Abstract
Background
Extracranial internal carotid artery dissection (eICAD) is a leading cause of stroke in younger patients.
Objectives
1. To determine whether, in patients with eICAD, treatment with anticoagulants, antiplatelet agents or control was associated with a better functional outcome. 2. To compare, among patients treated with either anticoagulants or antiplatelet agents, the risk of ischaemic strokes and major bleeding episodes.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched 3 October 2009). In addition, we performed comprehensive searches of the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library Issue 2, 2009), MEDLINE (January 1966 to November 2009) and EMBASE (January 1980 to November 2009), checked all relevant papers for additional eligible studies and contacted authors and researchers in the field.
Selection criteria
Randomised controlled trials, controlled clinical trials and non‐randomised studies (if they reported on outcome stratified by antithrombotic treatment and included at least four patients) of anticoagulants or antiplatelet agents for the treatment of extracranial internal carotid artery dissection. Two review authors independently extracted data.
Data collection and analysis
Primary outcomes were death (all causes) and death or disability. Secondary outcomes were ischaemic stroke, symptomatic intracranial haemorrhage, and major extracranial haemorrhage during the reported follow‐up period. The first choice treatment was taken for analyses.
Main results
We did not find any completed randomised trials. Comparing antiplatelets with anticoagulants across 36 observational studies (1285 patients), there were no significant differences in the odds of death (Peto odds ratio (Peto OR) 2.02, 95% CI 0.62 to 6.60), or the occurrence of ischaemic stroke (OR 0.63, 95% CI 0.21 to 1.86) (34 studies, 1262 patients). For the outcome of death or disability, there was a non‐significant trend in favour of anticoagulants (OR 1.77, 95% CI 0.98 to 3.22; P = 0.06) (26 studies, 463 patients). Symptomatic intracranial haemorrhages (5/627; 0.8%) and major extracranial haemorrhages (7/425; 1.6%) occurred only in the anticoagulation group; however, for both these outcomes, the estimates were imprecise and indicated no significant difference between the two treatment modalities.
Authors' conclusions
There were no randomised trials comparing either anticoagulants or antiplatelet drugs with control, thus there is no evidence to support their routine use for the treatment of extracranial internal carotid artery dissection. There were also no randomised trials that directly compared anticoagulants with antiplatelet drugs and the reported non‐randomised studies did not show any evidence of a significant difference between the two.
Keywords: Humans; Anticoagulants; Anticoagulants/therapeutic use; Carotid Artery, Internal, Dissection; Carotid Artery, Internal, Dissection/drug therapy; Controlled Clinical Trials as Topic; Fibrinolytic Agents; Fibrinolytic Agents/therapeutic use; Platelet Aggregation Inhibitors; Platelet Aggregation Inhibitors/therapeutic use
Plain language summary
Antithrombotic drugs for carotid artery dissection
Carotid artery dissection means a tear in the lining in one of the main blood vessels carrying blood to the brain. Dissection can be caused by injury to the neck, but can sometimes develop for no obvious reason. Blood clots can form where the artery is torn. These blood clots can then block the artery and cause a stroke. Blood thinning drugs such as aspirin and anticoagulants might prevent clots forming and so prevent stroke in people with carotid artery dissection. We did not find any completed randomised trials testing these drugs in people with carotid artery dissection. However, there is one ongoing trial. We found only poor quality non‐randomised studies that compared anticoagulants with aspirin. There was no evidence that anticoagulants were better than aspirin. Aspirin is likely to be similarly effective and safe as anticoagulants in such patients. More research is needed.
Background
Extracranial internal carotid artery dissection (eICAD) can lead to the occlusion of the artery. It is the underlying stroke mechanism in approximately 2.5% of all strokes (Bogousslavsky 1987b), compared with between 5% and 22% in young stroke patients, hence being among the leading causes of stroke in patients younger than 45 years (Bogousslavsky 1987a; Gautier 1989; Leys 2002Lisovoski 1991; Rouhart 1993). It was first recognised as a cause of ischaemic stroke in the mid‐1950s (Anderson 1959; Jentzer 1954), although there are pathological reports on the condition dating from 1872 (Richaud 1980). The incidence is about 1.7 to 3/100,000 per year (Giroud 1994; Lee 2006; Schievink 1993). The recurrence rate of CAD is less than 1% per year (Beletsky 2003; Giroud 1994; Lee 2006; Schievink 1993; Touze 2003) except for familial cases. It is still debated whether, in eICAD patients, anticoagulation or antiplatelet agents are superior, balancing risk and benefits of either approach (New Reference; Lyrer 2004; Lyrer 2005; Norris 2005). Anticoagulation is widely advocated (Cimini 2004; Hart 1983; Sturzenegger 1995) and often used (Menon 2008b). However, there is no reliable evidence from randomised trials for the efficacy of this therapy (Leys 1997; Schievink 2001). The beneficial effect of anticoagulants over antiplatelets may be offset by an increase in the number of bleedings (IST 1997).
Case observations of worsening of carotid stenosis suggested the occurrence of anticoagulation‐mediated perpetuation of intramural bleeding in some patients with eICAD (Dreier 2004; Fluri 2007; Mokri 1986). As a consequence, haemodynamic worsening might occur, which implies the risk of low‐flow infarcts (Arauz 2006; Dreier 2004).
Objectives
The objective of this systematic review was to evaluate the efficacy and safety of anticoagulants (AC) versus antiplatelet drugs (AP) in patients with eICAD. Our primary objective was to determine whether patients with eICAD receiving AC were more likely to have a better functional outcome such as not being dead or not being disabled, compared with those receiving AP.
Our secondary objectives were to evaluate:
whether patients had fewer ischaemic strokes, defined as the occurrence or recurrence of cerebral or retinal ischaemic events lasting more than 24 hours, when treated with AC compared with AP;
whether patients had more haemorrhages (symptomatic intracranial or major extracranial bleedings) when treated with AC compared with those treated with AP.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs), controlled clinical trials (CCTs), non‐randomised studies or case series including at least four patients with eICAD that allowed comparisons between antithrombotic treatments for eICAD were eligible.
We sought information on the description of the diagnostic methods, the clinical presentation and the diagnostic findings. We searched for all information concerning treatment and all outcomes stratified to the used antithrombotic option (i.e. AP and AC). We included all studies that reported at least one primary outcome comparing patients treated with AC versus those treated with AP. We excluded studies reporting on a single treatment modality.
We excluded studies from any analysis when:
there were three or fewer cases;
they consisted of reviews summarising case reports;
they were series with data repetition from former citations (we included only the most recent series);
we could not make the distinction between dissections of internal carotid artery, common carotid artery, vertebral artery, or intracranial carotid artery dissection.
Types of participants
Studies and series reporting patients who had experienced eICAD were eligible. Patients with stroke, transient ischaemic attacks or local neurological deficits as an initial event were taken together. Studies with patients whose diagnosis of eICAD was made by arterial angiography, duplex scanning, computed tomography or magnetic resonance imaging demonstrating the specific features of dissection were eligible. We accepted the following angiographic signs consistent with eICAD: mural haematoma, pseudoaneurysm, long tapering stenosis, intimal flap, double lumen, or occlusion more than 2 cm above the carotid bifurcation revealing a pseudoaneurysm or a long tapering stenosis after recanalisation.
Types of interventions
We sought to identify all trials and studies where antithrombotic treatment (AP or AC) was given for eICAD. Antithrombotic treatment was defined as administration of any AP drug (i.e. acetylsalicylic acid (ASA), ticlopidine, clopidogrel, sulfinpyrazone, dipyridamole) or administration of full dose AC (such as intravenous or subcutaneous fractionated or unfractionated heparin or oral coumarin).
We only analysed the initially‐used antithrombotic treatment. For example, if a patient had AC and later AP, the patient was analysed in the AC treatment group. If surgical intervention was mentioned as a treatment modality, we excluded the patient from the comparative analysis of AC versus AP treatment.
In patients receiving thrombolysis, the first antithrombotic agent used thereafter was deemed the 'initially‐used antithrombotic treatment'. In cases of bleeding complications, we sought information on whether the bleed was associated with the thrombolytic treatment (rather than with the antithrombotic treatment).
Types of outcome measures
Primary outcomes
The primary outcomes were:
death from all causes;
death or disability (defined according to the modified Rankin Scale (mRS), see below) at the end of the follow‐up period.
In the studies where the outcomes no disability and disability was not defined, we assessed the outcome based on the clinical information mentioned in the publications as follows.
Where the mRS (UK‐TIA Study 1988) is reported, mRS 0, 1 and 2 are judged as no or minor disability and mRS 3, 4 and 5 as major disability. We classified patients who are reported to be able to return to their original or similar job (part time or full time) as having no disability.
We classified patients described as mild/slight or no deficits, asymptomatic or those who markedly improved as minor disability.
We classified patients described as improved (without further detailed information) as major disability, as were patients with persisting neurological deficits such as hemiparesis. We also classified patients with some neurological deficits, requiring some assistance of activities in daily living but can still be in the home setting in the major disability group, and also patients who had to be transferred to a nursing home or who needed permanent help for daily living.
We intended to specify the length of the follow up after which outcome assessment should take place, i.e. three months or one year. However, we had to use the latest outcome evaluations extractable from each study because of the lack of such information in the vast majority of studies.
Secondary outcomes
Ischaemic stroke ‐ according to the WHO definition (Hatano 1976) ‐ occurring in patients under antithrombotic therapy, such as confirmed recurrent strokes during follow up, as well as the occurrence of ischaemic stroke in patients initially without stroke. We also included patients with retinal infarctions.
The occurrence of symptomatic intracranial haemorrhage according to the definition used in the individual study/series. If no definition was given, we considered any neurological worsening associated with intracranial blood visible on neuroimages as a symptomatic intracranial haemorrhage.
The occurrence of major extracranial haemorrhage as defined in the individual study/series. If no definition was given, we considered any clinically apparent extracranial bleeding resulting in a surgical or endoscopic intervention or a transfusion a major extracranial haemorrhage.
Search methods for identification of studies
See the 'Specialized register' section in the Cochrane Stroke Group module.
We searched the Cochrane Stroke Group Trials Register, which was last searched by the Managing Editor on 3 October 2009. In addition, we performed comprehensive searches of the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library Issue 2, 2009), MEDLINE (January 1966 to November 2009) and EMBASE (January 1980 to November 2009), checked all relevant papers for additional eligible studies including recent review papers (Debette 2009; Engelter 2007; Kim 2009; Menon 2008a) and contacted authors and researchers in the field. We searched for relevant studies in all languages and arranged translation of reports published in languages other than English, German, French or Italian.
We used the following strategies for MEDLINE (Appendix 1) and EMBASE (Appendix 2) and adapted them for the Cochrane Central Register of Controlled Trials (CENTRAL).
Data collection and analysis
In order to estimate treatment effects, we sought to analyse data from non‐randomised studies. One of the review authors (SE) selected which trials met the inclusion criteria and another author (PL) independently reviewed the decisions. We extracted all outcome measures from the eligible studies. We resolved disagreements on inclusion (one study) and outcomes by discussion. We contacted study authors for additional information on the outcome stratified to the type of antithrombotic treatment, in any cases of uncertainty. We excluded studies without concise information on treatment or lacking follow‐up information from further analysis.
We calculated a weighted estimate of the odds for each outcome event across studies using the Peto odds ratio method.
Results
Description of studies
We did not identify any completed RCTs or CCTs. There is one ongoing RCT comparing AC with AP in cervical artery dissection ‐ Cervical Artery Dissection in stroke (CADISS). The trial started in August 2006. The randomisation goal is 250 patients (CADISS 2009). As at 21 November 2009, 51 randomised and 66 non‐randomised participants have participated in the trial and three endpoints have occurred (personal communication) (CADISS 2009).
We contacted the authors of an abstract about a planned trial (ECAD 1993); the trial never started because of lack of funding (personal communication).
Among the non‐randomised studies for the primary outcome death from all causes, data from 36 studies were eligible. In some studies, patients with malignant infarction who died early (e.g. within seven days: Georgiadis 2009) were excluded. For the outcome death or disability, 26 studies fulfilled the eligibility criteria.
We collected and analysed data on secondary outcomes if data on primary outcomes were available. Six studies included only trauma patients (Colella 1996; Eachempati 1998; Li 1994; Richaud 1980; Wahl 2002; Zelenock 1982). This might be a confounding factor. Studies were heterogenous in respect to their main issue. They included observational case reports or case series on the disease (Ast 1993; Biousse 1998; Campos 2007; Chen 1984; Dziewas 2003; Engelter 2000; Friedman 1980; Gonzales‐Portillo 2002; Kaps 1990; Landre 1987; Lepojärvi 1988; Luken 1979; Marx 1987; Metso 2009; Miller‐Fisher 1978; Mokri 1986; Pieri 2007; Schievink 1990; Sellier 1983; Treiman 1996; Vanneste 1984) or after blunt trauma (Colella 1996; Eachempati 1998; Li 1994; Richaud 1980; Wahl 2002; Zelenock 1982), communications on surgical interventions (Luken 1979), angiographic case reports (Biller 1986), ultrasound diagnostic studies (De Bray 1989; Eljamel 1990; Kaps 1990; Müller‐Forell 1989), or clinical overviews drawn from databases or registries (Arauz 2006; Biller 1986; Bogousslavsky 1987b; Caso 2004; Georgiadis 2009; Touze 2003).
