Hu WT, Zhang H, McMillan C, et al. Distinct white matter changes in frontotemporal dementia associated with FTLD and Alzheimer’s pathology or CSF biomarkers. Neurology. 2010;74:A569. [Google Scholar]
- 27••.Avants BB, Cook PA, Ungar L, et al. Dementia induces correlated reductions in white matter integrity and cortical thickness: a multivariate neuroimaging study with sparse canonical correlation analysis. Neuroimage. 2010;50:1004–1016. doi: 10.1016/j.neuroimage.2010.01.041. Novel support vector machine approach that integrates multiple imaging modalities for the purpose of categorizing individual patients as FTLD or Alzheimer’s disease based on autopsy or CSF-based criteria. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klunk W, Engler H, Nordberg A, et al. Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann Neurol. 2004;55:306–319. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- 29.Rabinovici GD, Furst AJ, O’Neil JP, et al. 11C-PIB PET imaging in Alzheimer disease and frontotemporal lobar degeneration. Neurology. 2007;68:1205–1212. doi: 10.1212/01.wnl.0000259035.98480.ed. [DOI] [PubMed] [Google Scholar]
- 30.Rabinovici GD, Jagust WM, Furst AJ, et al. Abeta amyloid and glucose metabolism in three variants of primary progressive aphasia. Ann Neurol. 2008;64:388–401. doi: 10.1002/ana.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Munoz D, Woulfe J, Kertesz A. Argyrophilic thorny astrocyte clusters in association with Alzheimer’s disease pathology in possible primary progressive aphasia. Acta Neuropathol. 2007;114:347–357. doi: 10.1007/s00401-007-0266-x. [DOI] [PubMed] [Google Scholar]
- 32.Hu WT, Wang Z, Lee VMY, et al. Distinct cerebral perfusion patterns in FTLD and AD. Neurology. 2010;75:881–888. doi: 10.1212/WNL.0b013e3181f11e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chow TW, Miller BL, Hayashi VN, Geschwind DH. Inheritance of frontotemporal dementia. Arch Neurol. 1999;56:817–822. doi: 10.1001/archneur.56.7.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seelaar H, Kamphorst W, Rosso SM, et al. Distinct genetic forms of frontotemporal dementia. Neurology. 2008;71:1220–1226. doi: 10.1212/01.wnl.0000319702.37497.72. [DOI] [PubMed] [Google Scholar]
- 35.Snowden JS, Pickering-Brown SM, Mackenzie IR, et al. Progranulin gene mutations associated with frontotemporal dementia and progressive nonfluent aphasia. Brain. 2006;129:3091–3102. doi: 10.1093/brain/awl267. [DOI] [PubMed] [Google Scholar]
- 36.Mesulam M, Johnson N, Krefft TA, et al. Progranulin mutations in primary progressive aphasia: the PPA1 and PPA3 families. Arch Neurol. 2007;64:43–47. doi: 10.1001/archneur.64.1.43. [DOI] [PubMed] [Google Scholar]
- 37.Baker M, Mackenzie IR, Pickering-Brown SM, et al. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature. 2006;442:916–919. doi: 10.1038/nature05016. [DOI] [PubMed] [Google Scholar]
- 38.Davidson Y, Kellley T, Mackenzie IR, et al. Ubiquitinated pathological lesions in frontotemporal lobar degeneration contain the TAR DNA-binding protein, TDP-43. Acta Neuropathol. 2007:113. doi: 10.1007/s00401-006-0189-y. [DOI] [PubMed] [Google Scholar]
- 39.Mackenzie I. The neuropathology and clinical phenotype of FTD with progranulin mutations. Acta Neuropathol. 2007;114:49–54. doi: 10.1007/s00401-007-0223-8. [DOI] [PubMed] [Google Scholar]
- 40.Gass J, Cannon A, Mackenzie IR, et al. Mutations in progranulin are a major cause of ubiquitin-positive frontotemporal lobar degeneration. Hum Molec Genet. 2006;15:2988–3001. doi: 10.1093/hmg/ddl241. [DOI] [PubMed] [Google Scholar]
- 41.Hong M, Zhukareva V, Vogelsberg-Ragaglia V, et al. Mutation-specific functional impairments in distinct tau isoforms of hereditary FTDP-17. Science. 1998;282:1914–1917. doi: 10.1126/science.282.5395.1914. [DOI] [PubMed] [Google Scholar]
- 42.Lee VMY, Goedert M, Trojanowski JQ. Neurodegenerative tauopathies. Annu Rev Neurosci. 2001;24:1121–1159. doi: 10.1146/annurev.neuro.24.1.1121. [DOI] [PubMed] [Google Scholar]