We excluded some studies from further analysis because of overlapping with other published case series (Arnold 2006; Baumgartner 2001; Bui 1993; Sturzenegger 1995; Watridge 1989), lack of information concerning treatment or outcome stratified to treatment (Barbour 1994; Bassetti 1996; Baumgartner 2001; Biousse 1995; ; Desfontaines 1995; Gelbert 1991; Kirsch 1998; Lisovoski 1991; Lucas 1998; Mokri 1990; O'Dwyer 1980; Pozzati 1990; Provenzale 1995; Schievink 1994; Thie 1993), and in part of the analysis about primary outcomes because of lack of information concerning disability (Ast 1993; Biller 1986; Bogousslavsky 1987b; Dziewas 2003; Georgiadis 2009; Gonzales‐Portillo 2002; Müller‐Forell 1989; Sellier 1983; Touze 2003; Treiman 1996). We excluded other studies because patients with eICAD were not reported separately from patients with other localisations of dissecting arteries, such as the vertebral artery, the common carotid artery or the intracranial carotid artery (Bassi 2003; Biffl 2002; Carrillo 1999; Chabrier 2003; Cimini 2004; Hughes 2000; Kerwin 2001; Lee 2006; Leys 1995; Miller 2001; Molina 2000; Nishino 2008; Pelkonen 2003).
Five studies were written in French, two in Italian, two in German, one in Dutch, and one in Portuguese. We obtained additional information for six studies from the authors (Campos 2007; Caso 2004; Dziewas 2003; Metso 2009; Pieri 2007; Touze 2003).
Risk of bias in included studies
None of the identified and completed studies were RCTs or CCTs. All studies were observational case series and none reported results from a pre‐defined treatment protocol. In general, treatment was decided by the treating physician. The length of follow up was heterogeneous among studies and also varied within studies. Only one large study assessed outcome after three months in all patients (Georgiadis 2009). Among the identified studies there was limited consistency in reporting outcome measures and in six studies it was not reported for all patients which treatment they received (see Characteristics of included studies) (Ast 1993; De Bray 1989; Miller‐Fisher 1978; Mokri 1986; Müller‐Forell 1989; Richaud 1980).
Effects of interventions
Randomised studies
No results of RCTs are currently available.
Non‐randomised studies
Primary outcomes
Death from all causes
For the outcome death from all causes, we analysed data from 36 studies with 1285 patients. In total, 20 of 1285 (1.56%) patients were reported dead at the end of follow up. The Peto odds ratio of 2.02 with a 95% CI ranging from 0.62 to 6.60 (P = 0.25) indicated neither harm nor benefit of anticoagulation with respect to death during the follow‐up period. There was no significant heterogeneity between the included series (I2 = 0%) (Analysis 1.1).
1.1. Analysis.
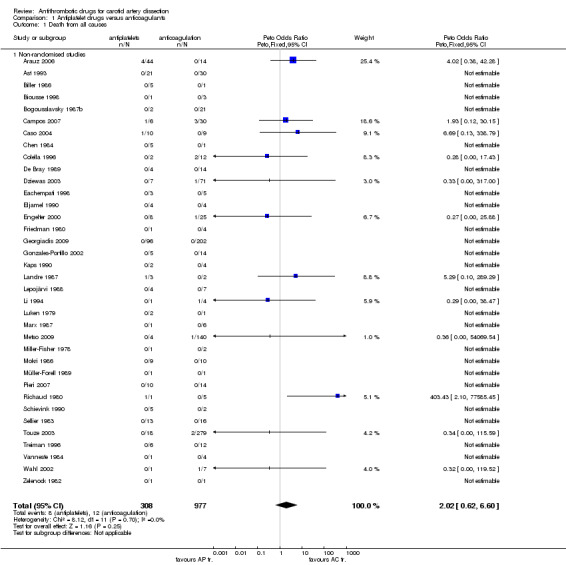
Comparison 1 Antiplatelet drugs versus anticoagulants, Outcome 1 Death from all causes.
Death or disability
For the outcome death or disability, based on 26 studies (463 patients) there was a non‐significant trend in favour of anticoagulants (OR 1.77, 95% CI 0.98 to 3.22; P = 0.06). There was no significant heterogeneity between the included series (I2 = 0%) (Analysis 1.2).
1.2. Analysis.
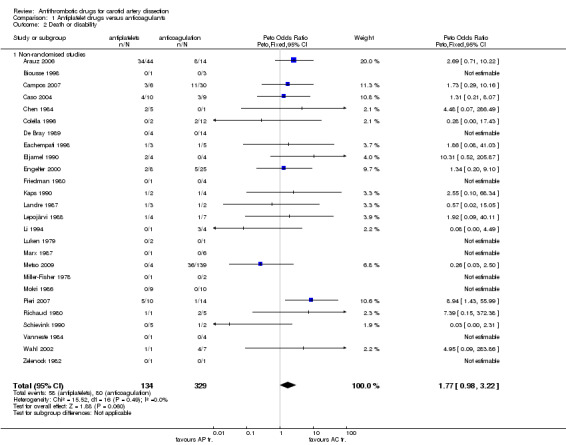
Comparison 1 Antiplatelet drugs versus anticoagulants, Outcome 2 Death or disability.
Secondary outcomes
Ischaemic stroke
Thirty‐four studies with 1262 patients reported on ischaemic strokes at the end of the follow‐up period. In 24 patients (1.9%) ischaemic strokes, including two retinal infarcts, were recorded. Among the 16 patients in whom details about the timing were provided, strokes occurred or recurred in 10/16 patients within eight days after treatment with antithrombotic agents had been started; i.e. on day one (two patients), at day three (three patients), at day four (two patients), at day seven (two patients) and at day eight (one patient). In one patient, a stroke occurred at day 12. In another five patients, strokes happened "within two weeks". In four patients, strokes recurred or occurred at 80 days (one patient) and in between 30 to 39 months (three patients). In three patients no information about the time to recurrent ischaemic strokes was provided. The stroke rate in the anticoagulation group was 1.87% (18/962) and 2.0% (6/300) in the AP group. The Peto odds ratio of 0.63 (95% CI 0.21 to 1.86, P = 0.41) indicated no significant difference between treatment options. There was some, but no significant heterogeneity between the included series (I2 = 19%) (Analysis 1.3).
1.3. Analysis.
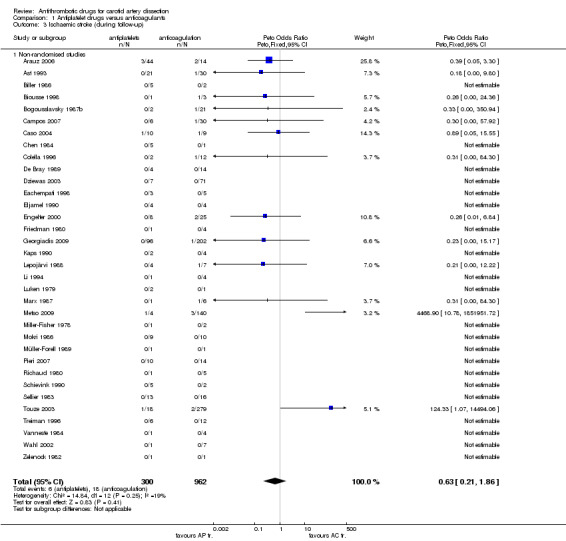
Comparison 1 Antiplatelet drugs versus anticoagulants, Outcome 3 Ischaemic stroke (during follow‐up).
Symptomatic intracranial haemorrhage
Twenty‐five studies with 885 patients provided data about symptomatic intracranial haemorrhage stratified on the type of antithrombotic treatment. Symptomatic intracranial haemorrhages occurred only in the AC group and were present in five of 627 patients (0.8%). The Peto odds ratio of 0.25 with a 95% CI of 0.02 to 3.36 indicated no significant difference between the treatment options (P = 0.3). There was no significant heterogeneity between the included series (I2 = 0%) (Analysis 1.4).
1.4. Analysis.
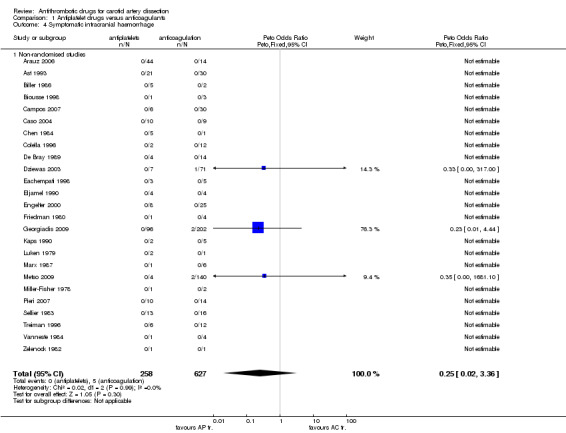
Comparison 1 Antiplatelet drugs versus anticoagulants, Outcome 4 Symptomatic intracranial haemorrhage.
Major extracranial haemorrhage
Analysis in respect of major extracranial haemorrhage was based on 12 studies with 622 patients. Major extracranial haemorrhages occurred only in the AC group and were present in seven of 425 patients (1.6%). The Peto odds ratio of 0.19 with a 95% CI of 0.02 to 1.48 indicated no significant difference between the treatment options (P = 0.11). There was no significant heterogeneity between the included series (I2 = 0%) (Analysis 1.5).
1.5. Analysis.
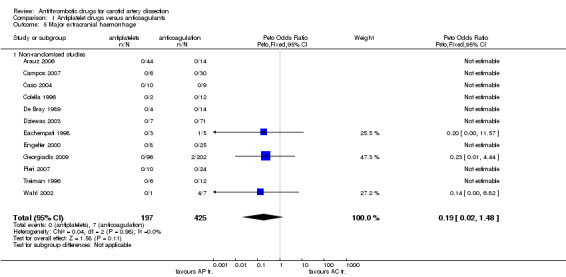
Comparison 1 Antiplatelet drugs versus anticoagulants, Outcome 5 Major extracranial haemorrhage.
Discussion
Extracranial internal carotid artery dissection (eICAD) is a major cause of ischaemic stroke in young individuals (Biller 1986; Bogousslavsky 1987b; Leys 2002) but currently there are no data based on randomised trials available to assess the effects of anticoagulation versus antiplatelets. Thus, it is impossible to draw any definite conclusions. Nevertheless, this systematic review of all relevant observational case studies provides findings important for the design and promotion of antithrombotic RCTs in eICAD. In addition, the findings about the frequency of outcome events and complications stratified to the type of antithrombotic treatment may also be useful for management decisions and counselling of individual eICAD patients.
There was no significant difference in the odds of death comparing antiplatelet drugs with anticoagulants among 1285 patients. Interestingly, the frequency of death (i.e. 1.6%, 95% CI 1.0 to 2.4%) was low, and certainly lower than originally suggested (Richaud 1980; Saver 1992). However, some patients with severe infarctions from several studies were excluded because they had received neither anticoagulants nor antiplatelet agents (Ast 1993; Bogousslavsky 1987b; Colella 1996; Wahl 2002) or had malignant infarctions (Georgiadis 2009) without information about antithrombotic treatment. Therefore, the estimated death rate of this review reflects not that of eICAD patients in general but that of patients who are well enough to receive any kind of antithrombotic treatment. The assumption that the risk of dying due to eICAD is probably higher than 2.4% (i.e. the upper end of the 95% CI) is supported by the three‐month death rate of 5.5% in a recent series of 55 dissection patients treated with intravenous thrombolysis (Engelter 2009).
For the outcome death or disability, this systematic review showed a trend towards superiority of anticoagulants over antiplatelets across all relevant observation case series. The point estimate indicates that patients treated with anticoagulants might have a more than 70% higher chance of avoiding death or disability compared with patients treated with antiplatelets. However, the wide confidence interval (0.98 to 3.22) indicates that this effect could be either much smaller or larger.
For the outcome ischaemic strokes during follow up, there was no significant difference between patients treated with anticoagulants versus those who were treated with antiplatelets. Interestingly, the point estimate of 0.63 might suggest rather a superiority of antiplatelets over anticoagulants than vice versa. This is perhaps surprising as it might be assumed that emboli arising from the distal part of the dissected artery may be of clinical importance and may cause fatal or disabling strokes (Anson 1991; Droste 2001; Koennecke 1997; Oliveira 2001; Steinke 1996). Approximately, two out of three strokes occurred (or recurred in those with an initial stroke) within a week and three out of four (16 of 21 patients) within two weeks. These findings support the main results of a smaller previous series (Biousse 1995). Interestingly, while stroke recurrence/occurrence within one day was most common in the series reported by Biousse 1995, such a very early stroke occurrence was rare (2/16) in this review. These observations may have important implications. Firstly, there might be a chance to prevent strokes in eICAD patients, but preventive means have to start early. Secondly, randomising patients more than two weeks after the first symptom bears a remarkable risk of missing the most important treatment period in a randomised controlled trial.