- 43.Zhukareva V, Vogelsberg-Ragaglia V, Van Deerlin VMD, et al. Loss of brain tau defines novel sporadic and familial tauopathies with frontotemporal dementia. Ann Neurol. 2001;49:165–175. doi: 10.1002/1531-8249(20010201)49:2<165::aid-ana36>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 44.Rademakers R, Baker M, Gass J, et al. Phenotypic variability associated with progranulin haploinsufficiency in patients with the common 1477C–>T (Arg493X) mutation: an international initiative. Lancet Neurol. 2007;6:857–868. doi: 10.1016/S1474-4422(07)70221-1. [DOI] [PubMed] [Google Scholar]
- 45.Le Ber I, Camuzat A, Hannequin D, et al. Phenotype variability in progranulin mutation carriers: a clinical, neuropsychological, imaging and genetic study. Brain. 2008;131:732–746. doi: 10.1093/brain/awn012. [DOI] [PubMed] [Google Scholar]
- 46.Leverenz JB, Yu CE, Montine TJ, et al. A novel progranulin mutation associated with variable clinical presentation and tau, TDP43 and alpha-synuclein pathology. Brain. 2007;130:1360–1374. doi: 10.1093/brain/awm069. [DOI] [PubMed] [Google Scholar]
- 47.Bird TD, Nochlin D, Poorkaj P, et al. A clinical pathological comparison of three families with frontotemporal dementia and identical mutations in the tau gene (P301L) Brain. 1999;122:741–756. doi: 10.1093/brain/122.4.741. [DOI] [PubMed] [Google Scholar]
- 48.Houlden H, Baker M, Morris HR, et al. Corticobasal degeneration and progressive supranuclear palsy share a common tau haplotype. Neurology. 2001;56:1702–1706. doi: 10.1212/wnl.56.12.1702. [DOI] [PubMed] [Google Scholar]
- 49.Hughes A, Mann DMA, Pickering-Brown S. Tau haplotype frequency in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Experiment Neurol. 2003;181:12–16. doi: 10.1016/s0014-4886(03)00024-4. [DOI] [PubMed] [Google Scholar]
- 50.Pittman AM, Myers AJ, Duckworth J, et al. The structure of the tau haplotype in controls and in progressive supranuclear palsy. Hum Mol Genet. 2004;13:1267–1274. doi: 10.1093/hmg/ddh138. [DOI] [PubMed] [Google Scholar]
- 51.Morris HR, Baker M, Yasojima K, et al. Analysis of tau haplotypes in Pick’s disease. Neurology. 2002;59:443–445. doi: 10.1212/wnl.59.3.443. [DOI] [PubMed] [Google Scholar]
- 52.Foulds P, McAuley E, Gibbons L, et al. TDP-43 protein in plasma may index TDP-43 brain pathology in Alzheimer’s disease and frontotemporal lobar degeneration. Acta Neuropathol. 2008;116:141–146. doi: 10.1007/s00401-008-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Foulds P, Davidson Y, Mishra M, et al. Plasma phosphorylated-TDP-43 protein levels correlate with brain pathology in frontotemporal lobar degeneration. Acta Neuropathol. 2009;118:647–658. doi: 10.1007/s00401-009-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grossman M, Farmer J, Leight S, et al. Cerebrospinal fluid profile distinguishes frontotemporal dementia from Alzheimer’s disease. Ann Neurol. 2005;57:721–729. doi: 10.1002/ana.20477. [DOI] [PubMed] [Google Scholar]
- 55.Bian H, van Sweiten JC, Leight S, et al. Cerebrospinal fluid biomarkers in frontotemporal lobar degeneration with known pathology. Neurology. 2008;70:1827–1835. doi: 10.1212/01.wnl.0000311445.21321.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Steinacker P, Hendrich C, Sperfeld AD, et al. TDP-43 in cerebrospinal fluid of patients with frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Arch Neurol. 2008;65:1481–1487. doi: 10.1001/archneur.65.11.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kasai T, Tokuda T, Ishigami N, et al. Increased TDP-43 protein in cerebrospinal fluid of patients with amyotrophic lateral sclerosis. Acta Neuropathol. 2009;117:55–62. doi: 10.1007/s00401-008-0456-1. [DOI] [PubMed] [Google Scholar]
- 58.Hu WT, Chen-Plotkin A, Arnold SE, et al. Novel CSF biomarkers for Alzheimer’s disease and mild cognitive impairment. Acta Neuropathol. 2010;119:669–678. doi: 10.1007/s00401-010-0667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59•.Hu WT, Chen-Plotkin A, Grossman M, et al. Novel CSF biomarkers for frontotemporal lobar degenerations. Neurology. 2010 doi: 10.1212/WNL.0b013e318200d78d. in press Battery of CSF analytes that distinguishes between FTLD-TDP and FTLD-tau in autopsy-proven cases. [DOI] [PMC free article] [PubMed] [Google Scholar]