For bleeding complications (i.e. symptomatic intracranial haemorrhages or major extracranial haemorrhages) there were no significant differences between the AC and the AP group. Such bleeding complications were rare (0.8% for symptomatic intracranial haemorrhages, 1.6% for major extracranial haemorrhages). Interestingly, they occurred exclusively in patients with anticoagulation. Likewise, the point estimates may suggest the possibility of a higher risk of relevant bleeding complications associated with anticoagulation ‐ similar to the results from the International Stroke Trial (IST 1997). The lack of a statistically significant difference might be a matter of the sample size in combination with the infrequency of bleeding events.
Although there was an apparent trend in favour of anticoagulants (non‐significant) for the outcome death or disability, this may have arisen from methodological biases. Antiplatelets could have been primarily applied in patients who were considered to have a poor prognosis, for example due to large infarcts (Bogousslavsky 1987b; Chen 1984) or who were in a poor condition. Anticoagulation might be preferred in patients with a transient ischaemic attack (TIA). The lack of information on baseline characteristics including stroke severity prevented us from studying whether imbalances in baseline variables might have influenced the seemingly better result for the anticoagulation group in avoiding death or disability.
We are aware of other limitations. Outcome measurement was not applied uniformly in the included studies and the studies differed in their focus. It is therefore likely that there are important biases. Non‐randomised studies are known to be highly susceptible to bias and outcome events may be under‐represented (Chalmers 1983). Such biases encountered in the reported studies may be: reporting favourable cases; reports on selected cases as well as editorial biases, such as not allowing reports on already published issues by different authors; the choice of treatments may have been biased by the preference and experience of the treating physicians, and the habits and infrastructure of the institutions (Sackett 1979). In addition, the sample size of the only outcome with a result close to significance (i.e. death or disability P = 0.06) was much smaller than that of the other outcomes, as several studies did not provide data about disability. Thus, the trend towards superiority of anticoagulation with regard to death or disability among less than 500 patients might also be a chance finding.
As another limitation, we did not further study the impact of surgery in eICAD. As already shown in the 2003 update of this review, surgery appeared to have a higher rate of death (6% in excluded studies, 11% in included studies) compared with those who received antithrombotic drugs (i.e. 1.6%) (New Reference). We also did not study the effect of hyperacute treatment options such as thrombolysis or intra‐arterial interventions including stenting, which was beyond the scope of this review. Furthermore, we focused on eICAD rather than on craniocervical artery dissections as it remains unclear whether carotid artery dissection and vertebral artery dissection as well as extracranial and intracranial dissections can be regarded as one entity.
This review attempted to systematically assess the evidence on antithrombotic eICAD treatment. Further steps could be to establish an international systematic registry for eICAD with standardised recording of diagnosis, therapeutic modalities and outcome. This would allow the gathering of more uniform information on the disease and its prognosis. The Cervical Artery Dissection and Ischemic Stroke Patients (CADISP) Group (CADISP 2009a; CADISP 2009b) has initiated such a registry. Results are expected in early 2011.
A large RCT comparing anticoagulants with antiplatelets in eICAD is important and could solve the decades‐long debate whether to use immediate anticoagulation or not. Indeed, a UK‐based feasibility study is ongoing (CADISS 2009). If possible, randomisation of eICAD patients in such a RCT is encouraged. Other groups intend to initiate RCTs too (CADISP 2009a). All current and planned RCTs should consider predefining an individual patient data meta‐analysis ‐ as done in the carotid stenting versus endarterectomy trials ‐ in order to gather the best evidence for antithrombotic treatment in eICAD. Taking into account our findings, protocols for RCTs should include a stringent definition of carotid dissection, a standardised diagnostic protocol, strictly random allocation to antiplatelet agents versus anticoagulants, as well as accurate unbiased assessment of outcome. In addition, imbalances in important prognostic variables must be avoided.
Our findings allow some estimation about the sample sizes. On the basis of our results, we recommended using death or disability as the outcome measure. We estimate a sample size of at least 1600 patients in each treatment arm in order to detect (power 90%) a 5% difference in the proportion of patients dead or disabled from 30% to 25% (a 25% relative odds reduction). For ischaemic stroke, the sample size to detect a 1% absolute odds reduction (from 2.5% to 1.5 %) is estimated to be at least 8000 patients (4000 in each arm) (power 90%, significance level 5%). Interestingly, if we had based a sample size calculation on the figures observed for either antithrombotic modality in this review, a sample size greater than 300,000 patients would have been required to detect a significant difference for ischaemic stroke (power 80%, significance level 5%). Fewer than 300 patients would have been necessary to detect a significant difference for the outcome death or disability (power 90%, significance level 5%).
Until more evidence‐based information is available, our data showed that patients with eICAD are unlikely to be harmed by antiplatelet drugs and there seems little justification for giving anticoagulants as a first line therapy in all patients.
Authors' conclusions
Implications for practice.
There is no randomised evidence to determine whether, for patients with carotid artery dissection, either antiplatelet or anticoagulant therapy is superior to control, or whether anticoagulant is superior to antiplatelet therapy. Participation in randomised controlled trials is strongly encouraged. If this is not possible, individually tailored treatment decisions should be made.
Implications for research.
(1) Randomised trials comparing antiplatelet with anticoagulant therapy in carotid artery dissection are justified, and at least one randomised trial is ongoing. (2) Death or disability is an appropriate measure of outcome for such trials
Feedback
Feedback
Summary
Feedback received for the previous version of this review, and other reviews and protocols of anticoagulants, is available on the Cochrane Editorial Unit website at http://www.editorial‐unit.cochrane.org/anticoagulants‐feedback
What's new
| Date | Event | Description |
|---|---|---|
| 7 March 2011 | Feedback has been incorporated | Link to feedback added. |
History
Protocol first published: Issue 4, 1998 Review first published: Issue 4, 2000
| Date | Event | Description |
|---|---|---|
| 23 August 2010 | New citation required but conclusions have not changed | After the updated review was published in Issue 7 2010 of The Cochrane Library, it was subsequently agreed that the review merits a new citation because a significant number of new studies had been added and new secondary outcomes were included in the update. This republished version only amends the citation date of the review; there have been no changes to the content of the review since it was last updated on 3 May 2010 (see History). |
| 3 May 2010 | New search has been performed | The Cochrane Stroke Group Trials Register was last searched for randomised trials on 3 October 2009. No results from randomised trials are currently available (one feasibility RCT is ongoing). Since the second publication of the review, searches of MEDLINE (November 2009), EMBASE (November 2009), and the Cochrane Central Register of Controlled Trials (The Cochrane Library Issue 2, 2009) have identified 10 additional non‐randomised trials and case series eligible for the update. In addition, the following secondary outcomes were studied: ischaemic stroke, symptomatic intracranial haemorrhage, and major extracranial haemorrhage. The conclusions of the review are unchanged. |
| 23 June 2008 | New search has been performed | Converted to new review format. |
Acknowledgements
We wish to thank Hazel Fraser and Brenda M Thomas for searching and providing us with lists of the relevant trials from the Cochrane Stroke Group trials register. We are thankful to Catherine Operschall for her help with collecting papers for the first review.
For the current update, we are in particular thankful to Prof E Touze (Paris, France), Prof V Caso (Perugia, Italy), Dr T Metso (Helsinki, Finland), Dr R Dziewas (Munster, Germany), Dr C Herrer [Campos] (Sao Paulo, Brazil) and Dr A Pieri (Sao Paulo, Brazil) for providing unpublished data and information adding to their publications. Furthermore, we thank Prof John Norris, the principle investigator of CADISS, for providing us with updated information on this trial. We very much appreciate these valuable contributions.
We are grateful to the Editorial Board of the Cochrane Stroke Group and external peer reviewers for making constructive comments on this as well as on earlier versions of this review, namely: Prof Peter Sandercock, UK; Prof Charles Warlow, UK; Dr Carl Counsell, UK; Prof Jan van Gijn, The Netherlands; Prof Livia Candelise, Italy; Prof Graeme Hankey, Australia; Dr Stephanie Lewis, UK; Brenda Thomas, UK; and Ashma Krishan, UK.
Appendices
Appendix 1. MEDLINE search strategy
We used the following search strategy, using a combination of controlled vocabulary and text word terms, for MEDLINE (Ovid) and modified it to search the Cochrane Central Register of Controlled Trials.
MEDLINE (Ovid) 1966‐November 2009 1 exp carotid artery injuries/ or carotid artery, internal, dissection/ 2 (carotid adj5 (injur$ or dissection or trauma$)).tw. 3 exp carotid arteries/ 4 carotid artery diseases/ 5 carotid artery thrombosis/ 6 carotid$.tw. 7 3 or 4 or 5 or 6 8 exp aneurysm, dissecting/ or aneurysm, false/ or exp aneurysm, ruptured/ 9 exp wounds, nonpenetrating/ 10 (traumatic adj5 (dissection or aneurysm or pseudoaneurysm)).tw. 11 (blunt adj5 (injur$ or trauma)).tw. 12 dissecting aneurysm.tw. 13 rupture, spontaneous/ or rupture/ 14 spontaneous dissection.tw. 15 8 or 9 or 10 or 11 or 12 or 13 or 14 16 7 and 15 17 1 or 2 or 16 18 exp platelet aggregation inhibitors/ 19 blood platelets/de 20 platelet aggregation/de 21 exp fibrinolytic agents/ 22 exp anticoagulants/ 23 Thrombolytic therapy/ 24 exp thromboembolism/dt 25 thrombosis/dt 26 (antiplatelet$ or antithromb$ or anticoag$).tw. 27 (aspirin or acetylsalicylic acid or indobufen).tw. 28 (dipyridamole or ticlopidine or clopidogrel or sulfinpyrazone or sulphinpyrazone).tw. 29 (heparin$ or coumarin$ or coumadin$ or warfarin).tw. 30 or/18‐29 31 17 and 30 32 limit 31 to human
Appendix 2. EMBASE search strategy
We used the following search strategy, using a combination of controlled vocabulary and text word terms, for EMBASE (Ovid)
EMBASE (Ovid) 1980‐November 2009 1 carotid artery thrombosis/dt 2 carotid artery obstruction/dt 3 carotid artery aneurysm/dt 4 internal carotid artery occlusion/dt 5 internal carotid artery aneurysm/dt 6 1 or 2 or 3 or 4 or 5 7 exp carotid artery/ 8 exp carotid artery disease/ 9 carotid.tw. 10 Artery dissection/ or Artery injury/ or Artery rupture/ or Artery thrombosis/ 11 artery wall dissection/ 12 blood vessel injury/ 13 False aneurysm/ 14 blunt trauma/ 15 rupture/ 16 (traumatic adj5 (dissection or aneurysm or pseudoaneurysm)).tw. 17 (blunt adj5 (injur$ or trauma)).tw. 18 dissecting aneurysm.tw. 19 spontaneous dissection.tw. 20 7 or 8 or 9 21 or/10‐19 22 20 and 21 23. carotid artery injury/ or (carotid adj5 (injur$ or dissection or trauma$)).tw 24 6 or 22 or 23 25 exp Anticoagulant agent/ 26 exp Antithrombocytic agent/ 27 Thrombocyte aggregation/ 28 Thrombocyte/ 29 Fibrinolytic therapy/ 30 thromboembolism/dt 31 (antiplatelet$ or anticoagulant$ or antithromb$).tw. 32 (aspirin or acetylsalicylic acid or indobufen).tw. 33 (dipyridamole or ticlopidine or clopidogrel or sulfinpyrazone or sulphinpyrazone).tw. 34 (heparin$ or coumarin$ or coumadin$ or warfarin).tw. 35 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 36 24 and 35 37 Limit 36 to human
Data and analyses
Comparison 1. Antiplatelet drugs versus anticoagulants.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Death from all causes | 36 | 1285 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.02 [0.62, 6.60] |
| 1.1 Non‐randomised studies | 36 | 1285 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.02 [0.62, 6.60] |
| 2 Death or disability | 26 | 463 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.77 [0.98, 3.22] |
| 2.1 Non‐randomised studies | 26 | 463 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.77 [0.98, 3.22] |
| 3 Ischaemic stroke (during follow‐up) | 34 | 1262 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.63 [0.21, 1.86] |
| 3.1 Non‐randomised studies | 34 | 1262 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.63 [0.21, 1.86] |
| 4 Symptomatic intracranial haemorrhage | 25 | 885 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.25 [0.02, 3.36] |
| 4.1 Non‐randomised studies | 25 | 885 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.25 [0.02, 3.36] |
| 5 Major extracranial haemorrhage | 12 | 622 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.19 [0.02, 1.48] |
| 5.1 Non‐randomised studies | 12 | 622 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.19 [0.02, 1.48] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Arauz 2006.
| Methods | Observational study, single‐centre, stroke registry based, traumatic and spontaneous dissections | |
| Participants | 58 eICAD stroke patients (among 130 patients with cervical artery dissection) | |
| Interventions | 13 anticoagulation, 45 antiplatelets | |
| Outcomes | Death, stroke during follow up, modified Rankin scale at 6 months, recanalisation, intracranial or systemic bleeding | |
| Notes | Mexico | |
Ast 1993.
| Methods | Observational study, multicentre, retrospective from medical records | |
| Participants | 68 patients with eICAD 21 with stroke, 15 with TIA or AF | |
| Interventions | 30 anticoagulants, 21 antiplatelet drugs, 9 'no treatment', 2 surgery, 6 not mentioned | |
| Outcomes | Death, stroke (ischaemic, haemorrhagic), TIA | |
| Notes | France | |
Biller 1986.
| Methods | Observational study, retrospective from angiographical database | |
| Participants | 11 patients with eICAD, 10 with stroke, 1 with Horner's syndrome | |
| Interventions | 2 anticoagulants, 5 antiplatelet drugs, 4 surgery | |
| Outcomes | Death, complications including stroke (ischaemic, haemorrhagic) | |
| Notes | USA | |
Biousse 1998.
| Methods | Observational study, selection from large series of eICAD | |
| Participants | 4 patients with eICAD, 4 with ocular ischaemia | |
| Interventions | 3 anticoagulants, 1 antiplatelet drugs | |
| Outcomes | Death, disability, stroke, symptomatic intracranial haemorrhage | |
| Notes | France | |
Bogousslavsky 1987b.
| Methods | Observational study, data from Lausanne Stroke Registry, consecutive patients with first‐ever stroke | |
| Participants | 30 patients with eICAD, 12 with stroke, 5 TIA or AF, 2 monocular blindness, 11 headache | |
| Interventions | 21 anticoagulants, 2 antiplatelet drugs, 7 'no treatment' (these patients died) | |
| Outcomes | Death, stroke Reopening at 6 months | |
| Notes | Switzerland | |
Campos 2007.
| Methods | Observational study | |
| Participants | 60 patient with cervical artery dissection, among those 36 with eICAD; all but 2 patients had ischaemic events before diagnosis of dissection | |
| Interventions | 6 eICAD patients had anticoagulation, 30 had antiplatelets | |
| Outcomes | Death, disability, stroke, bleeding complications | |
| Notes | Sao Paulo, Brazil Additional information obtained by personal communication | |
Caso 2004.
| Methods | Observational study, single centre, consecutive patients | |
| Participants | 19 eICAD with stroke or TIA (all had visible infarcts), only spontaneous eICAD | |
| Interventions | 9 anticoagulants, 10 antiplatelets | |
| Outcomes | Death, disability, stroke, recanalisation, symptomatic intracranial haemorrhage, major extracranial haemorrhage | |
| Notes | Italy, additional information obtained by personal communication 1 patient with anticoagulation suffered a retinal infarction | |
Chen 1984.
| Methods | Observational study, selection not reported | |
| Participants | 7 patients with eICAD | |
| Interventions | 1 anticoagulants, 5 antiplatelet drugs, 1 surgery (EC/IC bypass) | |
| Outcomes | Death, disability, stroke (ischaemic, haemorrhagic) | |
| Notes | Taiwan | |
Colella 1996.
| Methods | Observational study, case series from motor vehicle accidents or other trauma (2 falls) | |
| Participants | 18 patients with eICAD | |
| Interventions | 12 anticoagulants, 2 antiplatelet drugs, 2 no treatment, 2 surgery (type of intervention not stated) | |
| Outcomes | Death, disability, stroke (ischaemic, haemorrhagic) | |
| Notes | USA Confounding with primary trauma possible | |
De Bray 1989.
| Methods | Observational study for ultrasound diagnosis | |
| Participants | 20 patients with eICAD, 12 with stroke, 6 with TIA, referred for ultrasound | |
| Interventions | 12 anticoagulants, 4 antiplatelet drugs, 2 no treatment, 2 not mentioned | |
| Outcomes | Death, disability, stroke, bleeding complications | |
| Notes | France | |
Dziewas 2003.
| Methods | Observational study of cervical artery dissection | |
| Participants | 78 patients with eICAD, 55 with stroke, 10 with TIA, 13 with only local signs | |
| Interventions | 7 antiplatelets, 71 anticoagulation | |
| Outcomes | Death, stroke, symptomatic intracranial haemorrhage, major extracranial haemorrhage Follow up 6 months | |
| Notes | Munster, Germany Additional information obtained by personal communication | |
Eachempati 1998.
| Methods | Observational study, case series of trauma registry | |
| Participants | 11 patients with traumatic eICAD | |
| Interventions | 2 no treatment, 3 antiplatelet drugs, 5 anticoagulants, 1 surgery | |
| Outcomes | Death, disability, bleeding complication | |
| Notes | USA Confounding with primary trauma injuries possible | |
Eljamel 1990.
| Methods | Observational study for ultrasound diagnosis | |
| Participants | 8 patients with eICAD, 5 stroke, 3 TIA | |
| Interventions | 4 anticoagulants, 4 antiplatelet drugs | |
| Outcomes | Death, disability | |
| Notes | UK | |
Engelter 2000.
| Methods | Observational, retrospective study on long‐term outcome | |
| Participants | 33 patients with eICAD: 20 stroke, 6 TIA, 7 non‐ischaemic | |
| Interventions | 25 anticoagulants, 8 antiplatelets | |
| Outcomes | Death, disability, stroke, TIA, any haemorrhage, seizures | |
| Notes | Basel, Switzerland | |
Friedman 1980.
| Methods | Observational study, consecutive patients | |
| Participants | 12 patients with eICAD, symptoms not mentioned | |
| Interventions | 4 anticoagulants, 1 antiplatelet drugs, 5 no treatment, 2 surgery (1 trapping, 1 EC/IC bypass) | |
| Outcomes | Death, disability, stroke, symptomatic intracranial haemorrhage | |
| Notes | USA | |
Georgiadis 2009.
| Methods | Observational study, databank‐based, consecutive patients | |
| Participants | 298 patients with eICAD Presenting symptoms: ischaemic stroke 118/202 with anticoagulants and 47/96 with antiplatelets; TIA 25/202 with anticoagulants and 12/96 with antiplatelets; AF 7/202 with anticoagulants and 1/96 with antiplatelets; pure local signs 45/202 with anticoagulants and 35/96 with antiplatelets; asymptomatic 7/202 with anticoagulants and 1/96 with antiplatelets | |
| Interventions | 202 anticoagulants, 96 antiplatelet agents alone Those with surgical/endovascular treatment were excluded (17) as were those on aspirin followed by warfarin (30), those with no antithrombotic treatment and those who died within 7 days due to malignant MCA infarction (8, no treatment modalities mentioned) | |
| Outcomes | Death, ischaemic stroke, TIA, symptomatic intracranial haemorrhage, major extracranial haemorrhage (assessment at 3 months) | |
| Notes | Swizerland (Zurich, Bern) | |
Gonzales‐Portillo 2002.
| Methods | Observational study, databank‐based, consecutive patients | |
| Participants | 27 patients with cervical artery dissection (22 spontaneous, 5 traumatic): 21 strokes, 3 TIA, 3 non‐ischaemic symptoms) 19 patients had eICAD (2 bilateral), 8 had eVAD | |
| Interventions | 5 eICAD patients had antiplatelets, 14 had anticoagulants | |
| Outcomes | Death (strokes mentioned, but not stratified to treatment), mean follow up 58 months | |
| Notes | Indiana, USA | |
Kaps 1990.
| Methods | Observational study for ultrasound diagnosis | |
| Participants | 11 patients with eICAD, 2 with stroke, 3 with TIA | |
| Interventions | 4 anticoagulants, 2 antiplatelet drugs, 2 no treatment | |
| Outcomes | Death, disability, stroke (ischaemic, haemorrhagic) | |
| Notes | Germany | |
Landre 1987.
| Methods | Observational study, consecutive cases | |
| Participants | 5 patients with eICAD, 5 with stroke | |
| Interventions | 2 anticoagulants, 3 antiplatelet drugs | |
| Outcomes | Death, disability | |
| Notes | France | |
Lepojärvi 1988.
| Methods | Observational study, selection not reported | |
| Participants | 13 patients with eICAD, 8 with stroke, 3 with TIA | |
| Interventions | 7 anticoagulants, 4 antiplatelet drugs, 1 no treatment, 1 surgery (ligation) | |
| Outcomes | Death, disability, stroke | |
| Notes | Finland | |
Li 1994.
| Methods | Observational study, case series from trauma patients | |
| Participants | 7 patients with eICAD, 7 with stroke | |
| Interventions | 4 anticoagulants, 1 antiplatelet drugs, 2 surgery (1 embolectomy, 1 endarterectomy) | |
| Outcomes | Death, disability, stroke, TIA | |
| Notes | Canada 2 deaths due to suicide, confounding with trauma and premorbid status possible | |
Luken 1979.
| Methods | Observational study, consecutive case series | |
| Participants | 10 patients with eICAD, 4 with TIA or AF, 9 with pain | |
| Interventions | 1 anticoagulants, 2 antiplatelet drugs, 3 no treatment, 4 surgery (2 ligations, 1 silverstone clamp, 1 embolectomy) | |
| Outcomes | Death, disability, stroke, symptomatic intracranial haemorrhage | |
| Notes | USA | |
Marx 1987.
| Methods | Observational study on spontaneous dissections of cervical arteries | |
| Participants | 8 patients with eICAD, 4 with stroke, 2 with Horner's syndrome, 2 TIA | |
| Interventions | 6 anticoagulants, 1 antiplatelet drugs, 1 no treatment | |
| Outcomes | Death, disability, stroke (ischaemic, haemorrhagic) | |
| Notes | Germany | |
Metso 2009.
| Methods | Observational study, single centre, consecutive patients with cervico‐cerebral artery dissection | |
| Participants | 301 patients with either extra or intracranial internal carotid or vertebral artery dissection Data about outcome stratified to the type of antithrombotic treatment were obtained by personal communication | |
| Interventions | For the 144 eICAD patients: 140 anticoagulants, 4 antiplatelets | |
| Outcomes | Death, dependency, stroke, TIA, symptomatic intracranial haemorrhage | |
| Notes | Finland Additional information obtained by personal communication In 1 of the 140 patients treated with anticoagulation there was no information on disability available | |
Miller‐Fisher 1978.
| Methods | Observational study on spontaneous dissections of cervical arteries | |
| Participants | 16 patients with eICAD, 10 with TIA, 0 with stroke, 10 with pain | |
| Interventions | 2 anticoagulants, 1 antiplatelet drugs, 5 surgery (3 explorations, 2 embolectomies) 8 not mentioned | |
| Outcomes | Death, disability, stroke, symptomatic intracranial haemorrhage | |
| Notes | USA Information on treatment for 8 patients not given | |
Mokri 1986.
| Methods | Observational study, retrospective assessment | |
| Participants | 36 patients with eICAD, 30 with headache, 2 with stroke, 2 with TIA or AF, 1 syncope, 1 neck pain | |
| Interventions | 10 anticoagulants, 9 antiplatelet drugs, 14 no treatment, 1 surgery (EC/IC bypass), 3 not mentioned | |
| Outcomes | Death, disability, stroke (ischaemic, haemorrhagic), TIA | |
| Notes | USA Information on initial therapy not reported in 2; 6 patients had EC/IC bypass surgery later | |
Müller‐Forell 1989.
| Methods | Observational study, angiographical and ultrasound diagnosis | |
| Participants | 4 patients with eICAD, 2 with stroke, 2 with pain | |
| Interventions | 1 anticoagulants, 1 antiplatelet drugs, 1 no treatment, 1 not mentioned | |
| Outcomes | Death, stroke | |
| Notes | Germany Initial therapy not reported in 1 patient | |
Pieri 2007.
| Methods | Observational study, case series | |
| Participants | 66 patients with cervical artery dissection, 24/66 had eICAD | |
| Interventions | 10/24 had antiplatelets, 14/24 had anticoagulation | |
| Outcomes | Death, disability, stroke (ischaemic, haemorrhagic), symptomatic intracranial bleedings, TIA | |
| Notes | Sao Paulo, Brazil Additional information obtained by personal communication | |
Richaud 1980.
| Methods | Observational study, case series from trauma patients | |
| Participants | 17 patients with eICAD, 9 with stroke, 2 with TIA (information or other patients not conclusive) | |
| Interventions | 5 anticoagulants, 1 antiplatelet drugs, 4 no treatment, 3 surgery (non‐arterial operations), 4 not mentioned | |
| Outcomes | Death, disability, stroke | |
| Notes | France Confounding from trauma possible No report on initial therapy in 4 patients | |
Schievink 1990.
| Methods | Observational study, consecutive case series | |
| Participants | 7 patients with eICAD, 3 with stroke, 4 with local symptoms | |
| Interventions | 2 anticoagulants, 5 antiplatelet drugs | |
| Outcomes | Death, disability, stroke | |
| Notes | The Netherlands | |
Sellier 1983.
| Methods | Observational study, case series on spontaneous eICAD, traumatic cases excluded | |
| Participants | 46 patients with eICAD, 18 with stroke, 24 with TIA | |
| Interventions | 16 anticoagulants, 13 antiplatelet drugs, 10 no treatment, 7 surgery (intervention not specified) | |
| Outcomes | Death, stroke (ischaemic, haemorrhagic) | |
| Notes | France | |
Touze 2003.
| Methods | Multicentre observational study, databank‐based, 24 neurology departments | |
| Participants | Consecutive patients with cervical artery dissection (eICAD or eVAD or both) The data for the subgroup of patients with eICAD alone were obtained by personal communication | |
| Interventions | For the 311 'eICAD alone' patients: 279 anticoagulants; 18 antiplatelets, 12 no antithrombotics, 2 tPA | |
| Outcomes | Stroke, TIA, death, recurrent dissection | |
| Notes | France Additional information obtained by personal communication | |
Treiman 1996.
| Methods | Observational case series | |
| Participants | 24 patients with eICAD, diagnosis made by angiography | |
| Interventions | 3 no antithrombotic treatment (died), 21 patients who survived the initial hospitalisation, 12 anticoagulation, 6 antiplatelets, 3 with combined antiplatelets plus anticoagulation | |
| Outcomes | Vascular death, stroke, recurrent dissection, bleeding complication | |
| Notes | USA No information about type of initial antithrombotic treatment available in 2 patients with non‐vascular death years after the eICAD | |
Vanneste 1984.
| Methods | Observational study, selection not reported | |
| Participants | 5 patients with eICAD, 2 with stroke, 3 with pain | |
| Interventions | 4 anticoagulants, 1 antiplatelet drugs | |
| Outcomes | Death, disability, stroke, symptomatic intracranial bleeds | |
| Notes | The Netherlands | |
Wahl 2002.
| Methods | Observational study, traumatic carotid dissections (i.e. dissection of common carotid artery, eICAD, and intracranial dissections, trauma centre registry) | |
| Participants | 11 patients with traumatic eICAD (among 22 patients with carotid dissections of any kind) | |
| Interventions | In subgroup of 11 patients with eICAD: 7 anticoagulants, 1 antiplatelets only, 1 no antithrombotic agents, 2 stents | |
| Outcomes | Death, disability, stroke, major extracranial haemorrhage | |
| Notes | USA Confounding of outcome assessment with trauma possible | |
Zelenock 1982.
| Methods | Observational study, case series of trauma patients | |
| Participants | 6 patients with eICAD | |
| Interventions | 1 anticoagulants, 1 antiplatelet drugs, 3 no treatment, 1 surgery (ligation) | |
| Outcomes | Death, disability, stroke (ischaemic, haemorrhagic) | |
| Notes | USA Confounding with trauma possible | |
AF: amaurosis fugax EC/IC bypass: extracranial‐intracranial bypass eICAD: extracranial internal carotid artery dissection eVAD: extracranial vertebral artery dissection MCA: middle cerebral artery TIA: transient ischaemic attack tPA: tissue plasminogen activator
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alimi 1996 | No treatment with antithrombotic drugs Observational study |
| Andre‐Sereys 1996 | No treatment with antiplatelet drugs Observational study |
| Arnold 2006 | No information on outcome stratified by type of antithrombotic treatment Outcome not stratified by type of affected cervical artery dissection (i.e. eICAD and vertebral artery dissection reported together) Gender differences was primary objective Overlap with included study Georgiadis 2009; the latter focused on treatment and outcome |
| Bakke 1996 | No treatment with anticoagulants Observational study |
| Barbour 1994 | No information on management and outcome |
| Bassetti 1996 | No information on treatment No separation between dissection of ICAD and VA |
| Bassi 2003 | Outcome information not stratified to treatment Observational study |
| Baumgartner 2001 | No information on treatment |
| Berne 2004 | None of the eICAD patients was treated with antiplatelet agents alone |
| Biffl 2002 | No separation between dissection of ICAD and VA No separation of traumatic eICAD from patients with carotid injury other than dissection All trauma patients Observational study |
| Biousse 1995 | Information on outcomes not available in respect to treatment |
| Bradac 1981 | No treatment with antithrombotic drugs Observational study |
| Bui 1993 | Diagnostic study, no outcome information |
| Carrillo 1999 | No separation between dissections of ICA and those of the CCA |
| Chabrier 2003 | Outcome not stratified by type of involved artery |
| Chan 2001 | No treatment with antiplatelets drugs All patients treated with anticoagulants |
| Cimini 2004 | Outcome not stratified to type of treatment |
| Cusmano 1988 | Treatment only with antiplatelet drugs Observational study |
| Davis 1990 | Treatment only with anticoagulants Observational study |
| Desfontaines 1995 | Outcome information not stratified to treatment Observational study |
| Djouhri 2000 | No information on treatment Diagnostic study (MRA) Overlapping with included study Biousse 1998 and excluded studies Biousse 1995 and Guillon 1999 |
| Dreier 2004 | Treatment only with anticoagulants |
| Droste 2001 | Diagnostic study (transcranial doppler sonography) 'Recurrent ischemic events' not specified |
| Early 1991 | Treatment only with anticoagulants Observational study |
| Ehrenfeld 1976 | No treatment with antithrombotic drugs Observational study |
| Fabian 1990 | No treatment with antiplatelet drugs Observational study |
| Fabian 1996 | No separation of ICA dissection from ICA thrombosis or carotid cavernous fistulas |
| Gelbert 1991 | No information on therapy |
| Guillon 1999 | No antiplatelet therapy Overlapping with included study Biousse 1998and excluded studies Biousse 1995 and Djouhri 2000 All patients included had aneurysms (observational study) |
| Hughes 2000 | No separation between extra and intracranial ICA dissection Observational study Only trauma patients |
| Kerwin 2001 | No outcome and therapy‐related separation between A: eICAD and vertebral artery dissection B: eICAD and other non‐dissection ICA injuries (e.g. carotid‐cavernous sinus fistula) All patients had trauma |
| Kirsch 1998 | No information on treatment Diagnostic study (MRA) |
| Koennecke 1997 | No treatment with antiplatelet drugs No follow‐up information |
| Landini 1996 | No treatment with anticoagulants Observational study |
| Leclerc 1998 | Diagnostic study (CT follow up) No treatment with antiplatelet drugs Overlapping with excluded study Leys 1995 |
| Lee 2006 | Information on outcomes not available in respect to treatment and affected artery Epidemiological, population‐based study |
| Leys 1995 | No separation between ICAD and VA dissection |
| Lisovoski 1991 | No information on management |
| Lucas 1998 | No information on therapy |
| Miller 2001 | No outcome and therapy‐related separation between A: eICAD, CCA and VA dissection B: eICAD and other non‐dissection ICA injuries (e.g. carotid‐cavernous sinus fistula) All patients had trauma |
| Mokri 1990 | Information on outcomes not available in respect to treatment Confounding with included study Mokri 1986 possible |
| Molina 2000 | No separation between extra and intracranial ICA dissection All patients had anticoagulation Diagnostic study (emboli detection by transcranial doppler sonography) |
| Morgan 1994 | No treatment with antiplatelets Observational study |
| Mueller 2000 | Study on surgery for eICAD (all patients had surgery) |
| Müllges 1992 | No treatment with anticoagulants Observational study |
| Nishino 2008 | Outcome not stratified to involved artery and treatment Observational study |
| O'Dwyer 1980 | No separation between ICAD and CCA dissection Observational study |
| Oliveira 2001 | Outcome not stratified to treatment Diagnostic study (transcranial doppler emboli monitoring) Observational study |
| Parenti 1989 | No treatment with anticoagulants Observational study |
| Pelkonen 2003 | Outcome information not stratified to treatment Observational study |
| Perry 1980 | No treatment with antithrombotic drugs Observational study |
| Petro 1987 | No treatment with antiplatelet drugs Observational study |
| Power 1991 | No treatment with antiplatelet drugs Observational study |
| Pozzati 1990 | No treatment with antithrombotics Observational study |
| Pretre 1994 | No treatment with antiplatelet drugs Observational study |
| Provenzale 1995 | No information on management Observational study |
| Schievink 1994 | No information on management Observational study |
| Sperling 1996 | No treatment with antiplatelet drugs Observational study |
| Steiger 1988 | No treatment with antiplatelet drugs Observational study |
| Steinke 1994 | No treatment with antiplatelet drugs Observational study |
| Stringer 1980 | No treatment with antiplatelet drugs Observational study |
| Sturzenegger 1995 | Data included in Georgiadis 2009 |
| Sue 1992 | No treatment with antiplatelet drugs Observational study |
| Thie 1993 | Missing information on treatment and outcomes |
| Touze 2001 | No information on treatment No separation between dissections of ICA and those of VA |
| Van Damme 1990 | No treatment with anticoagulants |
| Verdalle 2001 | No treatment with antiplatelets |
| Vishteh 1998 | No separation between extracranial ICAD and intracranial ICA pathologies (e.g. cavernous ICAD, carotid cavernous fistula) |
| Watridge 1989 | Confounding with data from excluded study Fabian 1990 possible |
| Welling 1989 | No treatment with antiplatelet drugs Observational study |
CCA: common carotid artery CT: computerised tomography eICAD: extracranial internal carotid artery dissection ICA: internal carotid artery ICAD: internal carotid dissection MRA: magnetic resonance angiography VA: vertebral artery
Characteristics of ongoing studies [ordered by study ID]
CADISS.
| Trial name or title | Cervical Artery Dissection In Stroke Study |
| Methods | Randomised prospective multicentre study comparing antiplatelet therapy with anticoagulation |
| Participants | Patients with carotid and vertebral dissection Recruitment must be within 7 days of onset of symptoms |
| Interventions | Either antiplatelet or anticoagulation therapy initially for at least 3 months, and thereafter at the discretion of the attending physician (1) Antiplatelet therapy: aspirin, dipyridamole or clopidogrel alone or in dual combination (2) Anticoagulation with heparin (either unfractionated heparin or a therapeutic dose of low‐molecular‐weight heparin) followed by warfarin aiming for an INR in the range 2 to 3 |
| Outcomes | Primary endpoint: ipsilateral stroke or death (any cause) within 3 months from randomisation Secondary endpoints: ipsilateral TIA, stroke or death (any cause) within 3 months from randomisation; any TIA and stroke; any stroke, major bleeding; presence of residual stenosis at 3 months (> 50%); mortality |
| Starting date | August 2006 |
| Contact information | http://www.dissection.co.uk/ |
| Notes | Recrutiment status 51 patients (update November 2009) |
INR: International normalisation ratio TIA:transient ischaemic attack
Contributions of authors
Philippe Lyrer developed the protocol, undertook fund raising, analysed the data, wrote the (first) review, and made critical revisions to the current update.
Stefan Engelter did the literature search, extracted outcome measures, prepared the figures, undertook fund raising, contacted authors of studies for additional data, and drafted the updated review.
Sources of support
Internal sources
Scientific fund of the Stroke Programme, Neurology Department, University Hospital, Basel, Switzerland.
-
Scientific grant of the Neurology Department, University Hospital, Basel, Switzerland.
(Support for the current update)
External sources
Freiwillige Akademische Gesellschaft (FAG), Basel (supported the first review), Switzerland.
Declarations of interest
Both authors were investigators in the Engelter 2000 study.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Arauz 2006 {published data only}
- Arauz A, Hoyos L, Espinoza C, Cantú C, Barinagarrementeria F, Román G. Dissection of cervical arteries: Long‐term follow‐up study of 130 consecutive cases. Cerebrovascular Diseases 2006;22(2‐3):150‐4. [DOI] [PubMed] [Google Scholar]
Ast 1993 {published data only}
- Ast G, Woimant F, Georges B, Laurian C, Haguenau M. Spontaneous dissection of the internal carotid artery in 68 patients. European Journal of Medicine 1993;2:466‐72. [PubMed] [Google Scholar]
Biller 1986 {published data only}
- Biller J, Hingtgen WL, Adams HP Jr, Smoker WRK, Godersky JC, Toffol GJ. Cervicocephalic arterial dissections. A ten‐year experience. Archives of Neurology 1986;43:1234‐8. [DOI] [PubMed] [Google Scholar]
Biousse 1998 {published data only}
- Biousse V, Schaison M, Touboul P‐J, D'Anglejan‐Chatillon J, Bousser M‐G. Ischemic optic neuropathy associated with internal carotid artery dissection. Archives of Neurology 1988;55:715‐9. [DOI] [PubMed] [Google Scholar]
Bogousslavsky 1987b {published data only}
- Bogousslavsky J, Despland P‐A, Regli F. Spontaneous carotid artery dissection with acute stroke. Archives of Neurology 1987;44:137‐40. [DOI] [PubMed] [Google Scholar]
Campos 2007 {published and unpublished data}
- Campos CR, Calderaro M, Scaff M, Conforto AB. Primary headaches and painful spontaneous cervical artery dissection. Journal of Headache and Pain 2007;8(3):180‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos CR, Evaristo EF, Yamamoto FI, Puglia P Jr, Lucato LT, Scaff M. Spontaneous cervical carotid and vertebral arteries dissection: study of 48 patients. Arquivos de Neuro‐psiquiatria 2004;62(2B):492‐8. [DOI] [PubMed] [Google Scholar]
Caso 2004 {published and unpublished data}
- Caso V, Paciaroni M, Corea F, Hamam M, Milia P, Pelliccioli GP, et al. Recanalization of cervical artery dissection: influencing factors and role in neurological outcome. Cerebrovascular Diseases 2004;17:93–7. [DOI] [PubMed] [Google Scholar]
Chen 1984 {published data only}
- Chen ST, Ryu SJ, Hsi MS. Cervico‐cerebral artery dissection. Journal of the Formosan Medical Association 1984;83:846‐61. [PubMed] [Google Scholar]
Colella 1996 {published data only}
- Colella JJ, Diamond DL. Blunt carotid injury: reassessing the role of anticoagulation. American Surgeon 1996;62:212‐7. [PubMed] [Google Scholar]
De Bray 1989 {published data only}
- Bray JM, Dubas F, Joseph PA, Causeret H, Pasquier JP, Emile J. [Etude ultrasonique de 22 dissections carotidiennes]. Revista de Neurologia 1989;145(10):702‐9. [PubMed] [Google Scholar]
Dziewas 2003 {published and unpublished data}
- Dziewas R, Konrad C, Drager B, Evers S, Besselmann M, Ludemann P, et al. Cervical artery dissection: clinical features, risk factors, therapy and outcome in 126 patients. Journal of Neurology 2003;250(10):1179‐84. [DOI] [PubMed] [Google Scholar]
Eachempati 1998 {published data only}
- Eachempati SR, Vaslef SN, Sebastian MW, Reed RL. Blunt vascular injuries of the head and neck: is heparinisation necessary?. Journal of Trauma 1998;45(6):997‐1004. [DOI] [PubMed] [Google Scholar]
Eljamel 1990 {published data only}
- Eljamel MSM, Humphrey PRD, Shaw MDM. Dissection of the cervical internal carotid artery. The role of doppler/duplex studies and conservative management. Journal of Neurology, Neurosurgery and Psychiatry 1990;53:379‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Engelter 2000 {published data only}
- Engelter ST, Lyrer PA, Kirsch EC, Steck AJ. Long‐term follow‐up after extracranial carotid artery dissection. European Neurology 2000;44:199‐204. [DOI] [PubMed] [Google Scholar]
Friedman 1980 {published data only}
- Friedman WA, Day AL, Quisling RG, Sypert GW, Rhoton AL Jr. Cervical carotid dissecting aneurysms. Neurosurgery 1980;7:207‐14. [DOI] [PubMed] [Google Scholar]
Georgiadis 2009 {published data only}
- Georgiadis D, Arnold M, Buedingen HC, Valko P, Sarikaya H, Rousson V, et al. Aspirin vs anticoagulation in carotid artery dissection: a study of 298 patients. Neurology 2009;72:1810‐5. [DOI] [PubMed] [Google Scholar]
Gonzales‐Portillo 2002 {published data only}
- Gonzales‐Portillo F, Bruno A, Biller J. Outcome of extracranial cervicocephalicarterial dissections: a follow‐up study. Neurological Research 2002;24:395–8. [DOI] [PubMed] [Google Scholar]
Kaps 1990 {published data only}
- Kaps M, Dorndorf W, Damian MS, Agnoli L. Intracranial haemodynamics in patients with spontaneous carotid artery dissection. European Archives of Psychiatry and Neurological Sciences 1990;239:246‐56. [DOI] [PubMed] [Google Scholar]
Landre 1987 {published data only}
- Landre E, Roux FX, Cioloca C. [Dissection spontanee de la carotide interne exocranienne]. Presse Medicale 1987;16:1273‐6. [PubMed] [Google Scholar]
Lepojärvi 1988 {published data only}
- Lepojärvi M, Tarkka M, Leinonen A, Kallanranta T. Spontaneous dissection of the internal carotid artery. Acta Chirurgica Scandinavica 1988;154:559‐66. [PubMed] [Google Scholar]
Li 1994 {published data only}
- Li MS, Smith BM, Espinosa J, Brown RA, Richardson P, Ford R. Non‐penetrating trauma to the carotid artery: seven cases and a literature review. Journal of Trauma 1994;36:265‐72. [DOI] [PubMed] [Google Scholar]
Luken 1979 {published data only}
- Luken MG III, Ascherl GF Jr, Correll JM, Hilal SK. Spontaneous dissecting aneurysm of the extracranial internal carotid artery. Clinical Neurosurgery 1979;26:353‐75. [DOI] [PubMed] [Google Scholar]
Marx 1987 {published data only}
- Marx A, Messing B, Storch B, Busse O. [Spontane dissektionen hirnversorgender arterien]. Der Nervenarzt 1987;58:8‐18. [PubMed] [Google Scholar]
Metso 2009 {published and unpublished data}
- Metso TM, Metso AJ, Salonen O, Haapaniemi E, Putaala J, Artto V, et al. Adult cervicocerebral artery dissection: a single‐center study of 301 Finnish patients. European Journal of Neurology 2009;16(6):656‐61. [DOI] [PubMed] [Google Scholar]
Miller‐Fisher 1978 {published data only}
- Miller‐Fisher C, Ojemann RG, Roberson GH. Spontaneous dissection of cervico‐cerebral arteries. Canadian Journal of Neurological Sciences 1978;5:9‐19. [PubMed] [Google Scholar]
Mokri 1986 {published data only}
- Mokri B, Sundt TM, Houser W, Piepgras DG. Spontaneous dissection of the cervical internal carotid artery. Annals of Neurology 1986;19:126‐38. [DOI] [PubMed] [Google Scholar]
Müller‐Forell 1989 {published data only}
- Müller‐Forell W, Rothacher G, Krämer G. [Carotis‐dissektionen]. Radiologe 1989;29:432‐6. [PubMed] [Google Scholar]
Pieri 2007 {published and unpublished data}
- Pieri A, Spitz M, Valiente RA, Avelar WM, Silva GS, Massaro AR. Spontaneous carotid and vertebral arteries dissection in a multiethnic population. Arquivos de Neuro‐psiquiatria 2007;65:1050‐5. [DOI] [PubMed] [Google Scholar]
Richaud 1980 {published data only}
- Richaud J, Lagarrigue J, Lazorthes Y. [Les lésions traumatiques fermées de la carotide interne au cou. A propos de 17 cas]. Neurochirurgie 1980;26:109‐21. [PubMed] [Google Scholar]
Schievink 1990 {published data only}
- Schievink W I, Limburg M. [Dissectie van cervicale arterien als oorzaak van hersenischemie of uitival van hersenzenuwen]. Nederlands Tijdschrift voor Geneeskunde 1990;134:1843‐8. [PubMed] [Google Scholar]
Sellier 1983 {published data only}
- Sellier N, Chiras J, Benhamou M, Bories J. Spontaneous dissection of the internal carotid artery. Journal of Neuroradiology 1983;10:243‐59. [PubMed] [Google Scholar]
Touze 2003 {published data only}
- Touze E, Gauvrit JY, Moulin T, Meder JF, Bracard S, Mas JL. Risk of stroke and recurrent dissection after a cervical artery dissection: a multicenter study. Neurology 2003;61(10):1347‐51. [DOI] [PubMed] [Google Scholar]
Treiman 1996 {published data only}
- Treiman GS, Treiman RL, Foran RF, Levin PM, Cohen JL, Wagner WH, et al. Spontaneous dissection of the internal carotid artery: a nineteen‐year clinical experience. Journal of Vascular Surgery 1996;24(4):597‐605. [DOI] [PubMed] [Google Scholar]
Vanneste 1984 {published data only}
- Vanneste JAL, Davies G. Spontaneous dissection of cervical internal carotid artery. Clinical Neurology and Neurosurgery 1984;86(4):307‐14. [DOI] [PubMed] [Google Scholar]
Wahl 2002 {published data only}
- Wahl WL, Brandt MM, Thompson BG, Taheri PA, Greenfield LJ. Antiplatelet therapy: an alternative to heparin for blunt carotid injury. Journal of Trauma 2002;52:896‐901. [DOI] [PubMed] [Google Scholar]
Zelenock 1982 {published data only}
- Zelenock GB, Kazmers A, Whitehouse WM Jr, Graham LM, Erlandson EE, Cronenwett JL, et al. Extracranial internal carotid artery dissections. Archives of Surgery 1982;117:425‐32. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alimi 1996 {published data only}
- Alimi YS, Mauro P, Fiacre E, Magnan J, Juhan C. Blunt injury to the internal carotid artery at the base of the scull: Six cases of venous graft restoration. Journal of Vascular Surgery 1996;24:249‐57. [DOI] [PubMed] [Google Scholar]
Andre‐Sereys 1996 {published data only}
- Andre‐Serys P, Petit E, Benrabah R, Abanouh A, Rancurel G, Haut J. [Dissection spontanée de la carotide interne en milieu ophtalmologique. A propos de dix cas]. Journal Français d'Ophtalmologie 1996;19(4):259‐64. [PubMed] [Google Scholar]
Arnold 2006 {published data only}
- Arnold M, Kappeler L, Georgiadis D, Berthet K, Keserue B, Bousser MG, et al. Gender differences in spontaneous cervical artery dissection. Neurology 2006;67:1050‐2. [DOI] [PubMed] [Google Scholar]
Bakke 1996 {published data only}
- Bakke S J, Smith H ‐J, Kerty E, Dahl A. Cervicocranial artery dissection. Detection by Doppler ultrasound and MR angiography. Acta Radiologica 1996;37:529‐34. [DOI] [PubMed] [Google Scholar]
Barbour 1994 {published data only}
- Barbour PJ, Castaldo JE, Rae Grant AD, et al. Internal carotid artery redundancy is significantly associated with dissection. Stroke 1994;25:1201‐6. [DOI] [PubMed] [Google Scholar]
Bassetti 1996 {published data only}
- Bassetti C, Carruzzo A, Sturzenegger M, Tuncdogan E. Recurrence of cervical artery dissection. Stroke 1996;27:1804‐7. [DOI] [PubMed] [Google Scholar]
Bassi 2003 {published data only}
- Bassi P, Lattuada P, Gomitoni A. Cervical cerebral artery dissection: a multicenter prospective study (preliminary report). Neurological Sciences 2003;24 Suppl 1:S4‐S7. [DOI] [PubMed] [Google Scholar]
Baumgartner 2001 {published data only}
- Baumgartner RW, Arnold M, Baumgartner I, Mosso M, Goenner F, Studer A, et al. Carotid dissection with and without ischemic events. Neurology 2001;57:827‐32. [DOI] [PubMed] [Google Scholar]
Berne 2004 {published data only}
- Berne JD, Norwood SH, McAuley CE, Villareal DH. Helical computed tomographic angiography: an excellent screening test for blunt cerebrovascular injury. Journal of Trauma 2004;57:11‐7. [DOI] [PubMed] [Google Scholar]
Biffl 2002 {published data only}
- Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: implications of a new grading scale. Journal of Trauma 1999;47(5):845‐52. [DOI] [PubMed] [Google Scholar]
- Biffl WL, Moore EE, Ryu RK, Offner PJ, Novak Z, Coldwell DM, et al. The unrecognized epidemic of blunt carotid arterial injuries: early diagnosis improves neurologic outcome. Annals of Surgery 1998;228(4):462‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biffl WL, Ray CE Jr, Moore EE, Franciose RF, Aly S, Heyrosa MG, et al. Treatment‐related outcomes from cerebrovascular injuries. Annals of Surgery 2002;235:699‐707. [DOI] [PMC free article] [PubMed] [Google Scholar]
Biousse 1995 {published data only}
- Biousse VD, Anglejan‐Chatillon J, Touboul P‐J, Amarenco P, Bousser M‐G. Time course of symptoms in carotid artery dissections. Stroke 1995;26:235‐9. [DOI] [PubMed] [Google Scholar]
Bradac 1981 {published data only}
- Bradac GB, Kaernbach A, Bolk‐Weischedel D, Finck GA. Spontaneous dissecting aneurysm of cervical cerebral arteries. Neuroradiology 1981;21:149‐54. [DOI] [PubMed] [Google Scholar]
Bui 1993 {published data only}
- Bui LN, Brant‐Zawadzki M, Verghese P, Gillan G. Magnetic resonance angiography of cervicocranial dissection. Stroke 1993;24:126‐31. [DOI] [PubMed] [Google Scholar]
Carrillo 1999 {published data only}
- Carrillo EH, Osborne DL, Spain DA, Miller FB, Senler SO, Richardson JD. Blunt carotid artery injuries: difficulties with the diagnosis prior to neurologic event. Journal of Trauma 1996;46(6):1120‐5. [DOI] [PubMed] [Google Scholar]
Chabrier 2003 {published data only}
- Chabrier S, Lasjaunias P, Husson B, Landrieu P, Tardieu M. Ischaemic stroke from dissection of the craniocervical arteries in childhood: report of 12 patients. European Journal of Paediatric Neurology 2003;7:39‐42. [DOI] [PubMed] [Google Scholar]
Chan 2001 {published data only}
- Chan C, Paine M, O'Day J. Carotid dissection: a common cause of Horner's syndrome. Clinical and Experimental Ophthalmology 2001;29:411‐5. [DOI] [PubMed] [Google Scholar]
Cimini 2004 {published data only}
- Cimini N, D'Andrea P, Gentile M, Berletti R, Ferracci F, Candeago RM, et al. Cervical artery dissection: a 5‐year prospective study in the Belluno district. European Neurology 2004;52:207‐10. [DOI] [PubMed] [Google Scholar]
Cusmano 1988 {published data only}
- Cusmano F, Piazza P, Donatis M, Montanari E, Saginario A, Bassi P. [Dissecazione dell'arteria carotide interna. Casistica personale e revisione della letteratura]. La Radiologia Medica 1988;76:262‐73. [PubMed] [Google Scholar]
Davis 1990 {published data only}
- Davis JW, Holbrook TL, Hoyt DB, Mackersie RC, Field TO, Shackford SR. Blunt carotid artery dissection: incidence, associated injuries, screening, and treatment. Journal of Trauma 1990;30:1514‐7. [PubMed] [Google Scholar]
Desfontaines 1995 {published data only}
- Desfontaines P, Despland PA. Dissection of internal carotid artery: etiology, symptomatology, clinical and neurosonological follow‐up, and treatment in 60 consecutive cases. Acta Neurologica Belgica 1995;95:226‐34. [PubMed] [Google Scholar]
Djouhri 2000 {published data only}
- Djouhri H, Guillon B, Brunereau L, Levy C, Bousson V, Biousse V, et al. MR Angiography for the long‐term follow‐up of dissecting aneurysms of the extracranial internal carotid artery. American Journal of Roentgenology 2000;174:1137‐40. [DOI] [PubMed] [Google Scholar]
Dreier 2004 {published data only}
- Dreier JP, Lurtzing F, Kappmeier M, Bohner G, Klingebiel R, Leistner S, et al. Delayed occlusion after internal carotid artery dissection under heparin. Cerebrovascular Diseases 2004;18(4):296‐303. [DOI] [PubMed] [Google Scholar]
Droste 2001 {published data only}
- Droste DW, Junker K, Stogbauer F, Lowens S, Besselmann M, Braun B, et al. Clinically silent circulating microemboli in 20 patients with carotid or vertebral artery dissection. Cerebrovascular Diseases 2001;12(3):181‐5. [DOI] [PubMed] [Google Scholar]
Early 1991 {published data only}
- Early TF, Gregory RT, Wheeler JR, Snyder SO Jr, Gayle RG, Parent FN III, et al. Spontaneous carotid artery dissection: duplex scanning in diagnosis and management. Journal of Vascular Surgery 1991;14:391‐7. [DOI] [PubMed] [Google Scholar]
Ehrenfeld 1976 {published data only}
- Ehrenfeld WK, Wylie EJ. Spontaneous dissection of the internal carotid artery. Archives of Surgery 1976;111:1294‐301. [DOI] [PubMed] [Google Scholar]
Fabian 1990 {published data only}
- Fabian TC, George SM Jr, Croce MA, Mangiante EC, Voeller GR, Kudsk KA. Carotid artery trauma: management based on mechanism of injury. Journal of Trauma 1990;30:953‐61. [DOI] [PubMed] [Google Scholar]
Fabian 1996 {published data only}
- Fabian T, Patton JH Jr, Croce MA, Minard G, Kudsk KA, Prichard FE. Blunt carotid injury: importance of early diagnosis and anticoagulant therapy. Annals of Surgery 1996;223(5):513‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gelbert 1991 {published data only}
- Gelbert F, Assouline E, Hodes JE, Reizine D, Woimant F, George B, et al. MRI in spontaneous dissection of vertebral and carotid arteries. 15 cases studies at 0.5 Tesla. Neuroradiology 1991;33:111‐3. [DOI] [PubMed] [Google Scholar]
Guillon 1999 {published data only}
- Guillon B, Brunereau L, Biousse V, Djouhri H, Levy C, Bousser MG. Long‐term follow‐up on aneurysms developed during extracranial internal artery dissection. Neurology 1999;53:117‐22. [DOI] [PubMed] [Google Scholar]
Hughes 2000 {published data only}
- Hughes KM, Collier B, Green KA, Kurek S. Traumatic carotid artery dissection: a significant incidental finding. American Surgeon 2000;66(11):1023‐7. [PubMed] [Google Scholar]
Kerwin 2001 {published data only}
- Kerwin AJ, Bynoe RP, Murray J, Hudson ER, Close TP, Gifford RRM, et al. Liberalized screening for blunt carotid and vertebral artery injuries is justified. Journal of Trauma 2001;51:308‐14. [DOI] [PubMed] [Google Scholar]
Kirsch 1998 {published data only}
- Kirsch E, Kaim A, Engelter S, Lyrer P, Stock KW, Bongartz G, et al. MR angiography in internal carotid artery dissection: improvement of diagnosis by selective demonstration of the intramural haematoma. Neuroradiology 1998;40:704‐9. [DOI] [PubMed] [Google Scholar]
Koennecke 1997 {published data only}
- Koennecke H‐C, Trocio SH, Mast H, Mohr JP. Microemboli on transcranial doppler in patients with spontaneous carotid artery dissection. Journal of Neuroimaging 1997;7:217‐20. [DOI] [PubMed] [Google Scholar]
Landini 1996 {published data only}
- Landini G, Cordopatri F, Scarti L, Spolveri S, Pennati P, Rosselli A. [Dissezione dei vasi epiaortici: una patalogia emergente come causa di ischemia cerebrale focale. Valutazione di una casistica di 7 pazienti]. Annali Italiani de Medicina Interna 1996;11:12‐6. [PubMed] [Google Scholar]
Leclerc 1998 {published data only}
- Leclerc X, Lucas C, Godefroy O, Tessa H, Martinat P, Leys D, et al. Helical CT for the follow‐up of cervical artery dissections. American Journal of Neuroradiology 1998;19:831‐7. [PMC free article] [PubMed] [Google Scholar]
Lee 2006 {published data only}
- Lee VH, Brown RD, Jr, Mandrekar JN, Mokri B. Incidence and outcome of cervical artery dissection: a population‐based study. Neurology 2006;67:1809‐12. [DOI] [PubMed] [Google Scholar]
Leys 1995 {published data only}
- Leys D, Moulin TH, Stoikovic T, Begey S, Chavot D, DONALD Investigators. Follow up of patients with history of cervical artery dissection. Cerebrovascular Diseases 1995;5:43‐9. [Google Scholar]
Lisovoski 1991 {published data only}
- Lisovoski F, Rousseaux P. Cerebral infarction in young people: a study of 148 patients with early cerebral angiography. Journal of Neurology, Neurosurgery and Psychiatry 1991;54:576‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lucas 1998 {published data only}
- Lucas C, Moulin T, Deplanque D, Tatu L, Chavot D, DONALD investigators. Stroke patterns of internal carotid artery dissection in 40 patients. Stroke 1998;29:2646‐8. [DOI] [PubMed] [Google Scholar]
Miller 2001 {published data only}
- Miller PR, Fabian TC, Bee TK, Timmons S, Chamsuddin A, Finkle R, et al. Blunt cerebrovascular injuries: diagnosis and treatment. Journal of Trauma 2001;51:279‐86. [DOI] [PubMed] [Google Scholar]
Mokri 1990 {published data only}
- Mokri B. Traumatic and spontaneous extracranial internal carotid artery dissections. Journal of Neurology 1990;237:356‐61. [DOI] [PubMed] [Google Scholar]
Molina 2000 {published data only}
- Molina CA, Alvarez‐Sabin J, Schonewille W, Montaner J, Rovira A, Abilleira S, et al. Cerebral microembolism in acute spontaneous internal carotid artery dissection. Neurology 2000;55:1738‐40. [DOI] [PubMed] [Google Scholar]
Morgan 1994 {published data only}
- Morgan MK, Sekhon LHS. Extra cranial‐intracranial saphenous vein bypass for carotid or vertebral artery dissections: a report of six cases. Journal of Neurosurgery 1994;80:237‐46. [DOI] [PubMed] [Google Scholar]
Mueller 2000 {published data only}
- Mueller TB, Luther B, Hort W, Neumann‐Haefelin T, Aulich A, Sandmann W. Surgical treatment of 50 carotid dissections: indications and results. Journal of Vascular Surgery 2000;31:980‐8. [DOI] [PubMed] [Google Scholar]
Müllges 1992 {published data only}
- Müllges W, Ringelstein EB, Leibold M. Non‐invasive diagnosis of internal carotid artery dissections. Journal of Neurology, Neurosurgery and Psychiatry 1992;55:98‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nishino 2008 {published data only}
- Nishino A, Suzuki I, Utsunomiya A, Suzuki S, Uenohara H, Sakurai Y. Clinical manifestation and treatment strategy for non‐hemorrhagic cerebral arterial dissection. Acta Neurochirurgica Supplement 2008;103:57‐60. [DOI] [PubMed] [Google Scholar]
O'Dwyer 1980 {published data only}
- O'Dwyer JA, Moscow N, Trevor R, Ehrenfeld WK, Newton TH. Spontaneaous dissection of the carotid artery. Radiology 1980;137:379‐85. [DOI] [PubMed] [Google Scholar]
Oliveira 2001 {published data only}
- Oliveira V, Batista P, Soares F, Ferro JM. HITS in internal carotid artery dissection. Cerebrovascular Diseases 2001;11:330‐4. [DOI] [PubMed] [Google Scholar]
Parenti 1989 {published data only}
- Parenti G, Marconi F, Canapicchi R, Puglioli M, Giraldi C. Spontaneous recanalization of carotid artery occlusion following non traumatic dissection. Italian Journal of Neurological Sciences 1989;10:361‐7. [DOI] [PubMed] [Google Scholar]
Pelkonen 2003 {published data only}
- Pelkonen O, Tikkakoski T, Leinonen S, Pyhtinen J, Lepojarvi M, Sotaniemi K. Extracranial internal carotid and vertebral artery dissections: angiographic spectrum, course and prognosis. Neuroradiology 2003;45:71‐7. [DOI] [PubMed] [Google Scholar]
Perry 1980 {published data only}
- Perry MO, Snyder WH, Thal ER. Carotid artery injuries caused by blunt trauma. Annals of Surgery 1980;192:74‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petro 1987 {published data only}
- Petro GR, Witwer GA, Cacayorin ED, Hodge CJ, Bredenberg CE, Jastremski MS, et al. Spontaneous dissection of the cervical internal carotid artery: correlation of arteriography, CT and pathology. American Journal of Roentgenology 1987;148:393‐8. [DOI] [PubMed] [Google Scholar]
Power 1991 {published data only}
- Power T, Hanlon D, Brillman J. Dissections of the cervicocerebral arteries. Annals of Emergency Medicine 1991;20:1032‐5. [DOI] [PubMed] [Google Scholar]
Pozzati 1990 {published data only}
- Pozatti E, Giuliani G, Acciarri N, Nuzzo G. Long term follow up of occlusive cervical carotid dissection. Stroke 1990;21:528‐31. [DOI] [PubMed] [Google Scholar]
Pretre 1994 {published data only}
- Pretre R, Reverdin A, Kolonji T, Faidutti B. Blunt carotid artery injury: difficult therapeutic approaches for an underrecognized entity. Surgery 1994;115:375‐81. [PubMed] [Google Scholar]
Provenzale 1995 {published data only}
- Provenzale JM, Barboriak DP, Taveras JM. Exercise related dissection of craniocervical arteries: CT, MR, and angiographic findings. Journal of Computer Assisted Tomography 1995;19:268‐76. [DOI] [PubMed] [Google Scholar]
Schievink 1994 {published data only}
- Schievink WI, Piepgras DG, McCaffrey TV, Mokri B. Surgical treatment of extracranial carotid artery dissecting aneurysms. Neurosurgery 1994;35:809‐15. [DOI] [PubMed] [Google Scholar]
Sperling 1996 {published data only}
- Sperling W, Kolominski P, Pfau M, Huk WJ, Stefan H. Dissection of the carotid and vertebral arteries ‐ diagnosis and treatment [Die dissektion der arteria carotis und arteria vertebralis ‐ diagnostik und therapie]. Fortschritte der Neurologie‐Psychiatrie 1996;64:153‐60. [DOI] [PubMed] [Google Scholar]
Steiger 1988 {published data only}
- Steiger H J. [Zur behandlung der traumatischen karotisdissektion]. Neurochirurgia 1988;31:128‐33. [DOI] [PubMed] [Google Scholar]
Steinke 1994 {published data only}
- Steinke W, Rautenberg W, Schwartz A, Hennerici M. Noninvasive monitoring of internal carotid artery dissection. Stroke 1994;25:998‐1005. [DOI] [PubMed] [Google Scholar]
Stringer 1980 {published data only}
- Stringer WL, Kelly DL. Traumatic dissection of the extracranial internal carotid artery. Neurosurgery 1980;6:123‐30. [DOI] [PubMed] [Google Scholar]
Sturzenegger 1995 {published data only}
- Sturzenegger M. Spontaneous internal carotid artery dissection: early diagnosis and management in 44 patients. Journal of Neurology 1995;242:231‐8. [DOI] [PubMed] [Google Scholar]
- Sturzenegger M, Mattle HP, Rivoir A, Baumgartner RW. Ultrasound findings in carotid artery dissection. Neurology 1995;45:691‐8. [DOI] [PubMed] [Google Scholar]
Sue 1992 {published data only}
- Sue DE, Brant‐Zawadzki MN, Chance J. Dissection of cranial arteries in the neck: correlation of MRI and angiography. Neuroradiology 1992;34:273‐8. [DOI] [PubMed] [Google Scholar]
Thie 1993 {published data only}
- Thie A, Helmer D, Lachenmayer L, Janzen RWC, Kunze K. Bilateral blunt traumatic dissections of the extracranial internal carotid artery: report of eleven cases and review of the literature. Cerebrovascular Diseases 1993;3:295‐303. [Google Scholar]
Touze 2001 {published data only}
- Touze E, Randoux B, Meary E, Arquizan C, Meder JF, Mas JL. Aneurysmal forms of cervical artery dissection. Stroke 2001;32:418‐23. [DOI] [PubMed] [Google Scholar]
Van Damme 1990 {published data only}
- Damme H, Martin D, Stassen M P, Limet R. [Dissections spontanées de la carotide interne. A propos de sept cas avec revue de la littérature]. Journal des Maladies Vasculaires 1990;15:14‐22. [PubMed] [Google Scholar]
Verdalle 2001 {published data only}
- Verdale P, Herve S, Kossowski M, Felten D, Courtois A, Garcia D, et al. Spontaneous dissection of the internal carotid artery in its extracranial portion, revealed by hypoglossal paralysis: report of four cases. Annals of Otology, Rhinology and Laryngology 2001;110:794‐8. [DOI] [PubMed] [Google Scholar]
Vishteh 1998 {published data only}
- Vishteh AG, Marciano FF, David CA, Schievink WI, Zabramski JM, Spetzler RF. Long‐term graft patency rates and clinical outcomes after revascularisation for symptomatic traumatic internal carotid artery dissections. Neurosurgery 1998;43:761‐7. [DOI] [PubMed] [Google Scholar]
Watridge 1989 {published data only}
- Watridge CB, Muhlbauer MS, Lowery RD. Traumatic carotid artery dissection: diagnosis and treatment. Journal of Neurosurgery 1989;71:854‐7. [DOI] [PubMed] [Google Scholar]
Welling 1989 {published data only}
- Welling RE, Kremchek TE, Rath RK, Tew JM Jr, Johnson JK. Blunt arterial injuries associated with multiple trauma. Annals of Vascular Surgery 1989;3:345‐50. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
CADISS {published and unpublished data}
- The CADISS Trial Investigators. Antiplatelet therapy vs anticoagulation in cervical artery dissection: rationale and design of the Cervical Artery Dissection in Stroke Study (CADISS). International Journal of Stroke 2007;2(4):292. [DOI] [PubMed] [Google Scholar]
Additional references
Anderson 1959
- Anderson RMD, Schechter MM. A case of spontaneous dissecting aneurysm of the internal carotid artery. Journal of Neurology, Neurosurgery and Psychiatry 1959;22:195‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anson 1991
- Anson J, Crowell RM. Cervicocranial arterial dissection. Neurosurgery 1991;28:89‐96. [DOI] [PubMed] [Google Scholar]
Beletsky 2003
- Beletsky V, Nadareishvili Z, Lynch J, Shuaib A, Woolfenden A, Norris JW. Cervical arterial dissection: time for a therapeutic trial?. Stroke 2003;34:2856‐60. [DOI] [PubMed] [Google Scholar]
Bogousslavsky 1987a
- Bogousslavsky J, Regli F. Ischemic stroke in adults younger than 30 years of age. Archives of Neurology 1987;44:479‐82. [DOI] [PubMed] [Google Scholar]
CADISP 2009a
- Cervical artery dissection and ischemic stroke patients. http://www.cadisp.org/CADISP‐therapeutic aspects: Antiplatelets versus anticoagulation in cervical artery dissection (accessed 22 November 2009).
CADISP 2009b
- Debette S, Metso TM, Pezzini A, Engelter ST, Leys D, Lyrer P, et al. CADISP‐genetics: an international project searching for genetic risk factors of cervical artery dissections. International Journal of Stroke 2009;4(3):224‐30. [DOI] [PubMed] [Google Scholar]
CADISS 2009
- The CADISS Trial Investigators. Cervical Artery Dissection in Stroke Study. http://www.dissection.co.uk/ (accessed 16 November 2009) plus personal commuincation with the principal investigator Professor John Norris on 21 November 2009.
Chalmers 1983
- Chalmers TC, Celano P, Sacks HS, Smith H. Bias in treatment assignment in controlled clinical trials. New England Journal of Medicine 1983;309:1358‐61. [DOI] [PubMed] [Google Scholar]
Cimini 2004
- Cimini N, D'Andrea P, Gentile M, Berletti R, Ferracci F, Candeago RM, et al. Cervical artery dissection: a 5‐year prospective study in the Belluno district. European Neurology 2004;52(4):207‐10. [DOI] [PubMed] [Google Scholar]
Debette 2009
- Debette S, Leys D. Cervical‐artery dissections: predisposing factors, diagnosis and outcome. Lancet Neurology 2009;8:668–78. [DOI] [PubMed] [Google Scholar]
Dreier 2004
- Dreier JP, Lurtzing F, Kappmeier M, Bohner G, Klingebiel R, Leistner S, et al. Delayed occlusion after internal carotid artery dissection under heparin. Cerebrovascular Diseases 2004;18:296‐303. [DOI] [PubMed] [Google Scholar]
ECAD 1993
- Kraemer G, Ringelstein EB, Thie A. European carotid artery dissection (ECAD) study. Abstract Book, 2nd International Conference on Stroke, Geneva. 1993:17.
Engelter 2007
- Engelter ST, Brandt T, Debette S, Caso V, Lichy C, Pezzini A, et al. Antiplatelets versus anticoagulation in cervical artery dissection ‐ a review. Stroke 2007;38:2605‐11. [DOI] [PubMed] [Google Scholar]
Engelter 2009
- Engelter ST, Rutgers MP, Hatz F, Georgiadis D, Fluri F, Sekoranja L, et al. Intravenous thrombolysis in stroke attributable to cervical artery dissection. Stroke 2009;40:3772‐6. [DOI] [PubMed] [Google Scholar]
Fluri 2007
- Fluri F, Lyrer PA, Steck AJ, Engelter ST. Internal carotid artery dissection with occlusion during heparin therapy. Schweizer Archiv für Neurologie und Psychiatrie 2007;158:331‐3. [Google Scholar]
Gautier 1989
- Gautier JC, Pradat‐Diehl P, Loron P, Lechat P, Lascault G, Juillard JB, et al. [Accidents vasculaires cerebraux des sujets jeunes]. Revista de Neurologia 1989;145(6‐7):437‐42. [PubMed] [Google Scholar]
Giroud 1994
- Giroud M, Fayolle H, Andre N. Incidence of internal carotid artery dissection in the community of Dijon. Journal of Neurology, Neurosurgery and Psychiatry 1994;57:1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hart 1983
- Hart RG, Easton JD. Dissection of cervical and cerebral arteries. Neurologic Clinics 1983;1(1):155‐82. [PubMed] [Google Scholar]
Hatano 1976
- Hatano S. Experience from a multicentre stroke register: a preliminary report. Bulletin of the World Health Organization 1976;54:541–53. [PMC free article] [PubMed] [Google Scholar]
IST 1997
- International Stroke Trial Collaborative Group. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both or neither among 19435 patients with acute ischaemic stroke. Lancet 1997;349:1569‐81. [PubMed] [Google Scholar]
Jentzer 1954
- Jentzer A. Dissecting aneurysm of the left ICA. Angiology 1954;5:232‐4. [DOI] [PubMed] [Google Scholar]
Kim 2009
- Kim YK, Schulman S. Cervical artery dissection: pathology, epidemiology and management. Thrombosis Research 2009;123:810‐21. [DOI] [PubMed] [Google Scholar]
Leys 1997
- Leys D, Lucas Ch, Gobert M, Deklunder G, Pruvo J‐P. Cervical artery dissections. European Neurology 1997;37:3‐12. [DOI] [PubMed] [Google Scholar]
Leys 2002
- Leys D, Bandu L, Henon H, Lucas C, Mounier‐Vehier F, Rondepierre P, et al. Clinical outcome in 287 consecutive young adults (15 to 45 years) with ischemic stroke. Neurology 2002;59(1):26‐33. [DOI] [PubMed] [Google Scholar]
Lyrer 2004
- Lyrer P, Engelter S. Antithrombotic drugs for carotid artery dissection. Stroke 2004;35(2):613‐4. [DOI] [PubMed] [Google Scholar]
Lyrer 2005
- Lyrer PA. Extracranial arterial dissection: anticoagulation is the treatment of choice: against. Stroke 2005;36(9):2042‐3. [DOI] [PubMed] [Google Scholar]
Menon 2008a
- Menon R, Kerry S, Norris JW, Markus HS. Treatment of cervical artery dissection: a systematic review and meta‐analysis. Journal of Neurology, Neurosurgery and Psychiatry 2008;79:1122‐7. [DOI] [PubMed] [Google Scholar]
Menon 2008b
- Menon RK, Markus HS, Norris JW. Results of a UK questionnaire of diagnosis and treatment in cervical artery dissection. Journal of Neurology, Neurosurgery and Psychiatry 2008;79:612. [DOI] [PubMed] [Google Scholar]
Norris 2005
- Norris JW. Extracranial arterial dissection: anticoagulation is the treatment of choice: for. Stroke 2005;36(9):2041‐2. [DOI] [PubMed] [Google Scholar]
Rouhart 1993
- Rouhart F, Zagnoli F, Goas J‐Y, Mocquard. Arterial ischemic strokes in young adults (40 cases) [Accidents arteriels ischemiques cerebraux de l adulte jeune. 40 cas]. Revista de Neurologia 1993;149(10):547‐53. [PubMed] [Google Scholar]
Sackett 1979
- Sackett DL. Bias in analytic research. Journal of Chronic Diseases 1979;32:51‐63. [DOI] [PubMed] [Google Scholar]
Saver 1992
- Saver JL, Easton JD, Hart RG. Dissections and trauma of cervicocerebral arteries. In: Barnett HJM, Mohr JP, Stein BM, Yatsu FM editor(s). Stroke. Second Edition. New York: Churchill Livingstone Inc, 1992. [Google Scholar]
Schievink 1993
- Schievink WI, Mokri B, Whisnant JP. Internal carotid artery dissection in a community. Rochester, Minnesota 1987‐1992. Stroke 1993;24:1678‐80. [DOI] [PubMed] [Google Scholar]
Schievink 2001
- Schievink WJ. Spontaneous dissection of the carotid and vertebral arteries. New England Journal of Medicine 2001;344(12):898‐906. [DOI] [PubMed] [Google Scholar]
Steinke 1996
- Steinke W, Schwartz W, Hennerici M. Topography of cerebral infarction associated with carotid artery dissection. Journal of Neurology 1996;243:323‐8. [DOI] [PubMed] [Google Scholar]
UK‐TIA Study 1988
- UK‐TIA Study Group. The UK‐TIA aspirin trial: interim results. BMJ 1988;296:316‐20. [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Lyrer 2003
- Lyrer P, Engelter S. Antithrombotic drugs for carotid artery dissection. Cochrane Database of Systematic Reviews 2003, Issue 3. [Art. No.: CD000255. DOI: 10.1002/14651858.CD000255] [DOI] [PubMed] [Google Scholar]


